Abstract
Purpose
Anterior cervical discectomy and fusion (ACDF) with titanium- or polyetheretherketone (PEEK)-cage reconstruction is widely used in the treatment of cervical spondylotic myelopathy (CSM). This study was to compare outcomes of titanium and PEEK cages in the treatment of multilevel CSM.
Methods
Between November 2002 and December 2004, a total of 80 patients with 3-level CSM were randomized in a 1:1 ratio to titanium group and PEEK group. The overall follow-up period of the patients ranged from 86 to 116 months (average 99.7 months). Clinical and radiological results were compared between titanium group and PEEK group.
Results
At the final follow-up, the clinical outcomes including JOA score, NDI score, and the excellent and good rates of clinical outcomes in the PEEK group were better than those in the titanium group. More loss of the Cobb angles and the intervertebral height was observed in the titanium group, resulting in the radiological parameters in the titanium group becoming inferior to the PEEK group at the final follow-up. Cage subsidence rates were 34.5 and 5.4 % in the titanium and PEEK groups, respectively. Fusion was observed in all patients of two groups at the final follow-up. Two patients presented with cage dislocation without clinical symptoms in the titanium group.
Conclusions
In surgical treatment of multilevel CSM, PEEK cage is superior to titanium cage in maintenance of intervertebral height and cervical lordosis, resulting in better clinical outcomes in the long-term follow-up.
Keywords: Anterior cervical discectomy and fusion, Titanium, PEEK, Cervical spondylotic myelopathy
Introduction
Since Cloward [11] and Smith and Robinson [27] described anterior cervical discectomy and fusion (ACDF), it has been widely used as an ideal surgical treatment method for cervical disc degenerative disorders. Although much improvement has carried out on this technique, the surgical outcome depends on decompression of the spinal cord and nerve roots, stabilization of fused segments, restoration of intervertebral height and cervical lordsis, as well as avoidance of complications. Iliac crest grafting has ever been considered as a gold standard for solid bony fusion, but the traditional autologous bone graft was reported to have a high incidence of donor sit complications, including subcutaneous hematoma, wound infection, and chronic wound pain [37, 38]. As a solution to these problems, several kinds of interbody fusion cages have been developed, which claimed advantages of comparable fusion rate and no donor complications [4, 7, 20, 31].
Currently, titanium cage and polyetheretherketone (PEEK) cage are available on the market in China. Each type of cage has its own characteristics. Titanium cages have been criticized to produce more cage subsidence due to higher elasticity modules. Nevertheless, due to structural properties titanium implants are likely to provide a good immediate stability and osseointegration, and several clinical studies demonstrated successful results after implantation of titanium cages [15, 16, 30]. PEEK cages have a modulus of elasticity closely resembling that of cortical bone, which might lead to advantages in load sharing and stress distribution. This might result in a lower subsidence rate with less loss of cervical lordosis [7, 9].
A direct comparison of titanium and PEEK cages in the treatment of cervical disc degenerative disease is very rarely found in the literature [21, 22]. Recently, two studies compared clinical and radiological results of titanium and PEEK cages, but discrepant results were reported [6, 24]. Cabraja et al. [6] concluded that there was no difference between titanium and PEEK cages in the treatment single-level cervical disc degenerative disorders. However, Niu et al. [24] study showed the PEEK implants are superior in maintaining cervical interspace height and achieving radiographic fusion, but the rates of successful clinical outcomes were comparable between two groups in 1 and 2-level ACDF patients.
To our knowledge, there were no comparative studies on titanium and PEEK cage in the treatment of multilevel cervical spondylotic myelopathy (CSM). To compare the differences in the treatment of multilevel CSM between titanium and PEEK cages, we prospectively observed the clinical and radiological results of the patients with 3-level CSM who had undergone ACDF with titanium or PEEK cages based on a minimum 7-year follow-up.
Materials and methods
Patient population
This is a prospective, randomized, control clinical study. Between November 2002 and December 2004, a total of 80 patients who met the selection criteria of this study and agreed with participation in the randomization process were recruited for enrollment. The inclusion criteria included: (1) symptoms of cervical myelopathy and/or radiculopathy; (2) the cervical spine radiography, CT, and MRI showed intervertebral disc degeneration and herniation, and the posterior vertebral body osteophyte formation; (3) cervical pathology in three consecutive levels; and (4) no response to at least 6 weeks of conservative treatment. Those, who presented with significant segmental instability, cervical anatomic deformity, ossification of the posterior longitudinal ligament (OPLL), as well as symptomatic disorders at the other spinal region, were excluded from the study.
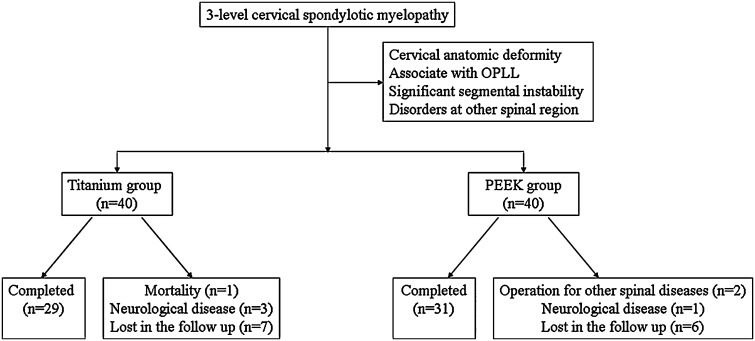
Patients were provided informed consent and randomized in a 1:1 ratio to titanium group and PEEK group by envelope method. The overall follow-up period of the patients ranged from 86 to 116 months (average 99.7 months). Among the patients randomized, 20 (25 %) withdrew from the study. In the titanium group, one patient died from heart disease, three withdrew from the study because of neurological diseases, and seven lost correspondence. In the PEEK group, one withdrew form the study because of operation for thoracic canal stenosis, two because of neurological diseases, and six lost correspondence (Fig. 1). The demographic data including age, sex, treated level, preoperative symptoms, smoking status and diabetes mellitus in each group were summarized in Table 1.
Fig. 1.
Flowchart of the study comparing the titanium cage and PEEK cage
Table 1.
Demographic data of patients
| Titanium group | PEEK group | P | |
|---|---|---|---|
| Patients, no. | 29 | 31 | |
| Age, year | 45.7 ± 7.2 | 47.2 ± 6.8 | >0.05 |
| Sex | |||
| Male | 17 | 16 | >0.05 |
| Female | 12 | 15 | |
| Active smokers | 7 | 8 | >0.05 |
| Patient with diabetes | 4 | 4 | >0.05 |
| Preoperative symptoms | |||
| Myelopathic | 16 | 18 | >0.05 |
| Radicular | 1 | 1 | |
| Combined | 12 | 12 | |
| Operated segments | |||
| C3–C6 | 14 | 18 | >0.05 |
| C4–C7 | 15 | 13 | |
| Follow-up period, mo. | 97.2 (86–107) | 102.1 (88–116) | >0.05 |
Operation and device
The surgical technique was similar in both groups. A standard Smith–Robinson right approach was made to expose the symptomatic levels. After appropriate exposure and localization of the disc, a discectomy was performed. Besides, a local decompression was accomplished via resection of osteophyte and the posterior longitudinal ligament if necessary. The cartilage endplates were removed with curettage while the bony endplates were protected. After decompression, an appropriate sized cage packed with local decompression bone harvested from the anterior hypertrophic osteophyte and potential decompression of the posterior border of vertebral body was implanted as a stand-alone device. In the titanium group, the titanium box cage SynCage C (Synthes, Oberdorf, Switzerland) was used. In the PEEK group, the PEEK box cage (Depuy Spine, Raynham, MA, USA) was used. Postoperatively, the patients were encouraged to resume their normal activities as soon as possible with a soft collar to avoid over-extension for 6 weeks.
Clinical and radiological evaluation
Clinical outcomes were assessed using the Japanese orthopedic association (JOA) score, Neck disability index (NDI) score, and Odom’s criteria (Table 2). The cervical lordosis was assessed using the Cobb angles of C2–C7 and operated segments. The former was formed by lines along the inferior endplate of C2 to inferior endplate of C7 in a neutral position, and the latter was formed by lines along the superior endplate of the cephalad vertebral body and along the inferior endplate of caudal vertebral body of the operated segments. Lordosis is shown as a positive value and kyphosis is shown as a negative value (Fig. 2). The intervertebral height was calculated as the mean value of the height of the anterior border (AH) and posterior border (PH) (Fig. 3). Cage subsidence was recorded when the loss of intervertebral height was over 3 mm (Fig. 4) [3]. Fusion was considered according to the following accepted criteria: (1) absence of motion between the spinous processes at dynamic lateral radiographs, (2) absence of a radiolucent gap between the graft and endplates, (3) presence of continuous bridging bony trabeculae at the graft-endplate interface [14].
Table 2.
Odom criteria
| Grade | Definition |
|---|---|
| Excellent | All preoperative symptoms relieved, able to carry out daily occupations without impairment |
| Good | Minimum persistence of preoperative symptoms, able to carry out daily occupations without significant interference |
| Fair | Relief of some preoperative symptoms, but whose physical activities were significantly limited |
| Poor | Symptoms and signs unchanged or worse |
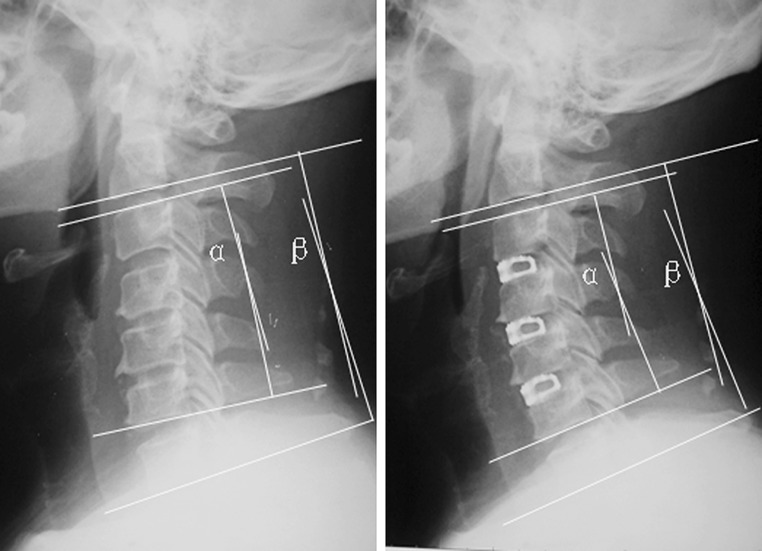
Fig. 2.
a Preoperative Cobb angle of operated segments (segmental Cobb, α); Preoperative Cobb angle of C2–C7 (C2–C7 Cobb, β). b Postoperative Cobb angle of operated segments (segmental Cobb, α); Postoperative Cobb angle of C2–C7 (C2–C7 Cobb, β)
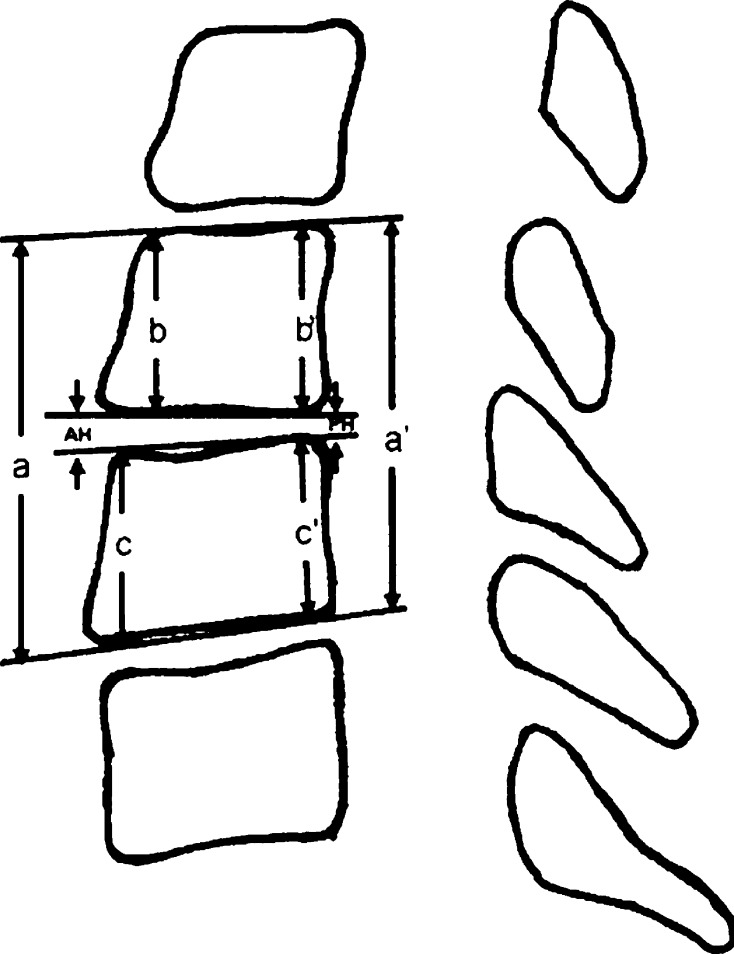
Fig. 3.
Measurement of intervertebral height of the involved segments (anterior height of intervertebral space: AH = a–b–c; posterior height of intervertebral space: AH = a′–b′–c′)
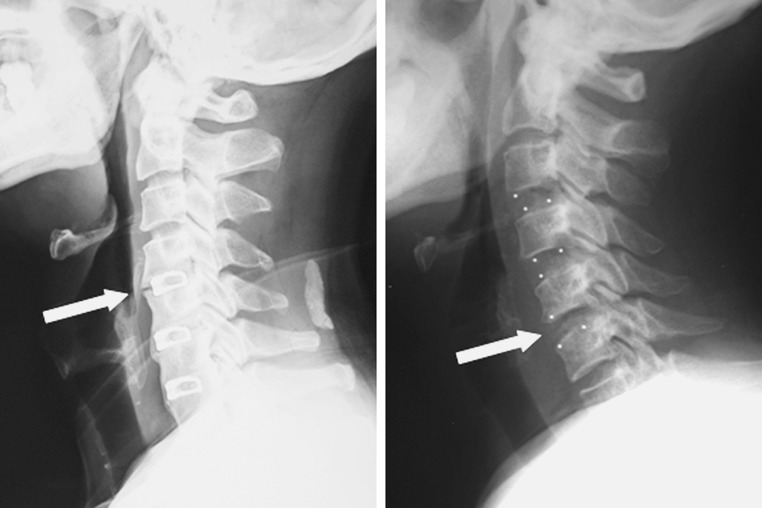
Fig. 4.
Cage subsidence could be seen in the titanium group (a) and PEEK group (b)
Statistical analysis
To correct the intraobserver and interobserver reliability of the radiological measurements, three experienced observers were assigned to independently evaluate the radiographs of the patients. Each of them took measurements three times and mean values were used for statistical analysis. The changes in clinical and radiological parameters in each group after surgeries were analyzed by the Wilcoxon rank-sum test. The Kruskal–Wallis H test was used to investigate whether the statistical differences of results exist among the groups. The χ2 test was used in the comparisons of the incidences of dysphagia and heterotopic ossification between groups. All the statistical tests were completed by the Statistical Package for Social Science software for Windows (Ver. 17.0; SPSS Inc, Chicago, IL, USA) and the difference was considered to be statistically significant at the P < 0.05 level.
Results
Clinical outcome
The JOA scores significantly increased from 9.6 ± 1.4 to 12.8 ± 1.8 in the titanium group (P < 0.05), from 9.8 ± 1.4 to 14.2 ± 1.8 in the PEEK group (P < 0.05), respectively. The corresponding NDI scores significantly decreased from 36.2 ± 3.7 to 21.6 ± 2.6 in the titanium group (P < 0.05), from 35.4 ± 3.6 to 15.2 ± 2.3 in the PEEK group (P < 0.05), respectively. According to the Odom criteria, the percentage of patients with excellent and good clinical outcomes was 55.2 % in the titanium group, 74.2 % in the PEEK group, respectively. Although significant neurological symptoms release and functional activity improvement have been achieved in the two groups at the final follow-up, there were significant differences in the JOA score, NDI score, and the excellent and good rates of clinical outcomes between two groups (P < 0.05, Table 3).
Table 3.
Clinical results of patients
| Titanium group | PEEK group | P | |
|---|---|---|---|
| JOA scores | |||
| Preoperative | 9.6 ± 1.4 | 9.8 ± 1.4 | >0.05 |
| Final | 12.8 ± 1.8# | 14.2 ± 1.8# | <0.05 |
| NDI scores | |||
| Preoperative | 36.2 ± 3.7 | 35.4 ± 3.6 | >0.05 |
| Final | 21.6 ± 2.6# | 15.2 ± 2.3# | <0.05 |
| Clinical outcomes according to Odom criteria | Excellent: 7, Good: 9, Fair: 8, Bad: 5 | Excellent: 11, Good: 12, Fair: 5, Bad: 3 | <0.05 |
JOA Japanese orthopedic association, NDI neck disability index
#P < 0.05 comparing with preoperative value
Radiological analysis
In the titanium group, the Cobb angles of the operated segment and C2–C7 significantly increased from 5.63° ± 8.26° to 14.75° ± 9.98° (P < 0.05) and from 6.83° ± 8.83° to 16.49° ± 10.27° (P < 0.05) after operation, respectively. In the PEEK group, the corresponding parameters significantly increased from 6.45° ± 7.28° to 16.27° ± 9.45° (P < 0.05) and from 8.23° ± 7.62° to 18.72° ± 11.24° (P < 0.05) after operation, respectively. The intervertebral height of the operated segment significantly increased from 4.2 ± 0.7 to 5.8 ± 0.8 mm in the titanium group (P < 0.05), from 4.3 ± 0.8 to 6.0 ± 0.8 mm in the PEEK group (P < 0.05), respectively. Statistical analysis showed there were no significant differences in radiological parameters between two groups before and after operation. However, more loss of the Cobb angles and the intervertebral height in the titanium group led to the significant differences in these mentioned radiological parameters between two groups at the final follow-up (P < 0.05, Table 4; Fig. 5). The loss of intervertebral height over 3 mm recorded as subsidence occurred in 34.5 % of cages in the titanium group versus 5.4 % of cages in the PEEK group (P < 0.05). Fusion was observed in all patients of two groups at the final follow-up. In addition, two patients presented with cage dislocation without clinical symptoms in the titanium group (Fig. 6).
Table 4.
Radiological results of patients
| Titanium group | PEEK group | P | |
|---|---|---|---|
| Cobb angle of the operated segment (°) | |||
| Preoperative | 5.63 ± 8.26 | 6.45 ± 7.28 | >0.05 |
| Postoperative | 14.75 ± 9.98# | 16.27 ± 9.45# | >0.05 |
| Final | 7.38 ± 8.34 | 12.34 ± 8.37# | <0.05 |
| Loss of correction | 7.64 ± 4.23 | 3.96 ± 1.34 | <0.05 |
| Cobb angle of C2–C7 (°) | |||
| Preoperative | 6.83 ± 8.83 | 8.23 ± 7.62 | >0.05 |
| Postoperative | 16.49 ± 10.27# | 18.72 ± 11.24# | >0.05 |
| Final | 7.86 ± 8.52 | 13.65 ± 8.92# | <0.05 |
| Loss of correction | 8.59 ± 4.67 | 4.84 ± 2.39 | <0.05 |
| Intervertebral height of the operated segment (mm) | |||
| Preoperative | 4.2 ± 0.7 | 4.3 ± 0.8 | >0.05 |
| Postoperative | 5.8 ± 0.8# | 6.0 ± 0.8# | >0.05 |
| Final | 4.3 ± 0.6 | 5.3 ± 0.7# | <0.05 |
| Loss of correction | 1.5 ± 0.4 | 0.6 ± 0.2 | <0.05 |
| Subsidence (≥3 mm) | 17/87 (34.5 %) | 5/93 (5.4 %) | <0.05 |
| Fusion | 87/87 (100 %) | 93/93 (100 %) | >0.05 |
| Dislocation | 2/87 (2.3 %) | 0/93 (0 %) | <0.05 |
#P < 0.05 comparing with preoperative value
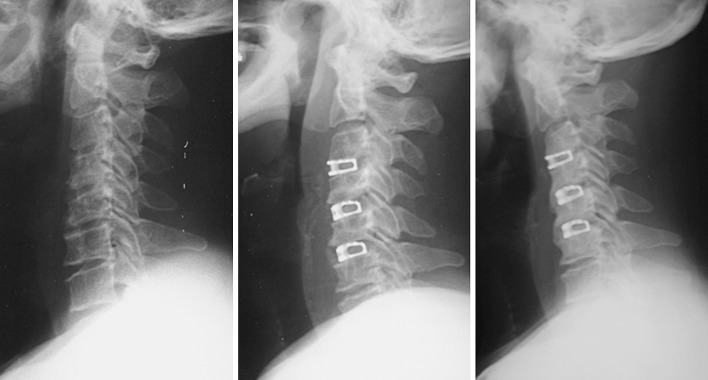
Fig. 5.
Loss of sagittal lordosis of the cervical spine due to cage subsidence in the titanium group: a radiograph before operation, b radiograph immediately after operation, c radiograph at the final follow-up
Fig. 6.

Dislocation of titanium cage
Discussion
Cervical spondylotic myelopathy (CSM) usually arises in the disc level, including disc herniation, osteophyte formation at endplates, and uncovertebral joints. This pathophysiology of CSM determines that the relief of the anterior compression of the spinal cord is the most direct treatment of CSM. In the past few years, cervical motion preserved through implantation of artificial disc prosthesis has been proved to be an effective and safe alternative option in 1 and 2 level pathologies [10, 17, 23, 39]. However, anterior cervical discectomy and fusion (ACDF) remains the gold standard in the surgical treatment of the patients with multilevel CSM, resulting in well established results and less complications [19, 28, 36].
The use of stand-alone cage technology in cervical spondylosis was first introduced by Bagby [1]. Distraction after discectomy could restore disc height and increase the volume of neuroforamen. Initial stability could be maintained by use of a cage and the tension forces of residual annuls and ligaments. Stand-alone cages have been widely applied in 1 and 2-level pathologies [7, 12, 15, 18]. Recently, spine surgeons started to use the stand-alone cage construct in multilevel cervical disc disease [5, 8, 16]. Hwang et al. [16] evaluated titanium cage-augmented fusion in three-level and four-level anterior cervical discectomies with and without anterior plate fixation. They even reported a low complication rate and a shorter hospital stay in the group without plate fixation and concluded that stand-alone cage in multilevel cervical disc disease are better than with plate fixation. These results have been also confirmed by Cho et al. [8] who included a group of 26 patients with three-level disease undergoing stand-alone PEEK cage fusion and reported also satisfactory results comparable with graft-plate construct. The same subject has been studied by Bucciero et al. [5] who applied stand-alone PEEK cage fusion in four-level cervical disc disease. They concluded that this method of treatment is an effective procedure for the treatment of such cages.
Based on the clinical and radiological results of this study with over 7-year follow-up, we achieved a more comprehensive understanding of stand-alone cage technology in the treatment of multilevel CSM, especially the difference between titanium and PEEK cages. Radiological analysis showed that the Cobb angles and intervertebral height were significantly increased by implanting titanium cages or PEEK cages, without significant differences between two groups after operation. However, more loss of the Cobb angles and intervertebral height in the titanium group led to the significant differences in these mentioned radiological parameters between two groups at the final follow-up. Correspondingly, the clinical outcome including JOA score, NDI score and the rate of excellent and good clinical outcomes in the titanium group was significantly inferior to the PEEK group. Without other significant bias between two groups, we speculated that the higher incidence of cage subsidence in the titanium group was responsible for this result.
Cage subsidence is the most considered problem for stand-alone cage technology. Subsidence of titanium cages is observed in 13 to 45 % of cases in larger series [3, 25]. The reported rate of PEEK cage subsidence varies from 8 to 15 % [13, 35]. Risk factors related to the cage subsidence may include endplate preparation, size of the contact area between implant and endplate, over-distraction of the involved segment, and the bone mineral density of the vertebral body. However, the most important factor resulting in subsidence is the cage material. The modulus of the elasticity of PEEK is similar to that of bone. This distinguishing feature is thought to be able to reduce cage subsidence compared with titanium cages. The long-term results of our study were consistent with the previous reports. The subsidence rate was significantly higher in the titanium group. Actually, titanium cage subsidence was more common than what the result demonstrated. The mean loss of intervertebral height reached 1.5 mm in the titanium group, and subsidence rate was 34.5 % according to the criteria of loss of intervertebral height over 3 mm.
The relationship between cage subsidence with loss of intervertebral height and kyphotic deformity, as well as clinical outcome, has been discussed in the literature [3, 24, 33]. Some authors considered case subsidence did not necessarily mean loss of local and general cervical lordosis. If the collapse of the anterior part of involved disc space was not greater than that of the posterior part, the local lordosis would be preserved, despite the disc space collapse. Niu et al. [24] compared clinical and radiological results between titanium cages and PEEK cages. The results showed the cage subsidence in the titanium group was significantly higher, but there was no significant difference between two groups in loss of cervical lordosis and clinical outcome. Barsa and Suchomel [3] prospectively analyzed 100 consecutive patients, who underwent ACDF with box-shaped titanium cages. They found the subsidence of the device was associated with segmental loss of lordosis; however, the overall alignment between C2 and C7 did not change significantly. Wu et al. [33] performed a similar observation with 5-year follow-up. The results showed the change of the local and general alignment of subsidence and non-subsidence group was not significantly different. Cage subsidence did not exert significant impact upon the long-term clinical outcome, but the cervical lordosis was more important. However, our study demonstrated a contrary result in the treatment of multilevel CSM. As we observed in Fig. 5 if cage subsidence occurred at 2–3 levels, the loss of height of the cervical anterior column would lead to significant loss of cervical lordosis, which eventually resulted in inferior clinical outcomes.
Multilevel stand-alone cages were reported to be associated with high rates of pseudarthrosis [32]. To increase fusion rates, prevent subsidence and restore cervical sagittal alignment, additional anterior cervical plating has been recommended for cage fixation [29]. However, rigid anterior cervical plate fixation may shield the mechanical load that is very important for fusion. On the other hand, there are some complications associated with anterior cervical plating [34]. Moreover, the cost of additional plating would increase the burden of the patient, and no significant differences in clinical outcomes between stand-alone cage with and without plate augmentation [8, 26]. To achieve successful fusion, the fusion materials embedded in the cage are another key point. The autologous iliac bone was the most suitable for biologic bone healing ability, but it is still necessary to create an iliac wound, even though the wound is small. In this study, the local decompression bone was harvested and packed into the cages. 100 % fusion rate of all patients at the final follow-up confirmed it was effective alternative material for bony fusion without donor site complications [2]. In addition, without anterior cervical plate augmentation, stand-alone PEEK cages provided good maintenance of intervertebral height and cervical lordosis, as well as better clinical outcomes compared with titanium cages in the long-term follow-up. These advantages were added in the treatment of multilevel CSM.
Conflict of interest
No funds were received in supported of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Footnotes
Y. Chen and X. Wang have equally contributed to the writing of this article.
References
- 1.Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics. 1988;11(6):931–934. doi: 10.3928/0147-7447-19880601-13. [DOI] [PubMed] [Google Scholar]
- 2.Bao Z, Zhao W, Wu D, Shen B, Yu B, Wang Z. Box cages packed with local decompression bone were efficient in anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2012;37(20):E1260–E1263. doi: 10.1097/BRS.0b013e318265df75. [DOI] [PubMed] [Google Scholar]
- 3.Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence cage assisted anterior cervical fusion. Eur Spine J. 2007;16(9):1395–1400. doi: 10.1007/s00586-006-0284-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brooke NS, Roeke AW, King AT, Gullan RW. Preliminary experience of carbon fiber cage prostheses for treatment of cervical spine disorders. Br J Neruosurg. 1997;11(3):221–227. doi: 10.1080/02688699746285. [DOI] [PubMed] [Google Scholar]
- 5.Bucciero A, Zorzi T, Piscopo GA. Peek cage-assisted anterior cervical discectomy and fusion at four levels: clinical and radiographic results. J Neurosurg Sci. 2008;52(2):37–40. [PubMed] [Google Scholar]
- 6.Cabraja M, Oezdemir S, Koeppen D, Kroppenstedt S. Anterior cervical discectomy and fusion: comparison of titanium and polyetheretherketone cages. BMC Musculoskelet Disord. 2012;13:172. doi: 10.1186/1471-2474-13-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery. 2002;51(6):1343–1349. [PubMed] [Google Scholar]
- 8.Cho DY, Lee WY, Sheu PC. Treatment of multilevel cervical fusion with cages. Surg Neurol. 2004;62(5):378–385. doi: 10.1016/j.surneu.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 9.Chou YC, Chen DC, Hsleh WA, Chen WF, Yen PS, Harnod T, Chlou TL, Chang YL, Su CF, Lin SZ, Chen SY. Efficacy of anterior cervical fusion: comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone graft. J Clin Neurosci. 2008;12(11):1240–1245. doi: 10.1016/j.jocn.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 10.Cheng L, Nie L, Zhang L, Hou Y. Fusion versus Bryan cervical disc in two-level cervical disc disease: a prospective, randomized study. Int Orthop. 2009;33(5):1347–1351. doi: 10.1007/s00264-008-0655-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cloward R. The anterior approach for removal of ruptured cervical discs. J Neurosurg. 1958;15(6):602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 12.Dufour T, Huppert J, Louis C, Beaurain J, Stecken J, Aubourg L, Vila T. Radiological analysis of 37 segments in cervical implanted with a peek standalone device, with at least one year follow-up. Br J Neurosurg. 2010;24(6):633–640. doi: 10.3109/02688691003793029. [DOI] [PubMed] [Google Scholar]
- 13.Ha SK, Park JY, Kim SH, Lim DJ, Kim SD, Lee SK. Radiologic assessment of subsidence in stand-alone cervical polyetheretherketone (PEEK) cage. J Korean Neurosurg Soc. 2008;44(6):370–374. doi: 10.3340/jkns.2008.44.6.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harker RJ, Cauthen JC, Gillbert TJ, Griffth SL. A prospective randomized multicenter clinical evaluation of anterior cervical fusion cage. Spine (Phila Pa 1976) 2000;25(20):2646–2654. doi: 10.1097/00007632-200010150-00017. [DOI] [PubMed] [Google Scholar]
- 15.Hwang SL, Hwang YF, Lieu AS, Lin CL, Kuo TH, Su YF, Howng SL, Lee KS. Outcome analysis of interbody titanium cage fusion used in the anterior discectomy for cervical degenerative disc disease. J Spinal Disord Tech. 2005;18(4):326–331. doi: 10.1097/01.bsd.0000164198.30725.2d. [DOI] [PubMed] [Google Scholar]
- 16.Hwang SL, Lin CL, Lieu AS, Lee KS, Kuo TH, Hwang YF, Su YF, Howng SL. Three-level and four-level anterior cervical discectomies and titanium cage augmented fusion with and without plate fixation. J Neurosurg Spine. 2004;1(2):160–167. doi: 10.3171/spi.2004.1.2.0160. [DOI] [PubMed] [Google Scholar]
- 17.Kim SW, Limson MA, Kim SB, Arbatin JJ, Chang KY, Park MS, Shin JH, Ju YS. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J. 2009;18(2):218–231. doi: 10.1007/s00586-008-0854-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kolstad F, Nygaard QP, Andresen H, Leivseth G. Anterior cervical arthrodesis using a “stand alone” cylindrical titanium cage: prospective analysis of radiographic parameters. Spine (Phila Pa 1976) 2010;35(16):1545–1550. doi: 10.1097/BRS.0b013e3181d259c1. [DOI] [PubMed] [Google Scholar]
- 19.Liu Y, Hou Y, Yang L, Chen H, Wang X, Wu X, Gao R, Wang C, Yuan W. Comparison of 3 reconstructive techniques in the surgical management of multilevel cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2012;37(23):E1450–E1458. doi: 10.1097/BRS.0b013e31826c72b4. [DOI] [PubMed] [Google Scholar]
- 20.Maid ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine (Phila Pa 1976) 1999;24(15):1604–1610. doi: 10.1097/00007632-199908010-00016. [DOI] [PubMed] [Google Scholar]
- 21.Matge G. Cervical fusion with 5 different implants: 250 cases. Acta Neurochir (Wien) 2002;144(6):539–549. doi: 10.1007/s00701-002-0939-0. [DOI] [PubMed] [Google Scholar]
- 22.Meier U, Kemmesies D. Experience with six different intervertebral disc spacers for spondylodesis of the cervical spine. Orthopaed. 2004;33(11):1290–1299. doi: 10.1007/s00132-004-0707-3. [DOI] [PubMed] [Google Scholar]
- 23.McAfee PC, Reah C, Gilder K, Eisermann L, Cunningham B. A meta-analysis of comparative outcomes following cervical arthroplasty or anterior cervical fusion: results from 4 prospective multicenter randomized clinical trials and up to 1226 patients. Spine (Phila Pa 1976) 2012;37(11):943–952. doi: 10.1097/BRS.0b013e31823da169. [DOI] [PubMed] [Google Scholar]
- 24.Niu CC, Liao JC, Chen WJ, Chen LH. Outcomes of interbody fusion cases used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Tech. 2010;23(5):310–316. doi: 10.1097/BSD.0b013e3181af3a84. [DOI] [PubMed] [Google Scholar]
- 25.Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 2006;4(6):447–453. doi: 10.3171/spi.2006.4.6.447. [DOI] [PubMed] [Google Scholar]
- 26..Shousha M, Ezzati A, Boehm H. Four-level anterior cervical discectomies and cage-augmented fusion with and without fixation. Eur Spine J. 2012;21(12):2512–2519. doi: 10.1007/s00586-012-2307-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40A(3):607–624. [PubMed] [Google Scholar]
- 28.Song KJ, Lee KB, Song JH. Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J. 2012;21(8):1551–1557. doi: 10.1007/s00586-012-2296-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Song KJ, Yoon SJ, Lee KB. Three- and four-level anterior cervical discectomy and fusion with a PEEK cage and plate construct. Eur Spine J. 2012;21(12):2492–2497. doi: 10.1007/s00586-012-2447-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thome C, Krauss JK, Zevgaridls D. A prospective clinical comparison of rectangular titanium cages and iliac crest autografts in anterior cervical discectomy and fusion. Neurosurg Rev. 2004;27(1):34–41. doi: 10.1007/s10143-003-0297-2. [DOI] [PubMed] [Google Scholar]
- 31.Wang X, Chen Y, Chen D, Yaun W, Chen X, Zhou X, Xiao J, Ni B, Jia L. Anterior decompression and interbody fusion with BAK/C for cervical disc degenerative disorders. J Spinal Disord Tech. 2009;22(4):240–245. doi: 10.1097/BSD.0b013e31816d5f7e. [DOI] [PubMed] [Google Scholar]
- 32.Wang JC, McDonough PW, Kanim LE, Endow KK, Delamarter RB. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2001;26(6):643–646. doi: 10.1097/00007632-200103150-00015. [DOI] [PubMed] [Google Scholar]
- 33.Wu WJ, Jiang LS, Liang Y, Dai LY. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J. 2012;21(7):1374–1382. doi: 10.1007/s00586-011-2131-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xie N, Yuan W, Ye X, Ni B, Chen D, Xiao J, Jia L. Anterior cervical locking plate-related complications; prevention and treatment recommendations. Int Orthop. 2008;32(5):649–655. doi: 10.1007/s00264-007-0369-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 2011;3(1):16–23. doi: 10.4055/cios.2011.3.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang L, Gu Y, Liang L, Gao R, Shi S, Shi J, Yuan W. Stand-alone anchored spacer versus anterior plate for multilevel anterior cervical discectomy and fusion. Orthopedics. 2012;35(10):e1503–e1510. doi: 10.3928/01477447-20120919-20. [DOI] [PubMed] [Google Scholar]
- 37.Young WF, Rosenwasser RH. An early comparative analysis of the fibular allograft versus autologous iliac crest graft for interbody fusion after anterior cervical discectomy. Spine (Phila Pa 1976) 1993;18(9):1123–1124. doi: 10.1097/00007632-199307000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma. 1989;3(3):192–195. doi: 10.1097/00005131-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Zhang X, Zhang X, Chen C, Zhang Y, Wang Z, Wang B, Yan W, Li M, Yuan W, Wang Y. Randomized, controlled, multicenter, clinical trial comparing BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion in China. Spine (Phila Pa 1976) 2012;37(6):433–438. doi: 10.1097/BRS.0b013e31822699fa. [DOI] [PubMed] [Google Scholar]