Abstract
Recently proposed international guidelines for screening for gestational diabetes mellitus (GDM) recommend additional screening in early pregnancy for sub-populations at a high risk of type 2 diabetes mellitus (T2DM), such as indigenous women. However, there are criteria that should be met to ensure the benefits outweigh the risks of population-based screening. This review examines the published evidence for early screening for indigenous women as related to these criteria. Any publications were included that referred to diabetes in pregnancy among indigenous women in Australia, Canada, New Zealand and the United States (n = 145). The risk of bias was appraised. There is sufficient evidence describing the epidemiology of diabetes in pregnancy, demonstrating that it imposes a significant disease burden on indigenous women and their infants at birth and across the lifecourse (n = 120 studies). Women with pre-existing T2DM have a higher risk than women who develop GDM during pregnancy. However, there was insufficient evidence to address the remaining five criteria, including the following: understanding current screening practice and rates (n = 7); acceptability of GDM screening (n = 0); efficacy and cost of screening for GDM (n = 3); availability of effective treatment after diagnosis (n = 6); and effective systems for follow-up after pregnancy (n = 5). Given the impact of diabetes in pregnancy, particularly undiagnosed T2DM, GDM screening in early pregnancy offers potential benefits for indigenous women. However, researchers, policy makers and clinicians must work together with communities to develop effective strategies for implementation and minimizing the potential risks. Evidence of effective strategies for primary prevention, GDM treatment and follow-up after pregnancy are urgently needed. Copyright © 2013 John Wiley & Sons, Ltd.
Keywords: diabetes, pregnancy, indigenous
Introduction
Diabetes in pregnancy (DIP) causes serious complications in pregnancy and birth 1 and is an important driver of the type 2 diabetes mellitus (T2DM) epidemic in indigenous populations 2. T2DM is one of the leading causes of death globally 3 and imposes a disproportionately large burden on indigenous people 4. The scale of the public health impact requires a coordinated public health response incorporating a range of primary, secondary and tertiary prevention strategies5–7, based on evidence to ensure it reduces health disparities and is relevant for policy and practice 8.
Diabetes in pregnancy refers to any diabetes in pregnancy, including gestational diabetes mellitus (GDM), type 2 diabetes mellitus (T2DM) and type 1 diabetes mellitus (T1DM). GDM is defined as ‘any degree of glucose intolerance with onset or first recognition during pregnancy’9, although recent international guidelines recommend differentiation between probable T2DM identified early in pregnancy that has not been previously diagnosed and GDM that develops later in pregnancy 10. DIP is associated with poor outcomes for both the mother and her infant during pregnancy, at birth and across the lifecourse 11. The risks for the mother include an increased risk of caesarean section 12, pre-eclampsia and developing T2DM after pregnancy13,14. The risks for the infant include an increased risk of congenital abnormalities 15, macrosomia 12, neonatal hypoglycaemia 1 and developing T2DM in later life 16, which implicates DIP as having a major compounding effect on the diabetes epidemic 2. Mothers with pre-existing T1DM or T2DM before pregnancy, and their infants, have a higher risk's of complications than those who develop GDM during pregnancy17–19.
Existing GDM screening guidelines were developed more than 40 years ago by adapting methods for non-pregnant women or to identify those at a higher risk of developing T2DM after pregnancy 12. However, a growing evidence base demonstrating the increased risks of hyperglycaemia in pregnancy 1 and the longer term2,20,21 to both mother and infant, the rising prevalence of GDM 22, and intervention trials demonstrating that there is effective treatment for GDM which improves pregnancy outcomes11,23,24, has led to a revision of these international recommendations10,25. A key point of debate during this revision process has been whether early pregnancy screening for GDM should be offered universally for all women or selectively to sub-populations at higher risk of T2DM26,27. Furthermore, the type of tests (particularly in early pregnancy) 28, the timing of tests, what thresholds should be used29–32, as well as the most effective preventive, treatment and follow-up strategies26,33,34 continue to be discussed26,35–38. However, one area of apparent consensus is that women in sub-populations at high risk of T2DM should be offered screening in early pregnancy at 6–12 weeks of gestation10,25,26,39, in addition to screening at 24–28 weeks of gestation as is currently recommended.
Screening is a secondary prevention strategy where the aim is to reduce the burden of disease in the community through early detection of disease, providing an opportunity for therapeutic intervention and improved health outcomes40,41. There are, however, long established criteria40–42 that should be met before introducing population-based screening, to ensure that the benefits outweigh any risks, inconvenience and costs (Table 1).
Table 1.
Criteria for population-based screening
| Criterion | Evidence required |
|---|---|
| Epidemiology of disease | Prevalence and natural history are understood, and the condition poses a significant disease burden |
| Current screening practice and rates | Barriers and facilitators are understood |
| Acceptability | Women's preferences and values are understood |
| Efficacy and cost | Sensitive and specific cost-effective screening tests are available |
| Effective treatment | Available and accessible after diagnosis |
| Reliable follow-up systems | In place for those diagnosed at risk |
There are a number of potential benefits to offering early screening for GDM, which may be particularly important for indigenous women who have a high risk of T2DM. Primarily, the early detection and treatment of DIP has been shown to reduce the associated health risks in pregnancy and birth among non-indigenous women11,23,24,43,44. Furthermore, pregnancy offers a ‘window of opportunity’ for health interventions, as predominantly young healthy pregnant women have frequent scheduled contacts with health-care providers. They are often highly motivated to adapt their behaviour to improve the health of their infant45,46, with any effective lifestyle interventions potentially benefitting the whole family47,48. In addition, pregnancy mimics a ‘natural stress test’ 49 for insulin resistance as a result of naturally occurring placental hormones50,51, offering a unique opportunity for detecting the disease at an earlier stage in the natural history of this metabolic disorder.
However, there also is the potential for harm to result from the introduction of early pregnancy GDM screening. The increased diagnosis of any medical condition in a generally healthy population can be associated with an increased psychological stress 52. This is particularly the case during pregnancy as women are concerned about the health of their infant53–56. Although recent studies among non-indigenous women suggest that this is not necessarily the case with a GDM diagnosis11,54, indigenous women may experience unique stressors 57, including dislocation from families if required to move from a remote community to a regional centre for obstetric care. There is potential for any intervention during pregnancy to interfere with the normal processes and initiate a ‘cascade of medical interventions’ 58, such as induction of labour, caesarean section and artificial infant feeding23,35,59. There are also risks with selectively applying a preventive strategy to sub-populations, including ‘labelling’ 60, which can exacerbate existing social stigma, as well as internalised racism and negative self-esteem61,62.
In addition to specific risks, the evidence in relation to the specific population-based screening criteria (Table 1) is likely to be different for indigenous women 63. Indigenous people continue to experience poorer health than other people living in the same country 63, and the epidemiological patterns of diabetic disease are markedly different, implicating DIP as a major contributing factor 2. Efforts to reduce these health inequalities have led to an identified need to assess the potential differential impact of interventions8,64. Compounding this is evidence that indigenous people experience reduced access to treatment for diabetic complications65–69 and DIP 70. Although the efficacy of screening tests and pharmaceutical treatments is based on biological evidence that is likely to be similar for all population groups, the effectiveness may differ according to the setting and population (context) in which an intervention is delivered 71, further supporting the need to examine indigenous-specific evidence.
To our knowledge, this is the first review to examine the evidence in relation to the recent International Association of Diabetes and Pregnancy Study Groups recommendations for early GDM screening in indigenous populations. This systematic review aims to assess the level of evidence for early screening for GDM among indigenous women in Australia, Canada, New Zealand and the United States.
Materials and methods
The methodology for this review has been described in detail elsewhere 72.
Inclusion criteria
All publications, with the exception of abstracts, that focused on DIP among indigenous women in Australia, Canada, New Zealand or the United States in the title or abstract were included. We excluded publications that focused on diabetes among children or adults where there was only a very brief reference to DIP. This broad inclusion criterion was used to ensure all study designs could be examined and included if they contained any qualitative or quantitative data relevant to the population-based screening criteria40,42. It was decided to focus on published studies concerning indigenous women in these four countries because they have been compared in other related reviews73,74 as they share similar experiences associated with colonisation, marginalisation, institutionalisation, poverty, a rapid transition from a traditional to a westernised lifestyle and an increased risk of diabetes.
Search method for identification of studies
We searched the Cochrane Database for Systematic Reviews (1995 to July 2012), Medline (1950 to July 2012), Embase (1949 to July 2012), CINAHL (1937 to July 2012) and PsychINFO (1905 to July 2012) to identify published literature. A comprehensive key word and MeSH heading search strategy for related terms associated with ‘pregnancy’ and ‘diabetes’ and ‘indigenous’ was used 72. Appendix A shows the full search strategy used for Embase, with adapted MeSH terms for other databases. No language restrictions were applied.
Data collection
The abstracts of all search results were reviewed by two authors (C. C. and E. W.) to determine those potentially meeting the inclusion criteria. The full texts of these publications were then reviewed by one author (C. C.), with a random selection (10%) independently reviewed by another author (D. Y.) for validation. Data from publications meeting inclusion criteria were extracted by one author (C. C.) and a random selection of 10% independently extracted by another author (D. Y.) for validation. Data items included the population description, study details and the main findings relevant to the population-based screening criteria 40.
Appraisal of external validity (generalisability)
To assess the potential generalisability of the study, data were extracted on the basis of whether the study was conducted in a population that was remote, rural, urban or mixed, and whether the data source used was population, community or clinic based.
Appraisal of internal validity (risk of bias)
Intervention studies, measurement studies and systematic reviews were assessed using appraisal tools developed by the Centre for Evidence Based Medicine75–77. Qualitative studies were appraised using tools developed by the Australian Department of General Practice and other local experts78,79. There was no standard tool for appraising quantitative descriptive observational studies; therefore, one was adapted for this review from the Strengthening the Reporting of Observational Studies in Epidemiology statement 80 and other published tools developed for reviewing epidemiological studies81,82.
Data synthesis
The study results were synthesised under each of the relevant screening criteria. General ‘evidence statements’ were generated from the publications, and a ‘level of evidence’ reported according to pre-specified criteria based on an adapted83,84 GRADE tool 72 (Table 1). The ‘level of evidence’ related only to the internal validity (risk of bias) appraisal of the study from which the evidence statement was generated and does not bear any relationship with whether the screening criteria are met. The country in which the study was conducted was reported as an indication of generalisability (external validity) for each evidence statement. An assessment of whether the evidence was sufficient or insufficient to meet each criterion was made by the authors, taking into the consideration the ‘level of the evidence’ (risk of bias) of the studies from which the evidence statements were generated and the scope of the issues addressed by the evidence statements (Table 2).
Table 2.
Classification of the level of evidence for included studies
| Symbol | Level of evidence | Risk of bias criteria |
|---|---|---|
| H | High | One or more study with low risk of bias |
| M | Moderate | One or more studies appraised with moderate risk of bias |
| L | Low | One or more studies were appraised with high risk of bias |
| VL | Very low | The publications were not in a format that allowed appraisal of the effect estimate (e.g. opinion piece) |
Results
The initial search using terms related to ‘diabetes’ and ‘pregnancy’ yielded over 40 000 results, which was reduced to 1134 when the ‘indigenous’ terms were applied as a filter. The abstracts of these 1134 publications were screened, and 854 abstracts were excluded as they were clearly unrelated to DIP among indigenous women in Australia, Canada, New Zealand or the United States. The full text of 280 publications was reviewed, and an additional 135 were excluded. The most common reason for exclusion was that the abstract discussed diabetes and pregnancy as separate factors, rather than discussing diabetes in pregnancy. A total of 145 publications were included, and a detailed table of the study characteristics and risk of bias appraisal is available on request. Validation checks showed that there was good agreement (>96%) with assessment of whether studies met inclusion criteria and high levels of agreement (>80%) for the risk of bias appraisals (Figure 1).
Figure 1.
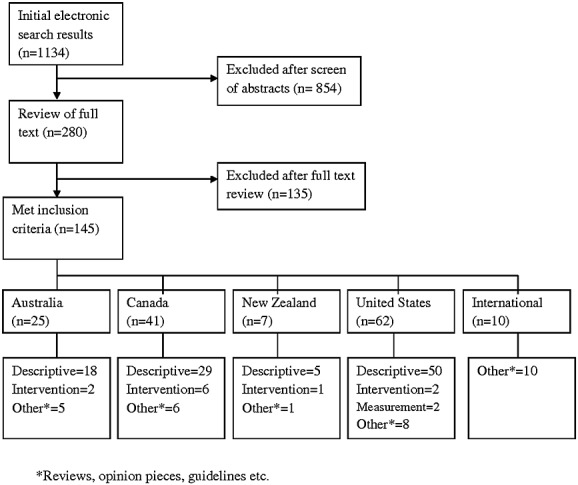
Flow chart for included studies
Description of included publications
The majority (96/145 or 66%) of included studies were quantitative descriptive studies, with a range of study designs, including findings from over 12 million people. There were only six qualitative descriptive studies including 140 participants. Eleven (8%) publications (7073 participants) described or evaluated interventions, but only one of these studies was randomised, and therefore, 12 of these studies were appraised as having a high risk of bias. Two measurement studies (308 participants) evaluated screening test efficacy. A total of 30 (21%) other publications did not report primary research, including 23 reviews and seven opinions, commentaries, editorials or guidelines.
Risk of bias (internal validity)
Only 22/96 (23%) of the quantitative descriptive studies met all the criteria for ‘low risk of bias’ in this review; the majority (n = 16) of which were generated from a longitudinal study among Pima and Papago Indian communities in the United States. The major risk of bias identified in the quantitative studies was outcome assessment bias, as diabetes was often indirectly measured using medical records or hospital registers (49/96 or 51%). The majority of quantitative descriptive studies (64/96 or 67%) adequately described the diagnostic criteria used for the identification of DIP or GDM. However, the lack of diagnostic criteria in 33% of studies was a major limitation given the variability of diagnostic and screening criteria used in practice. Selection bias is a complex issue in reviews involving identification of ethnicity. There were 70/96 (73%) that included whole or consecutive samples and were therefore coded as low risk of selection bias because they were representative of the group described (if the participation rate was high). Only one study in Australia attempted to quantify the identification rate 85 and estimated that approximately 20% of Aboriginal and Torres Strait Islander people were not identified in the sample. In Canada and the United States, where indigenous people are registered according to proportion of indigenous heritage, the inclusion criteria was frequently limited to registered people with over 50% heritage. The risk of bias for studies according to each of the screening criteria is summarised in Figure 2.
Figure 2.
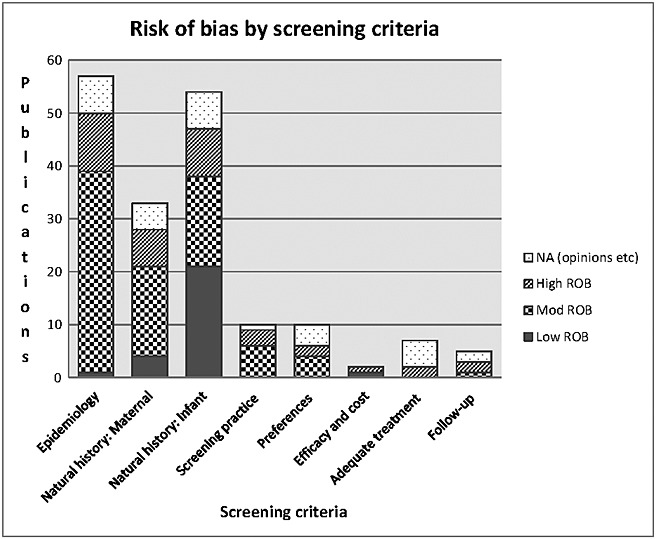
Number of studies graded as high, moderate, low or not appraisable under each of the population-based screening criteria
External validity (generalisability)
Only two descriptive studies were conducted among indigenous women living in urban areas, compared with 50 conducted in remote communities (Figure 3). Although the 40 descriptive studies in mixed populations were potentially generalisable to a wider population, many of the mixed population studies were appraised as having a high risk of outcome assessment bias due to their reliance on database reporting.
Figure 3.
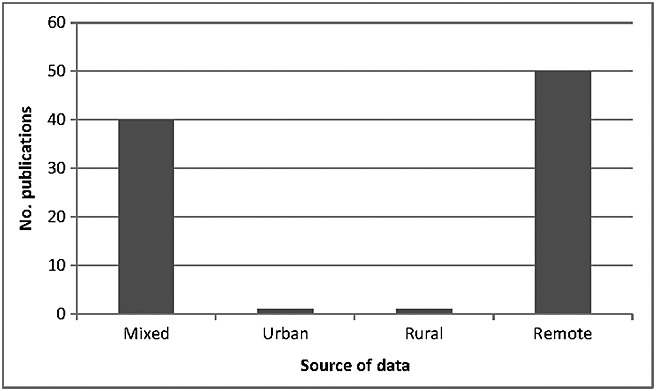
Number of descriptive studies conducted in mixed, urban, rural and remote populations (generalisability)
Main findings and strength of evidence for each of the screening criteria 40
The results are summarised in Table 3. The first column lists the screening criteria, with the number of studies addressing that criterion in parentheses below, and some papers addressing more than one criterion. The first screening criterion (epidemiology) is disaggregated into seven sub-categories as most of the included studies (70%) addressed this factor. The second column lists ‘evidence statements’ generated, with the third column summarising the number of studies appraised at each ‘level of evidence’ (high [H], medium [M], low [L] and very low [VL]), with the respective references in parentheses. The final column states the country where the studies generating those evidence statements were conducted.
Table 3.
Summary of evidence for population-based screening for diabetes in early pregnancy among indigenous women in Australia, Canada, New Zealand and the United States
| Screening criterion (no. publications) | Evidence statement | Quality of evidence for each statement and study references (H, high; M, moderate; L, low; VL, very low) | Country |
|---|---|---|---|
| 1. Prevalence (n = 49) | Higher risk of undiagnosed T2DM in pregnancy and GDM | H 86 | Aus, Can, NZ, US, Int |
| M14,15,18,21,87–115,123,127 | |||
| L13,116–122,220 | |||
| VL126,145,169,221,222 | |||
| Prevalence (trends) (n = 7) | Prevalence of GDM and T2DM in pregnancy is increasing | M21,125,167 | Aus, Can, US, Int |
| L [223,224] | |||
| VL [225,226] | |||
| Natural history: risk for maternal development of DIP (n = 10) | Maternal birth-weight low and high (u-shaped association) | H 156 | US |
| M [227] | |||
| Obesity | M99,123 | Can, US Aus | |
| L 122 | |||
| Genetic variants | H [228] | US | |
| Thrifty genotype theory | VL2,145,161 | Can, Int | |
| Thrifty phenotype theory | VL 160 | US | |
| Natural history: risk to woman during pregnancy and birth (n = 12) | Adverse birth outcomes (e.g. caesarean section and shoulder dystocia) | H 140 | Aus, Can, NZ, US |
| M92–95,111,113,129,133 | |||
| Increased risk of hospitalisation, associated with acute renal disease | M 136 | Can, US | |
| L118,137 | |||
| Natural history: maternal progression to T2DM (n = 8) | Non-pregnant women with impaired glucose intolerance have higher risk of T2DM than pregnant women with impaired glucose tolerance | H [229] | US |
| L 13 | |||
| Increased risk of progressing from GDM to T2DM | M14,21,144 | Can, US | |
| L 13 | |||
| VL 145 | |||
| Faster progression from GDM to T2DM | M96,112 | Aus, Can | |
| L 13 | |||
| Progress from GDM to T2DM at a younger age | M 96 | Aus | |
| Natural history: risk to infant in pregnancy and birth (n = 21) | Increased risk of congenital abnormalities | H 131 | Aus, US |
| M15,108,132 | |||
| VL 138 | |||
| Increased risk of macrosomia | H128,139,140 | Aus, Can, NZ, US | |
| M109,130,135,141–143 | |||
| L 128,230,231 | |||
| Increased risk NICU admissions or poor birth outcomes | M94,113,232 | Aus, Can | |
| L [233] | |||
| VL [234] | |||
| Natural history: long terms risks to infant (n = 31) | Increased risk of obesity | H146–148 | Can, US |
| L 128 | |||
| VL 149 | |||
| Increased risk of glucose intolerance | H148,150–152, M 153 | US | |
| Increased risk of GDM and T2DM | H16,148,154–157 | Can, US, Int | |
| M16,127,135,158,165,166,235 | |||
| L128,163,164 | |||
| VL2,159–162 | |||
| Increased risk renal disease | H [236,237] | US | |
| 2. Current screening practice and rates (n = 7) | GDM screening practice and rates is variable | M88,89,167,238 | Aus, Can, NZ, US |
| L13,168 | |||
| VL 169 | |||
| Highest risk women (e.g. obese women) may be less likely to be screened | M88,89 | NZ, US | |
| 3. Preferences or values (n = 8) | Suggest resources be culturally adapted, programs provide blood sugar data and emphasize opportunity to save money with health diet | M 176 | Can |
| Prefer greater community involvement (especially midwives and elders) and recognise importance of family ties and cultural values | M 176 | Can | |
| VL171,177 | |||
| Prefer group sessions and less direct advice (e.g. story-telling) | VL 171 | Can | |
| Concern about weight gain in pregnancy but many barriers | VL 178 | Can | |
| Many mixed understandings of risk and causes of DIP | M 172 | Aus, Can, US | |
| L173,174 | |||
| Diet (grandmothers), exercise and stress (mothers) cause DIP | L 175 | Can | |
| 4. Efficacy and cost (n = 3) | Screening more sensitive than risk factor analysis alone | H 180 | US |
| One-step WHO method more sensitive than two-step NDDG method | L 179 | US | |
| HBA1C tests not appropriate screening tool among indigenous women | L 181 | Int | |
| 5. Adequate treatment pathways (n = 6) | Integrated community care may improve self-monitoring | L 186 | Aus |
| Standards for diagnosis and treatment | VL 182 | US | |
| Early screening needed to reduce risk of GDM to mother and baby | VL144,183,184 | Aus, Can | |
| Insulin pumps may improve glycaemic control | L 185 | NZ | |
| 6. Follow-up after pregnancy (n = 5) | Low rates of follow-up screening for T2DM after pregnancy for women diagnosed with GDM | M 14 | Can, NZ, US |
| L 13 | |||
| VL 188 | |||
| Registers may improve follow-up | VL 189 | Can | |
| High rates of glucose intolerance in women with DIP followed up after pregnancy | L 188 | NZ |
DIP, diabetes in pregnancy; GDM, gestational diabetes mellitus; NDDG, National Diabetes Data Group; NICU, neonatal intensive care unit; T2DM, type 2 diabetes mellitus; WHO, World Health Organisation.
Epidemiology (prevalence and natural history)
A large amount of evidence (over 70%), much of which was appraised as a moderate to high level, described the epidemiology of DIP among indigenous women and their infants. Indigenous women generally showed a significantly higher risk of GDM and T2DM13–15,18,21,85–125, often occurring at a younger age 126, compared with other women in the same country 127. The main risk factor for developing T2DM was obesity 122, with over 50% of DIP among Native Americans attributed to obesity 123. DIP was clearly associated with a range of adverse consequences in the short term for both women and their infants, and women diagnosed with pre-existing T2DM demonstrated the highest risk15,108,128–132. These risks included caesarean section 133, shoulder dystocia, increased hospitalisation, congenital abnormalities, macrosomia134,135, neonatal intensive care admissions and hypoglycaemia15,92–95,108,109,111,113,118,128–132,136–143. In the longer term, indigenous women were shown to have a higher risk of developing T2DM after pregnancy13,14,21,96,112,144,145. Despite the search strategy not being designed for capturing all research about the risk of DIP to infants, 21% (31/145) of included studies demonstrated that infants born to women with DIP have a higher risk of developing obesity, hyperglycaemia, T2DM and renal disease16,128,146–165. One modelling study estimated that approximately 19–30% of T2DM among Canadian First Nations people is attributable to in utero exposure to GDM, compared with only 6% among the rest of the Canadian population 166. An impaired ‘acute insulin response’ among children exposed to DIP150,151 was proposed as a possible mechanism for the apparent intergenerational effect.
2. Current screening practice and rates
Seven studies described current screening practice and rates13,88,89,167–170. They suggested there has been little consistency in GDM screening rates among indigenous women, with some studies reporting less than 50% of women receiving screening in pregnancy13,88,89. One study in a remote island community in Australia reported 99.5% of women were screened during pregnancy 167; however, a review of other services in remote areas reported screening rates ranging from 3% to 78% 170. Two studies reported that women at high risk of GDM due to obesity were even less likely to receive screening than women of normal weight88,89.
3. Acceptability
No publications reported the acceptability of GDM screening for indigenous women, and only eight publications reported the preferences and values of indigenous women related to DIP more generally171–178. One opinion piece outlined from an indigenous perspective why a particular intervention that had intended to reduce GDM rates had not been effective 171, and another argued for the importance of looking at the ‘root cause’ of behavioural risk factors and engaging with indigenous communities to become advocates for social change 177. Three qualitative studies appraised as providing a moderate level of evidence described mixed levels of understanding of the risks and causes of DIP among both indigenous women and their care providers 172; outlined the importance of family ties, preserving cultural values and adapting resources, and ensuring access to blood sugar data as a means of control 176; and described the perceptions of weight gain and the challenges in losing it after pregnancy 178.
4. Screening test efficacy and cost
Two descriptive studies reported GDM screening efficacy at 24–28 weeks among indigenous women179,180. However, no studies reported the efficacy for GDM screening early in pregnancy in this population. One study, appraised as providing a high level of evidence, demonstrated that universal screening for GDM is significantly more sensitive than risk factor analysis alone 180. The second study suggested that the ‘one-step’ 2-h 75 g oral glucose tolerance test was more sensitive than the ‘two-step’ O'Sullivan criteria 179. One review suggested that the use of the HbA1c test is not appropriate as a diagnostic or screening test among non-European populations, as it has specificity and higher variability as a result of biological and genetic factors 181.
5. Effective treatment available after diagnosis
Six publications related to treatment strategies for DIP among indigenous women were identified, all of which were appraised as providing a low to very low level of evidence. Four publications were opinion pieces about the recommended treatment regimes for DIP144,182–184. One case–control study suggests insulin pumps may provide better glycaemic control; however, there were increased neonatal intensive care unit admissions in the intervention group, although they did have higher baseline insulin requirements 185. Another intervention study, with no control group, indicated that the development of an integrated care programme in a community-controlled health service improved monitoring for women 186. One study, appraised as providing a moderate level of evidence, reported higher rates of macrosomia for indigenous infants compared with non-indigenous infants, despite controlling for body mass index and GDM, and the authors suggested that the difference may be due to different treatment strategies for indigenous women 187.
6. Follow-up after pregnancy for women at risk of T2DM
Despite clear evidence that indigenous women have a higher risk of developing T2DM after pregnancy14,21,144,188, only five publications discussed follow-up after pregnancy. Three studies reported low rates (<40%) of follow-up screening for T2DM after pregnancy for indigenous women13,14,188. One project report described the development of a register designed to improve follow-up 189 but did not report whether this strategy was effective.
Other publications (including primary prevention)
One randomised controlled trial demonstrated a significant increase in the rate of knowledge of diabetes and obesity in the intervention group 190. Three studies, appraised as providing a low level of evidence, reported no effect from exercise or nutritional interventions191,192 and reported significant barriers to recruiting women to participate in the intervention 193. No rigorous evaluations of strategies to increase and support breastfeeding for indigenous women with DIP were found, despite solid evidence identifying breastfeeding as having a protective effect for infants against the development of T2DM16,194 and its feasibility for implementation in indigenous communities 195. Furthermore, although the importance of addressing broader environmental issues was proposed in four published opinion pieces177,196–198, there were no published evaluations of any environmental strategies to reduce DIP.
Discussion
This article has reviewed published studies related to DIP among indigenous women in Australia, Canada, New Zealand and the United States to evaluate the level of evidence available to address the criteria for population-based screening in early pregnancy. There was sufficient evidence describing the epidemiology of DIP, which clearly demonstrates that indigenous women have a higher risk of DIP, particularly T2DM, compared with other women in the same country. This has serious health consequences for both women and their infants in pregnancy, at birth and across the lifecourse. There was good evidence to suggest indigenous women meet the criteria for a population at ‘high risk’ of T2DM26,39, which is associated with a higher risk than GDM in pregnancy for women and their infants15,108,128–132. Early detection of DIP therefore offers potential benefits for women, their infants and the broader community, if effective interventions are provided.
However, there was insufficient evidence to determine that the remaining five criteria are met for introducing population-based screening for GDM in early pregnancy among indigenous women and to assess whether the potential benefits outweigh the risks. There was insufficient evidence to demonstrate that current screening practices are effective, with variable rates reported, and some evidence suggesting that women with the highest risk due to obesity may be even less likely to be screened. There was insufficient evidence to understand whether the proposed changes are acceptable to indigenous women or their preferences and values in relation to screening in early pregnancy. That no evidence exists concerning the acceptability of DIP screening options among indigenous women is a critical consideration because acceptability affects the overall sensitivity and effectiveness of screening when offered at a population level, irrespective of test efficacy199. Furthermore, there were no studies found evaluating the potential risks of early GDM diagnosis on indigenous women, including psychological stress or negative self-esteem, social dislocation or physical outcomes as a result of increased intervention 57. There was insufficient evidence to demonstrate which screening test is the most efficacious and cost effective in early pregnancy and that effective treatment options are available. There is a need to demonstrate effectiveness of strategies to improve screening and treatment in real-world settings, particularly as it has been suggested that differential rates of infant macrosomia may have been due to inequitable treatment for First Nations Canadian women diagnosed with GDM70,187. There was insufficient evidence that demonstrates an effective system to ensure follow-up after pregnancy for women diagnosed with GDM who have a high risk of developing T2DM. Studies among non-indigenous people suggest simple reminders may be effective200. In addition, there was very limited research conducted among indigenous women living in urban areas, despite this being where the majority of indigenous women now live201.
That only two publications written from an indigenous perspective were identified by this review represents an inherent perspective bias in the evidence-base for this topic area. The low rate of participation of indigenous people in higher education and research is likely to be a major reason for this paucity202. Another may be that public health research strives to portray an image of objectivity and rarely recognises the subjectivity of the standpoint of the people developing the research agendas or programmes64,203. However, diabetes is grounded in a complex web of social, historical and personal factors, and understanding perspectives and recognising relativity are critical to understanding and addressing this major public health issue204. In addition, the notion of ‘race’ itself is often used as a crude proxy marker for presumed biological and social differences, and therefore, research in this area would be better informed with social science input203.
There are several limitations to this review. Firstly, the heterogeneity of the study designs prohibited meta-analysis, so study findings were not weighted, and there were no analysis of the combined effect or sensitivity analysis for the effect of multiple confounders identified, including the risk of bias of included studies. Secondly, the data extraction and risk of bias appraisal was primarily conducted by one reviewer, and we were unable to calculate kappa scores as the high rates of expected concordance required a larger sample size than was feasible within the resource constraints of this review. Thirdly, the Australian population-based screening criteria used may differ from criteria used elsewhere 42. Fourth, it is likely that we have not captured all studies that have included indigenous women in a general sample, and some of the evidence from other populations may be relevant. However, this is likely to have been captured and assessed in recent similar reviews among the general population 26, and our reviews serves to shine the spotlight on the evidence for this sub-population. Finally, only published literature was used in this review, and a significant amount of grey literature was excluded. Inclusion of grey literature would have biased the search results in favour of the country the authors of the review originated (Australia), as familiarity and access to unpublished information was not as readily available across the other three countries.
Our finding that there is the limited evidence for GDM screening among indigenous women is similar to a review examining the evidence-base among non-indigenous women 26, although our analysis has shown that the quality and quantity of evidence for indigenous women is significantly more limited. This review makes similar conclusions to other major studies among non-indigenous women with regard to the risks of DIP 12, low rates of screening during and after pregnancy205,206, and the challenges with nutritional and exercise interventions to prevent or reduce GDM207–209. A review of research gaps for the general community also identified a need for more research into effective treatment and management strategies for women with DIP and for improved post-pregnancy follow-up210. This review reinforces the findings of other reviews, which conclude that indigenous women have a higher risk of DIP, particularly T2DM, at a younger age 2, and this will significantly increase following adoption of the proposed recommendations43,211–216. Although this review did not include studies with a sole focus on long-term risk to offspring of mothers with DIP, over 20% of included studies identified significant risks, which is consistent with findings of a recent review of the origins of cardiometabolic disease among indigenous populations217. Our findings are similar to another review that concluded there is a paucity of high quality interventions for T2DM in indigenous populations 73. This is of particular concern as several opinion pieces in this review argued for broader environmental approaches to reduce the burden of diabetes177,196–198, and it appears there is limited primary prevention interventions in diabetes research more generally. However, one study reported that an intervention that supported breastfeeding218 and promoted reduced soft-drink consumption was both feasible and effective in reducing obesity among Native American children219. This review was unable to identify any evidence that demonstrated treatment is as effective for indigenous women as it has been demonstrated for non-indigenous women23,24 or that demonstrated there are no detrimental psychological 54, social or physical consequences following GDM diagnosis, in either early or late pregnancy. Rather, one excluded abstract suggests this may be a greater concern for indigenous women 57.
Although this review highlights that the evidence-base is not sufficient to address the population-based screening criteria for indigenous women, studies in this review also demonstrate that more descriptive research alone is unlikely to improve health outcomes for indigenous women. Despite over 40 years of research in Pima Indian communities, which generated a predominance of high quality research compared with work from other indigenous communities 128, there has been little or no apparent improvement in related health outcomes.
There is an urgent need for strong evidence that demonstrates effective interventions for primary (prevention), secondary (early detection) and tertiary (treatment) prevention to mitigate the significant public health impact of DIP among indigenous women. All research in relation to DIP needs to consider equity. The level of uncertainty in the current evidence-base for population-based screening must be considered when introducing changes, and strategies should be employed to reduce the risks of intervening without sufficient evidence. These strategies include active collaboration and formative research with the communities involved and designing implementation plans with a capacity for reflective cycles and flexibility to respond to unforeseen consequences (e.g. action research), as well as comprehensive evaluation, so that learning can be shared with other communities. There is a need for evidence to develop strategies to improve consistency of screening during and after pregnancy. This should be informed by an understanding of women's preferences and values in relation to screening, evaluation of strategies where screening rates are high or low, and evidence from other screening programmes.
Conclusion
Diabetes in pregnancy imposes an inequitable disease burden on indigenous women and their infants. Recent International Association of Diabetes and Pregnancy Study Groups recommendations to provide early pregnancy screening for GDM for women in populations with a high risk of T2DM10,25 offer potential benefits through earlier detection and offering an opportunity to provide effective interventions to reduce the risk for both the mother and her infant in the short and longer term 11. However, evidence is urgently needed to demonstrate that these potential benefits outweigh the risks, including that the early GDM screening recommendations are acceptable to indigenous women, and that once diagnosed, effective treatment and follow-up after pregnancy are available. Researchers, clinicians and policy makers must work together with communities to develop effective primary, secondary and tertiary strategies to reduce the impact of DIP in indigenous populations.
Acknowledgments
Catherine Chamberlain is supported by a National Health and Medical Research Council PhD scholarship (607247) and a Population Health Capacity Building grant (457379). We are grateful to the staff at the Ian Potter Library, Monash University, for the assistance with searching for this review.
Appendix A
Sample search from Embase
exp "PARAMETERS CONCERNING THE FETUS, NEWBORN AND PREGNANCY" / or exp PREGNANCY/ or exp PREGNANCY OUTCOME/ or exp PREGNANCY COMPLICATION/
pregnan*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
exp prenatal diagnosis/ or exp prenatal care/
antenatal.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
prenatal.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
exp PRENATAL GROWTH/ or exp PRENATAL STRESS/ or exp PRENATAL DISORDER/ or exp PRENATAL PERIOD/ or exp PRENATAL DIAGNOSIS/ or exp PRENATAL MORTALITY/ or exp PRENATAL DEVELOPMENT/ or exp PRENATAL CARE/ or exp PRENATAL SCREENING/ or exp PRENATAL EXPOSURE/
1 or 2 or 3 or 4 or 5 or 6
newborn/
newborn*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
neonatal.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
infan*.mp.
fetal.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
exp " EMBRYONIC AND FETAL FUNCTIONS" / or exp FETAL WELL BEING/
fetus.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
fetus/
foetal.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
foetus.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
fetus/
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
7 or 19
exp diabetes mellitus/
diabet*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
21 or 22
hyperglyc?mi*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
exp hyperglycemia/
exp OBESITY/
obes*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
exp glucose intolerance/
glucose intoleran*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
24 or 25 or 26 or 27 or 28 or 29
23 or 30
20 and 31
exp pregnancy diabetes mellitus/
gestational diabet*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
33 or 34
exp INDIGENOUS PEOPLE/
indigen*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
exp ABORIGINE/
aborigin*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
36 or 37 or 38 or 39
32 or 35
40 and 41
31 and 40
20 and 40
limit 42 to yr = “2010 -Current”
torres strait*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
first nation*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
American Indian/
native*.mp.
Eskimo/
alaska* native*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
Maori/
maori*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
inuit*.mp.
46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54
(41 and 55) not 42
*American Samoa/
american samoa*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
native hawai*.mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
aleut.mp.
57 or 58 or 59 or 60
(61 and 41) not (42 or 56)
Author contributions
C. C. planned the research, extracted data, conducted analysis and drafted the manuscript. B. M. provided assistance with drafts and designing the evidence table (Table 2). D. Y. co-reviewed some publications and provided input into drafts. E. W. co-reviewed abstracts for inclusion and provided input into drafts. J. O. and B. O. provided input into drafts. S. E. provided advice on planning the review and provided input into drafts. All authors read and approved the final manuscript.
Conflict of interest
The authors have no conflicts of interest.
Supplementary material
Supporting information may be found in the online version of this article.
References
- 1.HAPO Study Cooperative Research Group. Hyperglycaemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991–2002. doi: 10.1056/NEJMoa0707943. [DOI] [PubMed] [Google Scholar]
- 2.Bhattarai MD. Three patterns of rising type 2 diabetes prevalence in the world: need to widen the concept of prevention in individuals into control in the community. J. Nepal Med. Assoc. 2009;48(174):173–179. [PubMed] [Google Scholar]
- 3.Sicree R, Shaw J, Zimmet P. The global burden diabetes and impaired glucose tolerance. Diabetes. 2009;27:1–105. [Google Scholar]
- 4.Naqshbandi M, Harris S, Esler J, Antwi-Nsiah F. Global complication rates of type 2 diabetes in indigenous peoples: a comprehensive review. Diabetes Res Clin Pract. 2008;82(1):1–17. doi: 10.1016/j.diabres.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 5.Bowman BA, Gregg EW, Williams DE, Engelgau MM, Jack LJ. Translating the science of primary, secondary, and tertiary prevention to inform the public health response to diabetes. J Public Health Manag Pract. 2003;9:S8–S14. doi: 10.1097/00124784-200311001-00002. [DOI] [PubMed] [Google Scholar]
- 6.Mazze RS, Langer O. Primary, secondary, and tertiary prevention program for diabetes in pregnancy. Diabetes Care. 1988;11(3):263–268. doi: 10.2337/diacare.11.3.263. [DOI] [PubMed] [Google Scholar]
- 7.Iams JD, Romero R, Culhane JF, Goldenberg RL. Primary, secondary, and tertiary interventions to reduce the morbidity and mortality of preterm birth. Lancet. 2008;371(9607):164–175. doi: 10.1016/S0140-6736(08)60108-7. [DOI] [PubMed] [Google Scholar]
- 8.Tugwell P, Petticrew M, Kristjansson E, et al. Assessing equity in systematic reviews: realising the recommendations of the Commission on Social Determinants of Health. BMJ. 2010:341. doi: 10.1136/bmj.c4739. (c4739) [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association. Diagnosis and classification of diabetes mellitus (position statement) Diabetes Care. 2009;32(Suppl 1):S62–S67. doi: 10.2337/dc09-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care. 2011;34(Supplement 1):S11–S61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coustan DR. Finding and treating gestational diabetes mellitus–does it help? Nat Rev Endocrinol. 2010;6(10):540(543). doi: 10.1038/nrendo.2010.148. [DOI] [PubMed] [Google Scholar]
- 12.Coustan DR, Lowe LP, Metzger BE, Dyer AR. The Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) study: paving the way for new diagnostic criteria for gestational diabetes mellitus. Am J Obstet Gynecol. 2010;202:654.e651. doi: 10.1016/j.ajog.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohamed N, Dooley J. Gestational diabetes and subsequent development of NIDDM in aboriginal women of northwestern Ontario. Int J Circumpolar Health. 1998;57(Suppl 1):355–358. [PubMed] [Google Scholar]
- 14.Steinhart JR, Sugarman JR, Connell FA. Gestational diabetes is a herald of NIDDM in Navajo women. High rate of abnormal glucose tolerance after GDM. Diabetes Care. 1997;20(6):943–947. doi: 10.2337/diacare.20.6.943. [DOI] [PubMed] [Google Scholar]
- 15.Bower C, Stanley F, Connell AF, Gent CR, Massey MS. Birth defects in the infants of aboriginal and non-aboriginal mothers with diabetes in Western Australia. Med J Aust. 1992;156(8):520–524. doi: 10.5694/j.1326-5377.1992.tb121410.x. [DOI] [PubMed] [Google Scholar]
- 16.Pettitt DJ, Knowler WC. Long-term effects of the intrauterine environment, birth weight, and breast-feeding in Pima Indians. Diabetes Care. 1998;21(Suppl 2):B138–141. [PubMed] [Google Scholar]
- 17.Cheung NW, McElduff A, Ross G. Type 2 diabetes in pregnancy: a wolf in sheep's clothing. Aust N Z J Obstet Gynaecol. 2005;45(6):479–483. doi: 10.1111/j.1479-828X.2005.00480.x. [DOI] [PubMed] [Google Scholar]
- 18.Australian Institute of Health and Welfare. Diabetes in pregnancy: its impact on Australian women and their babies. Canberra: AIHW; 2010. [Google Scholar]
- 19.Porter C, Skinner T, Ellis I. What is the impact of diabetes for Australian Aboriginal women when pregnant? Diabetes Res Clin Pract. 2011;93(1):e29–32. doi: 10.1016/j.diabres.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 20.Osgood ND, Dyck RF, Grassmann WK. The inter- and intragenerational impact of gestational diabetes on the epidemic of type 2 diabetes. Am J Public Health. 2011;101(1):173–179. doi: 10.2105/AJPH.2009.186890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dyck R, Osgood N, Lin TH, Gao A, Stang MR. Epidemiology of diabetes mellitus among First Nations and non-First Nations adults. Can Med Assoc J. 2010;182(3):249–256. doi: 10.1503/cmaj.090846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrara A. Increasing prevalence of gestational diabetes mellitus. Diabetes Care. 2007;30(Supplement 2):S141–S146. doi: 10.2337/dc07-s206. [DOI] [PubMed] [Google Scholar]
- 23.Landon M, Spong C, Thom E, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009;361:1339–1348. doi: 10.1056/NEJMoa0902430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crowther C, Hiller J, Moss J, McPhee A, Jeffries W, Robinson J. Australian carbohydrate intolerance study in pregnant women (ACHOIS) trial group: effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477–2486. doi: 10.1056/NEJMoa042973. [DOI] [PubMed] [Google Scholar]
- 25.International Association of Diabetes and Pregnancy Study Groups. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycaemia in pregnancy. Diabetes Care. 2010;33(3):676–682. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waugh N, Pearson D, Royle P. Screening for hyperglycaemia in pregnancy: consensus and controversy. Best Pract Res Clin Endocrinol Metab. 2010;24:553–571. doi: 10.1016/j.beem.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Hiéronimusa S, Le Meauxb J. Relevance of gestational diabetes mellitus screening and comparison of selective with universal strategies. Diabetes Metab. 2010;36:575–586. doi: 10.1016/j.diabet.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 28.Huynh J, Ratnaike S, Bartalotta C, Permezel M, Houlihan C. Challenging the glucose challenge test. Aust N Z J Obstet Gynaecol. 2011;51:22–25. doi: 10.1111/j.1479-828X.2010.01247.x. [DOI] [PubMed] [Google Scholar]
- 29.Holt RI, Jacklin PB, Round JA, Mugglestone MA, Hughes RG. Gestational diabetes mellitus: NICE for the US? A comparison of the American Diabetes Association and the College of Obstetricians and Gynecologists Guidelines with the UK National Institute for health and Clinical Excellence Guidelines. Diabetes Care. 2010;33(3):e46–47. doi: 10.2337/dc09-2234. [DOI] [PubMed] [Google Scholar]
- 30.Simmons D, McElduff A, McIntyre HD, Elrish M. Gestational diabetes mellitus: NICE for the US? A comparison of the American Diabetes Association and the American College of Obstetricians and Gynecologists Guidelines with the UK National Institute for Health and Clinical Excellence Guidelines. Diabetes Care. 2010;33(3):e48. doi: 10.2337/dc09-1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brill D. New gestational diabetes plan divides expert opinion. Diabetes Care. 2010;33:690–691. [Google Scholar]
- 32.Riskin-Mashiah S, Damti A, Younes G, Auslander R. Normal fasting plasma glucose levels during pregnancy: a hospital-based study. J Perinat Med. 2011;39:209–211. doi: 10.1515/jpm.2010.142. [DOI] [PubMed] [Google Scholar]
- 33.Argarwal M, Weigl B, Hod M. Gestational diabetes screening: the low cost algorithm. Int J Gynaecol Obstet. 2011;115(Suppl 1):S30–S33. doi: 10.1016/S0020-7292(11)60009-X. [DOI] [PubMed] [Google Scholar]
- 34.Karakash S, Einstein F. Diabetes in pregnancy: glycaemia control guidelines and rationale. Curr Opin Endocrinol Diabetes Obes. 2011;18:99–103. doi: 10.1097/MED.0b013e3283446ed2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cundy T. Proposed new diagnostic criteria for gestational diabetes – a pause for thought? Diabet Med. 2012;29:176–180. doi: 10.1111/j.1464-5491.2011.03407.x. [DOI] [PubMed] [Google Scholar]
- 36.Blackwell S, Rouse D. Gestational diabetes—staying with old or marrying new guidelines. Am J Obstet Gynecol. 2011;204(5):371–372. doi: 10.1016/j.ajog.2011.02.073. [DOI] [PubMed] [Google Scholar]
- 37.Long H. Diagnosing gestational diabetes: can expert opinion replace scientific evidence. Diabetologica. 2011;54:2211–2213. doi: 10.1007/s00125-011-2228-z. [DOI] [PubMed] [Google Scholar]
- 38.Wendland EM, Torloni MR, Falavigna M, et al. Gestational diabetes and pregnancy outcomes – a systematic review of the World Health Organization (WHO) and the International Association of Diabetes in Pregnancy Study Groups (IADPSG) diagnostic criteria. BMC Pregnancy Childbirth. 2012;12:23. doi: 10.1186/1471-2393-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leary J, Pettitt DJ, Jovanovic L. Gestational diabetes guidelines in a HAPO world. Best Pract Res Clin Endocrinol Metab. 2010;24:673–685. doi: 10.1016/j.beem.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 40.Australian Health Ministers' Advisory Council. Population Based Screening Framework. Commonwealth of Australia: Barton; 2008. p. P3-4669. [Google Scholar]
- 41.Wilson J, Jungner G. Principles and Practice of screening for disease. Public Health Paper Number 34. Geneva: WHO; 1968. [Google Scholar]
- 42.UK National Screening Committee. Criteria for appraising the viability, effectiveness and appropriateness of a screening programme. 2010. http://www.screening.nhs.uk/criteria. Accessed 24/2/2010.
- 43.Lindsay RS. Gestational diabetes: costs and consequences. Diabetologica. 2011;54:227–229. doi: 10.1007/s00125-010-1979-2. [DOI] [PubMed] [Google Scholar]
- 44.Oteng-Ntim E, Varma R, Croker H, Poston L, Doyle P. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: systematic review and meta-analysis. BMC Med. 2012;10(1):47. doi: 10.1186/1741-7015-10-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kalra S, Malik S, John M. Gestational diabetes mellitus: a window of opportunity. Indian J. Endocrinol. Metab. 2011;15(3):149–151. doi: 10.4103/2230-8210.83395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Altman J. Pregnancy, a window of opportunity for diabetes prevention: a case study from France. 2011.
- 47.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 48.Orleans CT, Barker DC, Kaufman NJ, Marx JF. Helping pregnant smokers quit: meeting the challenge in the next decade. Tob Control. 2000;9(suppl 3):iii6–iii11. doi: 10.1136/tc.9.suppl_3.iii6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bilhartz T, Bilhartz P, Bilhartz T, Bilhartz R. Making use of a natural stress test: pregnancy and cardiovascular risk. J Womens Health. 2011;20(5):695–701. doi: 10.1089/jwh.2010.2291. [DOI] [PubMed] [Google Scholar]
- 50.Brown W, Trost S. Life transitions and changing physical activity patterns in young women. Am J Prev Med. 2003;25(2):140–143. doi: 10.1016/s0749-3797(03)00119-3. [DOI] [PubMed] [Google Scholar]
- 51.Moran LJ, Lombard CB, Lim S, Noakes M, Teede HJ. Polycystic ovary syndrome and weight management. Womens Health. 2010;6(2):271(213). doi: 10.2217/whe.09.89. [DOI] [PubMed] [Google Scholar]
- 52.Sable MJ, Wilkinson DS. Impact of perceived stress, major life events and pregnancy attitudes on low birth weight. Fam Plann Perspect. 2000;32(6):288–294. [PubMed] [Google Scholar]
- 53.Daniells S, Grenyer B, Davis W, Coleman K, Burgess J, Moses R. Gestational diabetes mellitus: is a diagnosis assoicated with an increase in maternal anxiety and stress in the short and intermediate term? Diabetes Care. 2003;26:385–389. doi: 10.2337/diacare.26.2.385. [DOI] [PubMed] [Google Scholar]
- 54.Rumbold A, Crowther C. Women's experiences of being screened for gestational diabetes mellitus. Aust N Z J Obstet Gynaecol. 2002;42:131–137. doi: 10.1111/j.0004-8666.2002.00131.x. [DOI] [PubMed] [Google Scholar]
- 55.Langer N, Langer O. Emotional adjustment to diagnosis and intensified treatment of gestational diabetes. Obstet Gynecol. 1994;84:329–334. [PubMed] [Google Scholar]
- 56.Cosson E. Diagnostic criteria for gestational diabetes mellitus. Diabetes Metab. 2010;36:538–548. doi: 10.1016/j.diabet.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 57.Jones EJ, Appel SJ. High levels of cardiometabolic risk, knowledge, and risk perception co-occur with low self-efficacy to prevent cardiometabolic disease in American indian women with previous gestational diabetes. JOGNN. 2011;41(2):246–57. doi: 10.1111/j.1552-6909.2012.01339.x. [DOI] [PubMed] [Google Scholar]
- 58.Roberts C, Tracy S, Peat B. Rates for obstetric intervention among private and public patients in Australia: population based descriptive study. BMJ. 2000;321:137–141. doi: 10.1136/bmj.321.7254.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Naylor M, Sermer C, Chen E, Sykora K. Caesarean delivery in relation to birthweight and gestational glucose intolerance; pathophysiology or pactice style? JAMA. 1996;275:1165–1170. [PubMed] [Google Scholar]
- 60.Rose G. The Strategy of Preventive Medicine. Oxford: Oxford University Press; 1992. [Google Scholar]
- 61.Jones CP. Invited Commentary: “Race,” Racism, and the Practice of Epidemiology. Am J Epidemiol. 2001;154(4):299–304. doi: 10.1093/aje/154.4.299. [DOI] [PubMed] [Google Scholar]
- 62.Tull E, Sheu Y, Butler C, Cornelious K. Relationships between perceived stress, coping behavior and cortisol secretion in women with high and low levels of internalized racism. J Natl Med Assoc. 2005;97(2):206–212. [PMC free article] [PubMed] [Google Scholar]
- 63.Anderson I, Whyte J, editors. Populations at Special Health Risk: Indigenous Populations. San Diego, USA: Academic Press; 2008. International Encyclopedia of Public Health; [Google Scholar]
- 64.Morgan M. Sociological investigations. In: Holland W, Detels R, Knox G, editors. Oxford Textbook of Public Health. VII. Oxford: Oxford University Press; 1997. pp. 309–330. [Google Scholar]
- 65.Yeates K, Tonelli M. Indigenous health: update on the impact of diabetes and chronic kidney disease. Curr Opin Nephrol Hypertens. 2006;15:588–592. doi: 10.1097/01.mnh.0000247495.54882.e4. [DOI] [PubMed] [Google Scholar]
- 66.Yeates K, Schaubel D, Cass A, Sequist T, Ayanian J. Access to renal transplantation for minority patients with ESRD in Canada. Am J Kidney Dis. 2004;44(6):1083–1089. doi: 10.1053/j.ajkd.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 67.Sequist T, Narva A, Stiles S, Karp S, Cass A, Ayanian J. Access to renal transplantation among American Indians and Hispanics. Am J Kidney Dis. 2004;44(2):344–352. doi: 10.1053/j.ajkd.2004.04.039. [DOI] [PubMed] [Google Scholar]
- 68.Epstein A, Ayanian J, Keogh J, et al. Racial disparities in access to renal transplantation—clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343(21):1537–1544. doi: 10.1056/NEJM200011233432106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.McDonald SP, Russ GR. Current incidence, treatment patterns and outcome of end-stage renal disease among indigenous groups in Australia and New Zealand. Nephrol. 2003;8(1):42–48. doi: 10.1046/j.1440-1797.2003.00131.x. [DOI] [PubMed] [Google Scholar]
- 70.Liu SL, Shah BR, Naqshbandi M, Tran V, Harris SB. Increased rates of adverse outcomes for gestational diabetes and pre-pregnancy diabetes in on-reserve First Nations Women in Ontario, Canada. Diabet Med. 2012;29(8):1464–5491. doi: 10.1111/j.1464-5491.2012.03691.x. [DOI] [PubMed] [Google Scholar]
- 71.Albertsen P. Efficacy vs effectiveness in prostate-specific antigen screening. J Natl Cancer Inst. 2010;102(5):288–289. doi: 10.1093/jnci/djq002. [DOI] [PubMed] [Google Scholar]
- 72.Chamberlain C, Yore D, Li H, et al. Diabetes in pregnancy among indigenous women in Australia, Canada, New Zealand, and the United States: a method for systematic review of studies with different designs. BMC Pregnancy Childbirth. 2011;11(104) doi: 10.1186/1471-2393-11-104. doi: 10.1186/1471-2393-11-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McNamara BJ, Sanson-Fisher R, D'Este C, Eades S. Type 2 diabetes in Indigenous populations: quality of intervention research over 20 years. Prev Med. 2011;52:3–9. doi: 10.1016/j.ypmed.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 74.Sanson-Fisher R. Indigenous health research: a critical review of outputs over time. Med J Aust. 2006;184(10):502–505. doi: 10.5694/j.1326-5377.2006.tb00343.x. [DOI] [PubMed] [Google Scholar]
- 75.Centre for Evidence-Based Medicine. Critical Appraisal Sheet for Treatment. 2010. http://www.cebm.net/index.aspx?o=1157. Accessed 3/12/2010, 2010.
- 76.Centre for Evidence-Based Medicine. Diagnostic Critical Appraisal Sheet. 2010. http://www.cebm.net/index.aspx?o=1157. Accessed 3/12/2010, 2010.
- 77.Centre for Evidence-Based Medicine. Critical Appraisal Sheet for Systematic Reviews. 2010. http://www.cebm.net/index.aspx?o=1157. Accessed 3/12/2010, 2010.
- 78.Department of General Practice. Critical Appraisal Checklist for an article on Qualitative Research. 2010. http://www.gla.ac.uk/media/media_64038_en.pdf. Accessed 3/12/2010, 2010.
- 79.Treloar C, Champness S, Simpson P, Higginbotham N. Critical appraisal checklist for qualitative research studies. Indian J Pediatr. 2000;67(5):347–351. doi: 10.1007/BF02820685. [DOI] [PubMed] [Google Scholar]
- 80.von Elm E, Altman D, Egger M, Pocock S, Gotzsche P, Vandenbrouke J. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 81.Shah P. Paternal factors and low birth weight, preterm, and small for gestational age births: a systematic review. Am. College Obstetrics Gynecology. 2010:103–120. doi: 10.1016/j.ajog.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 82.Centre for Clinical Effectiveness. Evidence-Based Answers to Clinical Questions for Busy Clinicians Workbook. 2009. http://www.southernhealth.org.au/icms_docs/2145_EBP_workbook.pdf Accessed 14/12/2012.
- 83.Balshem H, Helfand M, Schunemann H, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 84.Cochrane HIV/AIDS Group. The GRADE Approach to Rating the Quality of Evidence. 2010. http://www.igh.org/Cochrane/grade-intro.ppt. Accessed 8/3/2011.
- 85.Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander health performance framework. Canberra: Australian Institute of Health and Welfare; 2008. [Google Scholar]
- 86.Dyck R, Klomp H, Tan LK, Turnell RW, Boctor MA. A comparison of rates, risk factors, and outcomes of gestational diabetes between aboriginal and non-aboriginal women in the Saskatoon health district. Diabetes Care. 2002;25(3):487–493. doi: 10.2337/diacare.25.3.487. [DOI] [PubMed] [Google Scholar]
- 87.Wu PL, Sadler GR, Nguyen V, et al. Diabetes management in San Diego's Chamorro community. Diabetes Educ. 2005;31(3):379–390. doi: 10.1177/0145721705276579. [DOI] [PubMed] [Google Scholar]
- 88.Yapa M, Simmons D. Screening for gestational diabetes mellitus in a multiethnic population in New Zealand. Diabetes Res Clin Pract. 2000;48:217–223. doi: 10.1016/s0168-8227(99)00150-3. [DOI] [PubMed] [Google Scholar]
- 89.Rith-Najarian SJ, Ness FK, Faulhaber T, Gohdes DM. Screening and diagnosis for gestational diabetes mellitus among Chippewa women in northern Minnesota. Minn Med. 1996;79(5):21–25. [PubMed] [Google Scholar]
- 90.Simmons D, Khan MA, Teale G, Simmons D, Khan MA, Teale G. Obstetric outcomes among rural Aboriginal Victorians. Aust N Z J Obstet Gynaecol. 2005;45(1):68–70. doi: 10.1111/j.1479-828X.2005.00331.x. [DOI] [PubMed] [Google Scholar]
- 91.Aljohani N, Rempel B, Ludwig S, et al. Gestational diabetes in Manitoba during a twenty-year period. Clin Invest Med. 2008;31(3):E131–137. doi: 10.25011/cim.v31i3.3470. [DOI] [PubMed] [Google Scholar]
- 92.Hughes R, Rowan J. Perinatal outcomes and macrosomia in a multi-ethnic population of women with type 2 diabetes. Aust N Z J Obstet Gynaecol. 2006;46(6):552–555. doi: 10.1111/j.1479-828X.2006.00659.x. [DOI] [PubMed] [Google Scholar]
- 93.Godwin M, Muirhead M, Huynh J, Helt B, Grimmer J. Prevalence of gestational diabetes mellitus among Swampy Cree women in Moose Factory, James Bay. Can Med Assoc J. 1999;160(9):1299–1302. [PMC free article] [PubMed] [Google Scholar]
- 94.Davis B, Bond D, Howat P, et al. Maternal and neonatal outcomes following diabetes in pregnancy in Far North Queensland, Australia. Aust N Z J Obstet Gynaecol. 2009;49(4):393–399. doi: 10.1111/j.1479-828X.2009.01021.x. [DOI] [PubMed] [Google Scholar]
- 95.Hart G, MacHarper T, Moore D, Roder D. Aboriginal pregnancies and births in South Australia, 1981-1982. Med J Aust. 1985;143(9 Suppl):S54–56. doi: 10.5694/j.1326-5377.1985.tb120103.x. [DOI] [PubMed] [Google Scholar]
- 96.Yue DK, Molyneaux LM, Ross GP, Constantino MI, Child AG, Turtle JR. Why does ethnicity affect prevalence of gestational diabetes? The underwater volcano theory. Diabet Med. 1996;13(8):748–752. doi: 10.1002/(SICI)1096-9136(199608)13:8<748::AID-DIA164>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 97.Stone CA, McLachlan KA, Halliday JL, et al. Gestational diabetes in Victoria in 1996: incidence, risk factors and outcomes. Med J Aust. 2002;177(9):486–491. doi: 10.5694/j.1326-5377.2002.tb04916.x. [DOI] [PubMed] [Google Scholar]
- 98.Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander Health Performance Framework 2008 report: detailed analyses. 2008. Canberra: Cat. no. IHW 22.
- 99.Rodrigues S, Robinson EJ, Ghezzo H, Gray-Donald K. Interaction of body weight and ethnicity on risk of gestational diabetes mellitus. Am J Clin Nutr. 1999;70(6):1083–1089. doi: 10.1093/ajcn/70.6.1083. [DOI] [PubMed] [Google Scholar]
- 100.Templeton M, Pieris-Caldwell I. Canberra: Australian Institute of Health and Welfare; 2008. Gestational diabetes mellitus in Australia, 2005-06. [Google Scholar]
- 101.Livingston RC, Bachman-Carter K, Frank C, Mason WB. Diabetes mellitus in Tohon O'odham pregnancies. Diabetes Care. 1993;16(1):318–321. doi: 10.2337/diacare.16.1.318. [DOI] [PubMed] [Google Scholar]
- 102.Sugarman JR. Prevalence of gestational diabetes in a Navajo Indian community. West J Med. 1989;150(5):548–551. [PMC free article] [PubMed] [Google Scholar]
- 103.Ishak M, Petocz P, Ishak M, Petocz P. Gestational diabetes among Aboriginal Australians: prevalence, time trend, and comparisons with non-Aboriginal Australians. Ethn Dis. 2003;13(1):55–60. [PubMed] [Google Scholar]
- 104.Murphy NJ, Bulkow LR, Schraer CD, Lanier AP. Prevalence of diabetes mellitus in pregnancy among Yup'ik Eskimos, 1987-1988. [Erratum appears in Diabetes Care 1993 Apr;16(4):667] Diabetes Care. 1993;16(1):315–317. doi: 10.2337/diacare.16.1.315. [DOI] [PubMed] [Google Scholar]
- 105.Oster RT, Toth EL, Oster RT, Toth EL. Differences in the prevalence of diabetes risk-factors among First Nation, Metis and non-Aboriginal adults attending screening clinics in rural Alberta, Canada. Rural Remote Health. 2009;9(2):1170. [PubMed] [Google Scholar]
- 106.Harris SB, Caulfield LE, Sugamori ME, Whalen EA, Henning B. The epidemiology of diabetes in pregnant Native Canadians. A risk profile. Diabetes Care. 1997;20(9):1422–1425. doi: 10.2337/diacare.20.9.1422. [DOI] [PubMed] [Google Scholar]
- 107.Brennand EA, Dannenbaum D, Willows ND, Brennand EA, Dannenbaum D, Willows ND. Pregnancy outcomes of First Nations women in relation to pregravid weight and pregnancy weight gain. J Obstet Gynaecol Can. 2005;27(10):936–944. doi: 10.1016/s1701-2163(16)30739-3. [DOI] [PubMed] [Google Scholar]
- 108.Stanley FJ, Priscott PK, Johnston R, Brooks B, Bower C. Congenital malformations in infants of mothers with diabetes and epilepsy in Western Australia, 1980-1982. Med J Aust. 1985;143(10):440–442. doi: 10.5694/j.1326-5377.1985.tb123132.x. [DOI] [PubMed] [Google Scholar]
- 109.Silva JK, Kaholokula JKa, Ratner R, Mau M. Ethnic differences in perinatal outcome of gestational diabetes mellitus. Diabetes Care. 2006;29(9):2058–2063. doi: 10.2337/dc06-0458. [DOI] [PubMed] [Google Scholar]
- 110.Blair E. Why do aboriginal newborns weigh less? Determinants of birthweight for gestation. J Paediatr Child Health. 1996;32(6):498–503. doi: 10.1111/j.1440-1754.1996.tb00962.x. [DOI] [PubMed] [Google Scholar]
- 111.Schiff M, Rogers C. Factors predicting cesarean delivery for American Indian women in New Mexico. Birth. 1999;26(4):226–231. doi: 10.1046/j.1523-536x.1999.00226.x. [DOI] [PubMed] [Google Scholar]
- 112.Benjamin E, Winters D, Mayfield J, Gohdes D. Diabetes in pregnancy in Zuni Indian women. Prevalence and subsequent development of clinical diabetes after gestational diabetes. Diabetes Care. 1993;16(9):1231–1235. doi: 10.2337/diacare.16.9.1231. [DOI] [PubMed] [Google Scholar]
- 113.Bennett PH, Rushforth NB, Miller M, LeCompte PM. Epidemiologic studies of diabetes in the Pima Indians. Recent Prog Horm Res. 1976;32:333–376. doi: 10.1016/b978-0-12-571132-6.50021-x. [DOI] [PubMed] [Google Scholar]
- 114.Moum KR, Holzman GS, Harwell TS, et al. Increasing rate of diabetes in pregnancy among American Indian and white mothers in Montana and North Dakota, 1989-2000. Matern Child Health J. 2004;8(2):71–76. doi: 10.1023/b:maci.0000025729.65328.73. [DOI] [PubMed] [Google Scholar]
- 115.Murphy NJ, Bulkow LR, Schraer CD, Lanier AP. Prevalence of diabetes mellitus in pregnancy among Yup'ik Eskimos and Alaska Coastal Indians, 1987-1988. Arctic Med Res. 1991;(Suppl):423–426. [PubMed] [Google Scholar]
- 116.Patel M. Should all pregnant women be offered a test for diabetes? Aboriginal Health Inf. Bull. 1989;12:24–29. [Google Scholar]
- 117.LaVallie DL, Gabbe SG, Grossman DC, et al. Birth outcomes among American Indian/Alaska Native women with diabetes in pregnancy. J Reprod Med. 2003;48(8):610–616. [PubMed] [Google Scholar]
- 118.Kuberski TT, Bennett PH. Diabetes mellitus as an emerging public health problem on Guam. Diabetes Care. 1980;3(2):235–241. doi: 10.2337/diacare.3.2.235. [DOI] [PubMed] [Google Scholar]
- 119.Scavini M, Stidley CA, Shah VO, et al. Prevalence of diabetes is higher among female than male Zuni indians. Diabetes Care. 2003;26(1):55–60. doi: 10.2337/diacare.26.1.55. [DOI] [PubMed] [Google Scholar]
- 120.Kieffer EC, Martin JA, Herman WH. Impact of maternal nativity on the prevalence of diabetes during pregnancy among U.S. ethnic groups. Diabetes Care. 1999;22(5):729–735. doi: 10.2337/diacare.22.5.729. [DOI] [PubMed] [Google Scholar]
- 121.Alur P, Kodiyanplakkal P, Del Rosario A, et al. Epidemiology of infants of diabetic mothers in indigenous Micronesian population-Guam experience. Pac Health Dialog. 2002;9(2):219–221. [PubMed] [Google Scholar]
- 122.Campbell SK, Lynch J, Esterman A, McDermott R. Pre-pregnancy predictors of diabetes in pregnancy among aboriginal and Torres Strait Islander women in north Queensland, Australia. Matern Child Health J. 2012;16(6):1284–1292. doi: 10.1007/s10995-011-0889-3. [DOI] [PubMed] [Google Scholar]
- 123.Kim SY, England L, Sappenfield W, et al. Racial/ethnic differences in the percentage of gestational diabetes mellitus cases attributable to overweight and obesity, Florida, 2004-2007. Prev Chronic Dis. 2012;9:E88. doi: 10.5888/pcd9.110249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Denny CH, Floyd RL, Green PP, Hayes DK. The prevalence of multiple risk factors for poor birth outcomes among women of childbearing age. Alcohol Clin Exp Res. 2010;34(6):212A. [Google Scholar]
- 125.Devlin HM, Desai J, Holzman GS, Gilbertson DT. Trends and disparities among diabetes-complicated births in Minnesota, 1993-2003. Am J Public Health. 2008;98(1):59–62. doi: 10.2105/AJPH.2006.095877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Anonymous. Diabetes and impaired glucose tolerance in women aged 20-39 years. World Health Organization Ad Hoc Diabetes Reporting Group. World Health Statistics Q. Rapport Trimestriel de Statistiques Sanitaires Mondiales. 1992;45(4):321–327. [PubMed] [Google Scholar]
- 127.Caughey AB, Cheng YW, Stotland NE, Washington AE, Escobar GJ. Maternal and paternal race/ethnicity are both associated with gestational diabetes. Am J Obstet Gynecol. 2010;202(616):e1–5. doi: 10.1016/j.ajog.2010.01.082. [DOI] [PubMed] [Google Scholar]
- 128.Lindsay RS, Hanson RL, Bennett PH, Knowler WC. Secular trends in birth weight, BMI, and diabetes in the offspring of diabetic mothers. Diabetes Care. 2000;23(9):1249–1254. doi: 10.2337/diacare.23.9.1249. [DOI] [PubMed] [Google Scholar]
- 129.Aljohani N, Rempel B, Ludwig S, et al. Impact of diabetes on maternal-fetal outcomes in Manitoba: relationship with ethnic and environmental factors. Clin Invest Med. 2008;31(6):E338–345. doi: 10.25011/cim.v31i6.4919. [DOI] [PubMed] [Google Scholar]
- 130.Caulfield LE, Harris SB, Whalen EA, Sugamori ME. Maternal nutritional status, diabetes and risk of macrosomia among Native Canadian women. Early Hum Dev. 1998;50(3):293–303. doi: 10.1016/s0378-3782(97)00074-1. [DOI] [PubMed] [Google Scholar]
- 131.Bennett PH, Webner C, Miller M. Congenital Anomalies and the Diabetic and Prediabetic Pregnancy. In: Elliott K, O'Connor M, editors. In Ciba Foundation Symposium 63 - Pregnancy Metabolism, Diabetes and the Fetus. Chichester, UK: John Wiley & Sons, Ltd; 2008. pp. 207–225. [DOI] [PubMed] [Google Scholar]
- 132.Comess LJ, Bennett PH, Burch TA, Miller M. Congenital anomalies and diabetes in the Pima Indians of Arizona. Diabetes. 1969;18(7):471–477. doi: 10.2337/diab.18.7.471. [DOI] [PubMed] [Google Scholar]
- 133.Roberts AB, Pattison NS. Pregnancy in women with diabetes mellitus, twenty years experience: 1968-1987. N Z Med J. 1990;103:211–213. [PubMed] [Google Scholar]
- 134.Cundy T, Gamble G, Manuel A, Townend K, Roberts A. Determinants of birth-weight in women with established and gestational diabetes. Aust N Z J Obstet Gynaecol. 1993;33(3):249–254. doi: 10.1111/j.1479-828x.1993.tb02078.x. [DOI] [PubMed] [Google Scholar]
- 135.Dyck R, Osgood N, Lin TH, Gao A, Stang MR. Epidemiology of diabetes mellitus among First Nations and non-First Nations adults. Can Med Assoc J. 2010;182(3):249–256. doi: 10.1503/cmaj.090846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Nicolle LE, Friesen D, Harding GK, Roos LL. Hospitalization for acute pyelonephritis in Manitoba, Canada, during the period from 1989 to 1992; impact of diabetes, pregnancy, and aboriginal origin. Clin Infect Dis. 1996;22(6):1051–1056. doi: 10.1093/clinids/22.6.1051. [DOI] [PubMed] [Google Scholar]
- 137.Jin A, Martin JD, Sarin C, Jin A, Martin JD, Sarin C. Diabetes mellitus in the First Nations population of British Columbia, Canada. Part 2. Hospital morbidity. Int J Circumpolar Health. 2002;61(3):254–259. doi: 10.3402/ijch.v61i3.17459. [DOI] [PubMed] [Google Scholar]
- 138.Mendola P, Buck G, Starr ER. Developmental disabilities prevention and the distribution of risk among American Indians. Am Indian Alsk Native Ment Health Res. 1994;5(3):30–44. doi: 10.5820/aian.0503.1994.30. [DOI] [PubMed] [Google Scholar]
- 139.Adams MS, Brown KS, Iba BY, Niswander JD. Health of Papago Indian children. Public Health Rep. 1970;85(12):1047–1061. [PMC free article] [PubMed] [Google Scholar]
- 140.Pettitt DJ, Knowler WC, Baird HR, Bennett PH. Gestational diabetes: infant and maternal complications of pregnancy in relation to third-trimester glucose tolerance in the Pima Indians. Diabetes Care. 1980;3(3):458–464. doi: 10.2337/diacare.3.3.458. [DOI] [PubMed] [Google Scholar]
- 141.Thomson M. Heavy birthweight in Native Indians of British Columbia. Can. J. Publ. Health Revue Canadienne de Sante Publique. 1990;81(6):443–446. [PubMed] [Google Scholar]
- 142.Claydon J, Mitton C, Sankaran K, Lee S. Ethnic differences in maternal risk factors and infant outcomes in Canadian high-risk births. Perinatology. 2007;9(1):1–8. [Google Scholar]
- 143.Blair E, Morich P, Stanley F. Why do aboriginal newborns weigh less? Gestational age at delivery: estimation, distribution and determinants. Aust N Z J Obstet Gynaecol. 1994;34(2):158–163. doi: 10.1111/j.1479-828x.1994.tb02680.x. [DOI] [PubMed] [Google Scholar]
- 144.Young TK, Martens PJ, Taback SP, et al. Type 2 diabetes mellitus in children: prenatal and early infancy risk factors among native canadians. Arch Pediatr Adolesc Med. 2002;156(7):651–655. doi: 10.1001/archpedi.156.7.651. [DOI] [PubMed] [Google Scholar]
- 145.Kmetic A, Reading J, Estey E, Kmetic A, Reading J, Estey E. Taking a life course perspective on cardiovascular disease and diabetes in First Nations peoples. Can J Nurs Res. 2008;40(3):58–78. [PubMed] [Google Scholar]
- 146.Pettitt DJ, Knowler WC, Bennett PH, Aleck KA, Baird HR. Obesity in offspring of diabetic Pima Indian women despite normal birth weight. Diabetes Care. 1987;10(1):76–80. doi: 10.2337/diacare.10.1.76. [DOI] [PubMed] [Google Scholar]
- 147.Pettitt DJ, Baird HR, Aleck KA, Bennett PH, Knowler WC. Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy. N Engl J Med. 1983;308(5):242–245. doi: 10.1056/NEJM198302033080502. [DOI] [PubMed] [Google Scholar]
- 148.Pettitt DJ, Nelson RG, Saad MF, Bennett PH, Knowler WC. Diabetes and obesity in the offspring of Pima Indian women with diabetes during pregnancy. Diabetes Care. 1993;16(1):310–314. doi: 10.2337/diacare.16.1.310. [DOI] [PubMed] [Google Scholar]
- 149.Cloutier JM, Dean HJ. E.A.C. S. Conference: IDF 2009 – 20th World Diabetes Congress Montreal, QC Canada. Can. J. Diabetes. 2009;33(3):196. [Google Scholar]
- 150.Gautier JF, Wilson C, Weyer C, et al. Low acute insulin secretory responses in adult offspring of people with early onset type 2 diabetes. Diabetes. 2001;50(8):1828–1833. doi: 10.2337/diabetes.50.8.1828. [DOI] [PubMed] [Google Scholar]
- 151.Bogardus C, Tataranni PA, Bogardus C, Tataranni PA. Reduced early insulin secretion in the etiology of type 2 diabetes mellitus in Pima Indians. Diabetes. 2002;51(Supplement 1):S262–264. doi: 10.2337/diabetes.51.2007.s262. [DOI] [PubMed] [Google Scholar]
- 152.Bunt JC, Tataranni PA, Salbe AD, Bunt JC, Tataranni PA, Salbe AD. Intrauterine exposure to diabetes is a determinant of hemoglobin A(1)c and systolic blood pressure in Pima Indian children. J Clin Endocrinol Metab. 2005;90(6):3225–3229. doi: 10.1210/jc.2005-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pettitt DJ, Bennett PH, Saad MF, Charles MA, Nelson RG, Knowler WC. Abnormal glucose tolerance during pregnancy in Pima Indian women. Long-term effects on offspring. Diabetes. 1991;40(Supplement 2):126–130. doi: 10.2337/diab.40.2.s126. [DOI] [PubMed] [Google Scholar]
- 154.Dabelea D, Hanson RL, Bennett PH, Roumain J, Knowler WC, Pettitt DJ. Increasing prevalence of Type II diabetes in American Indian children. Diabetologia. 1998;41(8):904–910. doi: 10.1007/s001250051006. [DOI] [PubMed] [Google Scholar]
- 155.Dabelea D, Knowler WC, Pettitt DJ. Effect of diabetes in pregnancy on offspring: follow-up research in the Pima Indians. J Matern Fetal Med. 2000;9(1):83–88. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<83::AID-MFM17>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 156.McCance DR, Pettitt DJ, Hanson RL, Jacobsson LT, Knowler WC, Bennett PH. Birth weight and non-insulin dependent diabetes: thrifty genotype, thrifty phenotype, or surviving small baby genotype? BMJ. 1994;308(6934):942–945. doi: 10.1136/bmj.308.6934.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Franks PW, Looker HC, Kobes S, et al. Gestational glucose tolerance and risk of type 2 diabetes in young Pima Indian offspring. Diabetes. 2006;55(2):460–465. doi: 10.2337/diabetes.55.02.06.db05-0823. [DOI] [PubMed] [Google Scholar]
- 158.Dyck RF, Klomp H, Tan L. From “thrifty genotype” to “hefty fetal phenotype”: the relationship between high birthweight and diabetes in Saskatchewan Registered Indians. Can J Public Health. 2001;92(5):340–344. doi: 10.1007/BF03404975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Alberti G, Zimmet P, Shaw J, Bloomgarden Z, Kaufman F, Silink M. Type 2 diabetes in the young: the evolving epidemic. The International Diabetes Federation Consensus Workshop. Diabetes Care. 2004;27(7):1798–1811. doi: 10.2337/diacare.27.7.1798. [DOI] [PubMed] [Google Scholar]
- 160.Benyshek DC, Martin JF, Johnston CS. A reconsideration of the origins of the type 2 diabetes epidemic among Native Americans and the implications for intervention policy. Med Anthropol. 2001;20(1):25–64. doi: 10.1080/01459740.2001.9966186. [DOI] [PubMed] [Google Scholar]
- 161.Dyck RF. Tracking ancient pathways to a modern epidemic: diabetic end-stage renal disease in Saskatchewan aboriginal people. Kidney Int Suppl. 2005;97:S53–57. doi: 10.1111/j.1523-1755.2005.09709.x. [DOI] [PubMed] [Google Scholar]
- 162.Jaiyeola AO, Stabler W. Health Disparities Among Native American People of the United States. Jones and Bartlett PublishersBoston, MA; US: Jones and Bartlett PublishersBoston; 2009. [Google Scholar]
- 163.Franks PW, Hanson RL, Knowler WC, et al. Childhood predictors of young-onset type 2 diabetes. Diabetes. 2007;56(12):2964–2972. doi: 10.2337/db06-1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Pratley RE. Gene-environment interactions in the pathogenesis of type 2 diabetes mellitus: lessons learned from the Pima Indians. Proc Nutr Soc. 1998;57(2):175–181. doi: 10.1079/pns19980029. [DOI] [PubMed] [Google Scholar]
- 165.Whincup PH, Kaye SJ, Owen CG, et al. Birth weight and risk of type 2 diabetes a systematic review. JAMA. 2008;300(24):2886–2897. doi: 10.1001/jama.2008.886. [DOI] [PubMed] [Google Scholar]
- 166.Osgood ND, Dyck RF, Grassmann WK. The inter- and intragenerational impact of gestational diabetes on the epidemic of type 2 diabetes. Am J Public Health. 2011;101(1):173–179. doi: 10.2105/AJPH.2009.186890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Falhammar H, Davis B, Sinha A. Maternal and neonatal outcomes in the Torres Strait with a sixfold increase in type 2 diabetes in pregnancy over six years. Aust N Z J Obstet Gynaecol. 2010;50(2):120–126. doi: 10.1111/j.1479-828X.2009.01133.x. [DOI] [PubMed] [Google Scholar]
- 168.Cleary E, Ludwig S, Riese N, Grant L. Educational strategies to improve screening for gestational diabetes mellitus in aboriginal women in a remote northern community. Can. J. Diabetes. 2006;30(3):264–268. [Google Scholar]
- 169.Joshy G, Simmons D, Joshy G, Simmons D. Epidemiology of diabetes in New Zealand: revisit to a changing landscape. N Z Med J. 2006;119(1235):U1999. [PubMed] [Google Scholar]
- 170.Rumbold AR, Bailie RS, Si D, et al. Delivery of maternal health care in Indigenous primary care services: baseline data for an ongoing quality improvement initiative. BMC Pregnancy Childbirth. 2011;11:16. doi: 10.1186/1471-2393-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Anonymous. Planning research for greater community involvement and long-term benefit. Special working group of the Cree Regional Child and Family Services Committee. Can Med Assoc J. 2000;163(10):1273–1274. [PMC free article] [PubMed] [Google Scholar]
- 172.Smith-Morris CM. Diagnostic controversy: gestational diabetes and the meaning of risk for Pima Indian women. Med. Anthropol. 2005;24(2):145–177. doi: 10.1080/01459740590933902. [DOI] [PubMed] [Google Scholar]
- 173.Shen G. Insights into weight gain during pregnancy among first nations women living on remote reserves. Can. J. Diabetes. 2008;32(3):172–173. [Google Scholar]
- 174.Doran F, O'Brien AP, Doran F, O'Brien AP. A brief report of attitudes towards physical activity during pregnancy. Health Promot J Austr. 2007;18(2):155–158. doi: 10.1071/he07155. [DOI] [PubMed] [Google Scholar]
- 175.Neufeld H, Marchessault G. Perceptions of 2 generations of aboriginal women on causes of diabetes during pregnancy. Can. J. Diabetes. 2006;30(2):161–168. [Google Scholar]
- 176.Gaudreau S, Michaud C. Cultural factors related to the maintenance of health behaviours in Algonquin women with a history of gestational diabetes. Chronic Dis Inj Can. 2012;32(3):140–148. [PubMed] [Google Scholar]
- 177.Lavallee LF. An indigenous approach to diabetes research: don't just tell us we're fat. Can. J. Diabetes. 2011;35(4):324–325. [Google Scholar]
- 178.Vallianatos H, Brennand EA, Raine K, et al. Beliefs and practices of first nation women about weight gain during pregnancy and lactation: implications for women's health. Can J Nurs Res. 2006;38(1):102–119. [PubMed] [Google Scholar]
- 179.Pettitt DJ, Bennett PH, Hanson RL, Narayan KM, Knowler WC. Comparison of World Health Organization and National Diabetes Data Group procedures to detect abnormalities of glucose tolerance during pregnancy. Diabetes Care. 1994;17(11):1264–1268. doi: 10.2337/diacare.17.11.1264. [DOI] [PubMed] [Google Scholar]
- 180.Massion C, O'Connor PJ, Gorab R, Crabtree BF, Nakamura RM, Coulehan JL. Screening for gestational diabetes in a high-risk population. J Fam Pract. 1987;25(6):569–575. [PubMed] [Google Scholar]
- 181.Dagogo-Jack S. Pitfalls in the use of HbA 1c as a diagnostic test: the ethnic conundrum. Nat Rev Endocrinol. 2010;6(10):589–593. doi: 10.1038/nrendo.2010.126. [DOI] [PubMed] [Google Scholar]
- 182.Sievers ML. Diabetes mellitus in American Indians – standards for diagnosis and management. Diabetes. 1976;25(6):528–531. doi: 10.2337/diab.25.6.528. [DOI] [PubMed] [Google Scholar]
- 183.Hunt JM. Pregnancy Care. South Melbourne: Oxford University Press; 2007. Aboriginal primary health care: an evidence based approach. [Google Scholar]
- 184.Alukura C, Inc NHC. Minymaku Kutju Tjukurpa – Women's Business Manual: Standard Treatment Manual for Women's Business in Central Australia. Alice Springs: Congress Alukura and Nganampa Health Council Inc; 1999. [Google Scholar]
- 185.Simmons D, Thompson CF, Conroy C, Scott DJ. Use of insulin pumps in pregnancies complicated by type 2 diabetes and gestational diabetes in a multiethnic community. Diabetes Care. 2011;24(12):2078–2082. doi: 10.2337/diacare.24.12.2078. [DOI] [PubMed] [Google Scholar]
- 186.Simmons D. Impact of an integrated approach to diabetes care at the Rumbalara Aboriginal Health Service. Intern Med J. 2003;33(12):581–585. doi: 10.1111/j.1445-5994.2003.00491.x. [DOI] [PubMed] [Google Scholar]
- 187.Rodrigues S, Robinson EJ, Kramer MS, Gray-Donald K. High rates of infant macrosomia: a comparison of a Canadian native and a non-native population. J Nutr. 2000;130(4):806–812. doi: 10.1093/jn/130.4.806. [DOI] [PubMed] [Google Scholar]
- 188.McGrath NM, Evans C, Holgate A. Post-partum follow-up of women with gestational diabetes mellitus from Northland, New Zealand. Diabet Med. 2007;24(2):218–219. doi: 10.1111/j.1464-5491.2007.02052.x. [DOI] [PubMed] [Google Scholar]
- 189.Dannenbaum D, Verronneau M, Torrie J, et al. Comprehensive computerized diabetes registry. Serving the Cree of Eeyou Istchee (eastern James Bay) Can. Family Phys. 1999;45:364–370. [PMC free article] [PubMed] [Google Scholar]
- 190.Richards J, Mousseau A. Community-based participatory research to improve preconception health among Northern Plains American Indian adolescent women. Amer. Indian Alaska Native Mental Health Res. (Online) 2012;19(1):154–185. doi: 10.5820/aian.1901.2012.154. [DOI] [PubMed] [Google Scholar]
- 191.Dyck RF, Sheppard MS, Cassidy H, Chad K, Tan L, Van Vliet SH. Preventing NIDDM among aboriginal people: is exercise the answer? Description of a pilot project using exercise to prevent gestational diabetes. Int J Circumpolar Health. 1998;57(Suppl 1):375–378. [PubMed] [Google Scholar]
- 192.Gray-Donald K, Robinson E, Collier A, David K, Renaud L, Rodrigues S. Intervening to reduce weight gain in pregnancy and gestational diabetes mellitus in Cree communities: an evaluation. CMAJ Can. Med. Assoc. J. 2000;163(10):1247–1251. [PMC free article] [PubMed] [Google Scholar]
- 193.Klomp H, Dyck R, Sheppard S. Description and evaluation of a prenatal exercise program for urban aboriginal women. Can. J. Diabetes. 2003;27(3):231–238. [Google Scholar]
- 194.Pettitt DJ, Forman MR, Hanson RL, Knowler WC, Bennett PH. Breastfeeding and incidence of non-insulin-dependent diabetes mellitus in Pima Indians. Lancet. 1997;350(9072):166–168. doi: 10.1016/S0140-6736(96)12103-6. [DOI] [PubMed] [Google Scholar]
- 195.Murphy S, Wilson C. Breastfeeding promotion: a rational and achievable target for a type 2 diabetes prevention intervention in Native American communities. J Hum Lact. 2008;24(2):193–198. doi: 10.1177/0890334408317434. [DOI] [PubMed] [Google Scholar]
- 196.O'Dea K, Rowley K, Brown A. Diabetes in Indigenous Australians: possible ways forward. Med J Aust. 2007;186(10):494–495. doi: 10.5694/j.1326-5377.2007.tb01020.x. [DOI] [PubMed] [Google Scholar]
- 197.Campbell A, Campbell A. Type 2 diabetes and children in Aboriginal communities: the array of factors that shape health and access to health care. Health Law J. 2002;10:147–168. [PubMed] [Google Scholar]
- 198.Stephenson J. Diabetes in the Aboriginal community. Aboriginal Islander Health Worker J. 1993;17(5):25–26. [Google Scholar]
- 199.Middleton P. Preventing infant deaths among Aboriginal and teenage women in South Australia. 2009. http://aboriginalhealth.flinders.edu.au/Newsletters/2010/Downloads/SHRP%20FINAL%20REPORT%20PART%20TWO%20July%202009.pdf Accessed 14/12/2012.
- 200.Lega IC, McLaughlin H, Coroneos M, Handley-Derry F, Donovan N, Lipscombe LL. A physician reminder to improve postpartum diabetes screening in women with gestational diabetes mellitus. Diabetes Res Clin Pract. 2012;95(3):352–357. doi: 10.1016/j.diabres.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 201.Eades SJ, Taylor B, Bailey S, Williamson AB, Craig JC, Redman S, for the SEARCH Investigators The health of urban Aboriginal people: insufficient data to close the gap. Med J Aust. 2010;193(9):521–524. doi: 10.5694/j.1326-5377.2010.tb04036.x. [DOI] [PubMed] [Google Scholar]
- 202.Rigney L. A first perspective of Indigenous Australian participation in science: framing Indigenous research towards Indigenous Australian intellectual sovereignty. Kaurna Higher Educ. J. 2001;7:1–13. [Google Scholar]
- 203.Fee M. Racializing narratives: obesity, diabetes and the “Aboriginal” thrifty genotype. Soc Sci Med. 2006;62(12):2988–2997. doi: 10.1016/j.socscimed.2005.11.062. [DOI] [PubMed] [Google Scholar]
- 204.Lavallee LF. An indigenous approach to diabetes research: don't just tell us we're fat. Can. J. Diabetes. 2011;35(4):324–325. [Google Scholar]
- 205.Moses R, Colagiuri S. The extent of undiagnosed gestational diabetes mellitus in New South Wales. Med J Aust. 1997;167:14–16. doi: 10.5694/j.1326-5377.1997.tb138756.x. [DOI] [PubMed] [Google Scholar]
- 206.Russell MA, Phipps MG, Olson CL, Welch HG, Carpenter MW. Rates of postpartum glucose testing after gestational diabetes mellitus. Obstet Gynecol. 2006;108(6):1456–1462. doi: 10.1097/01.AOG.0000245446.85868.73. doi:1410.1097/1401.AOG.0000245446.0000285868.0000245473. [DOI] [PubMed] [Google Scholar]
- 207.Tieu J, Middleton P, McPhee AJ, Crowther CA. Screening and subsequent management for gestational diabetes for improving maternal and infant health. Cochrane Database Syst Rev. 2010;(7) doi: 10.1002/14651858.CD007222.pub2. Art. No.: CD007222. DOI: 10.1002/14651858.CD007222.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Tieu J, Crowther C, Middleton P. Dietary advice in pregnancy for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2010;(7) doi: 10.1002/14651858.CD006674.pub2. Art. No.: CD007222. DOI: 10.1002/14651858.CD006674.pub2. [DOI] [PubMed] [Google Scholar]
- 209.Ceysens G, Rouiller D, Boulvain M. Exercise for diabetic pregnant women. Cochrane Database Syst Rev. 2006;(3) doi: 10.1002/14651858.CD004225.pub2. Art. No.: CD004225. 10.1002/14651858.CD004225.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Bennett WL, Robinson KA, Saldanha IJ, Wilson LM, Nicholson WK. High priority research needs for gestational diabetes mellitus. J Womens Health. 2012;21(9):925–932. doi: 10.1089/jwh.2011.3270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Round JA, Jacklin PB, Fraser RB, Hughes RG, Mugglestone MA, Holt RIG. Screening for gestational diabetes mellitus: cost-utility of different screening strategies based on a woman's individual risk of disease. Diabetologica. 2010;54(2):256–263. doi: 10.1007/s00125-010-1881-y. [DOI] [PubMed] [Google Scholar]
- 212.Moses R, Morris G, Petocz P, San Gil F, Garg D. The impact of potential new diagnostic criteria on the prevalence of gestational diabetes mellitus in Australia. Med J Aust. 2011;194(7):338–340. doi: 10.5694/j.1326-5377.2011.tb03001.x. [DOI] [PubMed] [Google Scholar]
- 213.Morikawa M, Yamada T, Yamada T, Akaishi R, Nishida R, Cho K. Changes in the number of patients after the adoption of IADSPG criteria for hyperglycaemia during pregnancy in Japanese women. Diabetes Res Clin Pract. 2010;90:339–342. doi: 10.1016/j.diabres.2010.08.023. [DOI] [PubMed] [Google Scholar]
- 214.Leiberman N, Kalter-Leibovici O, Hod M. Global adoption of IADSPG recommendations: a national approach. Int. J. Obstetrics Gynaecology. 2011;115(Suppl 1):S45–47. doi: 10.1016/S0020-7292(11)60013-1. [DOI] [PubMed] [Google Scholar]
- 215.Flack J, Ross G, Ho S, McElduff A. Recommended changes to diagnostic criteria for gestational diabetes: impact on workload. Aust N Z J Obstet Gynaecol. 2010;50:439–443. doi: 10.1111/j.1479-828X.2010.01218.x. [DOI] [PubMed] [Google Scholar]
- 216.O'Sullivan E, Avalos G, O'Reilly M, Dennedy M, Gaffney G, Dunne F on behalf of the Atlantic DIP collaborators. Atlantic Diabetes in Pregnancy (DIP): the prevalence and outcomes of gestational diabetes mellitus using new diagnostic criteria. Diabetologica. 2011;54:1670–1675. doi: 10.1007/s00125-011-2150-4. [DOI] [PubMed] [Google Scholar]
- 217.McNamara BJ, Gubhaju L, Chamberlain C, Stanley F, Eades SJ. Early life influences on cardio-metabolic disease risk in aboriginal populations – what is the evidence? A systematic review of longitudinal and case-control studies. Int J Epidemiol. 2012;41(6):1661–1682. doi: 10.1093/ije/dys190. [DOI] [PubMed] [Google Scholar]
- 218.O'Reilly MW, Avalos G, Dennedy MC, O'Sullivan EP, Dunne F. Atlantic DIP: high prevalence of abnormal glucose tolerance post partum is reduced by breast-feeding in women with prior gestational diabetes mellitus. Eur J Endocrinol. 2011;165(6):953–959. doi: 10.1530/EJE-11-0663. [DOI] [PubMed] [Google Scholar]
- 219.Karanja N, Lutz T, Ritenbaugh C, et al. The TOTS community intervention to prevent overweight in American Indian toddlers beginning at birth: a feasibility and efficacy study. J Community Health. 2010;35(6):667–675. doi: 10.1007/s10900-010-9270-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Denny CH, Floyd RL, Green PP, Hayes DK. Racial and ethnic disparities in preconception risk factors and preconception care. J Womens Health. 2012;21(7):720–729. doi: 10.1089/jwh.2011.3259. [DOI] [PubMed] [Google Scholar]
- 221.Naylor JL, Schraer CD, Mayer AM, Lanier AP, Treat CA, Murphy NJ. Diabetes among Alaska Natives: a review. Int J Circumpolar Health. 2003;62(4):363–387. doi: 10.3402/ijch.v62i4.17581. [DOI] [PubMed] [Google Scholar]
- 222.Hadden DR. Geographic, ethnic, and racial variations in the incidence of gestational diabetes mellitus. Diabetes. 1985;34(suppl 2):8–12. doi: 10.2337/diab.34.2.s8. [DOI] [PubMed] [Google Scholar]
- 223.Mackerras D. Evaluation of the strong women, strong babies, strong culture program: results for the period 1990-1996 in the three pilot communities. Darwin: Menzies School of Health Research; 1998. [Google Scholar]
- 224.Johnson S, Martin D, Sarin C. Diabetes mellitus in the First Nations population of British Columbia, Canada. Part 3. Prevalence of diagnosed cases. Int J Circumpolar Health. 2002;61(3):260–264. doi: 10.3402/ijch.v61i3.17460. [DOI] [PubMed] [Google Scholar]
- 225.Hunt KJ, Schuller KL. The increasing prevalence of diabetes in pregnancy. Obstet Gynecol Clin North Am. 2007;34(2):173–199. doi: 10.1016/j.ogc.2007.03.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Gohdes D, Ose CS, Harwell TS, Moore KR, McDowall JM, Helgerson SD. Diabetes in Montana's Indians: the epidemiology of diabetes in the Indians of the Northern Plains and Canada. Curr Diab Rep. 2004;4(3):224–229. doi: 10.1007/s11892-004-0028-2. [DOI] [PubMed] [Google Scholar]
- 227.Williams MA, Emanuel I, Kimpo C, Leisenring WM, Hale CB. A population-based cohort study of the relation between maternal birthweight and risk of gestational diabetes mellitus in four racial/ethnic groups. Paediatr Perinat Epidemiol. 1999;13(4):452–465. doi: 10.1046/j.1365-3016.1999.00219.x. [DOI] [PubMed] [Google Scholar]
- 228.Muller YL, Hanson RL, Bian L, Mack J, Shi X, Pakyz R, Shuldiner AR, Knowler WC, Bogardus C, Baier LJ. Functional variants in MBL2 are associated with type 2 diabetes and pre-diabetes traits in Pima Indians and the old order Amish. Diabetes. 2010;59(8):2080–2085. doi: 10.2337/db09-1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Pettitt DJ, Narayan KM, Hanson RL, Knowler WC. Incidence of diabetes mellitus in women following impaired glucose tolerance in pregnancy is lower than following impaired glucose tolerance in the non-pregnant state. Diabetologia. 1996;39(11):1334–1337. doi: 10.1007/s001250050579. [DOI] [PubMed] [Google Scholar]
- 230.Cundy T, Gamble G, Manuel A, Townend K. Determinants of birth-weight in women with established and gestational diabetes. Aust N Z J Obstet Gynaecol. 1993;33(3):249–254. doi: 10.1111/j.1479-828x.1993.tb02078.x. [DOI] [PubMed] [Google Scholar]
- 231.Schaefer O. Pre- and post-natal growth acceleration and increased sugar consumption in Canadian Eskimos. Can Med Assoc J. 1970;103(10):1059–1068. [PMC free article] [PubMed] [Google Scholar]
- 232.Coory M. Is birthweight an appropriate health-outcome measure for Torres Strait Islander babies. Aust N Z J Public Health. 2000;24(1):60–63. doi: 10.1111/j.1467-842x.2000.tb00724.x. [DOI] [PubMed] [Google Scholar]
- 233.Dooley JP, Sugamori ME. Pregnancy outcome in aboriginal women with NIDDM in the Sioux Lookout Zone. Int J Circumpolar Health. 1998;57(suppl 1):359–363. [PubMed] [Google Scholar]
- 234.Sayers SM. Indigenous Newborn Care. Pediatr Clin North Am. 2009;56(6):1243–1261. doi: 10.1016/j.pcl.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 235.Charles MA, Pettitt DJ, Hanson RL, Bennett PH, Saad MF, Liu QZ, Knowler WC. Familial and metabolic factors related to blood pressure in Pima Indian childrenes. Am J Epidemiol. 1994;140(2):123–131. doi: 10.1093/oxfordjournals.aje.a117223. [DOI] [PubMed] [Google Scholar]
- 236.Nelson RG, Morgenstern H, Bennett PH. Birth weight and renal disease in Pima Indians with type 2 diabetes mellitus. Am J Epidemiol. 1998;148(7):650–656. doi: 10.1093/aje/148.7.650. [DOI] [PubMed] [Google Scholar]
- 237.Nelson RG, Morgenstern H, Bennett PH. Intrauterine diabetes exposure and the risk of renal disease in diabetic Pima Indians. Diabetes. 1998;47(9):1489–1493. doi: 10.2337/diabetes.47.9.1489. [DOI] [PubMed] [Google Scholar]
- 238.Rumbold AR, Bailie RS, Si D, Dowden MC, Kennedy CM, Cox RJ, et al. Delivery of maternal health care in Indigenous primary care services: baseline data for an ongoing quality improvement initiative. BMC Pregnancy and Childbirth. 2011;11(16) doi: 10.1186/1471-2393-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


