Abstract
About half of all cancer patients show a syndrome of cachexia, characterized by anorexia and loss of adipose tissue and skeletal muscle mass. Cachexia can have a profound impact on quality of life, symptom burden, and a patient’s sense of dignity. It is a very serious complication, as weight loss during cancer treatment is associated with more chemotherapy-related side effects, fewer completed cycles of chemotherapy, and decreased survival rates. Numerous cytokines have been postulated to play a role in the etiology of cancer cachexia. Cytokines can elicit effects that mimic leptin signaling and suppress orexigenic ghrelin and neuropeptide Y (NPY) signaling, inducing sustained anorexia and cachexia not accompanied by the usual compensatory response. Furthermore, cytokines have been implicated in the induction of cancer-related muscle wasting. Cytokine-induced skeletal muscle wasting is probably a multifactorial process, which involves a protein synthesis inhibition, an increase in protein degradation, or a combination of both. The best treatment of the cachectic syndrome is a multifactorial approach. Many drugs including appetite stimulants, thalidomide, cytokine inhibitors, steroids, nonsteroidal anti-inflammatory drugs, branched-chain amino acids, eicosapentaenoic acid, and antiserotoninergic drugs have been proposed and used in clinical trials, while others are still under investigation using experimental animals. There is a growing awareness of the positive impact of supportive care measures and development of promising novel pharmaceutical agents for cachexia. While there has been great progress in understanding the underlying biological mechanisms of cachexia, health care providers must also recognize the psychosocial and biomedical impact cachexia can have.
Keywords: Cachexia, Anorexia, Cytokine, Skeletal muscle, Palliative care
Pathophysiology
Hormones and mediators
Leptin is a protein hormone that sends afferent signals from the periphery to the brain that regulates adipose tissue mass [1–3]. The level of leptin is positively correlated with body fat mass, and dynamic changes in plasma leptin concentrations in either direction can activate the efferent energy regulation pathways [1, 4]. Leptin reduces appetite and increases energy expenditure and evidently elicits these effects via the central nervous system [1, 4]. This is achieved by hypothalamic neuropeptides downstream of leptin that regulate food intake and energy expenditure. Starvation or a loss of body fat can lead to a decrease in leptin, which in turn leads to a state of positive energy balance; conversely, food intake exceeds energy expenditure. This compensatory response is mediated by the increased production of ghrelin, neuropeptide Y (NPY), and other appetite-stimulating neuropeptides, and decreased activity of anorexigenic neuropeptides such as corticotropin-releasing factor (CRF) and melanocortin (Fig. 1a). Thus, if a disease process such as cancer was to produce factors that induce or mimic the hypothalamic effect of excess negative feedback signaling from leptin, the expected outcome would be sustained anorexia (lack of appetite) and cachexia (muscle wasting and uncontrolled weight loss), without the usual compensatory response [5]. In fact, in tumor-bearing states, cachectic factors such as cytokines can elicit effects on energy homeostasis that mimic leptin and suppress orexigenic ghrelin and NPY signaling. Consequently, the increases and decreases in hypothalamic actions caused by these mediators induce anorexia and unopposed weight loss (Fig. 1b).
Fig. 1.
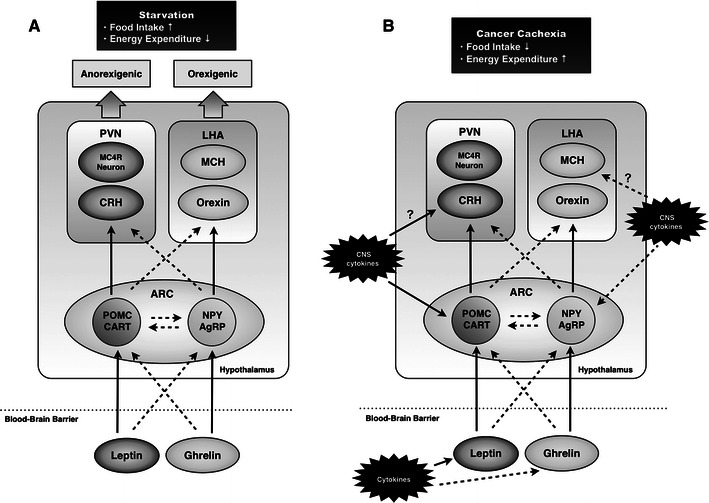
A simplified model of the hypothalamic neuropeptide circuitry in response to starvation (a) and cancer cachexia (b). Full line arrows indicate the activation of the process, and broken line arrows indicate the inhibition of the process. Under normal conditions, energy intake is determined by the hypothalamic integration of peripheral signals conveying inputs on adiposity status, digestive processes, and metabolic profile. Some of these signals such as adipocyte-derived leptin inhibit energy intake, while other signals such as stomach-derived ghrelin stimulate energy intake. In the hypothalamus, the arcuate nucleus (ARC) receives information from the periphery and integrates these inputs to modulate food intake via second-order neurons. According to the information conveyed to the brain, peripheral signals may differentially activate or inhibit POMC/CART and NPY/AgRP neurons. When an energy deficit (e.g., starvation) is signaled, orexigenic NPY/AgRP neurons are activated and anorexigenic POMC/CART neurons are inhibited, resulting in increased energy intake. When an energy excess is signaled, NPY/AgRP neurons are inhibited and POMC/CART neurons are activated. During cancer, cachectic factors such as cytokines elicit effects on energy homeostasis that mimic leptin in some respects and suppress orexigenic Ghrelin-NPY/AgRP signaling. Increased brain cytokine expression disrupts hypothalamic neurochemistry, particularly in the ARC where cytokines activate POMC/CART neurons, while inactivate NPY/AgRP neurons. The anorexia and unopposed weight loss in cachexia could be accomplished through persistent inhibition of the NPY orexigenic network and stimulation of anorexigenic neuropeptides, although the hypothalamic pathways participating in this response remain to be determined. AgRP Agouti-related peptide, MCH melanin-concentrating hormone, CART cocaine- and amphetamine-related transcript, NPY neuropeptide Y, POMC pro-opiomelanocortin, CRH corticotropin-releasing hormone, MC4R melanocortin-4 receptor, PVN paraventricular nucleus. LHA lateral hypothalamic area. Source: (5) with modification
Serotonin (5-HT) may also play a role in the development of cancer-induced anorexia. This is because increased levels of plasma and brain tryptophan, the precursor of 5-HT, and interleukin (IL)-1 may underlie the increased serotonergic activity seen in the cancer cachexia. In addition, cisplatin-induced anorexia has become problematic in clinical settings. Cisplatin is a widely used and effective anti-cancer chemotherapy drug, however, the undesirable gastrointestinal side effects associated with it, such as nausea, vomiting, and anorexia, markedly decrease patients’ quality of life, rendering continuation of chemotherapy difficult [6]. Cisplatin-induced gastrointestinal tract disorders are thought to be due to the release of large amounts of 5-HT from enterochromaffin cells, which then bind to 5-HT receptors [6]. 5-HT activates various serotonin receptor subtypes in the gastrointestinal tract and ganglia, exerting a range of biological and physiological effects [6]. It has been reported that a significant increase in 5-HT concentrations in the hypothalamus of cisplatin-treated rats [7]. Accumulated findings suggest that serotonin 2C (5-HT2C) receptor subtypes are involved in appetite regulation [8, 9]. The 5-HT2C receptor subtype is expressed in proopiomelanocortin neurons in the hypothalamus, which is the major site of its anorexigenic action [6]. In the present clinical setting, nausea and vomiting can be controlled by administering 5-HT3 receptor antagonists together with anticancer agents [6]. However, 5-HT3 receptor antagonists may not be sufficiently controlled in cisplatin-induced anorexia [6]. Recent studies have reported that cisplatin-induced anorexia is mediated through reduced gastric and hypothalamic ghrelin secretion, and peripheral 5-HT2B and cerebral 5-HT2C receptor activation are responsible for the phenomenon [6, 10, 11]. Facilitating the gastric and hypothalamic ghrelin secretion through 5-HT2C receptor inhibition can be a useful therapeutic approach for cisplatin-induced anorexia.
Cytokines
Cytokines are protein molecules released by lymphocytes and/or monocyte macrophages [5]. They are released into the circulation and transported to the brain through the blood–brain barrier (BBB) and circumventricular organs (i.e., ‘leaky’ areas in the BBB) [12–17]. Peripheral cytokines may influence the brain via neural pathways or second messengers such as nitric oxide (NO) and prostanoids [5]. Cytokines are also produced by neurons and glial cells within the brain, partly in response to peripheral cytokines [12–17]. Although the site of cytokine synthesis within the brain is dependent on the nature of the stimulus, systemic disease seems to predominantly influence expression in the hypothalamus, the area with the highest densities of receptors [16].
Numerous cytokines, including tumor necrosis factor-alpha (TNF-α), interleukin-1 (IL-1), interleukin-6 (IL-6), and interferon-gamma (IFN-γ), have been postulated to play a role in the etiology of cancer cachexia [12, 13, 18–21]. It is not certain whether the cytokine production is primarily from tumour or host inflammatory cells. It has been hypothesised that either tumour cell production of proinflammatory cytokines or the host inflammatory cell response to tumour cells is the source of the acute phase protein response (APPR) seen in many malignancies and in cachexia [22].
High serum levels of TNF-α, IL-6, and IL-1 have been found in some cancer patients, and the levels of these cytokines seem to correlate with the progression of some tumors [23–25]. Chronic administration of these cytokines, either alone or in combination, is capable of reducing food intake and inducing cancer cachexia [18, 23–26]. The role of TNF-α in mediating cancer cachexia is supported by evidence that intraperitoneal injection of a soluble recombinant human TNF-receptor antagonist improved anorexia in tumor-bearing animals [27]. In humans, IL-1 appears to play a significant role in mediating cachexia, as megestrol acetate has been shown to exert its effects via reduced expression of IL-1 by mononuclear cells beyond its influence on hypothalamic NPY concentrations, which shows orexigenic effect [28]. Interestingly, anorexigenic neurons, such as proopiomelanocortin (POMC)/cocaine and amphetamine-regulated transcript (CART) neurons in the arcuate nucleus of the hypothalamus express the type 1 IL-1 receptor, and intracerebroventricular injection of IL-1 increases the frequency of action potentials of POMC/CART neurons and stimulates the release of alpha-melanocyte-stimulating hormone (α-MSH), which shows anorexigenic effect as well [29].
TNF-α, IL-1, IL-6, and IFN-γ have been implicated in the induction of cancer-related muscle wasting [30]. There is growing evidence that the accelerated muscle proteolysis seen during malignant tumor growth is mediated by the activation of the non-lysosomal adenosine triphosphate-dependent (ATP-dependent) ubiquitin proteasome pathway [31, 32]. In addition, inflammatory cytokines influence the expression of functionally relevant enzymes in cardiac cachexia [30]. It has been demonstrated that TNF-α, IFN-γ, and IL-1β are potent activators of inducible nitric oxide synthase (iNOS) expression [30], which in turn produces toxic levels of NO high enough to inhibit the key enzymes of oxidative phosphorylation [30]. It has also been shown in vitro that NO is able to impair the contractile performance of skeletal muscle [33].
More direct evidence of cytokine involvement comes from experiments in which specific neutralization of cytokines can relieve anorexia and cachexia in experimental animal models [18, 24, 25, 34]. Examples of antibodies that have been shown to successfully relieve anorexia and cachexia when administered include the anti-TNF-α, anti-IL-6, anti-IL-1, and anti-IFN-γ antibodies, although no single antibody has been proven to reverse all of the features of wasting seen in cancer cachexia [24]. These studies revealed that cachexia can rarely be attributed to any one cytokine but rather is associated with a set of cytokines and other cachectic factors that work in concert [5]. Recent studies include the use of anti-IL-6 humanized monoclonal antibody, which appears to inhibit cancer cachexia in murine models [35] and may be of clinical significance in cancer patients [35].
The problem with ascribing specific tissue responses to individual cytokines is that considerable overlap and redundancy exists in the cytokine network [14–17, 21]. Administration of either TNF-α or IL-1 will induce the synthesis of a variety of other proinflammatory cytokines such as IL-6 [5]. Thus, studies that use pharmacological administration of recombinant cytokines may not discriminate between biological responses induced directly by the administered cytokine and those induced secondarily by other stimulated cytokines [5]. Systemic disease such as cancer and inflammation may elicit a cytokine cascade in which several cytokines are induced simultaneously [21].
Systemic changes in response to inflammation are denoted the acute phase response [36]. Up to 50 % of patients with solid epithelial cancers may have an elevated APPR [37]. APPR is correlated with elevated resting energy expenditure and reduced energy intake [38]. Other longitudinal studies have found a poorer prognosis in patients displaying this response, independent of weight loss [39].
C-reactive protein
C-reactive protein (CRP) is the most common method used to assess the magnitude of the systemic inflammatory response [36]. The modified Glasgow prognostic score combines CRP and plasma albumin concentrations to create a simple scoring system that serves as a prognostic factor that is independent of stage and treatment and that predicts survival [40, 41] (Table 1).
Table 1.
Modified Glasgow Prognostic Score (mGPS): an inflammation-based prognostic score
| Biochemical measure | Score |
|---|---|
| C-reactive protein ≤10 mg/L + albumin ≥35 g/L | 0 |
| C-reactive protein ≤10 mg/L + albumin <35 g/L | 0 |
| C-reactive protein >10 mg/L | 1 |
| C-reactive protein >10 mg/L + albumin <35 g/L | 2 |
Source: [41]
Raised CRP concentrations at the time of admission to hospital is indicative of an increased risk for all-cause mortality; there is a 22.8-fold increase in cancer mortality in patients with highly elevated CRP concentrations (>80 mg/L) [42]. It has been shown that patients with inoperable non-small cell lung cancer had at least 5 % weight loss and almost 80 % an elevated CRP levels [43]. In patients without weight loss, those who displayed evidence of a systemic inflammatory response reported more fatigue (P < 0.05) [43]. In another study of patients with gastroesophageal cancer, the rate of weight loss was also correlated with elevated CRP serum concentrations [44].
Negative nitrogen balance
In adults, muscle mass remains fairly constant in the absence of stimuli (e.g., exercise) and thus protein synthesis and degradation generally remain in balance [45]. However, in cachexia, muscle atrophy occurs, which results from a decrease in protein synthesis, an increase in protein degradation, or a combination of both [45]. In recent years, it has become evident that specific regulating molecules are upregulated (e.g., members of the ubiquitin–proteasome system, myostatin, and apoptosis inducing factors), whereas other factors (e.g., insulin-like growth factor 1) are down-regulated in cachexia muscle wasting [30]. A major barrier to the effective management of skeletal muscle wasting is the inadequate understanding of its underlying biological mechanisms [30]. The most evident metabolic explanation for muscle decline is an imbalance between protein catabolism and anabolism [30]. In addition to an increase in catabolism, a reduction in anabolism has been shown to occur in cancer cachexia [30]. Skeletal muscle wasting in cancer cachexia can be mediated by multiple factors derived from tumor and host cells [46].
At least four major proteolytic pathways (lysosomal, Ca2+-dependent, caspase-dependent, and ubiquitin–proteasome-dependent) operate in skeletal muscle and may be altered during muscle cachexia [30]. Aside from these four distinct pathways, the autophagic/lysosomal pathway must also be considered [30]. In this pathway, portions of the cytoplasm and cell organelles are sequestered into autophagosomes, which subsequently fuse with lysosomes, where the proteins are digested [47].
When dissecting the molecular regulation of the ubiquitin–proteasome-dependent system (UPS) and autophagy, it became evident that forkhead box O (FoxO) transcription factors play a central role [30]. FoxO transcription factors, which are normally phosphorylated and inactivated by phosphatidylinositol 3-kinase (PI3K)-Akt/PKB, translocate into the cell nucleus and induce the transcription of the skeletal muscle-specific E3 ubiquitin ligases, muscle RING-finger protein-1 (MuRF1), and atrogin-1/muscle atrophy F-box (MAFbx) [48], as well as autophagy-related genes such as LC3 and Bnip3 [49]. Upstream of PI3K-Akt, several factors including reactive oxygen species (ROS), TNF-α, tumor-released proteolysis-inducing factor (PIF), peroxisome proliferator-activated receptor gamma coactivator 1 alpha (PGC-1α), and IGF-1 have been shown to influence this regulatory system [48, 50–52]. In contrast, protein anabolic factors such as IGF-1 counteract muscle atrophy [30]. Aside from inhibiting autophagy and the UPS, IGF-1 activates protein synthesis via the Akt-mammalian target of rapamycin (mTOR)–p70 S6 kinase (p70S6K) signaling pathway [53, 54].
The UPS is a major intracellular system that regulates skeletal muscle wasting in response to tumor factors and inflammatory cytokines [46]. In cancer cachexia, the decrease in skeletal muscle protein synthesis is partly related to the increased serum levels of PIF [30]. Intravenous administration of PIF to normal mice produced a rapid decrease in body weight that was accompanied by increased mRNA levels of ubiquitin in the gastrocnemius muscle [51]. There were also increased protein levels of the 20 S proteasome core and the 19 S regulatory subunit, suggesting activation of the ATP–ubiquitin-dependent proteolytic pathway [30]. Recent evidence suggests that PIF decreases protein synthesis by inhibiting protein translation initiation through phosphorylation of the eukaryotic initiation factor 2 (eIF2-alpha) [55].
Myostatin
Myostatin is an extracellular cytokine that is mostly expressed in skeletal muscles and is known to play a crucial role in the negative regulation of muscle mass [56]. Upon binding to the activin type IIB receptor, myostatin can initiate several different signaling cascades, resulting in decreased muscle growth and differentiation [56]. Muscle size is regulated via a complex interplay of myostatin signaling with the IGF-1/PI3K/Akt pathway, which is responsible for increased protein synthesis in muscle [56]. Therefore, the regulation of muscle weight is a process in which myostatin plays a central role, but the mechanism of its action and the role of the signaling cascades involved are not fully understood [56]. Myostatin upregulation was observed in the pathogenesis of muscle wasting during cancer cachexia [56].
Data are available that demonstrate a beneficial effect of myostatin inhibition in cancer cachexia [57], but conflicting study results have also been reported [58]. With respect to apoptosis, several reports demonstrated an increase in apoptosis or apoptosis-related proteins in skeletal muscle after the induction of cachexia [30]. The skeletal muscle of cachectic tumor-bearing animals reveals the presence of DNA fragmentation, a hallmark of apoptosis [59]. In addition to DNA fragmentation, a significant up-regulation of caspase-1, -3, -6, -8, and -9 activity was also documented in the gastrocnemius muscles of tumor-bearing mice [60].
Insulin-like growth factor-1
One of the main positive regulators of muscle growth is IGF-1 [56]. Under normal conditions, IGF-1 signaling seems to be dominant and blocks the myostatin pathway [61]. However, an inhibition of IGF-1 can occur when myostatin is overexpressed [62, 63]. IGF-1 can prevent TGF-α family-mediated apoptosis [64], and it was shown that in the absence of IGF-1, the level of apoptosis in C2C12 cells treated with myostatin increased [56]. The mechanism by which IGF-1 regulates myostatin signaling includes the inhibition of transcription factors responsible for the induction of atrogenes via phosphorylation through the PI3K/Akt pathway [56]. Akt plays a significant role in different metabolic processes in the cell, particularly in the hypertrophic response to insulin and IGF-1 [65, 66]. Akt is the ‘crossing point’ between the IGF-1 and myostatin pathways [56]. It is likely that under conditions of muscle wasting, myostatin can reverse the Akt/mTOR pathway, which is normally responsible for protein synthesis, to inhibit protein synthesis via FoxO, GSK-3β, or other unknown patterns, leading to the loss of muscle mass [56] (Fig. 2).
Fig. 2.
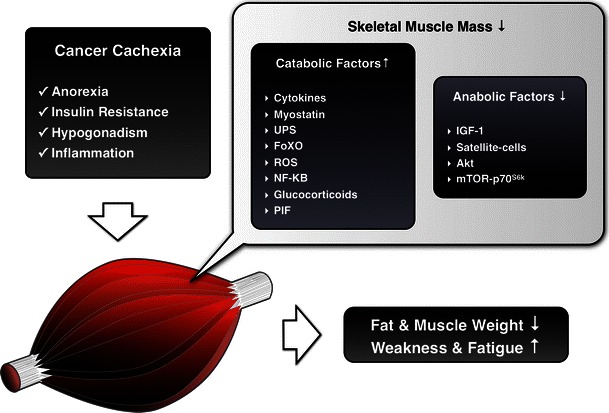
An abbreviated diagram of skeletal muscle in cancer cachexia. In adults, muscle mass remains fairly constant in the absence of stimuli (e.g., exercise) and thus protein synthesis and degradation generally remain in balance. However, in cachectic situation, the balance of skeletal muscle has been shifted towards protein breakdown, finally leading to the weight loss, weakness, and fatigue that characterize cancer cachexia. In recent years, it has become evident that catabolic factors are up-regulated (e.g., cytokines, myostatin and members of the ubiquitin–proteasome system), whereas anabolic factors (e.g., insulin-like growth factor 1) are down-regulated in cachexia muscle wasting. IGF-1 Insulin-like growth factor 1, FoxO forkhead box O, UPS ubiquitin–proteasome system, ROS reactive oxygen species, NF-κBPIF tumor-released proteolysis-inducing factor, mTOR mammalian target of rapamycin, p70S6K p70 S6 kinase
Another factor that may contribute to decreased anabolism is angiotensin II [30]. In an animal model of continuously administered angiotensin II, markedly reduced plasma IGF-1 levels occurred [67]. Compared with a sham treatment, angiotensin II-infused hypertensive rats lost 18–26 % of their body weight within a week, an effect that was completely reversed by losartan (an angiotensin II receptor type 1 receptor antagonist) [67].
Experimental data suggest that local IGF-1 may act as a regenerative agent, promoting the recruitment of stem cells to sites of muscle injury [68]. Because IGF-1 is reduced in experimental models of cachexia [69], it is reasonable to assume that under conditions of cachexia, the function of satellite cells is impaired [30].
Oxidative stress
There is a wealth of evidence suggesting that oxidative stress is associated with chronic diseases and it is assumed that an increase in ROS directs muscle cells into a catabolic state that leads to muscle wasting [30, 70, 71]. In cachexia, ROS are regarded as crucial players for muscle protein catabolism via their stimulation of the UPS [30]. Reaction products are measured as indirect markers of oxidative stress [30]. In cachexia, malondialdehyde (MDA) is regarded as one such indirect marker [30].
In addition, experimental cancer cachexia appears to be mediated by increased nitrosative stress secondary to increased nitric oxide formation. Indeed, protein tyrosine nitration is markedly increased in the muscles of tumor-bearing rats with advanced cachexia, due to lower levels of antioxidant enzymes [72, 73].
Anabolic hormones
There is a relative deficiency or resistance to anabolic hormones in cachectic states. Up to 50 % of men with metastatic cancer present with low concentrations of testosterone prior to chemotherapy [74]. A reduction in testosterone might lead to reduced bone mass, muscle strength, and sexual function in both men and women [75, 76]. Low concentrations of testosterone and other anabolic hormones are major contributors to cachexia-related wasting of skeletal muscle [77]. However, with respect to a correlation between body composition (including muscle mass) and the concentration of anabolic hormones, conflicting results have been reported in the current literature [30, 74, 78, 79].
Effects on antineoplastic therapy
Catabolic drivers
Antineoplastic therapies such as surgery, radiotherapy, and chemotherapy are known to have a negative impact on a patient’s nutritional intake through the development of systemic inflammation, exacerbation of already-reduced energy, and, particularly, on swallowing difficulties and anorexia due to nausea [22, 80]. Additionally, surgical patients may be fasted for prolonged periods perioperatively and both chemotherapy and radiotherapy can induce side-effects such as anorexia, nausea, vomiting, mucositis, taste change, or lethargy [80]. Consequently, antineoplastic therapies interfere with the maintenance of the nutritional state [81] (Tables 2, 3, 4).
Table 2.
Nutritional consequences of radical resection of alimentary tract organs
| Nutritional consequences | |
|---|---|
| Tongue or pharynx | Need for nutrition by tube (dysphagia) |
| Thoracic oesophagus | Gastric stasis (due to vagotomy), malabsorption of fats (due to vagotomy) |
| Stomach | Dumping syndrome, anaemia, malabsorption of fats, iron, calcium and vitamins |
| Duodenum | Biliary-pancreatic deficiency |
| Jejunum (up to 120 cm) | Reduced absorption of glucose, fats, protein, folic acid, vitamin B12, etc. |
| Ileum (60 cm) or ileocaecal valve | Malabsorption of vitamin B12, biliary salts and fats |
| Small intestine (75 %) | Malabsorption of fats, glucose, protein, folic acid, vitamin B12, etc., diarrhea |
| Jejunum and ileum | Complete malabsorption |
| Colon (subtotal or total resection) | Water and electrolyte loss |
| Pancreas | Malabsorption and diabetes |
| Liver | Transient hypoalbuminaemia |
Source: [81]
Table 3.
Nutritional complications associated with radiotherapy
| Region irradiated | Early effects | Late effects |
|---|---|---|
| Head and neck | Odynophagia, xerostomia, mucositis, anorexia, dysosmia, hypogeusia | Ulceration, xerostomia, dental caries, osteoradionecrosis, trismus, hypogeusia |
| Thorax | Dysphagia | Fibrosis, stenosis, fistula |
| Abdomen and pelvis | Anorexia, nausea, vomiting, diarrhea, acute enteritis, acute colitis | Ulceration, malabsorption, diarrhea, chronic enteritis, chronic colitis |
Source: [81]
Table 4.
Effects of chemotherapeutic drugs
| Drug | Severity and duration |
|---|---|
| Chemotherapeutic drugs commonly associated with severe nausea and vomiting | |
| Nitrogen mustard (mustine hydrochloride; mechlorethamine hydrochloride USP) | Occurs in virtually all patients. May be severe, but usually subsides within 24 h |
| Chloroethyl nitrosoureas, streptozotoci (streptozocin) | Variable, but may be severe. Occurs in nearly all patients. Tolerance improves with each successive dose given on a 5-day schedule |
| Cis-platinum (cisplatin) | May be very severe. Tolerance improves with intravenous hydration and continuous 5-day infusion. Nausea may persist for several days |
| Imidazole carboxamide (DTIC; dacarbazine) | Occurs in virtually all patients. Tolerance improves with each successive dose given on a 5-day schedule |
| Chemotherapeutic drugs commonly associated with mucositis | |
| Methotrexate | May be quite severe with prolonged infusions or if renal function is compromised. Severity is enhanced by irradiation. May be prevented with administration of adequate citrovorum rescue factor (folinic acid; leucovorin) |
| 5-Fluorouracil (fluorouracil USP) | Severity increase with higher doses, frequency of cycles, and arterial infusions |
| Actinomycin D (dactinomycin USP) | Very common; may prevent oral alimentation. Severity enhanced by irradiation |
| Adriamycin (doxorubicin) | May be severe and ulcerative. Increased in presence of liver disease. Severity enhanced by irradiation |
| Bleomycin | May be severe and ulcerative |
| Vinblastine | Frequently ulcerative |
Source: [81]
Symptoms will depend on the nature and course of the chemotherapeutic drugs being used and the location, volume, and dose of radiotherapy [80]. Some cytotoxic drugs may even generate their own cachexia-like side effects [82]. For example, treatment with antitubulin taxanes reduces body weight in tumor-bearing mice more than healthy mice, even when the agents significantly reduce tumor growth [82]. However, the complex relationship between cancer cachexia and the effects of antineoplastic drugs remains to be fully elucidated [82].
C-reactive protein
A key (but often variable) component of cachexia is hypercatabolism that is directly caused by tumor metabolism, systemic inflammation, or other tumor-mediated effects. The most widely accepted index of systemic inflammation is serum CRP [83]. CRP plasma values are positively correlated with weight loss, the occurence of cachexia, and recurrence in advanced cancer [84]. Its role as a predictor of survival has been shown in multiple myeloma, melanoma, lymphoma, ovarian, renal, pancreatic, and gastrointestinal tumors [84, 85].
Recent studies suggest that CRP is much more than a mere marker of the body’s inflammatory load [86, 87]. In cultured human umbilical vein endothelial cells, CRP was shown to activate endothelial cells, which, in turn, express Intracellular Adhesion Molecule-1 (ICAM-1) [86, 88]. CRP also induces other adhesion molecules in endothelial cells such as vascular-cell adhesion molecule-1 (VCAM-1) and E-selectin [86]. These molecules are involved in leukocyte-binding to the endothelial layer. CRP also activates the expression of monocyte chemotactic protein-1 (MCP-1) [87]. In addition, circulating factors, such as lipid-mobilising factors (LMF), and proteolysis-inducing factor (PIF) may play a role in the development of cancer anorexia and cachexia [88]. These are tumor-derived catabolic factors acting directly on adipose tissue and skeletal muscle, without affecting food intake [88].
However cachexia can exist without overt systemic inflammation, and thus indirect indices reflecting the catabolic drive such as responsiveness to chemotherapy and the rate of progression should also be assessed [83]. No consensus was reached about the usefulness of other factors contributing to catabolism [83]. These include insulin resistance, prolonged high-dose corticosteroid therapy, hypogonadism, and increased resting energy expenditure [83].
Increased nuclear factor-κB activity
Nuclear factor-κB (NF-κB), a nuclear transition activator factor, plays a major role in upregulating inflammatory gene expression, including expression of COX-2, nitric oxide synthase, TNF-α, IL-1, and IL-6 [89]. The proinflammatory response occurs particularly with the formation of p65–p50 dimers, which act as the central control to an inflammatory response. NF-κB is one of the principal transcription factors to transduce TNF-a signals into the cells. Moreover, it also activates gene transcription of cytokines, acute-phase response proteins, and cell adhesion molecules [90, 91].
Activation of NF-κB accelerates inflammation, increases cellular proliferation of tumors, and prevents apoptosis [90]. Inhibition of NF-κB therefore is both antineoplastic and can reduce cachexia. Inhibition of NF-κB also sensitizes tumors to chemotherapy and radiation, something that is the subject of multiple research trials [92].
In fact, genetic overexpression of IκB blocks NF-κB-dependent processes. Two studies have shown that glucocorticoid administration induces transcription of IκB gene [93, 94]. Increased levels of IκB gene trap NF-κB in inactive cytoplasmic complexes, hence inhibiting its ability to induce transcription of inflammatory cytokines. Moreover, fumar acid, which blocks the nuclear translocation of NF-κB, has a high anti-inflammatory capacity [93]. More recently, activation of NF-κB by overexpression of a IκB phosphorylating kinase has been shown sufficiently to block myogenesis, thus illustrating the link between NF-κB and cachexia development [94]. However, complete inhibition of NF-κB has proven detrimental; knockout studies targeting the major subunits of NF-κB show severe immunodeficiency in mice, which was lethal in some cases [95]. Resolution of inflammation also requires NF-κB expression and complete inhibition of NF-κB can lead to severe cellular apoptotic damage in critical illness [96].
Managing cancer cachexia
Treatment goals in current standard of care
The European Palliative Care Research Collaboration (EPCRC) has developed evidence-based recommendations for the classification and treatment of cachexia in advanced cancer patients [97]. These treatment guidelines focus on patients with advanced cancer that are likely to suffer from refractory cachexia. Many of these patients are receiving palliative care, and life expectancy often is short. Only little cachexia-specific research has been done on this patient group, and the EPCRC treatment guidelines had to consider whether research results taken from other disease stages could be applicable for patients with advanced and incurable disease with refractory cachexia [97].
Management of cachexia must take into account the patient’s prognosis [97], as it may take several weeks for patients to respond to anti-cachectic treatment [97]. For patients with a short life expectancy, treatment options for cachexia may add to the disease burden without offering adequate symptom relief and thus may not be appropriate [97]. Health care professionals should discuss all treatment options with the patient and ensure that they are well-informed about available treatments and expected treatment outcomes [97]. All patients should have equal access to appropriate assessment and management of cachexia, whether they are receiving home care, day care, or are hospital inpatients [97].
The best way to treat cancer cachexia is to cure the cancer, but unfortunately this remains an infrequent achievement among adults with advanced solid tumors [98, 99]. Therefore, the treatment goal for cachexia should be the reversal of the loss of body weight and muscle mass with a variety of pharmacological agents (Fig. 3) [99]. As a minimal goal, body weight should be maintained and further loss prevented [97]. The treatment approach should be multimodal and similar to treatment used in patients with pre-cachexia [97]. This includes detailed assessment and repeated monitoring, vigorous nutritional support, anti-inflammatory treatment, treatment of secondary gastrointestinal symptoms and other causes for decreased oral nutritional intake as well as evaluation of anti-neoplastic options to reduce the catabolic drive of the cancer [97]. However, for refractory cachexia, the primary treatment goal should not be reversal of weight loss, but the alleviation of cachexia-related symptoms and an overall increase of well-being [97].
Fig. 3.
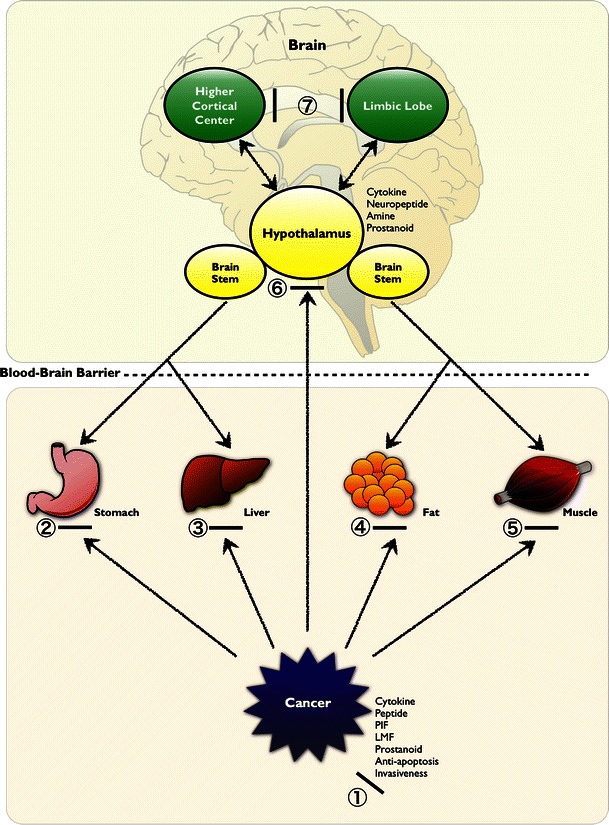
The potential modalities of pharmacological intervention of cancer anorexia-cachexia syndrome. Agents were classified as those established (first-line) or those unproven/investigational (second-line), depending on their site or mechanism of actions. ①, inhibitors of production/release of cytokines and other factors; ②, gastroprokinetic agents with or without antinausea effect; ③, blockers of Cori cycle; ④ ⑤, blockers of fat and muscle tissue wasting; ⑥, appetite stimulants with or without antinausea effect; and ⑦, anti-anxiety/depressant drugs. These agents should be selected on an individual basis according to the cause of cachexia or the state of the patient. *The precise actions of statins on skeletal muscle still remain controversial. First-line treatments: glucocorticoids ① ⑥, progesterones ① ⑥. Second-line treatments: cannabinoids ⑥, cyproheptadine ⑥, branched-chain amino acids ⑤ ⑥, metoclopramide ② ⑥, eicosapentanoic acid ① ④ ⑤, 5′-deoxy-5-fluorouridine ①, melatonin ①, thalidomide ①, β2-adrenoceptor agonists ⑤, non-steroidal anti-inflammatory drugs ① ⑥, others anabolic steroids ⑤, pentoxifylline ①, hydrazine sulfate ③, statin ① ⑤*, angiotensin-converting-enzyme inhibitor inhibitor ⑤, selective androgen receptor modulator ⑤. Source: [99] with modification
Pharmacological treatments
Appetite stimulants
Reversing the effects of cancer cachexia does not appear to be influenced by stimulating the appetite [100]. Thus, the decision to use an orexigenic drug should be based on tolerance of the side effects, cost effectiveness, and treatment burden [100]. Current studies are investigating an approach of drug combinations to reverse cancer cachexia [101, 102]. A recent study with 332 patients comparing medroxyprogesterone, megestrol acetate, oral supplementation with eicosapentaenoic acid, l-carnitine, and thalidomide found that the combination therapy was superior to any of the other treatment arms with single drug treatment [102]. Combination therapy led to increased lean body mass, decreased resting energy expenditure, and improved appetite [102]. Until an effective intervention for reversing cancer cachexia is developed, early intervention with nutritional support and prevention of treatment-related morbidities (e.g., nausea, vomiting, diarrhea, dysphagia, pain, or depression) is advised [102, 103].
Progestational drugs, cannabinoids, and cyproheptadine are used in the clinic as appetite stimulatus in the therapy of the cancer-induced anorexia and cachexia syndrome [99]. These drugs have been shown to be partially effective in reversing or maintaining the symptom of body weight loss in patients with chronic illness [99].
Cannabinoids are highly liquid-soluble substances with delta-9-tetrahydrocannabinol (THC) as an active ingredient that work synergistically, additively, or even antagonistically when ingested together (e.g., by smoking marijuana). Appetite stimulation and body weight gain are well-recognized effects of using marijuana and its derivatives [99]. This may have significant implications for the clinical usefulness of marijuana or its individual compounds in treating cachexia.
Dronabinol is the synthetic oral form of THC, which is the active ingredient responsible for the appetite-stimulating effect [99, 104–106]. Dronabinol and marinol (in the United States) and nabilone (in Canada) have been used as antiemetics in cancer, with many studies demonstrating their efficiency in treating chemotherapy-induced nausea and vomiting [99]. Several studies of THC in advanced cancer-associated anorexia have shown some improvement in mood and appetite, with either no or some improvement in body weight [107, 108]. However, randomized, controlled trials are needed to better determine the efficacy and usefulness of THC in cancer cachexia.
The effects of cannabinoids are mediated via specific receptors. Two types of cannabinoid receptors, CB1 and CB2 have been detected. However, the precise mechanism by which cannabinoids exert their effect has yet to be clarified. It has been shown that almost 20 percent of the cancer patients receiving chemotherapy along with dronabinol as an antiemetic experienced side effects, such as euphoria, dizziness, somnolence, and confusion resulting in a dose reduction or less frequently in withdrawal of the treatment [106]. It has been suggested that the drug could be taken at bedtime to avoid some psychotomimetic effects and that it might produce long-lasting appetite stimulation for 24-h period following ingestion [104].
Cyproheptadine is an antiserotoninergic drug with antihistaminic properties that has been shown to have a slight appetite-stimulant effect in a number of human conditions [109]. A randomized, controlled trial found mild appetite stimulation in patients with advanced cancer, although it did not prevent progressive weight loss [110]. Considerable evidence, both in humans and experimental animals, suggests that anorexia may be mediated by increased serotonergic activity in the brain. Its blockade, therefore, might be beneficial in reducing symptoms [111, 112]. Cyproheptadine also appeared to stimulate appetite and decrease diarrhea in patients with advanced carcinoid tumors [113]. Studies on the effects of cyproheptadine in progressive weight loss in patients with cancer or other causes of cachexia suggest that cyproheptadine has a beneficial effect on appetite stimulation but only slight effects on weight gain [110, 114, 115]. 5-hytroxytryptamine type 3 (5HT3) receptor antagonists, such as ondansetron and granisetron, have entered widespread clinical use as antiemetics for cancer chemotherapy [99].
Progestins
Megestrol acetate (MA) and medroxyprogesterone acetate (MPA) are synthetic, orally active progestational agents. In several randomized controlled studies, these compounds have been found to improve appetite, caloric intake, and nutritional status in patients with non-hormone responsive tumors and cancer anorexia-cachexia syndrome [104–106, 116–122].
MA has demonstrated a dose-related beneficial effect, in a dose range from 160 mg to 1600 mg/day on appetite, caloric intake, body weight gain (mainly fat), and sensation of well-being (with an optimal dosage of 800 mg daily) [118]. Increasing MA dosages from 160 mg to 800 mg/day improves response to a level beyond which no further improvement occurs [118]. It is recommended that a patient is started on the lowest dosage (i.e, 160 mg/day) and that the dose is uptitrated according to clinical response [105, 109].
MPA has similarly been shown to increase appetite and food intake with a stabilization of body weight at a dose of 1000 mg (i.e., 500 mg twice daily) [109]. Although the drug is safe at doses of 500–4000 mg daily, side effects have been shown to increase above oral doses of 1000 mg [104]. At present, there is considerable evidence for the effect of synthetic progestins on appetite and body weight in patients with cancer anorexia and cachexia [123]. However, further issues regarding the optimal treatment duration, the best time to start treatment during the natural history of the disease, and the eventual impact on the overall quality of life need to be clarified [123]. Moreover, optimal dose regimens for MA in different indications, such as appetite improvement, patients’ sense of well-being, weight gain, are still to be identified.
The following adverse events have been reported with MPA: thromboembolic phenomena, breakthrough uterine bleeding, peripheral edema, hyperglycemia, hypertension, adrenal suppression, and adrenal insufficiency if the drug is abruptly discontinued [104–106, 116–120, 124]. Although patients rarely need to stop taking these drugs because of adverse effects, these drugs should not be prescribed in cases of thromboembolic/thrombotic disease, heart disease, or for patients at risk for serious fluid retention [104].
Although the mechanism of weight gain of progestational drugs in presently uncertain, it might be related to glucocorticoid activity [105]. MA may induce appetite via stimulation of NPY, a potent central appetite stimulant in the hypothalamus, modulation of calcium channels in the ventromedial hypothalamus (VMH)—a well known satiety center [1, 4, 125–133] which reduces the firing tone of VMH neurons. On the other hand, MPA has been shown to inhibit the activity of proinflammatory cytokines such as IL-1, IL-6, and TNF-α [28, 109, 134]. Serum levels of such cytokines were reported to be decreased in cancer patients after MA or MPA treatment [109]. More studies are needed to finally clarify the pharmacologic effects of MA and MPA drugs and to confirm the anti-inflammatory effects.
Several other drugs have been evaluated as agents to ameliorate cancer anorexia-cachexia. Corticosteroids are frequently used in clinical practice for appetite stimulation in patients with advanced malignancies and randomized clinical trials showed that corticosteroid medications may stimulate appetites in patients with advanced cancer [135]. However, these studies were not able to show any substantial non-fluid weight gain in treated patients [135]. Efforts are also ongoing to evaluate both anabolic steroids and hydrazine sulfate as drugs for the treatment of patients with cancer cachexia [135].
Hydrazine is a substance that inhibits the enzyme phosphoenol pyruvate carboxykinase (PEP-CK) and interferes with gluconeogenesis [135]. However, hydrazine and hydrazine sulfate might be a human carcinogen based on evidence for carcinogenicity in animal studies [135, 136]. The preliminary nature of these investigations, however, precludes recommendations for the use of these drugs in routine clinical practice [135].
Other orexigenic agents
The orexigenic mediator ghrelin has been reported as having a key role in increasing appetite and, therefore, food intake. Ghrelin is an endogenous ligand for the growth hormone secretagogue receptors [137, 138]. It is synthesized principally in the stomach and is released in response to fasting [138].
Ghrelin strongly stimulates GH secretion in humans [139–142] and does so more potently than GHRH by several fold under similar circumstances [143]. Furthermore, ghrelin and GHRH synergistically increases GH release [141]. GH regulates IGF-1 levels and increases muscle strength [144, 145], whereas GH enhances lipolysis, IGF-1 stimulates protein synthesis, myoblast differentiation, and muscle growth [143]. Evidence that ghrelin exerts anti-inflammatory actions has been accumulating [143]. Ghrelin induces the anti-inflammatory cytokine IL-10 [146, 147], suppressing the production of proinflammatory cytokines, including IL-1β, IL-6, and TNF-α both in vitro [148, 149], and in vivo [146, 150, 151]. Additionally, ghrelin inhibits the activation of NF-κB, which controls the production of multiple proinflammatory cytokines during inflammatory insults [147, 149, 150]. Although the molecular mechanisms and cellular targets mediating ghrelin inhibition of NF-κB activation remain to be determined, the vagus nerve may play an important role in the ghrelin-mediated inhibition of proinflammatory cytokine release [150, 152]. MuRF1 and MAFbx are upregulated under cachectic catabolic conditions, and NF-κB activation may regulate skeletal muscle proteasome expression and protein degradation [143]. The elevations in MuRF1 and MAFbx expression seen in skeletal muscle after thermal injury, arthritis, and dexamethasone administration were normalized, attenuated, and prevented, respectively, by ghrelin or GHS administration [153–156]. IGF-1 prevents the expression of MuRF1 and MAFbx by inhibiting FoxO transcription factors via stimulation of the PI3K/Akt pathway [143]. The IGF-1 receptor triggers activation of several intracellular kinases, including PI3K [156]. Thus, the effects of ghrelin on NF-κB activation and IGF-1 synthesis are favorable for minimizing inflammatory responses and skeletal muscle wasting in patients with cachexia [143].
In addition to increasing food intake, an experimental study has shown that repeated administration of ghrelin improves cardiac structure and function, and attenuates the development of cardiac cachexia in chronic heart failure (CHF). These results suggest that ghrelin has cardiovascular effects and regulates energy metabolism through growth hormone-dependent and -independent mechanisms [157]. Thus, administration of ghrelin may be a new therapeutic strategy for the treatment of severe CHF [157].
At present, a phase II randomized, placebo-controlled, double-blind study, using an oral ghrelin mimetic, demonstrated an improvement in lean body mass, total body mass and hand grip strength in cachectic cancer patients [158]. Several clinical trials with ghrelin are currently on going.
Herbal medicine; translational aspects, particularly for cancer cachexia
There have been a number of published cases of cancer patients treated with Kampo, a form of Japanese traditional herbal medical practice, who reportedly experienced significant clinical benefits [159]. As an example, rikkunshito, a Kampo formula, has been shown to be useful in clinical practice for cachectic cancer patients.
Rikkunshito has been used to treat gastrointestinal tract disorders such as functional dyspepsia [160–164] and gastroesophageal reflux [165]. A recent study regarding the underlying mechanisms of rikkunshito has shown that rikkunshito and its component 10-gingerol may inhibit the degradation of acyl-ghrelin by inhibiting the circulating ghrelin degrading enzyme [166]. Another study has shown that administration of rikkunshito reversed the decrease in hypothalamic ghrelin secretion and food intake 24 h after cisplatin treatment [6]. A most recent study showed that rikkunshito improved anorexia, gastrointestinal dysmotility, muscle wasting, and anxiety-related behavior [10]. In this study, rikkunshito in tumor-bearing rats was effective not only against anorexia–cachexia, but also for promoting survival, particularly in combination with chemotherapy [10]. Moreover, median survival of pancreatic cancer patients with ascites who were treated with gemcitabine was significantly prolonged by administration of rikkunshito [10]. Active components of rikkunshito, hesperidin and atractylodin, potentiated ghrelin secretion and receptor signaling, respectively, and atractylodin prolonged survival in tumor-bearing rats [10]. The physiological functions of endogenous ghrelin are enhanced by the dual actions of rikkunshito; which involve the stimulation of ghrelin secretion and the activation of GHS-R activity, possibly due to allosteric changes in the receptor [10]. These studies suggest that rikkunshito may be useful in clinical practice for cachectic cancer patients.
Because Japanese Kampo has long been used, the potential risks and benefits of its use are well recognized despite the relative paucity of the mechanistic insights [159]. Unconventional therapies such as herbs and minerals that have been used in ancient medical traditions have led to the identification of active anticancer agents [159]. Although the working mechanisms of some of the herbs and minerals are unclear and remain to be elucidated, they are worth further studying as newly potential therapy agents for cancer treatment [167].
Non pharmacological treatments
Diet modification
Because cancer cachexia differs from starvation, to date, single modality therapies with traditional nutritional regimens have failed to demonstrate efficacy in improving weight gain, including a gain in lean body mass, in patients diagnosed with cancer cachexia [168]. The average caloric deficit in weight-losing patients with cancer cachexia is approximately 250–400 kcals/day [168]. An average supplementation of 1 calorie/mL has not been shown to improve the nutritional status of patients receiving chemotherapy [169, 170]. However, recent studies using a more calorie- protein-dense supplementation have suggested that weight stabilization can be achieved; however, improvements in lean body mass has not yet been observed [171].
Patients with cancer cachexia undergoing aggressive re-feeding are at risk for ‘re-feeding syndrome’ during the first 2–3 weeks of treatment [172]. This potentially lethal condition is characterized by severe electrolyte and fluid shifts due to metabolic abnormalities and bears a significant risk for morbidity and mortality [172]. The clinical features include fluid-balance disturbances, abnormal glucose metabolism, hypophosphatemia, hypomagnesiemia, and hypokalemia [173].
Before starting the re-feeding process, electrolyte disorders should be corrected and circulatory volume should be carefully restored. This may delay the administration of complete nutrition but is usually accomplished within 12–24 h. Caloric repletion should be at a slow rate of approximately 20 kcal/kg per day (or 1000 kcal per day) initially. However this rate may not meet the patients’ fluid, sodium, potassium, protein, or vitamin requirements unless these are specifically addressed.
Gradual introduction of calories, particularly over the first week of re-feeding, should be prudent until the patient is metabolically stable [174]. Hypophosphatemia has to be treated if the serum level is less than 0.30 mmol/l or the patient is symptomatic. Supplementation of phosphate should be given intravenously at 40–80 mmol/day, together with magnesium (8–16 mmol/day) and potassium (80–120 mmol per day). These dosages should be adjusted according to monitored serum levels [175].
Exercise
Physical exercise may be beneficial in the treatment of cancer cachexia, as it increases insulin sensitivity, protein synthesis rate, and anti-oxidative enzyme activity [97]. It also may lead to a suppression of the inflammatory response and an enhancement of immune function [176]. All of these mechanisms can help to curb the pathophysiological changes underlying cachexia.
There is significant evidence that endurance exercise (e.g., high number of repetitions performed over extended time periods against relatively low resistance) ameliorates cancer-related fatigue [177]. By contrast, resistance exercise (lower number of repetitions against higher resistance) attenuates muscle wasting in different catabolic conditions [97]. Physical therapy is also advised during periods of bed rest, as reduced fitness, strength, and loss of lean body mass may occur [178]. Physical therapy can help to counteract fatigue and depression, as well as maintain strength and range of motion [97].
Although it is increasingly recognized that exercise training seems to be a polypill against the dramatic changes in the skeletal muscle in cachexia, scientific proof is scarce [97]. As a matter of fact, there are only very few clinical trials investigating the impact of exercise training in cachexia [97]. A few small studies have shown that exercise training leads to changes in body composition [97]. Investigations with larger cohorts and hard end points are still missing [97]. Most of the research concerning exercise training and cachexia has been done in the field of cancer cachexia, preferably with animal models [97]. It is still under discussion as to which patients with refractory cachexia might profit from mild physical activity intervention [97]. Counseling patients on cancer-related fatigue can encourage patients to maintain a minimal form of activity and slow down the decrease in physical function and quality of life [97].
Nutritional counseling
The management of cachexia in advanced cancer patients should focus on maximizing oral intake by allowing the patient flexibility in type, quantity, and timing of meals [99]. Nutritional counseling has been reported to improve nutritional intake in patients undergoing chemotherapy [179]. Moreover, it has also been shown to improve quality of life in patients undergoing radiotherapy [180]. However, the influence of counseling on reducing psychological distress in patients with a palliative care setting remains to be established [97].
Adequate education and counseling should also address the concerns of family members who may worry that their relative appears to be ‘starving to death’ by underscoring the differences between starvation and cachexia [97]. The appropriate provision of counseling, for example dietetic consultation or information sheet has not been established for patients with refractory cachexia [97]. Professional health care teams of oncology physicians, nurses, and dietitians can diagnose specific needs and plan individualized treatment for improved nutritional health with patients and their families [97]. Counseling, which any member of the health care team may provide, is an effective and inexpensive intervention and should be combined with other nutritional interventions [181]. Nursing interventions to counteract cachexia should be aimed at minimizing the negative factors of nausea, vomiting, diarrhea, pain, fatigue, changes in taste or food preferences that may influence appetite [99].
Even if there is no evidence that nutritional counseling improves overall quality of life or physical functioning in patients with refractory cancer cachexia, there is a strong support by experts that nutritional counseling can aid cancer patients and family members to understand the changes, and to differentiate what they can improve and where the limitations of nutrition [97, 181]. However this requires advanced psychological and nutritional knowledge on the part of the counselors [97].
Palliative care and mental health support
The health care team should ensure that patients’ physical symptoms (e.g., pain, fatigue, breathlessness) are being assessed and managed effectively, as this may improve appetite, ability to take up food, and general well-being [97]. Psychological distress and psychiatric disorders are common among patients with cancer and have a prevalence ranging from 10 to 79 % [99]. These problems are also as common among the family members of people with cancer [99]. Anorexia and cachexia may result in secondary depression, or depression itself may be a prime contributor to anorexia and subsequent weight loss. Benzodiazepines can be helpful for persistent fear and anxiety, and antidepressant drugs are increasingly used in patients with cancer with comorbid depression [99].
The use of psychological and behavioral interventions (e.g., relaxation, hypnosis, and short-term group psychotherapy) in cancer is increasing and recent studies have suggested that some of these techniques may affect quality of life and, perhaps, survival rates [99]. However, there is no evidence that psychotherapeutic interventions have an effect on nutritional status [97]. Moreover, for refractory cachexia, reduced performance status and short prognosis may preclude this intervention [97].
Caring for a person with advanced disease can be physically and emotionally stressful [97]. Caregivers often note that when friction occurs between themselves and the individual for whom they are caring, it often occurs over the issue of eating [99]. These caregivers report that they find it hard to cope with the patient who relentlessly loses weight and strength and yet persistently refuses adequate food intake [99]. Effective communication with patients and their families is essential and is an important component of treatment [99].
Managing side effects
Many cancer interventions will exacerbate already reduced energy and nutrient intake [80]. Surgical patients may be fasted for prolonged periods peri-operatively, and both chemotherapy and radiotherapy can induce side-effects such as anorexia, nausea, vomiting, mucositis, taste change, or lethargy [80]. Symptoms will depend on the nature and course of the chemotherapeutic drugs being used and the location, volume, and dose of radiotherapy [80]. Some cytotoxic drugs may even generate their own cachexia-like side-effects [82]. For example, antitubulin taxanes induce greater loss of body weight in tumor-bearing mice than in healthy mice, even when the agents significantly reduce tumor growth [80]. The complex interaction between nutrition, cachexia, and chemotherapy still requires elucidation [80, 182, 183].
Adverse Effects of Chemotherapy and Radiation
Although chemotherapy and radiation treatments are usually directed by a subspecialist, the physician must be aware of potential adverse effects and, in some practice settings, may be called on to manage them [184].
Approximately 70–80 % of patients treated with chemotherapy experience nausea and vomiting [185], which may be acute (occurring within a few hours after chemotherapy), delayed (occurring 24 or more hours after chemotherapy), breakthrough or refractory (occurring despite prophylactic treatment), or anticipatory (occurring before chemotherapy treatment). The emetogenic (vomit-inducing) potential of chemotherapeutic agents varies from mild to severe [186]. Drug dose, schedule and route of administration, and patient variability are also factors [184].
Antiemetic therapy is most effective if given before chemotherapy and maintained while the emetic potential of the agent continues. Oral formulations are as effective as parenteral or rectal routes if the patient is able to swallow and digest tablets. Lorazepam, metoclopramide, and prochlorperazine often are used for moderate- to low emetic-risk chemotherapy and for breakthrough nausea.
Currently, 5-HT antagonists (ondansetron, granisetron, dolasetron and palonosetron) are most widely used in practice for patients given chemotherapy with a moderate-to-high risk of gastrointestinal side effects. Trials with these agents indicate that they are highly effective in controlling acute nausea and vomiting associated with chemotherapy and have minimal adverse effects [187–189]. They are equally effective for acute nausea [190], but palonosetron, which has a much higher affinity for the 5-HT receptor and a longer half-life than the other 5-HT antagonists, is more effective than dolasetron in preventing delayed emesis [191]. The co-administration of dexamethasone improves the effectiveness of 5-HT antagonists in controlling acute emesis. However, one study found that adding a 5-HT antagonist to dexamethasone for the treatment of delayed nausea and vomiting did not result in an improved antiemetic effect over dexamethasone alone [184, 192]. Aprepitant, the first neurokinin-1 receptor antagonist, augments the activity of 5-HT antagonists and dexamethasone to inhibit acute and delayed emesis induced by cisplatin [184, 193, 194].
Nausea and vomiting can also occur following radiation treatment and are most likely in patients undergoing whole body or upper abdominal radiation [184]. Higher total dose of radiation, larger amount of tissue radiated, and a higher daily fraction of radiation are also factors in the severity of nausea and vomiting [184].
Fever and neutropenia in a patient undergoing chemotherapy are also common and should be treated promptly [184]. Fever in a patient undergoing chemotherapy is common and worrisome [184]. In the guidelines developed by the Infectious Diseases Society of America (IDSA) [195], fever is defined as a single oral temperature higher than 100.9 °F (38.3 °C) or an oral temperature of 100.4 °F (38.0 °C) or higher for more than 1 h.
An absolute neutrophil count less than 500 per mm3 (0.5 × 109 per L) is defined as severe neutropenia. The severity of infection is inversely related to the neutrophil count, with the greatest risk of bacteremia at absolute neutrophil levels lower than 100 per mm3 (0.1 × 109 per L) [196]. Evaluation of the patient with neutropenia includes physical examination (with attention to indwelling vascular access devices), laboratory data, radiographs, and blood and urine cultures.
No single antibiotic or antibiotic combination can be uniformly recommended for all febrile neutropenic patients [184]. Initial therapy is selected after considering the most likely potential infecting organism, site of infection, organ function (e.g., kidney, liver), medication allergies, and recent antibiotic treatment [184].
The most widely used outpatient antibiotic choice is an oral fluoroquinolone or amoxicillin/clavulanate [184]. Commonly used empiric intravenous antibiotic monotherapies include carbapenems (e.g., imipenem/cilastatin, meropenem), and extended-spectrum antipseudomonal cephalosporins (e.g., ceftazidime, cefepime). Dual therapy agents include an aminoglycoside with antipseudomonal penicillin (with or without a betalactamase inhibitor) or an extended-spectrum antipseudomonal cephalosporin; and ciprofloxacin with antipseudomonal penicillin [184].
According to IDSA and National Comprehensive Cancer Network guidelines, diagnostic reassessment should occur if fever does not improve in 3–4 days [195]. Although most patients with cancer-related febrile neutropenia will recover without major complications, involvement of a subspecialist should be considered when the patient’s fever does not improve after 3 or 4 days of appropriate antimicrobial treatment or when the patient has septic shock, methicillin-resistant Staphylococcus aureus infection, or signs and symptoms of invasive fungal infection [184].
Cancer cachexia in special populations
Elderly
The management of cancer in the older person is an increasingly common problem, as 60 % of all neoplasms occur in individuals age 65 and older [197]. Cachexia is one of the major causes of weight loss in the elderly and numerous studies have shown that weight loss is associated with an increase in mortality [198–201]. Although body weight is easily measured, the evaluation of unintended weight loss in long-term care facilities is difficult [202]. Whether anorexia and weight loss are reversible or unavoidable requires a careful clinical evaluation in the individual patient [203]. A structured approach to the differential diagnosis of malnutrition in long-term care was developed by the Council for Nutritional Clinical Strategies in Long- Term Care [203].
Additionally, muscle mass loss is characteristic of physical frailty and sarcopenia (age-related loss of muscle mass). Physical frailty has been characterized as a condition that results from reduced strength, reduced gait velocity, reduced physical activity, weight loss, and exhaustion. Thus, sarcopenia and frailty could be classified as cachectic conditions because they are associated with muscle mass loss.
Treating weight loss in the elderly can ameliorate many medical conditions. For example, rehabilitation time following post-hip fractures has been shown to decrease with nutritional supplementation [204]. In hospitalised geriatric patients, nutritional supplementation resulted in improvement in serum protein and, nutritional status, and decreased mortality [205]. In a subset of geriatric inpatients, low serum albumin with weight loss predicts those patients at highest risk for dying during the subsequent 2 years [206].
Moreover, in elderly patients with cachexia, medical, cognitive, and psychiatric disorders may diminish self-sufficiency in activities of daily living (e.g., grooming, ambulation), thus reducing health-related quality of life and increasing the frequency of secondary procedures, hospitalizations, and need for skilled nursing care [198, 199]. Increased understanding of the pathophysiology of geriatric cachexia in geriatric patients has resulted in effective and safe nutritional measures [206]. In particular, a better understanding of the role of proinflammatory cytokines (e.g., increased levels of negative regulatory cytokines) in cancer cachexia in the elderly may lead to pharmacological treatment targeted for this population [207].
The potential involvement of IL-6, TNF-α, IL-1, serotonin, PGE2 and other cytokines (e.g., IL-10, IL-4, IL-15) in the pathophysiology of aging, chronic diseases, and wasting calls for additional research on ways to suppress the secretion, dysregulation, or downstream effects of the pharmacotherapy for the treatment of cachexia in elderly [207]. Further investigation with specific nutritional manipulations, and the administration of specific steroids, neuropeptides, and peptide hormones is necessary [207].
Children
Anorexia and cachexia is commonly seen in pediatric patients that receive cancer treatment. The most prominent clinical feature of cachexia in children is growth failure [97], and weight loss or decreased growth are valuable indicators of malnutrition [208]. Growth is important for children because it is an essential feature of their health [208, 209]. However, criteria for weight loss or decreased growth have seldom been used in the assessment of nutritional status in children with cancer [208]. To date, weight loss is mainly described in the literature concerning failure to thrive [210, 211], but not for describing malnutrition [208].
Children appear to be at greater nutritional risk than adults because of high protein and energy requirements and limited caloric reserves [212]. Malnutrition is associated with an increased rate of infection in children with malignant neoplasms [212].
Given the increasing attention to evidence suggesting the negative impact of cachexia on the quality of life of children with cancer, it is necessary to develop a scale that targets the concerns of pediatric patients with cancer that is specific to anorexia and cachexia [212]. An appropriate scale must have sound psychometric properties, be user friendly, and monitor cachexia-related effects on quality of life over time [212].
Conflict of interests
The authors of this manuscript have no conflict of interests to declare.
References
- 1.Friedman JM, Halaas JL. Leptin and the regulation of body weight in mammals. Nature. 1998;395(6704):763–770. doi: 10.1038/27376. [DOI] [PubMed] [Google Scholar]
- 2.Flier JS, Maratos-Flier E. Obesity and the hypothalamus: novel peptides for new pathways. Cell. 1998;92(4):437–440. doi: 10.1016/S0092-8674(00)80937-X. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz MW, Figlewicz DP, Baskin DG, Woods SC, Porte D. Insulin in the brain: a hormonal regulator of energy balance. Endocr Rev. 1992;13(3):387–414. doi: 10.1210/edrv-13-3-387. [DOI] [PubMed] [Google Scholar]
- 4.Inui A. Feeding and body-weight regulation by hypothalamic neuropeptides—mediation of the actions of leptin. Trends Neurosci. 1999;22(2):62–67. doi: 10.1016/S0166-2236(98)01292-2. [DOI] [PubMed] [Google Scholar]
- 5.Inui A. Cancer anorexia-cachexia syndrome: are neuropeptides the key? Cancer Res. 1999;59(18):4493–4501. [PubMed] [Google Scholar]
- 6.Yakabi K, Sadakane C, Noguchi M, Ohno S, Ro S, Chinen K, et al. Reduced ghrelin secretion in the hypothalamus of rats due to cisplatin-induced anorexia. Endocrinology [Internet]. 2010;151(8):3773–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20534732. [DOI] [PubMed]
- 7.Liu Y, Hamaue N, Endo T, Hirafuji M, Minami M. 5-hydroxytryptamine (5-HT) concentrations in the hippocampus, the hypothalamus and the medulla oblongata related to cisplatin-induced pica of rats. Res Commun Mol Pathol Pharmacol. 2003;113–114:97–113. [PubMed] [Google Scholar]
- 8.De Vry J, Schreiber R. Effects of selected serotonin 5-HT1 and 5-HT2 receptor agonists on feeding behavior: possible mechanisms of action. Neuroscience & Biobehavioral Reviews [Internet]. 2000;24(3):341–53. Available from: http://www.sciencedirect.com/science/article/pii/S0149763499000834. [DOI] [PubMed]
- 9.Schreiber R, Selbach K, Asmussen M, Hesse D, De Vry J. Effects of serotonin(1/2) receptor agonists on dark-phase food and water intake in rats. Pharmacol Biochem Behav. 2000;67(2):291–305. doi: 10.1016/S0091-3057(00)00357-9. [DOI] [PubMed] [Google Scholar]
- 10.Fujitsuka N, Asakawa A, Uezono Y, Minami K, Yamaguchi T, Niijima A, et al. Potentiation of ghrelin signaling attenuates cancer anorexia–cachexia and prolongs survival. Transl Psychiatry. 2011;1(7):e23. [DOI] [PMC free article] [PubMed]
- 11.Takeda H, Sadakane C, Hattori T, Katsurada T, Ohkawara T, Nagai K, et al. Rikkunshito, an herbal medicine, suppresses cisplatin-induced anorexia in rats via 5-HT2 receptor antagonism. Gastroenterology. 2008;134(7):2004–2013. doi: 10.1053/j.gastro.2008.02.078. [DOI] [PubMed] [Google Scholar]
- 12.Haslett PA. Anticytokine approaches to the treatment of anorexia and cachexia. Semin Oncol. 1998;25(2 Suppl 6):53–57. [PubMed] [Google Scholar]
- 13.Mantovani G, Maccio A, Lai P, Massa E. Cytokine activity in cancer-related anorexia/cachexia: role of megestrol acetate and medroxyprogesterone acetate. Semin Oncol. 1998;25:45–52. [PubMed] [Google Scholar]
- 14.Sternberg EM. Neural-immune interactions in health and disease. J Clin Invest. 1997;100(11):2641–2647. doi: 10.1172/JCI119807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Licinio J, Wong ML. Pathways and mechanisms for cytokine signaling of the central nervous system. J Clin Invest. 1997;100(12):2941–7. [DOI] [PMC free article] [PubMed]
- 16.Hopkins SJ, Rothwell NJ. Cytokines and the nervous system. I: expression and recognition. Trends Neurosci. 1995;18(2):83–88. doi: 10.1016/0166-2236(95)93881-W. [DOI] [PubMed] [Google Scholar]
- 17.Rothwell NJ, Hopkins SJ. Cytokines and the nervous system II: actions and mechanisms of action. Trends Neurosci. 1995;18(3):130–136. doi: 10.1016/0166-2236(95)93890-A. [DOI] [PubMed] [Google Scholar]
- 18.Tisdale M. Biology of cachexia. J Natl Cancer Inst. 1997;89:1763–1773. doi: 10.1093/jnci/89.23.1763. [DOI] [PubMed] [Google Scholar]
- 19.Plata-Salamán CR. Immunoregulators in the nervous system. Neurosci Biobehav Rev. 1991;15(2):185–215. doi: 10.1016/S0149-7634(05)80001-6. [DOI] [PubMed] [Google Scholar]
- 20.Plata-Salamán CR. Anorexia during acute and chronic disease. Nutrition. 1996;12(2):69–78. doi: 10.1016/S0899-9007(96)90702-9. [DOI] [PubMed] [Google Scholar]
- 21.Moldawer LL, Copeland EM. Proinflammatory cytokines, nutritional support, and the cachexia syndrome: interactions and therapeutic options. Cancer. 1997;79(9):1828–1839. doi: 10.1002/(SICI)1097-0142(19970501)79:9<1828::AID-CNCR28>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 22.Donohoe CL, Ryan AM, Reynolds JV. Cancer cachexia: mechanisms and clinical implications. Gastroenterol Res Pract. 2011;2011:601434. doi: 10.1155/2011/601434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moldawer LL, Rogy MA, Lowry SF. The role of cytokines in cancer cachexia. J Parenter Enteral Nutr. 1992;16(6 Suppl):43S–49S. doi: 10.1177/014860719201600602. [DOI] [PubMed] [Google Scholar]
- 24.Noguchi Y, Yoshikawa T, Matsumoto A, Svaninger GS, Gelin J. Are cytokines possible mediators of cancer cachexia? Surg Today. 1996;26(7):467–75. [DOI] [PubMed]
- 25.Matthys P, Billiau A. Cytokines and cachexia. Nutrition. 1997;13(9):763–770. doi: 10.1016/S0899-9007(97)00185-8. [DOI] [PubMed] [Google Scholar]
- 26.Gelin J, Moldawer L, Lönnroth C, Sherry B. Role of endogenous tumor necrosis factor α and interleukin 1 for experimental tumor growth and the development of cancer cachexia. Cancer Res. 1991;51:415–421. [PubMed] [Google Scholar]
- 27.Torelli G, Meguid M. Use of recombinant human soluble TNF receptor in anorectic tumor-bearing rats. Am J Physiol Regul Integr Comp Physiol. 1999;277:R850–R855. doi: 10.1152/ajpregu.1999.277.3.R850. [DOI] [PubMed] [Google Scholar]
- 28.McCarthy HD, Crowder RE, Dryden S, Williams G. Megestrol acetate stimulates food and water intake in the rat: effects on regional hypothalamic neuropeptide Y concentrations. Eur J Pharmacol. 1994;265(1–2):99–102. doi: 10.1016/0014-2999(94)90229-1. [DOI] [PubMed] [Google Scholar]
- 29.Scarlett JM, Jobst EE, Enriori PJ, Bowe DD, Batra AK, Grant WF, et al. Regulation of Central Melanocortin Signaling by Interleukin-1β. Endocrinology. 2007;148(9):4217–4225. doi: 10.1210/en.2007-0017. [DOI] [PubMed] [Google Scholar]
- 30.Lenk K, Schuler G, Adams V. Skeletal muscle wasting in cachexia and sarcopenia: molecular pathophysiology and impact of exercise training. J Cachex Sarcopenia Muscle. 2010;1(1):9–21. doi: 10.1007/s13539-010-0007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams A, Sun X, Fischer J. The expression of genes in the ubiquitin-proteasome proteolytic pathway is increased in skeletal muscle from patients with cancer. Surgery. 1999;1999(126):744–749. doi: 10.1016/S0039-6060(99)70131-5. [DOI] [PubMed] [Google Scholar]
- 32.Llovera M, García-Martínez C, López-Soriano J, Carbó N, Agell N, López-Soriano FJ, et al. Role of TNF receptor 1 in protein turnover during cancer cachexia using gene knockout mice. Mol Cell Endocrinol. 1998;142(1–2):183–189. doi: 10.1016/S0303-7207(98)00105-1. [DOI] [PubMed] [Google Scholar]
- 33.Ungureanu-Longrois D, Balligand J. Myocardial contractile dysfunction in the systematic inflammatory response syndrome: role of a cytokine-inducible nitric oxide synthase in cardiac myocytes. J Mol Cell Cardiol. 1995;1995(27):155–167. doi: 10.1016/S0022-2828(08)80015-6. [DOI] [PubMed] [Google Scholar]
- 34.Sherry B, Gelin J, Fong Y, Marano M, Wei H. Anticachectin/tumor necrosis factor-alpha antibodies attenuate development of cachexia in tumor models. FASEB J. 1989;3:1956–1962. doi: 10.1096/fasebj.3.8.2721856. [DOI] [PubMed] [Google Scholar]
- 35.Trikha M, Corringham R, Klein B. Targeted anti-interleukin-6 monoclonal antibody therapy for cancer. Clin Cancer Res. 2003;9:4653–4665. [PMC free article] [PubMed] [Google Scholar]
- 36.Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340(6):448–454. doi: 10.1056/NEJM199902113400607. [DOI] [PubMed] [Google Scholar]
- 37.Falconer JS, Fearon KC, Ross JA, Elton R, Wigmore SJ, Garden OJ, et al. Acute-phase protein response and survival duration of patients with pancreatic cancer. Cancer. 1995;75(8):2077–2082. doi: 10.1002/1097-0142(19950415)75:8<2077::AID-CNCR2820750808>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 38.Falconer JS, Fearon KC, Plester CE, Ross JA, Carter DC. Cytokines, the acute-phase response, and resting energy expenditure in cachectic patients with pancreatic cancer. Ann Surg. 1994;219(4):325–331. doi: 10.1097/00000658-199404000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Gorman P, McMillan DC, McArdle CS. Prognostic factors in advanced gastrointestinal cancer patients with weight loss. Nutr Cancer. 1999;37(1):36–40. doi: 10.1207/S15327914NC3701_4. [DOI] [PubMed] [Google Scholar]
- 40.McMillan DC. An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc. 2008;67(03):257–262. doi: 10.1017/S0029665108007131. [DOI] [PubMed] [Google Scholar]
- 41.McMillan DC. Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care. 2009;12(3):223–226. doi: 10.1097/MCO.0b013e32832a7902. [DOI] [PubMed] [Google Scholar]
- 42.Marsik C, Kazemi-Shirazi L, Schickbauer T, Winkler S, Joukhadar C, Wagner OF, et al. C-reactive protein and all-cause mortality in a large hospital-based cohort. Clin Chem. 2008;54(2):343–349. doi: 10.1373/clinchem.2007.091959. [DOI] [PubMed] [Google Scholar]
- 43.Scott HR, McMillan DC, Brown DJF, Forrest LM, McArdle CS, Milroy R. A prospective study of the impact of weight loss and the systemic inflammatory response on quality of life in patients with inoperable non-small cell lung cancer. Lung Cancer. 2003;40(3):295–299. doi: 10.1016/S0169-5002(03)00077-1. [DOI] [PubMed] [Google Scholar]
- 44.Deans D, Tan B, Wigmore S, Ross J, de Beaux A, Paterson-Brown S, et al. The influence of systemic inflammation, dietary intake and stage of disease on rate of weight loss in patients with gastro-oesophageal cancer. Br J Cancer. 2009;100(1):63–69. doi: 10.1038/sj.bjc.6604828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tisdale MJ. Mechanisms of Cancer Cachexia. Physiol Rev. 2009;89(2):381–410. doi: 10.1152/physrev.00016.2008. [DOI] [PubMed] [Google Scholar]
- 46.Guttridge DC. The biology of cancer cachexia and the role of TNF-α. In: Caligiuri MA, Lotze MT, editors. Cytokines in the genesis and treatment of cancer. Totowa, NJ: Humana Press; 2007. p. 285–303.
- 47.Lum JJ, DeBerardinis RJ, Thompson CB. Autophagy in metazoans: cell survival in the land of plenty. Nat Rev Mol Cell Biol. 2005;6(6):439–448. doi: 10.1038/nrm1660. [DOI] [PubMed] [Google Scholar]
- 48.Sandri M, Sandri C, Gilbert A, Skurk C, Calabria E, Picard A, et al. Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy. Cell. 2004;117(3):399–412. doi: 10.1016/S0092-8674(04)00400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mammucari C, Milan G, Romanello V, Masiero E, Rudolf R, Del Piccolo P, et al. FoxO3 controls autophagy in skeletal muscle in vivo. Cell Metab. 2007;6(6):458–471. doi: 10.1016/j.cmet.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 50.Dodd SL, Gagnon BJ, Senf SM, Hain BA, Judge AR. Ros-mediated activation of NF-kappaB and Foxo during muscle disuse. Muscle Nerve. 2010;41(1):110–113. doi: 10.1002/mus.21526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lorite MJ, Smith HJ, Arnold JA, Morris A, Thompson MG, Tisdale MJ. Activation of ATP-ubiquitin-dependent proteolysis in skeletal muscle in vivo and murine myoblasts in vitro by a proteolysis-inducing factor (PIF) Br J Cancer. 2001;85(2):297–302. doi: 10.1054/bjoc.2001.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sandri M, Lin J, Handschin C, Yang W, Arany ZP, Lecker SH, et al. PGC-1alpha protects skeletal muscle from atrophy by suppressing FoxO3 action and atrophy-specific gene transcription. Proc Natl Acad Sci USA. 2006;103(44):16260–16265. doi: 10.1073/pnas.0607795103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Glass DJ. Signalling pathways that mediate skeletal muscle hypertrophy and atrophy. Nat Cell Biol. 2003;5(2):87–90. doi: 10.1038/ncb0203-87. [DOI] [PubMed] [Google Scholar]
- 54.Guttridge DC. Signaling pathways weigh in on decisions to make or break skeletal muscle. Curr Opin Clin Nutr Metab Care. 2004;7(4):443–450. doi: 10.1097/01.mco.0000134364.61406.26. [DOI] [PubMed] [Google Scholar]
- 55.Eley HL, Russell ST, Tisdale MJ. Effect of branched-chain amino acids on muscle atrophy in cancer cachexia. Biochem J. 2007;407(1):113–120. doi: 10.1042/BJ20070651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Elkina Y, Haehling S, Anker SD, Springer J. The role of myostatin in muscle wasting: an overview. J Cachex Sarcopenia Muscle. 2011;2(3):143–151. doi: 10.1007/s13539-011-0035-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Benny Klimek ME, Aydogdu T, Link MJ, Pons M, Koniaris LG, Zimmers TA. Acute inhibition of myostatin-family proteins preserves skeletal muscle in mouse models of cancer cachexia. Biochem Biophys Res Commun. 2010;391(3):1548–54. [DOI] [PubMed]
- 58.Bonetto A, Penna F, Minero VG, Reffo P, Bonelli G, Baccino FM, et al. Deacetylase inhibitors modulate the myostatin/follistatin axis without improving cachexia in tumor-bearing mice. Curr Cancer Drug Targets. 2009;9(5):608–616. doi: 10.2174/156800909789057015. [DOI] [PubMed] [Google Scholar]
- 59.van Royen M, Carbó N, Busquets S, Alvarez B, Quinn LS, López-Soriano FJ, et al. DNA fragmentation occurs in skeletal muscle during tumor growth: a link with cancer cachexia? Biochem Biophys Res Commun. 2000;270(2):533–537. doi: 10.1006/bbrc.2000.2462. [DOI] [PubMed] [Google Scholar]
- 60.Belizário JE, Lorite MJ, Tisdale MJ. Cleavage of caspases-1, -3, -6, -8 and -9 substrates by proteases in skeletal muscles from mice undergoing cancer cachexia. Br J Cancer. 2001;84(8):1135–1140. doi: 10.1054/bjoc.2001.1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Trendelenburg AU, Meyer A, Rohner D, Boyle J, Hatakeyama S, Glass DJ. Myostatin reduces Akt/TORC1/p70S6K signaling, inhibiting myoblast differentiation and myotube size. Am J Physiol Cell Physiol. 2009;296(6):C1258–70. [DOI] [PubMed]
- 62.Amirouche A, Durieux A-C, Banzet S, Koulmann N, Bonnefoy R, Mouret C, et al. Down-regulation of Akt/mammalian target of rapamycin signaling pathway in response to myostatin overexpression in skeletal muscle. Endocrinology. 2009;150(1):286–294. doi: 10.1210/en.2008-0959. [DOI] [PubMed] [Google Scholar]
- 63.Morissette MR, Cook SA, Buranasombati C, Rosenberg MA, Rosenzweig A. Myostatin inhibits IGF-I-induced myotube hypertrophy through Akt. Am J Physiol Cell Physiol. 2009;297(5):C1124–C1132. doi: 10.1152/ajpcell.00043.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen RH, Su YH, Chuang RL, Chang TY. Suppression of transforming growth factor-beta-induced apoptosis through a phosphatidylinositol 3-kinase/Akt-dependent pathway. Oncogene. 1998;17(15):1959–1968. doi: 10.1038/sj.onc.1202111. [DOI] [PubMed] [Google Scholar]
- 65.Bodine SC, Stitt TN, Gonzalez M, Kline WO, Stover GL, Bauerlein R, et al. Akt/mTOR pathway is a crucial regulator of skeletal muscle hypertrophy and can prevent muscle atrophy in vivo. Nat Cell Biol. 2001;3(11):1014–1019. doi: 10.1038/ncb1101-1014. [DOI] [PubMed] [Google Scholar]
- 66.Zdychová J, Komers R. Emerging role of Akt kinase/protein kinase B signaling in pathophysiology of diabetes and its complications. Physiol Res. 2005;54(1):1–16. doi: 10.33549/physiolres.930582. [DOI] [PubMed] [Google Scholar]
- 67.Brink M, Wellen J, Delafontaine P. Angiotensin II causes weight loss and decreases circulating insulin-like growth factor I in rats through a pressor-independent mechanism. J Clin Invest. 1996;97(11):2509–2516. doi: 10.1172/JCI118698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Musarò A, Giacinti C, Borsellino G, Dobrowolny G, Pelosi L, Cairns L, et al. Stem cell-mediated muscle regeneration is enhanced by local isoform of insulin-like growth factor 1. Proc Natl Acad Sci USA. 2004;101(5):1206–1210. doi: 10.1073/pnas.0303792101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Costelli P, Muscaritoli M, Bossola M, Penna F, Reffo P, Bonetto A, et al. IGF-1 is downregulated in experimental cancer cachexia. Am J Physiol Regul Integr Comp Physiol. 2006;291(3):R674–R683. doi: 10.1152/ajpregu.00104.2006. [DOI] [PubMed] [Google Scholar]
- 70.Buck M, Chojkier M. Muscle wasting and dedifferentiation induced by oxidative stress in a murine model of cachexia is prevented by inhibitors of nitric oxide synthesis and antioxidants. EMBO J. 1996;15(8):1753–1765. [PMC free article] [PubMed] [Google Scholar]
- 71.Laviano A, Meguid MM, Preziosa I, Fanelli FR. Oxidative stress and wasting in cancer. Curr Opin Clin Nutr Metab Care. 2007;10(4):449–56. [DOI] [PubMed]
- 72.Barreiro E, la Puente de B, Busquets S. Both oxidative and nitrosative stress are associated with muscle wasting in tumour-bearing rats. FEBS Lett. 2005;579:1646–52. [DOI] [PubMed]
- 73.Mantovani G, Macciò A, Madeddu C, Mura L, Gramignano G, Lusso MR, et al. Antioxidant agents are effective in inducing lymphocyte progression through cell cycle in advanced cancer patients: assessment of the most important laboratory indexes of cachexia and oxidative stress. J Mol Med. 2003;81(10):664–673. doi: 10.1007/s00109-003-0476-1. [DOI] [PubMed] [Google Scholar]
- 74.Chlebowski RT, Heber D. Hypogonadism in male patients with metastatic cancer prior to chemotherapy. Cancer Res. 1982;42(6):2495–2498. [PubMed] [Google Scholar]
- 75.Zitzmann M. Hormone substitution in male hypogonadism. Mol Cell Endocrinol. 2000;2000(161):73–88. doi: 10.1016/S0303-7207(99)00227-0. [DOI] [PubMed] [Google Scholar]
- 76.Lobo RA. Androgens in postmenopausal women: production, possible role, and replacement options. Obstet Gynecol Surv. 2001;56(6):361–376. doi: 10.1097/00006254-200106000-00022. [DOI] [PubMed] [Google Scholar]
- 77.Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, et al. Cachexia: a new definition. Clin Nutr. 2008;27(6):793–799. doi: 10.1016/j.clnu.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 78.Hein L, Barsh G, Pratt R, Dzau V. Behavioural and cardiovascular effects of disrupting the angiotensin II type-2 receptor gene in mice. Nature. 1995;1995(377):744–747. doi: 10.1038/377744a0. [DOI] [PubMed] [Google Scholar]
- 79.Garcia J, Li H, Mann D, Epner D, Hayes T. Hypogonadism in male patients with cancer. Cancer. 2006;2006(106):2583–2591. doi: 10.1002/cncr.21889. [DOI] [PubMed] [Google Scholar]
- 80.Fearon K, Dahele M, Skipworth R. Citation information. In: Nicholson J, Hofbauer K, Anker S, Inui A, editors. Pharmacotherapy of Cachexia. Boca Raton: CRC Press; 2009. p. 117–42.
- 81.Bozzetti F. Basics in clinical nutrition: nutritional support in cancer. Eur J Clin Nutr Metab (e-SPEN). 5(3):e148–52.
- 82.Tohgo A, Kumazawa E, Akahane K, Asakawa A, Inui A. Anticancer drugs that induce cancer-associated cachectic syndromes. Expert Rev Anticancer Ther. 2002;2(1):121–129. doi: 10.1586/14737140.2.1.121. [DOI] [PubMed] [Google Scholar]
- 83.Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489–95. [DOI] [PubMed]
- 84.Mahmoud FA, Rivera NI. The role of C-reactive protein as a prognostic indicator in advanced cancer. Curr Oncol Rep. 2002;4(3):250–255. doi: 10.1007/s11912-002-0023-1. [DOI] [PubMed] [Google Scholar]
- 85.Deans CC, Wigmore SJS. Systemic inflammation, cachexia and prognosis in patients with cancer. Curr Opin Clin Nutr Metab Care. 2005;8(3):265–269. doi: 10.1097/01.mco.0000165004.93707.88. [DOI] [PubMed] [Google Scholar]
- 86.Pasceri V, Willerson JT, Yeh ET. Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation. 2000;102(18):2165–2168. doi: 10.1161/01.CIR.102.18.2165. [DOI] [PubMed] [Google Scholar]
- 87.Pasceri V, Cheng JS, Chang J. 5. Modulation of C-reactive protein-mediated monocyte chemoattractant protein-1 induction in human endothelial cells by anti-atherosclerosis drugs. Circulation. 2001;103(21):2531–2534. doi: 10.1161/01.CIR.103.21.2531. [DOI] [PubMed] [Google Scholar]
- 88.Mantovani G. The Current Management of Cancer Cachexia. Mantovani G, Anker SD, Inui A, Morley JE, Fanelli FR, Scevola D, et al., editors. Cachexia and wasting: a modern approach. link.springer.com. Milan: Springer; 2006. p. 563–79.
- 89.Straus DS, Pascual G, Li M, Welch JS, Ricote M, Hsiang CH, et al. 15-deoxy-delta 12,14-prostaglandin J2 inhibits multiple steps in the NF-kappa B signaling pathway. Proc Natl Acad Sci USA. 2000;97(9):4844–4849. doi: 10.1073/pnas.97.9.4844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schwartz SA, Hernandez A, Mark Evers B. The role of NF-kappaB/IkappaB proteins in cancer: implications for novel treatment strategies. Surg Oncol. 1999;8(3):143–53. [DOI] [PubMed]
- 91.Ghosh S, May MJ, Kopp EB. NF-kappa B and Rel proteins: evolutionarily conserved mediators of immune responses. Annu Rev Immunol. 1998;16:225–260. doi: 10.1146/annurev.immunol.16.1.225. [DOI] [PubMed] [Google Scholar]
- 92.Lawrence T, Gilroy DW, Colville-Nash PR, Willoughby DA. Possible new role for NF-kappaB in the resolution of inflammation. Nat Med. 2001;7(12):1291–1297. doi: 10.1038/nm1201-1291. [DOI] [PubMed] [Google Scholar]
- 93.Loewe R, Holnthoner W, Gröger M, Pillinger M, Gruber F, Mechtcheriakova D, et al. Dimethylfumarate inhibits TNF-induced nuclear entry of NF-kappa B/p65 in human endothelial cells. J Immunol. 2002;168(9):4781–4787. doi: 10.4049/jimmunol.168.9.4781. [DOI] [PubMed] [Google Scholar]
- 94.Langen RCR, Schols AMA, Janssen-Heininger YMY. 5. Inflammatory cytokines inhibit myogenic differentiation through activation of nuclear factor-kappaB. FASEB J. 2001;15(7):1169–1180. doi: 10.1096/fj.00-0463. [DOI] [PubMed] [Google Scholar]
- 95.Fiorentino DF, Bond MW, Mosmann TR. Two types of mouse T helper cell. IV. Th2 clones secrete a factor that inhibits cytokine production by Th1 clones. J Exp Med. 1989;170(6):2081–2095. doi: 10.1084/jem.170.6.2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Groesdonk HV, Senftleben U. Modulation of inhibitor kappaB kinase/nuclear factor kappaB signaling during critical illness: a double-edged sword. Crit Care Med. 2004;32(5):1239–1240. doi: 10.1097/01.CCM.0000115255.43177.2C. [DOI] [PubMed] [Google Scholar]
- 97.Radbruch L, Elsner F, Trottenberg P, Strasser F, Fearon K. Clinical practice guidelines on cancer cachexia in advanced cancer patients. Aachen, Department of Palliative Medicinen/European Palliative Care Research Collaborative. 2010.
- 98.Barber MD, Ross JA, Fearon KC. Cancer cachexia. Surg Oncol. 1999;8(3):133–141. doi: 10.1016/S0960-7404(99)00045-6. [DOI] [PubMed] [Google Scholar]
- 99.Inui A. Cancer anorexia-cachexia syndrome: current issues in research and management. CA Cancer J Clin. 2002;52(2):72–91. doi: 10.3322/canjclin.52.2.72. [DOI] [PubMed] [Google Scholar]
- 100.Del Fabbro E, Dalal S, Bruera E. Symptom control in palliative care—Part II: cachexia/anorexia and fatigue. J Palliat Med. 2006;9(2):409–421. doi: 10.1089/jpm.2006.9.409. [DOI] [PubMed] [Google Scholar]
- 101.Topkan E, Yavuz AA, Ozyilkan O. Cancer cachexia: pathophysiologic aspects and treatment options. Asian Pac J Cancer Prev. 2007;8(3):445–451. [PubMed] [Google Scholar]
- 102.Mantovani G, Macciò A, Madeddu C, Serpe R, Massa E, Dessì M, et al. Randomized Phase III Clinical Trial of Five Different Arms of Treatment in 332 Patients with Cancer Cachexia. Oncologist. 2010;15(2):200–211. doi: 10.1634/theoncologist.2009-0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tazi E, Errihani H. Treatment of cachexia in oncology. Indian J Palliat Care. 2010;16(3):129–137. doi: 10.4103/0973-1075.73644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nelson KA. The cancer anorexia-cachexia syndrome. Semin Oncol. 2000;27(1):64–68. [PubMed] [Google Scholar]
- 105.Gagnon B, Bruera E. A review of the drug treatment of cachexia associated with cancer. Drugs. 1998;55(5):675–688. doi: 10.2165/00003495-199855050-00005. [DOI] [PubMed] [Google Scholar]
- 106.Argiles JM, Meijsing SH, Pallarés-Trujillo J, Guirao X, López-Soriano FJ. Cancer cachexia: a therapeutic approach. Med Res Rev. 2000;21(1):83–101. doi: 10.1002/1098-1128(200101)21:1<83::AID-MED4>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 107.Nelson K, Walsh D, Deeter P, Sheehan F. A phase II study of delta-9-tetrahydrocannabinol for appetite stimulation in cancer-associated anorexia. J Palliat Care. 1993;10(1):14–18. [PubMed] [Google Scholar]
- 108.Plasse TF, Gorter RW, Krasnow SH, Lane M, Shepard KV, Wadleigh RG. Recent clinical experience with dronabinol. Pharmacol Biochem Behav. 1991;40(3):695–700. doi: 10.1016/0091-3057(91)90385-F. [DOI] [PubMed] [Google Scholar]
- 109.Mantovani G, Maccio A, Massa E, Madeddu C. Managing cancer-related anorexia/cachexia. Drugs. 2001;61(4):499–514. doi: 10.2165/00003495-200161040-00004. [DOI] [PubMed] [Google Scholar]
- 110.Kardinal CG, Loprinzi CL, Schaid DJ, Hass AC, Dose AM, Athmann LM, et al. A controlled trial of cyproheptadine in cancer patients with anorexia and/or cachexia. Cancer. 1990;65(12):2657–2662. doi: 10.1002/1097-0142(19900615)65:12<2657::AID-CNCR2820651210>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 111.Meguid MM, Fetissov SO, Varma M, Sato T, Zhang L, Laviano A, et al. Hypothalamic dopamine and serotonin in the regulation of food intake. Nutrition. 2000;16(10):843–857. doi: 10.1016/S0899-9007(00)00449-4. [DOI] [PubMed] [Google Scholar]
- 112.Laviano A, Meguid MM, Yang ZJ, Gleason JR, Cangiano C, Fanelli FR. Cracking the riddle of cancer anorexia. Nutrition. 1996;12(10):706–10. [DOI] [PubMed]
- 113.Moertel CG, Kvols LK, Rubin J. A study of cyproheptadine in the treatment of metastatic carcinoid tumor and the malignant carcinoid syndrome. Cancer. 1990;67(1):33–36. doi: 10.1002/1097-0142(19910101)67:1<33::AID-CNCR2820670107>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 114.Daviss WB, Scott J. A chart review of cyproheptadine for stimulant-induced weight loss. J Child Adolesc Psychopharmacol. 2004;14(1):65–73. doi: 10.1089/104454604773840508. [DOI] [PubMed] [Google Scholar]
- 115.Genazzani AD, Strucchi C, Malavasi B, Tortolani F, Vecchi F, Luisi S, et al. Effects of cyproheptadine clorhydrate, a serotonin receptor antagonist, on endocrine parameters in weight-loss related amenorrhea. Gynecol Endocrinol. 2001;15(4):279–285. doi: 10.1080/gye.15.4.279.285. [DOI] [PubMed] [Google Scholar]
- 116.Feliui J, Gontález-Barón M, Berrocal A, Ordónez A, Barón-Saura JM. Treatment of cancer anorexia with megestrol acetate: which is the optimal dose? J Natl Cancer Inst. 1991;83(6):449–450. doi: 10.1093/jnci/83.6.449. [DOI] [PubMed] [Google Scholar]
- 117.Loprinzi CL, Ellison NM, Schaid DJ, Krook JE, Athmann LM, Dose AM, et al. Controlled trial of megestrol acetate for the treatment of cancer anorexia and cachexia. J Natl Cancer Inst. 1990;82(13):1127–1132. doi: 10.1093/jnci/82.13.1127. [DOI] [PubMed] [Google Scholar]
- 118.Loprinzi CL, Michalak JC, Schaid DJ, Mailliard JA, Athmann LM, Goldberg RM, et al. Phase III evaluation of four doses of megestrol acetate as therapy for patients with cancer anorexia and/or cachexia. J Clin Oncol. 1993;11(4):762–767. doi: 10.1200/JCO.1993.11.4.762. [DOI] [PubMed] [Google Scholar]
- 119.Bruera E, Macmillan K, Kuehn N, Hanson J, MacDonald RN. A controlled trial of megestrol acetate on appetite, caloric intake, nutritional status, and other symptoms in patients with advanced cancer. Cancer. 1990;66(6):1279–1282. doi: 10.1002/1097-0142(19900915)66:6<1279::AID-CNCR2820660630>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 120.Tchekmedyian NSN, Hickman MM, Siau JJ, Greco FAF, Keller JJ, Browder HH, et al. Megestrol acetate in cancer anorexia and weight loss. Cancer. 1992;69(5):1268–1274. doi: 10.1002/cncr.2820690532. [DOI] [PubMed] [Google Scholar]
- 121.Loprinzi CL, Schaid DJ, Dose AM, Burnham NL, Jensen MD. Body-composition changes in patients who gain weight while receiving megestrol acetate. J Clin Oncol. 1993;11(1):152–154. doi: 10.1200/JCO.1993.11.1.152. [DOI] [PubMed] [Google Scholar]
- 122.Rowland KM, Loprinzi CL, Shaw EG, Maksymiuk AW, Kuross SA, Jung SH, et al. Randomized double-blind placebo-controlled trial of cisplatin and etoposide plus megestrol acetate/placebo in extensive-stage small-cell lung cancer: a North Central Cancer Treatment Group study. J Clin Oncol. 1995;14(1):135–141. doi: 10.1200/JCO.1996.14.1.135. [DOI] [PubMed] [Google Scholar]
- 123.Maltoni M, Nanni O, Scarpi E, Rossi D, Serra P, Amadori D. High-dose progestins for the treatment of cancer anorexia-cachexia syndrome: a systematic review of randomised clinical trials. Ann Oncol. 2001;12(3):289–300. doi: 10.1023/A:1011156811739. [DOI] [PubMed] [Google Scholar]
- 124.Bruera EE. Pharmacological treatment of cachexia: any progress? Support Care Cancer. 1998;6(2):109–113. doi: 10.1007/s005200050143. [DOI] [PubMed] [Google Scholar]
- 125.Schwartz M, Dallman M. Hypothalamic response to starvation: implications for the study of wasting disorders. Am J Physiol. 1995;269:R949–R957. doi: 10.1152/ajpregu.1995.269.5.R949. [DOI] [PubMed] [Google Scholar]
- 126.Elmquist JK, Maratos-Flier E, Saper CB, Flier JS. Unraveling the central nervous system pathways underlying responses to leptin. Nat Neurosci. 1998;1(6):445–450. doi: 10.1038/2164. [DOI] [PubMed] [Google Scholar]
- 127.Woods SC, Seeley RJ, Porte D, Schwartz MW. Signals that regulate food intake and energy homeostasis. Science. 1998;280(5368):1378–1383. doi: 10.1126/science.280.5368.1378. [DOI] [PubMed] [Google Scholar]
- 128.Bray G, York D. The MONA LISA hypothesis in the time of leptin. Recent Prog Horm Res. 1998;53:95–117. [PubMed] [Google Scholar]
- 129.Kalra SP, Dube MG, Pu S, Xu B, Horvath TL, Kalra PS. Interacting appetite-regulating pathways in the hypothalamic regulation of body weight. Endocr Rev. 1999;20(1):68–100. doi: 10.1210/er.20.1.68. [DOI] [PubMed] [Google Scholar]
- 130.Schwartz MW, Woods SC, Porte D, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404(6778):661–671. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- 131.Inui A. Transgenic approach to the study of body weight regulation. Pharmacol Rev. 2000;52(1):35–61. [PubMed] [Google Scholar]
- 132.Inui A. Transgenic study of energy homeostasis equation: implications and confounding influences. FASEB J. 2000;14(14):2158–2170. doi: 10.1096/fj.00-0291rev. [DOI] [PubMed] [Google Scholar]
- 133.Plata-Salamán C. Central nervous system mechanisms contributing to the cachexia–anorexia syndrome. Nutrition. 2000;16:1009–1012. doi: 10.1016/S0899-9007(00)00413-5. [DOI] [PubMed] [Google Scholar]
- 134.Costa AM, Spence KT, Plata-Salamán CR, ffrench-Mullen JM. Residual Ca2+ channel current modulation by megestrol acetate via a G-protein alpha s-subunit in rat hypothalamic neurones. J Physiol (Lond.). 1995;487 (Pt 2):291–303. [DOI] [PMC free article] [PubMed]
- 135.John M. Appetite stimulants. In: Nicholson JR, Hofbauer KG, Anker SD, Inui A, editors. Pharmacotherapy of cachexia. Boca Raton: CRC Press; 2005. p. 291–302. http://www.crcnetbase.com/doi/abs/10.1201/9781420048957.ch16.
- 136.Kaegi E. Unconventional therapies for cancer: 4. Hydrazine sulfate. Task force on alternative therapies of the Canadian breast cancer research initiative. CMAJ. 1998;158(10):1327–1330. [PMC free article] [PubMed] [Google Scholar]
- 137.Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402(6762):656–660. doi: 10.1038/45230. [DOI] [PubMed] [Google Scholar]
- 138.Inui A. Ghrelin: an orexigenic and somatotrophic signal from the stomach. Nat Rev Neurosci. 2001;2(8):551–560. doi: 10.1038/35086018. [DOI] [PubMed] [Google Scholar]
- 139.Takaya K, Ariyasu H, Kanamoto N, Iwakura H, Yoshimoto A, Harada M, et al. Ghrelin strongly stimulates growth hormone release in humans. J Clin Endocrinol Metab. 2000;85(12):4908–4911. doi: 10.1210/jc.85.12.4908. [DOI] [PubMed] [Google Scholar]
- 140.Arvat E, Maccario M, Di Vito L, Broglio F, Benso A, Gottero C, et al. Endocrine activities of ghrelin, a natural growth hormone secretagogue (GHS), in humans: comparison and interactions with hexarelin, a nonnatural peptidyl GHS, and GH-releasing hormone. J Clin Endocrinol Metab. 2001;86(3):1169–1174. doi: 10.1210/jc.86.3.1169. [DOI] [PubMed] [Google Scholar]
- 141.Hataya Y, Akamizu T, Takaya K, Kanamoto N, Ariyasu H, Saijo M, et al. A low dose of ghrelin stimulates growth hormone (GH) release synergistically with GH-releasing hormone in humans. J Clin Endocrinol Metab. 2001;86(9):4552. doi: 10.1210/jc.86.9.4552. [DOI] [PubMed] [Google Scholar]
- 142.Akamizu T, Takaya K, Irako T, Hosoda H, Teramukai S, Matsuyama A, et al. Pharmacokinetics, safety, and endocrine and appetite effects of ghrelin administration in young healthy subjects. Eur J Endocrinol. 2004;150(4):447–455. doi: 10.1530/eje.0.1500447. [DOI] [PubMed] [Google Scholar]
- 143.Akamizu T, Kangawa K. Ghrelin for cachexia. J Cachex Sarcopenia Muscle. 2010;1(2):169–176. doi: 10.1007/s13539-010-0011-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Gibney J, Healy ML, Sonksen PH. The growth hormone/insulin-like growth factor-I Axis in exercise and sport. Endocr Rev. 2007;28(6):603–624. doi: 10.1210/er.2006-0052. [DOI] [PubMed] [Google Scholar]
- 145.Velloso CP. Regulation of muscle mass by growth hormone and IGF-I. Br J Pharmacol. 2008;154(3):557–568. doi: 10.1038/bjp.2008.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gonzalez-Rey E, Chorny A, Delgado M. Therapeutic action of ghrelin in a mouse model of colitis. Gastroenterology. 2006;130(6):1707–1720. doi: 10.1053/j.gastro.2006.01.041. [DOI] [PubMed] [Google Scholar]
- 147.Waseem T, Duxbury M, Ito H, Ashley SW, Robinson MK. Exogenous ghrelin modulates release of pro-inflammatory and anti-inflammatory cytokines in LPS-stimulated macrophages through distinct signaling pathways. Surgery. 2008;143(3):334–342. doi: 10.1016/j.surg.2007.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Dixit VD, Schaffer EM, Pyle RS, Collins GD, Sakthivel SK, Palaniappan R, et al. Ghrelin inhibits leptin- and activation-induced proinflammatory cytokine expression by human monocytes and T cells. J Clin Invest. 2004;114(1):57–66. doi: 10.1172/JCI21134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Li WG, Gavrila D, Liu X, Wang L, Gunnlaugsson S, Stoll LL, et al. Ghrelin inhibits proinflammatory responses and nuclear factor-κB activation in human endothelial cells. Circulation. 2004;109:2221–2226. doi: 10.1161/01.CIR.0000127956.43874.F2. [DOI] [PubMed] [Google Scholar]
- 150.Wu R, Dong W, Zhou M, Zhang F, Marini CP, Ravikumar TS, et al. Ghrelin attenuates sepsis-induced acute lung injury and mortality in rats. Am J Respir Crit Care Med. 2007;176(8):805–813. doi: 10.1164/rccm.200604-511OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Theil M–M, Miyake S, Mizuno M, Tomi C, Croxford JL, Hosoda H, et al. Suppression of experimental autoimmune encephalomyelitis by ghrelin. J Immunol. 2009;183(4):2859–2866. doi: 10.4049/jimmunol.0803362. [DOI] [PubMed] [Google Scholar]
- 152.Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. J Clin Invest. 2007;117(2):289–296. doi: 10.1172/JCI30555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Balasubramaniam A, Joshi R, Su C, Friend LA, Sheriff S, Kagan RJ, et al. Ghrelin inhibits skeletal muscle protein breakdown in rats with thermal injury through normalizing elevated expression of E3 ubiquitin ligases MuRF1 and MAFbx. Am J Physiol Regul Integr Comp Physiol. 2009;296(4):R893–R901. doi: 10.1152/ajpregu.00015.2008. [DOI] [PubMed] [Google Scholar]
- 154.Sheriff S, Joshi R, Friend LA, James JH, Balasubramaniam A. Ghrelin receptor agonist, GHRP-2, attenuates burn injury-induced MuRF-1 and MAFbx expression and muscle proteolysis in rats. Peptides. 2009;30(10):1909–1913. doi: 10.1016/j.peptides.2009.06.029. [DOI] [PubMed] [Google Scholar]
- 155.Yamamoto D, Ikeshita N, Matsubara T, Tasaki H, Herningtyas EH, Toda K, et al. GHRP-2, a GHS-R agonist, directly acts on myocytes to attenuate the dexamethasone-induced expressions of muscle-specific ubiquitin ligases, Atrogin-1 and MuRF1. Life Sci. 2008;82(9–10):460–466. doi: 10.1016/j.lfs.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 156.Stitt TN, Drujan D, Clarke BA, Panaro F, Timofeyva Y, Kline WO, et al. The IGF-1/PI3K/Akt pathway prevents expression of muscle atrophy-induced ubiquitin ligases by inhibiting FOXO transcription factors 10.1016/S1097-2765(04), 00211–4: molecular Cell | ScienceDirect.com. Mol Cell. 2004;14:395–403. doi: 10.1016/S1097-2765(04)00211-4. [DOI] [PubMed] [Google Scholar]
- 157.Nagaya N, Kojima M, Kangawa K. Ghrelin, a novel growth hormone-releasing peptide, in the treatment of cardiopulmonary-associated cachexia. Intern Med. 2005;45(3):127–134. doi: 10.2169/internalmedicine.45.1402. [DOI] [PubMed] [Google Scholar]
- 158.Garcia J, Boccia R, Graham C. A phase II randomized, placebo-controlled, double-blind study of the efficacy and safety of RC-1291 (RC) for the treatment of cancer cachexia. J Clin Oncol. 2007;25:9133.
- 159.Olaku O, White JD. Herbal therapy use by cancer patients: a literature review on case reports. Eur J Cancer. 2011;47(4):508–514. doi: 10.1016/j.ejca.2010.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kusunoki H, Haruma K, Hata J, Ishii M, Kamada T, Yamashita N, et al. Efficacy of Rikkunshito, a traditional Japanese medicine (Kampo), in treating functional dyspepsia. Intern Med. 2010;49(20):2195–2202. doi: 10.2169/internalmedicine.49.3803. [DOI] [PubMed] [Google Scholar]
- 161.Takahashi T, Endo S, Nakajima K, Souma Y, Nishida T. Effect of rikkunshito, a chinese herbal medicine, on stasis in patients after pylorus-preserving gastrectomy. World J Surg. 2009;33(2):296–302. doi: 10.1007/s00268-008-9854-8. [DOI] [PubMed] [Google Scholar]
- 162.Oyachi N, Takano K, Hasuda N, Arai H. Effects of Rikkunshi-to on infantile hypertrophic pyloric stenosis, refractory to atropine. Pediatr Int. 2008;2008(50):581–583. doi: 10.1111/j.1442-200X.2008.02682.x. [DOI] [PubMed] [Google Scholar]
- 163.Oka T, Tamagawa Y, Hayashida S, Kaneda Y, Kodama N, Tsuji S. Rikkunshi-to attenuates adverse gastrointestinal symptoms induced by fluvoxamine. Biopsychosoc Med. 2007;1:21. doi: 10.1186/1751-0759-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Yagi M, Homma S, Kubota M, Iinuma Y. The herbal medicine Rikkunshi-to stimulates and coordinates the gastric myoelectric activity in post-operative dyspeptic children after gastrointestinal surgery. Pediatr Surg Int. 2004;2004(19):760–765. doi: 10.1007/s00383-003-1053-y. [DOI] [PubMed] [Google Scholar]
- 165.Kawahara H, Okuyama H, Nose K, Nakai H, Yoneda A, Kubota A, et al. Physiological and clinical characteristics of gastroesophageal reflux after congenital diaphragmatic hernia repair. J Pediatr Surg. 2010;45(12):2346–2350. doi: 10.1016/j.jpedsurg.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 166.Sadakane C, Muto S, Nakagawa K, Ohnishi S, Saegusa Y, Nahata M, et al. 10-Gingerol, a component of rikkunshito, improves cisplatin-induced anorexia by inhibiting acylated ghrelin degradation. Biochem Biophys Res Commun. 2011;412(3):506–511. doi: 10.1016/j.bbrc.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 167.Huang C, Lin S, Liao P, Young S. The immunopharmaceutical effects and mechanisms of herb medicine. Cell Mol Immunol. 2008;5:23–31. doi: 10.1038/cmi.2008.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kumar NB, Kazi A, Smith T, Crocker T, Yu D, Reich RR, et al. Cancer cachexia: traditional therapies and novel molecular mechanism-based approaches to treatment. Curr Treat Options Oncol. 2010;11(3–4):107–117. doi: 10.1007/s11864-010-0127-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Couch M, Lai V, Cannon T, Guttridge D, Zanation A, George J, et al. Cancer cachexia syndrome in head and neck cancer patients: part I. Diagnosis, impact on quality of life and survival, and treatment. Head Neck. 2007;29(4):401–411. doi: 10.1002/hed.20447. [DOI] [PubMed] [Google Scholar]
- 170.Fearon KCH, Von Meyenfeldt MF, Moses AGW, Van Geenen R, Roy A, Gouma DJ, et al. Effect of a protein and energy dense N-3 fatty acid enriched oral supplement on loss of weight and lean tissue in cancer cachexia: a randomised double blind trial. Gut. 2003;52(10):1479–1486. doi: 10.1136/gut.52.10.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Fearon KCH. Cancer cachexia: developing multimodal therapy for a multidimensional problem. Eur J Cancer. 2008;44(8):1124–1132. doi: 10.1016/j.ejca.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 172.Palesty JA, Dudrick SJ. Cachexia, malnutrition, the refeeding syndrome, and lessons from Goldilocks. Surg Clin North Am. 2011;91(3):653–673. doi: 10.1016/j.suc.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 173.Khan LUR, Ahmed J, Khan S, Macfie J. Refeeding syndrome: a literature review. Gastroenterol Res Pract. 2010;2011. [DOI] [PMC free article] [PubMed]
- 174.Solomon SM, Kirby DF. The refeeding syndrome: a review. J Parenter Enteral Nutr. 1990;14(1):90–97. doi: 10.1177/014860719001400190. [DOI] [PubMed] [Google Scholar]
- 175.Sobotka L. Refeeding syndrome. Basics in clinical nutrition. 3rd ed. Prague: Galen; 2004. p. 288–91.
- 176.Ardies CM. Exercise, cachexia, and cancer therapy: a molecular rationale. Nutr Cancer. 2001;42(2):143–157. doi: 10.1207/S15327914NC422_1. [DOI] [PubMed] [Google Scholar]
- 177.al-Majid S, McCarthy DO. Cancer-induced fatigue and skeletal muscle wasting: the role of exercise. Biol Res Nurs. 2001;2(3):186–97. [DOI] [PubMed]
- 178.Doyle CC, Kushi LHL, Byers TT, Courneya KSK, Demark-Wahnefried WW, Grant BB, et al. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin. 2005;56:323–53. [DOI] [PubMed]
- 179.Strasser F. Eating-related disorders in patients with advanced cancer. Support Care Cancer. 2003;11(1):11–20. doi: 10.1007/s00520-002-0391-y. [DOI] [PubMed] [Google Scholar]
- 180.Ravasco P, Monteiro Grillo I, Camilo M. Cancer wasting and quality of life react to early individualized nutritional counselling! Clin Nutr. 2007;26(1):7–15. [DOI] [PubMed]
- 181.Whitman MM. The starving patient: supportive care for people with cancer. Clin J Oncol Nurs. 2000;4(3):121–125. [PubMed] [Google Scholar]
- 182.Samuels SE, Knowles AL, Tilignac T, Debiton E, Madelmont JC, Attaix D. Protein metabolism in the small intestine during cancer cachexia and chemotherapy in mice. Cancer Res. 2000;60(17):4968–4974. [PubMed] [Google Scholar]
- 183.Nelson K, Walsh D, Sheehan F. Cancer and chemotherapy-related upper gastrointestinal symptoms: the role of abnormal gastric motor function and its evaluation in cancer patients. Support Care Cancer. 2002;10(6):455–461. doi: 10.1007/s00520-002-0340-9. [DOI] [PubMed] [Google Scholar]
- 184.SMITH GF, TOONEN TR. Primary care of the patient with cancer. [Internet]. Am Fam Physician. 2007 [cited 2012 Mar 9]. pages 1207–14. Available from: http://www.aafp.org/afp/2007/0415/p1207.html. [PubMed]
- 185.Jenns K. Importance of nausea. Cancer Nurs. 1994;17:488–93. [PubMed]
- 186.Hesketh PJ, Kris MG, Grunberg SM, Beck T, Hainsworth JD, Harker G, et al. Proposal for classifying the acute emetogenicity of cancer chemotherapy. J Clin Oncol. 1997;15(1):103–109. doi: 10.1200/JCO.1997.15.1.103. [DOI] [PubMed] [Google Scholar]
- 187.Hesketh PJ, Gandara DR. Serotonin antagonists: a new class of antiemetic agents. J Natl Cancer Inst. 1991;83(9):613–620. doi: 10.1093/jnci/83.9.613. [DOI] [PubMed] [Google Scholar]
- 188.Koeller J, Aapro M, Gralla R, Grunberg S, Hesketh P, Kris M, et al. Antiemetic guidelines: creating a more practical treatment approach. Support Care Cancer. 2002;10(7):519–22. [DOI] [PubMed]
- 189.Grunberg SM, Koeller JM. Palonosetron: a unique 5-HT3-receptor antagonist for the prevention of chemotherapy-induced emesis. Expert Opin Pharmacother. 2012;4(12):2297–303. [DOI] [PubMed]
- 190.McNulty R. Are all 5-HT3 receptor antagonists the same? J Natl Compr Canc Netw. 2007;5(1):35–43. [DOI] [PubMed]
- 191.Eisenberg PP, Figueroa-Vadillo JJ, Zamora RR, Charu VV, Hajdenberg JJ, Cartmell AA, et al. Improved prevention of moderately emetogenic chemotherapy-induced nausea and vomiting with palonosetron, a pharmacologically novel 5-HT3 receptor antagonist: results of a phase III, single-dose trial versus dolasetron. Cancer. 2003;98(11):2473–2482. doi: 10.1002/cncr.11817. [DOI] [PubMed] [Google Scholar]
- 192.Roila F, Tonato M, Cognetti F, Cortesi E, Favalli G, Marangolo M, et al. Prevention of cisplatin-induced emesis: a double-blind multicenter randomized crossover study comparing ondansetron and ondansetron plus dexamethasone. J Clin Oncol. 1991;9(4):675–678. doi: 10.1200/JCO.1991.9.4.675. [DOI] [PubMed] [Google Scholar]
- 193.Hesketh PJ, Grunberg SM, Gralla RJ, Warr DG, Roila F, de Wit R, et al. The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin–the Aprepitant Protocol 052 Study Group. J Clin Oncol. 2003;21(22):4112–4119. doi: 10.1200/JCO.2003.01.095. [DOI] [PubMed] [Google Scholar]
- 194.de Wit R, Herrstedt J, Rapoport B, Carides AD, Guoguang-Ma J, Elmer M, et al. The oral NK(1) antagonist, aprepitant, given with standard antiemetics provides protection against nausea and vomiting over multiple cycles of cisplatin-based chemotherapy: a combined analysis of two randomised, placebo-controlled phase III clinical trials. Eur J Cancer. 2004;40(3):403–410. doi: 10.1016/j.ejca.2003.08.028. [DOI] [PubMed] [Google Scholar]
- 195.Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, et al. Guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis. 2002;2002:730–751. doi: 10.1086/339215. [DOI] [PubMed] [Google Scholar]
- 196.Bodey GP, Buckley M, Sathe YS, Freireich EJ. Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med. 1966;64(2):328–340. doi: 10.7326/0003-4819-64-2-328. [DOI] [PubMed] [Google Scholar]
- 197.Balducci L, Hardy CL, Lyman GH. Hematopoietic growth factors in the older cancer patient. Curr Opin Hematol. 2001;8(3):170–187. doi: 10.1097/00062752-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 198.Sullivan DH, Walls RC. Impact of nutritional status on morbidity in a population of geriatric rehabilitation patients. J Am Geriatr Soc. 1994;42(5):471–477. doi: 10.1111/j.1532-5415.1994.tb04966.x. [DOI] [PubMed] [Google Scholar]
- 199.Sullivan DH. Impact of nutritional status on health outcomes of nursing home residents. J Am Geriatr Soc. 1995;43(2):195–196. doi: 10.1111/j.1532-5415.1995.tb06390.x. [DOI] [PubMed] [Google Scholar]
- 200.Sullivan DH, Walls RC, Bopp MM. Protein-energy undernutrition and the risk of mortality within one year of hospital discharge: a follow-up study. J Am Geriatr Soc. 1995;43(5):507–512. doi: 10.1111/j.1532-5415.1995.tb06097.x. [DOI] [PubMed] [Google Scholar]
- 201.Sullivan DH. The role of nutrition in increased morbidity and mortality. Clin Geriatr Med. 1995;11(4):661–674. [PubMed] [Google Scholar]
- 202.Omran ML, Morley JE. Assessment of protein energy malnutrition in older persons, part I: history, examination, body composition, and screening tools. Nutrition. 2000;16(1):50–63. doi: 10.1016/S0899-9007(99)00224-5. [DOI] [PubMed] [Google Scholar]
- 203.Thomas DR, Ashmen W, Morley JE, Evans WJ. Nutritional management in long-term care: development of a clinical guideline. Council for Nutritional Strategies in Long-Term Care. J Gerontol A Biol Sci Med Sci. 2000;55:M725–34. [DOI] [PubMed]
- 204.Bastow M, Rawlings J, Allison S. Benefits of supplementary tube feeding after fractured neck of femur: a randomised controlled trial. Br Med J. 1983;287:1589–1592. doi: 10.1136/bmj.287.6405.1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Woo J, Ho SC, Mak YT, Law LK, Cheung A. Nutritional status of elderly patients during recovery from chest infection and the role of nutritional supplementation assessed by a prospective randomized single-blind trial. Age Ageing. 1994;23(1):40–48. doi: 10.1093/ageing/23.1.40. [DOI] [PubMed] [Google Scholar]
- 206.McMurtry CT, Rosenthal A. Predictors of 2-year mortality among older male veterans on a geriatric rehabilitation unit. J Am Geriatr Soc. 1995;43(10):1123–1126. doi: 10.1111/j.1532-5415.1995.tb07012.x. [DOI] [PubMed] [Google Scholar]
- 207.Yeh S-S, Schuster MW. Treatment of cachexia in the elderly. In: Mantovani G, Anker SD, Inui A, Morley JE, Fanelli FR, Scevola D, et al., editors. Cachexia and wasting: a modern approach. link.springer.com. Milan: Springer; 2006. p. 701–17.
- 208.Brinksma A, Huizinga G, Sulkers E, Kamps W, Roodbol P, Tissing W. Malnutrition in childhood cancer patients: a review on its prevalence and possible causes. Crit Rev Oncol Hematol. 2012;83:249–75. [DOI] [PubMed]
- 209.Cole TJ. Assessment of growth. Best Pract Res Clin Endocrinol Metab. 2002;16(3):383–398. doi: 10.1053/beem.2002.0209. [DOI] [PubMed] [Google Scholar]
- 210.Wilcox WD, Nieburg P, Miller DS. Failure to thrive. A continuing problem of definition. Clin Pediatr (Phila) 1989;28(9):391–394. doi: 10.1177/000992288902800901. [DOI] [PubMed] [Google Scholar]
- 211.Jolley CD. Failure to thrive. Curr Probl Pediatr Adolesc Health Care. 2003;33(6):183–206. doi: 10.1016/S1538-5442(03)00020-8. [DOI] [PubMed] [Google Scholar]
- 212.Lai J-S, Cella D, Goldman S. 5. Anorexia/cachexia-related quality of life for children with cancer. Cancer. 2005;104(7):1531–1539. doi: 10.1002/cncr.21315. [DOI] [PubMed] [Google Scholar]


