Abstract
Purpose
To compare the clinical features of patients with sacroiliac joint (SIJ)-related sciatica-like symptoms to those with sciatica from nerve root compression and to investigate the necessity to perform radiological imaging in patients with sciatica-like symptoms derived from the SIJ.
Methods
Patients with pain radiating below the buttocks with a duration of 4 weeks to 1 year were included. After physical and radiological examinations, a diagnosis of SI joint-related pain, pain due to disk herniation, or a combination of these two causes was made.
Results
Patients with SIJ-related leg pain (n = 77/186) were significantly more often female, had shorter statue, a shorter duration of symptoms, and had more often pain radiating to the groin and a history of a fall on the buttocks. Muscle weakness, corkscrew phenomenon, finger-floor distance ≥25 cm, lumbar scoliosis, positive Bragard or Kemp sign, and positive leg raising test were more often present when radiologic nerve root compression was present. Although these investigations may help, MRI of the spine is necessary to discriminate between the groups.
Conclusions
Sciatica-like symptoms derived from the SIJ can clinically mimic a radiculopathy. We suggest to perform a thorough physical examination of the spine, SI joints, and hips with additional radiological tests to exclude other causes.
Keywords: Sacroiliac joint, Leg pain, Sciatica, Lumbar disk, Differential diagnosis
Introduction
Radiating pain in the leg is a very common complaint and can have many causes. Lumbosacral radicular syndrome (LSR) or sciatica can be one of them. Sciatica is generally defined as “pain in the lower back and hip radiating in the distribution of the sciatic nerve”. There are a multitude of intra- and extra-spinal possibilities ranging from primary nerve disorders to tumors and metabolic disorders, which can be the underlying cause of sciatica. In the 1920s, the sacroiliac joint (SIJ) was considered to be an important cause for sciatica. A decade later, it became apparent that the lumbar disk could create sciatica and interest in the SIJ faded [1]. The SIJ is a common cause of low back pain, but there is hardly any data indicating that SIJ sciatica can mimic radiating pain due to nerve compression [2–5].
Many patients with leg pain as the major complaint are referred to a primary care, physiatry, neurology or orthopedic outpatient clinic, to assess presence of nerve root compression. In 30 % of the patients with a presumptive diagnosis of a lumbar disk herniation, the diagnosis could not be confirmed by radiological imaging studies or even during operation [6, 7]. The question is whether the SIJ is the source of leg pain in these patients. In this prospective study, we included patients with radiating pain below the buttocks, performed neurological and musculoskeletal system examinations with specific clinical pain provocation SIJ tests and additional radiological and laboratory studies to assess the incidence of SIJ-related pain in this patient group. Furthermore, we investigated the clinical features of patients with SIJ-related pain and compared these findings with those of patients with (1) radiating pain caused by a radiologically confirmed nerve root compression due to lumbar disk herniation and (2) both radiological signs of nerve root compression due to disk herniation and positive SIJ provocation tests.
Materials and methods
The medical ethical committee of our hospital approved the design of this study.
Study population
Patients with complaints of leg pain and low back pain were referred by their general practitioners to our department. Consecutive patients were included in this prospective study during a 3.5-year period. A flowchart of the diagnostic process is shown in Fig. 1.
Fig. 1.
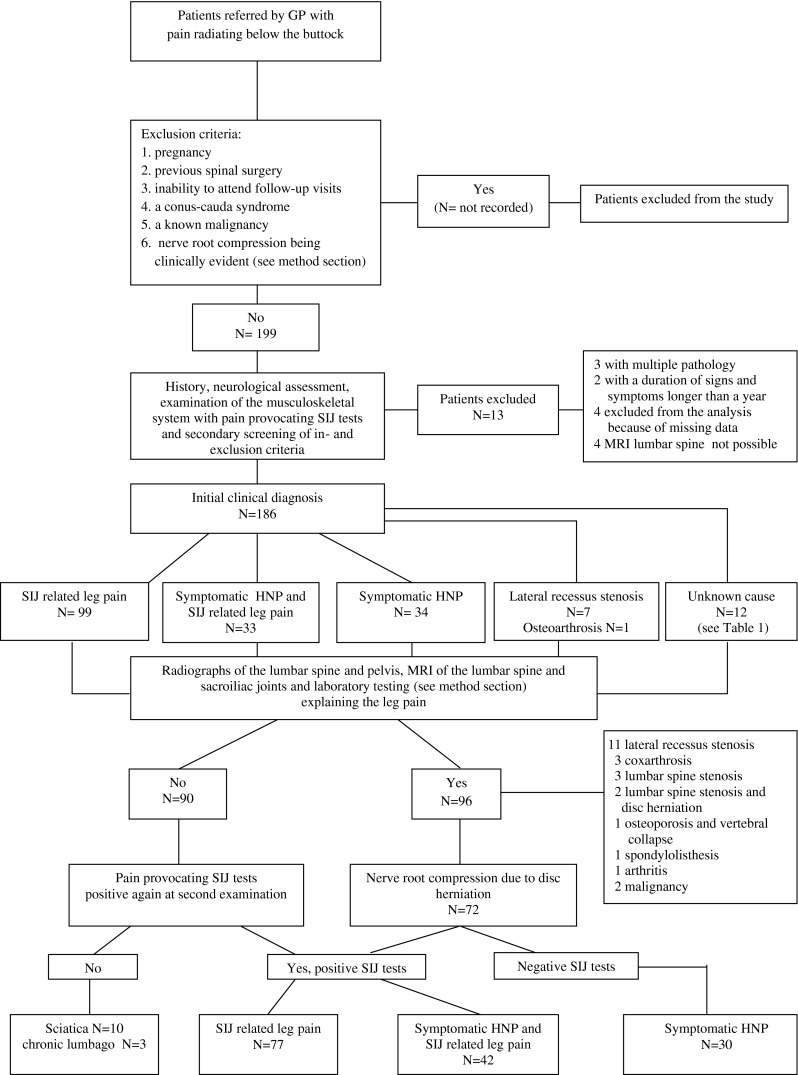
Flow chart of the patient entry, drop-outs, grouping, the initial clinical diagnoses, and for the initial SIJ-related pain group the definite diagnoses after additional laboratory and radiological examinations
Inclusion criteria
Inclusion criteria for the study were as follows: presence of pain radiating below the buttock with a duration for more than 4 weeks but <1 year. Exclusion criteria were: (1) pregnancy, (2) previous spinal surgery, (3) inability to attend follow-up visits, (4) patients with a conus-cauda syndrome, (5) patients with a known malignancy, (6) patients with obvious clinical nerve root compression (the neurologist did not doubt about the diagnosis), e.g., on physical examination obvious paresis (MRC < 4), dermatomal sensory loss, straight leg raising test <60° and reflex changes indicating an involvement of a specific nerve root. For clarity, patients with radiating pain with later radiologically confirmed nerve root compression were not excluded, only those patients in whom the clinicians did not have any doubt about the clinical diagnosis of nerve root compression with the physical findings described above.
All patients underwent physical neurological examination and clinical pain provocation SIJ tests.
Neurological and musculoskeletal system examinations
The neurological examination consisted of testing the strength of the muscles of the lower extremity, the ankle and knee tendon reflexes, a leg raising test (LRS) and reversed LRS as well as the Bragard test. The spine was also examined for lumbar scoliosis, hypertonic dorsolumbar muscles, mobility of the spine, Kemp test, and pressure pain at the SIJ.
SIJ provocation tests
Four different SIJ provocation tests were performed. These were the Gaenslen’s test, compression test, thigh trust, and Yeoman’s test [8, 9].
Radiological investigations
Radiographs of the lumbar spine and pelvis and MRI of the lumbar spine and SIJs were performed in all patients. An independent radiologist blinded to the clinical results assessed the radiological images. The assessment focused on the presence or absence of nerve root or nerve root sleeve compression by extruded nucleus material or lateral recessus narrowing.
Laboratory investigations
Laboratory testing included: ESR, leucocytes, calcium, alkaline phosphatase, rheumatoid factor, and Borrelia burgdorferi serology.
At the second visit shortly after the MRI and usually within 4–6 weeks after the first physical examination, these data were reviewed and then a second physical and neurological examination together with clinical pain SIJ provocation tests were performed by one of the two primary involved neurologists (JS and LV). These two physicians made the final diagnosis of SIJ-related pain, pain due to disk herniation, or a combination of these two causes (Fig. 1).
Definitions of the patient groups
Diagnosis of SIJ-related pain
The diagnosis of SIJ-related pain was based on clinical and radiological grounds. We defined SIJ-related pain as:
radiating pain below the buttocks,
pain present in the region of SIJ,
three or more positive provocation SIJ tests confirmed at the second visit,
- exclusion of other causes which can give rise to radiating pain in the leg,
- absence of nerve root compression caused by a herniated disk, foramen stenosis or tumor,
- absence of Lyme disease, or other infectious diseases
Exclusion of sacroiliitis.
This group is called the SIJ-related pain group.
The diagnosis of radiating pain caused by nerve root compression due to lumbar disk herniation in the patients who were included in the study was defined as:
radiating pain below the buttocks,
presence of nerve root compression caused by a herniated disk on the MRI of the lumbar spine, explaining the radicular pattern in the leg,
absence of pain in the region of SIJ,
absence of positive provocation SIJ tests,
- exclusion of other causes which can give radiating pain in the leg at this level
- absence of nerve root compression by foramen stenosis or tumor,
- absence of Lyme disease, or other infectious diseases.
This group is called the disk herniation group.
Some patients had a combination of both. This group is called the SIJ- disk herniation group.
The diagnosis of radiating pain caused by nerve root compression due to lumbar disk herniation with positive provocation SIJ tests was defined as:
radiating pain below the buttocks,
presence of nerve root compression caused by a herniated disk on the MRI of the spine, explaining the radicular pattern in the leg,
pain present in the region of SIJ,
three or more positive provocation SIJ tests confirmed at the second visit,
- exclusion of other causes which can give radiating pain in the leg,
- absence of nerve root compression caused by a foramen stenosis or tumor,
- absence of Lyme disease, or other infectious diseases.
The medical history and clinical findings of the three groups were compared to assess whether by clinical history and physical examination, these three groups can be differentiated before additional radiological examinations are performed.
Statistics
Clinical imaging and laboratory assessment results of the three different groups were analyzed using the Chi-square test for comparison of proportions, or the Kruskal–Wallis test for comparison of means of ordinal variables between more than two groups.
Results
Of the 199 patients, who were referred by GPs, we excluded 13 patients. Three patients had multiple pathology, four patients did not get or could not get an MRI of the lumbar spine, two patients had a duration of signs and symptoms longer than a year, and four patients were excluded from the analyses because of missing data. Figure 1 shows a flow chart of the patient entry, drop-outs, and diagnostic process.
In Table 1, the diagnosis at the initial visit (before the additional laboratory and radiological examinations) and the final diagnosis obtained after laboratory testing, radiological investigations and a second physical examination are presented. All patients with the clinical diagnosis of a lateral recessus stenosis (group D) had radiological evidence of a foramen stenosis. Initially one patient (group E) had signs and symptoms of coxarthrosis, which was confirmed by X-ray of the hip. Twelve patients (group F) had initially sciatica with a normal physical examination. During follow-up, 2 of these 12 patients had positive SIJ provocation tests, 2 patients had radiological signs of nerve root compression, and 1 patient appeared to have a malignancy. After a second physical examination and radiological imaging, 8 of the 12 patients could not be categorized in one of our earlier defined groups. Although initially SIJ-related leg pain was the most likely diagnosis in 99 patients, this number was reduced to 77 (69 of these 99 patients and eight new cases from the other groups) after the radiological and clinical investigations. At the second visit, 3 of the 99 patients did not have positive provocative tests anymore, 13 patients had another cause of the pain, such as lateral recessus stenosis or coxarthrosis, and 15 patients had radiological evidence of nerve root compression.
Table 1.
The diagnosis at the initial visit (so before the additional laboratory and radiological examinations) in relation to the final diagnosis, obtained after laboratory testing, radiological investigations and a second physical examination
| Initial diagnosis A-F | Definite diagnosis | ||||||
|---|---|---|---|---|---|---|---|
| Only SI-related leg pain | Symptomatic HNP and SI-related leg pain | Symptomatic HNP without positive SI-prov. tests | Lateral recessus stenosis | Other known cause | Unknown cause for the leg pain | Total number | |
| (A) only SI-related leg pain | 69 | 14 | 1 | 3 | 10 | 2 | 99 |
| (B) Symptomatic HNP and SI-related leg pain | 7 | 23 | 2 | 0 | 1 | 0 | 33 |
| (C) Symptomatic HNP without positive SI-prov. tests | 0 | 4 | 26 | 1 | 1 | 2 | 34 |
| (D) lateral recessus stenosis | 0 | 0 | 0 | 7 | 0 | 0 | 7 |
| (E) other known cause | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| (F) unknown cause for the leg pain | 1 | 1 | 1 | 0 | 1 | 8 | 12 |
| Total number | 77 | 42 | 30 | 11 | 14 | 12 | |
The baseline characteristics between the SIJ, SIJ-disk herniation (SIJ-HNP), and disk herniation (HNP) groups are shown in Table 2. The patients with SI-related leg pain were significantly more often women (p < 0.0001), had a shorter statue (p = 0.0001) and had a shorter duration of symptoms (p = 0.003). The history revealed that patients with HNP had more often sensory loss or numbness (p = 0.02) (Table 3). There were no significant differences between the three groups concerning the acute onset of pain, pain on coughing or sneezing, feeling of coldness in the leg, subjective muscle weakness, disturbed urinary passage, urine incontinence, or pain occurring in certain positions (Table 3).
Table 2.
Patient’s baseline characteristics in relation to diagnosis
| Characteristics | SIJ-group (n = 77) | SIJ-HNP group (n = 42) | HNP group (n = 30) | p value |
|---|---|---|---|---|
| Male gender | 21 | 14 | 23 | <0.0001 |
| Length (IQR) | 168 (165–178) | 171 (165–177) | 177 (175–181) | 0.0001 |
| Weight in kg | 73 (63–85) | 74 (66–85) | 80 (70–90) | 0.21 |
| BMI, mean (IQR) | 22 (19–24) | 22 (19–25) | 23 (20–25) | 0.49 |
| Duration of disease (weeks, median, IQR) | 20 (17–24) | 15 (8,5–25,5) | 13 (6–24) | 0.003 |
| Smoking | 30/68 (44 %) | 13/38 (34 %) | 6/26 (23 %) | 0.15 |
| Family history of HNP | 30/77 (38 %) | 20/42 (47 %) | 12/28 (42 %) | 0.65 |
Bold values indicate statistical significance (p < 0.05)
Table 3.
Patient’s history in relation to diagnosis
| Characteristics | SIJ group (n = 77) | SIJ-HNP group (n = 42) | HNP group (n = 30) | p value |
|---|---|---|---|---|
| Sudden onset | 30/74 (40 %) | 21/42 (50 %) | 16/30 (53 %) | 0.32 |
| More pain on coughing/sneezing or straining | 32/75 (42 %) | 21/41 (51 %) | 17/30 (56 %) | 0.60 |
| Dermatomal coldness in the leg | 19/75 (25 %) | 17/41 (41 %) | 9/29 (31 %) | 0.51 |
| Sensory loss/numbness | 31/77 (40 %) | 27/42 (64 %) | 19/30 (63 %) | 0.02 |
| Muscle weakness | 26/77 (33 %) | 17/42 (40 %) | 11/30 (36 %) | 0.71 |
| Disturbed urinary passage | 4/77 (5 %) | 2/42 (4 %) | 3/20 (15 %) | 0.59 |
| Urine incontinence | 2/77 (2 %) | 1/42 (2 %) | 1/30 (3 %) | 0.96 |
| More pain | ||||
| On sitting | 58/74 (78 %) | 30/41 (73 %) | 21/29 (72 %) | 0.69 |
| Lying down | 38/75 (50 %) | 19/42 (45 %) | 12/30 (40 %) | 0.26 |
| Turning around | 58/75 (78 %) | 33/41 (80 %) | 7/28 (25 %) | 0.86 |
| Standing | 37/73 (50 %) | 30/42 (71 %) | 25/39 (64 %) | 0.34 |
| Walking | 28/74 (37 %) | 25/41 (60 %) | 8/29 (27 %) | 0.83 |
| Often sleeping supine | 16/69 (23 %) | 7/37 (18 %) | 3/28 (10 %) | 0.37 |
| Pain radiating to the groin | 35/77 (45 %)* | 16/42 (38 %) | 6/30 (20 %)* | 0.05 (0.03)* |
| Previous back pain | 46/72 (63 %) | 25/36 (69 %) | 16/26 (61 %) | 0.69 |
| History of car accident | 10/76 | 6/42 | 4/30 | 0.99 |
| History of fall on the buttocks | 18/75 | 5/42 | 1/30 | 0.02 |
Bold values indcate difference between SIJ group and HNP group at p = 0.03
* indicates statiscal significance at p = 0.05
Radiating pain to the groin (p = 0.05 overall and p = 0.03: difference between SIJ group and HNP group) and a history of a fall on the buttocks (p = 0.02) occurred more frequently in the SIJ group (Table 3).
On clinical examination, muscle weakness (p = 0.04), corkscrew phenomenon (p = 0.05), finger-floor distance ≥25 cm (p = 0.02), lumbar scoliosis (p = 0.04), positive Bragard (p = 0.005), Kemp sign (p < 0.0001), positive leg raising test (p < 0.0001) were more often found when radiologic nerve compression was present (Table 4).
Table 4.
Patient’s clinical examination in relation to the final diagnosis
| Characteristics | SIJ-group (n = 77) | SIJ-HNP group (n = 42) | HNP-group (n = 30) | p value |
|---|---|---|---|---|
| Abnormal walking on toes | 1/77 (1 %) | 5/42 (11 %) | 3/30 (10 %) | 0.04 |
| Abnormal walking on heels | 4/77 (5 %) | 6/42 (14 %) | 5/30 (16 %) | 0.12 |
| Parese extensor hallucis longus | ||||
| M. extensor hallucis longus | 3/77 (3 %) | 2/42 (4 %) | 5/30 (16 %) | 0.05 |
| M. gastrocnemius | 2/77 (2 %) | 4/42 (9 %) | 3/30 (10 %) | 0.19 |
| M. tibialis anterior | 2/77 (2 %) | 3/42 (7 %) | 2/30 (6 %) | 0.45 |
| M. tibialis posterior | 1/77 (1 %) | 2/42 (4 %) | 1/30 (3 %) | 0.52 |
| “corkscrew” phenomenon | 8/77 (10 %) | 10/42 (23 %) | 8/21 (38 %) | 0.05 |
| Finger-floor distance ≥ 25 cm | 17/77 (22 %) | 18/42 (42 %) | 13/28 (46 %) | 0.02 |
| Lumbar scoliosis | 19/77 (24 %) | 9/42 (21 %) | 14/30 (46 %) | 0.04 |
| Decreased knee reflex | 11/77 (14 %) | 11/42 (26 %) | 2/30 (6 %) | 0.07 |
| Decreased ankle reflex | 23/77 (29 %) | 12/42 (28) | 7/30 (23 %) | 0.79 |
| Positive Bragard | 8/77 (10 %) | 13/42 (30 %) | 10/30 (33 %) | 0.005 |
| Positive Kemp’s sign | 5/77 (6 %) | 15/42 (35 %) | 16/30 (53 %) | <0.0001 |
| Positive SLR | 13/77 (16 %) | 18/42 (42 %) | 21/30 (70 %) | <0.0001 |
| Positive reversed SLR | 8/77 (10 %) | 6/42 (14 %) | 3/30 (10 %) | 0.79 |
| Laboratory findings | ||||
| ESR > 12 | 17/68 (22 %) | 12/34 (35 %) | 1/11 (9 %) | 0.15 |
| Leucocytes > 10. 109 | 9/61 (14 %) | 9/32 (28 %) | 1/10 (10 %) | 0.22 |
Bold values indicate statistical significance (p < 0.05)
Two male patients in the SIJ group had a positive rheumatoid factor. Laboratory tests were not helpful to discriminate between the three groups (Table 4). None of the patients had positive Borrelia burgdorferi serology.
Discussion
In this study, we tried to answer three questions. Does SIJ-related radiating leg pain exist, is MRI of the lumbar spine necessary to exclude other causes and can factors from the medical history or clinical examination be used to differentiate between SIJ-related pain, leg pain due to disk herniation or a combination?
Few studies have investigated the SIJ as a source of pain in the leg [2–5]. Our clinical impression was that at our outpatients clinic many patients are seen with leg pain and positive SIJ provocation tests without nerve compression on MRI of the lumbar spine. So, we decided to undertake a study to assess this. A strength of our study is that we applied a strict definition for SIJ-related leg pain: radiating pain below the buttocks, three or more positive provocation SIJ tests confirmed by two examiners, exclusion of other causes which can give radiating pain in the leg, e.g., absence of nerve root compression caused by a herniated disk, foramen stenosis or tumor, absence of Lyme disease or other infectious diseases, and exclusion of sacro-iliitis. We suggest that these criteria are going to be used in further studies. It is not clear why SIJ-related leg pain did not receive much attention in recent medical literature, since our data suggest that SI-related leg pain is not a rare occurrence in the practice of neurologists.
Are radiological examinations, such as MRI of the lumbar spine necessary to exclude other causes in patients with presumed SIJ-related leg pain? Performing additional radiological examinations changed the initial diagnosis in 30 of the 99 patients with presumable SIJ-related leg pain. It also influenced treatment decision-making because sometimes an underlying lateral stenosis or root compression by disk herniation was found. So, the diagnosis SIJ-related leg pain without additional diagnostic imaging is insensitive. Although additional diagnostic imaging may be common practice in certain countries, this is certainly not the case in Dutch patients with a presumed diagnosis with SIJ-related leg pain. We therefore advocate to perform at least an MRI of the spine before a definitive diagnosis of SIJ-related leg pain is made. Moreover, as described by Galm et al. [10] SIJ dysfunction can occur in patients with low back pain and sciatica and imaging-proven disk herniation. When therapy is focused on the presence of SIJ dysfunction nucleotomy can be prevented in these patients [10].
Can factors from the medical history or clinical examination be used to differentiate between SIJ-related pain, leg pain due to disk herniation or a combination of both? The patients were referred by their GPs, usually with the question whether the patients had a nerve root compression due to disk herniation. Therefore, the patients are not a representative group for SIJ-related pain but for SIJ-related leg pain mimicking a lumbosacral radicular pain. Literature indicates that consistency of history taking and physical examination in patients with suspected lumbar nerve root involvement is low [11, 12]. In this study, we found that SIJ-related leg pain occurred especially in women. The history revealed that patients with an underlying disk herniation more often had sensory loss or numbness, but otherwise there were no significant differences between the groups concerning the acute onset of pain, pain on coughing or sneezing, feeling of coldness in the leg, subjective muscle weakness, disturbed urinary passage, urine incontinence, or pain occurring in certain positions. Factors that can differentiate between the groups are: (1) radiating pain to the groin and a history of a fall on the buttocks, which occurred more often when the SIJ was involved, and (2) muscle weakness, corkscrew phenomenon, finger-floor distance ≥25 cm, lumbar scoliosis, positive Bragard and Kemp sign and positive leg raising test at clinical examination, which occurred more often when radiologic nerve compression was present. The occurrence of radiating pain to the groin in patients with SIJ pain has been described before [14].
Explanations for the radiating pattern of pain into the leg due to the SI joint are several, as described earlier [1]. First, it can be interpreted as referred pain from this joint. The radiating pattern depends upon the segmental nerve supply of the SI-joint, which is described as primarily deriving from branches from L5 to S4 spinal nerves [13]. Second, it has been reported that radiating SI joint-related pain may also be considered as segmental nerve-related pain because of the close relationship between the ventral capsule of the SI joint and the spinal nerves L5 and S1, just prior to where these nerves join to form part of the sciatic nerve [2]. Arthrograms of patients with SIJ-related pain sometimes show tears of this ventral capsule [14]. It has been suggested that SI capsular irritation and cytokine release may cause adjacent neural insult by these communications [15]. Finally, one should take into account that radiating pain into the leg can also derive from structures in the lower back other than the SI-joint, particularly when they are supplied by branches from the same spinal nerves, i.e. L5–S4 [16].
Our study has a number of limitations. One limitation of the study is that we did not collect all the data of the patients presenting with radiating pain. Patients with a clear clinical picture of an underlying disk herniation were excluded. The second important remark is the lack of a golden standard for SIJ (related leg) pain diagnosis. To make a clinical diagnosis, the International Association for the study of Pain (IASP) has proposed a set of criteria for diagnosing SIJ pain [17]. According to these criteria, SIJ pain refers to patients with pain in the area of the SI joint, which should be reproducible by performing specific provocation SIJ tests or should be completely relieved by infiltration of the SIJ with local anesthetics [18]. The first criterion, the presence of pain in the SIJ is not specific and pain can extend to the buttock, groin or lower extremity. It has been shown that the compression and thigh thrust test (used in this study) are helpful in diagnosing SIJ pain [18, 19]. Multiple SI provocation tests are helpful, but the gold standard for establishing the diagnosis SIJ-related pain is said to be an intra-articular blockade with low volume local anesthetics [1, 18]. We did not perform selective infiltration as a reference test. We had several reasons for this. The first one is the diagnostic value of the SI provocation tests, which were used in this study. Using a threshold of 3 or more positive provocation test has shown to give a sensitivity of 0.85 and specificity of 0.76 with a diagnostic odds ratio of 17 [18]. It is not known whether the combination of these tests with an intra-articular injection in the SIJ increases sensitivity and specificity. Moreover, with the intra-articular injection only the joint cavity is infiltrated, while pain can also occur from the structures surrounding the SIJ [18]. Furthermore, the validity of an intra-articular injection is questioned [20]. Most importantly, at a follow-up study, we wanted to examine prospectively the therapeutic effects of physiotherapy, manual therapy, and intra-articular injection on pain scores in the patients with SIJ-related leg pain. Therefore, we did not want to expose patients to an intra-articular injection of the SIJ prior to the entry to this second study.
The third limitation is that we did not perform a McKenzie evaluation prior to SIJ tests to reduce the probability of diskogenic low back pain.
We conclude that sciatica-like symptoms derived from the SIJ can clinically mimic a radiculopathy. We suggest to perform a thorough physical examination of the spine, SI joints and hips with additional radiological tests to exclude other causes. Recognizing that sciatica can be referred pain from the SI joint is important, since it may prevent unnecessary investigations and operations.
Conflict of interest
There is no actual or potential conflict of interest in relation to this article.
References
- 1.Buijs E, Visser L, Groen G. Sciatica and the sacroiliac joint: a forgotten concept. Br J Anaesth. 2007;99:713–716. doi: 10.1093/bja/aem257. [DOI] [PubMed] [Google Scholar]
- 2.Fortin JD, Dwyer AP, West S, Pier J. Sacroiliac joint: pain referral maps upon applying a new injection/arthrography technique. Part I: asymptomatic volunteers. Spine. 1994;19:1475–1482. doi: 10.1097/00007632-199407000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Fortin JD, Aprill CN, Ponthieux B, Pier J. Sacroiliac joint: pain referral maps upon applying a new injection/arthrography technique. Part II: clinical evaluation. Spine. 1994;19:1483–1489. doi: 10.1097/00007632-199407000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Fortin JD, Vilensky JA, Merkel GJ. Can the sacroiliac joint cause sciatica? Pain Physician. 2003;6:269–271. [PubMed] [Google Scholar]
- 5.Hiltz DL. The sacroiliac joint as a source of sciatica. Phys Ther. 1976;56:1373. doi: 10.1093/ptj/56.12.1373. [DOI] [PubMed] [Google Scholar]
- 6.Modic MT, Ross JS, Obuchowski NA, Browning KH, Cianflocco AJ, Mazanec DJ. Contrast-enhanced MR imaging in acute lumbar radiculopathy: a pilot study of the natural history. Radiology. 1995;195:429–435. doi: 10.1148/radiology.195.2.7724762. [DOI] [PubMed] [Google Scholar]
- 7.Ohnmeiss DD, Vanharanta H, Ekholm J. Degree of disc disruption and lower extremity pain. Spine. 1997;22:1600–1605. doi: 10.1097/00007632-199707150-00015. [DOI] [PubMed] [Google Scholar]
- 8.Laslett M. Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 2008;16:142–152. doi: 10.1179/jmt.2008.16.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laslett M. Pain provocation tests for diagnosis of sacroiliac joint pain. Aust J Physiother. 2006;52:229. doi: 10.1016/S0004-9514(06)70037-X. [DOI] [PubMed] [Google Scholar]
- 10.Galm R, Frohling M, Rittmeister M, Schmitt E. Sacroiliac joint dysfunction in patients with imaging-proven lumbar disc herniation. Eur Spine J. 1998;7:450–453. doi: 10.1007/s005860050107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vroomen PC, de Krom MC, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of sciatica due to disc herniation: a systematic review. J Neurol. 1999;246:899–906. doi: 10.1007/s004150050480. [DOI] [PubMed] [Google Scholar]
- 12.Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry. 2002;72:630–634. doi: 10.1136/jnnp.72.5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grob KR, Neuhuber WL, Kissling RO. Innervation of the sacroiliac joint of the human. Z Rheumatol. 1995;54:117–122. [PubMed] [Google Scholar]
- 14.Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine. 1995;20:31–37. doi: 10.1097/00007632-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Fortin JD, Washington WJ, Falco FJ. Three pathways between the sacroiliac joint and neural structures. AJNR Am J Neuroradiol. 1999;20:1429–1434. [PMC free article] [PubMed] [Google Scholar]
- 16.Groen GJ, Baljet B, Drukker J. Nerves and nerve plexuses of the human vertebral column. Am J Anat. 1990;188:282–296. doi: 10.1002/aja.1001880307. [DOI] [PubMed] [Google Scholar]
- 17.Merskey H, Bogduk N. Classification of chronic pain: Descriptions of chronic pain syndromes and definitions of pain terms; Seattle. WA: IASP Press; 1994. pp. 190–191. [Google Scholar]
- 18.Szadek KM, van der Wurff WP, van Tulder MW, Zuurmond WW, Perez RS. Diagnostic validity of criteria for sacroiliac joint pain: a systematic review. J Pain. 2009;10:354–368. doi: 10.1016/j.jpain.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 19.van der Wurff WP, Buijs EJ, Groen GJ. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch Phys Med Rehabil. 2006;87:10–14. doi: 10.1016/j.apmr.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 20.Berthelot JM, Labat JJ, Le GB, Gouin F, Maugars Y. Provocative sacroiliac joint maneuvers and sacroiliac joint block are unreliable for diagnosing sacroiliac joint pain. Joint Bone Spine. 2006;73:17–23. doi: 10.1016/j.jbspin.2004.08.003. [DOI] [PubMed] [Google Scholar]


