Abstract
Objectives. We examined time-varying and time-invariant characteristics of nonfatal intentional self-harm episodes in relation to subsequent episodes of self-harm and suicide.
Methods. We conducted a follow-up cohort study through 2007 of 3600 patients discharged from hospitals in New Jersey with a primary diagnosis of intentional self-harm in 2003. We determined repetition of self-harm from hospital records and suicide from state registers.
Results. Use of methods other than drug overdose and cutting in self-harm events, greater medical severity of nonfatal episodes, and a history of multiple self-harm episodes increased the risk of suicide. However, most suicides occurred without these risk factors. Most suicides took place without intervening episodes of self-harm, and most persons used a low-lethality method (drug overdose or cutting) in their index episode, but switched to a more lethal method in their fatal episode.
Conclusions. Our findings suggest that preventing suicide among persons with a history of self-harm must account for the possibility that they will adopt methods with higher case-fatality ratios than they previously tried.
Intentional self-harm predicts suicide better than any other known risk factor,1–7 yet the great majority (89%–95%) of those with a history of self-harm do not go on to die by suicide.8 Indeed, the positive predictive power of self-harm for subsequent death by suicide is poor, even when considered in combination with other well-established behavioral and demographic risk factors.6,9–29 One infrequently studied aspect of self-harm that may help differentiate those who die by suicide in a subsequent event from those who do not concerns the methods used in nonfatal episodes.3,25–29 Studies addressing this question have found that the risk of subsequent suicide among self-injurers who used methods with high case-fatality ratios (CFRs; the percentage of cases that are fatal, calculated as suicide divided by the sum of suicides plus nonfatal episodes), such as hanging or poisoning with gases, was 2 to 5 times as high among persons whose index episode of self-harm involved methods with a low CFR, such as drug overdose.25–27 However, a study in Taiwan that controlled for gender found no such increased risk.3 Risk of eventual suicide in these studies ranged from 1% to 5% overall and from 2% to 13% for index self-harm events involving methods with high CFRs. A recent Swedish study reported rates of suicide as high as 40% to 55% for some methods,28 but this study combined suicide decedents who died during the index hospitalization with those who died in a subsequent event (Bo Runeson, PhD, Department of Clinical Neuroscience, Karolinska Institute; e-mail communication to C. B.; August 2011), thereby conflating the poor predictive power of methods used in nonfatal episodes with the highly predictive relation between the method used and the probability of death in any given suicidal act (i.e., the method-specific CFR).30–35
Most studies examining whether method choice in a nonfatal event predicts subsequent suicide have focused on the method used in the index event.3,28,29 By contrast, Bergen et al. examined the suicide risk associated with the last known nonfatal episode of intentional self-harm and found that compared with persons who used drug overdose in their last known episode of self-harm, suicide risk was twice to 5 times as high among those who previously tried hanging, suffocation, or poisoning by carbon monoxide or other gases.25 Patterns of progression from one method to another across the 2 most recent self-harm events did not predict subsequent suicide.
We built upon previous work that analyzed health care utilization data in a cohort of patients with their first known hospitalized episode of self-harm to assess factors associated with the risk of subsequent episodes of fatal and, separately, nonfatal self-harm (i.e., suicide and repetition of nonfatal intentional self-harm). This was the first population-based US study to (1) examine the role of method choice and the medical severity of nonfatal intentional self-harm in relation to repetition of self-harm, (2) model risk as a function of time-varying covariates updated at each self-harm episode, and (3) examine whether most suicide decedents with a history of self-harm died by the same methods they used previously or switched to methods that, in general, have higher CFRs.
METHODS
We used New Jersey hospital discharge data for 2003 to identify inpatients aged 15 years and older who had at least 1 diagnosis or external cause of injury codes (E-codes) that indicated intentional self-harm (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]36 codes E950–E959). Nonfatal intentional self-harm encompasses both suicide attempts and nonsuicidal self-harm. We defined the index self-harm episode as the first nonfatal act that resulted in hospitalization. We excluded persons who had at least 1 hospitalized episode of intentional self-harm in the 3 years (2000–2002) prior to the study, died as result of the index self-harm episode, or were not residents of New Jersey.
Covariates
We characterized demographic characteristics of self-injurers from the discharge record for the index event: gender, age group (15–34, 35–55, or ≥ 55 years), and race/ethnicity (non-Hispanic White or other). We grouped past-year psychiatric diagnoses, assessed at the index and each subsequent self-harm episode, into 8 categories, according to ICD-9-CM codes: depressive disorder, anxiety disorder, personality disorder, bipolar disorder, drug abuse or dependence, alcohol abuse or dependence, schizophrenia, and other.
For each self-harm admission, we collected information on the method used (from ICD-9-CM codes E950–E959) and clinical features of the hospital admission, such as whether the admission included a stay in the intensive care unit (ICU), and whether the ICU stay was characterized by procedures that suggested a medically consequential injury or poisoning (spinal tap, temporary tracheostomy, insertion of intercostal catheter for drainage, venous catheterization for renal dialysis, hemodialysis, exploratory laparotomy, measurement of systemic arterial blood gases, noninvasive mechanical ventilation, insertion of endotracheal tube, enteral infusion of nutritional substances, continuous invasive mechanical ventilation, transfusion of packed cells, transfusion of other serum, and parenteral infusion of concentrated nutritional substances).
We classified methods of attempt into 3 groups: cutting or piercing (E956), drug overdose (E950.0–E950.5), and all other (drowning, falls, firearm, gas poisoning, nondrug poisoning, hanging or suffocation, and other methods; E950.6–E959, excluding E956). Although our category for other encompassed a diverse group of methods, each represented only a few index incidents in our data. The discharge data from 2003 to 2007 had 1 field for E-codes. Starting from 2008, the format for discharge data allowed up to 6 E-codes. To classify methods, we used the first E-code. If no E-code was available, we used the first E-code in the list of diagnosis codes.
We compared predictors of repetition of nonfatal intentional self-harm and death by suicide. We determined repetition of nonfatal self-harm by linking the index cohort to hospital discharge data for 2003 to 2009 by name, date of birth, race, and social security number. We also linked the index cohort to the state death certificate database by name and date of birth to determine who died by suicide during the study period (codes X60–X84 from the International Statistical Classification of Diseases, 10th Revision37).
Analysis
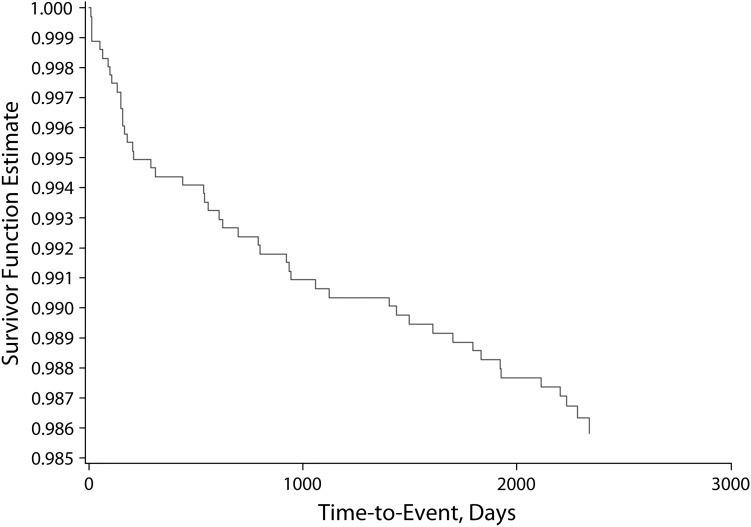
We used Cox hazard models for analyses with suicide as the outcome; time-varying covariates were method used, clinical features of the attempt (ICU stay and number and type of psychiatric diagnosis categories), and number of previous episodes of intentional self-harm. We used an extension of the Cox model38 for analyses with repetition of nonfatal self-harm as the outcome for recurrent events. We excluded the interval of hospitalization for any nonfatal episode from these analyses because currently hospitalized patients were not at risk for hospitalization for intentional self-harm. The hazard baseline was the same regardless of the number of previous episodes of self-harm. A sensitivity analysis allowed the hazard baseline to change with each subsequent episode of self-harm without substantively altering our findings (i.e., we found no substantive differences between common and event-specific hazard baseline). Observation time in all models stopped when a person died. Figure 1 shows a Kaplan–Meier plot for suicide after the index episode of self-harm.
FIGURE 1—
Probability of remaining free of suicide and time since index intentional self-harm episode: New Jersey, 2003–2007.
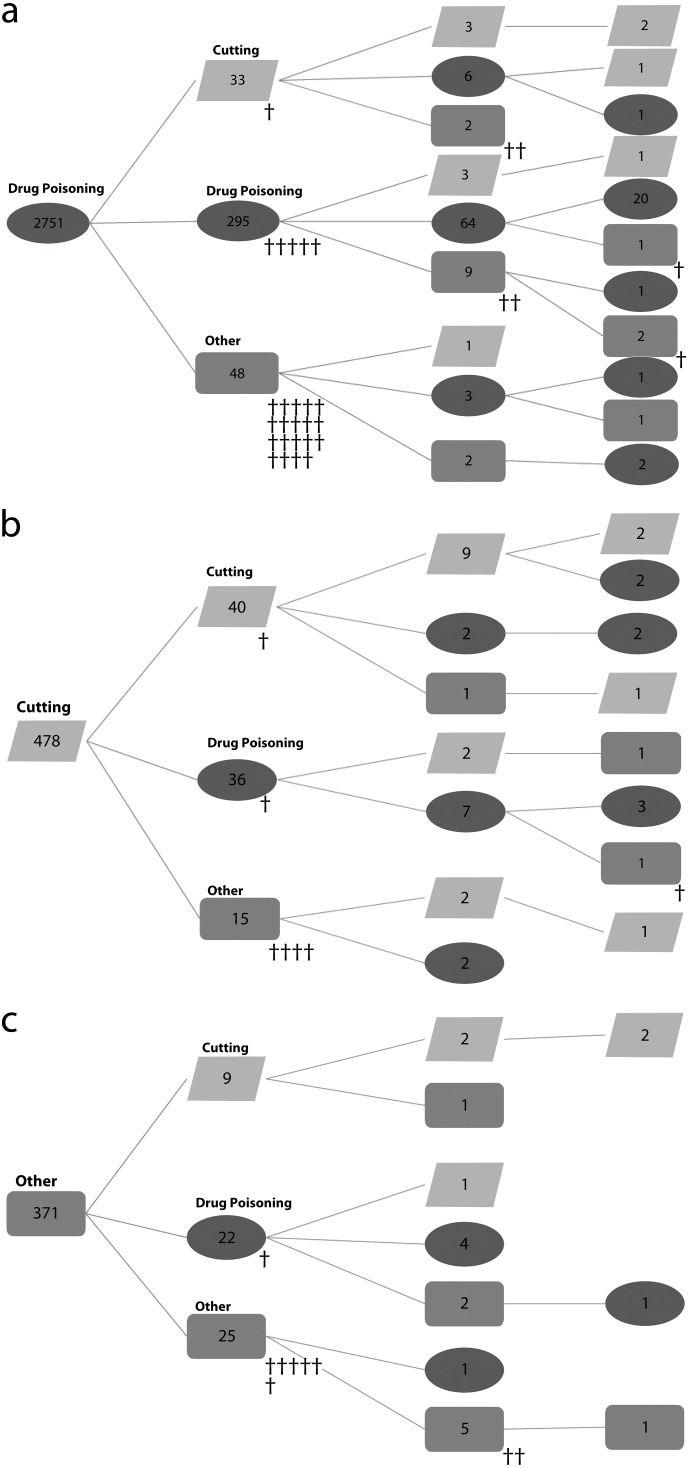
The event tree (Figure 2) illustrates the sequence of methods used in the index and subsequent episodes of self-harm up to and including the fourth event, because only 1 suicide occurred after a fourth nonfatal event. Summary measures of method switching among cohort members who subsequently died by suicide and those whose subsequent episodes of self-harm proved nonfatal are presented in tabular format, as are the method-specific and overall CFRs in each subsequent wave of self-injury, by the index method used.
FIGURE 2—
Methods used in index and subsequent self-harm episodes among persons with index episodes involving (a) drug overdose, (b) cutting or piercing, and (c) all other methods: New Jersey, 2003–2007.
Note. † = 1 death. The roots of the trees indicate the number of self-injurers who used a given method on their index self-harm episode. The number in each node to the right indicates the number of people with subsequent events by method used on their second, third, and fourth episodes. Of 3600 self-injurers, 25 had more than 4 episodes; 1 of these died by suicide. In total 48 persons died by suicide: 24 by suffocation, 8 by nondrug poisoning, 7 by drug overdose, 4 by firearm, 2 each by falls and cutting or piercing, and 1 by drowning.
RESULTS
Our cohort consisted of 3600 persons discharged alive from a New Jersey hospital in 2003 after an episode of nonfatal intentional self-harm (Table 1). By design, all 3600 had no record of having been hospitalized for self-harm between 2000 and their index event in 2003. Index episodes most frequently involved drug overdose (76%), followed by cutting or piercing (13%). Overall, 36% of study cohort members were admitted to the ICU on their index admission (22% of whom received procedures suggesting medically consequential injury or overdose). Approximately half of all patients were coded as having 2 or more psychiatric diagnoses during their index admission (52%), 41% received 1, and 7% received none. The most common categories of psychiatric diagnoses at the index episode were depressive disorders (56%), drug- and alcohol-related disorders (28% and 23%, respectively), anxiety disorders (15%), and bipolar disorders (15%).
TABLE 1—
Unadjusted Associations Between Baseline Characteristics and Repetition of Nonfatal Self-Harm and Dying by Suicide: New Jersey, 2003–2007
| Cohort Members With Subsequent Self-Harm Episodes |
|||
| Variable | Index Self-Harm Cohort, No. (%) | Nonfatal,a No. (%) | Suicide, No. (%) |
| Total | 3600 (100.0) | 486 (13.5) | 48 (1.3) |
| Gender | |||
| Male | 1497 (41.6) | 207 (13.8) | 34 (2.3) |
| Female | 2103 (58.4) | 279 (13.3) | 14 (0.7) |
| Baseline age group, y | |||
| 15–34 | 1813 (50.4) | 216 (11.9) | 20 (1.1) |
| 35–54 | 1363 (37.9) | 229 (16.8) | 21 (1.5) |
| ≥ 55 | 424 (11.8) | 41 (9.7) | 7 (1.7) |
| Race/ethnicity | |||
| White, non-Hispanic | 2403 (66.8) | 366 (15.2) | 43 (1.8) |
| Black, non-Hispanic | 443 (12.3) | 52 (11.7) | 0 (0.0) |
| Hispanic | 468 (13.0) | 48 (10.3) | 3 (0.6) |
| Other | 286 (7.9) | 20 (7.0) | 2 (0.7) |
| ICU visit at index episode | |||
| No | 2289 (63.6) | 313 (13.7) | 19 (0.8) |
| Yes (no procedures indicating severe injury)b | 1024 (28.4) | 135 (13.2) | 17 (1.7) |
| Yes (underwent procedures indicating severe injury)b | 287 (8.0) | 38 (13.2) | 12 (4.2) |
| Index method used | |||
| Cutting | 478 (13.3) | 85 (17.8) | 7 (1.5) |
| Drug overdose | 2751 (76.4) | 352 (12.8) | 32 (1.2) |
| Otherc | 371 (10.3) | 49 (13.2) | 9 (2.4) |
| Psychiatric diagnoses at baseline | |||
| 0 | 238 (6.6) | 18 (7.6) | 1 (0.4) |
| 1 | 1473 (40.9) | 145 (9.8) | 22 (1.5) |
| ≥ 2 | 1889 (52.5) | 323 (17.1) | 25 (1.3) |
| Baseline psychiatric diagnosis category | |||
| Depression | 2027 (56.3) | 271 (13.4) | 27 (1.3) |
| Anxiety | 542 (15.1) | 87 (16.1) | 4 (0.7) |
| Personality | 311 (8.6) | 61 (19.6) | 5 (1.6) |
| Bipolar | 550 (15.3) | 122 (22.2) | 9 (1.6) |
| Drug problem | 1014 (28.2) | 168 (16.6) | 13 (1.3) |
| Alcohol problem | 816 (22.7) | 138 (16.9) | 17 (2.1) |
| Schizophrenia | 233 (6.5) | 52 (22.3) | 7 (3.0) |
| Other | 625 (17.4) | 54 (8.6) | 4 (0.6) |
| Nonfatal self-harm episodes over study period | |||
| ≥ 1 (index) | 3600 (100.0) | 486 (13.5) | 48 (1.3) |
| ≥ 2 | 486 (13.5) | 128 (26.3) | 10 (2.1) |
| ≥ 3 | 128 (3.6) | 47 (36.7) | 4 (3.1) |
| ≥ 4 | 47 (1.3) | 25 (53.2) | 1 (2.1) |
Note. ICU = intensive care unit. Totals may not add to 100% because of rounding.
Percentage of index cohort with subsequent episode.
ICU procedures indicating medically severe injury were spinal tap, temporary tracheostomy, insertion of intercostal catheter for drainage, venous catheterization for renal dialysis, hemodialysis, exploratory laparotomy, measurement of systemic arterial blood gases, noninvasive mechanical ventilation, insertion of endotracheal tube, enteral infusion of nutritional substances, continuous invasive mechanical ventilation, transfusion of packed cells, transfusion of other serum, and parenteral infusion of concentrated nutritional substances.
Other methods were 6 drownings, 26 falls, 12 carbon monoxide poisonings, and 38 hangings.
Of the 3600 members of the cohort, 486 (13%) had at least 1 subsequent admission for nonfatal intentional self-harm and 48 (1.3%) died by suicide during the study period (Table 1). Subsequent nonfatal self-harm admissions were as frequent for males as for females and for patients admitted to and not admitted to the ICU. Persons with 2 or more psychiatric disorders were more likely than those with no psychiatric comorbidity to repeat self-harm over the study period (17% with comorbidity, 10% with a single psychiatric disorder, and 8% without a psychiatric disorder diagnosis).
Those who died by suicide, but not those with subsequent nonfatal episodes, were more likely to be male, to have been admitted to the ICU (and to have required procedures indicative of greater medical severity in the ICU), and to have used methods other than cutting, piercing, or drug overdose in their index episode (Table 1). Depressive disorders were diagnosed at the index event in more than half of all patients, but were underrepresented among those who were later admitted for another episode of nonfatal self-harm or who subsequently died by suicide (Table 1). Drug-related disorders and anxiety disorders were modestly overrepresented among those who were later admitted for repetition of nonfatal self-harm, but underrepresented among members of our cohort who eventually died by suicide. Among the 486 persons with episodes of nonfatal self-harm subsequent to their index event, 3 out of 4 (n = 358) had 2 episodes (the index and 1 repeat episode), 81 had 3 episodes, 22 had 4, and 25 had 5 or more (Table 1).
Of the 48 suicides over the 5-year follow-up period (Figure 1), 16 occurred within the first 6 months (4 occurred within 1 month after the index episode, 7 within 3 months, 16 within 6 months), more than half occurred within 2 years (20 within 1 year, 27 within 2 years), and approximately 70% within 3 years (33 within 3 years).
Table 2 shows adjusted estimates of association between characteristics of our cohort and the risk of (1) suicide, and (2) repetition of nonfatal self-harm. As observed in our bivariate model, which incorporated the index characteristics, female gender did not predict subsequent self-harm (hazard ratio [HR] = 1.1; 95% confidence interval [CI] = 0.9, 1.3) but was protective against subsequent suicide (HR = 0.3; 95% CI = 0.2, 0.6). Similarly, admission to the ICU did not predict subsequent nonfatal episodes of self-harm but did predict higher risk of suicide, especially if the ICU admission involved medical procedures suggestive of severe poisoning or medical injury (HR = 4.2; 95% CI = 1.8, 9.6). Persons who used cutting or piercing were modestly more likely than those who overdosed with drugs or injured themselves with other methods to be admitted for a repeat episode of nonfatal self-harm (HR = 1.3; 95% CI = 1.0, 1.6), but not significantly more likely to die by suicide. By contrast, those who used other methods (e.g., hanging) in an index or subsequent episode of nonfatal self-harm were not more likely than persons who self-injured with a drug overdose to nonfatally harm themselves in the future but were approximately twice as likely to die by suicide in a subsequent event (HR = 2.0; 95% CI = 1.0, 4.3; P < .06). Psychiatric comorbidity significantly increased the risk of nonfatal repetition of self-harm (HR = 1.5; 95% CI = 1.2, 1.7) but not of suicide (HR = 1.2; 95% CI = 0.6, 2.3). The number of repeated nonfatal episodes increased the risk of subsequent nonfatal self-harm and suicide, with suggestive evidence that risk may plateau at 3 previous episodes of self-harm. We had limited power to examine multivariable associations between separate psychiatric diagnoses and the risk of suicide. In models estimating the far more frequent outcome of repeated self-harm, several psychiatric disorders were significantly associated with elevated risk relative to depressive disorders: personality (HR = 1.4), bipolar (HR = 1.3), drug (HR = 1.9), and alcohol (HR = 1.4) disorders.
TABLE 2—
Cox Hazards Models for Time From Index Episode of Self-Harm to Subsequent Episode and to Suicide: New Jersey, 2003–2007
| Subsequent Self-Harm Episode |
||
| Variable | Nonfatal, HR (95% CI) | Suicide, HR (95% CI) |
| Gender | ||
| Male (Ref) | 1.0 | 1.0 |
| Female | 1.1 (0.9, 1.3) | 0.3 (0.2, 0.6) |
| Baseline age group, y | ||
| 15–34 (Ref) | 1.0 | 1.0 |
| 35–54 | 1.4 (1.2, 1.7) | 1.0 (0.5, 1.9) |
| ≥ 55 | 1.1 (0.8, 1.4) | 1.6 (0.6, 4.0) |
| Race/ ethnicity | ||
| White, non-Hispanic (Ref) | 1.0 | 1.0 |
| Other | 0.7 (0.6, 0.9) | 0.3 (0.1, 0.7) |
| ICU admission at index episode | ||
| No (Ref) | 1.0 | 1.0 |
| Yes (no procedures indicating severe injury)a | 1.1 (0.9, 1.3) | 2.3 (1.2, 4.6) |
| Yes (underwent procedures indicating severe injury)a | 1.1 (0.8, 1.4) | 4.2 (1.8, 9.6) |
| Method of nonfatal self-harm | ||
| Drug overdose (Ref) | 1.0 | 1.0 |
| Cutting/piercing | 1.3 (1.0, 1.6) | 1.7 (0.7, 4.2) |
| Other | 1.1 (0.8, 1.4) | 2.0 (1.0, 4.3) |
| Psychiatric diagnoses at baseline | ||
| 0 | 0.9 (0.6, 1.3) | 0.3 (0.0, 2.3) |
| 1 (Ref) | 1.0 | 1.0 |
| ≥ 2 | 1.5 (1.2, 1.7) | 1.2 (0.6, 2.3) |
| Nonfatal self-harm episodes over study period | ||
| ≥ 1 (index; Ref) | 1.0 | 1.0 |
| ≥ 2 | 3.9 (3.2, 4.9) | 2.2 (0.9, 5.5) |
| ≥ 3 | 9.2 (6.5, 13.1) | 8.4 (2.4, 29.8) |
| ≥ 4 | 29.3 (19.2, 44.8) | 6.9 (0.9, 51.9) |
Note. CI = confidence interval; HR = hazard ratio; ICU = intensive care unit.
ICU procedures indicating medically severe injury were spinal tap, temporary tracheostomy, insertion of intercostal catheter for drainage, venous catheterization for renal dialysis, hemodialysis, exploratory laparotomy, measurement of systemic arterial blood gases, noninvasive mechanical ventilation, insertion of endotracheal tube, enteral infusion of nutritional substances, continuous invasive mechanical ventilation, transfusion of packed cells, transfusion of other serum, and parenteral infusion of concentrated nutritional substances.
Figure 2 illustrates the sequence of nonfatal self-harm and suicide following the index episode, by method. Most suicide decedents (38/48) died on the first known act of intentional self-harm following the index event. The majority of suicide decedents who survived a second episode of self-harm died on their third attempt. Regardless of the index method used, most of the suicide deaths among our cohort involved methods in the other category (predominantly suffocation, hanging, or carbon monoxide poisoning). For example, of the 2751 cohort members whose index episode involved drug overdose, 32 died by suicide (Figure 1a), 26 (81%) of whom used other methods in their final act, 5 (16%) of whom used drug overdose, and 1 of whom (3%) used cutting or piercing. Among the 26 who died using other methods, 16 died by suffocation or hanging, 5 by carbon monoxide or other gas poisoning, 3 by firearm, and 1 each by drowning and fall from height. One person with an index episode involving drug overdose died by suicide after more than 3 subsequent episodes of self-harm; the final, fatal method was suffocation.
Table 3 summarizes some of the salient features depicted in Figure 1 and shows CFRs for various pathways from index episode through the fifth wave of subsequent acts of self-harm. We detected 6 noteworthy patterns. First, most suicides occurred among persons who were never admitted to a hospital for a second self-harm event (38/48). Second, the CFR associated with methods other than drug overdose and cutting (31.5%) was much higher than the CFR associated with either overdose (1.3%) or cutting (1.5%). Third, 81% of persons who overdosed with drugs and 71% of cutters who eventually died by suicide switched to more lethal methods in their final act. Indeed, most people who died by suicide in our cohort (31 out of 48) used a low-lethality method in their index episode but switched to other, generally more lethal, methods in their fatal episode. Fourth, among the 10% of self-injurers who used a method other than drug overdose or cutting in their index episode, those who died by suicide tended to continue to use methods with high CFRs. Fifth, the method-specific CFR in subsequent acts of self-harm was independent of the index method used. For example, if a subsequent episode involved methods other than drug overdose or cutting, the CFR was similar whether the first episode involved overdose (36.1%), cutting (27.8%), or other methods (23.5%). Finally, the method-specific CFR was independent of the number of previous acts of self-harm. For example, the CFR among index poisoners for subsequent nonfatal episodes involving overdose was unrelated to whether the overdose episode was the second (6.6%), third (4.3%), or fourth (6.1) episode after the index event.
TABLE 3—
Sequence, Lethality, Method, and Method Switching in Repeat Self-Harm Episodes, by Method of Index Episode: New Jersey, 2003–2007
| Index Self-Harm Method: Drug Overdose |
Index Self-Harm Method: Cutting |
Index Self-Harm Method: Other |
Index Self-Harm Method: Total |
|||||||||
| Variable | Nonfatal, No. or % | Suicide, No. or % | CFR, % | Nonfatal, No. | Suicide, No. or % | CFR, % | Nonfatal, No. or % | Suicide, No. or % | CFR, % | Nonfatal, No. or % | Suicide, No. or % | CFR, % |
| Self-harm episode | ||||||||||||
| Index | 2751 | NA | NA | 478 | NA | NA | 371 | NA | NA | 3600 | NA | NA |
| Second | 352 | 25 | 6.6 | 85 | 6 | 6.6 | 49 | 7 | 12.5 | 486 | 38 | 7.3 |
| Third | 89 | 4 | 4.3 | 25 | 0 | 0.0 | 14 | 2 | 12.5 | 128 | 6 | 4.5 |
| Fourth | 31 | 2 | 6.1 | 12 | 1 | 7.7 | 4 | 0 | 0.0 | 47 | 3 | 6.0 |
| Subsequent | 58 | 1 | 1.7 | 6 | 0 | 0.0 | 3 | 0 | 0.0 | 67 | 1 | 1.5 |
| Subsequent episode | ||||||||||||
| Drug overdose | 429 | 5 | 1.2 | 58 | 1 | 1.7 | 28 | 1 | 3.4 | 515 | 7 | 1.3 |
| Cutting | 55 | 1 | 1.8 | 57 | 1 | 1.7 | 16 | 0 | 0.0 | 128 | 2 | 1.5 |
| Othera | 46 | 26 | 36.1 | 13 | 5 | 27.8 | 26 | 8 | 23.5 | 85 | 39 | 31.5 |
| Proportion who ever used methods other than cutting or overdose after the index method | 11.1 | 81.3 | NA | 15.3 | 71.4 | NA | 44.9 | 88.9 | NA | 15.2 | 81.3 | NA |
| Proportion who ever switched method category | 21.6 | 84.4 | NA | 60.0 | 85.7 | NA | 63.3 | 11.1 | NA | 32.5 | 70.8 | NA |
Note. CFR = case fatality ratio; NA = not applicable. CFR indicates percentage of cases that are fatal (suicide divided by the sum of suicide plus nonfatal episodes).
All methods except cutting and overdoses, such as poisoning by gases or chemicals, hanging, suffocation, drowning, firearm.
DISCUSSION
Ours was the first US study to examine several characteristics of intentional self-harm as predictors of subsequent death by suicide and repetition of nonfatal self-harm. Our finding that the methods used in and the medical severity of nonfatal self-harm episodes were independently associated with subsequent suicide risk but not with subsequent risk of nonfatal self-harm has not been reported previously. Few studies have examined whether the medical severity of self-harm events predicts subsequent suicide; those that have did not examine the role of method choice independently.1,6 Consistent with others, we did not find a significant association between repetition of nonfatal self-harm and the potential lethality of index events (assessed in our work by the method used and in previous work by physicians’ estimation of the lethality of an index event had it not been treated).39
Our multivariate finding that intentional self-harm with methods other than drug overdose, cutting, or piercing at any time during the study period was associated with an increased risk of subsequent suicide is similar to observations from studies that analyzed the method used in the index event3,40 and in the penultimate episode of self-injury.25 Our finding that cutting or piercing (relative to drug overdose) was associated both with an increased risk of nonfatal repetition (HR = 1.3) and of suicide (HR = 1.7), though not statistically significant, is consistent with some studies4,25 but not others.40 This finding is of interest because self-injurers who use this method appear to be less likely than those who use other methods to receive referral for psychosocial assessment,41–43 possibly because some episodes of cutting may not be characterized by expressions of suicidal intent. Consistent with findings from previous work, we also found that the risk of repeated self-harm and of suicide was greatest immediately following discharge from the hospital for self-harm and that subsequent suicide risk was higher for males.1,3,5,6,8,15,17,25,44–46 In our cohort, the number of discrete psychiatric conditions was more strongly related to repetition of nonfatal self-harm than to subsequent suicide. To our knowledge, this has not been reported previously.
Our study was the first to describe the ramifications of method choice among a cohort of patients discharged alive after their first known hospitalized episode of self-harm. For most cohort members, the vast majority of whom used drug overdose or cutting in their index event, the pathway to suicide largely entailed switching to other methods. For the 10% of self-injurers who used a method other than overdose or cutting in their index episode, those who died by suicide in a subsequent episode tended to use methods with higher CFRs, whereas those who used cutting or overdose in subsequent episodes were as likely to survive those acts as were persons whose index episode involved overdose or cutting. Independent of the index method used, most suicides (38/48) occurred among people who were never admitted to a hospital for a second nonfatal self-harm event.
Limitations
Our cohort comprised residents of New Jersey and was not, therefore, representative of the larger US population. Indeed, with respect to rates of suicide and methods involved, New Jersey looks quite different from the country as a whole. For example, the suicide rate is lower (6.4 vs 12.0 per 100 000 population in 2009), and firearms are less frequently used in completed suicides (31% vs 51%).47 Only persons who survived an initial act of intentional self-harm were eligible for our study. Our cohort did not include self-injurers who failed to seek medical attention at a hospital, presented to a hospital but were not admitted, or presented to hospitals outside of New Jersey. Because we relied on information routinely collected in New Jersey hospital discharge records, we may have underestimated the risk of subsequent self-harm and may have introduced bias if members of our cohort who were lost to follow-up differed from those not lost to follow-up in ways relevant to our exposures of interest.
Because drug overdoses and cuttings were so numerous, we grouped all other methods into a third category, other. The other group combined higher-lethality methods (e.g., hanging) and lower-lethality methods (e.g., blunt trauma). With a larger data set we would have parsed the other category into groups reflecting relative lethality, or, ideally, specific methods. Finally, our analysis did not account for measures of suicidal intent, social class, marital status, or medical illnesses.
Conclusions
Our results add to the existing literature on repetition of self-harm and subsequent suicide. Our findings corroborate previous work among non-US cohorts of self-injurers and add to the emerging literature suggesting that method choice and medical severity of nonfatal intentional self-harm episodes heighten the risk of subsequent suicide. Our observation that most persons with a history of self-harm who die by suicide use a low-lethality method in their index episode but a high-lethality method in their fatal episode has not been reported previously.
Consistent with the poor predictive value reported in previous investigations,6,9–16 we were unable to reliably predict who among our high-risk cohort would subsequently die by suicide despite the elevated risk associated with several characteristics we analyzed. In most instances, for example, those who eventually died by suicide were people whose nonfatal episodes involved drug overdose or cutting, who had not been admitted to the ICU with procedures suggestive of medically severe injury, and who died without intervening episodes of nonfatal self-injury. Our findings suggest that preventing suicide among persons with a history of self-harm must account for the method switching most of our suicide decedents engaged in, moving to methods generally associated with higher CFRs.
Acknowledgments
Preparation of this article was supported by grants from the Joyce Foundation to M. Miller, C. Barber, and D. Azrael.
Note. The views and opinions expressed in this study are those of the authors and should not be construed to represent the views of any of the sponsoring organizations or agencies or the US government. The sponsors had no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; or the preparation, review, or approval of the article.
Human Participant Protection
This project was approved by the New Jersey Department of Health institutional review board.
References
- 1.Suokas J, Suominen K, Isometsa E, Ostamo A, Lonnqvist J. Long-term risk factors for suicide mortality after attempted suicide—findings of a 14-year follow-up study. Acta Psychiatr Scand. 2001;104(2):117–121. doi: 10.1034/j.1600-0447.2001.00243.x. [DOI] [PubMed] [Google Scholar]
- 2.Bilén K, Ottosson C, Castrén M et al. Deliberate self-harm patients in the emergency department: factors associated with repeated self-harm among 1524 patients. Emerg Med J. 2011;(12):1019–1025. doi: 10.1136/emj.2010.102616. [DOI] [PubMed] [Google Scholar]
- 3.Chen VC, Tan HK, Chen CY et al. Mortality and suicide after self-harm: community cohort study in Taiwan. Br J Psychiatry. 2011;198(1):31–36. doi: 10.1192/bjp.bp.110.080952. [DOI] [PubMed] [Google Scholar]
- 4.Cooper J, Kapur N, Webb R et al. Suicide after deliberate self-harm: a 4-year cohort study. Am J Psychiatry. 2005;162(2):297–303. doi: 10.1176/appi.ajp.162.2.297. [DOI] [PubMed] [Google Scholar]
- 5.Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182:537–542. doi: 10.1192/bjp.182.6.537. [DOI] [PubMed] [Google Scholar]
- 6.Owens D, Wood C, Greenwood DC, Hughes T, Dennis M. Mortality and suicide after non-fatal self-poisoning: 16-year outcome study. Br J Psychiatry. 2005;187:470–475. doi: 10.1192/bjp.187.5.470. [DOI] [PubMed] [Google Scholar]
- 7.Zahl DL, Hawton K. Repetition of deliberate self-harm and subsequent suicide risk: long-term follow-up study of 11,583 patients. Br J Psychiatry. 2004;185:70–75. doi: 10.1192/bjp.185.1.70. [DOI] [PubMed] [Google Scholar]
- 8.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry. 2002;181:193–199. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- 9.Pokorny AD. Prediction of suicide in psychiatric patients. Report of a prospective study. Arch Gen Psychiatry. 1983;40(3):249–257. doi: 10.1001/archpsyc.1983.01790030019002. [DOI] [PubMed] [Google Scholar]
- 10.Pokorny AD. Suicide prediction revisited. Suicide Life Threat Behav. 1993;23(1):1–10. [PubMed] [Google Scholar]
- 11.Mann JJ, Currier D, Stanley B, Oquendo MA, Amsel LV, Ellis SP. Can biological tests assist prediction of suicide in mood disorders? Int J Neuropsychopharmacol. 2006;9(4):465–474. doi: 10.1017/S1461145705005687. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein RB, Black DW, Nasrallah A, Winokur G. The prediction of suicide. Sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1906 patients with affective disorders. Arch Gen Psychiatry. 1991;48(5):418–422. doi: 10.1001/archpsyc.1991.01810290030004. [DOI] [PubMed] [Google Scholar]
- 13.Stefansson J, Nordstrom P, Jokinen J. Suicide Intent Scale in the prediction of suicide. J Affect Disord. 2012;136(1–2):167–171. doi: 10.1016/j.jad.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 14.Tidemalm D, Elofsson S, Stefansson CG, Waern M, Runeson B. Predictors of suicide in a community-based cohort of individuals with severe mental disorder. Soc Psychiatry Psychiatr Epidemiol. 2005;40(8):595–600. doi: 10.1007/s00127-005-0941-y. [DOI] [PubMed] [Google Scholar]
- 15.Harriss L, Hawton K. Suicidal intent in deliberate self-harm and the risk of suicide: the predictive power of the Suicide Intent Scale. J Affect Disord. 2005;86(2–3):225–233. doi: 10.1016/j.jad.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 16.Powell J, Geddes J, Deeks J, Goldacre M, Hawton K. Suicide in psychiatric hospital in-patients. Risk factors and their predictive power. Br J Psychiatry. 2000;176:266–272. doi: 10.1192/bjp.176.3.266. [DOI] [PubMed] [Google Scholar]
- 17.Haw C, Bergen H, Casey D, Hawton K. Repetition of deliberate self-harm: a study of the characteristics and subsequent deaths in patients presenting to a general hospital according to extent of repetition. Suicide Life Threat Behav. 2007;37(4):379–396. doi: 10.1521/suli.2007.37.4.379. [DOI] [PubMed] [Google Scholar]
- 18.Haw C, Hawton K, Casey D. Deliberate self-harm patients of no fixed abode: a study of characteristics and subsequent deaths in patients presenting to a general hospital. Soc Psychiatry Psychiatr Epidemiol. 2006;41(11):918–925. doi: 10.1007/s00127-006-0106-7. [DOI] [PubMed] [Google Scholar]
- 19.Hawton K, Harriss L. Deliberate self-harm in people aged 60 years and over: characteristics and outcome of a 20-year cohort. Int J Geriatr Psychiatry. 2006;21(6):572–581. doi: 10.1002/gps.1526. [DOI] [PubMed] [Google Scholar]
- 20.Hawton K, James A. Suicide and deliberate self harm in young people. BMJ. 2005;330(7496):891–894. doi: 10.1136/bmj.330.7496.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hawton K, Sutton L, Haw C, Sinclair J, Harriss L. Suicide and attempted suicide in bipolar disorder: a systematic review of risk factors. J Clin Psychiatry. 2005;66(6):693–704. doi: 10.4088/jcp.v66n0604. [DOI] [PubMed] [Google Scholar]
- 22.Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychol Med. 2001;31(5):837–845. doi: 10.1017/s0033291701003889. [DOI] [PubMed] [Google Scholar]
- 23.Crandall C, Fullerton-Gleason L, Aguero R, LaValley J. Subsequent suicide mortality among emergency department patients seen for suicidal behavior. Acad Emerg Med. 2006;13(4):435–442. doi: 10.1197/j.aem.2005.11.072. [DOI] [PubMed] [Google Scholar]
- 24.Oh SH, Park KN, Jeong SH, Kim HJ, Lee CC. Deliberate self-poisoning: factors associated with recurrent self-poisoning. Am J Emerg Med. 2011;29(8):908–912. doi: 10.1016/j.ajem.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 25.Bergen H, Hawton K, Waters K et al. How do methods of non-fatal self-harm relate to eventual suicide? J Affect Disord. 2012;136(3):526–533. doi: 10.1016/j.jad.2011.10.036. [DOI] [PubMed] [Google Scholar]
- 26.Holley HL, Fick G, Love EJ. Suicide following an inpatient hospitalization for a suicide attempt: a Canadian follow-up study. Soc Psychiatry Psychiatr Epidemiol. 1998;33(11):543–551. doi: 10.1007/s001270050092. [DOI] [PubMed] [Google Scholar]
- 27.Nielsen B, Petersen P, Rask PH, Krarup G. Selvmord og andre dødsårsager hos patienter indlagt efter selvmordsforsog. Ti ars [Suicide and other causes of death in patients admitted for attempted suicide. 10-year follow-up] Ugeskr Laeger. 1995;157(15):2149–2153. [PubMed] [Google Scholar]
- 28.Runeson B, Tidemalm D, Dahlin M, Lichtenstein P, Langstrom N. Method of attempted suicide as predictor of subsequent successful suicide: national long term cohort study. BMJ. 2010;341:c3222. doi: 10.1136/bmj.c3222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Skogman K, Alsen M, Ojehagen A. Sex differences in risk factors for suicide after attempted suicide—a follow-up study of 1052 suicide attempters. Soc Psychiatry Psychiatr Epidemiol. 2004;39(2):113–120. doi: 10.1007/s00127-004-0709-9. [DOI] [PubMed] [Google Scholar]
- 30.Miller M, Azrael D, Hemenway D. The epidemiology of case fatality rates for suicide in the northeast. Ann Emerg Med. 2004;43(6):723–730. doi: 10.1016/j.annemergmed.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 31.Spicer RS, Miller TR. Suicide acts in 8 states: incidence and case fatality rates by demographics and method. Am J Public Health. 2000;90(12):1885–1891. doi: 10.2105/ajph.90.12.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eddleston M, Bateman DN. Major reductions in global suicide numbers can be made rapidly through pesticide regulation without the need for psychosocial interventions. Soc Sci Med. 2011;72(1):1–2. doi: 10.1016/j.socscimed.2010.10.013. discussion 3–5. [DOI] [PubMed] [Google Scholar]
- 33.Gunnell D, Fernando R, Hewagama M, Priyangika WD, Konradsen F, Eddleston M. The impact of pesticide regulations on suicide in Sri Lanka. Int J Epidemiol. 2007;36(6):1235–1242. doi: 10.1093/ije/dym164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eddleston M, Gunnell D. Why suicide rates are high in China. Science. 2006;311(5768):1711–1713. doi: 10.1126/science.311.5768.1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides: a continuing tragedy in developing countries. Int J Epidemiol. 2003;32(6):902–909. doi: 10.1093/ije/dyg307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.International Classification of Diseases, Ninth Revision, Clinical Modification. Hyattsville, MD: National Center for Health Statistics; 1980. DHHS publication PHS 80–1260. [Google Scholar]
- 37.International Classification of Diseases, 10th Revision. Geneva, Switzerland: World Health Organization; 1992 [Google Scholar]
- 38.Kelly PJ, Lim LL. Survival analysis for recurrent event data: an application to childhood infectious diseases. Stat Med. 2000;19(1):13–33. doi: 10.1002/(sici)1097-0258(20000115)19:1<13::aid-sim279>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 39.Haw C, Hawton K, Houston K, Townsend E. Correlates of relative lethality and suicidal intent among deliberate self-harm patients. Suicide Life Threat Behav. 2003;33(4):353–364. doi: 10.1521/suli.33.4.353.25232. [DOI] [PubMed] [Google Scholar]
- 40.Christiansen E, Jensen BF. Risk of repetition of suicide attempt, suicide or all deaths after an episode of attempted suicide: a register-based survival analysis. Aust N Z J Psychiatry. 2007;41(3):257–265. doi: 10.1080/00048670601172749. [DOI] [PubMed] [Google Scholar]
- 41.Bennewith O, Gunnell D, Kapur N et al. Suicide by hanging: multicentre study based on coroners’ records in England. Br J Psychiatry. 2005;186:260–261. doi: 10.1192/bjp.186.3.260. [DOI] [PubMed] [Google Scholar]
- 42.Kapur N, Murphy E, Cooper J et al. Psychosocial assessment following self-harm: results from the multi-centre monitoring of self-harm project. J Affect Disord. 2008;106(3):285–293. doi: 10.1016/j.jad.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 43.Lilley R, Owens D, Horrocks J et al. Hospital care and repetition following self-harm: multicentre comparison of self-poisoning and self-injury. Br J Psychiatry. 2008;192(6):440–445. doi: 10.1192/bjp.bp.107.043380. [DOI] [PubMed] [Google Scholar]
- 44.Hawton K, Bergen H, Mahadevan S, Casey D, Simkin S. Suicide and deliberate self-harm in Oxford University students over a 30-year period. Soc Psychiatry Psychiatr Epidemiol. 2012;47(1):43–51. doi: 10.1007/s00127-010-0310-3. [DOI] [PubMed] [Google Scholar]
- 45.Pokorny AD, Kaplan HB. Suicide following psychiatric hospitalization. J Nerv Ment Dis. 1976;162(2):119–125. doi: 10.1097/00005053-197602000-00006. [DOI] [PubMed] [Google Scholar]
- 46.Suominen K, Isometsa E, Suokas J, Haukka J, Achte K, Lonnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. 2004;161(3):562–563. doi: 10.1176/appi.ajp.161.3.562. [DOI] [PubMed] [Google Scholar]
- 47. Injury prevention and control: data and statistics (WISQARS). Centers for Disease Control and Prevention. 2005. Available at: http://www.cdc.gov/ncipc/wisqars. Accessed December 31, 2012.