Abstract
Objective
Mortality from mouth and throat cancer (MTC) is higher among Black Americans than White Americans partially because of late stage detection through screening. The disparity in mortality is particularly problematic among Black Americans living in rural areas who have limited access to preventative resources. Our study explored barriers to screening for MTC among Black Americans.
Methods
We conducted nine focus groups among rural Black Americans age 40 years and older (N = 80).
Results
Content coding of the transcripts of the focus groups revealed three primary barriers to screening. Lack of knowledge (e.g., not knowing about MTC and not knowing MTC symptoms) accounted for 31.8% of all barriers mentioned, lack of resources (e.g., lack of money and health insurance) accounted for 25.0% of all barriers mentioned, and fear (e.g., fear of screening and diagnosis) accounted for 22.9% of all barriers mentioned.
Conclusions
We placed these barriers within the Theory of Planned Behavior and conclude that interventions aimed at increasing MTC screening among rural Black Americans should first focus on changing people's attitudes about screening by increasing knowledge about MTC and reducing fear.
Introduction
Mouth and throat cancer (MTC) is any malignant cancer of the mouth (e.g., lips, tongue, and cheeks) or throat (e.g., tonsils and esophagus). These types of cancers typically develop as squamous cell carcinomas (i.e., a scale-like layer of tissue that lines the surface of the cancer site) and can spread very quickly [1]. MTC is highly treatable if caught early, and the vast majority of people diagnosed with early stage (i.e., Stage 1 or 2) MTC survive 5 years (up to 96.3%). By contrast, as few as 29.7% of people diagnosed with advanced stage MTC (i.e., Stage 3 or 4) survive 5 years [1]. Thus, the American Dental Association recommends regular screening for patients over 40 years old, especially for patients with risk factors such as tobacco use or alcohol consumption. They emphasize that early detection is essential for surviving MTC [2].
Late stage detection and treatment seem particularly problematic for Black Americans. Although Black and White Americans have similar incidence rates of MTC, Black men die from MTC at almost twice the rate of White men [1]. The discrepancy in mortality between Blacks and Whites does not primarily arise from genetic differences [3] but rather from racial disparities in health behaviors such as screening [4,5]. For instance, evidence suggests that Black Americans typically begin treatment for MTC at later stages than do White Americans, in part because the cancer is not detected early through regular screening [6–8]. This issue is particularly problematic in rural Black Americans who, compared with urban Black Americans, have limited access to preventative resources, making them more susceptible to the problems of late detection [9]. Further, Blacks living in rural areas are historically understudied and underserved. In this research, we examine barriers to screening for MTC among rural Black Americans. In doing so, we hope to identify factors that underlie differential screening rates and to inform interventions aimed at increasing screening and decreasing mortality.
Barriers to screening for other types of cancer
To our knowledge, only one study has explored the barriers that contribute to lower or delayed screening rates for MTC among Black Americans [10]. This study examined patient–provider communication about oral cancer screening and indirectly identified lack of knowledge about MTC and failed patient–provider communication as barriers to screening for Black Americans. It did not directly and comprehensively assess barriers and thus provided only a partial understanding of barriers to MTC screening among Blacks. Furthermore, the paper targeted Blacks living in a major US city, rather than rural Black Americans.
Although research on barriers to screening for MTC is limited, several studies have examined barriers to screening for other types of racially disparate cancer (e.g., colorectal cancer, prostate cancer, and breast cancer), and these studies can provide insights into possible barriers to screening for MTC [11]. These studies reveal that Black Americans often face resource barriers such as lack of insurance [12], limited access to screening services [13,14], and an inability to take time off from work [15]. Even when they have resources, many rural Black Americans report a general mistrust of physicians and the healthcare system [12], which can contribute to ignorance of risk factors [16,17], and greater anticipated pain [7] and embarrassment [18,19] from screening and other medical procedures. Religious beliefs (e.g., a belief that a higher power has willed one to have cancer) can also pose barriers to screening, particularly when they lead to fatalistic beliefs about disease outcomes or beliefs about what body parts are acceptable for examination by health professionals [15,20]. Finally, Black Americans sometimes report fear about what might be learned through screening, especially when they anticipate a poor prognosis and have limited access to treatment [14,17,19,20].
Although research documents these concerns as responsible for low screening rates for colorectal, prostate, and breast cancer among Black Americans, it remains unknown whether they are responsible for low screening rates for MTC. MTC differs from other types of cancer in important ways that may yield a different set of barriers to screening. For example, anticipated pain and embarrassment, which factor strongly in avoidance of colorectal and prostate cancer screenings [19], likely play a trivial role in screening for MTC. Similarly, although studies suggest that religious beliefs may influence the decision to receive a breast or colorectal exam [21,22], these beliefs may play little or no role in the decision to receive an MTC exam. In short, it is unclear whether the barriers to screening for colorectal and breast cancer generalize to screening for MTC.
A theoretical perspective
The research on barriers to screening for various cancers hints at a broader limitation to understanding racial disparities in health behaviors and outcomes. Namely, the research lacks a unifying framework through which to organize and evaluate the barriers to screening. Past research identifies a litany of barriers without giving thought to how the barriers are theoretically related or to tap common, underlying constructs. To our knowledge, the only attempt to view the barriers collectively sorted the barriers according to whether they stemmed from the patient, the healthcare provider, or the medical system [23]. Yet this structural approach to thinking about barriers to screening does not address the psychological mechanisms that underlie the various barriers. Lacking is a theoretical framework that would speak to the underlying mechanisms, illuminate generalities, and suggest paths to possible interventions that target the core problems that contribute to low screening rates.
The Theory of Planned Behavior (TPB) [24] offers a potential framework for understanding barriers to screening for MTC among Black Americans, as well as screening other forms of cancer. According to the TPB, behavior (in our case, screening) flows from intentions, which are the result of three factors: attitudes, subjective norms, and perceived behavioral control. An attitude has two components: (i) how positively or negatively the person views the behavior and (ii) a belief about the consequences of the behavior (e.g., whether the behavior will be effective in producing the desired outcome). People may be disinclined to undergo screening for MTC because they are unaware of MTC, do not regard it as severe, believe that screening will be ineffective, or believe that screening will not increase their chances of living longer.
The second factor, subjective norms, refers to how other people feel about the behavior and reflects social pressures to engage or not engage in a behavior. According to the TPB, people may be disinclined to undergo screening for MTC because screening is not endorsed or encouraged by trusted community leaders or because they do not value the opinion of health professionals who advocate screening. The third factor, perceived behavioral control, refers to the perceived difficulty of engaging in the behavior and reflects personal control of behavior. Accordingly, people may be disinclined to undergo screening for MTC because they believe they do not have time to see a health professional or do not have access to a health professional because of transportation or financial problems.
The TPB enjoys considerable empirical support in predicting a variety of health-focused intentions and behavior, including screening for cervical cancer [25] and breast cancer [26]. As such, it can serve as a valuable model for understanding barriers to screening for MTC and for providing a framework for developing interventions to address the barriers.
In the present study, we used the TPB as a framework for understanding barriers to MTC screening. We conducted nine focus group sessions to identify barriers to screening for MTC among rural Black Americans. We then examined how well the barriers represented the components (attitudes, subjective norms, and perceived behavioral control) of the TPB.
Method
Participants
We conducted nine focus groups (each consisting of 5 to 10 participants) in three rural counties in north-central Florida. Participants were 80 Black adults (43 women) over the age of 40 years (Mage = 56.8, SDage = 11.0). We employed a community liaison from one of the target communities who had experience recruiting similar populations to recruit participants for our study. She recruited participants from local organizations (e.g., churches and community centers) and from flyers posted in public locations. Requirements for participation were English speaking, African American, age 40 years or older, and living in one of our target counties. Participants received a $35 gift card to a local retail store for their participation. Three focus groups consisted entirely of women, three consisted entirely of men, and three were mixed gender. We had one focus group of each composition for each county. These compositions allowed us to explore gender differences in barriers identified and whether mixed-sex groups affected the general content of discussions. Multiple, manageable-sized focus groups created a setting where all members had an opportunity to voice their opinions and allowed us to examine whether a barrier was unique to a specific group or emerged in multiple groups [27,28].
We used focus group methodology for several reasons. First, we wished to impose no assumptions about what barriers deterred screening for MTC. Second, a focus group creates a context where participants can hear and comment on the ideas and responses offered by other participants. Third, in other research carried out in our health disparity center, we have found that focus groups provide a useful format for understanding how people think and feel about MTC [28].
Procedure
Prior to the first focus group, we compiled a list of 23 possible barriers to screening for MTC. The list of barriers came from research describing barriers to screening for other types of cancer (e.g., breast cancer and colon cancer) and from discussions with members of a community advisory board consisting of representatives (e.g., religious leaders, elected officials, and directors of health clinics) from the Black communities in the target counties. The list included a variety of barriers such as fear of physicians, lack of awareness about MTC, fatalistic beliefs, and lack of resources.
We held our focus group meetings at local community centers and churches in the target communities. Either the first or the second author or our community liaison—who was from one of the target communities—served as moderator for the focus groups. We adapted our procedures from other successful focus group research in similar communities [10].
During the focus group meetings, the moderator led each focus group through a discussion aimed at identifying barriers to MTC screening. The moderator defined MTC and asked whether participants had ever heard of or been screened for MTC. Next, the moderator asked participants to describe what might keep them or people like them in their community from being screened for MTC. Next, the moderator presented one by one any barriers from the list compiled prior to the focus group meetings that were not already mentioned by focus group members. The focus groups discussed whether each of these additional barriers represented barriers to screening for MTC for them or for people like them from their community.
Data reduction and analysis
We audio-recorded the focus group sessions and transcribed the recordings for analysis. Ten independent raters, all research assistants on the project, read the transcripts and identified barriers to MTC screening. The raters independently generated a variety of possible broader categories for sorting the barriers. The raters and the primary investigators then evaluated each of the structures and agreed on the simplest and most-clear structure. The final result included seven broad categories (i.e., lack of knowledge, lack of resources, fear, lack of symptoms, pride, fatalism, and other). The investigators then placed each of these categories within the framework of the TPB (Table 1). It is important to note that we did not initially ask raters to code the data for the presence of the three TPB components because we wanted to eliminate the possibility of expectancy effects. That is, if raters expected certain barriers to emerge, they might have ignored alternative barriers that disconfirmed our hypotheses. Within each category, raters included subcategories that represented common barriers identified within each category. For example, subcategories in the lack of resources category included lack of time, transportation, money, and health insurance, as well as having ‘bigger problems’ in one's life. In the Results section, we describe only the subcategories acknowledged by every focus group at least once.
Table 1.
Categories identified by content coders
| Category | Example statement(s) | Theory of Planned Behavior predictor | Mean mentions per group | % of all barriers |
|---|---|---|---|---|
| 1 Lack of knowledge | ‘Most people just don't know anything about MTC.’ ‘My doctor's never said nothing about MTC.’ | Attitudes, subjective norms | 14.0 | 38 |
| 2 Lack of resources | ‘A lot of people just don't have money for exams.’ | Behavioral control | 9.4 | 25 |
| 3 Fear | ‘I can't deal with being diagnosed with [MTC].’ | Attitudes | 8.6 | 23 |
| 4 Lack of symptoms | ‘I don't have any MTC symptoms, so I don't need to get checked.’ | Attitudes | 2.6 | 7.1 |
| 5 Pride | ‘I don't like doctors telling me what I need to do.’ | Attitudes | 1.0 | 2.7 |
| 6 Fatalism | ‘God's [going to] do what he wants.’ | Attitudes | 0.8 | 2.1 |
| 7 Other | ‘I don't want to have to go to the clinic.’ | N/A | 0.8 | 2.1 |
MTC, mouth and throat cancer.
Nine new raters, who were also research assistants for the project, then coded the content of the transcripts. Each of the nine raters coded three different focus groups, and each focus group had three raters. We counterbalanced transcript assignments so that no two raters worked together more than once. Raters coded the number of times participants noted each category or subcategory as a barrier to screening for MTC. Table 2 shows the intraclass correlations between all three raters for each group and indicates that raters reliably identified a similar number of barriers and sub-barriers both within each group (average ICC = .85) and across groups (ICC = .74). The raters identified no differences in types of barriers identified as a function of group composition. Because analysis revealed consistency in the proportion of each type of barrier across groups (α = .97), we averaged group data to examine sample-level trends in barrier identification.
Table 2.
Intraclass correlations (ICC) for ratings in each group
| 95% confidence interval |
|||
|---|---|---|---|
| Group | ICC | Lower | Upper |
| 1 | 0.92 | 0.87 | 0.95 |
| 2 | 0.83 | 0.74 | 0.89 |
| 3 | 0.68 | 0.53 | 0.79 |
| 4 | 0.90 | 0.85 | 0.94 |
| 5 | 0.93 | 0.90 | 0.96 |
| 6 | 0.72 | 0.58 | 0.81 |
| 7 | 0.91 | 0.86 | 0.94 |
| 8 | 0.79 | 0.70 | 0.86 |
| 9 | 0.94 | 0.91 | 0.96 |
| Average | 0.85 | 0.77 | 0.90 |
Importantly, our primary goal was to describe the predominant barriers to MTC screening rather than to simply describe the content of the focus group discussions. Thus, we analyzed the frequency with which participants mentioned each barrier category and subcategory, allowing us to quantify the importance of each barrier.
Results
Our raters identified 40 barrier subcategories: 18 were on our original list of barriers and 22 were participant generated. Overall, 86% of the barriers mentioned fell into the categories lack of knowledge, lack of resources, or fear (see Table 1 for a comparison of frequencies; see Table 3 for a description of the subcategories comprising these categories; both tables include example quotes from participants). Of the remaining four categories, three (i.e., pride, fatalism, and other) accounted for less than 3% of the barriers identified, and lack of symptoms accounted for only 7% of the barriers identified. Because these remaining four categories appeared to play a minor role in deterring screening, we do not discuss them further.
Table 3.
Primary subcategories
| Category | Example statement | Theory of Planned Behavior Predictor | Mean mentions per group | % of categorya |
|---|---|---|---|---|
| Lack of knowledge | ||||
| Ignorance of MTC | ‘I don't really know anything about [MTC].’ | Attitudes | 3.9 | 27 |
| Important others never mention it | ‘We've never actually discussed [MTC] as long as he's been my doctor.’ | Subjective norms | 2.9 | 20 |
| Ignorance of symptoms | ‘Well, I don't have any idea what the symptoms are.’ | Attitudes | 1.8 | 13 |
| Lack of resources | ||||
| Lack money | ‘[You] can't get tested for stuff if you ... got no money.’ | Behavioral control | 3.5 | 37 |
| Lack insurance | ‘The first thing doctors ask is “do you have insurance?” If you say “no”, they say “bye”.’ | Behavioral control | 1.5 | 16 |
| Lack of transportation | ‘I take my sister everywhere she go[es], she [doesn't] have a car.’ | Behavioral control | 1.4 | 15 |
| Have bigger problems | ‘I've got diabetes; I can't be having [MT] cancer too.’ | Behavioral control | 1.2 | 13 |
| Lack time | ‘I'd have to schedule time off to go get checked.’ | Behavioral control | 1.2 | 12 |
| Fear of ... | ||||
| Results | ‘They may be afraid to find out they have [MTC].’ | Attitudes | 2.4 | 37 |
| Physicians | ‘The dentist ... terrifies me.’ | Attitudes | 1.9 | 21 |
| Screening | ‘It might hurt to have [a MTC screening] done.’ | Attitudes | 1.0 | 12 |
| Coping with a diagnosis | ‘I don't want to have to deal with knowing I have [MTC].’ | Attitudes | 1.0 | 12 |
Only subcategories that emerged at least once per group are included in this table; thus, percentage totals will sum to less than 100%.
MTC, mouth and throat cancer.
As Table 1 shows, lack of knowledge was the most common barrier to emerge, with participants mentioning it an average of 14.0 times per focus group and accounting for 38% of all barriers mentioned. As evident in Table 3, three major subcategories emerged: (i) ignorance of MTC; (ii) important others never mentioning MTC; and (iii) ignorance of symptoms of MTC. Within the TPB framework, the first and third subcategories represent attitudes, whereas the second subcategory represents subjective norms.
Lack of resources was the second most common barrier identified, with participants mentioning it an average of 9.4 times per focus group and accounting for 25% of all barriers mentioned. As Table 3 shows, five subcategories emerged: (i) lack of money; (ii) lack of insurance; (iii) lack of transportation; (iv) having bigger problems; and (v) lack of time. Within the TPB framework, all subcategories represent perceived behavioral control.
Fear was the third most common barrier identified, with participants mentioning it an average of 8.6 times per focus group and accounting for 23% of all barriers mentioned. As seen in Table 3, four subcategories emerged: (i) fear of the results; (ii) fear of physicians; (iii) fear of screening; and (iv) fear of coping with a diagnosis. Within the TPB framework, all subcategories represent attitudes.
Although we are aware of the possibility that the list of barriers that we compiled in advance may have influenced the final list of barriers that we gleaned from the focus groups, we think it unlikely for two reasons. First, the majority of barriers we compiled in advance were rarely mentioned by participants. Second, over half of the final barriers were participant generated; they were not on the list we compiled.
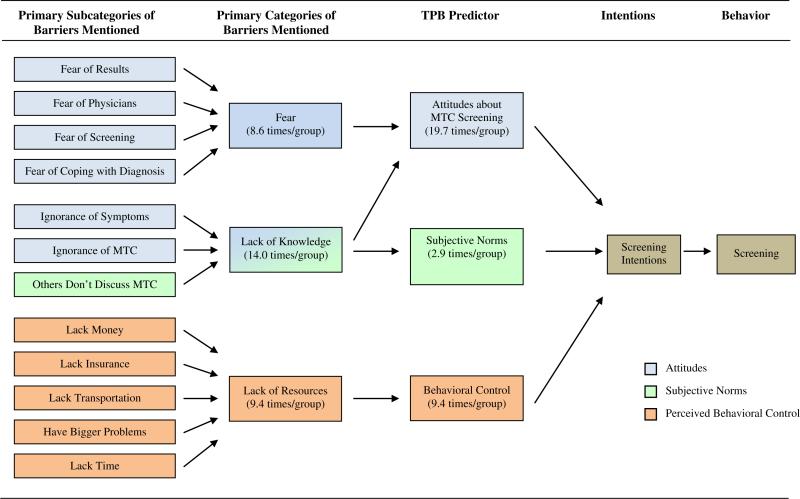
Theory of Planned Behavior
As Figure 1 shows, all the barriers discussed by participants can be placed within the TPB. However, participants primarily identified barriers pertaining to attitudes about MTC screening (seven barriers mentioned on average 19.7 times per group), followed by behavioral control (five barriers mentioned on average 9.4 times per group) and subjective norms (one barrier mentioned on average 2.9 times per group). Of note, the subcategories that comprised the category lack of knowledge represented a mix of attitudes (two-thirds of the barriers) and subjective norms (one-third of the barriers), indicating that each of the primary barriers identified did not track onto one specific TPB predictor.
Figure 1.
Primary barriers within the Theory of Planned Behavior (TPB) framework
Discussion
Content analysis of the discussions of nine focus groups of rural Black American participants identified three primary barriers to MTC screening. The foremost barrier, the lack of knowledge, included both a general lack of knowledge about MTC and symptoms as well as feelings that important others (one's doctor or one's family) had not discussed MTC screening. The second biggest barrier, lack of resources, consisted of a lack of time, money, insurance, and transportation, and the presence of bigger problems than MTC. The third barrier was fear, which consisted of fear of the results, fear of screening, fear of physicians, and fear of coping with a diagnosis. Considered within the framework of the TPB, these barriers constitute attitudes, subjective norms, and perceived behavioral control.
The ultimate goal of this research is to inform interventions that will increase screening for MTC among rural Black Americans. Our findings suggest that intervention should address first the lack of knowledge of MTC. For most of our participants, MTC is not on the radar. They have never heard of it and therefore regard it as relatively unimportant, because physicians, dentists, and other people in their community do not talk about it. As one participant noted, she hears in the media about breast cancer but never hears anyone talking about MTC. If health professionals want to increase screening for MTC, they must increase awareness of MTC. Importantly, addressing this first barrier is tied closely with addressing the second and third barriers to screening at the same time. Specifically, interventions designed to address the resource and fear barriers require that people be aware of MTC in the first place.
Perhaps the most important contribution of the present work comes from framing these barriers in terms of the TPB. Researchers across a variety of health domains have used TPB-based interventions to promote healthy behaviors, such as screening [29,30]. By placing our findings in the TPB, the present study offers an initial step in linking MTC screening to health promotion behaviors broadly. Thus, health professionals who wish to increase MTC screening rates can target their efforts toward fostering positive attitudes about screening using a TPB framework.
Like all research, our investigation has limitations. First, our analyses are primarily qualitative and based on the responses of participants in focus groups. It remains to be seen whether our findings will be replicated using quantitative methodology. However, we viewed the use of focus groups as an essential first step in the identification of the barriers to screening, a necessary step before pursuing other methods of scientific inquiry. Second, using focus groups allowed us to identify the barriers that our participants viewed as most deterring to screening for MTC. Nevertheless, without experimental investigation, it is unknown whether these self-identified barriers truly deter screening for MTC in our target population. Third, our findings are based on the focus group discussions of rural Black Americans in north-central Florida. We do not know whether the barriers we identify generalize to other populations in other locales. Finally, although the TPB offers a useful theoretical framework for understanding personal barriers to screening, it is not the only available theoretical framework. An alternative framework, the PEN-3 model of health behavior, emphasizes the role of culture in behavior and proposes culturally sensitive interventions to increase health-promoting behaviors, such as screening. Using this type of framework would broaden our focus to more community-level barriers to screening, rather than individual-level barriers.
Earlier, we noted a disparity between Black and White Americans in mortality for MTC that arises in part from delayed detection of MTC through screening. Our investigation reveals three primary barriers to screening for MTC among at-risk rural Black Americans: a lack of knowledge, a lack of resources, and fear. The task now facing investigators is to develop interventions that address these barriers to address the Black–White mortality discrepancy.
Acknowledgements
This work was supported by the National Institute of Dental and Craniofacial Research at the National Institutes of Health. HLOGAN PI 1U54DEO19261-01. All participants were treated according to APA guidelines for the treatment of human participants.
Footnotes
Conflict of interest
The authors have no conflicts of interest with respect to this article.
References
- 1.Piccirillo JF, Costas I, Reichman ME. Cancers of the head and neck. In: Ries LAG, Young LF, Keel GE, Eisner MP, Lin YD, Horner MJ, editors. SEER Survival Monograph: Cancer Survival among Adults: U.S. SEER Program, 1988–2001, Patient and Tumor Characteristics. National Cancer Institute; Bethesda, MD: 2007. [Google Scholar]
- 2.Rethman MP, Carpenter W, Cohen EE, et al. Evidence-based clinical recommendations regarding screening for oral squamous cell carcinomas. J Am Dent Assoc. 2010;141:509–520. doi: 10.14219/jada.archive.2010.0223. [DOI] [PubMed] [Google Scholar]
- 3.Worsham MJ, Divine G, Kittles RA. Race as a social construct in head and neck cancer outcomes. Otolaryngol Head Neck Surg. 2011;144:381–389. doi: 10.1177/0194599810393884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moore RJ, Doherty DA, Doherty DF, Do KA, Chamberlain RM, Khuri FR. Racial disparity in survival of patients with squamous cell carcinoma of the oral cavity and pharynx. Ethn Health. 2001;6:165–177. doi: 10.1080/13557850120078099. [DOI] [PubMed] [Google Scholar]
- 5.Horner M, Ries LAG, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2006. National Cancer Institute; Bethesda, MD: 2009. [Google Scholar]
- 6.Murdock JM, Gluckman JL. African-American and white head and neck carcinoma patients in a university medical center setting. Are treatments provided and are outcomes similar or disparate? Cancer. 2001;91:279–283. doi: 10.1002/1097-0142(20010101)91:1+<279::aid-cncr19>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 7.Madlensky L, Esplen MJ, Goel V. Reasons given by relatives of colorectal cancer patients for not undergoing screening. Prev Med. 2004;39:643–648. doi: 10.1016/j.ypmed.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Carroll WR, Kohler CL, Carter VL, Hannon L, Skipper JB, Rosenthal EL. Barriers to early detection and treatment of head and neck squamous cell carcinoma in African American men. Head Neck. 2009;31:1557–1562. doi: 10.1002/hed.21125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang P, Tao G, Irwin KL. Utilization of preventive medical services in the United States: a comparison between rural and urban populations. J Rural Health. 2000;16:349–356. doi: 10.1111/j.1748-0361.2000.tb00485.x. [DOI] [PubMed] [Google Scholar]
- 10.Choi Y, Dodd V, Watson J, Tomar SL, Logan HL, Edwards H. Perspectives of African Americans and dentists concerning dentist–patient communication on oral cancer screening. Patient Educ Couns. 2008;71:41–51. doi: 10.1016/j.pec.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Ries LAG, Melbert D, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2005, Section 16: Melanoma of the Skin. National Cancer Institute; Bethesda: 2008. [Google Scholar]
- 12.Fyffe DC, Hudson SV, Fagan JK, Brown DR. Knowledge and barriers related to prostate and colorectal cancer prevention in underserved Black men. J Natl Med Assoc. 2008;100:1161–1167. doi: 10.1016/s0027-9684(15)31478-4. [DOI] [PubMed] [Google Scholar]
- 13.Beeker C, Kraft JM, Goldman R, Jorgensen C. Strategies for increasing colorectal cancer screening among African Americans. J Psychosoc Oncol. 2001;19:113–132. [Google Scholar]
- 14.Forrester-Anderson IT. Prostate cancer screening perceptions, knowledge, and behaviors among African American men: focus group findings. J Health Care Poor Under-served. 2005;16:22–30. doi: 10.1353/hpu.2005.0122. [DOI] [PubMed] [Google Scholar]
- 15.Moy B, Park ER, Feibelmann S, Chiang S, Weissman JS. Barriers to repeat mammography: cultural perspectives of African-American, Asian, and Hispanic women. Psycho-Oncology. 2006;15:623–634. doi: 10.1002/pon.994. [DOI] [PubMed] [Google Scholar]
- 16.Messina CR, Kabat GC, Lane DS. Perceptions of risk factors for breast cancer and attitudes toward mammography among women who are current, ex- and non-smokers. Women Health. 2002;36:65–82. doi: 10.1300/J013v36n03_05. [DOI] [PubMed] [Google Scholar]
- 17.Wray RJ, McClure S, Vijaykumar S, et al. Changing the conversation about prostate cancer among African Americans: results of formative research. Ethn Health. 2009;14:27–43. doi: 10.1080/13557850802056448. [DOI] [PubMed] [Google Scholar]
- 18.Friedemann-Sanchez G, Griffin JM, Partin MR. Gender differences in colorectal cancer screening barriers and information needs. Health Expect. 2007;10:148–160. doi: 10.1111/j.1369-7625.2006.00430.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greiner KA, Born W, Nollen N, Ahluwalia JS. Knowledge and perceptions of colorectal cancer screening among urban African Americans. J Gen Intern Med. 2005;20:977–983. doi: 10.1111/j.1525-1497.2005.00165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peek ME, Sayaa JV, Markwardt R. Fear, fatalism and breast cancer screening in low-income African-American women: the role of clinicians and the health care system. J Gen Intern Med. 2008;23:1847–1853. doi: 10.1007/s11606-008-0756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Azaiza F, Cohen M. Health beliefs and rates of breast cancer screening among Arab women. J Women's Health. 2006;15:520–530. doi: 10.1089/jwh.2006.15.520. [DOI] [PubMed] [Google Scholar]
- 22.Husaini BA, Emerson JS, Hull PC, Sherkat DE, Levine RS, Cain VA. Rural–urban differences in breast cancer screening among African American women. J Health Care Poor Underserved. 2005;16:1–10. doi: 10.1353/hpu.2005.0124. [DOI] [PubMed] [Google Scholar]
- 23.Womeodu RJ, Bailey JE. Barriers to cancer screening. Med Clin North Am. 1996;80:115–133. doi: 10.1016/s0025-7125(05)70430-2. [DOI] [PubMed] [Google Scholar]
- 24.Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckman J, editors. Action-Control: From Cognition to Behavior. Springer-Verlag; Berlin: 1985. pp. 11–39. [Google Scholar]
- 25.Duffett-Leger LA, Letourneau NL, Croll JC. Cervical cancer screening practices among university women. J Obstet Gynecol Neonatal Nurs. 2008;37:572–581. doi: 10.1111/j.1552-6909.2008.00276.x. [DOI] [PubMed] [Google Scholar]
- 26.Rutter DR. Attendance and reattendance for breast cancer screening: a prospective 3-year test of the Theory of Planned Behaviour. Br J Health Psychol. 2000;5:1–13. [Google Scholar]
- 27.Kruger R, Casey M. Focus Groups: A Practical Guide for Applied Research. Sage; Thousand Oaks, CA: 2009. [Google Scholar]
- 28.Dodd VJ, Riley JL, Muller KE, Guo YI, Logan HL. Developing an oral and pharyngeal cancer (OPC) knowledge and behavioral survey. Am J Health Behav. 2012;36:12. doi: 10.5993/AJHB.36.5.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Godin G, Kok G. The theory of planned behavior: a review of its applications to health-related behaviors. Am J Health Promot. 1996;11:87–98. doi: 10.4278/0890-1171-11.2.87. [DOI] [PubMed] [Google Scholar]
- 30.Orbell S. Medical Adherence and Aging: Social and Cognitive Perspectives. American Psychological Association; Washington, DC, US: 2007. Motivational models and volitional processes in the promotion of health behaviors. pp. 169–200. [Google Scholar]