Abstract
Hepatocellular carcinoma (HCC) is the third-leading cause of cancer-related mortality worldwide. Although hepatitis B still remains the most common risk factor worldwide, chronic hepatitis C virus (HCV) infection is the driving force for the increased incidence of HCC especially in Western countries and Japan. In hepatitis B virus (HBV)-endemic areas, after successful vaccination programs against HBV, chronic HCV infection is now emerging as an important cause of chronic liver diseases. Unlike patients with chronic hepatitis B, those with chronic hepatitis C (CHC) develop HCC in the presence of established cirrhosis in most cases. However, a significant minority of CHC develops HCC in the absence of cirrhosis. Although HCV is a RNA virus with little potential for integrating its genetic material into host genome, various HCV proteins, including core, envelope, and nonstructural proteins, have oncogenic properties by inducing oxidative stress, disturbing cellular regulatory pathways associated with proliferation and apoptosis, and suppressing host immune responses. Overall, a combination of virus-specific, host genetic, environmental, and immune-related factors are likely to determine progression to HCC. Strategies aimed at eliminating the virus may provide opportunities for effective prevention of the development of HCC. Pegylated interferon plus ribavirin therapy appears to be effective at reducing the risk of HCC in patients who achieve sustained virologic responses. In summary, with the emerging importance of CHC, mechanisms of HCV-associated hepatocellular carcinogenesis should be clarified to provide insight into advanced therapeutic and preventive approaches, which eventually decrease the incidence and mortality of HCC.
Keywords: Hepatocellular carcinoma, Hepatitis C virus
Introduction
Hepatocellular carcinoma (HCC), accounting for >5 % of cancers globally, is ranked as the 6th most common cancer and the 3rd leading cause of cancer-related death worldwide. The incidence of HCC may continue increasing over the next 20 years and to peak around 2030 [1–3]. Etiologically, chronic hepatitis B (CHB) still remains the most common risk factor for HCC worldwide, however, after successful vaccination program against hepatitis B virus (HBV), chronic hepatitis C (CHC) has become an important cause of chronic liver diseases (CLDs) in both Western countries and the Asia–Pacific region. Nowadays, there are an estimated 170 million infected with hepatitis C virus (HCV) globally, and the incidence of HCC and HCV has increased in recent decades, suggesting an etiologic link. In Korea, about 10 % of cirrhosis and 12–17 % of HCC were due to HCV infection [1–3]. Even though the risk of transfusion-related HCV infection is almost zero in developed countries, infections via injection drug use and certain insanitary practices, such as acupuncture, tattooing, and body piercing, have become an emerging medical issue. HCC is a common cause of liver-related death among HCV-infected persons, developing predominantly in those with cirrhosis. Nevertheless, several studies have reported that HCC occurs in persons with bridging fibrosis without definite cirrhosis, although far less commonly [4–8]. To date, there are new insights into HCV-related hepatocarcinogenesis.
This article reviews hepatocarcinogenesis and measures for predicting and preventing the development of HCC in patients with chronic HCV infection.
Hepatocarcinogenesis in HCV
Since HCV lacks reverse transcriptase activity unlike HBV, it does not integrate into the host genome. Furthermore, as HCV is a completely cytoplasmic-replicating virus, the main hypothesis for carcinogenesis is that it occurs via indirect pathways through the effects of chronic inflammation, oxidative stress and subsequent hepatocellular injury. This assumption is supported by the fact that the presence of cirrhosis is almost a prerequisite for HCC development [9]. As a matter of fact, this is why patients with CHC are less likely to be candidates for hepatic resection in terms of preoperative liver functions and tumor locations, multiplicity, and invasiveness and have a higher cumulative recurrence rate, even after surgery, than those with CHB [10–12].
However, it is unlikely that necro-inflammation alone is sufficient to cause HCC. As a matter of fact, a significant minority arises in the absence of cirrhosis and other lines of evidence suggest that direct, virus-specific mechanisms may be involved [13, 14]. Recent studies have suggested that various HCV proteins, including the core, envelope, and nonstructural proteins, exert direct oncogenic effects by inducing oxidative stress, disturbing cellular regulatory pathways associated with proliferation and apoptosis, and suppressing host immune responses [13–15] (Fig. 1). HCV core protein, a 21-kDa nucleocapsid protein involved in binding viral RNA, is involved not only in viral particle assembly and generation of complete virions, but also in cell signalling, transcription activation, apoptosis, lipid metabolism and transformation [16, 17]. There are several hypotheses concerning its role in carcinogenesis [13, 18–22]. First, HCV core protein has been shown to induce reactive oxygen species even in the absence of inflammation. The oxidative stress may decrease metabolic processes within mitochondria, with a decline in microsomal triglyceride transfer protein activity, resulting in the development of steatosis [14, 23–26]. Second, it has also been shown to affect cellular regulatory pathways. For example, it can bind to p53 and pRb, tumor suppressor proteins and modulate the expression of p21/Waf, which is involved in cell cycle control, and interact with cytoplasmic signal transduction molecules to regulate transcription [16, 27]. More recently, HCV core protein seems to increase the serine phosphorylation of insulin receptor substrate (IRS)-1 and to activate c-Jun N-terminal kinase signaling and the proteasome activator 28γ, all of which are associated with insulin resistance [28–30]. Such hyperinsulinemia from insulin resistance—by its action on hepatic stellate cells, extracellular matrix, endothelial cells or connective growth factors—not only can accelerate the progression of fibrosis [31, 32], but also can increase accumulation of free fatty acids in the liver, leading to activation of some kinases, such as protein kinase C delta, inhibitor kappa B kinase, JNK, or mammalian target of rapamycin (mTOR) that are known to promote carcinogenesis [33, 34].
Fig. 1.
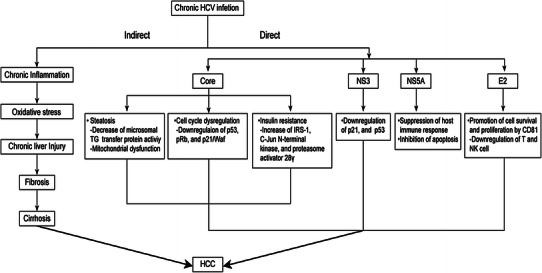
A schematic display of HCV-specific hepatocarcinogenesis. Various HCV proteins, including the core, nonstructural proteins (NS3, NS5A), and E2 exert direct oncogenic effects by inducing oxidative stress, disturbing cellular regulatory pathways associated with proliferation and apoptosis, and suppressing host immune responses. HCV hepatitis C virus, HCC hepatocellular carcinoma
Apart from the core proteins, other HCV proteins have also been shown to contribute to hepatocarcinogenesis. For example, NS3 can promote hepatocarcinogenesis by its interaction with certain proteins, such as p21 and p53, whereas NS5A can also interact with cellular signalling components and regulatory protein kinases, leading to the suppression of the host immune response and inhibition of apoptosis [35–38]. Furthermore, the truncated form of HCV NS5A can become localized to the nucleus to act as a transcriptional activator. Besides, The E2 protein can interact with CD81 and inhibit T and NK cells, thereby promoting cell survival and proliferation.
Taken together, complex interactions of the various HCV proteins with host cell factors have also been shown to be sufficient to induce hepatocarcinogenesis, through alteration of cellular signaling cascades involved in cell metabolism and division [13, 14]. Overall, the synergism of indirect chronic inflammation and direct virus-host cell interactions are likely to determine the progression to HCC in patients with CHC.
How to predict HCC development?
As aforementioned, although HCV-specific hepatocarcinogenesis had been spotlighted recently, chronic inflammation and oxidative stress from immune responses against infected hepatocytes and resultant hepatic fibrosis still remain the major pathogenesis for development of HCC. Since such processes facilitate the accumulation of genetic alterations simultaneously, approximately half of cirrhotic nodules harbor chromosomal abnormalities and a loss of alleles [38]. Thus, an accurate assessment of overall fibrotic burden is an important prerequisite for risk stratification of HCC development.
Recently, liver stiffness (LS) measured noninvasively by transient elastography (TE) has been reported to be well correlated with histologically assessed liver fibrosis degree [39–43]. The principle of TE is based on the principle that the propagation velocity of a wave through a homogenous tissue is proportional to its elasticity, so livers with increasing degrees of scarring have decreasing elasticity and that a shear wave propagating through stiffer material would progress faster than in one with more elastic material [41, 44]. From this viewpoint, the role of TE for risk stratification of development of HCC have been evaluated to date [45, 46]. The first large prospective cohort study of 866 Japanese patients with CHC tested whether TE can predict the future development of HCC [45, 46]. During a mean follow-up of 3 years, 77 patients developed HCC. By multivariate analysis, together with age, male gender, and clinical cirrhosis, stratified TE value was identified as an independent risk factor for HCC development, with relative risks of 16.7, 20.0, 25.6, and 45.5 for TE values of 10–15, 15–20, 20–25, and >25 kPa, respectively, versus an TE value of <10 kPa as the reference and the cumulative incidence of HCC showed a step-wise increase according to stratified TE value. Interestingly, in this study, even patients with not so high level of TE (10–15 kPa) were still more subject to HCC development with an adjusted HR of 16.7, compared to those with a TE value <10 kPa. Overall, the fibrotic burden estimated by TE has shown the potential for a clinical role in predicting the development of HCC and, in part, demonstrated superior performance to histology and other noninvasive tools [47–52]. This is most likely due to the wider dynamic range of TE values in the evaluation of liver cirrhosis. In fact, as the stage of ‘‘cirrhosis’’ has to date been defined by histopathological evidence of one or two qualitative categories (METAVIR stage F4 or ISHAK S5–S6), or more generally by the presence of so-called ‘‘regenerative’’ or ‘‘cirrhotic nodules,’’ an interval scale cannot be used in this setting. However, the degree of liver fibrosis may vary widely among patients in this category, and the risk of HCC may not be uniform. Thus, in this regard, because TE value, expressed in kPa as a continuous variable, has a wide dynamic range within the cirrhotic stage from the cutoff level from non-cirrhosis (15–17 kPa) to the upper measurement limit of present devices (75 kPa), it would seem to be a more reasonable tool for detailed prognostication.
Prevention of development of HCC in patients with chronic HCV infection
The first prevention for HCV-associated HCC is avoidance of chronic HCV infection. However, unfortunately, vaccination against de novo HCV infection is currently not available, in contrast to HBV infection. Accordingly, the next step to reduce HCV-associated HCC is the effective eradication of HCV from the host using antiviral therapy from the viewpoint of the 2nd prevention. For several decades, interferon (IFN)-based therapy appears to be effective at both controlling HCV infection and reducing the risk of HCC [46]. Its preventive effect is the highest among patients who achieve sustained virologic response (SVR). A meta-analysis found that SVR was associated with a 79 % (95 % CI 0.73–0.84) reduction in the risk of development of HCC by patients with HCV-related cirrhosis. Such treatment to eradicate HCV is contributable to reduce hepatic fibrosis and cirrhosis, and prevention of HCC [53–55]. The cumulative incidences of HCC in treated and control patients with cirrhosis were 7.8 and 24.2 %, respectively (hazard ratio [HR], 0.45; 95 % confidence interval [CI], 0.24–0.83). Table 1 summarizes several RCTs where the risk of developing HCC had been reduced after successful antiviral therapy. A recent study suggested the additional benefit of IFN-based therapy among patients with cirrhosis even though they did not have a SVR to therapy. However, several large scaled randomized trials (HALT-C, COPILOT, and EPIC) have demonstrated that maintenance pegylated (PEG)-IFN fails to prevent HCC in patients with HCV-related cirrhosis among nonresponders. Lok et al. [56] reported that extended follow-up of the HALT-C Trial cohort for a median of 6.1 years showed a modest benefit of long-term PEG-IFN therapy in reducing the incidence of HCC in patients with hepatitis C and cirrhosis but not in those with advanced pre-cirrhotic fibrosis. HCV therapy has been revolutionized recently by development and approval of direct-acting antiviral agents (DAA), yielded by extensive researches of the crystal structure of several critical viral proteins [57–59]. In the year 2011, the first two DAAs, telaprevir (Incivek; Vertex Pharmaceuticals Cambridge, MA, USA) and boceprevir (Victrelis; Merck & Co Whitehouse Station, NJ, USA), both inhibiting the NS3/4A protease, had been approved for use in patients with chronic HCV infection with genotype 1 and marked the beginning of a new era in HCV therapy. Several clinical trials demonstrated that these two drugs were potent for the efficacy and safety in treatment-naïve genotype 1 HCV infection [60–62]. The addition of telaprevir and boceprevir to the standard PEG-IFN and ribavirin regimen has provided a major advance in the treatment-naïve and –experienced genotype 1 patients. Moreover, with the improvement of SVR rate with these new drugs, the rate of HCC development will be lower accordingly.
Table 1.
Summary of randomized controlled trials on incidence of HCC among patients with HCV infection
| Author (year) | n | Control group (untreated) | Treatment group | P value | ||
|---|---|---|---|---|---|---|
| No. HCC/no. cases | (%) | No. HCC/no. cases | (%) | |||
| Mazzella et al. [77] | 284 | 9/92 | 9.8 | 5/193 | 2.6 | <0.05 |
| Valla et al. [78] | 99 | 9/52 | 17 | 5/47 | 11 | NS |
| Bernandinello et al. [79] | 61 | 1/23 | 4.3 | 2/38 | 5.3 | NS |
| Nishiguchi et al. [80] | 90 | 33/45 | 73 | 12/45 | 27 | <0.05 |
| Planas et al. [81] | 50 | 2/21 | 9.5 | 1/19 | 5.3 | NS |
| Azzaroli et al. [82] | 60 | 9/30 | 30 | 0/30 | 0 | <0.05 |
| Soga et al. [83] | 133 | 7/30 | 23.3 | 5/103 | 4.9 | <0.05 |
| Fartoux et al. [84] | 102 | 6/51 | 11.8 | 6/51 | 11.8 | NS |
| Lok et al. [56] | 427 | 34/220 | 15.5 | 14/207 | 6.8 | <0.05 |
| Bruix et al. [85] | 626 | 4/315 | 1.3 | 4/311 | 1.3 | NS |
HCC hepatocellular carcinoma, HCV hepatitis C virus, NS non significance
Although HCC has been treated curatively, such patients are still at risk of developing HCC in the future. As a matter of fact, more than half of the patients successfully treated with surgical resection experience recurrent HCCs within 5 years of surgery, despite successful resection. Therefore, for such “high-risk subjects”, so called the 3rd prevention might be beneficial. Recurrences should be differentiated into early and late recurrences. Early recurrences are the result of occult metastasis left behind after resection. Such tumors will usually become apparent within 2 years of surgery. In contrast, late or de novo recurrences are new, typically occurring more than 2 years after surgery, as the result of the underlying procarcinogenic liver disease, caused by cirrhosis itself or HCV. There have been several randomized controlled trials (RCTs) and at least one meta-analysis about effect of IFN therapy after resection of HCC, most of which consistently favors the use of IFN-based therapy [63, 64]. A meta-analysis by Singal et al. [63] showed that IFN-based therapy could reduce the risk of developing a new focus of HCC and that the benefit of IFN for HCC recurrence was stronger with SVR compared with non-responders [0.19 (0.06–0.60); P = 0.005]. However, notably, the benefit of antiviral therapy and SVR is primarily limited to prevention of late recurrence.
Taken together, since recent lines of evidence suggest the potential roles of virus-specific mechanisms [16, 17], the importance of an effective eradication of HCV from host can not be overestimated to reduce the risk of de novo development of HCC.
Management of HCC
Although surgical resection or local ablative therapies such as radiofrequency ablation (RFA) and percutaneous ethanol injection (PEI) achieve the best outcomes with a 5-year survival rate of 60–70 % in patients treated during early stages, only about 30 % are amenable to potentially curative treatments. Eventually, most patients are eligible for only palliative treatments in hope of prolonging life, and a multidisciplinary therapeutic approach is required for optimal treatment outcome. Nowadays, the molecular target agents have been spotlighted for several years. Sorafenib, an oral multikinase inhibitor blocking tumor cell proliferation and tumor angiogenesis by inhibiting serine/threonine kinase and several receptor tyrosine kinases such as vascular endothelial growth factor receptors (VEGFRs) 2 and 3, platelet-derived growth factor receptor-β, Fms-related tyrosine kinase (Flt), and c-kit had shown the proven survival benefits compared to the best supportive care through the two large trials [65–68].
In 2008, the SHARP trial in which 602 patients with advanced HCC were randomized to receive either sorafenib 400 mg b.i.d. (n = 299) or a placebo (n = 303) demonstrated that overall survival (OS) was significantly prolonged in sorafenib-treated patients compared with placebo group (10.7 vs. 7.9 months, respectively, p < 0.001) [65]. Furthermore, sorafenib significantly improved the time to disease progression (TTP) compared to placebo (5.5 vs. 2.8 months, respectively, p < 0.001). Following the SHARP trial, Cheng et al. [69] published a large-scale Asia–Pacific Phase III randomized trial of sorafenib versus placebo in 226 Asian patients (150 received sorafenib and 76 received placebo) from China, South Korea, and Taiwan study. This study had similar aims and design as the SHARP trial. The median OS was 6.5 vs. 4.2 months in the sorafenib and placebo groups, respectively (p = 0.014), whereas the median TTP was 2.8 vs. 1.4 months, respectively (p < 0.001). In this study, common drug-related adverse events included hand-foot skin reactions (45.0 %), diarrhea (25.5 %), alopecia (24.8 %), fatigue (20.1 %), rash or desquamation (20.1 %), hypertension (18.8 %), and anorexia (12.8 %). However, compared to the SHARP trial, more patients with hand-foot skin reactions and fewer with diarrhea were observed in the Asia–Pacific study [65, 69].
Notably, compared with the SHARP trial, the absolute median OS and TTP were shorter in the Asia–Pacific study, which might presumably have resulted from the difference in the baseline characteristics of enrolled subjects, suggesting the higher percentage of more advanced disease in the Asia–Pacific study. Similarly, a pilot study where 97 HCC patients with either main portal vein invasion or extrahepatic spread were treated with sorafenib demonstrated that the median TTP and OS were 2.2 and 7.7 months, respectively and that therapy was stopped due to adverse events or cost burden in 34 % of the patients [70]. Another Korean study also reported that the median TTP was 9.1 weeks [71]. The detailed differences between the two trials are summarized in Table 2.
Table 2.
Comparison of the SHARP and Asia–Pacific trials
| SHARP (n = 602) | Asia–Pacific (n = 226) | |
|---|---|---|
| Baseline characteristics | ||
| Median age (range), years | 67 (21–89) | 51 (23–86) |
| ECOG PS, 0/1/2 | 54/38/8 | 26/69/5 |
| Etiology, HBV/HCV | 18/28 | 73/8 |
| Extrahepatic spread | 51 | 69 |
| BCLC stage, B/C | 17/82 | 4/96 |
| End pointa | ||
| Median OS (months) | 10.7 | 6.5 |
| Median TTP (months) | 5.5 | 2.8 |
| Level of response (%)a | ||
| Complete | 0 | 0 |
| Partial | 2 | 3.3 |
| Stable | 71 | 54019858 |
| Disease control rate | 43 | 35.3 |
| Adverse eventsa | ||
| Hand-foot skin reaction | 21 | 67 |
| Hypertension | 5 | 28 |
| Alopecia | 14 | 37 |
Unless otherwise indicated, the values are percentages
ECOG PS Eastern Cooperative Oncology Group performance score, HBV hepatitis B virus, HCV hepatitis C virus, BCLC Barcelona Clinic liver cancer, OS Overall survival, TTP time to progression
aPatients in the sorafenib group were compared
Taken together, sorafenib became standard therapy for the treatment of advanced HCCin Asia as well as Western countries. However, the prognosis of HCC is generally worse than in Western countries. Furthermore, the high cost of sorafenib is an obstacle to its widespread use in clinical practice [69, 72–75]. Nevertheless, sorafenib has a firm position at the core of HCC therapy and its indications are anticipated to widen in the near future to intermediate HCC or as an adjuvant agent with or without a combination modality. A rational approach based on cost, quality of life, and survival will be urgently needed.
Besides, other small molecules, such as brivanib and erlotinib, and monoclonal antibodies, such as bevacizumab and cetuximab, are currently being studied in patients with HCC. Furthermore, the clinical implication of other conventional treatment modalities, including hepatic arterial infusion chemotherapy or localized concurrent chemoradiation therapy for advanced HCC, should be reilluminated in comparison with the novel molecular target agent and the combined methods should be considered to improve clinical outcomes [75, 76].
Conclusions
In Asia, a nationwide vaccination program would eventually decrease HBV-related HCC. Conversely, HCV infection has recently become a significant problem, leading to increase of HCV-related HCC. With the emerging importance of CHC as an etiology for CLDs, there is a pressing need for further research on HCV-associated carcinogenesis to identify the steps from chronic HCV infection to cancer, and that can help developing of prevention, early screening, and treatment. HCV-associated hepatocellular carcinogenesis should be clarified to provide insight into advanced therapeutic and preventive approaches for HCC, which will eventually decrease development of HCC risk and improved survival outcomes. Furthermore, continuous efforts have been put into finding new targets and molecular pathways for possible new drug development.
Acknowledgments
This study was supported by the Liver Cirrhosis Clinical Research Center, in part by a grant from the Korea Healthcare technology R & D project, Ministry of Health and Welfare, Republic of Korea (A102065).
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Yang JD, Roberts LR. Hepatocellular carcinoma: a global view. Nat Rev Gastroenterol Hepatol. 2010;7:448–458. doi: 10.1038/nrgastro.2010.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 3.El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 4.Bege T, Le Treut YP, Hardwigsen J, Ananian P, Richa H, Campan P, et al. Prognostic factors after resection for hepatocellular carcinoma in nonfibrotic or moderately fibrotic liver. A 116-case European series. J Gastrointest Surg. 2007;11:619–625. doi: 10.1007/s11605-006-0023-9. [DOI] [PubMed] [Google Scholar]
- 5.Lawson A, Hagan S, Rye K, Taguri N, Ratib S, Zaitoun AM, et al. The natural history of hepatitis C with severe hepatic fibrosis. J Hepatol. 2007;47:37–45. doi: 10.1016/j.jhep.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Bralet MP, Regimbeau JM, Pineau P, Dubois S, Loas G, Degos F, et al. Hepatocellular carcinoma occurring in nonfibrotic liver: epidemiologic and histopathologic analysis of 80 French cases. Hepatology. 2000;32:200–204. doi: 10.1053/jhep.2000.9033. [DOI] [PubMed] [Google Scholar]
- 7.Le Treut YP, Pons J, Hardwigsen J, Castellani P, Campan P, Hanna X, et al. Hepatocellular carcinoma in a non-cirrhotic liver: presentation of series of 77 operated patients. Chirurgie. 1999;124:485–493. doi: 10.1016/S0001-4001(00)88270-7. [DOI] [PubMed] [Google Scholar]
- 8.Nzeako UC, Goodman ZD, Ishak KG. Hepatocellular carcinoma in cirrhotic and noncirrhotic livers: a clinico-histopathologic study of 804 North American patients. Am J Clin Pathol. 1996;105:65–75. doi: 10.1093/ajcp/105.1.65. [DOI] [PubMed] [Google Scholar]
- 9.Fung J, Lai CL, Yuen MF. Hepatitis B and C virus-related carcinogenesis. Clin Microbiol Infect. 2009;15:964–970. doi: 10.1111/j.1469-0691.2009.03035.x. [DOI] [PubMed] [Google Scholar]
- 10.Yamanaka N, Tanaka T, Tanaka W, Yamanaka J, Yasui C, Kuroda N, et al. Correlation of hepatitis virus serologic status with clinicopathologic features in patients undergoing hepatectomy for hepatocellular carcinoma. Cancer. 1997;79:1509–1515. doi: 10.1002/(SICI)1097-0142(19970415)79:8<1509::AID-CNCR10>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 11.Miyagawa S, Kawasaki S, Makuuchi M. Comparison of the characteristics of hepatocellular carcinoma between hepatitis B and C viral infection: tumor multicentricity in cirrhotic liver with hepatitis C. Hepatology. 1996;24:307–310. doi: 10.1002/hep.510240204. [DOI] [PubMed] [Google Scholar]
- 12.Roayaie S, Haim MB, Emre S, Fishbein TM, Sheiner PA, Miller CM, et al. Comparison of surgical outcomes for hepatocellular carcinoma in patients with hepatitis B versus hepatitis C: a western experience. Ann Surg Oncol. 2000;7:764–770. doi: 10.1007/s10434-000-0764-8. [DOI] [PubMed] [Google Scholar]
- 13.Moriya K, Fujie H, Shintani Y, Yotsuyanagi H, Tsutsumi T, Ishibashi K, et al. The core protein of hepatitis C virus induces hepatocellular carcinoma in transgenic mice. Nat Med. 1998;4:1065–1067. doi: 10.1038/2053. [DOI] [PubMed] [Google Scholar]
- 14.Lerat H, Honda M, Beard MR, Loesch K, Sun J, Yang Y, et al. Steatosis and liver cancer in transgenic mice expressing the structural and nonstructural proteins of hepatitis C virus. Gastroenterology. 2002;122:352–365. doi: 10.1053/gast.2002.31001. [DOI] [PubMed] [Google Scholar]
- 15.Yoshida T, Hanada T, Tokuhisa T, Kosai K, Sata M, Kohara M, et al. Activation of STAT3 by the hepatitis C virus core protein leads to cellular transformation. J Exp Med. 2002;196:641–653. doi: 10.1084/jem.20012127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lai MM, Ware CF. Hepatitis C virus core protein: possible roles in viral pathogenesis. Curr Top Microbiol Immunol. 2000;242:117–134. doi: 10.1007/978-3-642-59605-6_6. [DOI] [PubMed] [Google Scholar]
- 17.Liang TJ, Heller T. Pathogenesis of hepatitis C-associated hepatocellular carcinoma. Gastroenterology. 2004;127:S62–S71. doi: 10.1053/j.gastro.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 18.Yamashita T, Honda M, Takatori H, Nishino R, Minato H, Takamura H, et al. Activation of lipogenic pathway correlates with cell proliferation and poor prognosis in hepatocellular carcinoma. J Hepatol. 2009;50:100–110. doi: 10.1016/j.jhep.2008.07.036. [DOI] [PubMed] [Google Scholar]
- 19.Yamashita T, Kaneko S, Hashimoto S, Sato T, Nagai S, Toyoda N, et al. Serial analysis of gene expression in chronic hepatitis C and hepatocellular carcinoma. Biochem Biophys Res Commun. 2001;282:647–654. doi: 10.1006/bbrc.2001.4610. [DOI] [PubMed] [Google Scholar]
- 20.Honda M, Yamashita T, Ueda T, Takatori H, Nishino R, Kaneko S. Different signaling pathways in the livers of patients with chronic hepatitis B or chronic hepatitis C. Hepatology. 2006;44:1122–1138. doi: 10.1002/hep.21383. [DOI] [PubMed] [Google Scholar]
- 21.Honda M, Kaneko S, Kawai H, Shirota Y, Kobayashi K. Differential gene expression between chronic hepatitis B and C hepatic lesion. Gastroenterology. 2001;120:955–966. doi: 10.1053/gast.2001.22468. [DOI] [PubMed] [Google Scholar]
- 22.Akuta N, Suzuki F, Kawamura Y, Yatsuji H, Sezaki H, Suzuki Y, et al. Amino acid substitutions in the hepatitis C virus core region are the important predictor of hepatocarcinogenesis. Hepatology. 2007;46:1357–1364. doi: 10.1002/hep.21836. [DOI] [PubMed] [Google Scholar]
- 23.Moriya K, Yotsuyanagi H, Shintani Y, Fujie H, Ishibashi K, Matsuura Y, et al. Hepatitis C virus core protein induces hepatic steatosis in transgenic mice. J Gen Virol. 1997;78(Pt 7):1527–1531. doi: 10.1099/0022-1317-78-7-1527. [DOI] [PubMed] [Google Scholar]
- 24.Perlemuter G, Sabile A, Letteron P, Vona G, Topilco A, Chretien Y, et al. Hepatitis C virus core protein inhibits microsomal triglyceride transfer protein activity and very low density lipoprotein secretion: a model of viral-related steatosis. FASEB J. 2002;16:185–194. doi: 10.1096/fj.01-0396com. [DOI] [PubMed] [Google Scholar]
- 25.Moriya K, Nakagawa K, Santa T, Shintani Y, Fujie H, Miyoshi H, et al. Oxidative stress in the absence of inflammation in a mouse model for hepatitis C virus-associated hepatocarcinogenesis. Cancer Res. 2001;61:4365–4370. [PubMed] [Google Scholar]
- 26.Okuda M, Li K, Beard MR, Showalter LA, Scholle F, Lemon SM, et al. Mitochondrial injury, oxidative stress, and antioxidant gene expression are induced by hepatitis C virus core protein. Gastroenterology. 2002;122:366–375. doi: 10.1053/gast.2002.30983. [DOI] [PubMed] [Google Scholar]
- 27.Kwun HJ, Jang KL. Dual effects of hepatitis C virus Core protein on the transcription of cyclin-dependent kinase inhibitor p21 gene. J Viral Hepat. 2003;10:249–255. doi: 10.1046/j.1365-2893.2003.00434.x. [DOI] [PubMed] [Google Scholar]
- 28.Miyamoto H, Moriishi K, Moriya K, Murata S, Tanaka K, Suzuki T, et al. Involvement of the PA28gamma-dependent pathway in insulin resistance induced by hepatitis C virus core protein. J Virol. 2007;81:1727–1735. doi: 10.1128/JVI.01683-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Banerjee S, Saito K, Ait-Goughoulte M, Meyer K, Ray RB, Ray R. Hepatitis C virus core protein upregulates serine phosphorylation of insulin receptor substrate-1 and impairs the downstream akt/protein kinase B signaling pathway for insulin resistance. J Virol. 2008;82:2606–2612. doi: 10.1128/JVI.01672-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bugianesi E, Salamone F, Negro F. The interaction of metabolic factors with HCV infection: does it matter? J Hepatol. 2012;56(Suppl 1):S56–S65. doi: 10.1016/S0168-8278(12)60007-5. [DOI] [PubMed] [Google Scholar]
- 31.Laron Z. Insulin–a growth hormone. Arch Physiol Biochem. 2008;114:11–16. doi: 10.1080/13813450801928356. [DOI] [PubMed] [Google Scholar]
- 32.White DL, Ratziu V, El-Serag HB. Hepatitis C infection and risk of diabetes: a systematic review and meta-analysis. J Hepatol. 2008;49:831–844. doi: 10.1016/j.jhep.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jiang W, Zhu Z, Thompson HJ. Dietary energy restriction modulates the activity of AMP-activated protein kinase, Akt, and mammalian target of rapamycin in mammary carcinomas, mammary gland, and liver. Cancer Res. 2008;68:5492–5499. doi: 10.1158/0008-5472.CAN-07-6721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Villanueva A, Chiang DY, Newell P, Peix J, Thung S, Alsinet C, et al. Pivotal role of mTOR signaling in hepatocellular carcinoma. Gastroenterology (2008);135:1972–1883, 83e1–11. [DOI] [PMC free article] [PubMed]
- 35.Kwun HJ, Jung EY, Ahn JY, Lee MN, Jang KL. p53-dependent transcriptional repression of p21(waf1) by hepatitis C virus NS3. J Gen Virol. 2001;82:2235–2241. doi: 10.1099/0022-1317-82-9-2235. [DOI] [PubMed] [Google Scholar]
- 36.Reyes GR. The nonstructural NS5A protein of hepatitis C virus: an expanding, multifunctional role in enhancing hepatitis C virus pathogenesis. J Biomed Sci. 2002;9:187–197. doi: 10.1007/BF02256065. [DOI] [PubMed] [Google Scholar]
- 37.Tanji Y, Kaneko T, Satoh S, Shimotohno K. Phosphorylation of hepatitis C virus-encoded nonstructural protein NS5A. J Virol. 1995;69:3980–3986. doi: 10.1128/jvi.69.7.3980-3986.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Levrero M. Viral hepatitis and liver cancer: the case of hepatitis C. Oncogene. 2006;25:3834–3847. doi: 10.1038/sj.onc.1209562. [DOI] [PubMed] [Google Scholar]
- 39.Foucher J, Chanteloup E, Vergniol J, Castera L, Le Bail B, Adhoute X, et al. Diagnosis of cirrhosis by transient elastography (FibroScan): a prospective study. Gut. 2006;55:403–408. doi: 10.1136/gut.2005.069153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ziol M, Handra-Luca A, Kettaneh A, Christidis C, Mal F, Kazemi F, et al. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Hepatology. 2005;41:48–54. doi: 10.1002/hep.20506. [DOI] [PubMed] [Google Scholar]
- 41.Sandrin L, Fourquet B, Hasquenoph JM, Yon S, Fournier C, Mal F, et al. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003;29:1705–1713. doi: 10.1016/j.ultrasmedbio.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 42.Ganne-Carrie N, Ziol M, de Ledinghen V, Douvin C, Marcellin P, Castera L, et al. Accuracy of liver stiffness measurement for the diagnosis of cirrhosis in patients with chronic liver diseases. Hepatology. 2006;44:1511–1517. doi: 10.1002/hep.21420. [DOI] [PubMed] [Google Scholar]
- 43.Castera L, Vergniol J, Foucher J, Le Bail B, Chanteloup E, Haaser M, et al. Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 2005;128:343–350. doi: 10.1053/j.gastro.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 44.Yeh WC, Li PC, Jeng YM, Hsu HC, Kuo PL, Li ML, et al. Elastic modulus measurements of human liver and correlation with pathology. Ultrasound Med Biol. 2002;28:467–474. doi: 10.1016/S0301-5629(02)00489-1. [DOI] [PubMed] [Google Scholar]
- 45.Masuzaki R, Tateishi R, Yoshida H, Sato S, Kato N, Kanai F, et al. Risk assessment of hepatocellular carcinoma in chronic hepatitis C patients by transient elastography. J Clin Gastroenterol. 2008;42:839–843. doi: 10.1097/MCG.0b013e318050074f. [DOI] [PubMed] [Google Scholar]
- 46.Masuzaki R, Tateishi R, Yoshida H, Goto E, Sato T, Ohki T, et al. Prospective risk assessment for hepatocellular carcinoma development in patients with chronic hepatitis C by transient elastography. Hepatology. 2009;49:1954–1961. doi: 10.1002/hep.22870. [DOI] [PubMed] [Google Scholar]
- 47.Jung KS, Kim SU. Clinical applications of transient elastography. Clin Mol Hepatol. 2012;18:163–173. doi: 10.3350/cmh.2012.18.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Poca M, Puente A, Graupera I, Villanueva C. Prognostic markers in patients with cirrhosis and portal hypertension who have not bled. Dis Markers. 2011;31:147–154. doi: 10.1155/2011/537970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robic MA, Procopet B, Metivier S, Peron JM, Selves J, Vinel JP, et al. Liver stiffness accurately predicts portal hypertension related complications in patients with chronic liver disease: a prospective study. J Hepatol. 2011;55:1017–1024. doi: 10.1016/j.jhep.2011.01.051. [DOI] [PubMed] [Google Scholar]
- 50.Pesce A, Scilletta R, Branca A, Nigro L, Montineri A, Larocca L, et al. Does transient elastography (FibroScan(R)) have a role in decision making in hepatocellular carcinoma? HPB (Oxford) 2012;14:403–408. doi: 10.1111/j.1477-2574.2012.00465.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Motosugi U, Ichikawa T, Koshiishi T, Sano K, Morisaka H, Ichikawa S, et al. Liver stiffness measured by magnetic resonance elastography as a risk factor for hepatocellular carcinoma: a preliminary case-control study. Eur Radiol. 2013;23(1):156–62. doi: 10.1007/s00330-012-2571-6. [DOI] [PubMed] [Google Scholar]
- 52.Masuzaki R, Tateishi R, Yoshida H, Arano T, Uchino K, Enooku K, et al. Assessment of disease progression in patients with transfusion-associated chronic hepatitis C using transient elastography. World J Gastroenterol. 2012;18:1385–1390. doi: 10.3748/wjg.v18.i12.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McHutchison JG, Poynard T, Esteban-Mur R, Davis GL, Goodman ZD, Harvey J, et al. Hepatic HCV RNA before and after treatment with interferon alone or combined with ribavirin. Hepatology. 2002;35:688–693. doi: 10.1053/jhep.2002.31870. [DOI] [PubMed] [Google Scholar]
- 54.McHutchison JG, Patel K. Future therapy of hepatitis C. Hepatology. 2002;36:S245–S252. doi: 10.1002/hep.1840360731. [DOI] [PubMed] [Google Scholar]
- 55.Shiratori Y, Imazeki F, Moriyama M, Yano M, Arakawa Y, Yokosuka O, et al. Histologic improvement of fibrosis in patients with hepatitis C who have sustained response to interferon therapy. Ann Intern Med. 2000;132:517–524. doi: 10.7326/0003-4819-132-7-200004040-00002. [DOI] [PubMed] [Google Scholar]
- 56.Lok AS, Everhart JE, Wright EC, Di Bisceglie AM, Kim HY, Sterling RK, et al. Maintenance peginterferon therapy and other factors associated with hepatocellular carcinoma in patients with advanced hepatitis C. Gastroenterology 2011;140:840–9; quiz e12 [DOI] [PMC free article] [PubMed]
- 57.Choo QL, Kuo G, Weiner AJ, Overby LR, Bradley DW, Houghton M. Isolation of a cDNA clone derived from a blood-borne non-A, non-B viral hepatitis genome. Science. 1989;244:359–362. doi: 10.1126/science.2523562. [DOI] [PubMed] [Google Scholar]
- 58.Kim JL, Morgenstern KA, Lin C, Fox T, Dwyer MD, Landro JA, et al. Crystal structure of the hepatitis C virus NS3 protease domain complexed with a synthetic NS4A cofactor peptide. Cell. 1996;87:343–355. doi: 10.1016/S0092-8674(00)81351-3. [DOI] [PubMed] [Google Scholar]
- 59.Bressanelli S, Tomei L, Roussel A, Incitti I, Vitale RL, Mathieu M, et al. Crystal structure of the RNA-dependent RNA polymerase of hepatitis C virus. Proc Natl Acad Sci USA. 1999;96:13034–13039. doi: 10.1073/pnas.96.23.13034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McHutchison JG, Everson GT, Gordon SC, Jacobson IM, Sulkowski M, Kauffman R, et al. Telaprevir with peginterferon and ribavirin for chronic HCV genotype 1 infection. N Engl J Med. 2009;360:1827–1838. doi: 10.1056/NEJMoa0806104. [DOI] [PubMed] [Google Scholar]
- 61.Hezode C, Forestier N, Dusheiko G, Ferenci P, Pol S, Goeser T, et al. Telaprevir and peginterferon with or without ribavirin for chronic HCV infection. N Engl J Med. 2009;360:1839–1850. doi: 10.1056/NEJMoa0807650. [DOI] [PubMed] [Google Scholar]
- 62.Kwo PY, Lawitz EJ, McCone J, Schiff ER, Vierling JM, Pound D, et al. Efficacy of boceprevir, an NS3 protease inhibitor, in combination with peginterferon alfa-2b and ribavirin in treatment-naive patients with genotype 1 hepatitis C infection (SPRINT-1): an open-label, randomised, multicentre phase 2 trial. Lancet. 2010;376:705–716. doi: 10.1016/S0140-6736(10)60934-8. [DOI] [PubMed] [Google Scholar]
- 63.Singal AK, Freeman DH, Jr, Anand BS. Meta-analysis: interferon improves outcomes following ablation or resection of hepatocellular carcinoma. Aliment Pharmacol Ther. 2010;32:851–858. doi: 10.1111/j.1365-2036.2010.04414.x. [DOI] [PubMed] [Google Scholar]
- 64.Ueno Y, Sollano JD, Farrell GC. Prevention of hepatocellular carcinoma complicating chronic hepatitis C. J Gastroenterol Hepatol. 2009;24:531–536. doi: 10.1111/j.1440-1746.2009.05814.x. [DOI] [PubMed] [Google Scholar]
- 65.Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 66.Wilhelm S, Chien DS. BAY 43–9006: preclinical data. Curr Pharm Des. 2002;8:2255–2257. doi: 10.2174/1381612023393026. [DOI] [PubMed] [Google Scholar]
- 67.Wilhelm SM, Carter C, Tang L, Wilkie D, McNabola A, Rong H, et al. BAY 43–9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004;64:7099–7109. doi: 10.1158/0008-5472.CAN-04-1443. [DOI] [PubMed] [Google Scholar]
- 68.Carlomagno F, Anaganti S, Guida T, Salvatore G, Troncone G, Wilhelm SM, et al. BAY 43–9006 inhibition of oncogenic RET mutants. J Natl Cancer Inst. 2006;98:326–334. doi: 10.1093/jnci/djj069. [DOI] [PubMed] [Google Scholar]
- 69.Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25–34. doi: 10.1016/S1470-2045(08)70285-7. [DOI] [PubMed] [Google Scholar]
- 70.Lee HC. Systemic chemotherapy of hepatocellular carcinoma–Korean experience. Oncology. 2008;75(Suppl 1):114–118. doi: 10.1159/000173432. [DOI] [PubMed] [Google Scholar]
- 71.Shim JH, Park JW, Choi JI, Park BJ, Kim CM. Practical efficacy of sorafenib monotherapy for advanced hepatocellular carcinoma patients in a Hepatitis B virus-endemic area. J Cancer Res Clin Oncol. 2009;135:617–625. doi: 10.1007/s00432-008-0496-x. [DOI] [PubMed] [Google Scholar]
- 72.Yeung YP, Lo CM, Liu CL, Wong BC, Fan ST, Wong J. Natural history of untreated nonsurgical hepatocellular carcinoma. Am J Gastroenterol. 2005;100:1995–2004. doi: 10.1111/j.1572-0241.2005.00229.x. [DOI] [PubMed] [Google Scholar]
- 73.Park KW, Park JW, Choi JI, Kim TH, Kim SH, Park HS, et al. Survival analysis of 904 patients with hepatocellular carcinoma in a hepatitis B virus-endemic area. J Gastroenterol Hepatol. 2008;23:467–473. doi: 10.1111/j.1440-1746.2007.05112.x. [DOI] [PubMed] [Google Scholar]
- 74.Cancer of the Liver Italian Program (CLIP) investigators. A new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients: the Cancer of the Liver Italian Program (CLIP) investigators. Hepatology 1998;28:751–5. [DOI] [PubMed]
- 75.Llovet JM, Bustamante J, Castells A, Vilana R, Ayuso Mdel C, Sala M, et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology. 1999;29:62–67. doi: 10.1002/hep.510290145. [DOI] [PubMed] [Google Scholar]
- 76.Han KH, Seong J, Kim JK, Ahn SH, Lee do Y, Chon CY. Pilot clinical trial of localized concurrent chemoradiation therapy for locally advanced hepatocellular carcinoma with portal vein thrombosis. Cancer. 2008;113:995–1003. doi: 10.1002/cncr.23684. [DOI] [PubMed] [Google Scholar]
- 77.Mazzella G, Accogli E, Sottili S, Festi D, Orsini M, Salzetta A, et al. Alpha interferon treatment may prevent hepatocellular carcinoma in HCV-related liver cirrhosis. J Hepatol. 1996;24:141–147. doi: 10.1016/S0168-8278(96)80022-5. [DOI] [PubMed] [Google Scholar]
- 78.Valla DC, Chevallier M, Marcellin P, Payen JL, Trepo C, Fonck M, et al. Treatment of hepatitis C virus-related cirrhosis: a randomized, controlled trial of interferon alfa-2b versus no treatment. Hepatology. 1999;29:1870–1875. doi: 10.1002/hep.510290616. [DOI] [PubMed] [Google Scholar]
- 79.Bernardinello E, Cavalletto L, Chemello L, Mezzocolli I, Donada C, Benvegnu L, et al. Long-term clinical outcome after beta-interferon therapy in cirrhotic patients with chronic hepatitis C: TVVH Study Group. Hepatogastroenterology. 1999;46:3216–3222. [PubMed] [Google Scholar]
- 80.Nishiguchi S, Shiomi S, Nakatani S, Takeda T, Fukuda K, Tamori A, et al. Prevention of hepatocellular carcinoma in patients with chronic active hepatitis C and cirrhosis. Lancet. 2001;357:196–197. doi: 10.1016/S0140-6736(00)03595-9. [DOI] [PubMed] [Google Scholar]
- 81.Planas R, Quer JC, Enriquez J, Barrera JM, Dalmau B, Casanovas T, et al. Induction therapy with interferon alfa-2a in compensated hepatitis C virus-related cirrhosis. Randomized, multicenter study. Med Clin (Barc). 2002;118:641–644. doi: 10.1016/S0025-7753(02)72483-4. [DOI] [PubMed] [Google Scholar]
- 82.Azzaroli F, Accogli E, Nigro G, Trere D, Giovanelli S, Miracolo A, et al. Interferon plus ribavirin and interferon alone in preventing hepatocellular carcinoma: a prospective study on patients with HCV related cirrhosis. World J Gastroenterol. 2004;10:3099–3102. doi: 10.3748/wjg.v10.i21.3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Soga K, Shibasaki K, Aoyagi Y. Effect of interferon on incidence of hepatocellular carcinoma in patients with chronic hepatitis C. Hepatogastroenterology. 2005;52:1154–1158. [PubMed] [Google Scholar]
- 84.Fartoux L, Degos F, Trepo C, Goria O, Cales P, Tran A, et al. Effect of prolonged interferon therapy on the outcome of hepatitis C virus-related cirrhosis: a randomized trial. Clin Gastroenterol Hepatol. 2007;5:502–507. doi: 10.1016/j.cgh.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 85.Bruix J, Poynard T, Colombo M, Schiff E, Burak K, Heathcote EJ, et al. Maintenance therapy with peginterferon alfa-2b does not prevent hepatocellular carcinoma in cirrhotic patients with chronic hepatitis C. Gastroenterology. 2011;140:1990–1999. doi: 10.1053/j.gastro.2011.03.010. [DOI] [PubMed] [Google Scholar]


