Abstract
Purpose
It has been known that inflammatory mechanisms play an important role in the coronary artery disease. Our aim in this study was to investigate the relationship between the neutrophil/lymphocyte (N/L) ratio and coronary flow velocity after primary percutaneous coronary intervention (PCI) in patients presenting with ST-segment elevation myocardial infarction (STEMI).
Methods
Two hundred and ten patients who had undergone primary PCI were included. The coronary flow velocities were evaluated using the recorded PCI procedures by Thrombolysis in Myocardial Infarction (TIMI) flow grades and corrected TIMI frame counts (cTFC) values. A value of >40 for the final cTFC was accepted as an index of insufficient coronary blood flow. The white blood cell subtypes and counts were determined in the blood samples obtained at the clinics.
Results
In 165 (78%) of the investigated patients, reperfusion was found to be sufficient (Group I) while in 45 (22%) of them (Group II) insufficient reperfusion was observed (Group II). In-hospital mortality was 7.2% (n=12) in Group I, whereas it was 17.7% (n=8) in Group II (P=0.033). Similarly, one-year mortality was higher in Group II (26.6%, n=12) than in Group I (13.3%, n=22) (P=0.031). N/L ratio was determined to be higher in Group I than in Group II (8.3±6.1 vs. 6.2±5.0; P=0.034). Also, N/L ratio was found as an independent predictor of severe no-reflow development (TIMI 0-1) and of one-year mortality (P=0.01 and P=0.047, respectively).
Conclusions
N/L ratio has been found to be an independent indicator for no-reflow development in patients who have undergone PCI for acute STEMI. This simple and low-cost parameter can provide useful information for the relevant risk evaluation in these patients.
KEY WORDS : Inflammation, acute ST-segment elevation myocardial infarction (acute STEMI), neutrophil/lymphocyte ratio (N/L ratio)
Introduction
It has been known for some time that inflammatory processes play a major role in coronary artery disease (1,2). This pathophysiology provides the basis for estimating some inflammatory indicators as predictors in the progression of coronary artery disease. Acquisition of prognostic information through white blood cell (WBC) counts in cardiac patients had been shown in earlier studies (3,4). Recently, neutrophil/lymphocyte (N/L) ratio has been shown to provide a reliable inflammatory index to be used in the coronary artery disease for prognostic stratification (5,6).
Coronary no-reflow phenomenon was described as the inability to obtain normal coronary flow (TIMI 3) or electrocardiographic ST segment resolution after coronary intervention. Many studies showed that it was related to poor prognosis and increased mortality (7-10). It continues to be one of the major fears of invasive cardiologists during primary percutaneous coronary intervention (PCI) despite recent advances in the procedural techniques and medications. Some researchers pay attention to the relation of this phenomenon with increased inflammatory status (11-13). Therefore, we aimed to evaluate the relationship between development of no-reflow and N/L ratio.
Methods
In this study, 210 consecutive patients with ST-segment elevation myocardial infarction (STEMI) who underwent primary PCI within 12 hours after diagnosis were included. Mean age was 58±12 years and 75% of them were male. The definition of STEMI was based on the criteria of the classic symptoms of coronary ischemia and detection of a 1-mm ST-segment elevation in the inferior leads, or a 2-mm ST-segment elevation in the anterior chest leads occurring in two contiguous leads, or on the presence of a new (or presumably new) left bundle branch block. Patients with active infection or previously proven systemic inflammatory disease, known malignancy, advanced stage liver or renal disorders were excluded from the study.
Angiographic analyses
The recorded angiographic parameters were analyzed by two experienced interventional cardiologists, blinded to the clinical data of the patients. The coronary angiograms were acquired at 15 frames/second with a digital angiographic system (ACOM.PC; Siemens AG, Germany). Data were then converted to the most common filming speed of 30 frames/second by multiplying with a factor of two. TIMI flow grades, TFC values and the degree of stenosis were measured by Quantitative Coronary Arteriography. TIMI flow grades and corrected TIMI frame counts (cTFC) values were measured by previously described methods (14). cTFC was regarded as 100 for flows not reaching the distal reference point (15).
At the completion of primary PCI, determination of a cTFC value of >40 in the concerned artery was taken to indicate insufficient reperfusion, while a value <40 was accepted to indicate sufficent reperfusion (14). Accordingly, the patients were subdivided into Group I (i.e., those who regained sufficient reperfusion) and Group II (i.e., those who could not). Further, those who had coronary flow indices of ‘TIMI 0 and 1’ were accepted to have severe no-reflow status.
The patients’ clinical and follow-up information was obtained during the patients’ visits to the clinic or by telephone interviews conducted 12 months after index PCI.
Laboratory analyses
From all patiens included in the study, blood samples were taken via the antecubital vein after arriving the emergency department. Automated cell counts and subtyping had been performed in these blood samples and N/L ratios were automatically calculated by loading all the data to the statistical program used.
Statistical analyses
All data were loaded to the SPSS 15 program. Subsequently, normal distribution of the data was tested using the Kolmogorov-Smirnov test. Datas were logarithmically transformed before analysis when distribution of the data was not normal. Group means for continuous variables were compared using independent-samples t test Comparison of categorical values was carried out by the chi-square test. Any correlation between the data was tested by the Pearson correlation analysis. Logistic regression analysis was used to test the indicative significance of the data on the final coronary flow velocity. The forward selection technique was preferred in the elimination of variables. While the continuous data were expressed with ‘mean ± SD (standard deviation)’, the categorical data were expressed with percentage values and a P value of <0.05 was accepted as statistically significant.
Results
Of the 210 patients, 165 (Group I, mean age 57.8±12.9 years, 76% males) had sufficient coronary flow while 45 (Group II, mean age 62±13.4 years, 67% males) had insufficient flow on the basis of final reperfusion sufficiency. The basal characteristics of the patients have been summarised in Table 1.
Table 1. Baseline characteristics.
| Group I final cTFC ≤40 [n=165] | Group II final cTFC>40 [n=45] | P | |
|---|---|---|---|
| Age [years] | 57.8±12.9 | 62±13.4 | 0.065 |
| Men [%] | 125 [75.7] | 30 [66.6] | 0.132 |
| Hypertension [%] | 76 [46.0] | 26 [57.7] | 0.186 |
| Diabetes mellitus [%] | 38 [23.0] | 11 [24.4] | 0.842 |
| Smoke [%] | 92 [55.7] | 20 [44.4] | 0.177 |
| High-sensitivity C-reactive protein [mg/L] | 39.3±49.9 | 54.4±61.4 | 0.103 |
| Total cholesterol [mg/dL] | 176.6±41.2 | 172.0±47.3 | 0.496 |
| Serum glucose [mg/dL] | 175.8±90.7 | 221.1±143.8 | 0.048 |
| Hemoglobin [g/L] | 14.0±1.8 | 13.7±2.0 | 0.261 |
| Platelet [mm3] | 247.9±75.6 | 249.1±75.3 | 0.863 |
| White blood cell count [103/µL] | 12.47±4.8 | 12.3±3.7 | 0.790 |
| Neutrophil/lymphocyte ratio | 6.2±5.0 | 8.3±6.1 | 0.017 |
| Glycoprotein IIb/IIIa antagonist [%] | 19 [12] | 10 [22] | 0.065 |
| Pain-to-balloon time [hours] | 4.12±1.1 | 4.9±1.6 | <0.001 |
| Infarct-related coronary artery | 0.404 | ||
| Left anterior descending artery | 73 [44] | 19 [42] | 0.907 |
| Circumflex coronary arter | 21 [12] | 3 [7] | 0.385 |
| Right coronary artery | 71 [43] | 23 [51] | 0.425 |
| Primary percutaneous coronary intervention | |||
| Stent length [mm] | 16.3±4.3 | 18.1±4.0 | 0.024 |
| Stent diameter [mm] | 3.1±0.3 | 3.3±0.6 | 0.114 |
| In-hospital mortality [%] | 12 [7.2] | 8 [17.7] | 0.033 |
| 1-year mortality [%] | 22 [13.3] | 12 [26.6] | 0.031 |
Total blood counts of the patients with respect to neutrophils, eosinophils, monocytes ve basophils were similar. However, the lymphocyte ratio in Group I were higher than in Group II (18.6±11.4% vs. 14.2±9.6%, P=0.007) and N/L ratio was lower in Group I (6.2±5.0 vs. 8.3±6.1, P=0.017) (Figure 1). The N/L ratio of all patients included in the study was 6.5±5.2.
Figure 1.
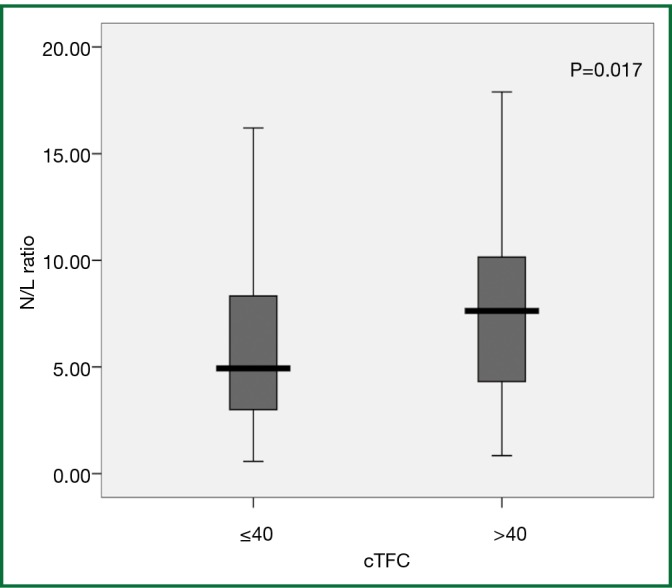
Neutrophil/lymphocyte ratio of the patients according to cTIMI frame counts.Student t test test was used to compare neutrophil/lymphocyte ratios between groups after logarithmic transformation.
Although incidences of diabetes mellitus were similar in both groups, the glucose level of Group II patients was significantly higher (221.1±143.8 vs. 175.8±90.7 mg/dL, P=0.048). The diameters of the stents used for PCI in the two groups were similar (3.1±0.3 mm in Group I and 3.3±0.6 mm in Group II, P=0.114), but the lengths of the stents used in Group I were 16.3±4.3 mm compared to 18.1±4.0 mm in Group II (P=0.024). Lastly, the pain-to-balloon time in Group I patients had been significantly shorter than in Group II (4.12±1.1 vs. 4.9±1.6 hours, P<0.001). Both in-hospital mortality and one-year mortality was higher in Group II (P=0.033 and P=0.031, respectively).
Significant positive correlation was demonstrated between serum N/L ratio and final cTFC values in all patients (r=0.161, P=0.019) (Figure 2). Significant correlation was also demonstrated between final cTFC value and age, pain-to-balloon time, initial cTFC value, post-wire flow, high sensitive C-reactive protein (hs-CRP) concentrations, and lympchocyte counts (Table 2).
Figure 2.
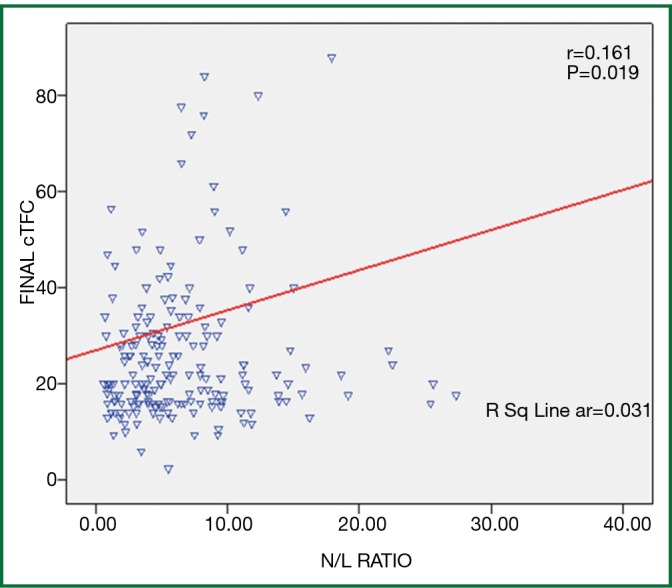
Correlation of final cTFC with neutrophil/lymphocyte ratio (r=0.161, P=0.019). Pearson correlation was used to assess the relation between final cTFC and neutrophil/lymphocyte ratio.
Table 2. Corelation of Final cTFC and other paramethers.
| Correlation coefficient | P | |
|---|---|---|
| Age | 0.165 | 0.017 |
| Creatinin | 0.096 | 0.167 |
| Pain-to-balloon time | 0.240 | 0.026 |
| Stent diameter | 0.147 | 0.780 |
| Stent length | 0.104 | 0.215 |
| Serum glucose | 0.028 | 0.689 |
| High-sensitivity C-reactive protein | 0.183 | 0.034 |
| White blood cell count | –0.040 | 0.566 |
| Lymphocytes | –0.197 | 0.004 |
| Neutrophils | 0.034 | 0.627 |
| Neutrophil/lymphocyte ratio | 0.161 | 0.019 |
| Hemoglobin | –0.080 | 0.246 |
| Mean platellet volume | 0.010 | 0.888 |
| TIMI flow at the beginning | –0.295 | 0.008 |
| cTFC at the beginning | 0.228 | 0.001 |
| Post wire TIMI flow | 0.301 | 0.050 |
According to the multivariate logistic regression analyses made, N/L ratio above 7.5 (OR: 5.072; 95% CI: 1.443-17.828; P=0.011) and serum glucose level (OR: 1.007; 95% CI: 1.001-1.014; P=0.022) were observed to be independent predictors for the development of no-reflow phenomenon. Also, patient’s age (OR: 1.104; 95% CI: 1.035-1.179; P=0.003), serum glucose level (OR: 1.008; 95% CI: 1.002-1.013; P=0.005) and serum creatinine level (OR: 4.692; 95% CI: 1.841-11.959; P=0.001) were found to be independent predictive indices of in-hospital mortality. Patient’s age (OR: 1.079; 95% CI: 1.034-1.125; P<0.001), serum glucose level (OR: 1.005; 95% CI: 1.001-1.009; P=0.009), serum creatinine level (OR: 2.294; 95% CI: 1.066-4.939; P=0.034), and N/L ratio above 7.5 (OR: 2.707; 95% CI: 1.013-7.239; P=0.047) were determined to be independent predictive indices for mortality within one year (Table 3).
Table 3. Effects of various variables on no-reflow and mortality in multivariate logistic regression analyses.
| Dependent variables | Covariates | Adjusted OR | 95% CI | P |
|---|---|---|---|---|
| No-reflow | N/L ratio >7.5 | 5.072 | 1.443-17.828 | 0.011 |
| Serum glucose | 1.007 | 1.001-1.014 | 0.022 | |
| In-hospital mortality | Age | 1.104 | 1.035-1.179 | 0.003 |
| Serum glucose | 1.008 | 1.002-1.013 | 0.005 | |
| Serum creatinin | 4.692 | 1.841-11.959 | 0.001 | |
| 1 year mortality (%) | N/L ratio >7.5 | 2.707 | 1.013-7.239 | 0.047 |
| Age | 1.079 | 1.034-1.125 | <0.001 | |
| Serum Glucose | 1.005 | 1.001-1.009 | 0.009 | |
| Serum Creatinin | 2.294 | 1.066-4.939 | 0.034 |
Multivariate logistic-regression analysis that included potential confounders (N/L ratio, age, serum glukoz, serum creatinin, male gender, mean platelet volume, hemoglobin, hypertension, smoking) for No-reflow, in-hospital mortality and 1 year mortality.
The ROC statistical analyses made showed that N/L ratio above 7.5 had 70% specificity with 72% sensitivity for the development of no-reflow status (Figure 3). When the patients were regrouped on the basis of this cut-off ratio, it was found that in the patients with N/L ratios above 7.5 the final cTFC values were higher than the patients with N/L ratios below 7.5 (39.6±31.2 vs. 29.1±21.2, P=0.023). Further, 30-day and 1-year mortality incidences and the incidence of no-reflow were higher in the group with high N/L ratios (Table 4).
Figure 3.
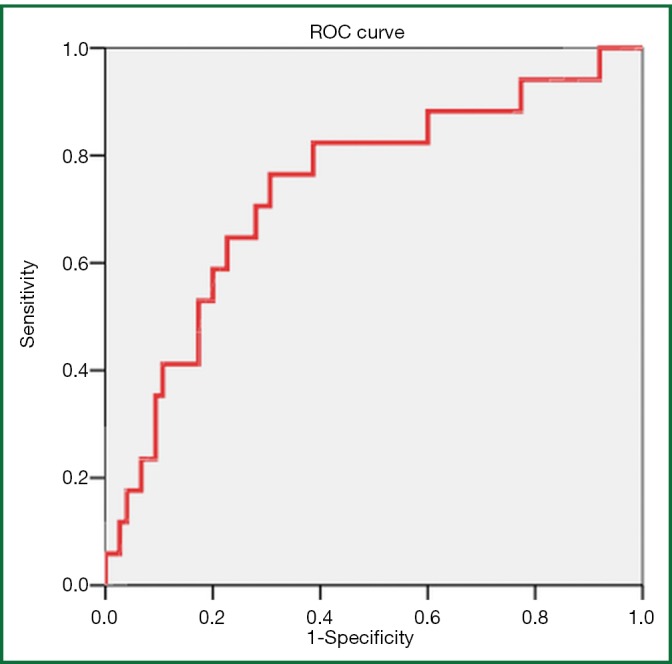
ROC analysis of N/L ratio data for severe no-reflow (AUC=0.737).
Table 4. Clinical and angiographic parameters according to N/L ratio (high or low).
| N/L ratio <7.5 (n=139) | N/L ratio ≥7.5 (n=71) | P | |
|---|---|---|---|
| Spontaneous recanalization (%) | 55 (39.5) | 26 (36.6) | 0.677 |
| cTFC at the beginning | 81.2±30.7 | 82.6±29.5 | 0.629 |
| TIMI flow at the beginning (%) | |||
| 0 | 85 (61.2) | 45 (63.4) | 0.753 |
| 1 | 10 (7.2) | 7 (9.8) | 0.503 |
| 2 | 29 (20.8) | 14 (19.7) | 0.846 |
| 3 | 15 (10.8) | 5 (7.1) | 0.381 |
| Postwire cTFC | 72.1±34.6 | 73.3±33.1 | 0.773 |
| cTFC after balloon angioplasty | 35.4±25.7 | 44.2±32.1 | 0.149 |
| Stenosis at the beginning (%) | 95.7±14.0 | 97.2±10.6 | 0.481 |
| Final cTFC | 29.1±21.2 | 39.6±31.2 | 0.023 |
| Severe No-reflow (TIMI 0-1) (%) | 6 (4.3) | 11 (15.4) | 0.005 |
| cTFC >40 (%) | 20 (14.4) | 21 (29.6) | 0.009 |
| In-hospital mortality (%) | 9 (6.4) | 11 (15.4) | 0.035 |
| 1 year mortality (%) | 15 (10.7) | 19 (26.7) | 0.003 |
Discussion
Up-to-date cardiology guidelines recommend mechanical techniques to restore coronary flow and reestablish myocardial perfusion in patients presenting with STEMI (16). Despite improvements in the techniques and materials used, the performance of primary PCI fails to normalize the coronary flow and myocardial perfusion in some of these patients. This phenomenon described as no-reflow is associated with an increased mortality as well as morbidity (17,18).
The aim during primary PCI is to achieve TIMI 3 flow in the occluded artery. However, this target is semi-quantitative and not objective. It cannot provide an objective discrimination between flows of TIMI 2 and 3. TIMI frame count is a quantitative and objective method to evaluate the coronary flow. In earlier works, the final cTFC values achieved by PCI had been demonstrated to be reliable indices of myocardial perfusion and size of the myocardial infarct (19,20). In our work, the coronary flow was evaluated by cTFC and cTFC value of >40 was taken as an indication of insufficient perfusion (14).
Studies have suggested possible mechanisms for no-reflow phenomenon such as endothelial ischemic damage, microvascular obstruction, leukocyte occlusions, mechanical compression due to interstitial oedema, reactive oxygen radicals and coagulation (21,22). Research also demonstrated the relationship of inflammation to no-reflow. Akpek et al. reported that N/L ratio and CRP had a significant and positive correlation with no-reflow in STEMI patients treated with PCI (12). Oduncu et al. showed that in STEMI patients treated with PCI, basal CRP levels were higher in patients developing no-reflow, while previous use of statins decreased the incidence of no-reflow (13). In our study, patients with insufficient final coronary flow had significantly elevated N/L ratios (8.3±6.1 vs. 6.2±5.0, P=0.017) and decreased lymphocyte ratio (14.2±9.6% vs. 18.6±11.4%, P=0.007). In addition, a significant correlation was present between final coronary flow and N/L ratio, and neutrophil and lymphocyte counts which suggested a relationship between the inflammatory response and leukocyte occlusions. Further, the possible contribution of duration of occlusion to the development of no-reflow has been demonstrated (23). In our study, a significant positive correlation between pain-to-balloon time and final cTFC has been determined. This suggests that a longer occlusion period will cause further microvascular damage and therefore worse final flow rates.
The results presented here showed that N/L ratio above 7.5 was an independent predictor for severe no-reflow (TIMI 0-1) development and mortality within one year. N/L ratio above 7.5 had 70% specificity with 72% sensitivity for the development of no-reflow phenomenon. Akpet et al. reported a cut-off value of 3.3 for the N/L ratio with 74% specificity and 83% sensitivity for no-reflow development (12). The different results may arise from the disparities in the methodology used or in the baseline clinical characteristics of the patients. In the literature, clinical value of N/L ratio was evaluated not only in no-reflow phenomenon but also in different STEMI patient groups. Sahin et al. found that N/L ratio of STEMI patients with a high Syntax score (>18) was also higher in comparison to N/L ratio of patients with a relatively lower Syntax score (<11) (6.5±3.9 vs. 4.0±2.9) (24). While Zazula et al. reported high N/L ratios of 6.9±5.7 in STEMI patients (25), Nunez et al. determined N/L ratios of 3.7 (2.4-6.7) in the same patient group (26).
Taking the cut-off value obtained in our study, patients with high N/L ratios had an increased incidence of worse final cTFC, severe no-reflow, and 30-day and 1-year mortality. In recently published studies, it was also shown that high N/L ratio was associated with increased mortality and major adverse cardiac events in patients with STEMI (5,27-29). Han et al. found that high N/L ratio in STEMI patients undergoing PCI was an independent predictor for 12-month MACE (29). Similarly, Muhammed Suliman et al. reported that mortality was higher among acute coronary syndrome patients with high N/L ratios (27). In our study, N/L ratio above 7.5 was an independent predictor for mortality within 1 year. Age, serum creatinine and glucose levels were also determined to be independent predictors for in-hospital and 1-year mortality.
C-reactive protein is a nonspecific acute phase reactant released from the liver into the bloodstream. CRP levels have been shown to be elevated during acute coronary syndromes (30,31). Ndrepepa et al. showed that CRP was an independent predictor for no-reflow development in STEMI patients treated with PCI (32). On the other hand, Niccoli et al. found similar final cTFC values and clinical no-reflow incidences irrespective of high or low CRP levels in a total of 60 patients treated with primary PCI or rescue PCI (33). In our study, hs-CRP levels in the patient group with insufficient final coronary flow were higher than those with sufficiently restored coronary flow, but the difference was not statistically significant (54.4±61.4 vs. 39.3±49.9, P=0.103). On the other hand, a significant positive correlation between final cTFC value and hs-CRP level was determined (r=0.183, P=0.034).
Conclusions
The results presented here demonstrated that raised N/L ratios in STEMI patients treated with primary PCI were related to the final coronary flow velocity and increased mortality. High N/L ratio was determined to be an independent predictor of no-reflow development and mortality within one year. Since N/L ratio depends on a simple and low-cost analysis, we believe that it will be useful in risk evaluation of patients treated with primary PCI.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Ross R.Atherosclerosis--an inflammatory disease. N Engl J Med 1999;340:115-26 [DOI] [PubMed] [Google Scholar]
- 2.Korkmaz L, Kul S, Korkmaz AA, et al. Increased leucocyte count could predict coronary artery calcification in patients free of clinically apparent cardiovascular disease. Turk Kardiyol Dern Ars 2012;40:223-8 [DOI] [PubMed] [Google Scholar]
- 3.Barron HV, Cannon CP, Murphy SA, et al. Association between white blood cell count, epicardial blood flow, myocardial perfusion, and clinical outcomes in the setting of acute myocardial infarction: a thrombolysis in myocardial infarction 10 substudy. Circulation 2000;102:2329-34 [DOI] [PubMed] [Google Scholar]
- 4.Yarnell JW, Baker IA, Sweetnam PM, et al. Fibrinogen, viscosity, and white blood cell count are major risk factors for ischemic heart disease. The Caerphilly and Speedwell collaborative heart disease studies. Circulation 1991;83:836-44 [DOI] [PubMed] [Google Scholar]
- 5.Shen XH, Chen Q, Shi Y, et al. Association of neutrophil/lymphocyte ratio with long-term mortality after ST elevation myocardial infarction treated with primary percutaneous coronary intervention. Chin Med J (Engl) 2010;123:3438-43 [PubMed] [Google Scholar]
- 6.Tamhane UU, Aneja S, Montgomery D, et al. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol 2008;102:653-7 [DOI] [PubMed] [Google Scholar]
- 7.Lee CH, Wong HB, Tan HC, et al. Impact of reversibility of no reflow phenomenon on 30-day mortality following percutaneous revascularization for acute myocardial infarction-insights from a 1,328 patient registry. J Interv Cardiol 2005;18:261-6 [DOI] [PubMed] [Google Scholar]
- 8.Brosh D, Assali AR, Mager A, et al. Effect of no-reflow during primary percutaneous coronary intervention for acute myocardial infarction on six-month mortality. Am J Cardiol 2007;99:442-5 [DOI] [PubMed] [Google Scholar]
- 9.Romano M, Buffoli F, Tomasi L, et al. The no-reflow phenomenon in acute myocardial infarction after primary angioplasty: incidence, predictive factors, and long-term outcomes. J Cardiovasc Med (Hagerstown) 2008;9:59-63 [DOI] [PubMed] [Google Scholar]
- 10.Ndrepepa G, Tiroch K, Fusaro M, et al. 5-year prognostic value of no-reflow phenomenon after percutaneous coronary intervention in patients with acute myocardial infarction. J Am Coll Cardiol 2010;55:2383-9 [DOI] [PubMed] [Google Scholar]
- 11.Charron T, Jaffe R, Segev A, et al. Effects of distal embolization on the timing of platelet and inflammatory cell activation in interventional coronary no-reflow. Thromb Res 2010;126:50-5 [DOI] [PubMed] [Google Scholar]
- 12.Akpek M, Kaya MG, Lam YY, et al. Relation of neutrophil/lymphocyte ratio to coronary flow to in-hospital major adverse cardiac events in patients with ST-elevated myocardial infarction undergoing primary coronary intervention. Am J Cardiol 2012;110:621-7 [DOI] [PubMed] [Google Scholar]
- 13.Oduncu V, Tanalp AC, Erkol A, et al. Impact of chronic pre-treatment of statins on the level of systemic inflammation and myocardial perfusion in patients undergoing primary angioplasty. Am J Cardiol 2011;107:179-85 [DOI] [PubMed] [Google Scholar]
- 14.Gibson CM, Cannon CP, Daley WL, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation 1996;93:879-88 [DOI] [PubMed] [Google Scholar]
- 15.Gibson CM, Schömig A. Coronary and myocardial angiography: angiographic assessment of both epicardial and myocardial perfusion. Circulation 2004;109:3096-105 [DOI] [PubMed] [Google Scholar]
- 16.Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569-619. [DOI] [PubMed]
- 17.Gibson CM, Cannon CP, Murphy SA, et al. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 2000;101:125-30 [DOI] [PubMed] [Google Scholar]
- 18.Topsakal R, Kaya MG, Karakaya E, et al. Relationship between no-reflow phenomenon and serotonin levels in patients with acute ST-elevation myocardial infarction who underwent primary percutaneous intervention. Anadolu Kardiyol Derg 2010;10:253-9 [DOI] [PubMed] [Google Scholar]
- 19.Esen AM, Acar G, Esen O, et al. The prognostic value of combined fractional flow reserve and TIMI frame count measurements in patients with stable angina pectoris and acute coronary syndrome. J Interv Cardiol 2010;23:421-8 [DOI] [PubMed] [Google Scholar]
- 20.De Luca G, Suryapranata H, de Boer MJ, et al. For theOngoing Tirofiban In Myocardial Infarction Evaluation (On-TIME) study group. Combination of electrocardiographic and angiographic markers of reperfusion in the prediction of infarct size in patients with ST-segment elevation myocardial infarction undergoing successful primary angioplasty. Int J Cardiol 2007;117:232-237 [DOI] [PubMed] [Google Scholar]
- 21.Kloner RA. No-reflow phenomenon: maintaining vascular integrity. J Cardiovasc Pharmacol Ther 2011;16:244-50 [DOI] [PubMed] [Google Scholar]
- 22.Reffelmann T, Kloner RA. The no-reflow phenomenon: A basic mechanism of myocardial ischemia and reperfusion. Basic Res Cardiol 2006;101:359-72 [DOI] [PubMed] [Google Scholar]
- 23.Kloner RA, Ganote CE, Jennings RB. The “no-reflow” phenomenon after temporary coronary occlusion in the dog. J Clin Invest 1974;54:1496-508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sahin DY, Elbasan Z, Gür M, et al. Neutrophil to Lymphocyte Ratio Is Associated With the Severity of Coronary Artery Disease in Patients With ST-Segment Elevation Myocardial Infarction. Angiology. 2012 doi: 10.1177/0003319712453305. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Zazula AD, Précoma-Neto D, Gomes AM, et al. An assessment of neutrophils/lymphocytes ratio in patients suspected of acute coronary syndrome. Arq Bras Cardiol 2008;90:31-6 [DOI] [PubMed] [Google Scholar]
- 26.Núñez J, Núñez E, Bodí V, et al. Usefulness of the neutrophil to lymphocyte ratio in predicting long-term mortality in ST segment elevation myocardial infarction. Am J Cardiol 2008;101:747-52 [DOI] [PubMed] [Google Scholar]
- 27.Muhmmed Suliman MA, Bahnacy Juma AA, Ali Almadhani AA, et al. Predictive value of neutrophil to lymphocyte ratio in outcomes of patients with acute coronary syndrome. Arch Med Res 2010;41:618-22 [DOI] [PubMed] [Google Scholar]
- 28.Park JJ, Jang HJ, Oh IY, et al. Prognostic value of neutrophil to lymphocyte ratio in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol 2013;111:636-42 [DOI] [PubMed] [Google Scholar]
- 29.Han YC, Yang TH, Kim DI, et al. Neutrophil to Lymphocyte Ratio Predicts Long-Term Clinical Outcomes in Patients with ST-Segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Korean Circ J 2013;43:93-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amanvermez R, Acar E, Günay M, et al. Hsp 70, hsCRP and oxidative stress in patients with acute coronary syndromes. Bosn J Basic Med Sci 2012;12:102-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liuzzo G, Biasucci LM, Gallimore JR, et al. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med 1994;331:417-24 [DOI] [PubMed] [Google Scholar]
- 32.Ndrepepa G, Tiroch K, Keta D, et al. Predictive factors and impact of no reflow after primary percutaneous coronary intervention in patients with acute myocardial infarction. Circ Cardiovasc Interv 2010;3:27-33 [DOI] [PubMed] [Google Scholar]
- 33.Niccoli G, Lanza GA, Spaziani C, et al. Baseline systemic inflammatory status and no-reflow phenomenon after percutaneous coronary angioplasty for acute myocardial infarction. Int J Cardiol 2007;117:306-11 [DOI] [PubMed] [Google Scholar]


