Abstract
Purpose
Recently, a new minimally invasive technique called ‘vertebral body stenting’ (VBS) was introduced for the treatment of osteoporotic vertebral fractures. The technique was developed to prevent the loss of reduction after deflation of the balloon and to reduce the complication rate associated with cement leakage.
Methods
The amount of kyphosis correction, improvement of vertebral body height and quantitative cement leakage rate by applying CT-based quantitative volumetry after VBS were measured in 27 patients (55 vertebra) and compared with a control group (29 patients, 61 vertebrae), which was treated with conventional vertebroplasty.
Results
After VBS, a significant improvement was seen in vertebral height, compared to conventional vertebroplasty. The mean improvement in segmental kyphosis and vertebral kyphosis were 5.8° (p < 0.05) and 3.5° (p < 0.05), respectively. In the VBS group, the mean injected volume of cement per vertebral body was 7.33 cm3 (3.34–10.19 cm3). The average amount of cement outside the vertebrae was 0.28 cm3 (0.01–1.64 cm3), which was 1.36 % of the applied total cement volume. In the vertebroplasty group, the applied mean volume of the cement per level was 2.7 cm3 (1–5.8 cm3) and the average amount of cement outside the vertebrae was 0.15 cm3 (0.01–1.8 cm3), which was 11.5 % (0.2–60 %) of the applied total volume of cement.
Conclusion
The frequency of cement leakage after VBS was 25.5 % compared to 42.1 % in the vertebroplasty group. VBS led to a significant decrease in the leakage rate compared with conventional vertebroplasty.
Keywords: Vertebral compression fractures, Augmentation, Cement leakage, Height loss/height resoration, Radiographic evaluation
Introduction
Vertebral compression fractures (VCF) are the most common complication of osteoporosis. VCF occur in approximately 26 % of women aged 50 years or older [1]. They cause pain and in many cases progressive collapse of the fractured osteoporotic vertebral body leads to a segmental spinal deformity [2]. Spinal deformities resulting from VCF have been shown to have adverse effects on the quality of life, physical function, mental health, as well as survival [3, 4]. These effects are related to the severity of the spinal deformity [3, 5] and are independent of the patient’s pain [3].
Percutaneous vertebroplasty and kyphoplasty are well-established minimally invasive surgical procedures for the treatment of vertebral compression fractures. Rapid pain reduction has been found in 80–90 % treated patients for both methods [6, 7]. Percutaneous vertebroplasty does not facilitate the restoration of vertebral height and is associated with a higher risk of cement leakage [3, 8]. Percutaneous kyphoplasty restores some vertebral height with a lower risk of cement leakage [2, 8, 9]. However, a significant loss of the restored height after balloon deflation prior to cement injection is a major disadvantage of percutaneous kyphoplasty. Recent studies have shown that the initial reduction achieved by the balloon is mostly lost after deflation [10], because the cavity created partially collapses before the bone cement can be injected [11]. Therefore, the expected spinal re-alignment cannot be completely achieved using percutaneous kyphoplasty [11]. The resulting hyperkyphotic alignment of the spine entails an increased risk of adjacent fractures [12], as well as adverse effects on patient outcome as described above. Especially in multi-level cases, this scenario may lead to a progressive kyphosis [11].
Due to these concerns, several efforts have been made to develop new technologies that allow vertebral fractures to be fully corrected and to stop the loss of restored vertebral body height after deflation [11]. A recently published cadaver study has shown superior results for a metallic implant [vertebral body stent (VBS)] for vertebral augmentation and height restoration compared to kyphoplasty [11]. VBS is based on the principles of balloon kyphoplasty and vascular stenting. The metallic stent remains in the vertebral cavity created and does not have to be removed after deflation. Vertebral body height can be restored physiologically and preserved while injecting the PMMA bone cement.
Only few clinical trials investigating traumatic fractures have been published so far on this new technique with the potential for height restoration and increased safety associated with a reduction in cement leakage rates [13].
99 % of the published vertebroplasty and kyphoplasty studies used simple X-rays to assess leakage, and therefore, leakage may be significantly underestimated because plain X-rays are not sensitive to detect cement leakage appropriately. Furthermore, the amount of leakage is also unknown when detected by plain X-rays and the exact anatomical location (A, B or C type of leakage) cannot be estimated using plain X-rays. In the literature, there are 14 studies using computer tomography (CT) scans to assess leakage, and only one study using quantitative CT measurement [26].
In the present study, we investigated the cement leakage rate using quantitative measures (CT volumetry) and vertebral body height restoration and spinal alignment after VBS. Cement leakage was compared with conventional vertebroplasty.
Materials and methods
Between January and November 2009, 56 patients were included in the current trial. All patients had suffered osteoporotic fractures without neurological deficit. All patients had persistent local midline back pain refractory to conservative treatment for at least 6 weeks and back pain related to the site of the fracture on magnetic resonance imaging (MRI) and showed the presence of bone marrow oedema in the collapsed vertebral body on MRI T2-weighted short tau inversion recovery (STIR) sequences. All the vertebral compression fractures were located in the lumbar spine or thoracolumbar junction and were classified as A1 fractures according to the AO classification. 29 patients were treated using a conventional viscosity controlled vertebroplasty (VERTECEM System, Synthes GmbH, Oberdorf, Switzerland). 27 patients were treated with the VBS (Synthes, Oberdorf, Switzerland) technique and cement augmentation was performed with PMMA cement (Vertecem,Synthes, Oberdorf, Switzerland).
Surgical procedure
Surgical approach for both groups
In our study, all the surgical procedures were performed using general anaesthesia. Patients were placed in a prone position. Two C-arms were placed at the level of the fractured vertebra in the anterior–posterior (AP) and in lateral projection. After a stab skin incision, guide wires were inserted through the soft tissue until the bony surface of the spine was reached. As the next step, guide wires were placed bipedicularly, according to the specifications of the manufacturer, under fluoroscopic control.
VBS group
A working sleeve was positioned over the guide wire until its tip was located about 1 or 2 mm anterior to the posterior wall of the vertebral body. Vertebral body stents are made of a strong and ductile cobalt–chromium alloy that is commonly used in coronary and peripheral artery stents (Fig. 1a). These expandable metal stents are attached onto a balloon catheter and can be manually expanded by the surgeon by means of contrast saline solution with upto 30 atm pressures. The unexpanded stent (Ø 4.2 mm) comes pre-crimped on the balloon and is gradually expanded until fracture reduction is satisfying, or a maximum diameter of 17 mm is reached. Like in kyphoplasty, the balloon can be extended and a cavity is created inside the vertebral body (Fig. 1b). To restore the maximum vertebral height possible, both stents should be expanded simultaneously. When fracture restoration is sufficient, the balloons are deflated and retrieved. The two stents remain in the vertebral body to maintain the restored height (Fig. 1c).
Fig. 1.
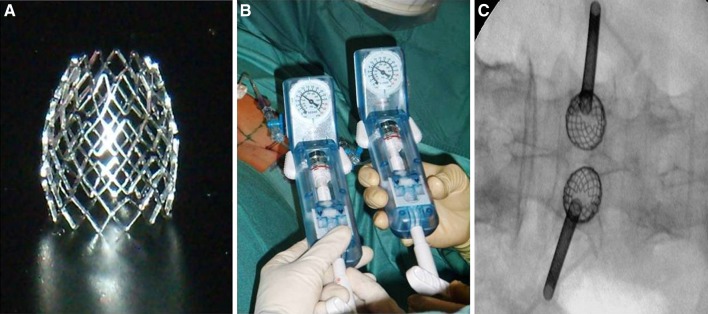
a Photo showing the expandable cobalt–chromium stent. b Photo showing the inflation system to expand the stent. c X-ray showing the expanded stent after balloon retrieval
After removal of the guide wires, a drill and a blunt plunger were inserted into the working sleeve to create an access channel for the stents in the vertebral body. Two VBS stents (diameter 17 mm, length 15 mm) were inserted simultaneously through the working sleeve and the expansion procedure was carried out as described above. Then two side-opening needles were inserted into the working sleeve in order to apply the PMMA cement (Vertecem, Synthes, Oberdorf, Switzerland) (Fig. 2a). Cement viscosity was tested using a viscometer (Viscosafe, Synthes, Oberdorf, Switzerland), and injection was performed step-wise. The cement was controlled to behave like a growing cloud, and the flow of cement was monitored by continuous fluoroscopic control (Fig. 2b, c). After cement injection, the working sleeves were removed and the wound was closed by means of a skin suture (Figs. 3, 4).
Fig. 2.
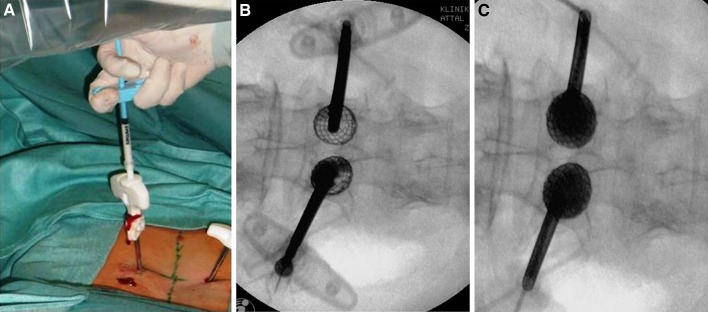
a Photo showing the application of the PMMA cement. b, c X-ray showing the application of the PMMA cement into the created cavity of expanded stent
Fig. 3.
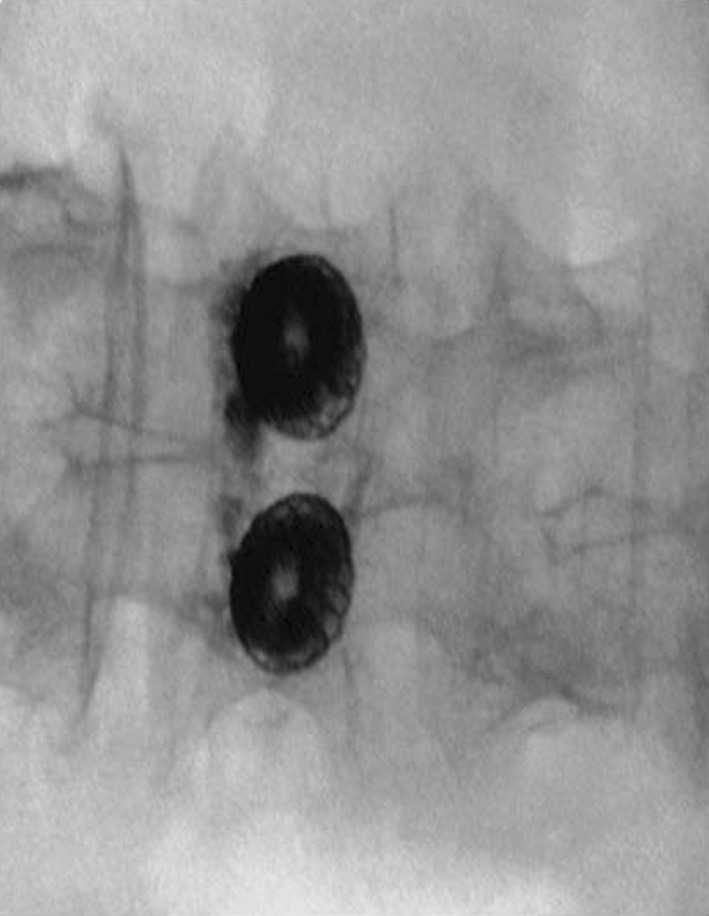
Anterior–posterior X-ray showing the restored vertebra
Fig. 4.
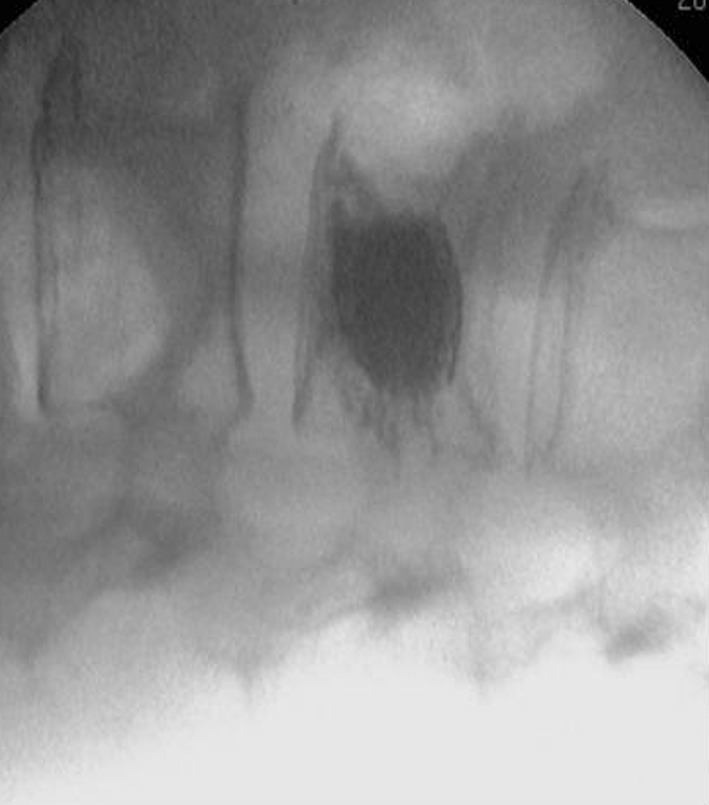
Lateral X-ray showing the restored vertebra
Vertebroplasty group
Side-opening needles were slided over the guide wires to the anterior half of the vertebral body. After removing the guide wire, the tip of the needle was cleared from bone preventing the cement injection with a trocar. As in the VBS group, cement viscosity was tested using a viscometer. The cement injection was done then through the side-opening slot of the needle, enabling directing the cement flow into the needed direction. The cement was controlled to behave like a growing cloud, and the flow of the cement was monitored with continuous fluoroscopic control.
Radiological evaluation
Pre-and post-operative X-rays, as well as a post-operative CT scan, were performed. The standardized pre- and post-operative lateral and anteroposterior radiographs were centred on the fractured (index) vertebra. All radiographs were evaluated by an experienced spine surgeon blinded to prior radiographs.
From the lateral radiograph, six points were hand-selected and marked on each vertebra. Points A and E were positioned at the most posterior- and anterior-superior endplate margins. Points B and F were set at the most posterior- and anterior-inferior endplate margins. Points C and D were defined at the intersection of a perpendicular drawn from the midpoints of line AE and BF. Vertebral body height measurements were assessed for fractured vertebrae and unfractured control vertebrae as distance in millimetres (mm) between the points defined: line EF, height anterior (Ha); line CD, height midline (Hm); line AB, height posterior (Hp). For each patient and each radiograph, the normal height of the fractured vertebra was estimated from the closest unfractured vertebrae, caudad and cephalad to the fractured vertebrae. All radiographs were analysed for the improvement in sagittal alignment (segmental) using the Cobb technique [14]. The Cobb angle was taken from the superior endplate of the vertebra above the fractured vertebra to the inferior endplate of the vertebra below (segmental kyphosis), and from the superior endplate to the inferior endplate of the affected vertebra (vertebral kyphosis).
Wedge (Ha/Hp) and biconcavity (Hm/Hp) ratios were calculated for fractured and adjacent control vertebrae.
Volumetry of applied cement
For the CT scans, a General Electrics Lightspeed 16© (GE Healthcare, Wisconsin, USA) was used with 100 kV, 100 mA source, rotation 0.8 s, DFOV 15, noise index 20 and a slice thickness of 0.625 mm. Scan coverage included the treated vertebral levels. Cement leakage was evaluated and quantified by an experienced radiologist. Volumetric assessment was performed using GE Medical Systems Volume Analysis 2 software. The threshold for the cement was set at 1,800. The volume inside and outside the vertebral bodies as well as the localization of the cement leakage was determined (Fig. 5a, b). Localization of cement leakage was classified according to Yeom et al. [15]: as type B (into the basivertebral vein), type S (into the segmental vein) or type C (cortical leakage: type C1 into the disc space; type C2 into the periphery).
Fig. 5.
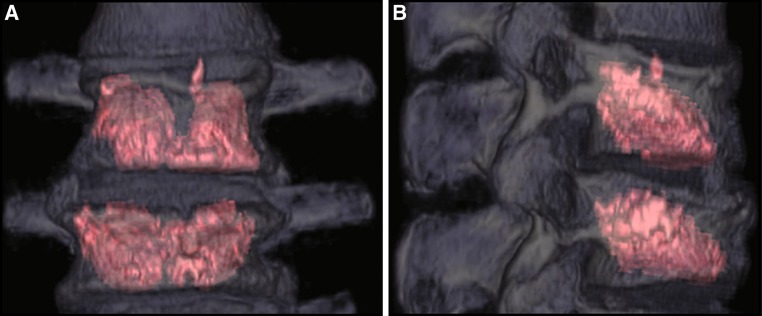
CT slides (a coronal, b sagittal) showing the volumetric assessment of applied cement inside and outside of the vertebral body (C1 type leakage)
Statistical analysis
Baseline continuous variables were compared by two independent sample t tests and are presented as means and standard deviation (SD). Paired t tests were used to compare measurements before and after surgery in each group. All the statistical assessments were two sided and evaluated at a statistical significance of p = 0.05. Statistical analyses were performed using SPSS 17.0 statistical software (SPSS Inc., Chicago, Illinois, USA).
Results
In both groups, all PMMA cement extravasations were asymptomatic, the cement remained in the immediate area of the treated vertebrae, and no medical or surgical intervention was required to remove the extravasated cement.
In the VBS group, one minor complication occurred in one patient. The patient had a surgical site infection, which was treated by debridement and antibiotic therapy. In the VBS group, two patients had a subsequent fracture (n = 3), occurring adjacent to treated segments and were again treated with VBS. The mean time between primary surgery and adjacent fracture was 9 days (range 5–13). No device-related or procedure-related complication occurred during the follow-up period. The mean follow-up time was 3.1 months.
Vertebroplasty group
A total of 29 patients (26 women, 3 men) were included. The mean patient age was 67.9 years (range 49.2–94.6 years). In 61 vertebrae, vertebroplasty was performed using the viscosimeter to control for appropriate cement viscosity. 17 patients had single level VCF, while 12 had multiple fractures (range 2–5). On average, vertebroplasty was performed on 2.1 levels in each patient (Table 1). The applied mean volume of the cement per level was 2.7 cm3 (range 1–5.8 cm3). The postoperative CT scan revealed leakage type B in 3 cases, type S in 14 cases and type C in 5 cases. The overall leakage rate was 42 %. The average amount of cement outside the vertebrae was 0.15 cm3 (range 0.01–1.8 cm3), which was 11.5 % (range 0.2–60 %) of the applied total volume of cement.
Table 1.
Operated levels in the two study groups
| Operated level | Vertebroplasty group | VBS group |
|---|---|---|
| T10 | 7 | 2 |
| T11 | 6 | 4 |
| T12 | 9 | 7 |
| L1 | 14 | 8 |
| L2 | 10 | 10 |
| L3 | 10 | 11 |
| L4 | 4 | 8 |
| L5 | 1 | 5 |
| Total | 61 | 55 |
T thoracic vertebra, L lumbar vertebra
Mean improvements in Hp, Hm and Ha, as well as improvement in segmental and vertebral kyphosis, are shown in Table 2.
Table 2.
Comparison of radiological parameters in VBS and vertbroplasty patients
| VBS | Vertebroplasty | p value | |
|---|---|---|---|
| Total applied cement (cm³) | 7.33 (1.4) | 2.7 (1.2) | <0.001 |
| Leakage volume (cm³) | 0.28 (0.2) | 0.15 (0.3) | 0.129 |
| Hp improvement | 2.2 (2.7) | 0.3 (2.6) | <0.001 |
| Hm improvement | 7.3 (4.1) | 1.3 (3.9) | <0.001 |
| Ha improvement | 3.6 (3.8) | 0.3 (3.7) | <0.001 |
| Improvement all vertebral heights (Ha, Hm, Hp) | 4.024 (2.925) | 0.642 (2.868) | <0.001 |
| Segmental kyphosis improvement | 2.826 (4.850) | 1.540 (8.639) | 0.378 |
| Vertebral kyphosis improvement | 0.964 (8.548) | 1.978 (4.731) | 0.042 |
Data are expressed in mean (SD). p value demonstrates the difference between these two techniques
The mean preoperative wedge index and biconcavity index for treated vertebrae were 0.85 (SD 0.18) and 0.65 (SD 0.16). The mean postoperative wedge index and biconcavity index for treated vertebrae were 0.86 (SD 0.17) and 0.68 (SD 0.14). Statistical analysis revealed no significant improvement in wedge or biconcavity index after surgery.
VBS
A total of 27 patients were included: 23 were women and 4 were men. The mean patient age was 66.9 years (range 46.5–87.4 years). The fractures treated were located between T10 and L5 (Table 1). Seventeen patients had single level VCF and 10 had multiple vertebral levels (2–5 vertebrae) treated by VBS. A total of 55 vertebral compression fractures with a mean of 1.9 per patient were investigated. The mean injected volume of cement per vertebral body was 7.33 cm3 (3.34–10.19 cm3). CT examination revealed cement leakage in 12 vertebrae. The postoperative CT scan revealed leakage type B in one level (0.06 cm3), type S in one level (0.07 cm3) and type C in ten levels (C1: mean 0.55 cm3, range 0.07–1.64; C2: mean 0.09 cm3, range 0.01–0.31). A combined C1 and C2 leakage was found in two levels. The overall leakage rate was 25.5 %. The average amount of cement outside the vertebrae was 0.28 cm3 (range 0.01–1.64 cm3), which was 1.36 % of the applied total volume of cement.
Mean improvements in Hp, Hm and Ha, as well as improvement in segmental and vertebral kyphosis, are shown in Table 2.
The mean preoperative wedge index and biconcavity index for treated vertebrae were 0.87 (SD 0.16) and 0.65 (SD 0.14). The mean postoperative wedge index and biconcavity index for treated vertebrae were 0.94 (SD 0.14) and 0.83 (SD 0.09). Preoperative and postoperative lateral radiographs were available for all patients.
No significant difference was found for wedge and biconcavity index between the VBS and vertebroplasty group before surgery. However, significant improvement in biconcavity and wedge index after surgery was seen in patients treated with VBS (p < 0.05).
Discussion
VCF affects the anterior part of the spinal column. The thoracolumbar junction, where two-thirds of the load is carried by the anterior spinal column, is that part of the spine where most fractures occur [14]. Without treatment, these fractures may lead to a kyphotic deformity. Surgical treatment options in case of VCF include vertebroplasty as well as kyphoplasty.
Percutaneous vertebroplasty has been reported to be an effective method of improving pain associated with VCF [6, 7]. Limitations of vertebroplasty include the inability to sufficiently restore vertebral body height and therefore kyphotic deformity is not addressed. Vertebroplasty does not address the associated spinal malalignement as it ‘freezes’ the deformity. However, vertebroplasty has some potential in achieving kyphosis correction. The prone positioning on the operating table may also lead to some amount of fracture reducing, especially in fresh fractures. Regarding cement leakage, there is a higher risk for the vertebroplasty technique compared to kyphoplasty resulting from the high-pressure cement injection required by this technique.
In contrast, kyphoplasty shows lower rates of cement leakage, because the created cavity allows low pressure injection of the cement [2, 8, 9] and sufficient vertebral height restoration is reported to be achieved by kyphoplasty. However, it has been shown that 34 % of kyphoplasties do not result in improvement of kyphotic angle or vertebral height [16]. One reason for insufficient height restoration is that the balloon tamp is deflated prior to cement injection. Therefore, the restored height cannot be preserved until the cement is injected [17].
The VBS system consists of an expandable stent which can be inserted in collapsed vertebrae. By inflation of this stent, the vertebral body height can be restored and, as in kyphoplasty, a cavity for PMMA cement injection is created. High viscosity cement can be easily injected. In contrast to kyphoplasty, the height restored can be preserved because the stent remains in the vertebral body after deflation of the balloon. A recently published cadaver study showed that, compared to kyphoplasty, height loss after balloon deflation was significantly reduced by using VBS [11]. Restoring vertebral body height and segmental lordosis are fundamental for patient’s quality of life, physical function, mental health, as well as survival [3, 8]. These adverse affects are strongly correlated with the degree of spinal deformity [3, 8]. Therefore, vertebral height restoration seems to be the key factor in treating VCF. The literature is still inconclusive as to the increased risk of adjacent-level fractures after vertebral augmentation procedures. Though the rates of adjacent-level fractures are widely varying, kyphoplasty (3–29 %) has a lower rate of adjacent fractures than vertebroplasty (8–52 %) [9, 18–20]. Moreover, kyphoplasty also leads to a decrease in the incidence of subsequent vertebral body fractures compared with medical therapy alone [9]. Though it has not yet been definitely proved that height gain and improved re-alignment are clinically relevant, biomechanical studies indicate the importance of full fracture reduction and vertebral height restoration [11].
The technique of VBS is more demanding compared to balloon kyphoplasty and vertebroplasty, because the surgeon places metallic hardware into the vertebral body. The key issue to prevent device related complications is stent positioning. The stents should be placed in a symmetric way, exactly into the middle of each hemivertebra to prevent impingement of the mesh surfaces during dilatation and achieve full mesh expansion. If the stents are placed too far laterally, close to the cortical border the vertebra, the mesh may be blocked during expansion, or the cortical shell may break, causing lateral stent misplacement. Mispalced or dislocated stents outside of the vertebral body may cause serious complications with possible injury to the lumbar plexus or the great vessels. A misplaced or dislocated stent cannot be removed out of the vertebra without open, extensive surgery. It may also be critical to use the device in old or irreducible fractures, because the mesh may not expand appropriately. The mesh may stay collapsed either anteriorly, posteriorly or as a whole. It may be difficult to inject the PMMA cement into a collapsed or funnel-shaped stent. If it is impossible to insert the cementing canula into the mesh, it must be placed lateral to it to perform a vertebroplasty around the stent, because a funnel-shaped mesh without PMMA is not weight bearing. Therefore, it is important to assess the potential amount of reduction prior to stent placement. This may be done by comparing the standing X-rays with either the supine MRI scans or intraoperative fluoroscopy with the patient prone to assess the amount of reduction of the fractured endplate by patient positioning.
In the present study, mean vertebral body height restoration was significantly higher in the VBS group compared to conventional vertebroplasty. The amounts of height and angular correction of both study samples are comparable to other reported results.
Height restorations of 0 % up to 90 % (percentage of normal adjacent vertebral height), and angular corrections of 0°–18° have been reported [8, 21, 22]. This would mean that both techniques investigated in our study have no advantage to improve segemental kyphosis correction compared to balloon kyphoplasty. In clinical practice, we noticed for balloon and stent kyphoplasty techniques that the time between fracture and surgery is crucial for the potential of height restoration. Older symptomatic fractures, though showing an edema in the MRI scan, are frequently difficult to reduce with the balloon/stent device. The time between injury and surgery in the current series was several weeks due to late referral and limited availability of MRI diagnostics, which may explain the limited potential of segmental kyphosis correction.
The most common complications of vertebral augmentation procedures are due to cement leakage, which is detected in up to 82 % of cases [23]. In our study, we observed a cement leakage rate of 1.36 % of the applied total volume of cement. We only included those patients with a postoperative CT for the measurement of cement leakage, because it is the most reliable way to detect cement leakage [24]. The detection rates using X-rays are low and complicated by only fair interobserver agreement [23]. The leakage rate strongly depends on the radiographical evaluation and varies from 7 % [25] detected via X-ray to 82 % detected by CT scan [23, 25]. In the current study, the cement inside and outside the vertebral bodies was measured by volumetry. Up to now, there is only one report published on the use of semiquantitative volumetry on three-dimensional CT scans (26).
Although the incidence of leakage was higher in the vertebroplasty group compared to VBS (25.5 vs. 42.1 %), no statistical difference between cement outside the vertebral body after VBS compared to vertebroplasty could be shown (Table 2). In VBS owing to the preformed cavity, the cement can be easily injected with low pressure. Extravasations are therefore rare. Different complications are associated with the type of leakage. B-type leakages may cause compression of neurologic structures, S-type leakages may cause pulmonary embolism, and C-type leakages into the disk space have been shown to increase the risk of new fractures of the adjacent vertebral body [20, 26]. It is unclear whether or not leakage is dependent on the amount of cement which is administered [24]. In the VBS group, one S-type and one B-type leakage with a small amount of extravasated cement were observed, compared with 14 S-type and three B-type leakage in the vertebroplasty group. However, twice the incidence of C-type leakage was found after VBS compared to vertebroplasty.
It is unlikely that there is a relation between the volume of cement injected into a vertebral body and the amount of height restoration, because the restoration of the fractured endplate is achieved either by patient positioning (vertebroplasty) or by expansion of the mesh stent (VBS). The cement cloud stabilizes the reduced endplate in the long term. A systematic review showed that there was no correlation between the volume of cement injected into the vertebral body and the clinical outcome [27].
There is some evidence in the literature that high filling volumes and endplate to endplate filling might increase adjacent level fractures due not only to increased stiffness of the index level [27–29], but also increase the risk of leakage [28].
To decide whether a cement leakage might be dangerous for a patient, the type of leakage is more important than the total volume of cement and total number of leakages per level.
One limitation of the current paper is the short follow-up period. A long-term follow-up would be needed to asses the rate of refracturing, the amount of loss of correction of the index level as well as the rate of adjacent level fractures. In this paper, we focused on cement leakage rates and the potential of vertebral height restoration immediately after surgery by the new technique of vertebral body stenting.
Conclusion
Clinical application of VBS showed a lower cement leakage rate (25.5 %) compared with conventional vertebroplasty (42 %). The rate of type B leakages could be significantly reduced to one in the VBS group. Therefore, VBS body stenting can be rated as a new promising option in the treatment of VCF.
Conflict of interest
None.
References
- 1.Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ., 3rd Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res. 1992;7(2):221–227. doi: 10.1002/jbmr.5650070214. [DOI] [PubMed] [Google Scholar]
- 2.Shen GW, Wu NQ, Zhang N, Jin ZS, Xu J, Yin GY. A prospective comparative study of kyphoplasty using the Jack vertebral dilator and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Bone Joint Surg Br. 2010;92(9):1282–1288. doi: 10.1302/0301-620X.92B9.23739. [DOI] [PubMed] [Google Scholar]
- 3.Hollingworth W, Jarvik JG. Evidence on the effectiveness and cost-effectiveness of vertebroplasty: a review of policy makers’ responses. Acad Radiol. 2006;13(5):550–555. doi: 10.1016/j.acra.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Rhyne A, 3rd, Banit D, Laxer E, Odum S, Nussman D. Kyphoplasty: report of eighty-two thoracolumbar osteoporotic vertebral fractures. J Orthop Trauma. 2004;18(5):294–299. doi: 10.1097/00005131-200405000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Muijs SP, Nieuwenhuijse MJ, Van Erkel AR, Dijkstra PD. Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures: evaluation after 36 months. J Bone Joint Surg Br. 2009;91(3):379–384. doi: 10.1302/0301-620X.91B3.20970. [DOI] [PubMed] [Google Scholar]
- 6.Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine. 2000;25(8):923–928. doi: 10.1097/00007632-200004150-00005. [DOI] [PubMed] [Google Scholar]
- 7.Heini PF, Walchli B, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J. 2000;9(5):445–450. doi: 10.1007/s005860000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garfin SR, Buckley RA, Ledlie J. Balloon kyphoplasty for symptomatic vertebral body compression fractures results in rapid, significant, and sustained improvements in back pain, function, and quality of life for elderly patients. Spine. 2006;31(19):2213–2220. doi: 10.1097/01.brs.0000232803.71640.ba. [DOI] [PubMed] [Google Scholar]
- 9.Taylor RS, Taylor RJ, Fritzell P. Balloon kyphoplasty and vertebroplasty for vertebral compression fractures: a comparative systematic review of efficacy and safety. Spine. 2006;31(23):2747–2755. doi: 10.1097/01.brs.0000244639.71656.7d. [DOI] [PubMed] [Google Scholar]
- 10.Voggenreiter G. Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine. 2005;30(24):2806–2812. doi: 10.1097/01.brs.0000190885.85675.a0. [DOI] [PubMed] [Google Scholar]
- 11.Rotter R, Martin H, Fuerderer S, Gabl M, Roeder C, Heini P, Mittlmeier T. Vertebral body stenting: a new method for vertebral augmentation versus kyphoplasty. Eur Spine J. 2010;19(6):916–923. doi: 10.1007/s00586-010-1341-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang MH, Barrett-Connor E, Greendale GA, Kado DM. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res. 2006;21(3):419–423. doi: 10.1359/JBMR.051201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klezl Z, Majeed H, Bommireddy R, John J. Early results after vertebral body stenting for fractures of the anterior column of the thoracolumbar spine. Injury. 2011;42(10):1038–1042. doi: 10.1016/j.injury.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Ulmar B, Brunner A, Guhring M, Schmalzle T, Weise K, Badke A. Inter- and intraobserver reliability of the vertebral, local and segmental kyphosis in 120 traumatic lumbar and thoracic burst fractures: evaluation in lateral X-rays and sagittal computed tomographies. Eur Spine J. 2010;19(4):558–566. doi: 10.1007/s00586-009-1231-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yeom JS, Kim WJ, Choy WS, Lee CK, Chang BS, Kang JW. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg Br. 2003;85(1):83–89. doi: 10.1302/0301-620X.85B1.13026. [DOI] [PubMed] [Google Scholar]
- 16.Tohmeh AG, Mathis JM, Fenton DC, Levine AM, Belkoff SM. Biomechanical efficacy of unipedicular versus bipedicular vertebroplasty for the management of osteoporotic compression fractures. Spine. 1999;24(17):1772–1776. doi: 10.1097/00007632-199909010-00004. [DOI] [PubMed] [Google Scholar]
- 17.Feltes C, Fountas KN, Machinis T, Nikolakakos LG, Dimopoulos V, Davydov R, Kassam M, Johnston KW, Robinson JS. Immediate and early postoperative pain relief after kyphoplasty without significant restoration of vertebral body height in acute osteoporotic vertebral fractures. Neurosurg Focus. 2005;18(3):e5. doi: 10.3171/foc.2005.18.3.6. [DOI] [PubMed] [Google Scholar]
- 18.Fribourg D, Tang C, Sra P, Delamarter R, Bae H. Incidence of subsequent vertebral fracture after kyphoplasty. Spine. 2004;29(20):2270–2276. doi: 10.1097/01.brs.0000142469.41565.2a. [DOI] [PubMed] [Google Scholar]
- 19.Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, Fardellone P. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford) 2000;39(12):1410–1414. doi: 10.1093/rheumatology/39.12.1410. [DOI] [PubMed] [Google Scholar]
- 20.Lin EP, Ekholm S, Hiwatashi A, Westesson PL. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004;25(2):175–180. [PMC free article] [PubMed] [Google Scholar]
- 21.Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26(14):1631–1638. doi: 10.1097/00007632-200107150-00026. [DOI] [PubMed] [Google Scholar]
- 22.Heini PF, Orler R. Kyphoplasty for treatment of osteoporotic vertebral fractures. Eur Spine J. 2004;13(3):184–192. doi: 10.1007/s00586-003-0654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidt R, Cakir B, Mattes T, Wegener M, Puhl W, Richter M. Cement leakage during vertebroplasty: an underestimated problem? Eur Spine J. 2005;14(5):466–473. doi: 10.1007/s00586-004-0839-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ryu KS, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg. 2002;96(1 Suppl):56–61. doi: 10.3171/spi.2002.96.1.0056. [DOI] [PubMed] [Google Scholar]
- 25.Eck JC, Nachtigall D, Humphreys SC, Hodges SD. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: a meta-analysis of the literature. Spine J. 2008;8(3):488–497. doi: 10.1016/j.spinee.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Komemushi A, Tanigawa N, Kariya S, Kojima H, Shomura Y, Komemushi S, Sawada S. Percutaneous vertebroplasty for osteoporotic compression fracture: multivariate study of predictors of new vertebral body fracture. Cardiovasc Intervent Radiol. 2006;29(4):580–585. doi: 10.1007/s00270-005-0138-5. [DOI] [PubMed] [Google Scholar]
- 27.Liebschner MA, Rosenberg WS, Keaveny TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine. 2001;26(14):1547–1554. doi: 10.1097/00007632-200107150-00009. [DOI] [PubMed] [Google Scholar]
- 28.Luo J, Daines L, Charalambous A, Adams MA, Annesley-Williams DJ, Dolan P. Vertebroplasty: only small cement volumes are required to normalize stress distributions on the vertebral bodies. Spine. 2009;34(26):2865–2873. doi: 10.1097/BRS.0b013e3181b4ea1e. [DOI] [PubMed] [Google Scholar]
- 29.Li YA, Lin CL, Chang MC, Liu CL, Chen TH, Lai SC. Subsequent vertebral fracture after vertebroplasty: incidence and analysis of risk factors. Spine. 2012;37(3):179–183. doi: 10.1097/BRS.0b013e3181f72b05. [DOI] [PubMed] [Google Scholar]


