Abstract
Objectives. We examined whether urban patients who suffered gunshot wounds (GSWs) farther from a trauma center would have longer transport times and higher mortality.
Methods. We used the Illinois State Trauma Registry (1999–2009). Scene address data for Chicago-area GSWs was geocoded to calculate distance to the nearest trauma center and compare prehospital transport times. We used multivariate regression to calculate the effect on mortality of being shot more than 5 miles from a trauma center.
Results. Of 11 744 GSW patients during the study period, 4782 were shot more than 5 miles from a trauma center. Mean transport time and unadjusted mortality were higher for these patients (P < .001 for both). In a multivariate model, suffering a GSW more than 5 miles from a trauma center was associated with an increased risk of death (odds ratio = 1.23; 95% confidence interval = 1.02, 1.47; P = .03).
Conclusions. Relative “trauma deserts” with decreased access to immediate care were found in certain areas of Chicago and adversely affected mortality from GSWs. These results may inform decisions about trauma systems planning and funding.
Traumatic injury is the leading cause of death in the United States among individuals aged 1 to 44 years.1 Trauma centers are specialized facilities within hospitals with the expertise to care for the injured patient; resources include trauma surgeons, interventional radiology, surgical subspecialists, and immediate availability of an operating room. The development of trauma centers and trauma systems grew out of wartime experiences from the 1950s through 1970s that increasingly emphasized early and aggressive care and treatment of injured combatants. Trauma centers and organized trauma systems, including prehospital triage criteria and transport plans, have been shown to significantly decrease mortality for injured patients.2,3
However, not all areas of the country have equal access to trauma centers. Although 84% of Americans live within 1 hour of a trauma center, rural areas are particularly underserved.4,5 Longer prehospital transport times likely contribute to the higher mortality rates among rural trauma patients as compared with similarly injured urban patients.6–8 For urban trauma patients, the relationship between transport times and outcomes is inconclusive. Feero et al. examined more than 800 urban trauma patients and found that shorter transport times were associated with improved survival.9 Gervin and Fischer also found this association for patients with penetrating cardiac injuries.10 Several other investigators, however, have not found a link between transport times and survival from trauma.11–13 The largest and most recent of these studies was from Newgard et al.,13 who used data from 10 cities and 51 trauma centers. The centers included a heterogeneous mix of urban and rural hospitals from the United States and Canada. They found that prehospital transport time was not associated with increased mortality for major trauma. The disparate results from these studies may be in part attributable to the heterogeneity of injury mechanisms in the patient populations12 or smaller sample sizes underpowered to detect the effects of transport times.11 The Newgard study did separately analyze patients injured by penetrating trauma (i.e., gunshot wounds [GSWs] or stab wounds), but nearly two thirds of those patients and 67% of GSW victims were within the first or second quartile of prehospital transport times (i.e., the shortest transport times). These patients also constituted only 22% of the sample size. Both of these facts may limit the generalizability of this study to areas of the country with higher rates of penetrating trauma.
The city of Chicago currently has 7 Illinois-verified level I adult trauma centers in and around the city, and a mature emergency medical services (EMS) system providing care to a population of 3 million people. There are no level II centers within the city limits. (Level I and level II centers both provide 24-hour comprehensive trauma services, including trauma surgeons, radiology, and EMS; however, level II facilities do not need to have a surgical residency or ongoing research programs.) Unfortunately, Chicago also has one of the highest homicide rates in the country, ranging from 450 to 650 deaths per year from 1999 to 2009 (averaging 16 per 100 000 annually), mostly attributable to firearm-related violence14 (Figure A; available as a supplement to the online version of this article at http://www.ajph.org). As in most major cities, socioeconomically distressed neighborhoods in Chicago suffer most of the burden of firearm-related homicide; these neighborhoods, as well as the 7 trauma centers, are not evenly distributed around the city (Figure B; available as a supplement to the online version of this article at http://www.ajph.org).
Urgent surgical intervention is much more frequently required for penetrating trauma than for blunt mechanisms of injury, and it is less likely that definitive care can be provided in the prehospital setting. As trauma centers are not equally distributed around the city, we hypothesized that patients who suffer GSWs in areas that are farther from trauma centers will have longer transport times and worse outcomes.
METHODS
Our data source was the Illinois State Trauma Registry (ISTR), a mandatory reporting database containing information about all traumas presenting to level I and level II centers in the state. This database is maintained by the Illinois Department of Public Health; it is de-identified with respect to name and hospital, but includes other demographic information, such as gender, age, race, physiological data, mortality and discharge outcomes, and incident address information.
Patient Population
We extracted data from all patients for the years 1999 through 2009 from the registry (n = 510 429). The data set was restricted to Chicago by zip code and city. We also included in the data set a 1-mile perimeter around the city to incorporate spatial effects beyond the city’s administrative demarcation, given that trauma center catchment areas include neighboring communities but do not necessarily adhere to published neighborhood or city boundaries (n = 119 349). We further limited the data set to GSWs (n = 12 475) by using the External Causes of Injury codes from the International Classification of Diseases, Ninth Revision15 (e-codes 922.0–922.9, 955.0–955.7, 965.0–965.4, 968.6, 985.0–985.7, 970, and 979.4). The longitudinal trend of GSW incidence in our data set paralleled homicide data publicly available from the city of Chicago (Figure C; available as a supplement to the online version of this article at http://www.ajph.org).
We mapped all incidents with available address data for the scene of the incident using ArcGIS software (Esri, Redlands, CA); more than 94% could be geocoded (n = 11 744). We then created maps of GSW incidence and superimposed them with a map of Chicago-area trauma centers. We calculated distance measurements as the Euclidean distance between the GSW incident and the nearest level I trauma center.
Predictors
We created a variable to denote being more than vs less than or equal to 5 miles from a trauma center. We selected 5 miles from 1-mile increments of distance between 1 and 10 miles because it provided the best balance of minimizing geographic overlap of trauma center radii but allowed for sufficient comparison proportions. The approximately two thirds of patients in the data set who were within this 5-mile boundary served as observational controls (Table A; available as a supplement to the online version of this article at http://www.ajph.org). We also analyzed important potential confounders, including age, gender, race, insurance status, injury severity score (ISS) greater than 16 (which is associated with higher likelihood of mortality), systolic blood pressure (SBP) in the emergency department of less than 90 millimeters of mercury, year of injury, and intent of injury. We coded insurance status as those self-paying being “uninsured” and everyone else being “insured.” We determined injury intent and whether the police were involved by E-codes. Older age,16 male gender,17 non-White race,18 lack of insurance,18 and injury severity as measured by ISS and blood pressure have all been shown to predict mortality after trauma.19 Insurance status is difficult to code because there is a wide spectrum between insured and uninsured, with many underinsured individuals in between. However, we have adopted a dichotomization that is consistent with current work in the trauma disparities literature.18,20,21
With respect to injury markers, there are many other methods to calculate injury severity (such as the Revised Trauma Score and the Trauma and Injury Severity Score), all of which have incrementally better performance than the ISS alone on mortality prediction and include anatomical and physiological markers of injury, along with demographic criteria. However, these are calculated values, some requiring use of a regression model, and they are not routinely included in all trauma data sets, including the ISTR.
We included year of injury to account for any longitudinal improvements or other changes in trauma care or systems. We included intent because firearm suicide attempts have been found to be highly lethal (over 90% fatal),22 but firearm-related assaults seem to be less so, judging from the nonfatal firearm assault rate in the United States.
Outcomes
Outcomes of interest were mean transport times and mortality. Transport time is divided into 3 components in the ISTR: response time, scene time (i.e., time spent by EMS personnel at the scene), and travel time from the scene to the hospital. These are all actual times recorded by the EMS providers and verified in the medical record by trauma registrars. Of the 3 components, we used travel time from the scene for our analysis because it should be the most directly correlated with distance from the scene to the closest trauma center. Response times vary irrespective of distance from the scene, because EMS personnel may or may not be in the area at any given time; although they are not all dispatched from a central location, response times are typically very brief. For this sample, 97% of response times were 10 minutes or less. Scene times for penetrating trauma are highly dependent on the ability of police to secure the scene and EMS personnel to safely evacuate the patient, and are therefore not readily modifiable. Because a scene time of more than 20 minutes is a quality indicator of the American College of Surgeons Committee on Trauma, we examined this for our sample, and 95% of scene times were 20 minutes or less. Because geographic boundaries such as the Chicago River, road construction, bridges, and traffic patterns might influence transport times, we first calculated the association between transport time and distance from a trauma center.
Mortality was defined as all patients who died in the hospital, excluding those “dead on arrival” (DOAs; i.e., individuals who were pronounced dead in the emergency department without any interventions). These latter patients were excluded because we posited that they would have a lower probability of survival due to greater injury burden and that injury severity would overwhelm any smaller effect of transport times. In addition, prehospital data (e.g., vital signs and injury severity) were largely incomplete for these patients, with some data collection points having greater than 70% missing values. In addition, prehospital decision-making with respect to transporting patients in extremis may also be dependent on distance from a trauma center, introducing bias into the study.
Statistical Analysis
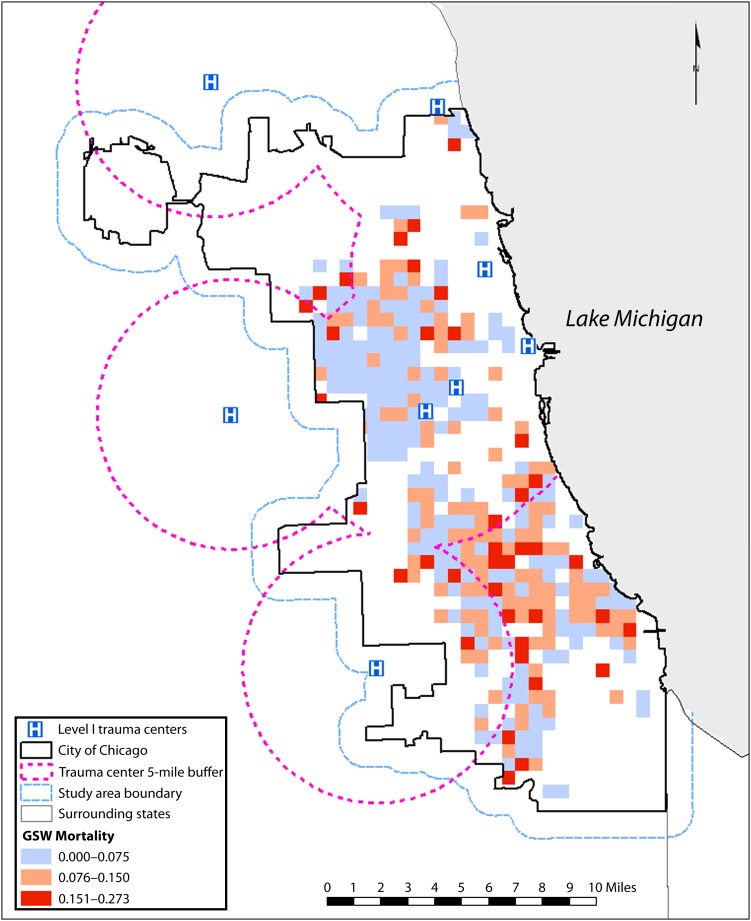
We calculated bivariate and multivariate analyses using Stata statistical software version 10 (StataCorp LP, College Station, TX). We estimated logistic regression models of mortality. Covariates included age, gender, race, insurance status, ISS greater than 16, SBP in the emergency department of less than 90 millimeters of mercury, year of injury, mechanism and intent of injury, and our variable of interest, being shot more than 5 miles from a trauma center. Using ArcGIS software, we then created maps of GSW mortality rates and superimposed them with a map of area trauma centers. The method used to depict mortality rates in the city was a quadrat grid of half-mile by half-mile cells symbolizing the mortality rate for GSW patients in each quadrat that contained 10 or more GSWs. We used this approach to limit small sample size or land use effects (because industrial areas have few GSWs) to optimize mortality rate mapping.
RESULTS
Of the 11 744 GSW victims in the data set, the overwhelming majority were male (91.6%), younger than 40 (98.4%), non-White (89.9%), and victims of assault (89.9%; P < .001 for all). A total of 4782 patients (38.3%) were shot more than 5 miles from a trauma center (Table 1).
TABLE 1—
Patient Demographics and Mortality From Gunshot Wounds: Chicago, IL, 1999–2009
| Variable | GSW Frequency, No. (%) or Mean ±SD | GSW Mortality, No. (%) or Mean ±SD |
| Total | 11 744 | 2204 (18.8) |
| Race/ethnicity | ||
| White, non-Hispanic | 495 (4.2) | 125 (25.3) |
| Black, non-Hispanic | 8027 (68.3) | 1489 (18.5) |
| Hispanic | 2529 (21.6) | 452 (17.9) |
| Other or unknown | 693 (5.9) | 138 (19.9) |
| Gender | ||
| Female | 988 (8.4) | 165 (16.7) |
| Male | 10 754 (91.6) | 2037 (18.9) |
| Age, y | ||
| Birth–9 | 109 (0.9) | 26 (23.9) |
| 10–19 | 3389 (28.9) | 515 (15.2) |
| 20–29 | 5274 (44.9) | 1025 (19.4) |
| 30–39 | 1815 (15.5) | 369 (20.3) |
| 40–49 | 750 (6.4) | 157 (20.9) |
| 50–59 | 260 (2.2) | 62 (23.8) |
| 60–69 | 89 (0.8) | 20 (22.5) |
| ≥ 70 | 58 (0.5) | 30 (51.7) |
| Insurance coverage | ||
| Insured | 5488 (47.4) | 704 (12.8) |
| Not insured | 6086 (52.6) | 1464 (24.0) |
| Incident within 5 miles of trauma center | ||
| Yes | 7736 (65.9) | 1430 (18.5) |
| No | 4008 (34.1) | 774 (19.3) |
| Intent | ||
| Unintentional | 695 (5.9) | 82 (3.7) |
| Suicide | 157 (1.3) | 107 (4.9) |
| Assault | 10 558 (89.9) | 1920 (87.1) |
| Legal intervention | 85 (0.7) | 17 (7.7) |
| Undetermined | 249 (2.1) | 78 (3.5) |
| ISSa | 10.9 ±12.8 | 22.3 ±14.9 |
| SBP, mm Hg | 117.6 ±50.5 | 82.0 ±64.2 |
Note. GSW = gunshot wound; ISS = injury severity score; SBP = systolic blood pressure. GSW mortality is a subset of GSW frequency. Column totals should approach 100% for each variable within each column. The totals may not add to 100% because of a small amount of missing data.
An ISS > 16 is associated with higher likelihood of mortality.
Overall mortality was 18.8%, with 64% of those deaths coded as DOA or dead in the emergency department without interventions provided. Among patients who were not DOA, mortality was very high for White patients, who tended to be older (≥ 50 years; 15% of White patients vs 3% of the cohort overall; P < .001) and more frequently had a suicidal intent (9% vs 3%; P < .001). Firearm-related suicide attempts were highly lethal; of patients surviving to the hospital, 68% ultimately died. The patients who were DOA had a much higher mean ISS (18.62 ±18.80 vs 9.89 ±10.45 for other deaths) and much lower mean SBP (28.49 ±54.39 vs 129.47 ±36.90; P < .001 for each).
Transport Times
The mean transport time was significantly higher for patients who were shot more than 5 miles away from a trauma center (16.6 ±7.6 minutes vs 10.3 ±6.5 minutes; P < .001).
Patients shot more than 5 miles away from a trauma center were disproportionately Black (P < .001), were less likely to be insured (P < .001), had a slightly higher ISS (10.4 vs 9.3; P < .001), were more likely to have suffered a primary abdominal wound (13% vs 8%; P < .001), and were more frequently the victim of an assault (P < .001; Table 2).
TABLE 2—
Demographics of Gunshot Wound Patients, by Distance From a Trauma Center: Chicago, IL, 1999–2009
| Variable | Distance ≤ 5 Miles | Distance > 5 Miles | P |
| Total, no. | 6786 | 3543 | |
| Unadjusted mortality | 0.070 | 0.087 | .002a |
| Race/ethnicity, no. | .001b | ||
| White, non-Hispanic | 343 | 86 | |
| Black, non-Hispanic | 4048 | 3013 | |
| Hispanic | 1959 | 279 | |
| Other or unknown | 433 | 165 | |
| Gender, no. (%) | .288b | ||
| Female | 589 (9) | 286 (8) | |
| Male | 6192 (91) | 3257 (92) | |
| Age, y, no. (%) | .029b | ||
| Birth–19 | 2142 (32) | 1027 (29) | |
| 20–39 | 3993 (59) | 2182 (62) | |
| 40–59 | 575 (8) | 289 (8) | |
| ≥ 60 | 73 (1) | 45 (1) | |
| Insurance coverage, no. (%) | .001b | ||
| Insured | 3541 (53) | 1515 (43) | |
| Not insured | 3145 (47) | 1977 (57) | |
| Abbreviated Injury Scale,c no. (%) | .001b | ||
| Head | 486 (13) | 185 (11) | |
| Neck | 79 (2) | 42 (2) | |
| Chest | 621 (16) | 289 (16) | |
| Abdomen | 290 (8) | 222 (13) | |
| Other | 2816 (62) | 1257 (58) | |
| Intent, no. (%) | .001b | ||
| Unintentional | 515 (8) | 124 (3) | |
| Suicide | 62 (1) | 42 (1) | |
| Assault | 6006 (89) | 3316 (94) | |
| Undetermined | 159 (2) | 28 (1) | |
| Legal Intervention | 41 (1) | 33 (1) | |
| SBP, mm Hg, mean | |||
| Overall | 130.7 | 131.1 | .494a |
| Among patients who died | 83.5 | 79.8 | .449 |
| ISS,d mean | |||
| Overall | 9.3 | 10.4 | .001a |
| Among patients who died | 22.7 | 21.6 | .335 |
Note. ISS = injury severity score; SBP = systolic blood pressure. The totals may not add to 100% because of a small amount of missing data.
P value determined by the t-test.
P value determined by the χ2 test.
Based on data from 1999 to 2003; no data from 2004 to 2009 were available.
An ISS > 16 is associated with higher likelihood of mortality.
Mean transport times did not vary significantly by time of day, day of week, or month of year (P > .05 for all). Transport times were directly proportional to distance from a trauma center. Linear regression modeling of transport time and distance found that each additional mile increased transport time by 1.5 minutes (95% confidence interval [CI] = 1.46, 1.56; P < .001; R 2 = 0.27).
Mortality
The strongest predictors of mortality were the 2 injury severity markers (SBP and ISS) and suicidal intent (Table 3). Lack of insurance was also associated with a higher mortality. Being Black was associated with lower mortality in this group. Being White and having a suicidal intent markedly increased the mortality risk. There was high correlation between these 2 variables, and injury severity was much worse for the group of White GSW patients with suicidal intent, which likely explains the association of increased mortality among Whites in our sample.
TABLE 3—
Adjusted Odds of Mortality From Gunshot Wounds: Chicago, IL, 1999–2009
| Variable | OR (95% CI) | P |
| Male | 1.1 (0.77, 1.55) | .61 |
| Black | 0.65 (0.44, 0.96) | .03 |
| Hispanic | 0.85 (0.56, 1.31) | .47 |
| Age > 55 y | 1.14 (0.58, 2.23) | .7 |
| Lack of insurance | 2.27 (1.86, 2.77) | < .001 |
| ED SBP < 90 | 16.93 (13.72, 20.91) | < .001 |
| ISS > 16a | 8.06 (6.72, 9.66) | < .001 |
| Trauma center > 5 miles away | 1.23 (1.02, 1.47) | .03 |
| Suicidal intent | 8.76 (5.04, 15.24) | < .001 |
| Suicidal intent and White | 16.06 (6.52, 39.54) | < .001 |
Note. CI = confidence interval; ED = emergency department; ISS = injury severity score; OR = odds ratio; SBP = systolic blood pressure.
An ISS > 16 is associated with higher likelihood of mortality.
Unadjusted mortality was higher for patients who were shot farther than 5 miles from the nearest trauma center (8.7% vs 7%; P < .001). In a multivariate model adjusting for injury severity, age, race, gender, insurance status, and intent of GSW, being shot more than 5 miles from a trauma center was independently associated with increased risk of mortality (odds ratio [OR] = 1.23; 95% CI = 1.02, 1.47; P = .03). To validate our model, we performed 3 additional analyses. We first compared our model using a 5-mile distance from a trauma center with a model that dichotomized patients using a 4-mile distance (46% of patients), which yielded similar results (OR = 1.19; 95% CI = 1.03, 1.27; P = .04). As a sensitivity analysis, we created a second regression model using SBP at the scene vs emergency department SBP. The results were the same, but there were fewer missing values for emergency department SBP, so the latter results are reported here. Third, distance from a trauma center was independently associated with increased mortality among GSW victims, irrespective of intent. Regression modeling that limited the sample to assaults demonstrated identical results. However, regression models for suicidal intent alone had insufficient power to determine associations between transport times and outcomes. Finally, we constructed a correlation matrix, which did not demonstrate severe multicollinearity.
A GSW mortality map demonstrated higher mortality rates for individuals living outside the 5-mile boundary, despite reasonable proximity to main roadways and freeways (Figure 1).
FIGURE 1—
Density map of gunshot wound (GSW) mortality and distance from a trauma center: Chicago, IL, 1999–2009.
Source. Illinois State Trauma Registry.
DISCUSSION
These data demonstrate an association between being shot more than 5 miles from a trauma center, longer prehospital transport times, and mortality from gunshot wounds from 1999 to 2009. Most of Chicago’s gun violence occurs on its south and west sides. There are a number of trauma centers located on the west side of the city. On the south side, however, particularly the southeast side, there is no nearby trauma center to serve this high-risk population. This same population with no local access to a level 1 trauma care has a higher mortality rate from GSWs. The high-profile death of a young activist on the southeast side has created tremendous interest in this issue among community activists and the media.23–25
However, solutions are neither simple nor easy. Creation, certification, and maintenance of a trauma center in these relative “trauma deserts” could be very expensive and resource-consuming, though potentially cost-effective.26 Another solution would be to facilitate existing local hospitals within these deserts to care for trauma patients, possibly in a level II capacity, akin to similar fresh produce initiatives in “food deserts” in the city.27 This is a possibility because there are at least 4 hospitals in this particular area that are not trauma centers but have surgical and emergency department facilities. Lastly, trauma centers could be rebalanced on the basis of volume and proximity as opposed to capacity, including perhaps reallocating resources or forging new partnerships between academic and community centers. However, any changes to the existing system would need to be studied prospectively because a positive impact is not guaranteed. For example, some researchers have found risk-adjusted mortality to be higher at level II centers than at level I centers, although these studies were not restricted to penetrating trauma.28,29
This study is not without limitations. Although there was an association between distance from a trauma center and mortality, we found that injury severity, lack of insurance, and suicidal intent were much stronger predictors of mortality. Modifications of trauma systems cannot address any of these issues. In addition, given that suicidal intent predicted higher mortality, but represented a small subset of our data and has very different prevention and public health implications, it might have been reasonable to exclude these patients from the analysis. However, we felt that they added value by encompassing a real-world spectrum of GSWs in which intent may not be immediately known.
Second, we excluded DOAs from the analysis; better information about these cases might have been useful. This remains a tremendous challenge in prehospital trauma research; the patients that are in extremis require intense resources, and data collection is often less rigorous, as was the case in this data set.
Third, we used a distance of 5 miles from a trauma center to compare outcomes, but this number was somewhat arbitrary given the lack of work regarding optimal trauma center proximity. However, for our particular sample, this distance yielded the optimal balance between comparison groups, and a separate model comparing patients that used a 4-mile radius did not elicit significantly different results. Fourth, systemic differences in prehospital interventions or trauma center care may partly explain mortality differences by proximity to a trauma center, but these have not been found in rigorous programmatic evaluations performed by state and local agencies. It is also possible that an as-yet-unidentified confounder exists that is correlated with both transport time and mortality that could explain these associations. Fifth, because of changes in data collection and reporting, and the problems associated with missing data in an administrative database, we were unable to completely control for anatomical location of injuries, which might have an independent effect on mortality, although overall injury severity and physiological measures of injury were taken into account.
The final question is one of generalizability. Chicago is unique in the comprehensiveness and maturity of its trauma system and the prevalence of penetrating trauma; results from this study may not be applicable to other communities. However, potential solutions to this problem could have national and global relevance. For example, designation of a new level II trauma center was employed in south Los Angeles, California, to help decrease the impact of closure of a busy level I center in 2004. Expanding the capacitance of local hospitals to act as trauma service providers may improve outcomes in Chicago, or it may be applicable to other communities with long travel distances to trauma centers or a heavy burden of penetrating trauma. As a second example, for states or communities that are beginning to implement trauma systems, such as Indiana, these data may help inform planning and infrastructure building, particularly in areas such as Gary or Hammond, which are demographically similar to Chicago.
Despite these limitations, to our knowledge this is the largest study to date looking specifically at the impact of distance from a trauma center and mortality from GSWs in a particular geographic area. To determine the effect of these results within a real-world context, an attributable risk analysis can easily be calculated for GSW patients. For example, the crude mortality for Blacks shot within 5 miles of a trauma center is 6.42%, whereas outside of 5 miles it is 8.73%; the overall mortality is 7.41%, so the percent attributable risk is 26.05%. This would translate to 6.3 excess deaths per year for this community, and, assuming a per-patient loss of 40 quality-adjusted life years, a total of approximately 240 quality-adjusted life years. Assuming a cost-effectiveness threshold of $100 000 per quality-adjusted life year, the sum is $24 million per year, far higher than the typical annual costs of maintaining a trauma center.30 It is unclear whether these data will affect policy or funding decisions, but they should certainly be used to inform discussions. In addition, future work should evaluate the effects of distance from a trauma center on other outcomes, such as hospital length of stay, permanent disability, and quality of life.
Gun violence remains endemic to Chicago, and GSWs account for the overwhelming majority of homicides within the city. We have demonstrated that incident proximity to a trauma center has a positive effect on survival outcomes for GSW victims. We have identified the southeast side of the city as a relative trauma desert in Chicago’s regional trauma system that is associated with increased GSW mortality. We hope that the data presented will inform discussions aimed at optimizing regional trauma care in Chicago and will also aid in planning regional trauma systems in other urban settings.
Acknowledgments
This study was funded in part through career development grants from the American College of Surgeons and the Robert Wood Johnson Foundation Physician Faculty Scholars Program. Data were provided by the Illinois Department of Public Health, Division of Emergency Medical Systems and Highway Safety.
Human Participant Protection
Institutional review board approval was obtained from Northwestern University and the Illinois Department of Public Health.
References
- 1.Centers for Disease Control and Prevention Scientific data, surveillance, and injury statistics. 2011. Available at: http://www.cdc.gov/injury/wisqars. Accessed December 1, 2012
- 2.Nathens AB, Jurkovich GJ, Cummings P, Rivara FP, Maier RV. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000;283(15):1990–1994 [DOI] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Rivara FP, Jurkovich GJet al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366–378 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Access to trauma care: getting the right care at the right place at the right time. January 2012. Available at: http://www.cdc.gov/traumacare/access_trauma.html. Accessed December 1, 2012 [Google Scholar]
- 5.Branas CC, MacKenzie EJ, Williams JCet al. Access to trauma centers in the United States. JAMA. 2005;293(21):2626–2633 [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez RP, Cummings G, Mulekar M, Rodning C. Increased mortality in rural vehicular trauma: identifying contributing factors through data linkage. J Trauma. 2006;61(2):404–409 [DOI] [PubMed] [Google Scholar]
- 7.Grossman DC, Kim A, Macdonald S, Klein P, Copass MK, Maier RV. Urban–rural differences in prehospital care of major trauma. J Trauma. 1997;42(4):723–729 [DOI] [PubMed] [Google Scholar]
- 8.Esposito TJ, Maier RV, Rivara FPet al. The impact of variation in trauma care times: urban versus rural. Prehosp Disaster Med. 1995;10(3):161–166, discussion 166–167 [DOI] [PubMed] [Google Scholar]
- 9.Feero S, Hedges JR, Simmons E, Irwin L. Does out-of-hospital EMS time affect trauma survival? Am J Emerg Med. 1995;13(2):133–135 [DOI] [PubMed] [Google Scholar]
- 10.Gervin AS, Fischer RP. The importance of prompt transport of salvage of patients with penetrating heart wounds. J Trauma. 1982;22(6):443–448 [DOI] [PubMed] [Google Scholar]
- 11.Pepe PE, Wyatt CH, Bickell WH, Bailey ML, Mattox KL. The relationship between total prehospital time and outcome in hypotensive victims of penetrating injuries. Ann Emerg Med. 1987;16(3):293–297 [DOI] [PubMed] [Google Scholar]
- 12.Petri RW, Dyer A, Lumpkin J. The effect of prehospital transport time on the mortality from traumatic injury. Prehosp Disaster Med. 1995;10(1):24–29 [DOI] [PubMed] [Google Scholar]
- 13.Newgard CD, Schmicker RH, Hedges JRet al. Emergency medical services intervals and survival in trauma: assessment of the “golden hour” in a North American prospective cohort. Ann Emerg Med. 2010;55(3):235–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.CLEARpath Crime summary. 2012. Available at: https://portal.chicagopolice.org/portal/page/portal/ClearPath. Accessed December 1, 2012 [Google Scholar]
- 15.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 16.Tornetta P, 3rd, Mostafavi H, Riina Jet al. Morbidity and mortality in elderly trauma patients. J Trauma. 1999;46(4):702–706 [DOI] [PubMed] [Google Scholar]
- 17.Haider AH, Crompton JG, Chang DCet al. Evidence of hormonal basis for improved survival among females with trauma-associated shock: an analysis of the National Trauma Data Bank. J Trauma. 2010;69(3):537–540 [DOI] [PubMed] [Google Scholar]
- 18.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE., 3rd Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945–949 [DOI] [PubMed] [Google Scholar]
- 19.Nakahara S, Yokota J. Revision of the International Classification of Diseases to include standardized descriptions of multiple injuries and injury severity. Bull World Health Organ. 2011;89(3):238–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maybury RS, Bolorunduro OB, Villegas Cet al. Pedestrians struck by motor vehicles further worsen race- and insurance-based disparities in trauma outcomes: the case for inner-city pedestrian injury prevention programs. Surgery. 2010;148(2):202–208 [DOI] [PubMed] [Google Scholar]
- 21.Salim A, Ottochian M, DuBose Jet al. Does insurance status matter at a public, level I trauma center? J Trauma. 2010;68(1):211–216 [DOI] [PubMed] [Google Scholar]
- 22.Rhyne CE, Templer DI, Brown LG, Peters NB. Dimensions of suicide: perceptions of lethality, time, and agony. Suicide Life Threat Behav. 1995;25(3):373–380 [PubMed] [Google Scholar]
- 23.In memoriam: Damian Turner. 2010. Available at: http://www.areachicago.org/p/issues/institutions-and-infrastructures/damian-turner. Accessed December 1, 2012 [Google Scholar]
- 24.Chicago Now 20th Ward aldermanic candidate Rev. Andre Smith demands Damian Turner’s killers to surrender. August 17, 2010. Available at: http://www.chicagonow.com/and-the-ordinary-people-said/2010/08/20th-ward-aldermanic-candidate-rev-andre-smith-demands-damian-turners-killers-to-surrender. Accessed December 1, 2012 [Google Scholar]
- 25.Health Care Now Activists call for trauma care from University of Chicago Medical Center. August 22, 2011. Available at: http://www.healthcare-now.org/activists-call-for-trauma-care-from-the-university-of-chicago-medical-center. Accessed December 1, 2012 [Google Scholar]
- 26.MacKenzie EJ, Weir S, Rivara FPet al. The value of trauma center care. J Trauma. 2010;69(1):1–10 [DOI] [PubMed] [Google Scholar]
- 27.Healthy Places Food. 2012. Available at: http://www.healthyplaceschicago.org/food/index.lasso. Accessed December 1, 2012 [Google Scholar]
- 28.Cudnik MT, Newgard CD, Sayre MR, Steinberg SM. Level I versus level II trauma centers: an outcomes-based assessment. J Trauma. 2009;66(5):1321–1326 [DOI] [PubMed] [Google Scholar]
- 29.Demetriades D, Martin M, Salim A, Rhee P, Brown C, Chan L. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg. 2005;242(4):512–517, discussion 517–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rotondo MF, Bard MR, Sagraves SGet al. What proce commitment: what benefit? The cost of a saved life in a developing level I trauma center. J Trauma. 2009;67(5):915–923 [DOI] [PubMed] [Google Scholar]