Abstract
Purpose
To determine whether motion preservation following oblique cervical corpectomy (OCC) for cervical spondylotic myelopathy (CSM) persists with serial follow-up.
Methods
We included 28 patients with preoperative and at least two serial follow-up neutral and dynamic cervical spine radiographs who underwent OCC for CSM. Patients with an ossified posterior longitudinal ligament (OPLL) were excluded. Changes in sagittal curvature, segmental and whole spine range of motion (ROM) were measured. Nathan’s system graded anterior osteophyte formation. Neurological function was measured by Nurick’s grade and modified Japanese Orthopedic Association (JOA) scores.
Results
The majority (23 patients) had a single or 2-level corpectomy. The average duration of follow-up was 45 months. The Nurick’s grade and the JOA scores showed statistically significant improvements after surgery (p < 0.001). 17 % of patients with preoperative lordotic spines had a loss of lordosis at last follow-up, but with no clinical worsening. 77 % of the whole spine ROM and 62 % of segmental ROM was preserved at last follow-up. The whole spine and segmental ROM decreased by 11.2° and 10.9°, respectively (p ≤ 0.001). Patients with a greater range of segmental movement preoperatively had a statistically greater range of movement at follow-up. The analysis of serial radiographs indicated that the range of movement of the whole spine and the range of movement at the segmental spine levels significantly reduced during the follow-up period. Nathan’s grade showed increase in osteophytosis in more than two-thirds of the patients (p ≤ 0.01). The whole spine range of movement at follow-up significantly correlated with Nathan’s grade.
Conclusions
Although the OCC preserves segmental and whole spine ROM, serial measurements show a progressive decrease in ROM albeit without clinical worsening. The reduction in this ROM is probably related to degenerative ossification of spinal ligaments.
Keywords: Cervical spondylotic myelopathy, Oblique corpectomy, Motion preservation, Range of motion, Cervical spine
Introduction
Surgical interventions to ameliorate progressive symptoms in cervical spondylotic myelopathy (CSM) have yielded good results via various approaches [1–7]. The oblique corpectomy has been used for over two decades and provides adequate decompression without the need for a graft or a stabilization device [8–15]. George et al. [16] introduced this procedure in 1992 and recommended it in patients with fused, degenerated spines in whom little movement was seen preoperatively. Since then, there is limited literature available on the results of oblique cervical corpectomy (OCC) and although good clinical outcomes have been reported, and there is insufficient data with regard to the maintenance of sagittal alignment and preservation of cervical motion [10–12, 15]. In a previous report, we demonstrated preserved cervical segmental motion at short-term follow-up in a younger cohort of patients with CSM who did not have hard, collapsed, fused disc spaces [17]. We undertook this study to determine whether this preserved motion persists in the long-term or whether progressive spinal fusion occurs to limit motion.
Methods
Patient population
Between 2001 and 2010 we operated on 153 patients with CSM using the OCC. In this study, we included only those 28 patients with complete sets of cervical lateral radiographs in flexion, extension and neutral positions on multiple annual follow-up visits beginning at least 1 year after surgery. Patients with ossified posterior longitudinal ligament (OPLL) were excluded. Their preoperative clinical and radiological data were entered into a proforma and subsequently into a database. Patients presenting with myelopathy underwent a detailed neurological examination, including assessment of functional status using the Nurick’s grading system [18] and a modified Japanese Orthopedic Association (JOA) scoring system for cervical myelopathy [19].
Radiological assessment
Patients were advised to return for follow-up annually after surgery or to send lateral cervical spine radiographs in neutral, flexion and extension views by post along with a questionnaire for the Nurick’s grade and JOA scores. Images done elsewhere were scanned into and stored on a general electric (GE) centricity 1.0 picture archival and retrieval computer system (PACS) server and measurements performed on GE Centricity 1.0 PACS workstations. Whole spine curvature was defined in relation to a line joining the postero-inferior edge of C2 to the postero-inferior edge of C7. The spine was called lordotic when the posterior surfaces of the C3–6 bodies were anterior to the line, straight when at least one vertebral body touched the line, and kyphotic when even one body lay behind the line. Whole spine range of motion (ROM) was measured directly on the workstation using the Cobb angles between the lower endplate of C2 and the upper endplate of C7 on lateral cervical radiographs in flexion and extension. The ROM was computed from the angles in flexion and extension. A minus sign was prefixed to the ROM in kyphotic spines.
The segmental angle at the level operated was measured using Cobb’s method on lateral cervical radiographs, that is, the angle between the lower endplate of the vertebra above and the upper endplate of the vertebra below the operated segment. Thus, for a C5 corpectomy, the upper line was on the inferior end plate of C4, and the lower line was on the superior end plate of C6. The segmental ROM was calculated from the segmental Cobb angle in flexion and extension.
The measurements were done independently by two authors (MT and SS) on their computers after doing a few trial measurements together to arrive at a protocol. Because the interobserver co-relation was 0.89, for further statistics we utilized the reading of one observer (MT) rather than the mean value of the two observers. In the event of a disparity of more than 10°, the images were reviewed by the senior author (AGC) and his measurements were taken as the final value.
Surgical technique
Only a brief description of the technique of the OCC will be made here since it has been described in detail before [9]. Through a longitudinal skin incision along the anterior border of the right sternocleidomastoid muscle, the carotid sheath is retracted medially to expose the transverse processes of the cervical vertebrae. The sympathetic chain lying on the longus colli is generally retracted medially, but on occasion when it is situated far laterally it is retracted laterally. The vertebral artery (VA) lies unprotected between two consecutive vertebrae, but is protected above C6 in the foramen transversarium by the costotransverse bar of the transverse process. The microscope is brought in and the diamond drill is used to thin down the costotransverse bar to the periosteum over the VA. An 8-mm cutting burr is then used to make a vertical trough down to the posterior longitudinal ligament on the lateral part of the vertebral body leaving about 3 mm of cortical bone to protect the VA laterally. Drilling then continues obliquely across to the contralateral side of canal along the posterior cortical margin minimizing vertebral body removal. Hemostasis is secured with particular attention to the epidural venous plexus and a tube drain is left in situ in the depth of the field. Postoperatively, the patient is mobilized on the same day and discharged after 2–3 days.
Statistics
We calculated descriptive statistics; mean and standard deviation for continuous variables and frequency and percentages for categorical variables. The Pearson’s correlation coefficient was used to assess the significance of association between continuous variables while the Student’s t test and ANOVA were used to test the significance of continuous variables when groups were compared. The paired t test was employed to assess the significance of changes in continuous variables and the Wilcoxon’s signed ranks test for change in categorical variables over time.
Results
All patients presented with gait difficulty. Paresthesiae was the next most common presentation seen in 24 (85.7 %) patients, Romberg’s sign was positive in 12 (42.8 %), bladder involvement was seen in 6 (21.4 %). Radicular pain was present in only two patients. The socio-demographic and clinical characteristics of the sample are shown in Table 1. The majority of patients were middle-aged and males. Most patients had a two vertebral level procedure with the C5 oblique corpectomy being the commonest. The average duration of follow-up was 45.1 months (range 12–116 months).
Table 1.
Clinical characteristics of 28 patients undergoing oblique corpectomy for CSM
| Characteristic | Mean (SD) | Frequency (%) |
|---|---|---|
| Age (in years) | 50.75 (11.55) | |
| Sex (male) | 24 (85.7) | |
| C4 oblique corpectomy | 14 (50.0) | |
| C5 oblique corpectomy | 19 (67.9) | |
| C6 oblique corpectomy | 17 (60.7) | |
| Number of vertebral levels | ||
| 1 | 11 (39.3) | |
| 2 | 12 (42.9) | |
| 3 | 5 (17.9) | |
| Total duration of follow-up after surgery in months (SD) | 45.14 (24.03) | |
Table 2 records the pre, postoperative and follow-up assessments. The average percentage change in whole spine range of movement was −24.9, −9.4, −26.7 % for 1, 2 and 3 level corpectomies, respectively. The average percentage change in segmental range of movement was −35.1, −36.9, −25.2 % for 1, 2 and 3 level corpectomies respectively. The change of range of movement over time and the percentage change of range of movement for both whole spine and segmental levels were not statistically associated with the number of level of corpectomy done.
Table 2.
Neurological and radiological assessment at baseline and on serial follow-up
| Characteristic | Mean (SD) | |||||||
|---|---|---|---|---|---|---|---|---|
| Preop (n = 28) | Year 1 (n = 28) | Year 2 (n = 28) | Year 3 (n = 15) | Year 4 (n = 6) | Year 5 (n = 2) | Last assessment (n = 28) | Change from baseline to last assessment | |
| Nurick’s score | 3.39 (0.88) | – | – | – | – | – | 2.11 (0.69) | −1.29 (0.90)a,c |
| JOA score | 12.00 (2.09) | – | – | – | – | – | 14.96 (1.43) | +2.96 (2.44)a,c |
| Whole spine range of movement | 49.70 (14.09) | 37.17 (13.50) | 39.71 (12.72) | 40.97 (10.88) | 37.53 (16.55) | 49.30 (6.22) | 38.47 (11.56) | −11.24 (15.48)a,c |
| Segmental range of movement | 28.74 (12.56) | 19.05 (10.50) | 18.35 (10.72) | 17.54 (10.35) | 12.52 (6.63) | 11.70 (3.39) | 17.83 (10.55) | −10.90 (10.27)a,c |
| Nathan’s grade | 2.04 (0.96) | – | – | – | – | 3.11 (0.79) | −1.07 (0.81)b,c | |
aPaired t test
bWilcoxon’s signed rank test
cp < 0.001
Although Nurick and JOA scores improved significantly during the immediate postoperative period after surgery, the range of movement of the whole spine and range of movement at the segmental spine levels significantly reduced during the follow-up period. There was no statistically significant correlation between baseline and last follow-up whole spine range of movement. However, the correlation between baseline and last follow-up segmental range of movement (Corr. coeff = 0.62; p = 0.000) was statistically significant suggesting that those with greater range of segmental movement preoperatively, had a greater range of movement at follow-up. At follow–up, the number of levels of vertebrae involved in the corpectomy was significantly associated with segmental range of movement (Anova F = 4.83; p = 0.017), but not with the whole spine range of movement.
The whole spine range of movement at follow-up significantly correlated pre (Corr coeff = −0.497; p = 0.007) and post-op (Corr coeff = −0.432; p = 0.022) Nathan’s grades. However, the correlation of these grades with segmental range of movement was not statistically significant.
The whole spine range of movement at follow-up was negatively associated with the age (Corr coeff = −0.402; p = 0.034), duration of symptoms (Corr coeff = −0.404; p = 0.033) and segmental movement at follow-up (Corr coeff = −0.432; p = 0.022). However, it did not correlate with sex, pre and post-op Nurick and pre and post-op JOA scores. Segmental range of movement was not correlated with the age, sex, duration of symptoms, Nurick and JOA scores.
Table 3 shows the change in whole spine curvature and the incidence of kyphosis. In the assessment of whole spine curvature, 23 (82.1 %) patients had lordotic spines, 4 (14.3 %) were straight while 1 (3.5 %) was kyphotic. A substantial majority of patients (82.6 %) with lordotic spines continued to have lordosis postoperatively, the remaining developed a straight spine (17.4 %) and none became kyphotic. There was no worsening of neurological status in these patients. The majority of patients (75 %) with preoperative straight spines continued to have straight spines and one became lordotic. The one patient with a kyphotic spine showed no change in curvature.
Table 3.
Preoperative versus postoperative spine curvatures in 28 patients with CSM at mean follow-up of 45 months
| Preop curvature | Postoperative cervical spine curvature | |||
|---|---|---|---|---|
| Lordotic | Straight | Kyphotic | ||
| Lordotic | 19 | 4 | 0 | 23 |
| Straight | 1 | 3 | 0 | 4 |
| Kyphotic | 0 | 0 | 1 | 1 |
| 20 | 7 | 1 | 28 | |
Table 4 shows the development of osteophyte formation in pre- and postoperative radiographs as assessed by the Nathans’s grading system [20]. Nathan’s grade increased postoperatively two-third of our patients. In 10 patients, the postoperative grade was one grade worse. In 10, it was two grades worse and in 8 patients, the Nathan’s grade was unchanged.
Table 4.
Pre and postoperative Nathan’s grading in 28 patients with CSM
| Preop grade | Postoperative Nathan’s Grade | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| 1 | 0 | 5 | 4 | 0 |
| 2 | 0 | 2 | 4 | 6 |
| 3 | 0 | 0 | 3 | 1 |
| 4 | 0 | 0 | 0 | 3 |
Bold numbers indicate those patients who did not have any change in Nathan’s grade
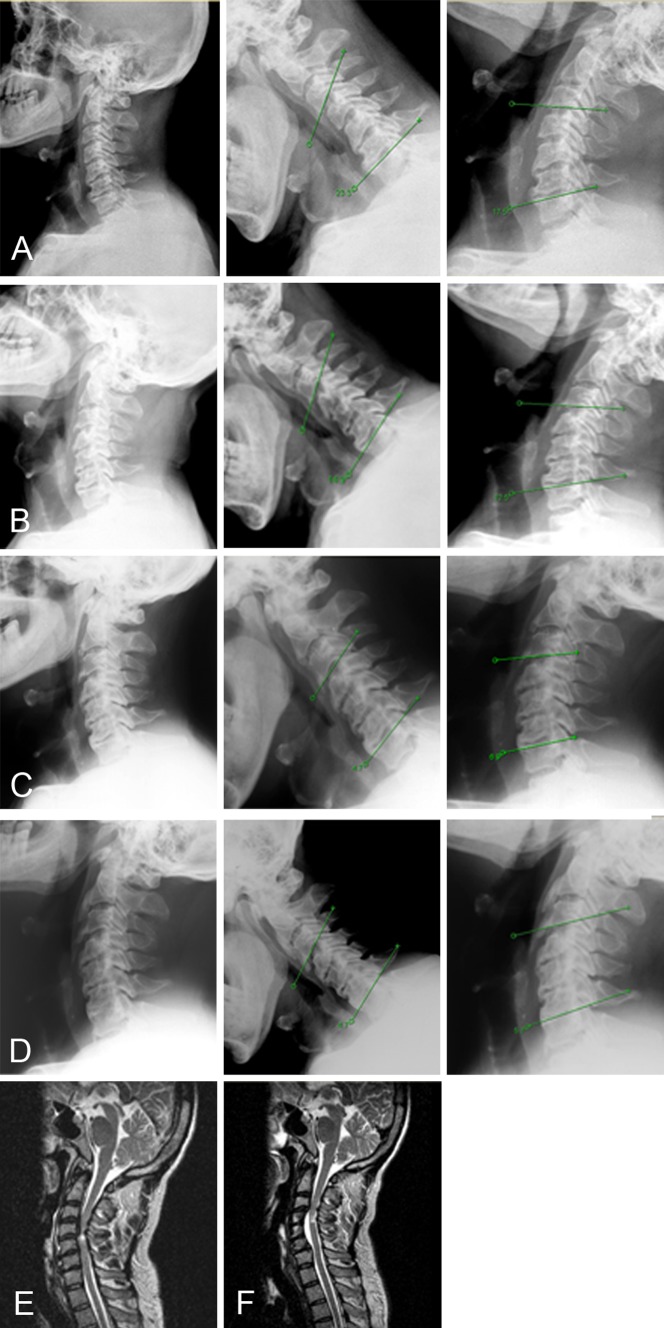
Figure 1 shows the preoperative and postoperative MR images and cervical spine radiographs in neutral, flexion and extension of a patient who underwent the OCC for CSM with long-term follow-up.
Fig. 1.
Preoperative (a) and serial postoperative follow-up cervical spine radiographs in neutral, flexion and extension (b, c, d) of a 47-year-old man who underwent a C4, 5, 6 OCC for CSM. The preoperative range of segmental motion was 40.8° (a), which subsequently reduced to 27.4° (b), 11.6° (c) and 10.4° (d) at 12, 30 and 60 months follow-up, respectively. The whole spine range of motion also reduced significantly from a preoperative value of 41.2° to 33.2°, 25.8° and 15.5° on serial follow-up. Note the progression of osteophytes, from a preoperative Nathan grade 2 (a) to grade of 4 at last follow-up (d). Pre- and postoperative MR sagittal views demonstrate decompression of the cord (e, f)
Discussion
Sagittal balance, segmental and whole spine range of motion
The main advantage of the OCC is that following the limited vertebral body resection no grafting or instrumentation is required. George et al. [16] reported preservation of sagittal alignment in the majority of their cases with no more than a 5° kyphotic change at the operated segment. Because they restrict the use of the OCC to those patients who had collapsed hard discs they did not discuss preservation of motion as most of these spines were rigid. In a previous report, we found a 4.7° mean loss of lordosis at the operated segments in patients undergoing the OCC at short-term follow-up contributing to a straightening of the whole spine in a third of the patients [17]. Because the mean age in our cohort of cases was about 5–10 years less than that reported in western series, our patients did not have hard, degenerated discs and had preserved cervical motion on flexion and extension before surgery. As the OCC does not involve fusing the spine, we therefore presumed that the preoperative cervical motion would be preserved postoperatively. Other western series do not comment on motion preservation since they were dealing with a population with more degenerated spines. Interestingly cadaver studies after OCC confirm an approximately 15 % increase in the range of segmental motion when compared with normal non-operated spines [21]. These in vitro studies cannot be simply transposed to in vivo practice as a result of limitations induced by the lack of muscle, healing and adaptation. We lacked early dynamic postoperative radiographs to comment on whether our patients had increased spine mobility immediately after surgery as we did not wish to subject them to discomfort. However, our previous radiological findings clearly show that more than 50 % of segmental motion is preserved at a mean follow-up of 2.5 years. [17].
In the present study, we included only those patients with serial imaging over a longer duration (mean 45 months). Our data show that although there is initial preservation of cervical motion after OCC, the ROM reduces with time; however, it appears that there was a mean residual segmental range of movement of 17° and residual whole spine range of movement of 38° at the last follow-up. This progressive reduction in movement had no clinical repercussions, since there was a significant improvement in the clinical grading at follow-up. In addition, those patients with a greater range of segmental motion preoperatively had greater preservation of motion at last follow-up arguing for the use of the oblique corpectomy without fusion for this group of patients.
Studies in patients with neck pain [22] without radiological evidence of spine degeneration clearly demonstrate a progressive reduction in segmental ROM with age, amounting to approximately 5° for every 10 years of aging. On the other hand, patients with preexisting degenerative spines tend to lose cervical motion more rapidly with aging. It may be pertinent to mention here that studies on cervical arthroplasty [23] that intend to preserve motion have shown that only 21 % of patients maintained physiological movement and complete fusion occurs in 19 % of patients at 2 years probably due to heterotropic ossification. Progression of ossification seems to be directly proportional to the duration of follow-up and cervical ROM was restricted in those patients with extensive ossification [24]; a phenomenon noted in our group of patients as well. The exact cause of heterotopic ossification is unclear, but has been attributed to the presence of bone dust, exposure of bone marrow after drilling of the endplates, dissection of the longus colli muscles or increased tendency to fusion when range of motion is decreased.
Osteophyte progression and range of movement of the adjacent segments
Patients undergoing corpectomy or discectomy with bone grafting tend to have a 2°–8° increase in adjacent segment ROM, with a third of patients developing osteophytes in the adjacent segments and no new degenerative changes at the fused level [25–27]. This accelerated osteophytic degeneration is attributed to the increased adjacent segment ROM. We noticed extensive osteophyte progression in two-thirds of our cases, more pronounced at the level of surgery, but also at the adjacent segments cranially and caudally in about 50 % of cases. Given the increased range of segmental movement noted after the OCC in cadaveric studies, it is likely that the increased osteophytes at the operated segment represents natures attempt at reducing movement. Interestingly, our patients showed no change in adjacent segment mobility; in fact the reduction in the whole spine ROM is completely explained by the reduction in movement at the operated segment—the mean segmental and whole spine ROM decreased by 10.9° and 11.24°, respectively.
Motion preservation or fusion
The treatment of degenerative cervical spine disease has shown good clinical outcomes with rigid immobilization, physiotherapy, corpectomy/discectomy with and without fusion as well as with arthroplasty [27–30]. Fusion does accelerate radiological and clinical adjacent segment disease in the long-term as younger patients with fusion operated for traumatic spine injury seem to have these changes earlier [31]. Conversely, cervical arthroplasty that has the potential advantage of retaining cervical motion and perhaps decreasing the incidence of adjacent-segment degeneration, has not been proved to be superior to anterior cervical discoidectomy with fusion in the short-term, however, the need for revision surgery following arthroplasty is reported to be less than after fusion procedures [32]. Similarly, in the OCC, we noted asymptomatic accelerated degenerative changes at the level of surgery and the adjacent segment in two-thirds of our cases. This lack of correlation between radiological and clinical adjacent segment disease has been noticed by others as well [27, 32] and may be because the heterotopic ossification occurred in the anterior longitudinal ligament and not posteriorly where it would be more likely to cause neurological symptoms through cord or root compression. As more long-term data on motion preservation and adjacent segment disease accrues, the clinical relevance of preserving motion in cervical spondylotic myelopathy may be determined.
Limitations of the study
Limitations inherent to this study include its retrospective analysis, although clinical functional grade was assigned prospectively. The small sample size is another drawback of this paper since we only included those patients with complete sets of neutral flexion, extension, lateral radiographs on serial follow-up.
Conclusions
The OCC provides significant clinical improvement in patients with CSM at long-term follow-up. Although 77 % of the whole spine ROM and 62 % of segmental ROM is preserved at last follow-up, serial annual plain radiographs show a gradual reduction in movement. The reduction in motion is probably due to the progression of anterior osteophytes at and adjacent to the operated level.
Acknowledgments
The authors would like to acknowledge Debashree Turel and Dr K. Srinivas Babu for their assistance in the artwork.
Conflict of interest
The authors report no financial support or conflict of interest.
Abbreviations
- CSM
Cervical spondylotic myelopathy
- GE
General electric
- JOA
Japanese Orthopedic Association
- MRI
Magnetic resonance imaging
- OCC
Oblique cervical corpectomy
- OPLL
Ossified posterior longitudinal ligament
- PACS
Picture archival and retrieval system
- ROM
Range of movement
- VA
Vertebral artery
Contributor Information
Mazda K. Turel, Email: mazdaturel@gmail.com
Sauradeep Sarkar, Email: sauradeepsarkar@gmail.com.
Krishna Prabhu, Email: krishnaprabhu@cmcvellore.ac.in.
Roy T. Daniel, Email: roy.daniel@chuv.ch
K. S. Jacob, Email: ksjacob@cmcvellore.ac.in
Ari G. Chacko, Phone: +91-416-2283031, Phone: +91-9487519464, FAX: +91-416-2232103, Email: agchacko@cmcvellore.ac.in
References:
- 1.Liu Y, Qi M, Chen H, Yang L, Wang X, Shi G, Gao R, Wang C, Yuan W. Comparative analysis of complications of different reconstructive techniques following anterior decompression for multilevel cervical spondylotic myelopathy. Eur Spine J. 2012;21(12):2428–2435. doi: 10.1007/s00586-012-2323-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajshekhar V, Muliyil J. Patient perceived outcome after central corpectomy for cervical spondylotic myelopathy. Surg Neurol. 2007;68:185–190. doi: 10.1016/j.surneu.2006.10.071. [DOI] [PubMed] [Google Scholar]
- 3.Houten JK, Cooper PR. Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment, spinal cord compression, and neurological outcome. Neurosurgery. 2003;52:1081–1097. doi: 10.1227/01.NEU.0000057746.74779.55. [DOI] [PubMed] [Google Scholar]
- 4.Song KJ, Lee KB, Song JH. Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J. 2012;21(8):1551–1557. doi: 10.1007/s00586-012-2296-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costa F, Tomei M, Sassi M, Cardia A, Ortolina A, Servello D, Fornari M. Evaluation of the rate of decompression in anterior cervical corpectomy using an intra-operative computerized tomography scan (O-Arm system) Eur Spine J. 2012;21(2):359–363. doi: 10.1007/s00586-011-2028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin Q, Zhou X, Wang X, Cao P, Tsai N, Yuan W. A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy. Eur Spine J. 2011;21(3):474–481. doi: 10.1007/s00586-011-1961-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kristof RA, Kiefer T, Thudium M, Ringel F, Stoffel M, Kovacs A, Mueller CA. Comparison of ventral corpectomy and plate-screw-instrumented fusion with dorsal laminectomy and rod-screw-instrumented fusion for treatment of at least two vertebral-level spondylotic cervical myelopathy. Eur Spine J. 2009;18(12):1951–1956. doi: 10.1007/s00586-009-1110-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bruneau M, Cornelius JF, George B. Multilevel oblique corpectomies: surgical indications and technique. Neurosurgery. 2007;61:106–112. doi: 10.1227/01.neu.0000289723.89588.72. [DOI] [PubMed] [Google Scholar]
- 9.Chacko AG, Daniel RT. Multilevel cervical oblique corpectomy in the treatment of ossified posterior longitudinal ligament in the presence of ossified anterior longitudinal ligament. Spine. 2007;32(20):E575–E580. doi: 10.1097/BRS.0b013e31814b84fe. [DOI] [PubMed] [Google Scholar]
- 10.Chibbaro S, Mirone G, Makiese O, George B. Multilevel oblique corpectomy without fusion in managing cervical myelopathy: long-term outcome and stability evaluation in 268 patients. J Neurosurg Spine. 2009;10(5):458–465. doi: 10.3171/2009.1.SPINE08186. [DOI] [PubMed] [Google Scholar]
- 11.Kiris T, Kilincer C. Cervical spondylotic myelopathy treated by oblique corpectomy: a prospective study. Neurosurgery. 2008;62(3):674–682. doi: 10.1227/01.neu.0000317316.56235.a7. [DOI] [PubMed] [Google Scholar]
- 12.Koc RK, Menku A, Akdemir H, Tucer B, Kurtsoy A, Oktem IS. Cervical spondylotic myelopathy and radiculopathy treated by oblique corpectomies without fusion. Neurosurg Rev. 2004;27(4):252–258. doi: 10.1007/s10143-004-0342-9. [DOI] [PubMed] [Google Scholar]
- 13.Moses V, Daniel RT, Chacko AG. The value of intraoperative ultrasound in oblique corpectomy for cervical spondylotic myelopathy and ossified posterior longitudinal ligament. Br J Neurosurg. 2010;24:518–525. doi: 10.3109/02688697.2010.504049. [DOI] [PubMed] [Google Scholar]
- 14.Turel MK, Chacko AG. Delayed resolution of extensive T2-weighted intramedullary signal changes after oblique corpectomy for cervical spondylotic myelopathy. Br J Neurosurg. 2011;25(6):772–774. doi: 10.3109/02688697.2011.584989. [DOI] [PubMed] [Google Scholar]
- 15.Rocchi G, Caroli E, Salvati M, Delfini R. Multilevel oblique corpectomy without fusion: our experience in 48 patients. Spine. 2005;30(17):1963–1969. doi: 10.1097/01.brs.0000176327.04725.1b. [DOI] [PubMed] [Google Scholar]
- 16.George B, Gauthier N, Lot G. Multisegmental cervical spondylotic myelopathy and radiculopathy treated by multilevel oblique corpectomies without fusion. Neurosurgery. 1999;44(1):81–90. doi: 10.1097/00006123-199901000-00046. [DOI] [PubMed] [Google Scholar]
- 17.Chacko AG, Joseph M, Turel MK, Prabhu K, Daniel RT, Jacob KS. Multilevel oblique corpectomy for cervical spondylotic myelopathy preserves segmental motion. Eur Spine J. 2012;21(7):1360–1367. doi: 10.1007/s00586-011-2137-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95(1):87. doi: 10.1093/brain/95.1.87. [DOI] [PubMed] [Google Scholar]
- 19.Benzel EC, Lancon J, Kesterson L, Hadden T. Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J Spinal Disord Tech. 1991;4(3):286. doi: 10.1097/00002517-199109000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Nathan H. Osteophytes of the Vertebral Column An Anatomical Study of Their Development According to Age, Race, and Sex with Considerations as to Their Etiology and Significance. J Bone Joint Surg Am. 1962;44:243–268. [Google Scholar]
- 21.Cagli S, Chamberlain RH, Sonntag VK, Crawford NR. The biomechanical effects of cervical multilevel oblique corpectomy. Spine. 2004;29(13):1420–1427. doi: 10.1097/01.BRS.0000129896.80044.B6. [DOI] [PubMed] [Google Scholar]
- 22.Simpson AK, Biswas D, Emerson JW, Lawrence BD, Grauer JN. Quantifying the effects of age, gender, degeneration, and adjacent level degeneration on cervical spine range of motion using multivariate analyses. Spine. 2008;33:183–186. doi: 10.1097/BRS.0b013e31816044e8. [DOI] [PubMed] [Google Scholar]
- 23.Choi D, Melcher R, Harms J, Crockard A. Outcome of 132 operations in 97 patients with chordomas of the craniocervical junction and upper cervical spine. Neurosurgery. 2010;66(1):59–65. doi: 10.1227/01.NEU.0000362000.35742.3D. [DOI] [PubMed] [Google Scholar]
- 24.Lee SE, Chung CK, Jahng TA. Early development and progression of heterotopic ossification in cervical total disc replacement. J Neurosurg Spine. 2012;16(1):31–36. doi: 10.3171/2011.8.SPINE11303. [DOI] [PubMed] [Google Scholar]
- 25.Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine. 1993;18(15):2167–2173. doi: 10.1097/00007632-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Shin DA, Yi S, Yoon DH, Kim KN, Shin HC. Artificial disc replacement combined with fusion versus two-level fusion in cervical two-level disc disease. Spine. 2009;34(11):1153–1159. doi: 10.1097/BRS.0b013e31819c9d39. [DOI] [PubMed] [Google Scholar]
- 27.Vedantam A, Revanappa KK, Rajshekhar V. Changes in the range of motion of the cervical spine and adjacent segments at ≥24 months after uninstrumented corpectomy for cervical spondylotic myelopathy. Acta Neurochir (Wien) 2011;153(5):995–1001. doi: 10.1007/s00701-011-0986-5. [DOI] [PubMed] [Google Scholar]
- 28.Kadaňka Z, Bednařík J, Novotný O, Urbánek I, Dušek L. Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. Eur Spine J. 2011;20(9):1533–1538. doi: 10.1007/s00586-011-1811-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nakamura K, Kurokawa T, Hoshino Y, Saita K, Takeshita K, Kawaguchi H. Conservative Treatment for Cervical Spondylotic Myelopathy: achievement and Sustainability of a Level of “No Disability”. J Spinal Disord. 1998;11(2):175–179. doi: 10.1097/00002517-199804000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Upadhyaya CD, Wu JC, Trost G, Haid RW, Traynelis VC, Tay B, Coric D, Mummaneni PV. Analysis of the three United States Food and Drug Administration investigational device exemption cervical arthroplasty trials. J Neurosurg Spine. 2012;16(3):216–228. doi: 10.3171/2011.6.SPINE10623. [DOI] [PubMed] [Google Scholar]
- 31.Goffin J, van Loon J, Van Calenbergh F, Plets C. Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord. 1995;8(6):500–508. doi: 10.1097/00002517-199512000-00014. [DOI] [PubMed] [Google Scholar]
- 32.Richards O, Choi D, Timothy J. Cervical arthroplasty: the beginning, the middle, the end? Br J Neurosurg. 2012;26(1):2–6. doi: 10.3109/02688697.2011.595846. [DOI] [PubMed] [Google Scholar]