Abstract
Objectives. We examined the impact of Massachusetts health reform and its public health component (enacted in 2006) on change in health insurance coverage by perceived health.
Methods. We used 2003–2009 Behavioral Risk Factor Surveillance System data. We used a difference-in-differences framework to examine the experience in Massachusetts to predict the outcomes of national health care reform.
Results. The proportion of adults aged 18 to 64 years with health insurance coverage increased more in Massachusetts than in other New England states (4.5%; 95% confidence interval [CI] = 3.5%, 5.6%). For those with higher perceived health care need (more recent mentally and physically unhealthy days and activity limitation days [ALDs]), the postreform proportion significantly exceeded prereform (P < .001). Groups with higher perceived health care need represented a disproportionate increase in health insurance coverage in Massachusetts compared with other New England states—from 4.3% (95% CI = 3.3%, 5.4%) for fewer than 14 ALDs to 9.0% (95% CI = 4.5%, 13.5%) for 14 or more ALDs.
Conclusions. On the basis of the Massachusetts experience, full implementation of the Affordable Care Act may increase health insurance coverage especially among populations with higher perceived health care need.
The sweeping health reform initiative in Massachusetts, An Act Providing Access to Affordable, Quality, Accountable Health Care (enacted April 12, 2006),1 provides a natural experiment with outcomes that may foreshadow those of the comprehensive national health reform President Obama signed into law 4 years later. The Patient Protection and Affordable Care Act (enacted March 23, 2010)2 and amendments in the Health Care and Education Reconciliation Act (enacted March 30, 2010),3 are collectively referred to as the Affordable Care Act (ACA).
This landmark federal law includes provisions to strengthen the public health system, provide mandatory funding for prevention and wellness programs and activities, strengthen the Medicare program, implement insurance market reforms, bolster public health and primary care workforce, and improve the overall quality of the nation’s health system. The act focuses on expanding health insurance coverage and improving the health care delivery system beginning with incremental reforms in 2010 and following up with more substantial changes such as individual mandates, employer requirements, expansion of public programs, premium and cost-sharing subsidies to individuals, premium subsidies to employers, tax changes, and health insurance exchanges in 2014. Importantly, the law also prevents insurers from denying health insurance coverage or charging higher premiums on the basis of health status.4,5 The Congressional Budget Office estimates that, when fully implemented in 2019, ACA will provide coverage to an additional 32 million Americans leaving about 23 million nonelderly people uninsured.6
Systematic reviews of the literature on the impact of health insurance on health care utilization and health outcomes provide some convincing and some nuanced conclusions. These reviews consistently report evidence of increased utilization of physician and preventive services, improvements in the health of vulnerable populations, and lower mortality, conditional on injury and disease; however, how health insurance affects health outcomes for nonelderly adults remains unclear.7,8
From a public health perspective, monitoring implementation of ACA at federal, state, and local levels will be important because this act will change health insurance coverage and access to care, and uptake of care, including preventive services and needed treatment; may alter health care finance and payment structures and care delivery systems as well as health expenditures; and may modify individual and population outcomes of care and health status. Studying the effects of health insurance would ideally rely on experimental evidence7 where health insurance was randomly assigned like the RAND Health Insurance Experiment and the Oregon Medicaid Lottery.9,10 In the absence of randomized experiments, owing to ethical and practical considerations, the need for conducting some social experiments or other approaches to infer causal conclusions from observational data are essential.7,11
Fortunately, a natural experiment of near universal health insurance coverage combined with a targeted public health intervention has been unfolding in Massachusetts for more than 3 years and has been the subject of many studies. Researchers have studied various aspects of the impact of Massachusetts health reform, after 1 year,12 over the short term, comparing 18 months before and 18 months after the reform,13 on young adults and children,14,15 and even the effects of the recession.16 This evolving new body of research leaves a gap in our understanding of the impact of health reform by perceived health care need. We examined the impact of the Massachusetts health reform and its public health component on change in health insurance coverage by perceived health. We examined the impact of the natural experiment in Massachusetts as a model to predict likely outcomes of implementing ACA. Because Medicare already covers most of those aged 65 years and older we compared the effectiveness of mandatory versus optional health insurance among only the nonelderly adult population (aged 18–64 years) residing in Massachusetts and other New England states (Connecticut, Maine, New Hampshire, Rhode Island, and Vermont).
To do this, we compared data between the 3 years (2003–2005) before and the 3 years (2007–2009) after Massachusetts enacted the health reform law and between Massachusetts and other New England states that had no similar health reform laws. Massachusetts and other New England states had similar sociodemographic population characteristics and macroeconomic profiles (e.g., gross domestic product, unemployment rates) over this time period, including a similar impact of 2 years of recession (2007–2009).17,18 This allows not only “before-versus-after” but also “with-versus-without” analyses, a strategy employed by other researchers to explicate the impact of health reform laws and policy as a control for other elements.16,19
We used the Behavioral Risk Factor Surveillance System (BRFSS), the largest and longest-running state-representative, population-based telephone survey that has asked questions about health insurance coverage, health-promoting and health-compromising behaviors, and doctor-diagnosed chronic conditions. Existing federal government and state-sponsored surveys generate different estimates of uninsurance possibly explained by differences in survey design including coverage, reference period, mode, and questionnaire design (wording and placement of questions).20–22 First, we established the quality and the consistency of BRFSS health insurance coverage estimates by comparing these estimates for selected demographic and socioeconomic characteristics with other federal surveys that gather data on health insurance—the American Community Survey (ACS), the Annual Social and Economic Supplement to the Current Population Survey (CPS ASEC), and the National Health Interview Survey (NHIS). The US Census Bureau added a question about health insurance to the 2008 ACS leading to the release of the first set of estimates in September 2009.23 The CPS ASEC is the most widely cited source for health insurance statistics. It is annual, timely, relatively large, and has a state-based design. The NHIS is a continuing nationwide survey conducted by the National Center for Health Statistics.23
We hypothesized a greater increase in the proportion of nonelderly adults with health insurance coverage in Massachusetts than in other New England states. We further hypothesized that nonelderly adults with greater perceived health care needs would be more likely to obtain health insurance coverage. Groups with greater perceived health care need would show a larger increase in health insurance coverage from prereform to postreform and in Massachusetts compared with other New England states.
METHODS
The BRFSS is a state-based, random-digit-dialed telephone survey. The objective of the BRFSS is to collect uniform, state-specific data on preventive health practices and risk behaviors linked to chronic diseases, injuries, and preventable infectious diseases in the adult population.24,25 The BRFSS questionnaire consists of 4 parts: (1) core questions asked in all 50 states and the District of Columbia each year; (2) a rotating set of core questions asked in all 50 states and the District of Columbia every alternate year; (3) supplemental modules, a series of questions on specific topics (e.g., adult asthma history, intimate partner violence, mental health) asked by some states; and (4) state-added questions, unique to a state. Except for state-added questions, all BRFSS questionnaires, data, and reports are available at http://www.cdc.gov/brfss.
As part of the BRFSS survey, trained interviewers administer identical questionnaires over the telephone to an independent probability sample. This report is based on data from 182 852 nonelderly adult (aged 18–64 years) participants in BRFSS for the years 2003 through 2009 (excluding 2006) residing in Massachusetts and other New England states. First, we grouped BRFSS data from 2003 to 2005 as representing the prereform period and 2007 to 2009 as the postreform period. We then considered Massachusetts respondents as “exposed” to health care reform and those in other New England states as “unexposed” to this reform.
Current Health Insurance Coverage and Perceived Health Care Need
We defined current health insurance coverage status as a “Yes” answer to the question, “Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare?”
The Centers for Disease Control and Prevention Health-Related Quality of Life-4 measures (also known as the Healthy Days measures) have demonstrated reliability and validity for population health surveillance. The measures predict health care use in addition to morbidity and mortality, and are associated with chronic diseases, disability, risky health behaviors, and sociodemographic factors.26,27 We used 3 of these measures as proxies for perceived health. Answers to the question “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?” defined physically unhealthy days. Answers to the question “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” defined mentally unhealthy days. Finally, answers to the question “During the past 30 days, for about how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation?” defined activity limitation days. For analysis, we dichotomized the answers to these 3 questions at 14 or more days and at 13 or fewer days. These questions are useful for identifying perceived health among demographic and socioeconomic subpopulations, characterizing the symptomatic burden of disabilities and chronic diseases, and tracking population patterns and trends.28
Andersen’s Behavioral Model of Health Services Use relates people’s use of health services to (1) their predisposition to use these services (demographic and social structure), (2) factors enabling or impeding service use (necessary but not sufficient), and (3) their perceived need for service. We extended the use of Andersen’s model to inform the selection of control variables, namely predisposing and enabling factors (age, gender, race/ethnicity, educational attainment, marital status, and employment status) known to be associated with obtaining health insurance coverage. Andersen’s model explains large observed disparities in the amount (frequency, duration) and quality of health care received.29–31
Statistical Analyses
We compared health insurance coverage before and after implementation of health reform law in Massachusetts, using difference-in-differences (DD) and difference-in-difference-in-differences (DDD) methods to examine the overall trend and the underlying trends in insurance coverage stratified by the levels of perceived health status.32–34 This estimation approach exploits variation over time (comparing pre- and postreform time periods), across states (comparing Massachusetts to other New England states), and between population groups (comparing perceived health care need status). Difference-in-differences or double difference is based on the precondition that outcome data are available for these states before and after the implementation of the Massachusetts health reform law.
To estimate the overall impact of health reform on health insurance coverage, we compared the change in health insurance coverage for adults aged 18 to 64 years in Massachusetts between prereform and postreform periods and for a similar group in other New England states using a DD framework. We used other New England states as the comparison group of neighboring states to control for underlying secular trends in insurance coverage not related to health reform and also adjusted for sociodemographic factors known to influence health insurance coverage such as age, gender, race/ethnicity, education, marital status, and employment status. To estimate the marginal impact of perceived health care need (14 or more physically unhealthy days [PUD+] or mentally unhealthy days [MUD+]) and physical activity limitations (14 or more activity limitation days [ALD+]), we use a DD framework to compare changes over time in health insurance coverage for nonelderly adults with higher perceived-care need or physical activity limitations to changes over time for nonelderly adults without perceived health care need or physical activity limitations (13 or fewer physically unhealthy days [PUD-], mentally unhealthy days [MUD-], or activity limitation days [ALD-]) in Massachusetts.
We tested the hypothesis that nonelderly adults with higher perceived health care need or physical activity limitations would have larger increases in health insurance coverage. We then extended the analysis to control for underlying trends in health insurance coverage not related to health reform by comparing the DD estimate in Massachusetts to an analogous DD estimate for other New England states, using a DDD framework (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org). We implemented these analyses both unadjusted and adjusted for age, gender, race/ethnicity, education, and employment, factors known to influence health insurance coverage. We used logistic regression to implement adjusted analyses and estimate the adjusted prevalence of health insurance and their 95% confidence intervals (CIs). We used SUDAAN software (release 9.0.1, Research Triangle Institute, Research Triangle Park, NC) to account for the complex sample design of the BRFSS.
RESULTS
The 2008 health insurance coverage estimates for nonelderly adults ranged from 79.7% (CPS ASEC) to 82.1% (BRFSS; Table A, available as a supplement to the online version of this article at http://www.ajph.org). The pattern in the health insurance coverage estimates from BRFSS, across levels of sociodemographic characteristics, was similar to estimates from ACS, CPS ASEC, and NHIS.35 Groups with less education, the unemployed, and those not currently married had lower proportions with health insurance coverage. Sociodemographic characteristics of the nonelderly adult civilian noninstitutionalized population in BRFSS by pre- and postreform periods in Massachusetts and other New England states were similar with a notable exception in the distribution by race/ethnicity (Table 1).
TABLE 1—
Sociodemographic Characteristics of the Nonelderly Adult Civilian Noninstitutionalized Population in BRFSS by Prereform (2003–2005) and Postreform (2007–2009) Status in Massachusetts and Other New England States
| Massachusetts (n = 60 388) |
Other New England States (n = 122 464 ) |
|||
| Characteristic | Prereform (n = 19 326), % (95% CI) | Postreform (n = 41 062), % (95% CI) | Prereform (n = 55 564), % (95% CI) | Postreform (n = 66 900), % (95% CI) |
| Age, y | ||||
| 18–34 | 33.8 (32.8, 34.9) | 30.4 (29.5, 31.3) | 31.2 (30.5, 31.8) | 30.2 (29.5, 30.9) |
| 35–64 | 66.2 (65.2, 67.2) | 69.6 (68.7, 70.5) | 68.9 (68.2, 69.5) | 69.8 (69.1, 70.5) |
| Gender | ||||
| Male | 49.2 (48.2, 50.2) | 49.1 (48.3, 49.9) | 49.5 (48.9, 50.1) | 49.6 (49.0, 50.2) |
| Female | 50.8 (49.8, 51.8) | 50.9 (50.1, 51.7) | 50.6 (50.0, 51.2) | 50.4 (49.8, 51.0) |
| Race/ethnicity | ||||
| White, non-Hispanic | 81.6 (80.8, 82.4) | 78.3 (77.5, 79.0) | 86.9 (86.5, 87.4) | 87.1 (86.6, 87.6) |
| Black, non-Hispanic | 4.0 (3.6, 4.3) | 5.3 (4.9, 5.6) | 3.0 (2.8, 3.3) | 2.8 (2.6, 3.1) |
| Hispanic | 9.2 (8.7, 9.9) | 9.3 (8.8, 9.8) | 5.9 (5.6, 6.3) | 5.7 (5.3, 6.0) |
| Other, non-Hispanica | 5.2 (4.7, 5.7) | 7.2 (6.7, 7.7) | 4.1 (3.8, 4.4) | 4.4 (4.1, 4.8) |
| Marital status | ||||
| Currently married | 56.6 (55.7, 57.6) | 61.0 (60.2, 61.8) | 60.4 (59.8, 61.0) | 62.4 (61.8, 63.1) |
| Previously marriedb | 12.4 (11.8, 12.9) | 11.2 (10.8, 11.6) | 13.2 (12.9, 13.5) | 11.5 (11.2, 11.8) |
| Never marriedc | 31.0 (30.0, 32.0) | 27.8 (26.9, 28.6) | 26.4 (25.8, 27.0) | 26.0 (25.4, 26.7) |
| Educational attainment | ||||
| < high school | 7.3 (6.8, 7.9) | 6.4 (6.0, 6.9) | 6.7 (6.4, 7.0) | 5.2 (4.9, 5.5) |
| ≥ high school | 23.3 (22.5, 24.2) | 22.9 (22.2, 23.6) | 27.8 (27.3, 28.4) | 25.4 (24.8, 25.9) |
| ≥ some college | 69.4 (68.5, 70.3) | 70.7 (70.0, 71.5) | 65.5 (63.9, 66.1) | 69.4 (68.8, 70.0) |
| Employment status | ||||
| Employed | 73.8 (72.9, 74.7) | 75.2 (74.5, 75.9) | 75.6 (75.1, 76.2) | 74.1 (73.6, 74.7) |
| Unemployedd | 18.9 (18.1, 19.7) | 17.2 (16.5, 17.9) | 16.8 (16.3, 17.3) | 17.9 (17.3, 18.4) |
| Retired | 3.0 (2.8, 3.3) | 2.8 (2.7, 3.0) | 3.5 (3.3, 3.7) | 3.6 (3.4, 3.8) |
| Unable to work | 4.3 (4.0, 4.7) | 4.8 (4.5, 5.1) | 4.1 (3.9, 4.3) | 4.4 (4.2, 4.6) |
Note. BRFSS = Behavioral Risk Factor Surveillance System; CI = confidence interval.
Asian, non-Hispanic; Native Hawaiian/Pacific Islander, non-Hispanic; American Indian/Alaska Native, non-Hispanic; other race, non-Hispanic; multirace, non-Hispanic.
Includes persons divorced, widowed, and separated.
Includes unmarried couples.
Includes persons out of work, homemakers, and students.
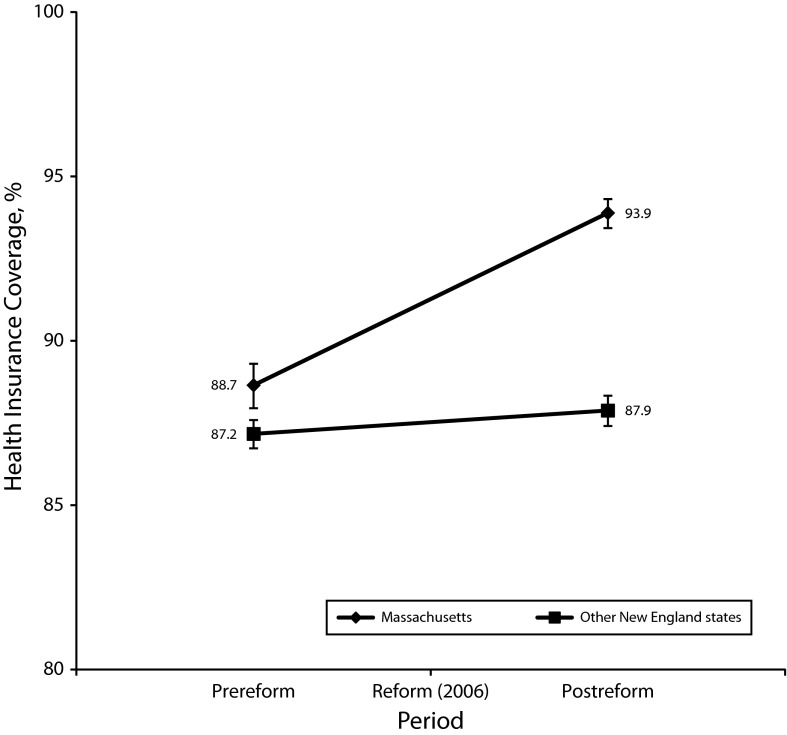
Health insurance coverage in Massachusetts was 88.7% prereform (2003–2005; 95% CI = 88.0, 89.3) and 93.9% postreform (2007–2009; 95% CI = 93.4, 94.3), a statistically significant increase of 5.2% (95% CI = 4.4, 6.1; P < .001; Figure 1; Table 2). Between prereform and postreform in Massachusetts, other New England states had a statistically significant increase in health insurance coverage of 0.7% (95% CI = 0.1, 1.3; P < .05). The overall unadjusted health insurance coverage in Massachusetts increased statistically significantly more than that in other New England states by 4.5% (95% CI = 3.5, 5.6; P < .001). After adjustment, the increase in coverage over time within Massachusetts was 4.7% (95% CI = 3.9, 5.4) whereas within other New England states there was a statistically nonsignificant increase of 0.1% (95% CI = −0.6, 0.7) resulting in a statistically significant difference in increase (DD between Massachusetts and other New England states and between postreform and prereform) of 4.6% (95% CI = 3.6, 5.6; P < 0.001; Table 3).
FIGURE 1—
Changes in health insurance coverage among nonelderly adults (18–64 years), residing in Massachusetts and other New England states, between prereform (2003–2005) and postreform (2007–2009) periods.
TABLE 2—
Health Insurance Coverage and Change Between Prereform (2003–2005) and Postreform Period (2007–2009), and Massachusetts and Other New England States Stratified by Proxy Measures of Health Care Need
| Massachusetts (n = 60 388) |
Other New England States (n = 122 464) |
||||||
| Variable | 2007–2009 Postreform, % (95% CI) | 2003–2005 Prereform, % (95% CI) | Differences and DD,a % (95% CI) | 2007–2009 Postreform, % (95% CI) | 2003–2005 Prereform, % (95% CI) | Differences and DD,a % (95% CI) | DDb and DDD,c % (95% CI) |
| All (n = 182 852) | 93.9 (93.4, 94.3) | 88.7 (88.0, 89.3) | 5.2** (4.4, 6.1) | 87.9 (87.4, 88.3) | 87.2 (86.7, 87.6) | 0.7* (0.1, 1.3) | 4.5** (3.5, 5.6) |
| Mentally unhealthy days | |||||||
| ≥ 14 d (n = 21 108) | 91.9 (90.4, 93.1) | 83.2 (80.7, 85.4) | 8.7** (6.0, 11.4) | 83.3 (81.8, 84.6) | 81.4 (79.8, 82.9) | 1.8 (-0.3, 4.0) | 6.8** (3.4, 10.3) |
| < 14 d (n = 159 629) | 94.3 (93.8, 94.7) | 89.4 (88.7, 90.1) | 4.9** (4.1, 5.7) | 88.5 (88.0, 88.9) | 88.0 (87.5, 88.4) | 0.5 (-0.2, 1.1) | 4.4** (3.3, 5.5) |
| Differences and DDd | -2.4** (-3.8, -1.0) | -6.2** (-8.6, -3.8) | 3.8* (1.0, 6.6) | -5.2** (-6.7, -3.7) | -6.6** (-8.2, -4.9) | 1.4 (-0.9, 3.6) | 2.4 (-1.2, 6.0) |
| Physically unhealthy days | |||||||
| ≥ 14 d (n = 18 982) | 93.1 (91.7, 94.2) | 87.0 (84.7, 89.1) | 6.1** (3.5, 8.6) | 84.0 (82.3, 85.5) | 83.8 (82.2, 85.3) | 0.2 (-2.0, 2.4) | 5.9** (2.5, 9.2) |
| < 14 d (n = 161 925) | 94.1 (93.6, 94.5) | 88.8 (88.1, 89.5) | 5.3** (4.4, 6.1) | 88.3 (87.8, 88.8) | 87.6 (87.2, 88.1) | 0.7* (0.0, 1.3) | 4.6** (3.6, 5.7) |
| Differences and DDc | -1.0 (-2.3, 0.4) | -1.8 (-4.1, 0.5) | 0.8 (-1.9, 3.5) | -4.3** (-5.9, -2.6) | -3.8** (-5.4, -2.2) | -0.5 (-2.8, 1.8) | 1.3 (-2.3, 4.8) |
| Activity limitation days | |||||||
| ≥ 14 d (n = 13 086) | 93.2 (91.5, 94.6) | 83.7 (80.1, 86.8) | 9.5** (5.8, 13.2) | 84.0 (82.1, 85.8) | 83.6 (81.6, 85.4) | 0.5 (-2.1, 3.1) | 9.0** (4.5, 13.5) |
| < 14 d (n = 168 602) | 94.0 (93.6, 94.5) | 89.0 (88.3, 89.7) | 5.1** (4.2, 5.9) | 88.2 (87.7, 88.6) | 87.4 (87.0, 87.9) | 0.7* (0.1, 1.4) | 4.3** (3.3, 5.4) |
| Differences and DDd | -0.9 (-2.5, 0.8) | -5.3,** (-8.7, -1.9) | 4.4* (0.6, 8.2) | -4.1** (-6.0, -2.2) | -3.9** (-5.8, -1.9) | -0.2 (-2.9, 2.5) | 4.7* (0.0, 9.3) |
Note. CI = confidence interval; DD = difference-in-differences; DDD = difference-in-difference-in-differences. Coverage percentages represent unadjusted estimates.
Difference-in-differences (postreform minus prereform).
Difference-in-differences (Massachusetts minus other New England states).
Difference-in-difference-in-differences (DDb ≥ 14 days minus DDd < 14 days).
Difference-in-differences (≥ 14 days minus < 14 days).
*P < .05; **P < .001.
TABLE 3—
Health Insurance Coverage and Change Between Prereform (2003–2005) and Postreform Period (2007–2009), and Massachusetts and Other New England States Stratified by Proxy Measures of Perceived Health
| Massachusetts (n = 60 388), % (95% CI) |
Other New England States (n = 122 464), % (95% CI) |
||||||
| Variable | 2007–2009 Postreform, % (95% CI) | 2003–2005 Prereform, % (95% CI) | Differences and DD,a % (95% CI) | 2007–2009 Postreform, % (95% CI) | 2003–2005 Prereform, % (95% CI) | Differences and DD,a % (95% CI) | DDb and DDD,c % (95% CI) |
| All (n = 182 852) | 94.0 (93.6, 94.4) | 89.4 (88.8, 90.0) | 4.7** (3.9, 5.4) | 87.2 (86.7, 87.6) | 87.1 (86.7, 87.5) | 0.1 (-0.6, 0.7) | 4.6** (3.6, 5.6) |
| Mentally unhealthy days | |||||||
| ≥ 14 d (n = 21 108) | 93.2 (92.1, 94.3) | 87.1 (85.3, 88.9) | 6.1** (3.9, 8.2) | 85.0 (83.7, 86.3) | 84.1 (82.7, 85.5) | 0.9 (−1.1, 2.8) | 5.2** (2.3, 8.1) |
| < 14 d (n = 159 629) | 94.2 (93.8, 94.7) | 89.8 (89.1, 90.4) | 4.5** (3.7, 5.3) | 87.6 (87.0, 88.0) | 87.6 (87.2, 88.1) | -0.1 (-0.8, 0.6) | 4.6** (3.6, 5.6) |
| Differences and DDd | -1.1 (-2.3, 0.2) | -2.6* (-4.6, -0.7) | 1.6 (-0.7, 3.9) | -2.6** (-4.0, -1.2) | -3.5** (-5.0, -2.1) | 1.0 (-1.1, 3.0) | 0.6 (-2.0, 3.3) |
| Physically unhealthy days | |||||||
| ≥ 14 d (n = 18 982) | 94.1 (93.7, 94.5) | 88.7 (86.9, 90.6) | 5.3** (3.1, 7.6) | 84.4 (82.9, 85.9) | 84.6 (83.1, 86.0) | -0.2 (-2.3, 1.9) | 5.5** (2.4, 8.6) |
| < 14 d (n = 161 925) | 94.1 (93.7, 94.5) | 89.4 (88.8, 90.1) | 4.7** (3.9, 5.4) | 87.5 (87.0, 88.0) | 87.5 (87.1, 87.9) | -0.0 (-0.6, 0.7) | 4.6** (3.6, 5.6) |
| Differences and DDd | -0.0 (-1.3, 1.0) | -0.7 (-2.7, 1.3) | 0.7 (-1.7, 3.0) | -3.2** (-4.8, -1.6) | -2.9** (-4.4, -1.5) | -0.2 (-2.4, 2.0) | 0.9 (-2.4, -4.1) |
| Activity limitation days | |||||||
| ≥ 14 d (n = 13 086) | 94.4 (93.1, 95.8) | 86.8 (84.1, 89.5) | 7.7** (4.7, 10.6) | 84.8 (83.0, 86.6) | 85.0 (83.1, 86.8) | -0.1 (-2.7, 2.5) | 7.7** (3.8, 11.7) |
| < 14 d (n = 168 602) | 94.1 (93.6, 94.5) | 89.6 (88.9, 90.2) | 4.5** (3.7, 5.2) | 87.4 (86.9, 87.9) | 87.3 (86.9, 87.7) | 0.1 (-0.6, 0.7) | 4.4** (3.4, 5.4) |
| Differences and DDd | 0.4 (-1.0, 1.8) | -2.8* (-5.5, 0.0) | 3.2* (0.1, 6.2) | -2.6** (-4.4, -0.7) | -2.4** (-4.2, -0.5) | -0.2 (-2.8, 2.5) | 3.4 (-0.7, 7.4) |
Note. CI = confidence interval; DD = difference-in-differences; DDD = difference-in-difference-in-differences. Adjusted for control variables in multivariate models: age, gender, race/ethnicity, educational attainment, marital status, and employment status.
Difference-in-differences (postreform minus prereform).
Difference-in-differences (Massachusetts minus other New England states).
Difference-in-difference-in-differences (DDb ≥ 14 days minus DDc < 14 days).
Difference-in-differences (≥ 14 days minus < 14 days).
*P < .05; **P < .001.
The unadjusted percentages of health insurance coverage in Massachusetts increased statistically significantly (P < .001) from the prereform period to the postreform period for those with more or less MUDs, PUDs, and ALDs (range = 4.9%–9.5%; Table 2). Adjusting for potential confounders somewhat attenuated these increases over time but remained statistically significant (P < .001; range = 4.5%–7.7%; Table 3). In other New England states, health care coverage increased statistically significantly over time only for those with PUD- (0.7%; 95% CI = 0.0, 1.3; P < .05) and those with ALD- (0.7%; 95% CI = 0.1, 1.4; P < .05); after adjustment, these increases were no longer statistically significant (Table 3).
Both before and after adjustment, the increase in health insurance coverage over time in Massachusetts significantly exceeded that for other New England states among all groups of perceived health (those with more or fewer MUDs, PUDs, and recent ALDs; unadjusted increases from 4.3% to 9.0% [Table 2] and adjusted increases from 4.4% to 7.7% [Table 3], both statistically significant at P < .001).
Before reform in Massachusetts, the difference in health insurance coverage between those with MUD+ and MUD- was −6.2% (95% CI = −8.6, −3.8), and between those with ALD+ and ALD- was −5.3% (95% CI = −8.7, −1.9; P < .001; Table 2). After adjustment, these differences were attenuated for MUDs (–2.6%; 95% CI = −4.6, −0.7; P < .05) and for recent ALDs (–2.8%; 95% CI = −5.5, 0.0; P < .05; Table 3).
After reform in Massachusetts, health insurance coverage for only those with MUD+ (91.9%; 95% CI = 90.4, 93.1) remained lower than that for those with MUD- (94.3%; 95% CI = 93.8, 94.7), a statistically significant difference of −2.4% (95% CI = −3.8, −1.0; P < .001; Table 2); after adjustment for potential confounders this difference was attenuated and no longer statistically significant (–1.1%; 95% CI = −2.3, 0.2; Table 3). After the Massachusetts reform, in other New England states, health insurance coverage among those with MUD+ (83.3%; 95% CI = 81.8, 84.6), PUD+ (84.0%; 95% CI = 82.3, 85.5), and ALD+ (84.0%; 95% CI = 82.1, 85.8) remained significantly less than that among those with MUD- (88.5%; 95% CI = 88.0, 88.9), PUD- (88.3%; 95% CI = 87.8, 88.8), and ALD- (88.2%; 95% CI = 87.7, 88.6) with statistically significant differences of −5.2% (95% CI = −6.7, −3.7), −4.3% (95% CI = −5.9, −2.6), and −4.1% (95% CI = −6.0, −2.2), respectively (Table 2); adjustment for potential confounders reduced all these differences about 2%, but these differences remained statistically significant (Table 3).
In Massachusetts, health insurance coverage increased statistically significantly over time for those with MUD+ (8.7%; 95% CI = 6.0, 11.4) than those with MUD- (4.9%; 95% CI = 4.1, 5.7; P < .001), for those with PUD+ (6.1%; 95% CI = 3.5, 8.6) than those with PUD- (5.3%; 95% CI = 4.4, 6.1; P < .001), and for those with ALD+ (9.5%; 95% CI = 5.8, 13.2) than those with ALD- (5.1%; 95% CI = 4.2, 5.9; P < .001; Table 2); adjustment for potential confounders attenuated these increases over time, but these increases remained statistically significant (P < .001; Table 3). In other New England states, health insurance coverage increased statistically significantly for those with PUD- (0.7; P < .05) and those with ALD- (0.7; P < .05; Table 2), but after adjustment, these increases were not statistically significant (Table 3).
Health insurance coverage in Massachusetts increased statistically significantly (P < .001) more than that in other New England states from before the Massachusetts reform to after this reform overall (4.5%; 95% CI = 3.5, 5.6; P < .001); in groups with MUD+ (6.8%; 95% CI = 3.4, 10.3; P < .001) and MUD- (4.4%; 95% CI = 3.3, 5.5; P < .001); in groups with PUD+ (5.9%; 95% CI = 2.5, 9.2; P < .001) and PUD- (4.6%; 95% CI = 3.6–5.7; P < .001); and in groups with ALD+ (9.0%; 95% CI = 4.5, 13.5; P < .001) and ALD- (4.3%; 95% CI = 3.3, 5.4; P < .001). These statistically significant increases persisted after adjustment.
DISCUSSION
We found that health care coverage increased markedly and statistically significantly in Massachusetts between 2006 and 2010 after passage of a health reform law, the Act Providing Access to Affordable, Quality, Accountable Health Care, than in other New England states. This increase was strong and statistically significant for those most in need of health care such as individuals reporting poor mental health, poor physical health, and more limitations in their activities because of poor physical or mental health. By comparing changes in health insurance coverage before and after reform, between Massachusetts, where this reform occurred, and other New England states where it did not, and after adjusting for sociodemographic factors affecting health insurance coverage, the evidence indicates that these increases in health care coverage in Massachusetts may have resulted from the health reform enacted there. An additional 5.24% of the nonelderly adult population in Massachusetts received new health insurance coverage between prereform (2003–2005) and postreform (2007–2009) periods, and an additional 0.71% of the nonelderly adults in other New England states received such coverage during the same period.
Results from this study suggest that populations with poorer perceived health (MUD+, PUD+, and ALD+) were more likely to purchase insurance than those with better perceived health (MUD-, PUD-, and ALD-). Previous research suggests that insurance companies have been more likely to deny or charge more for health insurance to those with preexisting conditions.36 This practice results in a pool of uninsured persons, comprised of young healthy individuals self-selecting to forgo health insurance coverage, those with pre-existing conditions who have been denied health insurance coverage, and those who cannot afford the premiums for health insurance coverage. Because health insurance coverage in subpopulations with poor mental health and limited activities because of poor physical or mental health increased disproportionately after health care reform in Massachusetts compared with other New England states, it is possible such a practice may have existed before this reform took place.
Because this study included only the nonelderly adult population (because most of those aged 65 years and older have health insurance coverage under Medicare) and aggregated over the prereform and postreform periods, it is not directly comparable with the other studies cited earlier. Furthermore, another BRFSS-based study that used additional state-added questions (not asked by other states) reported higher health insurance coverage than this study based on the single question in the BRFSS core questionnaire.13 In our study, 88.7% of Massachusetts nonelderly adult residents had coverage before reform, compared with 87.2% in other New England states, but well above that in most other states, possibly an advantage for Massachusetts in achieving high absolute compliance. The postreform insurance estimate of 93.9% among nonelderly adults in Massachusetts varies from other estimates of 97.4%37 to 96.3%13 to 95.2%16 possibly because of differences in survey design including coverage, reference period, mode, and questionnaire design.20–22 Nevertheless, the change in coverage in this study is about the same size and in the same direction as that in other studies.12–16 Even though the federal and Massachusetts subsidy and penalty structure for obtaining health care coverage differ, given the high compliance rate as a result of the Massachusetts individual mandate, there are enough similarities between the 2 programs to suggest the future degree of health care coverage in all states.
The BRFSS health insurance coverage estimates appear comparable for the overall population and selected demographic and socioeconomic characteristics to those in other federal surveys that gather data on such coverage—ACS, CPS ASEC, and NHIS. However, as postsurvey adjustments are becoming an increasingly important means of maintaining the representativeness of survey data commencing with the release of the 2011 BRFSS data, statistical raking techniques and postsurvey adjustments to match ACS will be used making the health insurance point estimates even closer. This new approach adjusts the data not only in terms of respondents’ gender and age, but also race (in a more consistent manner), education, and telephone coverage—variables all found to be significantly related to key health insurance coverage, health, and risk outcomes on BRFSS.38
Studies based on BRFSS data have several limitations. First, they represent only households with landline telephones but exclude cell phone–only households and households without telephones. Second, because BRFSS data depend on responses of survey participants, recall bias and biases related to the perceived social desirability of certain responses may affect their accuracy. Overall BRFSS response rates were low and have decreased between 2003 and 2009, though this decrease was similar in Massachusetts and other New England states. Despite these limitations, other BRFSS estimates have been shown to be valid and reliable when compared with estimates derived from national household survey data39,40 The BRFSS surveys are a cost-effective and timely means of collecting state and local data, and BRFSS data are often the only data source with which states and communities can assess local health conditions and track progress toward improving those conditions.
An analytic concern stems from possible differential effects of the deep and long recession that began in the United States in December 2007 and ended in June 2009, as determined by the US National Bureau of Economic Research.41 During the recession employer-sponsored health insurance coverage declined, contributing to a steady rise in the uninsured, an estimated 56.4 million in 2008, 58.7 million in 2009, and 59.1 million in the first quarter of 2010.42 States also have varying eligibility requirements for Medicaid. However, according to the Bureau of Economic Analysis and the Bureau of Labor Statistics, although the recession had differential effects across the nation, the impact on gross domestic product17 and on unemployment rates18 across all New England states (with the exception of Rhode Island, which experienced a disproportionately higher unemployment rate) were comparable, precluding the need to control for such economy-related area-level variables or conducting multilevel analysis.
This study indicates that if the health care coverage trends observed in the natural experiment in Massachusetts foreshadow what will occur in the United States following full implementation of the ACA, the rate of decrease in health insurance coverage will be slowed and an increase in health insurance coverage is predicted.6 Meanwhile, the Massachusetts experience may continue to offer lessons for national health reform efforts.
Acknowledgments
We acknowledge and thank Lydia Ogden, PhD, Senior Policy Advisor, Office of Prevention Through Healthcare, Centers for Disease Control and Prevention, for reading earlier versions of this article and making suggestions. We also acknowledge and thank Elena Hawk, PhD, Behavioral Risk Factor Surveillance System Coordinator, Massachusetts Department of Public Health, for her suggestions.
Human Participant Protection
No institutional review board approval was needed because this study involved analyses of secondary deidentified data.
References
- 1.Chapter 58: An Act Providing Access to Affordable, Quality, Accountable Health Care. The 186th General Court of the Commonwealth of Massachusetts. Available at: http://www.malegislature.gov/Laws/SessionLaws/Acts/2006/Chapter58. Accessed January 14, 2011. [Google Scholar]
- 2.Patient Protection and Affordability Act. Pub L No. 111–148 (March 23, 2010), 124 Stat. 119. Available at: http://www.gpo.gov/fdsys/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf. Accessed January 14, 2011.
- 3.Health Care and Education Reconciliation Act. Pub L No. 111–152 (March 30, 2010), 124 Stat. 1029. Available at: http://www.gpo.gov/fdsys/pkg/PLAW-111publ152/pdf/PLAW-111publ152.pdf. Accessed January 14, 2011.
- 4.The Commonwealth Fund. Health reform resource center. Overview timeline. Available at: http://www.commonwealthfund.org/Health-Reform/Health-Reform-Resource.aspx. Accessed January 14, 2011.
- 5.The Kaiser Family Foundation. Summary of new health reform law. Available at: http://kff.org/healthreform/upload/8061.pdf. Accessed January 14, 2011.
- 6.Letter to Honorable Nancy Pelosi from Douglas W. Elmendorf, Director of the Congressional Budget Office. RE: Estimate of the direct spending and revenue effects of an amendment in the nature of a substitute to H.R. 4872, the Reconciliation Act of 2010, March 18, 2010. Available at: http://www.cbo.gov/ftpdocs/113xx/doc11355/hr4872.pdf. Accessed January 14, 2011. [Google Scholar]
- 7.Levy H, Meltzer D. The impact of health insurance on health. Annu Rev Public Health. 2008;29:399–409 [DOI] [PubMed] [Google Scholar]
- 8.Freeman JD, Kadiyala S, Bell JF, Martin DP. The causal effect of health insurance on utilization and outcomes in adults: a systematic review of US studies. Med Care. 2008;46(10):1023–1032 [DOI] [PubMed] [Google Scholar]
- 9.Newhouse JP. A summary of the RAND health insurance study. Ann N Y Acad Sci. 1982;387:111–114 [DOI] [PubMed] [Google Scholar]
- 10.Allen H, Baicker K, Finkelstein Aet al. What the Oregon health study can tell us about expanding Medicaid. Health Aff (Millwood). 2010;29(8):1498–1506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levy H, Meltzer D. What do we really know about whether health insurance affects health? In: McLaughlin CG, ed. Health Policy and the Uninsured. Washington, DC: Urban Press; 2004 [Google Scholar]
- 12.Long SK. On the road to universal coverage: impacts of reform in Massachusetts at one year. Health Aff (Millwood). 2008;27(4):w270–w284 [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention Short-term effects of health-care coverage legislation—Massachusetts, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(9):262–267 [PubMed] [Google Scholar]
- 14.Long SK, Yemane A, Stockley K. Disentangling the effects of health reform in Massachusetts: how important are the special provisions for young adults? Session: Massachusetts Health Reform Experiment: Early Experiences. Available at: http://www.aeaweb.org/articles.php?doi=10.1257/aer.-1.2. Accessed December 5, 2012. [Google Scholar]
- 15.Kenney GM, Long SK, Luque A. Health reform in Massachusetts cut the uninsurance rate among children in half. Health Aff (Millwood). 2010;29(6):1242–1247 [DOI] [PubMed] [Google Scholar]
- 16.Long SK, Stockley K. Sustaining health reform in a recession: an update on Massachusetts as of fall 2009. Health Aff (Millwood). 2010;29(6):1234–1241 [DOI] [PubMed] [Google Scholar]
- 17.US Department of Commerce, Bureau of Economic Analysis Regional economic accounts. Available at: http://www.bea.gov/regional. Accessed November 27, 2012 [Google Scholar]
- 18.US Department of Labor, Bureau of Labor Statistics Local area unemployment statistics map. Available at: http://data.bls.gov/map. Accessed November 27, 2012 [Google Scholar]
- 19.Yelowitz A, Cannon MF. The Massachusetts Health Plan: Much pain, little gain. Policy Analysis, No. 657. Available at: http://www.cato.org/pubs/pas/pa657.pdf. Published January 20, 2010. Accessed January 14, 2011 [Google Scholar]
- 20.Long SK, Zuckerman S, Triplett T et al. Estimates of the uninsurance rate in Massachusetts from survey data: why are they so different? Available at: http://www.mass.gov/dhcfp. Published August 28, 2009. Accessed January 14, 2011. [Google Scholar]
- 21.Call KT, Davern M, Blewett LA. Estimates of health insurance coverage: comparing state surveys with the current population survey. Health Aff (Millwood). 2007;26(1):269–278 [DOI] [PubMed] [Google Scholar]
- 22.Lewis KM, Ellwood M, Czaka JL. Counting the Uninsured: A Review of the Literature. Assessing the New Federalism, Occasional Paper No. 8. Washington, DC: The Urban Institute; 1998 [Google Scholar]
- 23.Turner J, Boudreaux M, Lynch V. A preliminary evaluation of health insurance coverage in the 2008 American Community Survey. Available at: http://www.census.gov/hhes/www/hlthins/data/acs/2008/2008ACS_healthins.pdf. Published September 22, 2009. Accessed January 14, 2011 [Google Scholar]
- 24.Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System User’s Guide. Atlanta, GA: US Department of Health and Human Services; 2006. Available at: ftp://ftp.cdc.gov/pub/Data/Brfss/userguide.pdf. Accessed January 14, 2011 [Google Scholar]
- 25.Mokdad AH, Stroup DF, Giles WH. Public health surveillance for behavioral risk factors in a changing environment. Recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Recomm Rep. 2003;52(RR-9):1–12 [PubMed] [Google Scholar]
- 26.Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health. 2003;57(5):339–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dominick KL, Ahern FM, Gold CH, Heller DA. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clin Exp Res. 2002;14(6):499–508 [DOI] [PubMed] [Google Scholar]
- 28.Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s Healthy Days Measures—population tracking of perceived physical and mental health over time. Health Qual Life Outcomes. 2003;1(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51(1):95–124 [PubMed] [Google Scholar]
- 30.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10 [PubMed] [Google Scholar]
- 31.Andersen RM. National health surveys and the behavioral model of health services use. Med Care. 2008;46(7):647–653 [DOI] [PubMed] [Google Scholar]
- 32.Ashenfelter O. Estimating the effect of training programs on earnings. Rev Econ Stat. 1978;60(1):47–57 [Google Scholar]
- 33.Ashenfelter O, Card D. Using the longitudinal structure of earnings to estimate the effect of training programs. Rev Econ Stat. 1985;67(4):648–660 [Google Scholar]
- 34.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. 2nd ed Cambridge, MA: MIT Press; 2007 [Google Scholar]
- 35.Martinez ME, Cohen RA. Health insurance coverage: early release of estimates from the National Health Interview Survey, January–September 2008. Available at: http://www.cdc.gov/nchs/data/nhis/earlyrelease/insur200903.pdf. Published March 2009. Accessed December 5, 2012 [Google Scholar]
- 36.Cutler DM, Zeckhauser RJ. Adverse selection in health insurance. Available at: http://www.nber.org/papers/w6107.pdf?new_window=1. National Bureau of Economic Research working paper 6107. Published July 1997. Accessed January 14, 2011.
- 37.Long SK, Masi PB. Access and affordability: an update on health reform in Massachusetts, fall 2008. Health Aff (Millwood). 2009;28(4):w578–w587 [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System improvements to BRFSS methodology, design, and implementation. 2006. Available at: http://www.cdc.gov/brfss/pubs/methodology.htm. Accessed January 14, 2011 [Google Scholar]
- 39.Nelson DE, Holtzman D, Bolen J, Stanwyck CA, Mack KA. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS). Soz Praventivmed. 2001;46(1):S3–S42 [PubMed] [Google Scholar]
- 40.Nelson DE, Powell-Griner E, Town M, Kovar MG. A comparison of national estimates from the National Health Interview Survey and the Behavioral Risk Factor Surveillance System. Am J Public Health. 2003;93(8):1335–1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.US National Bureau of Economic Research Business Cycle Dating Committee. Available at: http://www.nber.org/cycles/sept2010.pdf. Published September 20, 2010. Accessed December 5, 2012 [Google Scholar]
- 42.Fox JB, Richards CL. Vital signs: health insurance coverage and health care utilization—United States, 2006–2009 and January–March 2010. Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2010;59(44):1448–1454 [PubMed] [Google Scholar]