Abstract
Purpose
The aim of this study was to analyze the correlation between cervical range of motion and cervical pedicle screw (CPS) misplacement in cervical posterior spinal fusion surgery using a CT-based navigation system.
Methods
A total of 46 consecutive patients with cervical posterior spinal fusion surgery using CPSs were evaluated retrospectively. We analyzed the cervical range of motion (ROM) and the misplacement of CPSs that were placed using either separate or single-time multilevel registration with a CT-based navigation system to determine the optimum registration procedure. The screw-inserted vertebra was indicated as Registered vertebra-Pedicle Screw inserted vertebra (Re-PS) = 0, 1, 2, or 3 depending on its distance (level) from the registered vertebra. Grades 0 (no perforation) and 1 (perforations <2 mm) were categorized as “no misplacement.” Grades 2 (perforations ≧2 mm but < 4 mm) and 3 (perforations ≧ 4mm) were categorized as “misplacement.” We analyzed the correlations between CPS misplacement and Re-PS, and between CPS misplacement and preoperative cervical ROM.
Results
Our analysis included 196 screws in patients having a mean age of 53.2 years (range 5–84 years). Level of insertion relative to registration was Re-PS = 0 in 129 screws, Re-PS = 1 in 53, Re-PS = 2 in 10 and Re-PS = 3 in 4. The misplacement rates were 12.2 % (24 screws) overall, 6.2 % in Re-PS = 0, 22.6 % in Re-PS = 1, 20 % in Re-PS = 2, and 50 % in Re-PS = 3. The rate of CPS misplacement increased significantly with a Re-PS = 1 and a Re-PS = 2 and 3 compared to a Re-PS = 0. There was a significant difference in the cervical ROM in each grade and both misplacement groups: 1.8 in Grade 0, 2.3 in Grade 1, 7.8 in Grade 2, 12.9 in Grade 3, 11 in the misplacement group and 1.9 in the no misplacement group.
Conclusions
The precision of CPS placement in CT-based navigation surgery was evaluated. The misplacement rate in single-time multilevel registration increased to 23.4 % compared to 6.2 % for separate registration. As the distance increased between the registered level and the level of CPS insertion, the preoperative cervical ROM and the rate of CPS misplacement significantly increased. Thus, the rate of misplacement of CPSs is reduced when performing separate registration. Furthermore, when there is greater preoperative cervical ROM, separate registration would likely improve the safety and accuracy of CPS insertion.
Keywords: Cervical, Pedicle screw, Misplacement, CT-based navigation, Range of motion
Introduction
Using a CT-based navigation system for spine surgery allows surgeons to navigate a pedicle screw into the vertebra with the help of real-time 3D images. Several clinical studies have reported that this technique improves the screw placement accuracy and safety of pedicle screw insertion [1–6] which is paramount for cervical spine surgery where misplacement of a cervical pedicle screw (CPS) may cause severe complications, such as injury to the vertebral artery, spinal cord or spinal nerves [7, 8]. Navigation systems have been very effective in decreasing these complications during cervical spine surgery. When using a navigation system for cervical posterior spinal fusion surgery, separate registration at each spinal level prior to CPS placement is currently recommended, although it requires more time in surgery. We have sometimes used single-time multilevel registration to decrease operative time, but when a CPS-inserted vertebra is far from the registered vertebra, navigation errors can occur. Navigation errors also can occur secondary to mobility of adjacent cervical vertebrae when we perform single-time multilevel registration. In addition, there were some disadvantages to relying on preoperative CT-based image guidance. Since the CT images are obtained before surgery with the patient in a supine position, and the surgery is usually performed in a prone position, intersegmental relationships between adjacent vertebrae can change [2]. Thus, single-time multilevel registration for CPS placement includes the risk of navigation errors and resultant complications.
There has been no published study on the correlation between preoperative cervical range of motion (ROM) and the misplacement of CPSs in cervical posterior spinal fusion surgery using a CT-based navigation system. In this report, we analyze the precision of CPS placement and preoperative cervical ROM between the registered vertebra and the CPS inserted vertebra.
Materials and methods
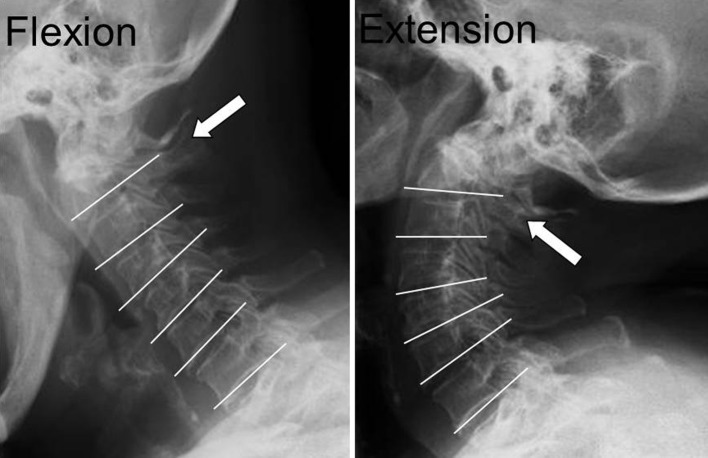
Between January 2004 and December 2011, we provided surgical treatment for patients with cervical disorders by a screw and rod system using a CT-based navigation system (VectorVision®, BrainLAB, Germany). We retrospectively evaluated 46 consecutive surgical patients (mean age 53.2 years range 5–84 years) with various cervical disorders who had CPSs inserted. Patients required surgery for the following cervical disorders: rheumatoid arthritis (RA) in 15 patients, cervical posterior spinal fusion surgery with tumor resection in 13 patients, cervical kyphosis in 10 patients, and atlanto-axial subluxation in 8 patients. When each vertebra was registered separately, the registered vertebra was indicated as Registered vertebra-Pedicle Screw inserted vertebra (Re-PS) = 0, whereas, for single-time multilevel registration, a CPS-inserted vertebra immediately adjacent to the registered level was indicated as Re-PS = 1, two levels from the registered level as Re-PS = 2, and three levels from the registered level as Re-PS = 3. We measured the cervical ROM with preoperative radiographs in flexion and extension positions and analyzed the correlation between misplacement of the CPS and cervical ROM. We calculated the ROM from the difference between the flexion and extension films: when the registered vertebra was also the screw-inserted vertebra, ROM was 0°; when Re-PS was ≥1, we added the ROMs of each level. For example, when we performed registration at the C2 vertebra and inserted the CPS at C4, the total ROM = ROM of C2/3 + ROM of C3/4 (Fig. 1). The accuracy of the postoperative CPS position was evaluated through CT scanning. We analyzed the correlations between CPS misplacement and Re-PS, and between CPS misplacement and preoperative cervical ROM.
Fig. 1.
We calculated the cervical ROM at each level between flexion and extension positions. For example, when we registered at C2 and inserted the CPS into the C2 pedicle, we defined the ROM as 0°. When we inserted it into another pedicle, we added the ROM at each level. For example, with single-time multilevel registration at C2 we calculated the total ROM as follows: ROM of C2/3 with insertion at C3; C2/3 + C3/4 with insertion at C4; C2/3 + C3/4 + C4/5 with insertion at C5
CT-based navigation procedure
The CT-based navigation system was based on a 1-mm, high-resolution CT scan. Image data were preserved using Digital Imaging and Communications in Medicine (DICOM) and then transferred to the navigation system via a network, which allowed reconstruction of a three-dimensional image. Registration was performed using the paired-matching algorithm with an acceptable predicted accuracy of <2 mm. If the accuracy was ≥2 mm, we used a surface-matching algorithm with an acceptable predicted accuracy of <2 mm. After registration of the vertebra, we verified that the virtual reality of the CT-based navigation system corresponded to the surgical reality. If accuracy was verified, the screw insertion was started, if not, we repeated the registration. Each pedicle screw insertion was performed after either separate registration or single-time multilevel registration.
Surgical procedure
Under general anesthesia, patients were placed in the prone position and a 4-point cranial fixation device was applied. Shoulders were pulled caudally and fixed using a heavy bandage to allow for an adequate lateral radiographic view. The posterior approach with a midline incision was used exposing the surface of the cervical spine. We attached the reference frame to the spinous process of a vertebra to perform the registration. Using the navigation guide, we made an entry point with a high-speed burr. After reconfirming the screw trajectory with a navigation probe, we inserted a pedicle probe into the pedicle and then inserted the CPS. Laminectomy, laminoplasty or tumor resection was performed if necessary.
Accuracy of CPS insertion
We evaluated the accuracy of all CPS placements with postoperative CTs in the multiplanar view as defined by Neo et al. [8]. CPS positions were categorized into four grades: Grade 0, no perforation and the screw was completely contained in the pedicle; Grade 1, perforations <2 mm; Grade 2, perforations ≥2 mm but <4 mm; and Grade 3, perforations ≥4 mm. We classified Grades 0 and 1 into a “no misplacement” group and Grades 2 and 3 into a “misplacement” group.
Statistical analysis
Data were analyzed using SPSS (version 18.0). The statistical difference was determined by Mann–Whitney’s U-test and Chi-square tests. Post hoc multiple comparisons were made using Tukey’s test. The threshold for significance was a p value of <0.05.
Results
There were 46 patients who received a total of 196 pedicle screws inserted using a CT-based navigation system. The numbers of screws inserted at each vertebral level were as follows: 37 screws in C2, 34 in C3, 33 in C4, 37 in C5, 24 in C6 and 31 in C7. The insertion level relative to the registration level was as follows: 129 in Re-PS = 0, 53 in Re-PS = 1, 10 in Re-PS = 2, 4 in Re-PS = 3. The mean registration accuracy was 1.25 mm. The mean registration accuracy of the misplacement group and no misplacement group were 1.29 and 1.24 mm, respectively. This difference was not significant. Using thin slice CT scans postoperatively to evaluate screw placement, we defined 150 (76.5 %) of the placements as Grade 0, 22 (11.2 %) as Grade 1, 9 (4.6 %) as Grade 2 and 15 (7.7 %) as Grade 3. Thus, there was misplacement of the CPS in 24 (12.2 %) of 196 total CPS insertions. The rate of misplacement relative to registration locations were as follows: 6.2 % in Re-PS = 0, 22.6 % in Re-PS = 1, 20.0 % in Re-PS = 2, 50.0 % in Re-PS = 3 (6.2 % in the separate registration procedures, 23.4 % in the single-time multilevel registration procedures).
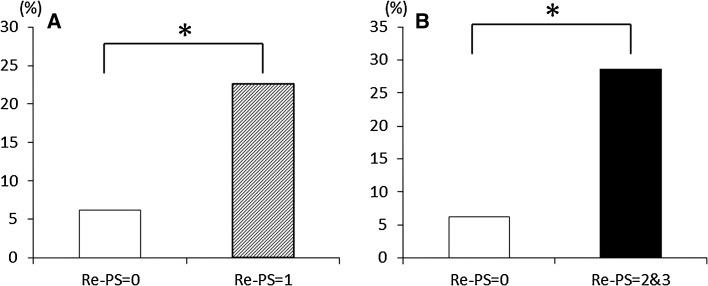
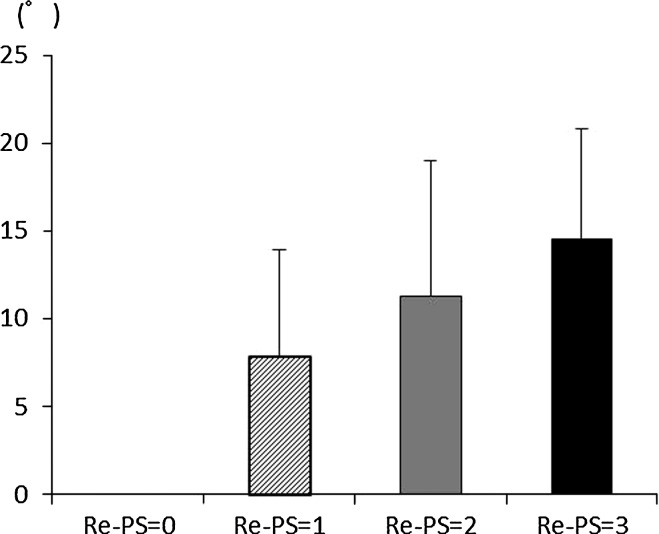
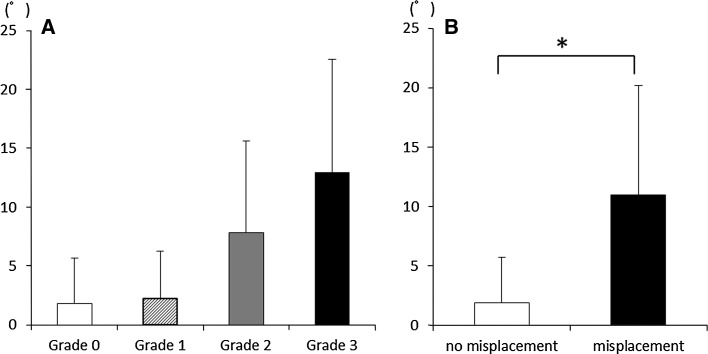
The rate of CPS misplacement increased significantly when the Re-PS = 1 and the Re-PS = 2 and 3 compared to a Re-PS = 0 (Fig. 2). The ROM of the cervical spine also increased significantly as the distance between the registered level and the level of CPS insertion increased (Fig. 3): 7.84° in Re-PS = 1, 11.3° in Re-PS = 2 and 14.5° in Re-PS = 3. The average cervical ROM relative to CPS misplacement was 1.8° in Grade 0, 2.3° in Grade 1, 7.8° in Grade 2 and 12.9° in Grade 3. There was a significant difference in ROM between the misplacement group (11°, Grades 2 and 3) and the no misplacement group (1.9°, Grades 0 and 1) (Fig. 4). With single-time multilevel registration, there was a significant difference between the average cervical ROM in the no misplacement group (6.3°) and the misplacement group (16.5°) (Table 1).
Fig. 2.
Rate of CPS misplacement. Re-PS indicates the distance between the registered level and the CPS insertion level. The rate of CPS misplacement increased significantly when the Re-PS = 1 (a) and Re-PS = 2 and 3 (b) compared to Re-PS = 0. *p < 0.01
Fig. 3.
ROM with respect to level of registration. As the distance between the registered level and the level of CPS insertion increased, the cervical ROM significantly increased
Fig. 4.
ROM with respect to CPS misplacement. a ROM by grade of CPS misplacement and b ROM in the no misplacement and misplacement groups. The preoperative cervical ROM of the misplacement group was significantly greater than that of the no misplacement group. *p < 0.05
Table 1.
CPS misplacement and ROM with separate and single-time multilevel registrations
| No misplacement (n = 172) | Misplacement (n = 24) | |||
|---|---|---|---|---|
| Re-PS = 0 | Re-PS ≥1 | Re-PS = 0 | Re-PS ≥1 | |
| Screws | 121 | 51 | 8 | 16 |
| Accuracy (mm) | 1.2 | 1.2 | 1.3 | 1.3 |
| ROM (°) | 0 | 6.3* | 0 | 16.5* |
* p < 0.01
Discussion
Since Abumi et al. [9] first reported that a subaxial cervical pedicle screw was successfully used in a human in 1994, and because of the improved biomechanical stability of the pedicle screw, there has been widespread usage of CPSs in cervical posterior spinal fusion surgery. Nevertheless, because of the cervical pedicle’s small size and its close proximity to the vertebral artery, placing a CPS may be considered very risky for the nearby neurovascular structures such as the vertebral artery, spinal cord or spinal nerves. Thus, computer-assisted surgery for the spine has been developed to correctly place the CPS.
In recent years, several authors have reported on the successful use of CT-based navigation systems for CPS insertion in cervical spinal disorders [3, 4, 6, 10]. These studies demonstrated a misplacement rate of 0.7–4 %, indicating these systems are safe and useful for spinal surgery. However, the cervical spine has ample mobility, especially compared to the lumbar and thoracolumbar segments, and cervical alignment can easily change when force is applied to the cervical spine while inserting a pedicle probe. Ideally, separate registration would be performed for CPS placement, but separate registration for each vertebra takes more time than a single-time multilevel registration. However, there are no established criteria as to which registration process should be used, and the limitations of single-time multilevel registration for CPS placement have been ambiguous.
Holly et al. [2] proposed separate registration at each vertebral level to prevent possible changes in intersegmental vertebral relationships. Lee et al. [11] also recommended separate registration to minimize the risk of cortical breaches and associated neurologic complications, even taking into account the added time required at surgery by separately registering each level. On the other hand, Kalfas et al. [12] stated that if there is no discrepancy between the navigation wand and the cursor position, the orientation of the second spinal level can proceed without another registration. Similarly, Schlenzka et al. [1] reported that the screw insertion to the adjacent vertebra could often be performed without additional matching. Papadopoulos et al. [13] proposed that single-time, multilevel registration may decrease operative time relative to repeated, separate registrations in the setting of degenerative disorders of the lumbar spine, and it may be used for up to four spinal levels. On the other hand, Scheufler [10] reported that image-guided spinal instrumentation using intraoperative CT-based neuronavigation with automated referencing allows for safe, highly accurate, multilevel instrumentation of the cervical and upper and midthoracic spine with a misplacement rate of only 0.7 %. We believe that single-time, multilevel registration may not be applicable for all surgical settings, especially if intersegmental instability is present. Moreover, there have been no reports discussing both preoperative cervical ROM and the single-time multilevel registration procedure.
In our study, the rate of CPS misplacement with separate registration was 6.2 %, whereas, the rate of CPS misplacement in single-time multilevel registration was 23.9 %. In addition, the rate of CPS misplacement increased significantly as the distance between the registered level and level of CPS insertion increased. In the future, when using a CT-based navigation system for pedicle screw insertion, we recommend using preoperative radiographs to determine cervical ROM prior to surgery and to establish which pedicle level is available and best suited for the single-time multilevel registration. This study’s limitation was a retrospective study with a small number of patients. However, our study does indicate guidelines for choosing the appropriate reference procedure when placing a CPS.
Conclusion
The precision of CPS placement in CT-based navigation surgery was evaluated. The overall misplacement rate was 12.2 %, however, the misplacement rate in single-time multilevel registration increased to 23.4 % compared to 6.2 % for separate registration. As the distance increased between the registered level and the level of CPS insertion, the cervical ROM and the rate of CPS misplacement significantly increased. Thus, the rate of misplacement of CPSs is reduced when performing separate registrations. Furthermore, as the preoperative cervical ROM increases, it becomes more important to use separate registrations for CPS insertion.
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Abbreviations
- CPS
Cervical pedicle screw
- ROM
Range of motion
- Re-PS
Registered vertebra-pedicle screw inserted vertebra
References
- 1.Schlenzka D, Laine T, Lund T. Computer-assisted spine surgery. Eur Spine J. 2000;9(Suppl 1):S57–S64. doi: 10.1007/PL00010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holly LT, Foley KT. Intraoperative spinal navigation. Spine (Phila Pa 1976) 2003;28:S54–S61. doi: 10.1097/01.BRS.0000076899.78522.D9. [DOI] [PubMed] [Google Scholar]
- 3.Kotani Y, Abumi K, Ito M, Minami A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 2003;99:257–263. doi: 10.3171/spi.2003.99.3.0257. [DOI] [PubMed] [Google Scholar]
- 4.Richter M, Cakir B, Schmidt R. Cervical pedicle screws: conventional versus computer-assisted placement of cannulated screws. Spine (Phila Pa 1976) 2005;30:2280–2287. doi: 10.1097/01.brs.0000182275.31425.cd. [DOI] [PubMed] [Google Scholar]
- 5.Ito H, Neo M, Yoshida M, Fujibayashi S, Yoshitomi H, Nakamura T. Efficacy of computer-assisted pedicle screw insertion for cervical instability in RA patients. Rheumatol Int. 2007;27:567–574. doi: 10.1007/s00296-006-0256-7. [DOI] [PubMed] [Google Scholar]
- 6.Rath SA, Moszko S, Schaffner PM, Cantone G, Braun V, Richter HP, Antoniadis G. Accuracy of pedicle screw insertion in the cervical spine for internal fixation using frameless stereotactic guidance. J Neurosurg Spine. 2008;8:237–245. doi: 10.3171/SPI/2008/8/3/237. [DOI] [PubMed] [Google Scholar]
- 7.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976) 2000;25:962–969. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 8.Neo M, Sakamoto T, Fujibayashi S, Nakamura T. The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine (Phila Pa 1976) 2005;30:2800–2805. doi: 10.1097/01.brs.0000192297.07709.5d. [DOI] [PubMed] [Google Scholar]
- 9.Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine (Phila Pa 1976) 1997;22:1853–1863. doi: 10.1097/00007632-199708150-00010. [DOI] [PubMed] [Google Scholar]
- 10.Scheufler KM, Franke J, Eckardt A, Dohmen H. Accuracy of image-guided pedicle screw placement using intraoperative computed tomography-based navigation with automated referencing, part I: cervicothoracic spine. Neurosurgery. 2011;69:782–795. doi: 10.1227/NEU.0b013e318222ae16. [DOI] [PubMed] [Google Scholar]
- 11.Lee TC, Yang LC, Liliang PC, Su TM, Rau CS, Chen HJ. Single versus separate registration for computer-assisted lumbar pedicle screw placement. Spine (Phila Pa 1976) 2004;29:1585–1589. doi: 10.1097/01.BRS.0000131438.68071.6C. [DOI] [PubMed] [Google Scholar]
- 12.Kalfas IH, Kormos DW, Murphy MA, McKenzie RL, Barnett GH, Bell GR, Steiner CP, Trimble MB, Weisenberger JP. Application of frameless stereotaxy to pedicle screw fixation of the spine. J Neurosurg. 1995;83:641–647. doi: 10.3171/jns.1995.83.4.0641. [DOI] [PubMed] [Google Scholar]
- 13.Papadopoulos EC, Girardi FP, Sama A, Sandhu HS, Cammisa FP., Jr Accuracy of single-time, multilevel registration in image-guided spinal surgery. Spine J. 2005;5:263–267. doi: 10.1016/j.spinee.2004.10.048. [DOI] [PubMed] [Google Scholar]