Abstract
Studies of aphasia treatment have shown that intensive speech-language therapy is associated with significant improvements. However, there is no standard definition of intensity and the simplistic notion that “more is better” is not necessarily supported by the research. First, current evidence regarding intensity and aphasia treatment was briefly summarized. Second, studies that directly compare conditions of higher- and lower-intensity treatment for aphasia were reviewed with regard to the inclusion of parameters that contribute to a definition of intensity. In addition to five parameters proposed by Warren, Fey and Yoder (2007) and highlighted by Baker (2012), total number of sessions was also often documented. The review illustrated the complexity of quantifying the dose of comprehensive treatments that target multiple modalities and utilize a variety of different strategies. Third, data from a study reporting a relationship between intensive computer-based script training and outcomes in aphasia were examined. Results serve to illustrate Baker’s contention that intensity alone is insufficient without also considering the active ingredients of the teaching episode. Information about dose, therapeutic inputs, and client acts can lead to better optimization of an intervention.
Keywords: Aphasia, treatment, intensity, dose, script training
Introduction
Studies of aphasia treatment have shown that intensive speech-language therapy is associated with significant improvements. Studies have demonstrated the efficacy of Constraint-Induced Language Therapy (CILT), a technique in which massed practice is an integral part of the intervention (Pulvermuller, Neininger, Elbert, Mohr, Rockstroh, Koebbel, & Taub, 2001;) Other studies supporting the efficacy of intensive aphasia therapy have evaluated a single treatment such as Melodic Intonation Therapy administered at a high intensity (Schlaug, Marchina & Norton, 2008, 2009) or comprehensive intensive aphasia programs in which various treatment approaches are individualized to the participant with aphasia (e.g. Code, Torney, Gildea-Howardine, & Willmes, 2010). Further evidence comes from studies that have compared two treatments given at the same high intensity (e.g. Maher, Kendall, Swearengin, Rodriguez, Leon, Pingel, Holland, & Rothi, 2006; Barthel, Meinzer, Djundja, & Rockstroh, 2008). However none of these studies determine the contribution of intensity separate from the treatment protocol and optimal intensity has not yet been established for even one type of aphasia treatment.
Baker (2012) has argued that establishing the optimal intensity of an intervention is an ambitious goal. Not only do clinicians need to know how often to apply an intervention and for how long, they also need to identify the active ingredients and best forms in which to deliver these ingredients. Baker (2012) discusses the problems of defining intensity and suggests that use of a framework derived from Warren, Fey and Yoder (2007) may be an important first step to defining intensity. This paper focuses on the definition of aphasia treatment intensity. After a brief summary of the state of the evidence, it assesses the utility of this framework by applying it to studies that have evaluated the efficacy of intensive treatment. The paper also examines previously published data from a study reporting the relationship between treatment intensity and outcomes in aphasia (Lee, Kaye & Cherney, 2009) to illustrate Baker’s point that intensity alone is insufficient without also considering the active ingredients of the teaching episode.
Aphasia Treatment Intensity: State of the Evidence
Cherney and colleagues (Cherney, Patterson, Raymer, Frymark, & Schooling, 2008, 2010; Cherney, Patterson & Raymer, 2011) conducted a series of systematic reviews of treatment studies that directly compared conditions of higher- and lower-intensity treatment for aphasia. Twenty-five expanded search terms were used to search 15 electronic data bases as well as specific journals and conference proceedings in the area of aphasia. An initial search from 1990–2006 identified six studies (Cherney et al., 2008); a follow-up search from 2007–2011 yielded an additional five studies (Cherney et al., 2010, 2011). Results were discussed in terms of aphasia chronicity (acute vs chronic) and type of outcome measure (language impairment vs communication activity/participation) described by the International Classification of Functioning, Disability and Health (World Health Organization, 2001). Language impairment outcomes included standard aphasia tests of word retrieval, auditory comprehension, and repetition whereas communication activity/participation outcomes included measures of functional real-life use of language in connected speech or communication rating scales. Details of these studies including methodological quality and results have been presented previously (Cherney et al., 2008, 2010, 2011).
Tables 1 and 2 summarize the findings from the 11 studies that span a total of 195 participants with aphasia. Although there is difficulty comparing across studies because of variations in treatment type, dose, and patient characteristics such as aphasia diagnosis and severity, what emerges is that the notion that “more is better” requires “cautious reexamination” (Cherney et al., 2011).
Table 1.
Studies of acute aphasia showing whether results favored intensive or non-intensive treatment or whether they were equivocal
| Study | Results
|
|||
|---|---|---|---|---|
| Intensive | Non-Intensive | Equivocal | ||
| Impairment | ||||
| Bakheit et al. (2007) | + | |||
| Denes et al. (1996) | + | |||
| Activity/Participation | ||||
| No studies | ||||
Table 2.
Studies of chronic aphasia showing whether results favored intensive or non-intensive treatment or whether they were equivocal
| Study | Results
|
|||
|---|---|---|---|---|
| Intensive | Non-Intensive | Equivocal | ||
| Impairment | ||||
| Basso & Caporali (2001) | + | |||
| Harnish et al. (2008) | + | |||
| Hinckley & Craig (1998). | + | |||
| Pulvermuller et al. (2001) | + | |||
| Ramsberger & Marie (2007). | + | |||
| Raymer et al., (2006) | + | |||
| Sage et al., (2011) | + | |||
| Activity/Participation | ||||
| Hinckley & Carr (2005) | + | |||
| Lee et al. (2009). | + | |||
Some studies had several outcomes with some at the impairment level and others at the activity/participation level. Table 2 shows only the major ICF level addressed.
For individuals with acute aphasia, two randomized controlled trials measure language impairment outcomes, with one favoring more intensive treatment (Denes, Perazzolo, Piani, & Piccione, 1996) and the other showing equivocal findings (Bakheit, Shaw, Barrett, Wood, Carrington, Griffiths et al., 2007). Differences in the findings may have resulted from differences in the acuity of the aphasia. Participants were more acute in the Bakheit et al. (2007) study where the mean time post onset was approximately one month. In this study, none of the participants randomized to the intensive treatment group received the designated amount of therapy (5 hrs per week for 12 weeks); many refused or were too ill to tolerate the prescribed treatment, especially in the first 4 weeks, suggesting that intensive treatment may not be feasible in the early acute stage. There are no studies of acute aphasia intervention intensity that have included outcomes at the level of activity/participation.
For individuals with chronic aphasia, four studies favor intensive treatment. Interestingly, in three of these studies, the intervention approach was comprehensive in that it targeted multiple modalities and utilized a variety of different strategies, typically individualized to the person with aphasia’s specific deficits and strengths (Basso & Caporali, 2001; Harnish, Neils-Strunjas, Lamy, & Eliassen, 2008; Hinckley & Craig, 1998). In the fourth study two different treatments were compared at two different intensities (Pulvermuller et al., 2001), although participants randomized to the intensive treatment fared better, a clear statement of the effect of intensity alone cannot be made. In contrast, the studies in which results were equivocal (Ramsberger & Marie, 2007; Raymer, Kohen, & Saffell, 2006) or favored the nonintensive group (Sage, Snell, & Lambon, 2011), utilized a treatment that was more restricted in that it targeted the learning of a specific word list. Differences in the therapy intervention may account for different results across studies.
At the level of communication activity/participation, Hinckley and Carr (2005) found no advantage of intensive treatment over non-intensive treatment for achieving mastery on a catalogue ordering task involving script practice, or in transferring those skills to other environments. In contrast, Lee, Kaye & Cherney (2009) found that amount of treatment per week was significantly correlated with percent change in script content and rate. Furthermore, severity impacted outcomes, illustrating the potential interaction of other variables in the therapeutic process that affect treatment intensity and outcomes.
Dose Parameters in Aphasia Studies
Differences in study outcomes may result partly from lack of a consistent definition of intervention intensity. Particularly intriguing is the suggestion that the concept of intervention intensity comprises five parameters, a notion originally proposed by Warren et al., (2007) and highlighted by Baker (2012). To ascertain the extent to which this concept could apply to intervention intensity in aphasia treatment, the 11 studies included in the systematic reviews of Cherney et al (2008, 2010, 2011) were examined to see which parameters were consistently included in the studies and whether additional parameters were needed..
Table 3 lists each of the studies and the reported dose parameters. Most of the studies reported session duration, session frequency and total intervention duration. However, only three studies reported dose i.e. the number of times a teaching episode containing a unique combination of active ingredients occurs per session. The intervention in each of these studies was a naming treatment where a specific number of words were trained, a sequence of steps to cue responses was carefully delineated, and the number of times that the entire word list would be repeated in a session was specified. For example, Raymer et al. (2006) presented three trials of 20 target words whereas Sage et al. (2011) presented three trials of 30 target words. Since session duration was dependent on the rate at which the participant progressed through the stimuli, this intensity parameter varied and was not always reported.
Table 3.
Dose parameters reported in selected aphasia studies
| Study, Design and Sample Size | Dose Form | Dose | Session Duration | Session Frequency | Total Intervention Duration | Cumulative Intervention Intensity | Other (Total # sessions/hours) |
|---|---|---|---|---|---|---|---|
|
Bakheit et al. (2007) RCT N=51 (Intensive) N=46 (Standard) |
Tasks targeted comprehension and expression of spoken and written language including picture/object selection, picture naming, describing, recognizing associations between items, expressing feelings and opinions, and conversation. | Not reported. | About 1 hour Versus About 1 hour |
5x per week Versus 2x per week |
12 weeks Versus 12 weeks |
Cannot calculate | Total hours should have been 60 hours versus 24 hours. In actuality, mean (SD) total hours were: 35.6 (16.4) Intensive 19.3 (6.4) Standard |
|
Basso & Caporali (2001) Descriptive study N=3 (Intensive) N=3 (Non-Intensive) |
Variety of tasks targeting specific deficits of each subject. | Not reported | 2–3 hours or 3–4 hours Versus 1 hour |
7x per week Versus 5x per week |
14, 40, 14 months respectively Versus 25, 20, 15 months respectively |
Cannot calculate | |
|
Denes et al. (1996) RCT N=8 (Intensive) N=9 (Standard) |
Targeted comprehension and production of oral language within a conversational setting. | Not reported | 45–60 minutes Versus 45–60 minutes |
5x per week Versus 3x per week |
6 months Versus 6 months |
Cannot calculate | In actuality, total number of sessions were: 130 (range 94–160) Intensive 60 (range 56–70) Standard |
|
Harnish et al. (2008) Cross-over study N=1 |
Variety of tasks - confrontation naming; naming from definitions or descriptions; describing pictures using complete sentences, correct pronoun and possessive use during structured activities; word generation with hierarchical cues; writing words to dictation | Not reported. | 1.5 hours versus 1 hour |
5x per week versus 2x per week |
2 weeks versus 7.5 weeks |
Cannot calculate | Total sessions = 15 per phase |
|
Hinckley & Carr (2005) Between groups design. N=8 (Intensive) N=5 (Non-Intensive) |
Context-based treatment approach using a catalogue-ordering task plus other personally relevant tasks such as calling a taxi, contacting a travel agent | Not reported | Not reported | Not reported. 25 hrs per week Versus 4 hours per week |
Not reported. Treatment continued until criterion reached (90% acc. on 3 consecutive probes of the catalogue-ordering task). | Cannot calculate | Mean number of minutes required to achieve criterion: 233 minutes, range 29 minutes – 597 minutes, across both groups. |
|
Hinckley & Craig (1998). Study 3. Retrospective Cross-Over Design N=10 |
Functionalist/Pragmatic approach. Included PACE and use of cuing hierarchies within discourse-based therapy activities. Intensive treatment included individual, group and computer treatment. | Not reported | Not reported | Not reported 23 hours per week Versus 3–5 hours per week |
6 weeks Versus 6 weeks |
Cannot calculate | |
|
Lee et al. (2009). Case series N=17 |
Computer-based practice of three personalized scripts | Not reported | Minimum of 30 minutes | 7x per week | 9 weeks | Cannot calculate | Minimum total hours should have been 31.5 hours. In actuality, mean (SD) total hours = 46.88 (30.75). Range = 17.40 – 151.85 hours |
|
Pulvermuller et al. (2001) RCT N=10 (Intensive) N=7 (Standard) |
Intensive = Constraint- Induced Language Therapy Standard = Conventional therapy including exercises involving naming, repetition, sentence completion, following instructions, and conversations on topics of the patients’ own choice. |
Not reported. | 3–4 hours Versus Not reported |
5x per week Versus Not reported |
10 days Versus 3–5 weeks |
Cannot calculate | In actuality, mean total hours were: 31.5 hours (range 23–33) Intensive 33.9 hours (range 20–54) Standard |
|
Ramsberger & Marie (2007). Cross-over study N=4 |
Cued Naming Module of MossTalk Words (Fink et al., 2001) | Therapeutic inputs = 80 (2 trials of 40 target words) Client acts=80 |
45–60 minutes | 2x per week versus 5x per week |
7.5 weeks (P1, P2) and 10 weeks (P3, P4) versus 3 weeks (P1, P2) and 4 weeks (P3, P4) |
Constant for both phases 1200 (P1, P2) 1600 (P3, P4) |
Total sessions per phase were 15 sessions (P1, P2) and 20 sessions (P3, P4) |
|
Raymer et al., (2006) Cross-over study N=5 |
MossTalk multi-mode matching exercises (spoken and written word/picture matching) paired with spoken rehearsal | Therapeutic inputs = 60 (3 trials of 20 target words) Client acts = 180 (9 productions of each target word) |
Not reported | 1–2x per week versus 3–4x per week |
6–12 weeks versus 3–4 weeks |
Constant for both phases Inputs = 720 Acts = 2160 |
Total sessions for each phase = 12 |
|
Sage et al., (2011) Cross-over study N=8 |
Confrontation naming with progressive orthographic and phonemic cues (up to a maximum of 4 cues per target) | Therapeutic inputs = 90 (3 trials of 30 target words) Client acts = 90 |
Not reported | 2x per week versus 5x per week |
5 weeks versus 2 weeks |
Constant for both phases Inputs = 900 Acts = 900 |
Total sessions for each phase = 10 |
Aphasia studies were previously identified in Cherney et al., (2008, 2010, 2011) as studies that directly compare conditions of higher- and lower-intensity of treatment.
Several studies provided information about the total number of sessions administered, a parameter not included in the Warren et al., (2007) framework. Total number of sessions may be an additional parameter that should be included in the definition of intervention intensity. It becomes increasingly important when session frequency and intervention duration are not explicitly reported because a cumulative intervention intensity can still be calculated (i.e. total number of sessions x dose). For example, Raymer et al (2006) indicated that the lower intensity schedule was 1–2 times a week, the higher intensity schedule was 3–4 times a week, with each phase of the treatment providing a total of 12 sessions. Since dose was also provided, a cumulative intervention intensity could be calculated.
The studies that did not provide information about dose were studies in which the treatment was more comprehensive, targeting multiple modalities and utilizing a variety of different strategies. These studies illustrate the difficulty of determining dose which is dependent on explicitly identifying a teaching episode for a given intervention in a way that allows an episode to be observed and counted (Warren et al., 2007). Warren et al. (2007) acknowledge that this is a challenging task especially for treatments that are “multi-faceted”. Determining dose is further complicated by the need to identify the active ingredients that make up the teaching episode. Baker (2012) stresses the importance of capturing and quantifying the active ingredients within a teaching episode (i.e., the quantity and quality of the therapeutic inputs and the quality and quantity of the client acts or responses), in order to optimize our speech-language pathology interventions. To this end, data from a study in Table 3 that did not provide information on dose (Lee et al., 2009) was reanalyzed to illustrate how information about dose, therapeutic inputs, and client acts can lead to better optimization of an intervention.
Scripting: Examining Dose, Therapeutic Inputs and Client Acts
Table 3 shows that Lee, Kaye & Cherney (2009) reported session frequency, total intervention duration, and total hours of treatment. Although dose was not reported, the study was a computer treatment in which logs of the therapeutic inputs and the participant responses were available. The study is described first followed by presentation and discussion of data from the treatment logs.
Participants received computerized conversational script treatment via a software program called AphasiaScripts™. The AphasiaScripts™ program uses a “virtual therapist” or digital agent who guides the participant through the treatment program and also serves as the conversational partner (Cherney, Halper, Holland & Cole, 2008). For each participant, three personalized scripts were developed, and each was practiced sequentially for three weeks. Therefore, the total intervention duration for each participant was nine weeks.
Each treatment session included three parts: First, participants listened to the entire script of the conversation; second, participants repeatedly practiced each sentence of their part of the conversation; and third, the entire conversation was rehearsed in turn-taking with the “virtual therapist”. During the sentence practice, a specific sequence of tasks occurred for each sentence including pointing to each word of the sentence, choral reading of the sentence, and independent reading aloud of the sentence. A component of the sentence practice sequences allows the participants to choose to listen to their choral and independent productions of the sentences.
Participants used the treatment program at home. They were instructed to practice a minimum of 30 minutes a day, 7 days a week. They were also instructed to listen only one time per practice session to the conversation. After that, they should control their own treatment session, self- selecting which parts of the program to practice.
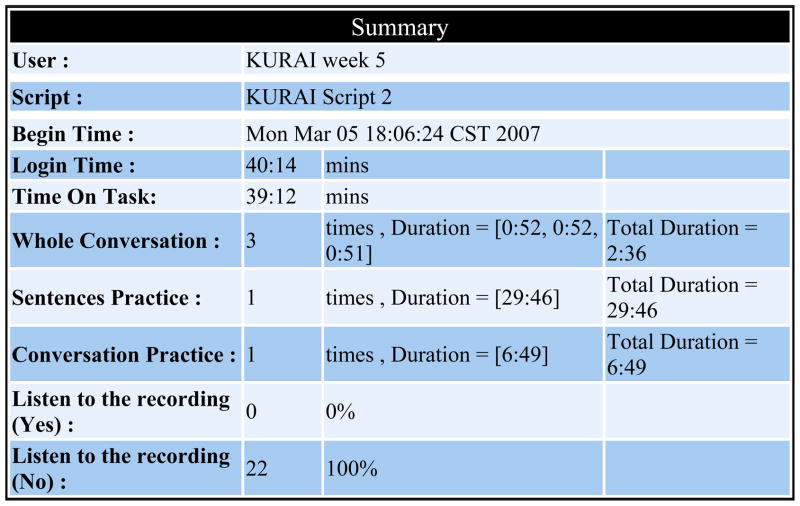
The computer program automatically provided a daily log of the amount of time spent by the participant in each part of the treatment. Figure 1 is an example. For this particular session, KURAI listened to the conversational script three times, spending a total of 2 minutes and 36 seconds on this part of the program. She practiced each of the sentences of the conversation once, which took 29 minutes and 46 seconds. She practiced the whole conversation once, which took 6 minutes, 49 seconds. During the sentence practice, she had 22 opportunities to listen to a recording of her sentence production, but she chose not to listen to any of them.
Figure 1.
Computer generated practice log showing one practice session
The computer-generated treatment log for each session also differentiated the amount of time the participant was logged into the program and the amount of time that he or she was actually engaged on a task (“Time on Task”). The participant’s active engagement in the treatment task could be measured because he or she was required to push the space bar to advance to the next sentence or part of the program. Any delay in advancing the program was measured as “pause time”. According to this log, KURAI was logged in for 40 minutes 14 seconds, with a time on task of 39 minutes 12 seconds. Using the daily logs and the weekly summary of participant treatment time (as illustrated in Figure 2), computer generated logs of 10 subjects were examined to answer some questions regarding the relationship between dose and change in performance.
Figure 2.
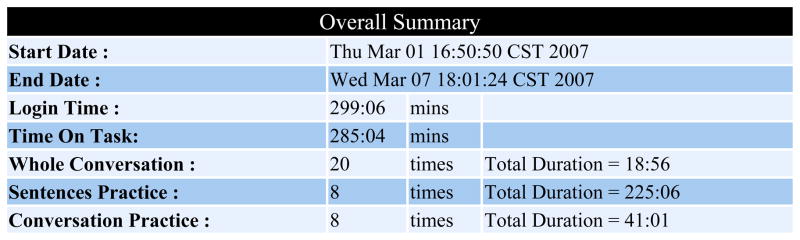
Computer-generated weekly summary
Performance was measured for content and rate. For each script, three baseline recordings of script performance were taken prior to treatment and one recording was taken following the three weeks of treatment on that script. Recordings of script performance were timed and transcribed. They were then scored for content i.e., percent of all words said by the participant that were in the target script; and rate i.e., number of script related words produced per minute. The percent change was calculated as the difference from the mean of the baseline to post treatment over the mean baseline score. The total hours practiced over all nine weeks in relation to the percent change in content and rate has been previously reported. However, the amount of time spent on each part of the treatment program in relation to change is new data. These data are presented in Table 4.
Table 4.
Distribution of practice time for 10 subjects from Lee, Kaye & Cherney, 2009.
| Subject | WAB AQ | % Change | Total Hours Practiced | % Practice Time | |||
|---|---|---|---|---|---|---|---|
| Content | Rate | Listen to Conv. | Sentence Practice | Conv. Practice | |||
| FITMA | 30.5 | 2.63 | −4.02 | 39.72 | 19.28 | 77.80 | 2.92 |
| PERMA | 34.1 | 235.28 | 425.67 | 68.61 | 9.37 | 66.92 | 23.71 |
| KURAI | 46.2 | 71.61 | 151.81 | 44.45 | 7.86 | 74.61 | 17.53 |
| SCHRO | 64.7 | 36.97 | 31.27 | 47.16 | 5.92 | 87.05 | 7.03 |
| AMACH | 64.9 | 34.53 | 43.84 | 40.41 | 3.94 | 76.01 | 20.05 |
| HEIED | 65.6 | 91.12 | 83.44 | 66.05 | 6.49 | 74.57 | 18.94 |
| DOWMI | 75.3 | 14.60 | 156.40 | 30.79 | 8.22 | 73.84 | 17.94 |
| WILPA | 75.3 | 15.38 | 130.76 | 17.40 | 18.17 | 69.08 | 12.75 |
| SCHBA | 76.8 | 0.74 | 25.69 | 21.38 | 5.81 | 14.99 | 79.20 |
| LUESH | 77.0 | 12.73 | 65.90 | 19.08 | 16.35 | 64.90 | 18.75 |
It was previously reported that all subjects demonstrated some improvement in content and rate except for one subject, FITMA who had the most severe aphasia (WAB AQ 30.5). However, another subject with a similarly severe aphasia (WAB AQ 34.1) demonstrated the greatest amount of improvement of all subjects in both content (increased 235.28%) and rate (increased 425.67%). Table 4 allows a comparison of the times spent by FITMA and PERMA on each part of the AphasiaScripts™ program. A very different practice pattern emerges. While both participants spent the largest percent of their time on the sentence practice, FITMA also spent a large percent of her time listening to the scripts with little time engaged in conversational practice. In contrast, PERMA spent relatively little time listening to the conversation and more time engaged in conversational practice.
Admittedly, PERMA practiced many more hours than FITMA. Therefore, comparing FITMA’s practice pattern to that of others who practiced about the same total number of hours (e.g. KURAI) or fewer hours (e.g. DOWMI) is also revealing. Both KURAI and DOWMI had made large changes in the content and rate of their scripts. Not surprisingly, their distribution of practice hours was similar to PERMA, with less time devoted to listening to the conversation and more time devoted to conversation practice. Again, the largest proportion of time was devoted to the sentence practice.
Table 4 shows that only one subject did not devote most of his practice time to sentence practice. SCHBA spent an excessive amount of time with the conversational practice (79.2%) with very little time in the sentence practice part of the program (14.99%). It is noted that after FITMA, SCHBA made the least amount of change - almost negligible change for content and the smallest positive change of all the participants for rate (25.69%).
To rule out variables such as severity of aphasia, a comparison of SCHBA’s practice pattern to two other subjects of similar severity is appropriate. WILPA and LUESH practiced fewer hours than SCHBA overall but still made improvements. They spent most of their treatment time with sentence practice (69.08% and 64.90% respectively). Listening to the conversation and conversation practice time was about equally distributed for LUESH (16.35 and 18.75%); distribution for WILPA was 18.17% for listening to the conversation and 12.75% for conversation practice, much less than the 79.20% of time that SCHBA spent on conversation practice.
These data suggest that there may be an optimum combination of the parts of the treatment program that contribute to best outcomes, with most of the treatment time being devoted to sentence practice; of the remaining time, less should be devoted to listening to the conversation and more should be devoted to conversation practice. Excluding the poor responders of FITMA and SCHBA, the mean practice time distribution for the remaining eight subjects is as follows: Listening to conversation is 9.54% (range 3.94 – 18.17); sentence practice is 73.37% (range 64.90 – 87.05); conversation practice is 17.09% (range 7.03 – 23.71). These data indicate that sentence practice is likely the active ingredient of the treatment, and may guide future research to determine optimum dose as well as current clinical applications of AphasiaScripts™.
Table 5 shows further analysis of FITMA’s treatment data. Although she did not show improvement overall when the change data was averaged for all three scripts, she did demonstrate improvement for Script 1. Performance decreased on Script 2 even though it was practiced about the same number of hours as Script 2. Script 3 was practiced for more hours than either Script 1 or 2, with some improvement occurring in content but with decreased rate. Script data in Table 5 includes not only the distribution of time spent with each part of the treatment program, but also the actual number of therapeutic inputs and participant acts (# items practiced).
Table 5.
Percent practice time and number of items practiced for each of FITMA’s scripts.
| FITMA SCRIPT | % Change | Total Hours Practiced | % Practice Time - # items practices | Listened to Productions | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Content | Rate | Listen to Conv. | Sentence Practice | Conv. Practice | Yes | No | |||||
| 1 | 15.38 | 25.70 | 11.67 | 23.64 | 86 | 73.22 | 49 | 3.14 | 9 | 11 | 248 |
| 2 | −20.00 | −2.51 | 11.8 | 18.64 | 61 | 79.10 | 25 | 2.26 | 9 | 176 | 177 |
| 3 | 12.50 | −35.25 | 16.23 | 16.58 | 53 | 80.19 | 23 | 3.23 | 16 | 230 | 210 |
Comparing Script 1 to the other scripts, many more items were practiced during sentence practice (49 for script 1 compared to 25 and 23 for scripts 2 and 3 respectively). Further analysis shows that FITMA was able to practice more sentences because less time was spent listening to her productions. Out of 259 opportunities, she listened to only 11 of her productions (4.2%), whereas she listened to about 50% of her productions in scripts 2 and 3. These data suggest that for FITMA, the essential teaching episodes occurred during sentence practice, with the actual production of the sentence being the active ingredient.
Conclusion
Determining the optimal intensity of treatment is essential to the design and implementation of any treatment program for aphasia. Currently there is no standard definition of intensity although levels have been artificially created from metaanalyses and retrospective reviews of the prevailing literature. The simplistic notion that “more is better” is not necessarily supported by the evidence. Optimal intensities may vary depending on the type of intervention, and the specific stimuli given and responses required of the participant. Additionally, participant characteristics and environmental variables impact treatment intensity and outcomes, further complicating the determination of optimal treatment intensity.
Baker’s (2012) thought-provoking and insightful article on treatment intensity has highlighted many of the issues involved in establishing the optimal intensity of an intervention. Baker asks whether it is possible to define, study and measure speech and language interventions in discrete doses. Having a common definition of intensity by utilizing the parameters suggested by Warren et al., (2007) - perhaps with the addition of total number of treatment sessions - is a first step towards achieving this goal. Quantification of stimuli and responses integral to an intervention and measurement of the essential elements or active ingredients that are necessary to bring about positive change can be accomplished, as illustrated by the data presented on AphasiaScripts™. In response to Baker’s question, certainly this is a worthy and possible goal for aphasiologists, both researchers and practitioners alike, to strive for.
Acknowledgments
Supported in part by Grant 1R01 DC011754 from the National Institute on Deafness and Other Communication Disorders, National Institutes of Health.
References
- Baker E. Optimal Intervention Intensity. International Journal of Speech-Language Pathology. 2012;14:401–409. doi: 10.3109/17549507.2012.700323. [DOI] [PubMed] [Google Scholar]
- Bakheit AM, Shaw S, Barrett L, Wood J, Carrington S, Griffiths S, et al. A prospective, randomized, parallel group, controlled study of the effect of intensity of speech and language therapy on early recovery from poststroke aphasia. Clinical Rehabilitation. 2007;21(10):885–894. doi: 10.1177/0269215507078486. [DOI] [PubMed] [Google Scholar]
- Barthel G, Meinzer M, Djundja D, Rockstroh B. Intensive language therapy in chronic aphasia: which aspects contribute most? Aphasiology. 2008;22(4):408–421. [Google Scholar]
- Basso AA, Caporali A. Aphasia therapy or the importance of being earnest. Aphasiology. 2001;15:307–332. [Google Scholar]
- Cherney LR, Halper AS, Holland AL, Cole R. Computerized Script Training for Aphasia: Preliminary Results. American Journal of Speech-Language Pathology. 2008;17:19– 34. doi: 10.1044/1058-0360(2008/003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherney LR, Patterson JP, Raymer AS. Intensity of Aphasia Therapy: Evidence and efficacy. Current Neurology and Neuroscience Reports. 2011;11(6):560–569. doi: 10.1007/s11910-011-0227-6. [DOI] [PubMed] [Google Scholar]
- Cherney LR, Patterson J, Raymer A, Frymark T, Schooling T. Evidence-Based Systematic Review: Effects of Intensity of Treatment and Constraint-Induced Language Therapy for Individuals with Stroke-Induced Aphasia. Journal of Speech, Language, and Hearing Research. 2008;51:1282–1299. doi: 10.1044/1092-4388(2008/07-0206). [DOI] [PubMed] [Google Scholar]
- Cherney LR, Patterson J, Raymer A, Frymark T, Schooling T. Updated evidence-based systematic review: Effects of Intensity of Treatment and Constraint-Induced Language Therapy for Individuals with Stroke-Induced Aphasia. Rockville Pike, MD: American Speech-Language-Hearing Association; 2010. [Accessed 2nd April 2012]. Available online at http://www.asha.org/uploadedFiles/EBSR-Updated-CILT.pdf. [DOI] [PubMed] [Google Scholar]
- Code C, Torney A, Gildea-Howardine E, Willmes K. Outcomes of a one-month therapy intensive for chronic aphasia: variable individual responses. Seminars in Speech and Language. 2010;31:21–33. doi: 10.1055/s-0029-1244950. [DOI] [PubMed] [Google Scholar]
- Denes G, Perazzolo C, Piani A, Piccione F. Intensive versus regular speech therapy in global aphasia: A controlled study. Aphasiology. 1996;10:385–394. [Google Scholar]
- Harnish SM, Neils-Strunjas J, Lamy M, Eliassen JC. Use of fMRI in the study of chronic aphasia recovery after therapy: a case study. Topics in Stroke Rehabilitation. 2008;15(5):468–483. doi: 10.1310/tsr1505-468. [DOI] [PubMed] [Google Scholar]
- Hinckley JJ, Craig HK. Influence of rate of treatment on the naming abilities of adults with chronic aphasia. Aphasiology. 1998;12:989–1006. [Google Scholar]
- Hinckley JJ, Carr T. Comparing the outcomes of intensive and non-intensive context-based aphasia treatment. Aphasiology. 2005;19:965–974. [Google Scholar]
- Lee JB, Kaye RC, Cherney LR. Conversational script performance in adults with non-fluent aphasia: Treatment intensity and aphasia severity. Aphasiology. 2009;23(7):885–897. [Google Scholar]
- Maher L, Kendall D, Swearengin J, Rodriguez A, Leon S, Pingel K, Holland A, Rothi L. A pilot study of use-dependent learning in the context of constraint induced language therapy. Journal of the International Neuropsychological Society. 2006;12:843–852. doi: 10.1017/S1355617706061029. [DOI] [PubMed] [Google Scholar]
- Meinzer M, Rodriguez AD, Rothi LJG. First decade of research on constraint-induced treatment approaches for aphasia rehabilitation. Archives of Physical Medicine and Rehabilitation. 2012;93:S33–45. doi: 10.1016/j.apmr.2011.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulvermuller FB, Neininger B, Elbert T, Mohr B, Rockstroh B, Koebbel P, Taub E. Constraint-induced therapy of chronic aphasia after stroke. Stroke. 2001;32:1621–1626. doi: 10.1161/01.str.32.7.1621. [DOI] [PubMed] [Google Scholar]
- Ramsberger G, Marie B. Self-administered cued naming therapy: a single-participant investigation of a computer-based therapy program replicated in four cases. American Journal of Speech Language Pathology. 2007;16(4):343–358. doi: 10.1044/1058-0360(2007/038). [DOI] [PubMed] [Google Scholar]
- Raymer A, Kohen F, Saffell D. Computerised training for impairments for word comprehension and retrieval in aphasia. Aphasiology. 2006;20:257–268. [Google Scholar]
- Sage K, Snell C, Lambon Ralph MA. How intense does anomia therapy for people with aphasia need to be? Neuropsychological Rehabilitation. 2011;21:26–41. doi: 10.1080/09602011.2010.528966. [DOI] [PubMed] [Google Scholar]
- Schlaug G, Marchina S, Norton A. From singing to speaking: Why singing may lead to recovery of expressive language function in patients with Broca’s aphasia. Music Perception. 2008;25:315–323. doi: 10.1525/MP.2008.25.4.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlaug G, Marchina S, Norton A. Evidence for plasticity in white matter tracts of patients with chronic Broca’s aphasia undergoing intense intonation-based speech therapy. Annals of the New York Academy of Sciences. 2009;1169:385–394. doi: 10.1111/j.1749-6632.2009.04587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren SF, Fey ME, Yoder PJ. Differential treatment intensity research: A missing link to creating optimally effective communication interventions. Mental Retardation and Developmental Disabilities Research Reviews. 2007;13:70–77. doi: 10.1002/mrdd.20139. [DOI] [PubMed] [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva, Switzerland: WHO; 2001. [Google Scholar]