Abstract
Purpose
Anterior foraminotomy (AF) is a surgical treatment for unilateral cervical radiculopathy that avoids fusion-related complications, but its long-term outcome has yet to be investigated. To clarify the efficacy of AF, the author retrospectively collected long-term data regarding the results of this technique.
Methods
Of 50 patients who underwent AF between November 1999 and June 2005, those who were followed for more than 6 years (n = 44) were enrolled in this study. The parameters studied included the number of revisions, additional surgeries, VAS/NDI, and Odom’s criteria. Plain radiographs were also obtained pre- and postoperatively.
Results
At discharge, 98 % of patients reported improvement, although 20 % temporarily experienced some residual symptoms. There were no other major postoperative complications. At final follow-up (FU, mean of 8.8 years), an excellent or good outcome was achieved in 39 patients (89 %). There was no index level reoperation required, but two additional operations for symptomatic adjacent-segment degeneration were needed (4.5 %). Six patients suffered from shoulder pain on the same side after surgery (mean onset: 3.6 years). At final FU, significant degeneration at the operated level was demonstrated on plain radiographs, resulting in a decreased range of motion. However, loss of lordosis of the segment was minimal. Radiographically, adjacent segment degeneration was noted in only 6 and 11 % at the cranial and caudal segments, respectively.
Conclusions
In this retrospective study, patients who underwent AF for one- or two- level cervical radiculopathy showed a good long-term outcome with minimal adjacent segment degeneration. However, more data should be collected to clarify possible associations with these findings, such as delayed shoulder problems and aggravation of degeneration at the operated level.
Keywords: Anterior cervical foraminotomy, Cervical spine, Intervertebral disc, Radiculopathy
Introduction
Anterior cervical foraminotomy (AF) is a surgical method intended to preserve the functional motion of the cervical spine while removing the underlying pathology. Fusion-related problems, graft site complications and morbidity of the adjacent segment are supposedly avoided with this method. Since its introduction, it has attracted much attention as the early results were encouraging [1–6], but nevertheless this procedure has been accepted by only a few experienced surgeons, mainly because it is a little more technically demanding. Hence, there are very few clinical studies in the literature. Furthermore, no studies of the clinical or radiographic long-term results of this procedure have yet been published.
Recent advances in the cervical artificial disc replacement technique (C-ADR) have changed the way one- or two-level cervical radiculopathy is treated. This motion preservation technique is appealing enough to catch our attention and has definitely reduced interest in AF. However, controversies exist concerning the superiority of C-ADR over standard anterior cervical discectomy and fusion (ACDF) [7, 8]. Furthermore, many patients are still treated with ACDF. The purpose of this study was to report the long-term clinical outcomes and radiographic data concerning the postoperative changes at both the operated and adjacent levels, to clarify the efficacy of AF in treatment of one- or two-level cervical radiculopathy and to show the degree to which motion is preserved.
Materials and methods
Patient population
Between November 1999 and June 2006, a total of 202 patients with degenerative one- or two-level cervical spondylosis with radiculopathy and with or without myelopathy, who did not respond to at least 6 weeks of conservative treatment, such as physical therapy, a reduction in activities, anti-inflammatory medications, and injections, underwent anterior cervical surgery. Among them, 50 were selected for AF. The inclusion criteria were an age of 20–69 years; diagnosis of unilateral one- or two-level cervical radiculopathy from a “soft” disc extrusion, spondylotic spur, or both; and radiological confirmation of the underlying pathology by magnetic resonance imaging (MRI) in all cases corresponding to the clinical symptoms. Patients were excluded if surgery had been previously carried out on the cervical spine. The patients with cervical myelopathy, cervical ossification of the posterior longitudinal ligament, kyphotic deformity or diminished vertebral canal diameter (Pavlov ratio <0.8) were also excluded. The remaining 152 patients with one- or two-level cervical radiculopathy who met the exclusion criteria were treated either with ACD and PEEK cage fusion (n = 107) or with ACD with iliac bone graft fusion with a titanium plate (n = 45). All procedures were performed by a single surgeon (Y.-K. Park).
Surgical procedure
A transuncal approach was performed in all cases [9]. A standard ACD approach was made with the skin incision located on the side of the lesion. After the longus colli muscle (LCM) was elevated, a cervical retractor was inserted, a regular sharp-tipped retractor blade was placed underneath the stripped LCM of the other side, and a half-width narrow blade was used to further retract the LCM on the side of the lesion, at which point the surgical microscope was introduced. The medial half of the LCM was incised and shifted laterally. A 5-mm burr, centered on the unco-vertebral joint, was used to drill straight down along the surface of the joint until the posterior surface was encountered. In agreement with previous authors [3, 6], we preserved a thin layer of the cortical bone of the lateral wall of the uncinate process to protect the vertebral artery. The drill hole was elliptically widened in a rostro-caudal direction and then the postero-lateral cortical layer and uncinate process were removed with a 1-mm punch. After removal, the herniated disc fragments were able to be mobilized with a microhook and removed with a microforcep. Next, the posterior longitudinal ligament was partly resected. Final decompression was achieved by resecting the base of the uncinate process and posterolateral osteophyte of the upper part, allowing them to be moved into the drilled cavity. We did not routinely remove these structures due to the risk of epidural bleeding from the venous plexus. When the path of the nerve root above and lateral to the pedicle of the lower vertebral body was finally decompressed and hemostasis was obtained using a gelatine sponge, the retractor was removed. The platysma and the skin were closed with absorbable sutures after the placement of suction drainage. The patients were mobilized the day after surgery and discharged after 4–7 days postoperatively. A surgical collar was used for 4–6 weeks.
Clinical outcome and radiographic assessments
Clinical outcomes were classified according to Odom et al. [10], which were obtained by trained, independent, and blinded nurse practitioners. The neck disability index (NDI) [11] and a 0- to 10-point visual analog scale for arm (VASa) and neck (VASn) pain were ascertained by self-assessment. These data were collected pre- and postoperatively [(at 4 and 12 months post-surgery and at the final follow-up (FU)] by one trained, independent and blinded nurse practitioner. To ascertain cases of adjacent- or same-segment disease, each patient’s complete medical record was reviewed. We used the criteria of Hilibrand et al. [12], in which a diagnosis is based on new radiculopathy or myelopathy symptoms referable to the same or an adjacent degenerated level on two consecutive visits, and a compressive lesion on MRI.
Radiographic measurements were performed on the lateral view of the pre- and postoperative cervical spine using the Patient Archiving Communication System (PACS) software. Disc height and the Cobb angle were measured in the neutral position. Segmental range of motion of the operated level was measured on dynamic lateral radiographs (Fig. 1). The height of the disc was measured along a straight line passing through the central points of the adjacent vertebral bodies. A disc height less than 10 % lower than the height of the C2/C3 disc was considered normal, a 10–20 % reduction was deemed mild degeneration, and a more than 20 % reduction was deemed severe. Radiological evidence of segmental degeneration was investigated by three reviewers (one neurosurgeon and two neurosurgical PGY 3 and 4 residents) and defined as increased or new narrowing of a disc space by more than 10 % [13] by consensus of two or more of the three reviewers.
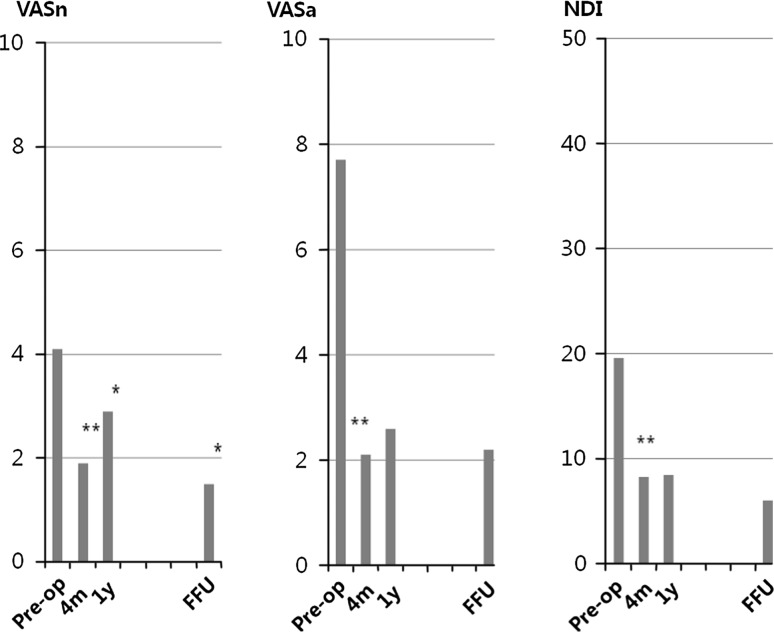
Fig. 1.
Clinical outcome measures (NDI and VAS) scores. Significant improvement occurred from baseline in all measures following anterior foraminotomy. A slight deterioration after 4 months was seen in the score for neck pain on the VAS. However, the score for arm pain and NDI results were sustainable and did not show significant change over time after 4 months. All measures were very satisfactory at final FU. NDI neck disability index, VAS visual analog scale. **p < 0.01, *p < 0.05
The magnification of all radiographs was corrected by the antero-posterior distance of the C2 vertebral body. Spontaneous bony fusion was evaluated by the absence of motion on flexion–extension radiographs and by visible bony bridges over the disc space.
Statistics
All data management and statistical analysis were performed using the Analyse-it software (Analyse-it Ltd, Leeds, UK). A paired t test was used to compare pre- and postoperative NDI, VAS, and the radiographic measurements. Fisher’s exact probability test was used to evaluate the difference between the upper and lower discs. Significance was accepted at a value of p < 0.05. Inter-rater reliability was evaluated by means of the Kappa coefficient.
Results
Demographics
The patients’ characteristics are shown in Table 1. There were 13 females and 37 males (age range 32–69 years, mean 51 ± 9 years). Single-level surgery was performed in 33 patients, and 17 were treated with consecutive two-level surgery. The most common operated spinal segments were C5–C6 (29 patients) and C6–C7 (27 patients). The most common presenting symptom was paresthesia. All patients had at least 1 year of FU, and 44 (88 %) had a final FU (mean 8.8 years; range 6.0–12.4 years) within 6 months of completion of this study. Follow-up examination was performed in 33 patients (66 %), and for a further 11 patients (22 %), telephone interviews were conducted. In six patients, data collection after 1 year was not possible.
Table 1.
Patients’ characteristics
| Number | Mean (range) | |
|---|---|---|
| Age (years) | 51 (32–69) | |
| Male/female | 37/13 | |
| Duration of symptoms (months) | ||
| Recent onset | 1.8 (0.25–6) | |
| <2 | 40 | |
| 2–12 | 10 | |
| Remote onset | 27.3 (1.5–240) | |
| <12 | 30 | |
| 12–36 | 7 | |
| >36 | 13 | |
| Symptoms (%) | ||
| Nuchal pain | 62 | |
| Shoulder pain | 66 | |
| Radicular pain | 76 | |
| Paresthesia | 82 | |
| Signs (%) | ||
| Sensory loss | 42 | |
| Motor weakness | 36 | |
| Decreased reflex | 36 | |
| Smoking (%) | ||
| Yes/no/missing | 38/52/10 | |
| Location (R/L) | 21/29 | |
| Operated levels (1-/2-) | 37/13 | 1.34 |
| C4–C5 | 8 | |
| C5–C6 | 29 | |
| C6–C7 | 27 | |
| C7–T1 | 3 | |
Early clinical outcomes
During the hospital stay after surgery, one patient complained of residual radicular symptoms similar to the preoperative status, but these became milder every day and finally disappeared at 6 weeks. Seven patients also reported some residual symptoms, but they were much weaker than preoperatively and subsided within 2 months. All eight subjects with residual symptoms required supplementary medical treatments including anti-inflammatory medication. The remaining 42 subjects reported that they were pain-free within 3 days after surgery (median, 0). One patient experienced transient hoarseness for 4 weeks, but there was no other noticeable complication. At discharge, 98 % of the patients reported improvement in their pain. At the 4-month FU, the average pain scores, which were preoperatively 4.1 in the neck (VASn) and 7.7 in the arm (VASa), improved postoperatively to 1.9 and 2.1, respectively (p < 0.0001 and p < 0.0000). In addition, the NDI improved from 19.6 to 8.3 (p < 0.0000) (Fig. 1). At the 1-year FU, the VASn had worsened to 2.9, a significant difference (p = 0.041); however, the VASa and NDI remained stable. The short-term outcome was excellent in 65 %, good in 29 % and fair in 6 %. No patient was left with significant radicular symptoms and no patient required repeat surgery for any reason within a year.
Long-term outcomes
Of the 50 consecutive cases included in this study, two patients died of unrelated causes at 4 and 7 years after surgery. Four patients moved after 1 year of FU without relocation notice. As a result, a total of 44 patients were available for FU examination or interview. No patient had required revision surgery for same-level recurrence or for secondary spinal instability. However, two patients (4.5 %) required additional surgery for adjacent-segment degeneration. One patient underwent surgery (ACDF) for a symptomatic lower-level disorder developed on the contra-lateral side at 18 months after the index operation at another institute. Another patient required posterior foraminotomy (PF) at the lower adjacent level on the same side after 11 years at our institute. Of the 33 patients who underwent final examination, 29 (88 %) achieved good or excellent (G/E) results. Of the 11 patients who had telephone interviews, 10 (91 %) reported G/E results. Overall, 39 patients (89 %) reported G/E results. Clinical status assessed by VASn, VASa, and NDI also remained very stable and satisfactory (Fig. 1). Regarding co-morbidity, seven patients had sought primary care for shoulder pain after the index operation, and six of these occurred on the side of the cervical radiculopathy. One of them had contra-lateral arm pain at POD 3 years, and had same side pain at POD 8 years. One patient described contra-lateral shoulder pain via a phone interview. The onset of pain unilateral to the index operation ranged from 4 months to 8 years (mean, 3.6 years). Three patients were diagnosed with adhesive capsulitis and three with a rotator cuff tear. Four patients recovered within 1 or 2 years after the onset, but one underwent surgery and one is still receiving conservative treatment. Three patients had four lumbar surgeries and three developed malignancy of other organs.
Radiological measurements
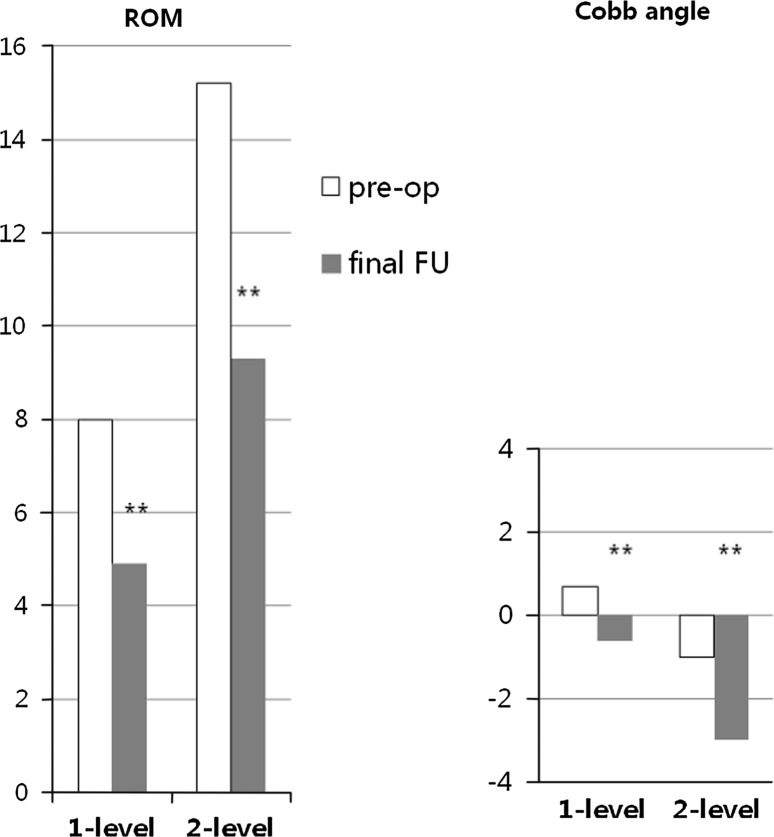
Pre- and postoperative radiographs were used to assess the severity of degenerative changes of the operated and adjacent segments in 33 patients who underwent a final FU examination; the results are summarized in Table 2. In four patients, data from the segment below were unobtainable due to invisibility of the C7–T1 segment on plain lateral radiographs. The majority of the operated levels had already shown certain degrees of disc degeneration before surgery. Only 9 of the 43 operated disc levels were initially identified as normal. In contrast, 18 of the 33 segments above and 23 of the 29 segments below were initially classified as normal. At final FU, a decrease in height was detected in all operated disc levels. Forty of the 43 operated levels were defined as degenerated. The remaining three also showed a decrease in height of somewhat less than 10 %. In agreement with the reduction in disc height, the mean segmental range of motion was also significantly reduced after surgery (from 8 to 4.9° in one-level, p < 0.0001, and from 15.2 to 9.3° in two-level, p < 0.0001), (Fig. 2). Spontaneous bony fusion with formation of anterior bony bridges occurred on four operated levels in three patients. However, the decrease in the segmental Cobb angle of the operated levels was minimal (−1.3° in one-level, p = 0.0002, −2° in two-level, p = 0.0005). In contrast to the operated levels, degeneration of the adjacent segment was minimal. The incidences of degenerative changes of the above and below segments were 6 and 11 %, respectively. The Kappa coefficients for the initial evaluation of disc degeneration status and sequential disc degeneration were 0.75 and 0.72, respectively. Kappa coefficients of 0.72–0.75 suggest good agreement among the observers.
Table 2.
Radiographic follow-up assessment of the segmental degenerative changes
| Pre-op status | Post-op change | |||||
|---|---|---|---|---|---|---|
| Above level | Operated level | Below level | ||||
| Same | Deg | Same | Deg | Same | Deg | |
| Normal | 17 | 1 | 0 | 9 | 21 | 2 |
| Mild | 10 | 1 | 0 | 26 | 3 | 0 |
| Severe | 4 | 0 | 3 | 5 | 2 | 1 |
| Total | 31 | 2 | 3 | 40 | 26 | 3 |
| Percentage | 94 | 6 | 7 | 93 | 89 | 11 |
Deg degenerated
Fig. 2.
Bar graph showing the follow-up of ROM and Cobb angle in patients who underwent 1- or 2-level AF from the preoperative status until final follow-up. Note a significant decrease in the range of motion and a small decrease in Cobb angle. **p < 0.01
Discussion
Cervical spondylosis and disc herniation are frequent causes of arm pain. In case conservative therapies fail operative intervention may be considered. The standard surgical technique is discectomy with or without fusion of the two adjacent vertebral bodies. ACDF has been reported to be a highly successful procedure with excellent clinical results and a relatively low rate of complications [14, 15]. However, long-term outcome studies increasingly emphasized the adverse effect of this procedure [12, 16]. These results led to development of C-ADR and revisiting of previous non-fusional procedures such as anterior or posterior foraminotomy (PF) for the treatment of cervical radiculopathy. AF was developed to avoid the complications associated with immobilization of the spine. Several studies reported that AF provided G/E outcomes in the short- [1–4] or mid-term [4–6], but no long-term studies have been conducted.
One of the interesting parts of this study is the inclusion of long-term radiographic outcomes after AF, which has also not been reported previously. In an attempt to maintain motion in the cervical spine, the patients underwent an uncovertebrectomy. However, our findings demonstrate that partial destruction of disc space, induced by the index procedure itself, seems primarily responsible for same-level degeneration. Aggravation of disc space narrowing was evident in all operated levels, together with restriction of the range of motion by about 40 %, and spontaneous fusion in 10 % (Fig. 3). Hence, as seen in ACD alone, same-level degeneration is the most striking radiological finding in patients who have undergone AF. In fact, it appears that disc space destruction correlates with spontaneous fusion. ACD leads to spontaneous bony fusion in 70–90 % of cases [17, 18] as a result of ongoing degeneration, which is assumed to be related to long-term deterioration of the clinical outcome [19]. Although there is no direct comparison with ACD, AF seems to induce less same-level degeneration, much less spontaneous fusion, and thus less long-term deterioration in the clinical outcome (Fig. 4). However, even in patients treated with C-ADR, heterotrophic ossification and similar amounts of spontaneous fusion occurred as a result of disc space destruction [20]. The possibility of spinal instability following resection of the unilateral uncovertebral joint has been suggested in some biomechanical studies [21, 22]. However, until recently there were no short- or mid-term studies of AF demonstrating clinical worsening due to the presence of postoperative spinal instability [4, 23]. Although slight but significant worsening of VASn was observed at 1-year FU, compared to 4-month FU, this is thought to be a clinical reflection of the postoperative ongoing degeneration, and could be a symptom of iatrogenic segmental instability. Basically, more data are required to exclude this possibility or to clarify the cause and duration of VASn changes. Nonetheless, the long-term clinical data, as well as our radiographic findings support further use of this procedure.
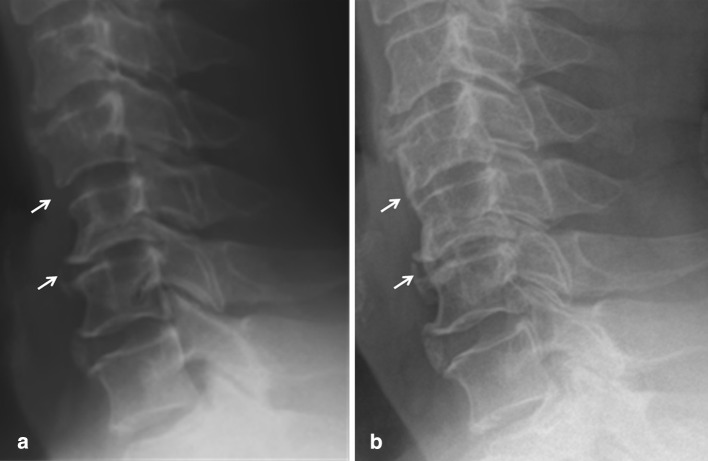
Fig. 3.
Lateral cervical radiographs obtained before (a) and at 1 (b) and 7 years (c) after C5/6 (arrows) AF in a 40-year-old male patient with soft disc herniation. This case showed remarkable postoperative reduction in disc height at the final FU. Aggravated disc degeneration is a routine radiological finding following AF. Early disc space narrowing (b) was followed by late spur formation (c). However, disc height reduction of the adjacent segments was not detected at 7 years and the segmental alignment had not changed markedly. This patient reported excellent results at the final FU
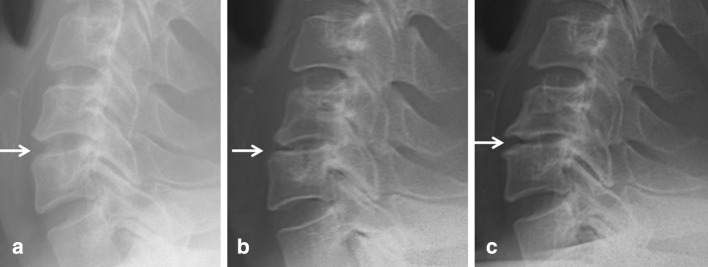
Fig. 4.
Lateral standard radiograph before (a) and 7 years after (b) C4–C5 and C5–C6 AF in a 69-year-old man. After 7 years, spontaneous fusion and bony bridge at the operated level occurred with little segmental loss of lordosis, while the heights of adjacent segment discs were largely unchanged. The clinical outcome of this patient was rated as excellent
To lessen violation of the disc space, some authors have used the so-called transcorporeal route [2, 23] or an anterolateral approach [4], which may prevent same-level degeneration. However, in our experience, removal of osteophytes and the uncinate process to perform bony decompression inevitably violates the posterolateral corner of the disc space, resulting in spillage of disc materials, narrowing of the disc space, and induction of degenerative processes. These sequelae are possible in every anterior approach that violates the disc space, regardless of the size of the opening; early disc height loss has already been described despite efforts to preserve the disc space [23]. Given this inherent disc-space narrowing, we used a wider foraminal decompression that offset both postoperative space narrowing or delayed spur formation and forgiving disc materials herniated through the iatrogenic opening to prevent same-level recurrence. So far, this strategy seems to be successful. Considering this postoperative disc-space narrowing and potential instability, the best candidate for AF is a patient with unilateral, mono- or bi-segmental radiculopathy mainly due to osseous foraminal stenosis with or without a lateral soft disc herniation. Some authors have reported that patients with pure soft disc herniation had shown better clinical outcomes [6]. However, AF in patients with normal or relatively mild degenerative disc disease usually leads to more rapid and prominent postoperative space narrowing than in those who are moderately or severely affected and who were relatively stable and rigid in motion due to a narrow space and a wide cross-sectional area of the end-plate related to degenerative spur formation. Hence, we recommend that patients with soft disc herniation with less degeneration of intervertebral discs undergo either C-ADR or PF.
In this small retrospective series, 89 % of patients had a favorable long-term clinical outcome after AF. Other than the two patients who required additional operations for adjacent-level disorders, only 3 of 42 patients reported a result worse than G/E (fair in all three cases), a success rate comparable with historical long-term PF data [24–27] and slightly better than those of ACD [19] or ACDF [12, 28, 29]. The PF is known to be a highly effective procedure for treatment of patients with cervical radiculopathy and results in long-lasting pain relief and improved quality-of-life outcomes in most patients in terms of motion preservation [27, 30]. In addition, no significant segmental degeneration or disc space narrowing is seen in AF, but only very small changes in focal or segmental kyphosis and segmental angulation were reported [30]. However, although it enables indirect bony decompression of the nerve root in cases of foraminal stenosis or removal of soft disc fragments, it does not allow removal of offending lesions located medioventral to the nerve root. Therefore, compared with the current technique, fewer adjacent-level disorders and more same-level recurrences are expected in the long term. To verify these issues, large-scale data on AF and comparative studies are required.
One interesting finding of long-term clinical FU is postoperative development of same side shoulder pain. The present patients were diagnosed with either adhesive capsulitis or rotator cuff tears at varying-level care centers, and their clinical courses were variable. Hence, the relationship between AF and delayed shoulder pathologies was not straightforward. However, the incidence reported herein (18.2 % in 8.8 years) is slightly higher than the reported annual incidence of shoulder pain in primary care centers (17.3 %/1,000/year in the 45- to 64-year age group) [31]. In addition, the side-specificity of shoulder pain (6:2, threefold higher on the same side) in this study was likely not due to simple coincidence. There must be a close association with pre-existing cervical radiculopathy or with the AF procedure itself. Despite having a history of shoulder pain, five patients reported G/E results, but one suffered a long period of bilateral shoulder pain and assessed the result as fair.
Radiographic assessment of adjacent-segment degeneration is the most complex and delicate part of this study, because there are no standard tools for assessment of this phenomenon. Many authors used the qualitative grading developed by Hilibrand et al. [12]. However, in this study, the semi-quantitative grading system used by Sugawara et al. [13] was adopted. First, the PACS software allows easy measuring of the height of the disc space. Second, the definition of degeneration (a more than 10 % loss of the original height) is more sensitive and practical. In fact, only 6–11 % of the adjacent segments were defined as degenerated according to the criteria in this study. Under the criteria commonly used in other studies, such as an increased or new narrowing of a disc space by more than 30 % [8, 32] or disc narrowing of more than 2 mm compared with adjacent segments [33], virtually no level could be defined as degenerated. Finally, exclusion of qualitative and subjective parameters, such as the presence of new anterior osteophyte formation, enlargement of existing osteophytes, or new or increasing anterior longitudinal ligament calcification, is another method of reducing inter-observer variation, although these are definitive clues of degeneration.
This study has several limitations. Because of its retrospective case observational design, direct comparisons with other available surgical options such as ACDF, PF, or C-ADR were not possible. In addition, some important characteristics, such as primary outcome measures, radiographic check-up results, and the onset, location, and duration of postoperative symptoms, were not regularly or precisely recorded. In addition, the small population size may have limited our ability to detect statistically meaningful differences. Therefore, large-scale comparative studies and prospective multicenter randomized controlled trials are necessary to confirm these results. Notwithstanding these limitations, our findings are both novel and significantly different from other published data, indicating the need for further investigation.
Conclusion
In this retrospective study, patients treated with AF for one- or two-level cervical radiculopathy showed a good long-term outcome with minimal adjacent-segment degeneration. Radiographic evidence of segmental loss of lordosis at the operated level was common at FU, but was minimal without any apparent delayed clinical effects after an average of 8.8 years following surgery. However, this technique is not recommended in cases with demonstrated instability or pre-existing segmental kyphosis. More data should be collected to clarify the clinical implications of our findings, such as delayed shoulder problems and aggravation of degeneration at the operated level.
Conflict of interest
None.
References
- 1.Johnson JP, Filler AG, McBride DQ, Batzdorf U. Anterior cervical foraminotomy for unilateral radicular disease. Spine (Phila Pa 1976) 2000;25:905–909. doi: 10.1097/00007632-200004150-00002. [DOI] [PubMed] [Google Scholar]
- 2.Jho HD, Kim WK, Kim MH. Anterior microforaminotomy for treatment of cervical radiculopathy: part 1—disc-preserving “functional cervical disc surgery”. Neurosurgery. 2002;51:S46–S53. [PubMed] [Google Scholar]
- 3.Saringer W, Nobauer I, Reddy M, Tschabitscher M, Horaczek A. Microsurgical anterior cervical foraminotomy (uncoforaminotomy) for unilateral radiculopathy: clinical results of a new technique. Acta Neurochir (Wien) 2002;144:685–694. doi: 10.1007/s00701-002-0953-2. [DOI] [PubMed] [Google Scholar]
- 4.Cornelius JF, Bruneau M, George B. Microsurgical cervical nerve root decompression via an anterolateral approach: clinical outcome of patients treated for spondylotic radiculopathy. Neurosurgery. 2007;61:972–980. doi: 10.1227/01.neu.0000303193.64802.8f. [DOI] [PubMed] [Google Scholar]
- 5.Balasubramanian C, Price R, Brydon H. Anterior cervical microforaminotomy for cervical radiculopathy—results and review. Minim Invasive Neurosurg. 2008;51:258–262. doi: 10.1055/s-0028-1082320. [DOI] [PubMed] [Google Scholar]
- 6.Pechlivanis I, Brenke C, Scholz M, Engelhardt M, Harders A, Schmieder K. Treatment of degenerative cervical disc disease with uncoforaminotomy—intermediate clinical outcome. Minim Invasive Neurosurg. 2008;51:211–217. doi: 10.1055/s-2008-1080914. [DOI] [PubMed] [Google Scholar]
- 7.Jawahar A, Cavanaugh DA, Kerr EJ, 3rd, Birdsong EM, Nunley PD. Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in the cervical spine: results of 93 patients in three prospective randomized clinical trials. Spine J. 2010;10:1043–1048. doi: 10.1016/j.spinee.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Maldonado CV, Paz RD, Martin CB. Adjacent-level degeneration after cervical disc arthroplasty versus fusion. Eur Spine J. 2011;20(Suppl 3):403–407. doi: 10.1007/s00586-011-1916-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jho HD. Microsurgical anterior cervical foraminotomy for radiculopathy: a new approach to cervical disc herniation. J Neurosurg. 1996;84:155–160. doi: 10.3171/jns.1996.84.2.0155. [DOI] [PubMed] [Google Scholar]
- 10.Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 1958;166:23–28. doi: 10.1001/jama.1958.02990010025006. [DOI] [PubMed] [Google Scholar]
- 11.Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–415. [PubMed] [Google Scholar]
- 12.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Sugawara T, Itoh Y, Hirano Y, Higashiyama N, Mizoi K. Long term outcome and adjacent disc degeneration after anterior cervical discectomy and fusion with titanium cylindrical cages. Acta Neurochir (Wien) 2009;151:303–309. doi: 10.1007/s00701-009-0217-5. [DOI] [PubMed] [Google Scholar]
- 14.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of 122 patients. J Bone Joint Surg Am. 1993;75:1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Teramoto T, Ohmori K, Takatsu T, Inoue H, Ishida Y, Suzuki K. Long-term results of the anterior cervical spondylodesis. Neurosurgery. 1994;35:64–68. doi: 10.1227/00006123-199407000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 1999;24:670–675. doi: 10.1097/00007632-199904010-00011. [DOI] [PubMed] [Google Scholar]
- 17.Savolainen S, Rinne J, Hernesniemi J. A prospective randomized study of anterior single-level cervical disc operations with long-term follow-up: surgical fusion is unnecessary. Neurosurgery. 1998;43:51–55. doi: 10.1097/00006123-199807000-00032. [DOI] [PubMed] [Google Scholar]
- 18.Palma L, Mariottini A, Carangelo B, Muzii VF, Zalaffi A. Favourable long-term clinical outcome after anterior cervical discectomy. A study on a series of 125 patients undergoing surgery a mean of 11 years earlier. Acta Neurochir (Wien) 2010;152:1145–1152. doi: 10.1007/s00701-010-0650-5. [DOI] [PubMed] [Google Scholar]
- 19.Nandoe Tewarie RD, Bartels RH, Peul WC. Long-term outcome after anterior cervical discectomy without fusion. Eur Spine J. 2007;16:1411–1416. doi: 10.1007/s00586-007-0309-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu JC, Huang WC, Tsai HW, Ko CC, Fay LY, Tu TH, Wu CL, Cheng H. Differences between 1- and 2-level cervical arthroplasty: more heterotopic ossification in two-level disc replacement. J Neurosurg Spine. 2012 doi: 10.3171/2012.2.SPINE111066. [DOI] [PubMed] [Google Scholar]
- 21.Kotani Y, McNulty PS, Abumi K, Cunningham BW, Kaneda K, McAfee PC. The role of anteromedial foraminotomy and the uncovertebral joints in the stability of the cervical spine. A biomechanical study. Spine (Phila Pa 1976) 1998;23:1559–1565. doi: 10.1097/00007632-199807150-00011. [DOI] [PubMed] [Google Scholar]
- 22.Chen BH, Natarajan RN, An HS, Andersson GB. Comparison of biomechanical response to surgical procedures used for cervical radiculopathy: posterior keyhole foraminotomy versus anterior foraminotomy and discectomy versus anterior discectomy with fusion. J Spinal Disord. 2001;14:17–20. doi: 10.1097/00002517-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Choi G, Lee SH, Bhanot A, Chae YS, Jung B, Lee S. Modified transcorporeal anterior cervical microforaminotomy for cervical radiculopathy: a technical note and early results. Eur Spine J. 2007;16:1387–1393. doi: 10.1007/s00586-006-0286-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clarke MJ, Ecker RD, Krauss WE, McClelland RL, Dekutoski MB. Same-segment and adjacent-segment disease following posterior cervical foraminotomy. J Neurosurg Spine. 2007;6:5–9. doi: 10.3171/spi.2007.6.1.2. [DOI] [PubMed] [Google Scholar]
- 25.Korinth MC, Kruger A, Oertel MF, Gilsbach JM. Posterior foraminotomy or anterior discectomy with polymethyl methacrylate interbody stabilization for cervical soft disc disease: results in 292 patients with monoradiculopathy. Spine (Phila Pa 1976) 2006;31:1207–1214. doi: 10.1097/01.brs.0000217604.02663.59. [DOI] [PubMed] [Google Scholar]
- 26.Silveri CP, Simpson JM, Simeone FA, Balderston RA. Cervical disk disease and the keyhole foraminotomy: proven efficacy at extended long-term follow up. Orthopedics. 1997;20:687–692. doi: 10.3928/0147-7447-19970801-07. [DOI] [PubMed] [Google Scholar]
- 27.Woertgen C, Rothoerl RD, Henkel J, Brawanski A. Long term outcome after cervical foraminotomy. J Clin Neurosci. 2000;7:312–315. doi: 10.1054/jocn.1999.0669. [DOI] [PubMed] [Google Scholar]
- 28.Gore DR, Sepic SB. Anterior discectomy and fusion for painful cervical disc disease. A report of 50 patients with an average follow-up of 21 years. Spine (Phila Pa 1976) 1998;23:2047–2051. doi: 10.1097/00007632-199810010-00002. [DOI] [PubMed] [Google Scholar]
- 29.Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 2005;30:2138–2144. doi: 10.1097/01.brs.0000180479.63092.17. [DOI] [PubMed] [Google Scholar]
- 30.Jagannathan J, Sherman JH, Szabo T, Shaffrey CI, Jane JA. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: a single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J Neurosurg Spine. 2009;10:347–356. doi: 10.3171/2008.12.SPINE08576. [DOI] [PubMed] [Google Scholar]
- 31.van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54:959–964. doi: 10.1136/ard.54.12.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine. 2005;3:417–423. doi: 10.3171/spi.2005.3.6.0417. [DOI] [PubMed] [Google Scholar]
- 33.Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004;4:624–628. doi: 10.1016/j.spinee.2004.04.011. [DOI] [PubMed] [Google Scholar]