Abstract
Objectives. We evaluated Legacy for Children, a public health strategy to improve child health and development among low-income families.
Methods. Mothers were recruited prenatally or at the birth of a child to participate in Legacy parenting groups for 3 to 5 years. A set of 2 randomized trials in Miami, Florida, and Los Angeles, California, between 2001 and 2009 assessed 574 mother-child pairs when the children were 6, 12, 24, 36, 48, and 60 months old. Intent-to-treat analyses from 12 to 60 months compared groups on child behavioral and socioemotional outcomes.
Results. Children of mothers in the intervention group were at lower risk for behavioral concerns at 24 months and socioemotional problems at 48 months in Miami, and lower risk for hyperactive behavior at 60 months in Los Angeles. Longitudinal analyses indicated that children of intervention mothers in Miami were at lower risk for behavior problems from 24 to 60 months of age.
Conclusions. Randomized controlled trials documented effectiveness of the Legacy model over time while allowing for implementation adaptations by 2 different sites. Broadly disseminable, parent-focused prevention models such as Legacy have potential for public health impact. These investments in prevention might reduce the need for later intervention strategies.
More than 15 million children were living below the Federal poverty line in 2009.1 These children are at increased risk for poor health and developmental outcomes concurrently, including lower vaccination rates,2 higher rates of severe chronic disease3 and conditions that require medical attention,4 and more cognitive and behavioral difficulties.5–12 Poverty-associated stress in childhood also contributes to dysregulated cardiovascular stress responses,13 which have been implicated in depressed immune function and the etiology of chronic diseases.14,15 A 2002 review16 concluded that lower socioeconomic status is reliably associated with rates of childhood injury, high blood pressure, respiratory illnesses, and active smoking. Poverty thus represents a significant risk factor for children’s health.
Socioeconomic disparities in childhood health persist and magnify as the child develops.17,18 Adolescents and adults with low socioeconomic childhoods are at greater risk for obesity19 and heart disease,20,21 have poorer dental health,22 engage in more risk behaviors, and have lower academic performance.23 As adults, they earn less than half as much and receive $826 per year more in food stamps than peers from more advantaged backgrounds.24 In addition, poverty’s adverse effects can be perpetuated through intergenerational transmission.25–28 This association between early socioeconomic disadvantage and long-term health makes childhood poverty a public health issue.
Parents of infants and young children control much of their children’s proximal environment, including providing and modeling safe, stable, nurturing relationships, facilitating cognitively stimulating activities, using effective discipline strategies, offering nutritious foods, reinforcing and sharing healthy habits, accessing health care, and selecting playmates and other caregivers. Poverty is reliably associated with decrements in parents’ ability to provide such health- and development-promoting environments. Documented pathways of this effect include higher levels of neighborhood chaos and violence,8,29,30 lower community social capital,8,31 higher exposure to pollutants and toxins,32 greater material hardship (e.g., food insecurity, inadequacy of medical care),33 and challenges to caregiver mental health.34 However, some parents exhibit healthy parenting despite these strong countervailing forces,35 and positive parenting behaviors serve as protective factors for children in low-income families and neighborhoods.36–41 Interventions to increase the number of parents who provide nurturing environments in socioeconomically disadvantaged circumstances could improve children’s short- and long-term health and development by placing vulnerable children on more optimal life-course trajectories. To produce the best return on investment, such strategies to promote human development are better targeted earlier, rather than later, in childhood.18
Between 1994 and 1998, the Centers for Disease Control and Prevention (CDC), noting the growing evidence on poverty-associated differences in children’s cognitive and developmental outcomes, convened meetings with experts and other federal agencies to identify potentially effective public health strategies for intervening with vulnerable children and families. Prevailing evidence-based models at the time included providing high-quality, center-based educational experiences directly to preschoolers,42–44 home visits to vulnerable mothers and infants,45 a combination of home visiting and educational intervention,46,47 and behavioral parent training to families with preschoolers at risk for or already evidencing problem behaviors.48–51 The CDC sought to maximize the potential impact with this population by developing a primary prevention program for low-income parents of infants and young children, using group-based implementation in community settings to foster widespread dissemination and sustainability.
Legacy for Children (Legacy) was designed to support mothers’ ability to engage in positive parenting behaviors and positive mother-child interactions by improving parenting efficacy and mothers’ sense of supportive community. A complete description of the study design and intervention has been provided elsewhere.52 Legacy is being evaluated via a set of 2 randomized controlled trials (NCT00164697) investigating the impact on children’s behavioral, socioemotional, cognitive, and language outcomes. This report contains the first results of the Legacy outcome evaluation, focusing on children’s behavioral and socioemotional outcomes, which are well-documented early predictors of long-term health.53–58
METHODS
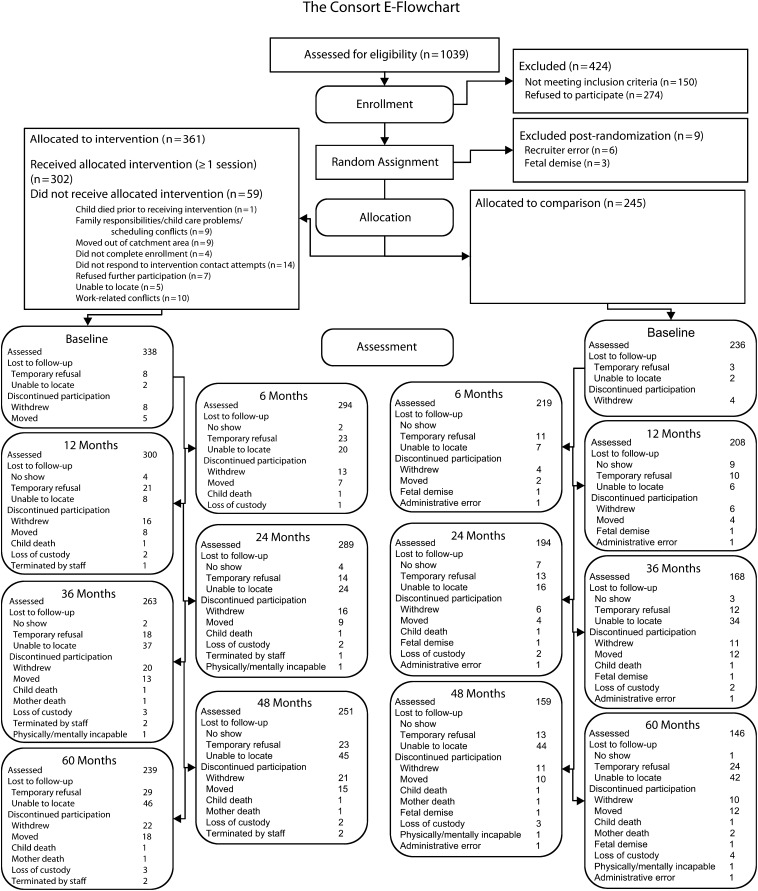
Data are from the 574 mother-child dyads who participated in the 2 sites of the Legacy trial between 2001 and 2009: 1 at the University of California at Los Angeles (UCLA) and 1 at the University of Miami, Florida. Figure 1 shows the CONSORT (CONsolidated Standards of Reporting Trials)59 flowchart depicting eligibility screening through the 60-month assessment. Study eligibility criteria were that mothers had to be at least 18 years of age, live within the catchment area, be comfortable speaking English, intend to raise their child to speak primarily English, have received at least some prenatal care, and have income below 200% of the poverty level (operationalized by receipt of Medi-Cal/Medicaid or food stamps, or Temporary Assistance for Needy Families eligibility). Los Angeles participants were recruited at prenatal clinics managed by the UCLA Medi-Cal Health Maintenance Organization. In Miami, mothers eligible for Medicaid, food stamps, or Temporary Assistance for Needy Families were recruited from 2 hospitals within 72 hours of delivery.
FIGURE 1—
Participant Flowchart for the Legacy for Children Project.
We randomized consenting study participants to intervention and comparison groups at a ratio of 3:2. Assessors naïve to group assignment conducted assessments at baseline and when the children were 6, 12, 24, 36, 48, and 60 months old. Procedures included extensive efforts to minimize study attrition, including transportation and child care assistance, regular mail or phone contact, and monetary compensation for each data collection session. Assessment participation rates ranged from 78% (at 12 months) to 62% (at 60 months) in Los Angeles, and from 89% (at 12 months) to 65% (at 60 months) in Miami, with 91% of the original randomized sample participating in at least 1 assessment time point.
Intervention
The 3 tenets of the Legacy philosophy52 hold that: the quality of the mother-child relationship is critical to healthy child development, there are multiple pathways to positive mother-child relationships (i.e., there is no single “right” way to parent), and mothers can have significant positive impact on their children’s development, no matter what their circumstances. Legacy’s theory of change posits that the key modifiable factors influencing mothers’ ability and willingness to provide nurturing and supportive environments for their children are mothers’ self-efficacy for parenting behaviors, commitment to the parenting role, and feeling supported for her parenting choices. Legacy’s intervention activities (weekly group meetings in a community or University location, occasional 1-on-1 sessions, and group outings in the community) targeted those factors by offering a forum for discussing and testing different parenting strategies, and providing a community of support for mothers’ parenting choices. These activities were designed to promote changes in parenting attitudes (specifically, parental responsibility, commitment to the parenting role, and sense of having a supportive community) and behaviors (i.e., guidance of their child’s emotional and behavioral regulation, and fostering children’s verbal and cognitive development). These attitudes and behaviors were expected to translate into more positive mother-child interactions, which would result in more positive socioemotional, behavioral, cognitive, and health outcomes for children.
Although based on a core set of Legacy goals, each site developed its own curriculum to be responsive to the needs of the demographically and culturally distinct populations served. As there was no consensus in the field of the optimal duration or dosage of this type of intervention, those varied between sites as well. The intervention began prenatally (Los Angeles) or at birth (Miami), and lasted until 3 or 5 years of age, respectively. Group sessions met weekly for 1.5 (Miami) or 2.5 (Los Angeles) hours, and included both mother-only time (e.g., talking about current milestones, discussing new or alternative parenting behaviors, reinforcing mother’s role in her child’s development) and mother–child interactive time (e.g., practicing skills, reinforcing mothers’ positive behaviors). The total number of possible group intervention sessions was 101 in Los Angeles and 250 in Miami. The curricula content capitalized on the accomplishments and challenges at different child ages, providing mothers with information and skills at times of high relevance and motivation. Specific parenting topics included sensitive responding, affection, establishing and maintaining routines, discipline, play and creativity, language, and fostering school readiness. Intervention specialists had at least a bachelor’s degree in social science or education, experience working with low-income mothers, and at least 2 years’ experience working with children. Fidelity monitoring included data from program records, program providers, participants, and direct observations.
Measures of Children’s Behavioral and Socioemotional Outcomes
The Brief Infant-Toddler Social and Emotional Assessment60 (BITSEA) is a 42-item parent-report instrument producing 2 scores: a competence score (including attention, compliance, imitation or play, social relatedness, empathy, and mastery motivation) and a problem score (including oppositional, inattentive, and hyperactive behaviors, and problems common to children with autistic spectrum and related disorders). A validation study60 reported that both scores correlated with observer ratings of behaviors and the problem score predicted Child Behavior Checklist problem scores 1 year later. Age- and gender-specific cutpoints allow for dichotomous indicators of high behavioral problems and low competence, with the most sensitive detection resulting from a “high screen,” indicating the presence of either high problem or low competence scores. The high screen criterion has documented 85% sensitivity and 75% specificity. Mothers completed the BITSEA at the 12-month assessment.
The Devereux Early Childhood Assessment61 (DECA) is a 37-item parent-reported rating scale containing 2 subscales: protective factors (measuring the socioemotional competence domains of initiative, self-control, and attachment) and behavioral concerns (measuring problem and challenging behaviors). The authors reported Cronbach’s α of 0.91 (protective factors) and 0.71 (behavioral concerns). LeBuffe and Naglieri62 demonstrated that a “concerns” cutoff of 1 SD beyond the means resulted in 71% and 68% correct classification (for behavioral concerns and protective factors, respectively) of clinical group membership. At the start of the study, we selected a cutpoint of 2 SDs beyond the means to identify the children at greatest risk for clinically significant problems, and created dichotomous outcomes from t-scores. Based on the t-distribution, only 2.5% of a typical sample would be expected to fall 2 SDs beyond the cutoff. Mothers completed the DECA at the 24-, 36-, 48-, and 60-month assessments.
The Strengths and Difficulties Questionnaire63 (SDQ) is a parent-reported behavioral screener, composed of 25 items on 5 subscales: conduct problems, hyperactivity, emotional symptoms, peer problems, and prosocial behavior. Mothers completed the SDQ at 48 and 60 months. Conventional cutoffs by Goodman et al.64 demonstrated acceptable sensitivity in predicting childhood psychiatric disorders, including attention-deficit hyperactivity disorder (ADHD), conduct disorders, depressive disorders, and certain anxiety disorders, with greatest sensitivity when parent and teacher ratings were used together. More recently, Ullebø et al.65 demonstrated acceptable sensitivity using only parent reports of the SDQ hyperactivity-inattention subscale to predict the ADHD phenotype with a lower cutoff. We therefore conducted group comparisons using the earlier and more recent recommended cutoffs.
Data Analyses
We first examined baseline demographic characteristics across groups. The main analyses began with a series of bivariate intent-to-treat analyses, separately at each time point. For these, we used logistic regression to predict scores outside the respective cutoff points of the BITSEA, DECA, and SDQ from group status, indicating the odds of meeting criteria for behavioral concerns or socioemotional problems for the treatment versus comparison groups. To facilitate comparison with other early intervention programs, we converted the resulting odds ratios to effect sizes analogous to Cohen’s d 66 using Chinn’s method.67 To incorporate the repeated-measures aspect of the DECA data, we next developed semiparametric regression models, using generalized estimating equations, to test for differences in the group-averaged effects of the intervention on the dichotomous DECA outcomes over time (at 24, 36, 48, and 60 months). To examine the potential impact of multiple comparisons on our conclusions, we conducted simulation analyses using permutation test methodology68 to determine the rate of replication for the demonstrated pattern of effects. We generated a series of 5000 simulations in which the intervention variable was re-randomized for each set of participant outcomes, and compared the simulated results to the observed outcomes to determine the likelihood of obtaining a superior pattern of effects.
Because the interventions were of different durations, data from the sites were analyzed separately. In Miami, the 60-month assessment represented the immediate postintervention point. In Los Angeles, the 36-month assessment represented the immediate postintervention point, and the 48- and 60-month assessments were 1 and 2 years postintervention. All other assessments were conducted while the intervention was ongoing for participants.
RESULTS
Examination of baseline demographics indicated that our sample of mothers was generally young (mean age = 24 years), unmarried (78%), and unemployed (74%). The total sample reported themselves as predominantly non-Hispanic Black (57%) or Hispanic (24.9%). Approximately 50% of the mothers reported household annual incomes below $20 000. Cross-site demographic comparisons revealed that Los Angeles mothers were significantly older and more educated, and were more likely to be married, Hispanic, employed, renting their residence, and speaking a language other than English at home than were Miami mothers. The site samples were statistically equivalent on household income, use of English in the home, child gender, and household composition. At both sites, randomization resulted in equivalence across the intervention and comparison groups at baseline on mother’s age, education, marital status, race/ethnicity, employment status, and income.
Table 1 shows the results of the logistic regressions, analyzing all available data from the groups as randomized, at individual time points. In Miami, children of mothers in the intervention group were less likely to meet criteria for behavioral concerns at 24 months, with 52.5% of the comparison group’s children meeting criteria versus 36.0% of the intervention group’s children (odds ratio [OR] = 0.51; 95% confidence interval [CI] = 0.30, 0.85), with both rates far exceeding the 2.5% expected in the general population. At 48 months, children of mothers in the intervention group were less likely to meet criteria for socioemotional problems (7.1% of the intervention group’s children vs 16.1% of the comparison group’s children) (OR = 0.40; 95% CI = 0.16, 0.99). In Los Angeles, children of mothers in the intervention group were somewhat less likely to meet the high screen criteria (for either behavioral concerns or socioemotional problems) at 12 months (OR = 0.62; 95% CI = 0.37, 1.05). Almost half of the comparison group met this criteria (49.5%), whereas only 38.0% of the intervention group met the criteria. Intervention children were somewhat less likely than comparison group children (6.8% vs 15.1%, respectively) to meet the socioemotional problems criteria at 60 months (OR = 0.41; 95% CI = 0.16, 1.10). Using the new recommended cutoff of Ullebø et al.,65 intervention children were significantly less likely to fall above the cutoff for hyperactivity at 60 months (OR = 0.50; 95% CI = 0.27, 0.93).
TABLE 1—
Intent-to-Treat Analyses by Site: Legacy for Children Project
| Miami |
Los Angeles |
|||||
| Scale/Age, Mo (Subscale) | No. | OR (95% CI) | Effect Sizea | No. | OR (95% CI) | Effect Sizea |
| BITSEA/12 | ||||||
| Behavioral concerns | 261 | 0.67 (0.41, 1.11) | −0.22 | 236 | 0.70 (0.41, 1.21) | −0.20 |
| Socioemotional problems | 261 | 0.81 (0.42, 1.59) | −0.12 | 235 | 0.75 (0.35, 1.59) | −0.16 |
| “High screen” (either indicator) | 268 | 0.69 (0.41, 1.15) | −0.21 | 236 | 0.62b (0.37, 1.05) | -0.26 |
| DECA/24 | ||||||
| Behavioral concerns | 254 | 0.51* (0.30, 0.85) | -0.37 | 226 | 0.79 (0.44, 1.41) | −0.13 |
| Socioemotional problems | 255 | 0.98 (0.54, 1.80) | −0.01 | 228 | 0.53 (0.22, 1.28) | −0.35 |
| DECA/36 | ||||||
| Behavioral concerns | 224 | 0.68 (0.38, 1.20) | −0.21 | 204 | 1.23 (0.64, 2.40) | 0.11 |
| Socioemotional problems | 225 | 1.78 (0.81, 3.91) | 0.32 | 206 | 1.07 (0.46, 2.46) | 0.04 |
| DECA/48 | ||||||
| Behavioral concerns | 208 | 0.60 (0.32, 1.13) | −0.28 | 202 | 0.62 (0.30, 1.29) | −0.26 |
| Socioemotional problems | 208 | 0.40*(0.16, 0.99) | −0.51 | 202 | 1.00 (0.37, 2.71) | 0.00 |
| DECA/60 | ||||||
| Behavioral concerns | 194 | 0.56 (0.28, 1.14) | −0.32 | 187 | 0.62 (0.27, 1.45) | −0.26 |
| Socioemotional problems | 195 | 1.00 (0.41, 2.40) | 0.00 | 190 | 0.41b (0.16, 1.10) | −0.49 |
| SDQ/48 | ||||||
| Emotional symptomsc | 208 | … | … | 202 | … | … |
| Conduct problems | 208 | 0.64 (0.36, 1.13) | −0.25 | 202 | 0.72 (0.40, 1.30) | −0.18 |
| Hyperactivity (Goodman et al.64 criteria) | 208 | 0.83 (0.37, 1.86) | −0.10 | 202 | 1.98 (0.62, 6.38) | 0.38 |
| Hyperactivity (Ullebø et al.65 criteria) | 208 | 0.63 (0.36, 1.11) | −0.26 | 202 | 0.92 (0.52, 1.64) | −0.05 |
| Peer problems | 208 | 0.94 (0.52, 1.69) | −0.03 | 202 | 1.24 (0.62, 2.46) | 0.12 |
| Prosocial behaviorc | 208 | … | … | 202 | … | … |
| SDQ/60 | ||||||
| Emotional symptomsc | 194 | … | … | 187 | … | … |
| Conduct problems | 194 | 0.72 (0.39, 1.30) | −0.18 | 187 | 1.06 (0.55, 2.03) | 0.03 |
| Hyperactivity (Goodman et al.64 criteria) | 194 | 0.57 (0.22, 1.44) | −0.31 | 187 | 0.74 (0.28, 1.98) | −0.17 |
| Hyperactivity (Ullebø et al.65 criteria) | 194 | 0.70 (0.39, 1.30) | −0.20 | 187 | 0.50* (0.27, 0.93) | −0.38 |
| Peer problems | 194 | 1.28 (0.65, 2.54) | 0.14 | 187 | 0.73 (0.35, 1.55) | −0.17 |
| Prosocial behaviorc | 194 | … | … | 187 | … | … |
Note. BITSEA = Brief Infant-Toddler Social and Emotional Assessment60; CI = confidence interval; DECA = Devereux Early Childhood Assessment61; OR = odds ratio; SDQ = Strengths and Difficulties Questionnaire.63 Prevention effects for all variables are indicated by smaller odds ratios and larger negative effect sizes.
Effect size, analogous to Cohen d,66 calculated using Chinn’s simple method for converting odds ratios.67
OR approached significance (P < .1).
Site sample sizes were too small (n < 5) to allow for meaningful statistical comparisons; therefore, those odds ratios were not calculated. The Fisher exact test failed to reveal statistical significance.
*P < .05.
Table 1 also presents effect sizes analogous to Cohen’s d.66 Negative effect sizes indicate positive program effects (i.e., lower likelihood of negative outcomes in the intervention group). Effect sizes for behavioral concerns indicators ranged from −0.17 to −0.37 in Miami and 0.11 to −0.26 in Los Angeles. Effect sizes for socioemotional problems ranged from 0.32 to −0.51 in Miami and 0.04 to −0.49 in Los Angeles. For the SDQ at 48 and 60 months, effect sizes on the subscales ranged from 0.03 to −0.25 (conduct), 0.38 to −0.31 (hyperactivity), and 0.14 to −0.17 (peer problems). The range of effect sizes for the new Ullebø et al.65 cutoff of the hyperactivity subscale was −0.05 to −0.38.
The semiparametric regression models, which consider group-averaged effects over time, indicated significant group differences on behavioral concerns between 24 and 60 months in Miami. Intervention group children were less likely than comparison group children to meet criteria for behavioral concerns over the 3-year span (Figure 2; OR = 0.56; 95% CI = 0.38, 0.84; χ2(1) = 7.66; P = .006). The models for behavioral concerns in Los Angeles and for socioemotional problems at both sites were not significant.
FIGURE 2—
Percentage of children falling 2 SDs above the mean for behavioral concerns in Miami, by intervention group: Legacy for Children Project.
The simulation analyses indicated that the pattern of obtained effects (i.e., that intervention outcomes were, with few exceptions, superior to comparison outcomes) were not duplicated in any of the 5000 simulated iterations. Therefore, the demonstrated pattern of effects was unlikely the result of type 1 error.
DISCUSSION
Both samples evidenced elevated rates of behavioral concerns and socioemotional problems, confirming the appropriateness of the populations for Legacy. In the individual time-point analyses, we documented significant differences in behavioral concerns at 24 months and socioemotional problems at 48 months in Miami, suggesting that the Legacy model was associated with a reduction in risk for meeting those criteria. In Los Angeles, Legacy was associated with lower rates of hyperactivity at 60 months using the most current SDQ hyperactivity cutoff, suggesting intervention children’s ADHD rates might be lower as they enter elementary school. These effects translated into 16% fewer children with behavioral concerns at 24 months and 9% fewer children with socioemotional problems at 48 months in Miami, and 16% fewer children meeting the current hyperactivity cutoff at 60 months in Los Angeles. The longitudinal group-averaged effects indicated significant effects on behavioral concerns in Miami from age 2 to 5 years. These conservative, intent-to-treat analyses suggested potential for population-level impact of Legacy on early childhood outcomes.
Patterns of effect sizes for behavioral concerns (all magnitudes ≥ 0.22 in Miami, and 4 of 5 time point magnitudes ≥ 0.13 in Los Angeles) suggested consistent effects on children’s problematic behaviors at both sites, although Miami evidenced a greater number of significant effects (including the longitudinal analyses). Site differences might have been influenced by the higher rates of behavioral concerns in the Miami sample or differential responsiveness to the intervention. Although both samples were a diverse set of mothers living in poverty, Miami mothers were generally a demographically higher risk group (e.g., younger, less educated, and more likely to be single and unemployed) and might have been more receptive to this type of intervention. Alternatively, variation in site results might stem from implementation differences, such as curriculum or dosage.
The socioemotional problems measures, which included items about subtler child characteristics and internal emotional processes, evidenced a wider range of effect sizes in both sites. However, actual rates of socioemotional problems varied less across sites and over time than rates of behavioral concerns. Whether these apparent inconsistencies were because of differential effectiveness of Legacy on the 2 domains analyzed here or on differential performance of the measures used to assess the domains will become clearer in the follow-up study, when these children are in third grade.
Table 2 shows the Legacy results at age 5 years, along with published effect sizes from comparable programs and meta-analyses. Two predecessors of Legacy, Early Head Start69 and the Infant Health and Development Program,46 reported weaker effects on similar behavior problem outcomes at similar ages than either Los Angeles or Miami. The reported effect sizes from meta-analyses of 4 other well-known program models—home visiting,70 family support programs,71 early education,72 and behavioral parent training73—showed that 3 of 4 Legacy effect sizes compared favorably with other intervention models. It was also notable that of the 4 meta-analyses, 3 had documented70,71,73 considerable variability in effects across outcome domains, as we did. In addition, the reported mean effect sizes on socioemotional competence70–73 were larger than the reported mean effect size on externalizing behaviors,73 similar to our results.
TABLE 2—
Published Effect Sizes on Comparable Measures and at Comparable Child Ages for Legacy for Children and Similar Programs and Models
| Program or Model | Target Population | Child Outcome | Effect Sizea |
| Legacy Miamib | Low-income mothers, recruited shortly after childbirth | Behavior problems (age 5 y) | 0.32 |
| Legacy Miamib | Low-income mothers, recruited shortly after childbirth | Socioemotional competence (age 5 y) | 0.00 |
| Legacy Los Angelesb | Low-income mothers, recruited while pregnant | Behavior problems (age 5 y) | 0.26 |
| Legacy Los Angelesb | Low-income mothers, recruited while pregnant | Socioemotional competence (age 5 y) | 0.49 |
| Early Head Start69 | Low-income pregnant women and families with infants and toddlers up to age 3 y | Aggressive behavior (age 3 y) | 0.11 |
| Infant Health & Development Program46 | Low birthweight, premature infants | Problem behaviors (age 5 y) | 0.06 |
| Home visiting (meta-analysis)70 | Families with young children, mostly ages birth to 3 y | Socioemotional outcomes | Mean ES = 0.10 |
| Family support programs (meta-analysis)71 | Families with children between birth and age 12 y | Socioemotional outcomes | Mean ES = 0.22 |
| Early educational programs (meta-analysis)72 | Children aged 3–5 y | Socioemotional outcomes | Mean ES = 0.16 |
| Behavioral parent training (meta-analysis)73 | Parents of children aged 0–7 y | Social skills | Mean ES = 0.13 |
| Behavioral parent training (meta-analysis)73 | Parents of children aged 0–7 y | Externalizing behaviors | Mean ES = 0.25 |
These findings through age 5 years were markers for potential later impact of Legacy. Early emotional and behavioral problems reliably have predicted adult outcomes, such as obesity,53 asthma,53 medical problems,54 overall health,54 and health burden55,56 in other studies. One 25-year longitudinal study estimated that rates of participation in crime, substance dependence, mental health problems, and unhealthy sexual or partner relationships were 1.5 to 19 times higher for adults who were in the top 5% of the sample with respect to severity of early behavioral and conduct problems at age 7 to 9 years.57 Scott et al.58 estimated that health costs through age 28 years were 5 times as high for children with conduct problems at age 10 years. By preventing the incidence or reducing the severity of early behavior problems, Legacy might have longer reaching impact on later health outcomes and societal costs.
Limitations included the reliance on parent report for all child behavioral and socioemotional outcomes included here. Analyses are currently under way of other outcomes—standardized cognitive tests and observations of mother-child interactions—to document the extent to which Legacy effects extend beyond mothers’ reports. Study attrition was also a consideration because these analyses assumed a missing-at-random pattern of nonresponse. Attrition patterns (analyses not shown) were similar for intervention and comparison groups at both sites. Nonetheless, generalizability was limited to those who completed at least 1 post-baseline assessment time analyzed here (91% of the randomized sample). Although 35% of Miami mothers and 50% of Los Angeles mothers reported speaking another language in addition to or instead of English at home, generalizability was also limited to families in which the mother was comfortable speaking English. Finally, the present analyses, conducted in a conservative, intent-to-treat manner, did not take into account intervention participation or dropout. Subsequent analyses are being conducted to examine potential dose-response relationships.
Although the Legacy intervention lasted 3 or 5 years, marginal effects were documented after the first year, and significant effects were documented after the second year. We are currently assessing Legacy’s longer term behavioral and health impacts when the children are in third grade, including: measures of school performance; aggressive, delinquent, and risky behaviors; contact with child protective services; physical activity and nutrition; injuries; identified behavioral or health conditions; and mental health. In collaboration with the Administration for Children and Families, we are also testing the feasibility of implementing Legacy in Early Head Start settings to inform efforts to scale up for widespread dissemination, thus magnifying the potential for public health impact. Investing in this type of early prevention may reduce the need for later intervention as well.
Acknowledgments
The Legacy for Children trials and their evaluation were sponsored and directed by the Centers for Disease Control and Prevention (CDC) under contracts with the University of Miami (200-1998-0110), the University of California at Los Angeles (200-1998-0111), and Research Triangle International (200-94-0828).
Legacy for Children is a registered trademark of the Centers for Disease Control and Prevention.
We would also like to acknowledge the following individuals for assistance with study design and conceptualization: Ed Brann, Bertha Gorham, Judy Thorne; conceptualization or participation in the evaluation: Angelika Claussen, Linda Iklé, Catherine Lesesne, Beth Miller, Betty Rintoul, Lissette Saavedra, Ina Wallace; development or delivery of the intervention: Sarah Doakes, Dane Fitzmorris, Awilda Gonzales, Michelle Gross, Lynne Katz, Elaine Maxwell, Rosalie Miller, Luisa DeSantis; and project oversight: Maria Gonzalez, Dianne Ochoa, Bill Ramsey.
Note. The findings and conclusions in this report are those of the authors, and do not necessarily reflect the official position of the Centers for Disease Control and Prevention.
Human Participant Protection
Four institutional review boards (Centers for Disease Control and Prevention, Research Triangle International, University of California–Los Angeles, and University of Miami) approved and monitored the protocol, which involved informed consent from all participating mothers.
References
- 1.DeNavas-Walt C, Proctor BD, Smith JC. US Census Bureau Current Population Reports (P60-238) Income, Poverty, and Health Insurance Coverage in the United States: 2009. Washington, DC: US Government Printing Office; 2010 [Google Scholar]
- 2.Smith PJ, Singleton JA. County-level trends in vaccination coverage among children aged 19-35 months–United States, 1995–2008. MMWR Surveill Summ. 2011;60(4):1–86 [PubMed] [Google Scholar]
- 3.Newacheck PW. Poverty and childhood chronic illness. Arch Pediatr Adolesc Med. 1994;148(11):1143–1149 [DOI] [PubMed] [Google Scholar]
- 4.Chen E, Martin AD, Matthews KA. Trajectories of socioeconomic status across children’s lifetime predict health. Pediatrics. 2007;120(2):e297–e303 [DOI] [PubMed] [Google Scholar]
- 5.Starfield B, Robertson J, Riley AW. Social class gradients and health in childhood. Ambul Pediatr. 2002;2(4):238–246 [DOI] [PubMed] [Google Scholar]
- 6.Duncan GJ, Brooks-Gunn J, Klebanov PK. Economic deprivation and early-childhood development. Child Dev. 1994;65(2):296–318 [PubMed] [Google Scholar]
- 7.McLeod JD, Nonnemaker JM. Poverty and child emotional and behavioral problems: racial/ethnic differences in processes and effects. J Health Soc Behav. 2000;41(2):137–161 [Google Scholar]
- 8.Pachter LM, Auinger P, Palmer R, Weitzman M. Do parenting and the home environment, maternal depression, neighborhood, and chronic poverty affect child behavioral problems differently in different racial-ethnic groups? Pediatrics. 2006;117(4):1329–1338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention QuickStats: percentage of children with serious emotional or behavioral difficulties, by age group and family income group — National Health Interview Survey, United States, 2004–2009. MMWR Morb Mortal Wkly Rep. 2011;60(17):555 [Google Scholar]
- 10.Centers for Disease Control and Prevention Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children – United States, 2003 and 2007. MMWR Morb Mortal Wkly Rep. 2010;59(44):1439–1443 [PubMed] [Google Scholar]
- 11.Brooks-Gunn J, Duncan GJ. The effects of poverty on children. Future Child. 1997;7(2):55–71 [PubMed] [Google Scholar]
- 12.Korenman S, Miller JE, Sjaastad JE. Long-term poverty and child development in the United States: results from the NLSY. Child Youth Serv Rev. 1995;17(1–2):127–155 [Google Scholar]
- 13.Evans GW, Kim P. Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychol Sci. 2007;18(11):953–957 [DOI] [PubMed] [Google Scholar]
- 14.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179 [DOI] [PubMed] [Google Scholar]
- 15.McEwen BS. The neurobiology of stress: from serendipity to clinical relevance. Brain Res. 2000;886(1-2):172–189 [DOI] [PubMed] [Google Scholar]
- 16.Chen E, Matthews KA, Boyce WT. Socioeconomic differences in children’s health: how and why do these relationships change with age? Psychol Bull. 2002;128(2):295–329 [DOI] [PubMed] [Google Scholar]
- 17.Case A, Lubotsky D, Paxson C. Economic status and health in childhood: the origins of the gradient. Am Econ Rev. 2002;92(5):1308–1334 [DOI] [PubMed] [Google Scholar]
- 18.Cunha F, Heckman JJ. The economics and psychology of inequality and human development. J Eur Econ Assoc. 2009;7(2–3):320–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Power C, Manor O, Matthews S. Child to adult socioeconomic conditions and obesity in a national cohort. Int J Obes Relat Metab Disord. 2003;27(9):1081–1086 [DOI] [PubMed] [Google Scholar]
- 20.Gliksman MD, Kawachi I, Hunter Det al. Childhood socioeconomic status and risk of cardiovascular disease in middle aged US women: a prospective study. J Epidemiol Community Health. 1995;49(1):10–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaplan GA, Salonen JT. Socioeconomic conditions in childhood and ischaemic heart disease during middle age. BMJ. 1990;301(6761):1121–1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poulton R, Caspi A, Milne BJet al. Association between children’s experience of socioeconomic disadvantage and adult health: a life-course study. Lancet. 2002;360(9346):1640–1645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Starfield B, Riley AW, Witt WP, Robertson J. Social class gradients in health during adolescence. J Epidemiol Community Health. 2002;56(5):354–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duncan GJ, Ziol-Guest KM, Kalil A. Early-childhood poverty and adult attainment, behavior, and health. Child Dev. 2010;81(1):306–325 [DOI] [PubMed] [Google Scholar]
- 25.Serbin LA, Karp J. The intergenerational transfer of psychosocial risk: mediators of vulnerability and resilience. Annu Rev Psychol. 2004;55(1):333–363 [DOI] [PubMed] [Google Scholar]
- 26.Scaramella LV, Neppl TK, Ontai LL, Conger RD. Consequences of socioeconomic disadvantage across three generations: parenting behavior and child externalizing problems. J Fam Psychol. 2008;22(5):725–733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Solon G. Intergenerational income mobility in the United States. Am Econ Rev. 1992;82(3):393–408 [Google Scholar]
- 28.Musick K, Mare RD. Recent trends in the inheritance of poverty and family structure. Soc Sci Res. 2006;35(2):471–499 [Google Scholar]
- 29.Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, Salpekar N. The role of chaos in poverty and children’s socioemotional adjustment. Psychol Sci. 2005;16(7):560–565 [DOI] [PubMed] [Google Scholar]
- 30.Evans GW, English K. The environment of poverty: multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Dev. 2002;73(4):1238–1248 [DOI] [PubMed] [Google Scholar]
- 31.Moren-Cross JL, Wright DR, LaGory M, Lanzi RG. Perceived neighborhood characteristics and problem behavior among disadvantaged children. Child Psychiatry Hum Dev. 2006;36(3):273–294 [DOI] [PubMed] [Google Scholar]
- 32.Dilworth-Bart JE, Moore CF. Mercy mercy me: social injustice and the prevention of environmental pollutant exposures among ethnic minority and poor children. Child Dev. 2006;77(2):247–265 [DOI] [PubMed] [Google Scholar]
- 33.Gershoff ET, Aber JL, Raver CC, Lennon MC. Income is not enough: incorporating material hardship into models of income associations with parenting and child development. Child Dev. 2007;78(1):70–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jackson AP, Brooks-Gunn J, Huang CC, Glassman M. Single mothers in low-wage jobs: financial strain, parenting, and preschoolers’ outcomes. Child Dev. 2000;71(5):1409–1423 [DOI] [PubMed] [Google Scholar]
- 35.McGroder SM. Parenting among low-income, African American single mothers with preschool-age children: patterns, predictors, and developmental correlates. Child Dev. 2000;71(3):752–771 [DOI] [PubMed] [Google Scholar]
- 36.Bassuk EL, Weinreb LF, Dawson R, Perloff JN, Buckner JC. Determinants of behavior in homeless and low-income housed preschool children. Pediatrics. 1997;100(1):92–100 [DOI] [PubMed] [Google Scholar]
- 37.Burchinal M, Roberts JE, Zeisel SA, Hennon EA, Hooper S. Social risk and protective child, parenting, and child care factors in early elementary school years. Parent: Sci Pract. 2006;6(1):79–113 [Google Scholar]
- 38.Klein K, Forehand R. Family processes as resources for African American children exposed to a constellation of sociodemographic risk factors. The Family Health Project Research Group. J Clin Child Psychol. 2000;29(1):53–65 [DOI] [PubMed] [Google Scholar]
- 39.Mistry RS, Vandewater EA, Huston AC, McLoyd VC. Economic well-being and children’s social adjustment: the role of family process in an ethnically diverse low-income sample. Child Dev. 2002;73(3):935–951 [DOI] [PubMed] [Google Scholar]
- 40.Oravecz LM, Koblinsky SA, Randolph SM. Community violence, interpartner conflict, parenting, and social support as predictors of the social competence of African American preschool children. J Black Psychol. 2008;34(2):192–216 [Google Scholar]
- 41.Vanderbilt-Adriance E, Shaw DS. Protective factors and the development of resilience in the context of neighborhood disadvantage. J Abnorm Child Psychol. 2008;36(6):887–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ramey CT, Campbell FA. Preventive education for high-risk children: cognitive consequences of the Carolina Abecedarian Project. Am J Ment Defic. 1984;88(5):515–523 [PubMed] [Google Scholar]
- 43.Reynolds AJ, Temple JA. Extended early childhood intervention and school achievement: age thirteen findings from the Chicago Longitudinal Study. Child Dev. 1998;69(1):231–246 [PubMed] [Google Scholar]
- 44.Weikart DP, Bond JT, McNeil JT. The Ypsilanti Perry Preschool Project: Preschool Years and Longitudinal Results Through Fourth Grade. Ypsilanti, MI: High/Scope Press; 1978 [Google Scholar]
- 45.Olds D, Henderson CJ, Kitzman H, Eckenrode J, Cole R, Tatelbaum R. The promise of home visitation: results of two randomized trials. J Community Psychol. 1998;26(1):5–21 [Google Scholar]
- 46.Brooks-Gunn J, McCarton CM, Casey PHet al. Early intervention in low-birth-weight premature infants: results through age 5 years from the Infant Health and Development Program. JAMA. 1994;272(16):1257–1262 [PubMed] [Google Scholar]
- 47.Johnson DL, Breckenridge JN. The Houston Parent–Child Development Center and the primary prevention of behavior problems in young children. Am J Community Psychol. 1982;10(3):305–316 [DOI] [PubMed] [Google Scholar]
- 48.Barkley RA, Shelton TL, Crosswait Cet al. Preliminary findings of an early intervention program with aggressive hyperactive children. Ann N Y Acad Sci. 1996;794:277–289 [DOI] [PubMed] [Google Scholar]
- 49.Eyberg SM, Boggs SR. Parent-Child Interaction Therapy for oppositional preschoolers. In: Schaefer CE, Briesmeister JM, eds. Handbook of Parent Training: Parents as Co-Therapists for Children’s Behavior Problems. 2nd ed. New York, NY: Wiley; 1998:61–97 [Google Scholar]
- 50.Forehand R, McMahon RJ. Helping the Noncompliant Child: A Clinician’s Guide to Effective Parent Training. New York, NY: Guilford; 1981 [Google Scholar]
- 51.Webster-Stratton C. Preventing conduct problems in Head Start children: strengthening parenting competencies. J Consult Clin Psychol. 1998;66(5):715–730 [DOI] [PubMed] [Google Scholar]
- 52.Perou R, Elliott MN, Visser SNet al. Legacy for ChildrenTM: a pair of randomized controlled trials of a public health model to improve developmental outcomes among children in poverty. BMC Public Health. 2012;12:691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Goodwin RD, Sourander A, Duarte CSet al. Do mental health problems in childhood predict chronic physical conditions among males in early adulthood? Evidence from a community-based prospective study. Psychol Med. 2009;39(2):301–311 [DOI] [PubMed] [Google Scholar]
- 54.Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. J Am Acad Child Adolesc Psychiatry. 1998;37(6):594–601 [DOI] [PubMed] [Google Scholar]
- 55.Odgers CL, Caspi A, Broadbent JMet al. Prediction of differential adult health burden by conduct problem subtypes in males. Arch Gen Psychiatry. 2007;64(4):476–484 [DOI] [PubMed] [Google Scholar]
- 56.Odgers CL, Moffitt TE, Broadbent JMet al. Female and male antisocial trajectories: from childhood origins to adult outcomes. Dev Psychopathol. 2008;20(2):673–716 [DOI] [PubMed] [Google Scholar]
- 57.Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven: the consequences of conduct problems in childhood for psychosocial functioning in adulthood. J Child Psychol Psychiatry. 2005;46(8):837–849 [DOI] [PubMed] [Google Scholar]
- 58.Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. 2001;323(7306):191–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schulz KF, Altman DG, Moher D, for the CONSORT Group CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV. The Brief-Infant Toddler Social and Emotional Assessment: screening for social emotional problems and delays in competence. J Pediatr Psychol. 2004;29(2):143–155 [DOI] [PubMed] [Google Scholar]
- 61.LeBuffe PA, Naglieri J. Devereux Early Childhood Assessment: Technical Manual. Lewisville, NC: Kaplan Press; 1999 [Google Scholar]
- 62.LeBuffe PA, Naglieri JA. The Devereux Early Childhood Assessment (DECA): a measure of within-child protective factors in preschool children. NHSA Dialog. 1999;3(1):75–80 [Google Scholar]
- 63.Bourdon KH, Goodman R, Rae DS, Simpson G, Koretz DS. The Strengths and Difficulties Questionnaire: U.W. normative data and psychometric properties. J Am Acad Child Adolesc Psychiatry. 2005;44(6):557–564 [DOI] [PubMed] [Google Scholar]
- 64.Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry. 2000;177:534–539 [DOI] [PubMed] [Google Scholar]
- 65.Ullebø AK, Posserud M, Heierbang E, Gillberg C, Obel C. Screening for the attention deficit hyperactivity disorder phenotype using the Strengths and Difficulties Questionnaire. Eur Child Adolesc Psychiatry. 2011;20(9):451–458 [DOI] [PubMed] [Google Scholar]
- 66.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988 [Google Scholar]
- 67.Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000;19(22):3127–3131 [DOI] [PubMed] [Google Scholar]
- 68.Good P. Permutation Tests: A Practical Guide to Resampling Methods for Testing Hypotheses. New York, NY: Springer-Verlag; 1994 [Google Scholar]
- 69.Love JM, Kisker EE, Ross CMet al. Making a difference in the lives of infants and toddlers and their families: The impacts of Early Head Start. Final Technical Report. Vol I Washington, DC: US Department of Health and Human Services, Head Start Bureau; 2002 [Google Scholar]
- 70.Sweet MA, Appelbaum MI. Is home visiting an effective strategy? A meta-analytic review of home visiting programs for families with young children. Child Dev. 2004;75(5):1435–1456 [DOI] [PubMed] [Google Scholar]
- 71.Layzer JI, Goodson BD, Bernstein L, Price C. National Evaluation of Family Support Programs, Final Report. The Meta-Analysis. Vol A Cambridge, MA: Abt Associates; 2001 [Google Scholar]
- 72.Camilli G, Vargas S, Ryan S, Barnett WS. Meta analysis of the effects of early education interventions on cognitive and social development. Teach Coll Rec. 2010;112(3):579–620 [Google Scholar]
- 73.Kaminski JW, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. J Abnorm Child Psychol. 2008;36(4):567–589 [DOI] [PubMed] [Google Scholar]