Abstract
Objectives. We examined the associations among school-based obesity policies, social capital, and adolescents’ self-reported weight control behaviors, focusing on how the collective roles of community and adopted policies affect gender groups differently.
Methods. We estimated state-level ecologic models using 1-way random effects seemingly unrelated regressions derived from panel data for 43 states from 1991 to 2009, which we obtained from the Centers for Disease Control and Prevention’s Youth Risk Behavior Surveillance System. We used multiplicative interaction terms to assess how social capital moderates the effects of school-based obesity policies.
Results. School-based obesity policies in active communities were mixed in improving weight control behaviors. They increased both healthy and unhealthy weight control behaviors among boys but did not increase healthy weight control behaviors among girls.
Conclusions. Social capital is an important contextual factor that conditions policy effectiveness in large contexts. Heterogeneous behavioral responses are associated with both school-based obesity policies and social capital. Building social capital and developing policy programs to balance outcomes for both gender groups may be challenging in managing childhood obesity.
Childhood obesity, long thought to be a private concern, is now on the national policy agenda. Obesity prevalence among children aged 6 to 11 years more than doubled in the past 20 years, and the rate among adolescents aged 12 to 19 years more than tripled.1 Causes of childhood obesity are complex and include several individual and environmental factors2–5; however, most studies have focused on behavioral influences, such as dietary changes and physical activity.6 Specifically, excessive consumption of sugar- and fat-enriched food, lack of exercise, and excessive television viewing are positively related to weight gain.7,8
Researchers focusing on the behavioral drivers of obesity have recognized that schools are an ideal site for behavioral interventions9,10 and have advocated school-based policies for addressing childhood obesity.11,12 For example, physical education policies helped prevent obesity in 3 randomized controlled trials.13 School policies restraining junk food reduced children’s body mass index (BMI; defined as weight in kilograms divided by the square of height in meters) scores.12 However, most studies have focused on programs that recruited a small number of schools, rather than studying widely implemented school-based obesity policies.14 Thus, randomized controlled trials have not clarified whether school-based obesity policies translate to consistent and positive effects when implemented at larger—namely national and state—levels.
Potential challenges exist for increasing the effectiveness of large-scale school-based obesity policies. First, successful interventions in randomized controlled trials may not always translate into large-scale policy effectiveness. In school-based randomized controlled trials, policy implementation conditions are well controlled. However, effectively implementing a large-scale policy requires collaboration between schools and supportive external communities. Researchers often discuss this community role as social capital—the civic engagement, trust, and social networks in a community.15 It is unclear whether these social capital measures affect school-based policies that address childhood obesity.
Social capital provides mixed results as an environmental factor for health, especially in obesity-related interventions. Some studies that examined social networks found that social capital reduces the risk of obesity16 and physical inactivity.17,18 Conversely, social contacts and community connections may increase tolerance to unhealthy lifestyles.19 Specifically, social networks can teach obesity-related behaviors through friend pairs and same-gender siblings.20 These mixed findings suggest social capital may inconsistently prevent childhood obesity, indicating a need to probe the community conditions in which school-based obesity policies may be effective.
The second large-scale obesity management challenge is determining how heterogeneous populations respond to both policy and social environments. Although researchers have recognized the importance of connecting social capital to childhood obesity,21,22 few studies link community to school-based policies and examine how both factors interactively produce different outcomes across groups.23
Gender is an important factor in assessing heterogeneous policy responses, especially for obesity-related behaviors. Specifically,
boys and girls differ in body composition, patterns of weight gain, hormone biology, and the susceptibility to certain social, ethnic, genetic, and environmental factors.24(p76)
A few studies have reported that physical education improved self-image and physical activity for girls25 and reduced BMI more for overweight girls than for overweight boys, implying boys have greater resistance to social environment and policy interventions than do girls.26 Children’s peer socialization mediated gender differences in unhealthy weight control behaviors and school-based obesity policies. Because girls have greater social punishment than do boys for being overweight, they are more likely to respond to policy interventions by fasting to lose weight.27,28
Taken together, social capital and policy interventions may link to different, even unhealthy, behavioral responses by gender. A challenge for school-based obesity policies is balancing different weight control needs for boys and girls, while raising awareness of unhealthy weight control behaviors. Therefore, unhealthy weight control activities were our empirical focus. Population-based studies have found that adolescents who engage in unhealthy weight control behaviors are at higher risk for being obese, of engaging in other health-compromising activities (e.g., eating disorders), and of being depressed.29
The combined association between social capital and statewide implementation of obesity policy on gendered weight control behaviors is less well known, even though many states have legislatively mandated various school-based obesity policies. Because of the national increase in school-based obesity policies, we conducted a state-level comparison, focusing on how school-based obesity policies combined with social capital affect weight control behaviors by gender. We chose a state-level analysis for 3 reasons. First, states are the primary policy adopters and key stakeholders to incorporate federal guidelines in school-based obesity policies.30 Second, school-based obesity policies vary considerably by state because of different legislative interests, making it necessary to incorporate different school-based policies that state governments mandate. Third, longitudinal empirical data that track both policy change and weight control behaviors by gender groups are more comprehensive and much better documented at the state level than at the local level.
METHODS
We pooled state-level data for 43 states from 1991 to 2009 to examine how social capital and childhood obesity policies interactively affect youth weight control behaviors. We did not include California, Washington, DC, Oregon, Pennsylvania, Virginia, and Washington State in the sample because no data were available for adolescents’ weight control behaviors for these states in the health behavior survey we used. We did not include Hawaii and Alaska because they lacked available data for social capital measures.
Weight Control Behaviors
Because school-based obesity policies aim to promote sound weight control practices (e.g., exercise and food intake reduction), we measured weight control behaviors by gender as the policy outcome variables. We drew data from the Centers for Disease Control and Prevention’s Youth Risk Behavior Surveillance System (YRBSS).31 Students were surveyed for 5 weight control behaviors during the prior 30 days: (1) not exercising to control weight; (2) not eating less food, fewer calories, or low-fat foods to lose weight or to keep from gaining weight; (3) fasting more than 24 hours to lose weight; (4) taking diet pills, powders, or liquids without a doctor’s advice to lose weight; and (5) vomiting or taking laxative pills to lose weight. At the state-level, each behavior was measured by using the percentage of students who engaged in a particular weight control behavior.
On the basis of a principal component factor analysis, we scaled the 5 behaviors by 2 factor indexes for each gender group. The first 3 behavior items loaded positively on 1 factor with eigenvalues of 1.74 (female index) and 1.91 (male index). We labeled this factor index “calorie-targeted weight control behavior” because all 3 weight control behaviors target caloric intake to control weight. Items 4 and 5 loaded positively on the second factor, with eigenvalues of 2.15 (female index) and 2.07 (male index). We labeled this factor index “medication-based weight control behavior” because both items capture pill intake weight control behaviors. For both indexes, higher values indicate unhealthier weight control activities.
School-Based Obesity Policy
We considered school-based obesity policies to be state government policies that mandate school district–level implementation with an explicit goal of addressing childhood obesity. To measure the overall policy inputs at the state level, we incorporated information on legislative initiatives and school district–level implementation status. First, we used data on state-level legislative initiatives from the Centers for Disease Control and Prevention database State Legislative and Regulatory Action to Prevent Obesity and Improve Nutrition and Physical Activity.32 We used the number of newly enacted bills that seek to mandate schools to improve children’s nutrition, enhance physical education, promote physical activities, mandate or recommend BMI screening at schools, and share children’s BMI information with parents. State policies vary substantially. From 2001 to 2011, 483 new legislative bills were passed to promote healthy nutrition in schools. A total of 137 new bills were enacted to address childhood obesity through BMI screening and reporting students’ BMI information, and 681 new bills were passed to promote physical activity.
Second, we used data from the Centers for Disease Control and Prevention’s database on School Health Policies and Programs Study (for 1994, 2000, and 2006), a national survey conducted every 6 years. We evaluated whether school districts in each state implemented state mandates on the corresponding categories: (1) restricting junk food in schools, (2) incorporating topics on healthy nutrition and dietary behavior in nutrition education, (3) enhancing physical education, and (4) administrating fitness tests.33
We created a state-level measure of the overall school-based policies by computing a policy index from available information for state legislative actions (annual data from 2001–2009) and then computed another policy index from School Health Policies and Programs Study surveys (1994, 2000, and 2006). We used the Pearson correlation between the index of legislative actions and the School Health Policies and Programs Study survey in 2006 (r = 0.991; P ≤ .001) to impute combined policy index scores across all years. The estimated annual policy index ranges from −1.554 to 1.118. Higher values mean that a state mandated more school-based policies to reduce and prevent childhood obesity. This estimated policy index indicates a positive trend in adopting more childhood obesity policies from 1990 to 2009. School-based policies increased dramatically after 2000.
Social Capital
We developed the social capital measure on the basis of Robert Putnam’s concept of social capital as 5 components: participation in public activities, participation in community organizations, community volunteerism, informal sociability, and social trust.15 A limitation of this empirical index, as Putnam15 notes, is that it does not capture changes in social capital over time. Focusing on the dimensions of collective community, we replicated Hawes and Rocha’s dynamic social capital index (from 1986 to 2000) and expanded the index to 2009.34
Our social capital index used data from the Survey of the American Consumer, which GfK Mediamark Research & Intelligence conducted. GfK Mediamark Research & Intelligence conducts annual consumer surveys on the basis of approximately 26 000 in-home, face-to-face consumer interviews. The survey implemented a randomly stratified sampling procedure to select households, and the face-to-face interview method generated response rates of approximately 60% to 70%. Household heads were the primary respondents of the survey. The original GfK Mediamark Research & Intelligence data aggregated individual-level measures on public activities, leisure activities, media usage, and political outlook by state clusters.
We measured community organizational life by group membership of fraternal orders, civic clubs, veteran clubs, local governments, and country clubs. We measured engagement in public affairs by 7 items: writing to an editor of a magazine or newspaper, writing to a radio or television station, writing to an elected official, writing something that has been published, working for a political party or candidate, engaging in fund raising, and voting for national and congressional elections. We measured community volunteerism by average contribution to public television or radio stations. We scaled all these collective community indicators into a single index on the basis of factor analysis. All items loaded positively in the first factor with an eigenvalue of 3.948. We extracted the first principal factor as the social capital index.
Data Analysis
We controlled for several factors associated with policy effectiveness and health outcomes: characteristics of state health care systems (state health care spending, public health employment, and children’s access to health insurance); state socioeconomic status (state poverty, unemployment, and average educational attainment); and 2 risk factors that affect weight control behaviors (the percentage of overweight infants and the percentage of YRBSS respondents who describe themselves as overweight).
To assess the combined effects of school-based obesity policy and social capital on behaviors by gender, we implemented a system of equations for female and male indexes of weight control behavior using the 1-way random effect estimation of seemingly unrelated regressions in a panel data framework. We estimated all the statistical models using Stata 12.0 (StataCorp LP, College Station, TX). Seemingly unrelated regression estimation produced 2 sets of slope coefficients to compare the heterogeneity in policy effects across the 2 gender groups. When unmeasured factors affecting the health outcomes for 1 gender group may also affect the other, seemingly unrelated regression estimation produces unbiased and more efficient estimation than does estimating the 2 equations separately.35,36
We conducted postregression diagnostic analysis and comparison of data variation along spatial and temporal dimensions to ensure the robustness of our estimation results. First, we included lagged dependent variables because we detected the panel unit root for all the dependent variables using the augmented Dickey–Fuller test and the Phillips–Perron test. The lagged dependent variables also allowed us to assess the inertia of the behavioral trends.37 Second, the empirical data contain much greater between-unit R2 (cross-sectional variance) than within-unit R2 (cross-time variance). Hence, random effects estimation is favored over state fixed effects. We also detected autocorrelation along time and cross-sectional dimensions, nonconstant variance caused by heterogeneity across states, and nonconstant variance caused by extreme value observations. In the panel seemingly unrelated regression analysis, we used a stepwise method to improve estimation efficiency. We obtained the overall generalized least squares estimator first and then corrected for unstable parameter estimates caused by autocorrelation and heteroskedasticity.38,39 Lastly, we controlled for a set of states with high obesity rates (Alabama, Arizona, Georgia, Louisiana, Mississippi, Tennessee, and Texas).
Because we substantively focused on the interactive link of social capital and obesity policy with heterogeneous group responses across states, we used the state-level cross-sectional time series design to track policy changes across time and compare social environments across states. Although we did not directly model individual students’ responses in our analysis, we aggregated the individual-level responses to create group-level variables for the gender-based weight control behavior indexes. The data we used to compute the 2 weight control behavior indexes contained unreliable mean scores between 1991 and 1995 because of relatively low survey participation in early YRBSS waves. This issue cautioned us against potential estimation bias. Robustness analyses by jackknifing our full sample and by dropping years before 1995 one by one did not create substantively different results. Therefore, we reported the estimated results derived from the full sample.
RESULTS
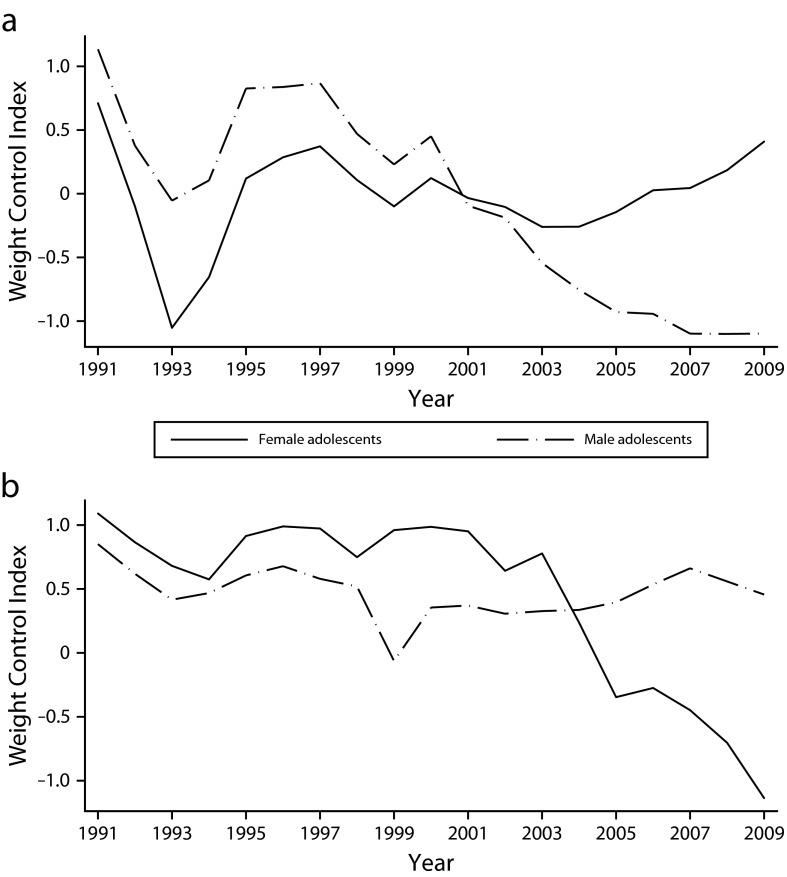
Figure 1 presents descriptive results of the 2 weight control behavior indexes for each gender. Each behavioral index takes a mean value of approximately 0 and a SD of approximately 1. Positive values show unhealthier behavioral trends and vice versa. In the overall index of calorie-targeted weight control behavior, the state–year case with the maximum estimated index score is New Jersey in 1991. The estimated trend of adolescents’ weight control behavior (in New Jersey in 1991) indicates 54.6% of students did not exercise to lose weight and 71.8% of students did not eat less to lose weight. Figure 1 also demonstrates gender differences in weight control behaviors. Before 2001, more male students than female students reported being physically inactive, and the group trends reversed after 2001. Before 2004, more female students reported taking diet or laxative pills to lose weight than did their male counterparts, and the group trends reversed after 2004.
FIGURE 1—
Self-reported behavioral trends of estimated youth weight control indexes for (a) calorie-targeted behavior and (b) medication-based behavior: Youth Risk Behavior Surveillance System, 1991–2009.
Table 1 presents the interactive relationship between social capital and school-based policies. We found a mixed pattern in obesity policies’ effects on adolescents’ weight control behavior. In general, levels of social capital condition policy effects and are associated with behavioral changes by gender.
TABLE 1—
Gender Comparison of the Effects of Obesity Policy and Social Capital on Adolescents’ Self-Reported Weight Control Behavior: Youth Risk Behavior Surveillance System, 1991–2009
| Variable | Model 1, b (SE) | Model 2, b (SE) |
| Female equation | ||
| Obesity policyt-1 | 0.123** (0.025) | −0.035 (0.033) |
| Social capital | −0.038** (0.014) | −0.149** (0.020) |
| Policyt-1 × social capital | −0.032 (0.021) | 0.008 (0.031) |
| Public health spendingt-1 | −0.059 (0.043) | 0.073 (0.063) |
| Public health employeet-1 | −0.003** (0.001) | −0.001 (0.001) |
| % uninsured children | 0.010** (0.003) | 0.014 (0.005) |
| Education | −0.038** (0.003) | −0.039** (0.003) |
| Poverty | 0.007 (0.005) | 0.003* (0.008) |
| Change in unemployment | −0.004 (0.011) | −0.032* (0.015) |
| % overweight infant | 0.004** (0.001) | 0.006** (0.001) |
| Risk perception | −0.120** (0.004) | 0.059** (0.007) |
| Lagged dependent variable | 0.393** (0.016) | 0.592** (0.019) |
| Male equation | ||
| Obesity policyt-1 | −0.111** (0.023) | 0.158** (0.038) |
| Social capital | −0.061** (0.013) | −0.073** (0.024) |
| Policyt-1 × social capital | −0.074** (0.020) | 0.019 (0.036) |
| Public health spendingt-1 | −0.049 (0.031) | 0.181** (0.064) |
| Public health employeet-1 | −0.001 (0.001) | −0.001 (0.001) |
| % uninsured children | 0.012** (0.003) | −0.005 (0.005) |
| Education | −0.039** (0.002) | −0.009** (0.002) |
| Poverty | −0.008 (0.005) | 0.025** (0.008) |
| Change in unemployment | −0.032** (0.010) | 0.020 (0.018) |
| % overweight infant | 0.021** (0.001) | 0.002* (0.001) |
| Risk perception | −0.199** (0.006) | −0.00004 (0.009) |
| Lagged dependent variable | 0.348** (0.016) | 0.684** (0.020) |
Note. In model 1, the dependent variable is the index of calorie-targeted weight control behavior. In model 2, the dependent variable is the index of medication-based weight control behavior. Lagged dependent variable refers to a 1-year lag of the dependent variable in each model. State dummy variables (AL, AR, GA, LA, MS, TN, and TX) are not reported. The sample size was n = 807.
*P < .05; **P < .01.
We estimated model 1 using the index of calorie-targeted weight control behavior as the dependent variable, which indicated differential policy effects by gender. When the social capital variable equals 0 (i.e., a low level of social capital), obesity policy has a positive and significant effect on the female index of physical inactiveness (b = 0.123; 95% confidence interval [CI] = 0.074, 0.171) but a negative and significant effect on the male index of physical inactiveness (b = −0.111; 95% CI = −0.155, −0.066).
We estimated model 2 using the index of medication-based weight control behavior as the dependent variable. Again, we found differential policy effects by gender. The coefficients in the equations show that, when the social capital variable equals 0, obesity policy does not significantly reduce girls’ unhealthy weight control behavior but obesity policy does positively and significantly affect boys’ unhealthy weight control behavior (b = 0.158; 95% CI = 0.083, 0.234).
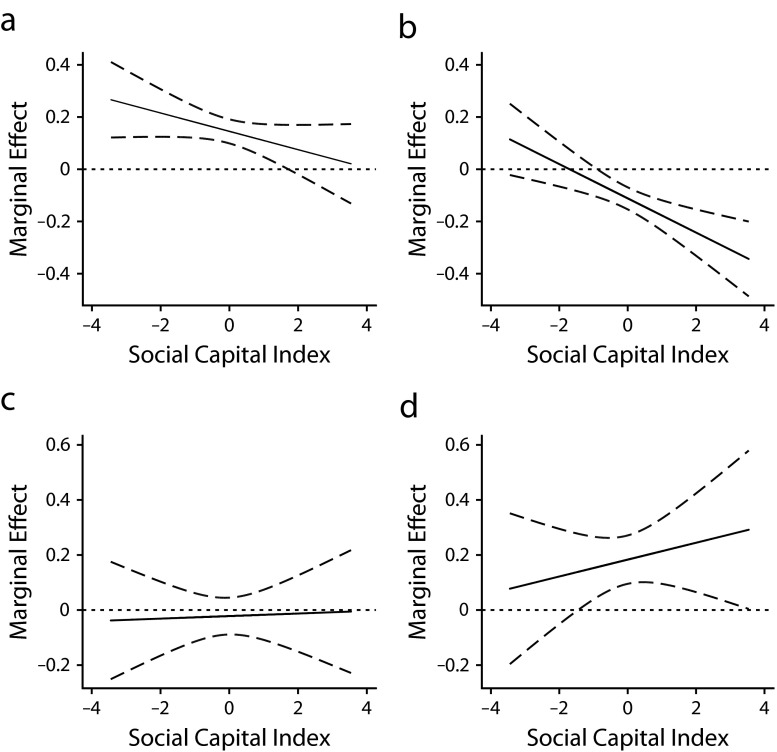
Because we included an interaction term multiplying the policy variable with the social capital variable, it is substantively more meaningful to graphically evaluate the interactive effects between obesity policy and social capital.40 In Figure 2, we plotted the marginal effects of obesity policy across the full range of the social capital variable and the corresponding 95% CIs. The top left panel in Figure 2 shows that when the level of social capital is low, obesity policy increases the female index of calorie-targeted weight control behavior. In other words, in states with low levels of social capital, more school-based obesity policies are associated with female students’ physical inactiveness, a higher proportion of female students who did not eat less to control weight, and a higher proportion of female students who fasted to control weight. These unintended policy effects diminish as social capital increases. The top right panel in Figure 2 shows that when social capital is low, obesity policy does not affect boys’ calorie-targeted weight control behavior (the 95% CIs overlap with 0). When social capital is high, however, obesity policy reduces the proportion of male students who did not exercise to lose weight, who did not eat less to lose weight, and who fasted to lose weight. In other words, obesity policy combined with high social capital produce desirable outcomes for male students, and the magnitude of such desirable policy effects increases as social capital increases.
FIGURE 2—
Social capital conditions of the marginal effects of obesity policy on weight control behavior for (a) female adolescents reporting calorie-targeted behavior, (b) male adolescents reporting calorie-targeted behavior, (c) female adolescents reporting medication-based behavior, and (d) male adolescents reporting medication-based behavior: Youth Risk Behavior Surveillance System, 1991–2009.
Note. Dotted lines indicate 95% confidence intervals.
The 2 bottom panels demonstrate how obesity policy and social capital are associated with heterogeneous medication-based weight control behavior by gender. School-based obesity policies do not significantly affect girls’ medication-based weight control activities, regardless of the level of social capital. However, more obesity policies combined with high levels of social capital are associated with a greater proportion of male students who reported taking diet or laxative pills to control weight, suggesting obesity policies implemented in active communities may lead to unintended policy effects for boys, that is, increasing male students’ pill intake weight control behavior.
In sum, we found a mixed pattern regarding the combined effects of school-based obesity policies and social capital. On one hand, school-based obesity policies can be effective in increasing exercise and reducing food intake but only for boys in states with high levels of social capital. Adopted policy interventions appear ineffective in promoting desirable behaviors among girls. On the other hand, social capital can benefit both boys and girls but through different mechanisms: it reduces the unintentional policy effects for female students but expands both the desirable and unintended effects for male students.
DISCUSSION
Several limitations of this study merit discussion. We did not use a multilevel design because the YRBSS surveys did not track the same cohort of students from 1991 to 2009. Therefore, we could not include repeated individual-level units in the sample. The macrolevel design, which links state-level policy and social capital measures to health behavior trends, is less informative in studying intergroup dynamics than is a multilevel data set. An extension of this study would use multilevel ecological models to longitudinally track how the 2 gender groups might influence each other and how the intragroup dynamics link to both policy and community conditions. They may also inform how intergroup dynamics increase the effectiveness of policy interventions.41,42
Second, the index of calorie-targeted weight control behavior entails a sample mean that dropped sharply between 1991 and 1993, primarily because of the low state participation rates in YRBSS 1991, 1993, and 1995.43 Future studies that use more reliable longitudinal data may produce more accurate estimations of the magnitude of policy effects. Lastly, the aggregated social capital index may mask social groups’ unequal access to social capital. Future studies using group-specific measures (e.g., comparing rural and urban populations or controlling for other socioeconomic factors) for social capital may produce more informative empirical findings on how social capital conditions the effect of obesity policies.
Despite limitations, our findings contribute to research on childhood obesity, social capital, and health. First, our research suggests that both adopted policies and social capital may be a source of, rather than a remedy for, unhealthy weight control behavior. Our findings on the positive association of obesity policy with adolescents’ unhealthy weight control behavior are consistent with those of previous studies44,45 that indicate a need to consider the potential harmful effects of school-based obesity policies. We identified a robust interactive relationship between school-based policies and social capital in adolescents’ weight control behaviors. The mixed policy outcomes suggest that the lack of social capital that supports school-based policies may impede effective policy interventions, highlighting the importance of building environments compatible with specific school-based policies.46 Effective policymaking for promoting healthy dietary behaviors and active lifestyles should balance the design of policy interventions and community conditions where the policies are implemented.
Second, we compared policy effects by gender and found that obesity policy and social capital are associated with heterogeneous responses. This supports a review of school-based policies, which reported that boys respond more to structural interventions facilitating physical activity, whereas girls are more influenced by social learning programs (e.g., family-oriented interventions).47 Conceivably, many large-scale school-based obesity policies may affect boys more than girls because they alter students’ health behaviors by changing their school environment. Furthermore, as policymakers and health professionals develop and revise obesity-related interventions, state legislative mandates may consider the gendered nature of obesity. For example, mandated physical education curricula could involve information on weight control. Policies targeting school dietary environments can combine with information-based programs to effectively convey messages for boys and girls. Policies that do not differentiate between girls’ and boys’ risk perceptions and behavioral patterns could incorporate inaccurate intervention goals, thus producing mixed results.
Acknowledgments
We thank Nathan Favero from Texas A&M University, for his assistance with the data collection process for this study. We thank Daniel Hawes from Kent State University and Rene Rocha from the University of Iowa for sharing their state-level social capital data and replication files. We also thank Kenneth J. Meier from Texas A&M University and Tim Reeskens from the University of Amsterdam for their perceptive comments.
Human Participant Protection
No protocol approval was needed for this study because data were obtained from secondary sources.
References
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405 [DOI] [PubMed] [Google Scholar]
- 2.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public health crisis, common sense cure. Lancet. 2002;360(9331):473–482 [DOI] [PubMed] [Google Scholar]
- 3.Chang VW, Christakis NA. Income inequality and weight status in US metropolitan areas. Soc Sci Med. 2005;61(1):83–96 [DOI] [PubMed] [Google Scholar]
- 4.Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am. 2001;48(4):893–907 [DOI] [PubMed] [Google Scholar]
- 5.Cohen-Cole E, Fletcher JM. Is obesity contagious? Social networks vs. environmental factors in the obesity epidemic. J Health Econ. 2008;27(5):1382–1387 [DOI] [PubMed] [Google Scholar]
- 6.Patrick K, Norman GJ, Calfas KJet al. Diet, physical activity, and sedentary behaviors as risk factors for overweight in adolescence. Arch Pediatr Adolesc Med. 2004;158(4):85–390 [DOI] [PubMed] [Google Scholar]
- 7.Wing RR. Behavioral interventions for obesity: recognizing our progress and future challenges. Obes Res. 2003;11(suppl):3S–6S [DOI] [PubMed] [Google Scholar]
- 8.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282(16):1561–1567 [DOI] [PubMed] [Google Scholar]
- 9.French SA, Story M, Fulkerson JA, Gerlach AF. Food environment in secondary schools: à la carte, vending machines, and food policies and practices. Am J Public Health. 2003;93(7):1161–1167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Hippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood gain in body mass index during the school year and during summer vacation. Am J Public Health. 2007;97(4):696–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carter RC. The impact of public schools on childhood obesity. JAMA. 2002;288(17):2180. [PubMed] [Google Scholar]
- 12.Veugelers PJ, Fitzgerald AL. Effectiveness of school programs at preventing childhood obesity: a multilevel comparison. Am J Public Health. 2005;95(3):432–435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flores R. Dance for health: improving fitness in African American and Hispanic adolescents. Public Health Rep. 1995;110(2):189–193 [PMC free article] [PubMed] [Google Scholar]
- 14.Robinson TN, Sirard JR. Preventing childhood obesity: a solution-oriented research paradigm. Am J Prev Med. 2005;28(2 suppl 2):194–201 [DOI] [PubMed] [Google Scholar]
- 15.Putnam R. Bowling Alone: The Collapse and Revival of American Community. New York, NY: Touchtone Books; 2000 [Google Scholar]
- 16.Cattell V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Soc Sci Med. 2001;52(10):1501–1516 [DOI] [PubMed] [Google Scholar]
- 17.Kim D, Subramanian SV, Gortmaker SL, Kawachi I. US state- and county-level social capital in relation to obesity and physical inactivity: a multilevel, multivariable analysis. Soc Sci Med. 2006;63(4):1045–1059 [DOI] [PubMed] [Google Scholar]
- 18.Franzini L, Elliott N, Cuccaro Pet al. Influences of physical and social neighborhood environments on children’s physical activity and obesity. Am J Public Health. 2008;99(2):271–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491–1498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379 [DOI] [PubMed] [Google Scholar]
- 21.Rose R. How much does social capital add to individual health? A survey study of Russians. Soc Sci Med. 2000;51(9):1421–1435 [DOI] [PubMed] [Google Scholar]
- 22.Runyan DK, Hunter WM, Socolar RRet al. Children who prosper in unfavorable environments: the relationship to social capital. Pediatrics. 1998;101(1 pt 1):12–18 [DOI] [PubMed] [Google Scholar]
- 23.Zierschm AM, Baum FE, MacDougall C, Putland C. Neighbourhood life and social capital: the implications for health. Soc Sci Med. 2005;60(1):71–86 [DOI] [PubMed] [Google Scholar]
- 24.Wisniewski AB, Chernausek SD. Gender in childhood obesity: family environment, hormones, and genes. Gend Med. 2009;6(suppl 1):76–85 [DOI] [PubMed] [Google Scholar]
- 25.Neumark-Sztainer D, Story M, Hannan PJ, Rex J. New moves: a school-based obesity prevention program for adolescent girls. Prev Med. 2003;37(1):41–51 [DOI] [PubMed] [Google Scholar]
- 26.Datar A, Sturm R. Physical education in elementary school and body mass index: evidence from the early childhood longitudinal study. Am J Public Health. 2004;94(9):1501–1506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105(1):e15. [DOI] [PubMed] [Google Scholar]
- 28.Paxton SJ, Schutz HK, Wertheim EH, Muir SL. Friendship clique and peer influences on body image concerns, dietary restraint, extreme weight-loss behaviors, and binge eating in adolescent girls. J Abnorm Psychol. 1999;108(2):255–266 [DOI] [PubMed] [Google Scholar]
- 29.Boutelle K, Neumark-Sztainer D, Story M, Resnick M. Weight control behaviors among obese, overweight, and nonoverweight adolescents. J Pediatr Psychol. 2002;27(6):531–540 [DOI] [PubMed] [Google Scholar]
- 30.Boehmer TK, Brownson RC, Haire-Joshu D, Dreisinger ML. Patterns of childhood obesity prevention legislation in the United States. Prev Chronic Dis. 2007;4(3):A56. [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Diseases Control and Prevention Youth Risk Behavior Survey. Available at: http://www.cdc.gov/HealthyYouth/yrbs/index.htm. Accessed April 10, 2011 [Google Scholar]
- 32.Centers for Diseases Control and Prevention State Legislative and Regulatory Action to Prevent Obesity and Improve Nutrition and Physical Activity. Available at: http://apps.nccd.cdc.gov/DNPALeg. Accessed April 10, 2011 [Google Scholar]
- 33.Centers for Disease Control and Prevention School Health Policies and Programs Study. Atlanta, GA; 1994–2006. Available at: http://www.cdc.gov/HealthyYouth/shpps/index.htm. Accessed July 15, 2011 [Google Scholar]
- 34.Hawes DP, Rocha RR. Social capital, racial diversity, and equity: evaluating the determinants of equity in the United States. Polit Res Q. 2011;64(4):924–937 [Google Scholar]
- 35.Zellner A. An effective method of estimating seemingly unrelated regressions and tests for aggregation bias. J Am Stat Assoc. 1962;57(3):348–368 [Google Scholar]
- 36.Martin S, Smith PC. Multiple public service performance indicators: toward an integrated statistical approach. J Public Admin Res Theory. 2005;15(4):599–613 [Google Scholar]
- 37.Maddala GS, Wu SW. A comparative study of unit root tests with panel data and a new simple test. Oxford Bull Econ Stat. 1999;61(S1):631–652 [Google Scholar]
- 38.Biorn E. Regression system for unbalanced panel data: a stepwise maximum likelihood procedure. J Econom. 2004;122(2):281–291 [Google Scholar]
- 39.Nguyen M, Nguyen H. XTSUR: Stata Module for Estimation of System of Regression Equations With Unbalanced Panel Data and Random Effects. Statistical Software Components. Boston, MA: Department of Economics, Boston College; 2010. Working Paper S456953, Revised version [Google Scholar]
- 40.Brambor T, Clark WR, Golder M. Understanding interaction models: improving empirical analysis. Polit Anal. 1994;14(1):63–82 [Google Scholar]
- 41.Oh HS, Labianca G, Chung MH. A multilevel model of group social capital. Acad Manage Rev. 2006;31(3):569–582 [Google Scholar]
- 42.McKay CM, Bell-Ellison BA, Wallace K, Ferron JM. A multilevel study of the associations between economic and social context, stage of adolescence, and physical activity and body mass index. Pediatrics. 2007;199(suppl 1):S84–S91 [DOI] [PubMed] [Google Scholar]
- 43.Centers for Diseases Control and Prevention Participation History & Data Quality, 1991–2009—High School. Available at: http://www.cdc.gov/healthyyouth/yrbs/history-states.htm. Accessed July 15, 2011 [Google Scholar]
- 44.Parcel GS, Green LW, Beetes BA. School-based programs to prevent or reduce obesity. In: Kranegor NA, Grave GD, Kretchmer N, eds. Childhood Obesity: A Biobehavioral Perspective. Caldwell, NJ: Telford Press; 1988:143–157 [Google Scholar]
- 45.Story M. School-based approaches for preventing and treating obesity. Int J Obes Relat Metab Disord. 1999;23(suppl 2):S43–S51 [DOI] [PubMed] [Google Scholar]
- 46.Sallis JF, Karen G. The role of built interventions in physical activity, eating, and obesity in childhood. Future Child. 2006;16(1):89–108 [DOI] [PubMed] [Google Scholar]
- 47.Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: an evidence-based review. Obesity (Silver Spring). 2008;16(5):1009–1018 [DOI] [PubMed] [Google Scholar]