Abstract
Adverse health and productivity outcomes have imposed a considerable economic burden on employers. To facilitate optimal worksite intervention designs tailored to differing employee risk levels, the authors established cutoff points for an Individual Well-Being Score (IWBS) based on a global measure of well-being. Cross-sectional associations between IWBS and adverse health and productivity outcomes, including high health care cost, emergency room visits, short-term disability days, absenteeism, presenteeism, low job performance ratings, and low intentions to stay with the employer, were studied in a sample of 11,702 employees from a large employer. Receiver operating characteristics curves were evaluated to detect a single optimal cutoff value of IWBS for predicting 2 or more adverse outcomes. More granular segmentation was achieved by computing relative risks of each adverse outcome from logistic regressions accounting for sociodemographic characteristics. Results showed strong and significant nonlinear associations between IWBS and health and productivity outcomes. An IWBS of 75 was found to be the optimal single cutoff point to discriminate 2 or more adverse outcomes. Logistic regression models found abrupt reductions of relative risk also clustered at IWBS cutoffs of 53, 66, and 88, in addition to 75, which segmented employees into high, high-medium, medium, low-medium, and low risk groups. To determine validity and generalizability, cutoff values were applied in a smaller employee population (N=1853) and confirmed significant differences between risk groups across health and productivity outcomes. The reported segmentation of IWBS into discrete cohorts based on risk of adverse health and productivity outcomes should facilitate well-being comparisons and worksite interventions. (Population Health Management 2013;16:90–98)
Introduction
Health care cost and lost productivity have created a significant economic burden for employers.1–5 Studies estimate that chronic conditions may comprise 10.7% of a company's total labor cost4 and that the total cost of presenteeism alone in United States accounted for more than $150 billion per year.6 To reduce cost burden in the long term, more than one third of employers in the United States currently provide health and wellness interventions to employees that are designed to promote health and well-being outcomes.7 There is evidence to indicate that workplace interventions are effective at targeting multiple health and productivity outcomes including improving healthy behaviors,8–10 physical health,11,12 mental health,13–15 disability,16 and preventing absenteeism,17–19 presenteeism,15,17 and employee turnover.20,21
Although many employers are now increasingly concerned about the cost burden driven by health care and loss of productivity, the major focus behind their efforts is to prevent disease and slow the progression of chronic conditions. Commonly used workplace assessment tools such as the Health and Work Performance Questionnaire (HPQ)22 and the Work Productivity and Activity Impairment Questionnaire were created based on this perspective. Health status, however, is not merely the absence of diseases. The World Health Organization has defined health as “a state of complete physical, mental, and social well-being.” Not by coincidence, this is a broad, holistic definition of the human condition. The social sciences, epidemiology, and even the biological sciences have demonstrated strong interaction between the multiple factors of environment, personality, experience, and genetic makeup. Humans and their health are far more than the sum of their parts. Publications following this comprehensive definition of well-being have demonstrated that well-being is significantly correlated with health and productivity outcomes.23,24 Specific assessment tools have attempted to measure well-being by incorporating multiple aspects of health at a more holistic level; for example, the Quality of Well-Being Scale25 that considers mobility, physical activity, mental health, and symptom status, the Göteborg Quality of Life Instrument26 that evaluates symptoms and well-being, and the Complaint Score27 that measures perceptions of well-being. However, these measures are still used mostly to measure conventional health outcomes, and little is known about the association of these measures with workplace-specific outcomes such as absenteeism, presenteeism, and job performance.
The Well-Being Assessment (WBA) provides a comprehensive measure of individual overall well-being, with the ability to link well-being to human performance. The Individual Well-Being Score (IWBS), derived from the WBA, captures the health and productivity risks that are predictive of outcomes relevant to employers. For example, the independent association of high IWBS with decreased risk of health care claims cost and utilization in employers has been established in recent literature.28 Such predictive capability has made the IWBS a potentially useful tool to guide optimal well-being worksite intervention designs and to measure well-being as a program outcome that is meaningful to employers through its association with health care costs and productivity.
Despite its potential use, IWBS has not been associated with stratified levels of worksite interventions. The major challenge comes from the fact that IWBS is a continuous scale, limiting the possibility of selecting employees for these discrete programs. Classifications of continuous anthropometric indicators have been employed widely in medical science to predict health risks. A well-known example is the use of body mass index—measured by height and weight to indicate underweight, normal weight, overweight, and obesity status—that is associated with different levels of diseases and conditions.29 The classification for comprehensive indicators derived from surveys, however, has not been broadly explored when attempting to link it to the risks of a particular adverse health- or productivity-related outcome. As a first attempt, this study provides empirical evidence for the nonlinear relationship between IWBS and employer-concerned outcomes. The continuous IWBS was classified into actionable segments that are associated with different levels of health and productivity risks in an employee population. The results that will be described have implications for worksite intervention design and health and productivity research.
Methods
Sample
Employees from a large commercial insurance company (Employer A) in the United States were invited to participate in a self-administered electronic survey of WBA between June 1, 2010 and July 31, 2010. The sample included 11,702 employees, representing approximately 35% of the total employee population. Characteristics of the study sample of Employer A: 36.2% were male; median age was 45 years; 35.3% held a high school diploma or lower, 54.8% had earned an undergraduate degree, and the rest (9.9%) had a master's degree or above; 63.9% were married.
Measures
In this study, the independent variable used was the IWBS derived from the WBA. The dependent variables analyzed were 7 measures of health and productivity outcomes including health care cost, health care utilization, short-term disability, absenteeism, presenteeism, job performance, and job retention. This broad range was considered to cover major sources of economic burdens pertaining to health and productivity for employers.
Individual Well-Being Score
The WBA was adapted from the Gallup-Healthways Well-Being Index (WBI), an ongoing, large-scale national representative survey originally developed to assess the well-being status of the general US population at the group level. The WBI measures 6 broad conceptual domains that encompass evaluative and experienced well-being, including physical health, emotional health, healthy behaviors, work environment, basic access, and life evaluation. Detailed information on WBI survey design and validity has been reported elsewhere.23,30 A brief summary of the questions asked in each domain follow:
Physical health
Evaluates peoples' perceptions and understanding of their physical health, including chronic illness diagnoses, experience of pain, sick days, and any health problems preventing them from doing normal activity.
Emotional health
Asks people about their positive and negative experiences and emotions.
Healthy behaviors
Contains questions on healthy diet and physical activity behaviors.
Work environment
Assesses employees' perceptions of the workplace and job satisfaction.
Basic access
Evaluates access to recourses in 3 areas: financial ability to afford basic needs, community quality, and health care access.
Life evaluation
Assesses how a person evaluates his or her life now and in the future.
The WBA adopts all questions from the 6 domains of WBI with additional depth of measurement on health risks and employee productivity and has adapted scoring for individual-level analysis of employee responses. Based on 40 original WBI questions, an IWBS was computed by weighting scores from each of the 6 domains equally; each domain score ranges from 0 (lowest possible well-being) to 100 (highest possible well-being) for each respondent. The IWBS has been found to have acceptable reliability and construct validity.31
Health costs and utilization measures
Employee health costs and utilization were generated from administrative claims data provided by insurers. The claims data contained individual claim-level information, including benefit plan enrollment, inpatient and outpatient health care utilization, and insurer's paid cost for services, pharmaceutical claims and costs, and short-term disability paid (STDP) days and costs. The individual claim-level records were rolled up into 12-month periods to represent individual total costs and health care utilization for the year preceding WBA administration. Three health outcomes measures were analyzed in this study: total claims cost (sum of medical expenses paid by insurer and prescription drug cost paid by insurer), emergency room (ER) visits, and annual STDP days. No attempt was made to examine hospital admissions and number of bed days because of the relative rarity of these events.
Productivity measures
Productivity was measured in 3 ways: absenteeism, presenteeism, and job performance.
Absenteeism
The absenteeism question was incorporated directly from the HPQ,22 which asks “In the past 4 weeks (28 days), how many days did you miss an entire work day because of problems with your physical or mental health?”
Presenteeism
Presenteeism was assessed using Well-Being Assessment for Productivity (WBA-P),32 a survey instrument evaluating productivity loss related to a range of personal and work-related barriers. It captures the frequency with which 11 potential barriers reduce one's working capability. The stem question asks, “During the past 4 weeks (28 days), how often have you had trouble at work concentrating or doing your best because of …”, followed by the 11 potential barriers. Response options include “not at all,” “some,” or “a lot,” which were keyed and computed into 1 summary score that ranged from 0 (“not at all” for all 11 reasons) to 100 (“a lot” for all 11 reasons).
Job performance
Employees reported their own job performance using the 0-to-10 global work performance rating scale found in the HPQ.22 The question asks, “On a ladder from 0 to 10 where 0 is the worst job performance anyone could have at your job and 10 is the performance of a top worker, how would you rate your overall job performance on the days you worked during the past 4 weeks (28 days)?”
Job retention measure
Intent to stay
An intent-to-stay score measured employees' perception of the likelihood of job continuation with Employer A. It was a summary score of 3 intent-to-stay questions, ranging between 0 and 100. This survey instrument was a proprietary tool developed and deployed by the employer, and was used as a part of their normal business and human resource operations.
Statistical procedures
Health and productivity measures for Employer A were coded into binary values where 0 represented a desired outcome and 1 represented an adverse outcome. For bell-shaped continuous variables that were not heavily skewed (claims cost conditional on having positive cost, WBA-P score, HPQ self-rated performance score, and intent-to-stay score), values at the population median were used to dichotomize the population into high (outcome value=1) and low (outcome value=0) risk groups, while variables with mass zeros (ER visits, STDP days, and self-report absence days) defined an adverse outcome (outcome value=1) if the value of the variable was positive. Optimal IWBS cutoff values were determined using the following 3 steps:
First, the association between IWBS and grouped adverse outcomes was examined by using a receiver operating characteristic (ROC) curve. Seven adverse outcomes were added together to obtain a total health and productivity risk score, including high claims cost, any ER visit, any STDP days, any self-reported absence days, high WBA-P score, low HPQ self-rated performance score, and low intent-to-stay score. The highest possible total health and productivity risk score for an employee was 7 and the lowest possible score was 0. An individual was defined as high risk if he or she had a total risk score of 2 or more. A ROC curve was then generated to obtain a single optimal cutoff point of IWBS in predicting high health and productivity risks. The trade-off between sensitivity and specificity was shown on the curve. Sensitivity was calculated as an index indicating the ability to correctly identify true cases with 2 or more adverse outcomes, and specificity suggested the ability to correctly identify true non-cases with less than 2 adverse outcomes. Diagnostic accuracy was measured by the area under the curve (AUC). The IWBS point that minimized the distance from the upper-left corner to the point on the ROC curve, computed by the square root of [(1-sensitivity)2+(1-specificity)2], and maximized Youden's index measured by [(sensitivity+specificity)−1], determined the optimal single threshold cutoff score for predicting high health and productivity risks. Separate ROC curves were plotted for male and female employees in order to assess the need for selecting cutoff points specific to either sex.
In the second step, cutoffs for multiple population segments were identified using a series of logistic regression models in addition to the single threshold identified by the ROC curves. Although ROC curve analysis has been widely adopted in medicine, its use is limited when applied to more than one cutoff value or when diagnosing more than 1 outcome (the goal of this study). The authors proposed that multiple cutoff values were more appropriate in the present study, because finer classification facilitates optimal worksite intervention designs that are tailored to an employee population at particular risk levels. Furthermore, basing cutoff values on the odds of multiple outcomes (as opposed to only 1 outcome) makes the segmentation more robust to any potential noise in 1 given outcome; it also becomes more relevant to employers seeking to align well-being measures with actual business and individual human performance. Logistic regression models have the ability to compute relative risk of adverse health and productivity outcomes over the entire range of IWBS, and therefore make the selection of multiple cutoff points for multiple outcomes possible. IWBS distribution was not uniform and the sample size of some extremely rare IWBS points was very small (less than 10 observations). Instead of calculating relative risk of adverse outcomes for each IWBS point, IWBS were grouped into segments in an interval of 4 percentiles, resulting in a total of 25 percentile segments for the analysis. The highest percentile segment (96–100) was used as the reference group in the regression. Regression analyses were repeated for each of 7 adverse health and productivity outcomes. Odds ratio (OR) results for 7 outcomes across 25 percentile segments were plotted on the same graph. The most appropriate potential cutoff points should fall in the percentile segments in which the risks for adverse health and productivity outcomes jointly and rapidly decreased. Cutoff points were then identified as the median values of the percentile segments in which abrupt and significant reductions in relative risks were found. The logistic regression model also accounted for sociodemographic characteristics including age, sex, marital status (married or not), and education categories (high school diploma or lower, college degree, master's degree or above).
In the final step, a separate sample (Employer B) was used to test the performance of the previously identified IWBS cutoff values in distinguishing high health and productivity risks. Employees in Employer B were classified into different risk groups based on IWBS cutoffs obtained from the first 2 steps. The relative risks across risk groups for high claims cost, any ER visits, low self-rating of performance, high presenteeism, and any absences were computed using logistic regression. STDP and intent-to-stay data were not available for Employer B. The significance of the differences in the relative risks was assessed using a 1-way Analysis of Variance (ANOVA) omnibus F test.
SAS Enterprise Guide (SAS Institute Inc., Cary, NC) statistical software was used for the statistical analysis. A P value <0.01 was considered statistically significant.
Results
Summary statistics of study sample (Employer A)
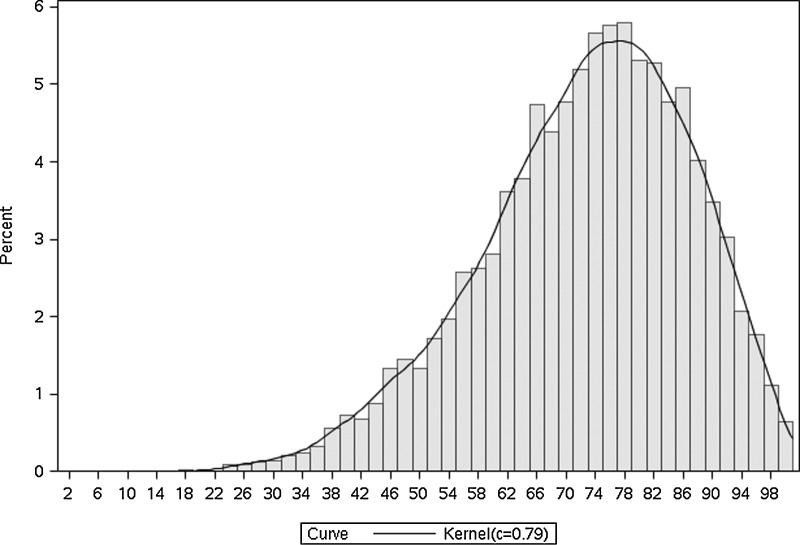
The average IWBS among the 11,702 employees in Employer A was 72.72, with a standard deviation of 14.24. The Kernel density distribution of IWBS was plotted in Figure 1. The distribution of IWBS had a slightly longer tail on the left-hand side, but was approximately bell-shaped.
FIG. 1.
Kernel Density Distribution of Individual Well-Being Score in Employer A.
Health and productivity measures are summarized in Table 1 in their raw scales.
Table 1.
Summary Statistics of Individual Well-Being Score and Health and Productivity Outcomes Measures in Employer A (n=11,702)
| Mean | Standard Deviation | Median | Minimum | Maximum | Percentage with Adverse Outcome | |
|---|---|---|---|---|---|---|
| Individual Well-Being Score | 72.72 | 14.24 | 74.16 | 10.83 | 100 | |
| Health measures | ||||||
| Claims cost ($)*# | 3725.43 | 12528.63 | 1100.36 | 0.03 | 563796.44 | 28.37% |
| Emergency room visits* | .075 | .37 | 0 | 0 | 13 | 5.64% |
| Short-term disability paid days* | 1.82 | 8.08 | 0 | 0 | 95 | 7.98% |
| Productivity measures | ||||||
| Subjective absenteeism: self-reported health-related absent days¥ | 0.51 | 2.05 | 0 | 0 | 28 | 47.16% |
| Subjective presenteeism: summary score of WBA-P¥ | 17.98 | 14.95 | 13.63 | 0 | 99.99 | 47.50% |
| Subjective job performance: HPQ work performance score¥ | 8.41 | 1.24 | 9 | 0 | 10 | 18.11% |
| Retention measures | ||||||
| Intent to stay | 50.06 | 46.31 | 66.67 | 0 | 100 | 48.88% |
| Total risk score | 1.97 | 1.29 | 2 | 0 | 7 | 60.92% |
Reference period: 12 months before WBA survey.
Reference period: past 4 weeks (28 days) before WBA survey.
Conditional on having positive cost.
HPQ, Health and Work Performance Questionnaire; WBA-P, Well-Being Assessment for Productivity.
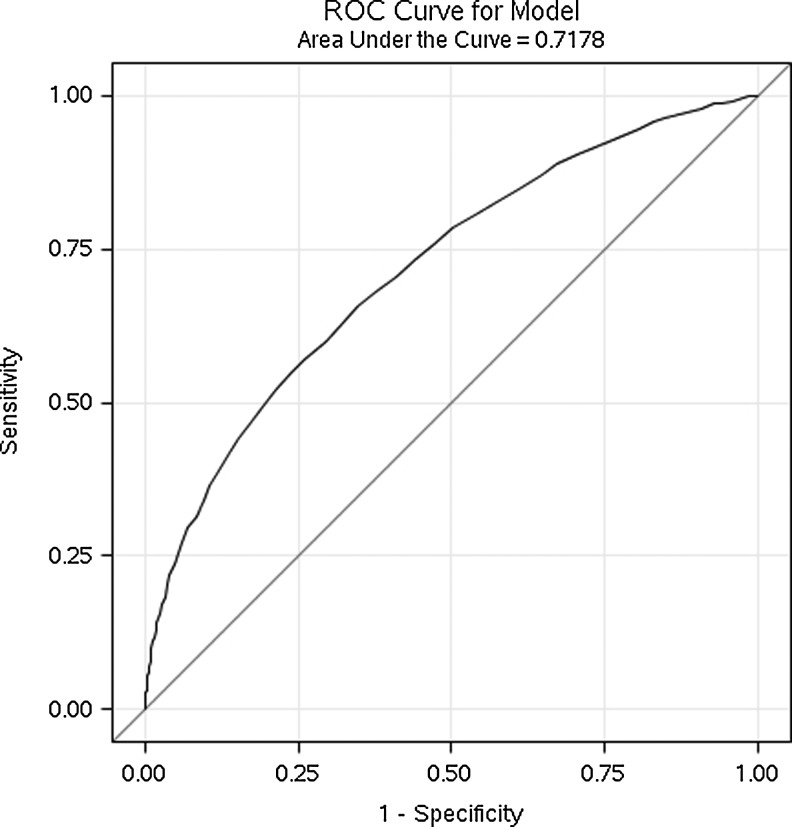
ROC curve
Figure 2 presents the ROC curve for predicting high health and productivity risks (total risk score≥2) using different potential IWBS cutoff points over the entire range, with sensitivity plotted on the y-axis and (1-specificity) on the x-axis. Accuracy statistics are reported in Table 2. AUC was 0.7198, indicating a good diagnostic accuracy. Comparing to other optimal IWBS cutoffs such as 74 and 76, the cutoff score of 75 showed equal capabilities to identify persons who are and who are not at high risk of having 2 or more adverse health and productivity outcomes, while 74 and 76 showed less ability in either specificity or sensitivity. The distance to ROC curve and Youden's index were not significantly different across these 3 cutoffs (Table 2).
FIG. 2.
Receiver Operating Characteristic (ROC) curve for predicting 2 or more health and productivity adverse outcomes for Employer A.
Table 2.
Measures of Diagnostic Accuracy from the Receiver Operating Characteristic Curve Predicting 2 or More Health and Productivity Adverse Outcomes for Employer A
| IWBS cutoff point | Sensitivity | Specificity | Distance to ROC Curve | Youden's Index | |
|---|---|---|---|---|---|
| Entire study sample (N=11702) | |||||
| Optimal cutoff 1 | 75 | 0.6563 | 0.6544 | 0.4873 | 0.3107 |
| Optimal cutoff 2 | 74 | 0.6309 | 0.6773 | 0.4901 | 0.3083 |
| Optimal cutoff 3 | 76 | 0.6816 | 0.6224 | 0.4938 | 0.3041 |
| Male sample (N=4239) | |||||
| Optimal cutoff 1 | 75 | 0.6298 | 0.6766 | 0.4914 | 0.3065 |
| Female sample (N=7463) | |||||
| Optimal cutoff 1 | 75 | 0.6698 | 0.6394 | 0.4888 | 0.3093 |
IWBS, Individual Well-Being Score.
Although female employees were 6.29% more likely to be at risk of having 2 or more health and productivity adverse outcomes than male employees (63.35% vs. 56.66%), separate ROC analysis for male and female employees suggested the same optimal IWBS cutoff point of 75 to dichotomize employees into high and low risk groups. Accuracy indicators including sensitivity, specificity, distance to ROC curve, and Youden's index associated with IWBS 75 also were comparable between female and male employees (Table 2). As a result, it was determined that cutoffs specific to either sex were unnecessary.
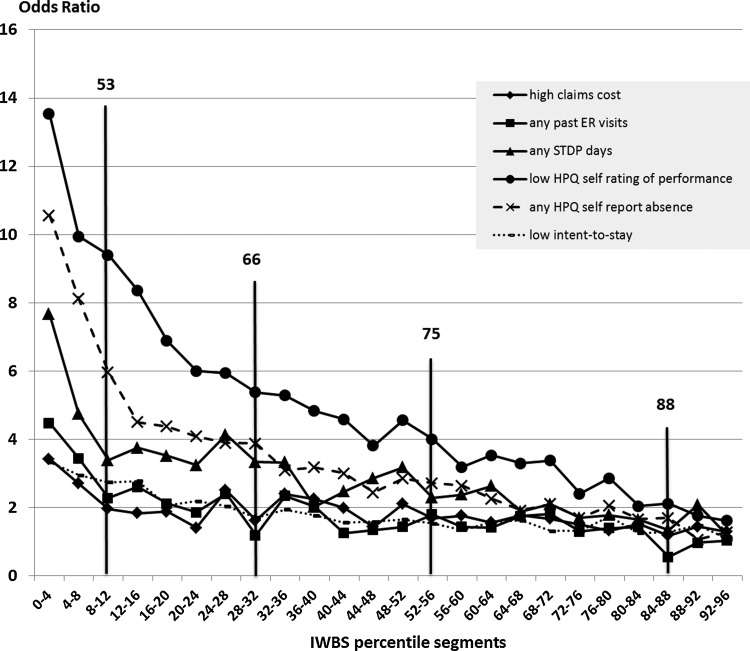
Relative risk analysis
To further group employees into smaller IWBS segments, logistic regression was performed for each of 7 adverse health and productivity outcomes. The relative risks (ORs) of each IWBS percentile segment against the highest IWBS percentile segment (96–100 percentile) were plotted in Figure 3, which suggested a nonlinear relationship between IWBS and outcomes. In addition to the IWBS of 75 that was identified by ROC curve analysis, abrupt reductions in relative risks of adverse health and productivity outcomes also were clustered at IWBS segments of 8–12, 28–32, and 84–88 percentiles based on visual inspection, corresponding to IWBS median values of 53, 66, and 88. Together with the IWBS cutoff of 75, which was the median score in the segment of the 52–56 percentile, the entire employee population was classified into 5 risk levels based on score ranges for having multiple adverse health and productivity outcomes: high (0–53), medium–high (53–66), medium (66–75), low–medium (75–88), and low (88–100). One-way ANOVA showed that differences in 7 adverse outcomes across 5 risk groups were all statistically significant (Table 3).
FIG. 3.
Odds Ratio Plots by adverse health and productivity outcomes for Employer A. Logistic regressions were used to compute odds ratios for each binary outcome, accounting for age, gender, marital status, and education. The reference group was the 96-100 IWBS percentile segment. The outcome of high WBA-P was not plotted in this graph because the odds ratio in low percentile segments considerably exceeded current scales. ER, emergency room; HPQ, Health and Work Performance Questionnaire; IWBS, Individual Well-Being Score; STDP, short-term disability paid; WPA-P, Well-Being Assessment for Productivity.
Table 3.
Proportion of Employees Having Adverse Health and Productivity Outcomes across 5 Identified Risk Groups in Employer A
| Risk Group | IWBS Score | % of sample | High claims cost (%) | Any ER visits (%) | Any STDP days (%) | Low HPQ self rating of performance (%) | High WBA-P (%) | Any HPQ absences (%) | Low intent-to-stay score (%) |
|---|---|---|---|---|---|---|---|---|---|
| High | 0–53 | 9.90 | 59.74 | 11.60 | 15.93 | 70.56 | 89.29 | 39.63 | 63.51 |
| Medium–High | 53–66 | 19.72 | 50.87 | 6.50 | 10.16 | 60.07 | 71.00 | 24.05 | 55.47 |
| Medium | 66–75 | 22.91 | 53.06 | 5.31 | 7.98 | 50.35 | 51.64 | 17.55 | 49.24 |
| Low–Medium | 75–88 | 33.25 | 46.67 | 4.66 | 5.88 | 39.94 | 32.33 | 12.76 | 44.28 |
| Low | 88–100 | 14.21 | 44.98 | 3.31 | 4.35 | 25.13 | 14.61 | 8.24 | 39.81 |
| F Value of ANOVA Test | 10.82 | 21.91 | 42.09 | 218.16 | 762.48 | 158.50 | 57.35 |
ANOVA, analysis of variance; ER, emergency room; HPQ, Health and Work Performance Questionnaire; IWBS, Individual Well-Being Score; STDP, short-term disability paid; WBA-P, Well-Being Assessment for Productivity.
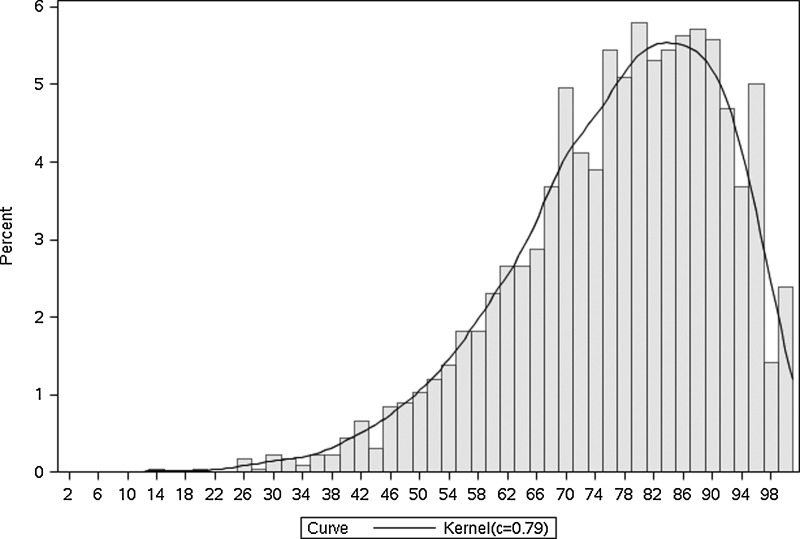
Validity of cutoffs in smaller employer sample (Employer B)
To test the validity and generalizability of IWBS cutoff values to differentiate other employee samples at different levels of health and productivity risks, the identified cutoff values were applied in a health and wellness company (Employer B). Employees of Employer B participated in the same WBA survey as the employees of Employer A during the period of March 1, 2010 and March 31, 2010. The response rate was 85%, resulting in 2257 employees in the study sample for Employer B. The IWBS average score in Employer B (77.07) was significantly higher than for Employer A (72.72), with a standard deviation of 14.34 and a range of 13.51–100 (Fig. 4).
FIG. 4.
Kernel Density Distribution of Individual Well-Being Score in Employer B.
Employees in the study sample of Employer B were grouped into 5 risk levels based on the recommended IWBS cutoff values 63, 66, 75, and 88 (Table 4). Logistic regressions were performed to compare relative risks of having each of 5 adverse health and productivity outcomes across 5 risk groups. Outcomes assessed are shown in Table 4. The ORs computed from logistic regressions after accounting for age, sex, marital status, and education are reported in Table 4. Overall, IWBS cutoff values performed well in predicting any adverse health and productivity risks. For example, the high-risk group in Employer B (IWBS score 0–53) was 7.09 times more likely to rate themselves with low job performance scores (0–8), and 7.01 times more likely to have any health-related absences in the past 28 days relative to low risk group employees (IWBS score 88–100). Differences across the 5 risk groups were statistically significant for all 5 outcomes, as indicated by 1-way ANOVA.
Table 4.
Odds Ratio Summary by Adverse Health and Productivity Outcomes across 5 Risk Groups in Employer B (N=2257)
| Risk Group | IWBS Score | % of sample | High claims cost (OR) | Any ER visits (OR) | Low HPQ self rating of performance (OR) | High WBA-P (OR) | Any HPQ absences (OR) |
|---|---|---|---|---|---|---|---|
| High | 0–53 | 6.60 | 4.84 | 1.86 | 7.09 | 28.88 | 7.01 |
| Medium–High | 53–66 | 14.00 | 2.57 | 1.28 | 3.11 | 14.78 | 3.01 |
| Medium | 66–75 | 18.70 | 2.33 | 1.35 | 2.95 | 7.02 | 2.47 |
| Low–Medium | 75–88 | 35.22 | 1.62 | 0.83 | 1.75 | 3.37 | 1.41 |
| Low | 88–100 | 25.48 | 1 | 1 | 1 | 1 | 1 |
| F Value of ANOVA Test | 12.23 | 4.07 | 35.52 | 126.87 | 39.82 |
Note: Logistic regressions were used to compute odds ratios for each binary outcome, accounting for age, sex, marital status, and education. Reference group was the lowest risk group (88–100 IWBS).
ANOVA, analysis of variance; ER, emergency room; HPQ, Health and Work Performance Questionnaire; IWBS, Individual Well-Being Score; OR, odds ratio; WBA-P, Well-Being Assessment for Productivity.
Discussion
This study benchmarked well-being cutoff points from a comprehensive well-being assessment for predicting adverse health and productivity outcomes. Based on a large employer sample, the study analyzed the association between a global well-being measure (IWBS) and health and productivity outcomes and found relationships that were significant and consistent across outcomes. Results showed that IWBS of 53, 66, 75, and 88 may be optimal cutoff points for classifying employees into different levels of health and productivity risk. Worksite interventions targeting employees with IWBS below 75 would have the greatest opportunity to reduce health and productivity risks. Application of the 5 risk segments in a smaller employer sample further confirmed the validity of the proposed cutoffs.
To the authors' knowledge, this is the first employee population-based study to assess the association between well-being and multiple health and productivity outcomes. The results confirmed recent evidence that showed that IWBS can predict health care utilization and health care claims cost.28 This study provides new evidence that IWBS also is associated with productivity measures that have substantial economic implications for employers including absenteeism, presenteeism, job performance, and job retention. According to the health condition-related cost estimates,2 presenteeism costs were higher than health care costs for most common conditions, accounting for 18%–60% of the total costs, and absenteeism costs were, on average, half of the health care costs, representing 2%–10% of the total costs. Therefore, IWBS classification is a valuable predictor of multiple health and productivity outcomes that are meaningful to employers.
Proposed IWBS cutoff points for adverse health and productivity outcomes potentially have many uses that are applicable to an employee population. Much like cutoff points in clinical medicine that have been widely applied to the assessment of health and nutrition risk, such as overweight and obesity risk thresholds defined by anthropometry,29 classification of IWBS helps identify employees at different health and productivity risk levels. This makes it possible to focus resources on segments of the population in greatest need. Risk stratification is a commonly accepted concept in clinical medicine and public health. Types and intensity of interventions can be tailored to employees in particular well-being segments. Furthermore, effects of well-being interventions can be evaluated and compared in a way that meaningfully links to outcomes important to employers. Well-being segmentation makes comparison across multiple employers (and over time) possible by applying consistent and universal IWBS cutoff points. Upward transition across the IWBS segments will be indicative of improvement in health and productivity outcomes, which is particularly meaningful when primary data for such outcomes are not readily available for evaluation.
Several strengths of this study are noteworthy. A relatively large employer sample was used for an in-depth examination on IWBS classification. The applicability of the classification was then tested in a smaller employer sample, which is stronger than the conventional split-sample validation from the same employer because it indicates the generalizability of the results to a different population. The results suggested that the IWBS cutoffs derived from a large employer sample can be applied to classify employees into meaningful segments in a separate smaller employer sample in a different industry. The classifications for this smaller employer were highly indicative of relative risks of having various adverse health and productivity outcomes, as they were for the large employer. Multiple diagnostic techniques were employed to select optimal cutoff points, including conventional ROC curves and a relative risk approach. ROC curves detected a single optimal cutoff that identified a general target population at risk for well-being interventions. The relative risk approach is more appropriate when the goal is to further classify a population into multiple risk levels so that the interventions can be tailored. A rich set of health and productivity measurements were evaluated that accounted for major sources of economic burden to employers. Multiple cutoffs were established for different intervention purposes and optimal intervention designs. By segmenting well-being based on the risks of actual outcomes occurring, well-being takes on a decisively diagnostic value for employers and researchers trying to understand the true impact of well-being improvement as it relates to true value creation for employers and the workforce.
Potential limitations included problems with calibration, generalizability, self-reporting bias for productivity measures, and lack of longitudinal analysis. Because the number of observations with extremely low IWBS was not sufficient to compute relative risk for each point of IWBS, the final recommended cutoff values were determined at the median of selected percentile groups. Thus, the cutoff value for the high-risk group was likely to be less precise than for the low-risk group because the range of IWBS percentile segments for high-risk groups was wider on the left-hand side tail of the IWBS distribution. Further analysis based on even larger employers or pooled employers may help to further refine these cutoffs. The optimal cutoff values of IWBS were determined from the analysis of 1 large employer sample whose participation was voluntary. Although an application in this study supported the predictive capability of IWBS cutoff points in a smaller employer sample, to what extent the recommended cutoff values were generalizable to nonparticipants of this employer and other employers is still unknown. Further validation studies are needed using national representative general employee populations or a pooled employer population. Recall bias and common method bias are concerns for almost any study that investigates self-reported measures. These problems were minimized by using validated self-report measures, such as HPQ absence and job performance, and incorporating objective claims data captured by a third party. Nevertheless, subsequent studies should investigate indicators of productivity from sources other than employees' own self-report. Lastly, the proposed IWBS cutoffs were based on cross-sectional analysis because of data availability. Future research should investigate longitudinal WBA data over multiple years to assess the capability of current recommended IWBS cutoff values to predict prospective health and productivity outcomes.
Given the strong association between well-being and outcomes relevant to employers, it is plausible to conclude that the implementation of worksite programs that target employees' overall well-being (eg, smoking cessation, disease management, healthy behavior coaching, on-site fitness, stress management, organizational development) will lead to improvements in associated outcomes. Subsequent research should investigate the causal nature of these relationships and test the efficacy of using IWBS segments to select participants who have the highest need for such interventions. Pragmatically, the well-being segments presented here are best suited to assess the level of risk across outcomes and inform the frequency and intensity of comprehensive intervention programs. For instance, those in the lowest well-being risk segment may not need much intervention, and so it may suffice to provide them with access to educational and motivational resources. In contrast, individuals in higher well-being risk segments may need more frequent outreach and contact with a coach to help hold them accountable for achieving goals. Future research should investigate how intervention content could be best tailored to individuals within these segments.
Conclusion
This study established a strong association between IWBS and multiple health and productivity outcomes in an employee population in which employees with lower IWBS generally were more likely to have adverse outcomes; this relationship was nonlinear. IWBS below 75 is recommended to distinguish employees likely to have 2 or more adverse outcomes, indicating the need for well-being improvement interventions in this group. IWBS 53, 66, and 88 are recommended when further segmentation is needed to determine the intensity of intervention in the group with IWBS below or above 75. These thresholds classify employees into high (IWBS 0–53), medium–high (IWBS 53–66), medium (IWBS 66–75), low–medium (75–88), and low (88–100) risk levels of having adverse health and productivity outcomes. Based on these results, the authors propose that IWBS is a strong indicator of outcomes that are meaningful to employers, and encourage the use of the proposed cutoff points when considering how to most effectively deliver worksite interventions for health and productivity improvement. Furthermore, the segments allow for comparisons of well-being between groups and over time in a manner aligned with those employee health and productivity outcomes that are important to business leaders.
Author Disclosure Statement
Drs. Shi, Sears, Coberley, and Pope were employed by or shareholders of Healthways, Inc. when this study was conducted and submitted.
References
- 1.Goetzel RZ. Hawkins K. Ozminkowski RJ. Wang S. The health and productivity cost burden of the "top 10" physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med. 2003;45:5–14. doi: 10.1097/00043764-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Goetzel RZ. Long SR. Ozminkowski RJ. Hawkins K. Wang S. Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. J Occup Environ Med. 2004;46:398–412. doi: 10.1097/01.jom.0000121151.40413.bd. [DOI] [PubMed] [Google Scholar]
- 3.Stewart WF. Ricci JA. Chee E. Morganstein D. Lost productive work time costs from health conditions in the United States: Results from the American Productivity Audit. J Occup Environ Med. 2003;45:1234–1246. doi: 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]
- 4.Collins JJ. Baase CM. Sharda CE, et al. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. J Occup Environ Med. 2005;47:547–557. doi: 10.1097/01.jom.0000166864.58664.29. [DOI] [PubMed] [Google Scholar]
- 5.Loeppke R. Taitel M. Haufle V. Parry T. Kessler RC. Jinnett K. Health and productivity as a business strategy: A multiemployer study. J Occup Environ Med. 2009;51:411–428. doi: 10.1097/JOM.0b013e3181a39180. [DOI] [PubMed] [Google Scholar]
- 6.Hemp P. Presenteeism: At work—but out of it. Harvard Bus Rev. 2004;155:49–58. [PubMed] [Google Scholar]
- 7.Fronstin P. Findings from the 2011 EBRI/MGA Consumer Engagement in Health Care Survey. New York: The Commonwealth Fund; 2011. [Google Scholar]
- 8.Hutchinson AD. Wilson C. Improving nutrition and physical activity in the workplace: A meta-analysis of intervention studies. Health Promot Int. 2012;27:238–249. doi: 10.1093/heapro/dar035. [DOI] [PubMed] [Google Scholar]
- 9.Bandoni DH. Sarno F. Jaime PC. Impact of an intervention on the availability and consumption of fruits and vegetables in the workplace. Public Health Nutr. 2011;14:975–981. doi: 10.1017/S1368980010003460. [DOI] [PubMed] [Google Scholar]
- 10.Plotnikoff RC. McCargar LJ. Wilson PM. Loucaides CA. Efficacy of an e-mail intervention for the promotion of physical activity and nutrition behavior in the workplace context. Am J Health Promot. 2005;19:422–429. doi: 10.4278/0890-1171-19.6.422. [DOI] [PubMed] [Google Scholar]
- 11.Christensen JR. Faber A. Ekner D. Overgaard K. Holtermann A. Sogaard K. Diet, physical exercise and cognitive behavioral training as a combined workplace based intervention to reduce body weight and increase physical capacity in health care workers. A randomized controlled trial. BMC Public Health. 2011;11:671. doi: 10.1186/1471-2458-11-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karlson B. Jönsson P. Pålsson B, et al. Return to work after a workplace-oriented intervention for patients on sick-leave for burnout–a prospective controlled study. BMC Public Health. 2010;10:301. doi: 10.1186/1471-2458-10-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kristensen TS. Workplace intervention studies. Occup Med. 2000;15:293–305. [PubMed] [Google Scholar]
- 14.Martin A. Sanderson K. Cocker F. Meta-analysis of the effects of health promotion intervention in the workplace on depression and anxiety symptoms. Scand J Work Environ Health. 2009;35:7–18. doi: 10.5271/sjweh.1295. [DOI] [PubMed] [Google Scholar]
- 15.Tsutsumi A. Nagami M. Yoshikawa T. Kogi K. Kawakami N. Participatory intervention for workplace improvements on mental health and job performance among blue-collar workers: A cluster randomized controlled trial. J Occup Environ Med. 2009;51:554–563. doi: 10.1097/JOM.0b013e3181a24d28. [DOI] [PubMed] [Google Scholar]
- 16.Bertera RL. The effects of workplace health promotion on absenteeism and employment costs in a large industrial population. Am J Public Health. 1990;80:1101–1105. doi: 10.2105/ajph.80.9.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderzen I. Arnetz BB. The impact of a prospective survey-based workplace intervention program on employee health, biologic stress markers, and organizational productivity. J Occup Environ Med. 2005;47:671–682. doi: 10.1097/01.jom.0000167259.03247.1e. [DOI] [PubMed] [Google Scholar]
- 18.Arnetz BB. Sjogren B. Rydehn B. Meisel R. Early workplace intervention for employees with musculoskeletal-related absenteeism: A prospective controlled intervention study. J Occup Environ Med. 2003;45:499–506. doi: 10.1097/01.jom.0000063628.37065.45. [DOI] [PubMed] [Google Scholar]
- 19.van Oostrom SH. Anema JR. Terluin B. de Vet HC. Knol DL. van Mechelen W. Cost-effectiveness of a workplace intervention for sick-listed employees with common mental disorders: Design of a randomized controlled trial. BMC Public Health. 2008;8:12. doi: 10.1186/1471-2458-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedman RA. Holtom B. The effects of network groups on minority employee turnover intentions. Human Resource Manage. 2002;41:405–421. [Google Scholar]
- 21.Palsha SA. Bailey DB. A study of employee stability and turnover in home-based early intervention. J Early Intervention. 1990;14:342–351. [Google Scholar]
- 22.Kessler RC. Barber C. Beck A, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ) J Occup Environ Med. 2003;45:156–174. doi: 10.1097/01.jom.0000052967.43131.51. [DOI] [PubMed] [Google Scholar]
- 23.Harter J. Gurley V. Measuring well-being in the United States. Assoc Psychol Sci. 2008;21:23–26. [Google Scholar]
- 24.James KH. Schmidt FL. Keyes CLM. Well-being in the workplace and its relationship to business outcomes. In: Keyes CLM, editor; Haidt J, editor. Flourishing: The Positive Person and the Good Life. Washington, DC: American Psychological Association; 2003. pp. 205–224. [Google Scholar]
- 25.Kaplan R. Anderson J. Ganiats T. The Quality of Well-being Scale: Rationale for a single quality of life index. In: Walker SR, editor; Rosser RM, editor. Quality of Life Assessment: Key Issues in the 1990s. London: Kluwer Academic Publishers; 1993. pp. 65–94. [Google Scholar]
- 26.Tibblin G. Tibblin B. Peciva S. Kullman S. Svardsudd K. "The Göteborg quality of life instrument"—An assessment of well-being and symptoms among men born 1913 and 1923. Methods and validity. Scand J Prim Health Care Suppl. 1990;1:33–38. [PubMed] [Google Scholar]
- 27.Al-Windi A. Dag E. Kurt S. The influence of perceived well-being and reported symptoms on health care utilization: A population-based study. J Clin Epidemiol. 2002;55:60–66. doi: 10.1016/s0895-4356(01)00423-1. [DOI] [PubMed] [Google Scholar]
- 28.Harrison PL. Pope JE. Coberley CR. Rula EY. Evaluation of the relationship between individual well-being and future health care utilization and cost. Popul Health Manag. 2012 Feb 22; doi: 10.1089/pop.2011.0089. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. Geneva, Switzerland: World Health Organization; 1995. [Google Scholar]
- 30.Gallup. Gallup-Healthways Well-Being Index: Methodology Report for Indexes. http://wbi.meyouhealth.com/files/GallupHealthwaysWBI-Methodology.pdf. [Jul 2;2012 ]. http://wbi.meyouhealth.com/files/GallupHealthwaysWBI-Methodology.pdf
- 31.Evers K. Prochaska J. Castle P, et al. Development of an individual well-being scores assessment. Psychol Well-Being Theory Res Pract. 2012;2:2. [Google Scholar]
- 32.Prochaska JO. Evers KE. Johnson JL, et al. The well-being assessment for productivity: A well-being approach to presenteeism. J Occup Environ Med. 2011;53:735–742. doi: 10.1097/JOM.0b013e318222af48. [DOI] [PubMed] [Google Scholar]