Abstract
Background:
Among the advice on prevent cross-infection was included usage of mechanical barriers on tips of photoactivation units. However, questions about the use of protective barriers placed on the light-curing unit's tips and the possibility of interference with the ability of guaranteeing an effective polymerization of composite resins need to be clarified.
Aims:
The aim of this study was to evaluate the effect of cross infection control barriers used on the light-curing device tips on the cure depth of composite resin.
Materials and Methods:
Power density measurements from the light-cure unit were recorded with a radiometer on ten separate occasions with different types and placement modes of each barrier (low-density polyethylene and polyvinyl chloride (PVC) film – smooth and folds) and no-barrier (control). Cure depth of TPH™ Spectrum™ resin, A2-A4, was evaluated by the scraping test.
Statistical Analysis:
The data were analyzed using Student's t-test or ANOVA one-way with Tukey's test (α =0.05).
Results:
Same type of barrier and different shades (A2, A4) of composite exhibited significant difference in the cure depth among all groups (P < 0.05). Both low-density polyethylene and PVC film folded barriers produced a significant reduction in the light intensity (P < 0.05).
Conclusions:
Regarding the resin shade, there was a significant reduction in the cure depth of A4 composite resin (dark shade) but this reduction is not enough to cause any adverse effect on the material's clinical performance. Therefore, disposable barriers can be recommended for use over the end of the light guide.
Keywords: Composite resins, cure depth, infection control barriers
INTRODUCTION
Dental professionals are exposed to a great variety of microorganisms present in the blood and saliva of patients. Preventing the occurrence of cross-infection in the dental clinic is mandatory for the patient care in dentistry. The use of effective infection control procedures prevents cross-contamination in between patients and the work team.[1]
Dental clinics ought to maintain a high level of infection control to protect both patients and professionals. Among the advice on prevent cross-infecction was included usage of mechanical barriers on tips of photoactivation units, which are in direct contact with oral cavity tissues and fluids.[2,3]
The contamination of the tips of curing units is common after the clinical use.[4] With the proven concern of occupational risk and resistance of both hepatitis B virus and acquired immunodeficiency syndrome virus (human immunodeficiency virus), it is the responsibility of the dentist to observe and implement measures to prevent cross infection, and the use of mechanical barriers to cover areas and peripherals devices in the offices should be considered.[3]
The use of disposable and translucent impermeable barriers, such as polyvinyl chloride (PVC) film, on dental equipment and on the tips of light-curing units, as part of the work surface and environment care, to reduce cross-contamination is recommended.[2,3,4,5]
The tip of light-curing units is one of the critical sites in the dental office. Autoclavable tips guarantee sterility, yet autoclaving can cause a reduction in the capacity of the tip to transmit light to the tooth, losing 50% of its original value, after three autoclaving cycles.[6]
The use of a protective barrier can offer a low-cost and an efficient alternative for preventing the transmission of diseases. However, care must be taken, such as the measuring of light intensity (LI), when employing barriers.[7,8]
Incomplete polymerization can be attributed to insufficient light penetration; duration of light exposure; distance between light source and the surface of the composite resin; direction of the light; condition of the light-curing unit; and possibly, the critical value of LI that devices must emit during polymerization.[9,10] Furthermore, the type of the curing units (Light emitting diode or halogen) can affect the depth of cure of dental composites.[11] On the other side, the curing time and different polymerization modes don’t affect the effectiveness of cure, since the time recommended by manufacturers had been used.[12]
The presence of non-polymerized or partially polymerized restorative material could result in the reduction of mechanical properties and dimensional stability, as well as marginal microleakage, recurrent caries, fractures, and poor marginal adaptation of the restoration.[13]
Since questions have been raised about the use of protective barriers placed on the light-curing units tips and the possibility of interference with the ability of guaranteeing an effective polymerization of composite resins, this study was conducted to evaluate the cure depth of a microhybrid composite resin, A2 and A4 shades, using different types, and usage methods of infection control mechanical barriers on light-curing unit tips. The null hypothesis to be tested in this study was that none of the types of mechanical barriers used on light-curing device tips for controlling cross-infection have a significant effect on the suitable polymerization of composite resins, irrespective of resin shade used.
MATERIALS AND METHODS
The irradiance (mW/cm2) of the unit was measured using a manual radiometer (Curing radiometer, Demetron/Kerr, Danbury, CT, USA). Ten measurements for each group were performed, before (control group) and after placing each type of protection barrier used for controlling cross-infection, and the average of the ten values became the representative value for the LI group.
Measurement of curing depth of a composite resin (TPH™ Spectrum Universal Restorer, Dentsply, Petrópolis, RJ, Brasil-shade A2 and A4), whose organic matrix is composed of bisphenol A diglycidylmethacrylate (Bis-GMA), urethane dimethacrylate (UDMA) and ethoxylated bisphenol A glycol dimethacrylate (Bis-EMA), and inorganic matrix composed of zirconia/silica (0.01 μm and 3.5 μm), with an average size of 0.6 μm, representing 60% of the volume, was performed.
One hundred samples were produced using a nylon matrix (6 mm in diameter by 6 mm in height) and distributed randomly into ten groups (n = 10). Composite resin was inserted on bulk into matrix, interposed between two polyester strips (K-Dent Quimidrol, Joinville, Santa Catarina-Brazil) and covered with a glass slide. A 500 g weight was maintained for 30 s upon these items, avoiding the formation of dispersion layer and air bubbles, aside from promoting standardization and a smooth surface finish on both sides of the samples.
Quartz tungsten halogen lamp unit (Optilux 401 Demetron/Kerr, Danburg, Connecticut, United States of America – 600 mW/cm2), with low-density polyethylene or PVC film barriers, smooth or folded on light tip [Figure 1], was used to irradiate the samples for 40 s, using the conventional continuous method. After activation, the specimens were immediately removed from the molds and the uncured material scraped away with a plastic spatula.
Figure 1.
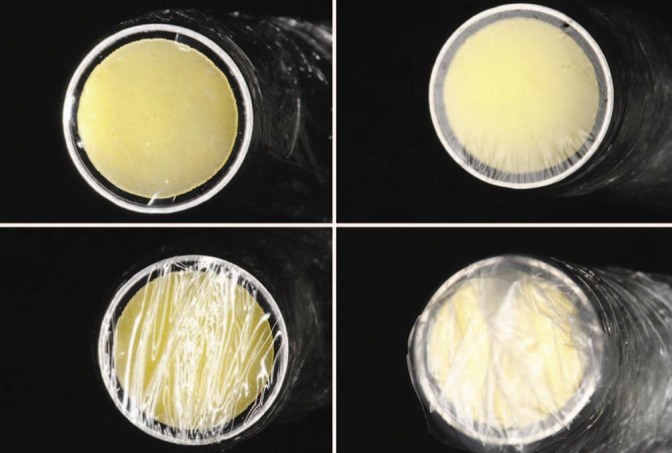
Types of cross infection control barriers tested and placing methods: (a) Smooth low density polyethylene; (b) Smooth polyvinylchloride; (c) Low density polyethylene with folds; and (d) Polyvinylchloride with folds
The non-polymerized resin was carefully removed from the non-irradiated surface (bottom) using a plastic spatula and the difference between initial thickness and thickness after scraping were measured by a micrometer, accurate to 0.01 mm, in three places and an average length was obtained. The difference between initial thickness and thickness after scraping was divided by two to obtain the depth of cure according to ISO 4049-2000.[14] Average values and standard deviations were calculated for the ISO depth cure for each material and shade.
The data were analyzed using Student's t-test or one-way factorial analysis of variance (ANOVA) with Tukey's test for pairwise comparisons between the means at the 95% confidence level. SPSS software, version 15.0 (SPSS, Chicago, IL, USA) was used for all statistical analyses.
RESULTS
The average cure depth values of each group are demonstrated in Table 1. These values were higher than those recommended by ISO 4049[14] standard for cure depth, whose quotient must be higher than 1.5 mm when each value is divided by two.
Table 1.
Average cure depth values (mm)±SD of resins tested, for each group (n=10), according to different cross infection control barriers and placement methods
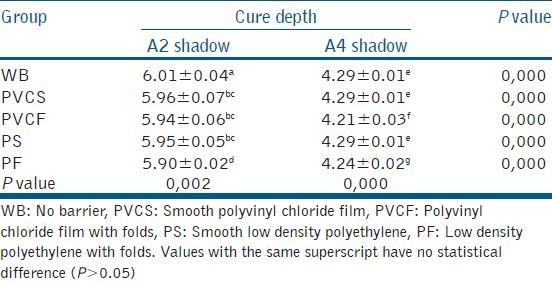
Comparing the groups of the A2 shade composite resin, there was no statistically significant difference (P > 0.05) between smooth PVC film (PVCS), PVC film with folds (PVCF) and smooth low density polyethylene (PS) groups. Between groups from A4 shade composite resin was recorded statistically lower (P < 0.05) cure depth values in folded barriers groups (PVCF and low density polyethylene with folds [PF]) than the no barrier (WB), PVCS, and PS groups.
When the groups with the same type of barrier and different shades of composite resin were observed, A4 shade groups showed significantly lower values of cure depth than the others A2 shade groups (P < 0.05).
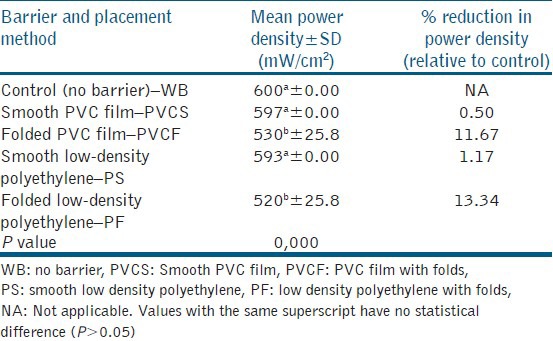
The Figure 2 shows reduction in LI after placement of different mechanical barriers. A one-way ANOVA was applied to the results to determine the effect of the different mechanical barriers on LI of light-curing device and showed that there was statistically significant difference (P < 0.05) among PVCF and PF groups when compared to the WB, PVCS, and PS groups [Table 2].
Figure 2.
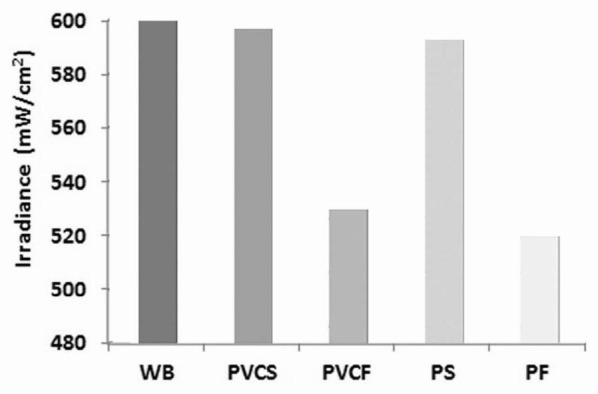
Mean light intensity values after cross infection control barriers placement. WB, No barrier; PVCS, Smooth PVC film; PVCF, PVC film with folds; PS, Smooth low density polyethylene; PF, Low density polyethylene with folds. ANOVA with Tukey's test showed significant difference (P< 0.05) among both with and without folds groups
Table 2.
Mean power density and percent reduction in power density for control (no barrier) and different cross infection control barriers and placement methods
DISCUSSION
In the present study, curing effectiveness was measured indirectly according to the ISO standard scrape test. Appropriate depth of cure is considered essential to achieve high physical properties of composite resin materials.
Mechanical barriers, which protects surfaces are an efficient means of controlling cross-infection and ought to be employed as often as possible.[3,5,15] This permits suggesting of the use of mechanical barriers on the tips of light-curing units as an alternative for infection control, since sterilizing these tips between patients results in the loss of LI.[6]
This perspective could cause uncertainties for dental professionals, since it is difficult to identify, visually, to what extent the LI can be reduced without compromising the cure depth of composite resins and/or reducing the physical and biological properties of these materials.[16]
Warren et al.[7] support that barriers are effective in controlling cross-infection, but should only be used after verifying that the LI is adequate.
Previous studies have shown that LI emitted from light-curing units is influenced by many factors, such as fluctuation in the voltage line, the condition maintenance of bulb and filter, depositing of composite resin on the tip of the device, and fractures in the fiber optic unit.[17,18,19] However, there is no concern observed among dental professionals about the possible interference of protective barriers on the polymerization of dental composites. Such attitudes should to be abolished and the scraping test should be encouraged amongst clinicians, since the procedure is simple and can be easily executed in the clinic.
In this study, it was possible to observe that protective barriers used on the tip of light-curing sources did not offer severe alterations in the LI, thus, agreeing with reports from Scott et al.[20] However, when the barriers contained folds at the site from which the light was emitted, there was a significant reduction in the LI, which could lead to an inadequate degree of polymerization when the equipment used to emit light at the minimum recommended limit of 400 mW/cm.[2,9] This reinforces the necessity of professionals to constantly observe the correct application of these barriers and the LI of the equipment that is being used. In the present study, light source, LI and composite were standardized in order to relate the polymerization depth strictly to the cross infection control barriers.
Among the other problems, associated with inadequate polymerization are inferior mechanical properties, insufficient retention of the resin to the dental substrate, higher degradation within the oral environment, aside from the presence of non-polymerized monomer in the resin, which could leak into the pulp and cause adverse responses due to its toxicity.[21]
Insufficient polymerization of the composite resin is responsible for the increase of water absorption, staining, reduction of surface hardness, recurrent caries, which can lead to the failure of the restoration.[9,13,20]
Another relevant aspect is in relation to the shade of the composite resin. Darker shades result in a lesser cure depth when compared to lighter shades.[10] The results of this study confirm this affirmation, because the average values of cure depth registered showed that the A2 shade of composite resin obtain higher values than that of the A4 shade. However, even with the use of barriers, they still remained within the clinical parameter considered for adequate polymerization, which establishes 2 mm as the maximum thickness for each increment.[22]
This study evaluated the same brand of resin composite, which is a limitation with the respect to generalizing the results. However, the aim was to show what's happens to the depth of cure when use mechanical protective barriers to control infection on the tip of the curing-light units.
The results of present study showed that both low-density polyethylene and PVC film barriers with folds on light tip produced a significant reduction in LI from the light-curing unit, acting as a light filter and consequently, diminishing the polymerization potential of composite resins. However, this reduction is not sufficient to produce adverse effects on the clinical performance of the material, seeing that in all of the groups the cure depth values were all superior to 2 mm.
Placement of disposable smooth barriers over the end of the light guide resulted in slight reduction in power density of light sources, therefore, it can be recommended for use in dental clinical practice.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Yüzbasioglu E, Saraç D, Canbaz S, Saraç YS, Cengiz S. A survey of cross-infection control procedures: Knowledge and attitudes of Turkish dentists. J Appl Oral Sci. 2009;17:565–9. doi: 10.1590/S1678-77572009000600005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. Recommended infection-control practices for dentistry, 1993. Morbity and Mortality Weekly Report. 1993;42((RR-8)):1–10. [PubMed] [Google Scholar]
- 3.Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM, et al. Guidelines for infection control in dental health-care settings – 2003. MMWR Recomm Rep. 2003;52:1–61. [PubMed] [Google Scholar]
- 4.Abreu MH, Lopes-Terra MC, Braz LF, Rímulo AL, Paiva SM, Pordeus IA. Attitudes and behavior of dental students concerning infection control rules: A study with a 10-year interval. Braz Dent J. 2009;20:221–5. doi: 10.1590/s0103-64402009000300009. [DOI] [PubMed] [Google Scholar]
- 5.Controle de Infecção na Prática Odontológica em Tempos de AIDS: Manual de Condutas. Brasília: Ministério da Saúde; 2000. Brasil. Ministério da Saúde. Secretaria de Políticas de Saúde, Coordenação Nacional de DST e Aids. [Google Scholar]
- 6.Rueggeberg FA, Caughman WF. Factors affecting light transmission of single-use, plastic light-curing tips. Oper Dent. 1998;23:179–84. [PubMed] [Google Scholar]
- 7.Warren DP, Rice HC, Powers JM. Intensity of curing lights affected by barriers. J Dent Hyg. 2000;74:20–3. [PubMed] [Google Scholar]
- 8.Williams HN, Singh R, Romberg E. Surface contamination in the dental operatory: A comparison over two decades. J Am Dent Assoc. 2003;134:325–30. doi: 10.14219/jada.archive.2003.0161. [DOI] [PubMed] [Google Scholar]
- 9.Asmussen E, Peutzfeldt A. Light-emitting diode curing: Influence on selected properties of resin composites. Quintessence Int. 2003;34:71–5. [PubMed] [Google Scholar]
- 10.Koupis NS, Vercruysse CW, Marks LA, Martens LC, Verbeeck RM. Curing depth of (polyacid-modified) composite resins determined by scraping and a penetrometer. Dent Mater. 2004;20:908–14. doi: 10.1016/j.dental.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Yaman BC, Efes BG, Dörter C, Gömeç Y, Erdilek D, Büyükgökçesu S. The effects of halogen and light-emitting diode light curing on the depth of cure and surface microhardness of composite resins. J Conserv Dent. 2011;14:136–9. doi: 10.4103/0972-0707.82613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poggio C, Lombardini M, Gaviati S, Chiesa M. Evaluation of Vickers hardness and depth of cure of six composite resins photo-activated with different polymerization modes. J Conserv Dent. 2012;15:237–41. doi: 10.4103/0972-0707.97946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knobloch L, Kerby RE, Clelland N, Lee J. Hardness and degree of conversion of posterior packable composites. Oper Dent. 2004;29:642–9. [PubMed] [Google Scholar]
- 14.Geneva, Switzerland: International Standards Organizations; 2000. International Standard 4049. Dentistry-polymer-based filling restorative and luting materials. [Google Scholar]
- 15.Oosthuysen J, Potgieter E, Blignaut E. Compliance with infection control recommendations in South African dental practices: A review of studies published between 1990 and 2007. Int Dent J. 2010;60:181–9. [PubMed] [Google Scholar]
- 16.Strydom C. Dental curing lights: Maintenance of visible light curing units. SADJ. 2002;57:227–33. [PubMed] [Google Scholar]
- 17.Dunn WJ, Bush AC. A comparison of polymerization by light-emitting diode and halogen-based light-curing units. J Am Dent Assoc. 2002;133:335–41. doi: 10.14219/jada.archive.2002.0173. [DOI] [PubMed] [Google Scholar]
- 18.Leonard DL, Charlton DG, Roberts HW, Cohen ME. Polymerization efficiency of LED curing lights. J Esthet Restor Dent. 2002;14:286–95. doi: 10.1111/j.1708-8240.2002.tb00524.x. [DOI] [PubMed] [Google Scholar]
- 19.Nitta K. Effect of light guide tip diameter of LED-light curing unit on polymerization of light-cured composites. Dent Mater. 2005;21:217–23. doi: 10.1016/j.dental.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 20.Scott BA, Felix CA, Price RB. Effect of disposable infection control barriers on light output from dental curing lights. J Can Dent Assoc. 2004;70:105–10. [PubMed] [Google Scholar]
- 21.Uhl A, Mills RW, Jandt KD. Photoinitiator dependent composite depth of cure and Knoop hardness with halogen and LED light curing units. Biomaterials. 2003;24:1787–95. doi: 10.1016/s0142-9612(02)00532-x. [DOI] [PubMed] [Google Scholar]
- 22.Van Noort R. Introduction to Dental Materials. In: O’Brien WJ, editor. 3rd ed. London: Mosby; 2007. [Google Scholar]


