Abstract
Objectives. We used the Stigma in Global Context–Mental Health Study to assess the core sentiments that represent consistent, salient public health intervention targets.
Methods. Data from 16 countries employed a nationally representative sampling strategy, international collaboration for instrument development, and case vignettes with Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition depression and schizophrenia criteria. We measured knowledge and prejudice with existing questions and scales, and employed exploratory data analysis to examine the public response to 43 items.
Results. Across countries, levels of recognition, acceptance of neurobiological attributions, and treatment endorsement were high. However, a core of 5 prejudice items was consistently high, even in countries with low overall stigma levels. The levels were generally lower for depression than schizophrenia, and exclusionary sentiments for more intimate venues and in authority-based roles showed the greatest stigma. Negative responses to schizophrenia and depression were highly correlated across countries.
Conclusions. These results challenge researchers to reconfigure measurement strategies and policymakers to reconsider efforts to improve population mental health. Efforts should prioritize inclusion, integration, and competences for the reduction of cultural barriers to recognition, response, and recovery.
A resurgence in research, programs, and policy efforts targeting prejudice and discrimination associated with mental illness has dramatically improved scientific understanding of causes, correlates, and change.1 Conceptual and methodological work has provided a solid framework for guiding research hypotheses,2–4 cross-disciplinary collaboration has accelerated scientific progress,5–7 and multifaceted approaches to stigma reduction have recently been put into play.8,9 Despite different designs, respondent groups, measures, and analytic models, results have shown a remarkable consistency in scientific conclusions (e.g., robust influence of contact on tolerance).10 Most notably, ironically, public acceptance of modern medical and public health views of mental illness appears to be coupled with a stubborn persistence of negative opinions, attitudes, and intentions.11–15 As recent path-breaking research has documented, cultures of stigma shape individual-level acceptance and rejection, reported willingness to seek treatment, and feelings of self-worth and efficacy that persons with mental illness hold.8,16
These findings have motivated renewed efforts to rethink standard approaches to stigma research and to reconsider stigma-reduction efforts aimed at improving population mental health.7,17,18 Yet, a major impediment to the next generation of effective stigma reduction programs lies in identifying the core public sentiments, or “backbone,” underlying misinformation, prejudice, and discrimination associated with mental illness. Certainly, early psychoanalytic ideas about the “schizophregenic mother,” the moral weakness of those with depression, or the inherent proclivity to violence among persons with mental illness mirror both a lack of scientific knowledge and negative appraisals. Findings have been disproportionately limited to North America and Europe and focused primarily upon schizophrenia.16,19–22 Antistigma campaigns have primarily targeted educational goals to reduce misinformation and mischaracterization of mental illness.11 Methodological differences in measurement strategies across studies hamper the development of strategically specific programs and policies.
We asked 3 fundamental questions in the service of the next generation of antistigma efforts: (1) Is there a “backbone” of larger cultural beliefs, attitudes, and opinions about mental illness that presents the greatest challenges to individuals, families, and providers? (2) Does a lack of knowledge, an unwillingness to include individuals with mental health problems in civil society, or concerns about treatment stand in the way of recovery? (3) Does the public react similarly or differently to schizophrenia and depression? We analyzed data from the Stigma in Global Context–Mental Health Study (SGC-MHS) to examine public responses to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)23 scenarios for schizophrenia and depression across 16 countries. Using multiple measures to tap ignorance, rejection, exclusion, and negative affect, we searched for those items that may form the backbone of stigma—a widely held damaging core of cultural attitudes and beliefs about causes, solutions, and inclusion.
METHODS
The SGC-MHS is a globally targeted, theoretically and methodologically coordinated study. With support from the US National Institutes of Health (Fogarty International Center, National Institute of Mental Health, Office of Behavioral and Social Science Research), the Icelandic Centre for Research, and Ghent University, we collected data from representative national samples of adults in 16 countries. The focus of this analysis was not to examine cross-national differences in detail; rather, we used the SGC-MHS global coverage and measurement detail to search for commonalities. The fielding platform was the International Social Survey Program (ISSP; http://www.issp.org), a program of cross-national survey collaboration. The ISSP countries were sent electronic invitations from the ISSP Secretariat describing the study and inclusion requirements (e.g., face-to-face administration). The participating countries represent remarkable variation geographically (at least 1 country on each inhabited continent), developmentally (high-, middle-, and low-income countries), and politically (long-term democracies and post–communist bloc countries; Table available as a supplement to the online version of this article at http://www.ajph.org). The total number of respondents in each country and the effective sample size for schizophrenia and depression are reported (SGC-MHS total n = 19 508; 6542 and 6539 of respondents receiving schizophrenia and depression vignettes, respectively). Remaining respondents receiving the “control” asthma vignette are not included here. Eligible respondents were noninstitutionalized adults (aged ≥ 18), with all national cross-sections based on multistage probability sampling methods. Trained interviewers conducted face-to-face interviews (overall SGC-MHS response rate = 65%).
The SGC-MHS interview schedule consisted of 2 parts: ISSP individual-level sociodemographic variables tailored to country differences (e.g., political systems), and 75 items on mental health and illness. We addressed cross-national comparability in 5 ways. First, a meeting of survey experts from 15 participating countries, held in Madrid in 2004, adapted a revised version of instrumentation used in the 1996 MacArthur Mental Health Study.24 Questions or response codes were added, eliminated, or changed; guidelines for tailoring to country-specific contexts were developed; items were tagged for tailoring (e.g., culturally specific religious attributions); and a staggered fielding plan across multiple years was scheduled.
Second, an outside psychiatric consultant assessed vignettes with meeting participants, and revised versions were approved by all participating countries. Third, a 2-step cultural translation process required traditional translation–back translation and a 2- to 4-hour cognitive interview with native speakers. Fourth, items with embedded cultural variation (e.g., treatment options) were modified in collaboration. For example, the American English idiom “talking behind his back” translates in Argentinian Spanish to “speaking at his shoulders” and was changed to simply “criticizing him behind his back.” Fifth, all questions were asked in blocks and in identical order.25–27
Schizophrenia and Depression Vignettes
Respondents evaluated 1 randomly assigned vignette describing a person meeting criteria for a DSM-IV or International Classification of Diseases and Related Health Problems, Tenth Revision diagnosis of either major depression or schizophrenia.23,28 No labels were offered. The US vignette versions, with random variation by gender and race, were:
Schizophrenia.
John/Mary [White]/Tyrone/Shontell [Black] is a White/Black man/woman. Up until a year ago, life was pretty okay for John/Mary/Tyrone/Shontell. But then, things started to change. He/She thought that people around him/her were making disapproving comments, and talking behind his/her back. John/Mary/Tyrone/Shontell was convinced that people were spying on him/her and that they could hear what he/she was thinking. John/Mary/Tyrone/Shontell lost his/her drive to participate in his/her usual work and family activities and retreated to his/her home, eventually spending most of his/her time on his/her own. John/Mary/Tyrone/Shontell became so preoccupied with what he/she was thinking that he/she skipped meals and stopped bathing regularly. At night, when everyone else was sleeping, he/she was walking back and forth at home. John/Mary/Tyrone/Shontell was hearing voices even though no one else was around. These voices told him/her what to do and what to think. He/She has been living this way for 6 months.
Depression.
John/Mary [White]/Tyrone/Shontell [Black] is a White/Black man/woman. For the last several weeks, John/Mary/Tyrone/Shontell has been feeling really down. He/she wakes up in the morning with a sad mood and a heavy feeling that sticks with him/her all day long. He/she isn’t enjoying things the way he/she normally would. In fact nothing gives him/her pleasure. Even when good things happen, they don’t seem to make John/Mary/Tyrone/Shontell happy. The smallest tasks are difficult to accomplish. He/she finds it hard to concentrate on anything. He/she feels out of energy, out of steam, and cannot do things he/she usually does. And even though John/Mary/Tyrone/Shontell feels tired, when night comes he/she can’t go to sleep. John/Mary/Tyrone/Shontell feels pretty worthless, very discouraged, and guilty. John’s/Mary’s/Tyrone’s/Shontell’s family has noticed that he/she has lost appetite and weight. He/she has pulled away from them and just doesn’t feel like talking.
Stigma as Lack of Knowledge
Sixteen items tapped into respondent knowledge. One item measured perceived severity (1 = very or somewhat serious; 0 = not very or not at all serious). Six questions measured attributions: “Is it very likely, somewhat likely, not very likely, not at all likely that [Name’s] situation is caused by…”: bad character, a brain disease, the way he or she was raised, genetics, God’s will, and bad luck. All questions had 4 responses recoded to 1 = likely; 0 = not likely. Items tapped problem recognition: “How likely do you think that [Name] is experiencing a mental illness?” and the same for “physical illness” (recoded to 1 = likely; 0 = not likely).
Respondents were asked whether they thought the vignette situation was schizophrenia or depression (recoded to 1 = correctly identified; 0 = otherwise). Treatment endorsements asked whether the situation would improve on its own and with treatment (recoded to 1 = likely; 0 = not likely). They also rated the importance of seeking help from doctors, psychiatrists, counselors, or religious leaders (10-point scale responses recoded to a dichotomy: ≥ 6 = 1 [yes]; ≤ 5 = 0 [no]).
Stigma as Prejudice
Seven widely used scales were divided into 27 individual items. The scales were:
social distance—the reluctance to interact with members of devalued groups29,30;
traditional prejudice—adherence to the belief that all members of the “marked” group are categorically inferior to others31–33;
exclusionary sentiments—the willingness to reject persons with mental illness from the full benefits of citizenship34,35;
negative affect—popular public views that people with mental illness are difficult to interact with36,37;
perceptions of dangerousness—fear that persons with mental illness represent a threat for violence to self and others19,38,39;
treatment carryover—assessments that being known to have received mental health care carries long-lasting consequences2,40,41; and
disclosure spillover—negative consequences of revealing mental illness.37
Specific items are provided in Figures 1 and 2.
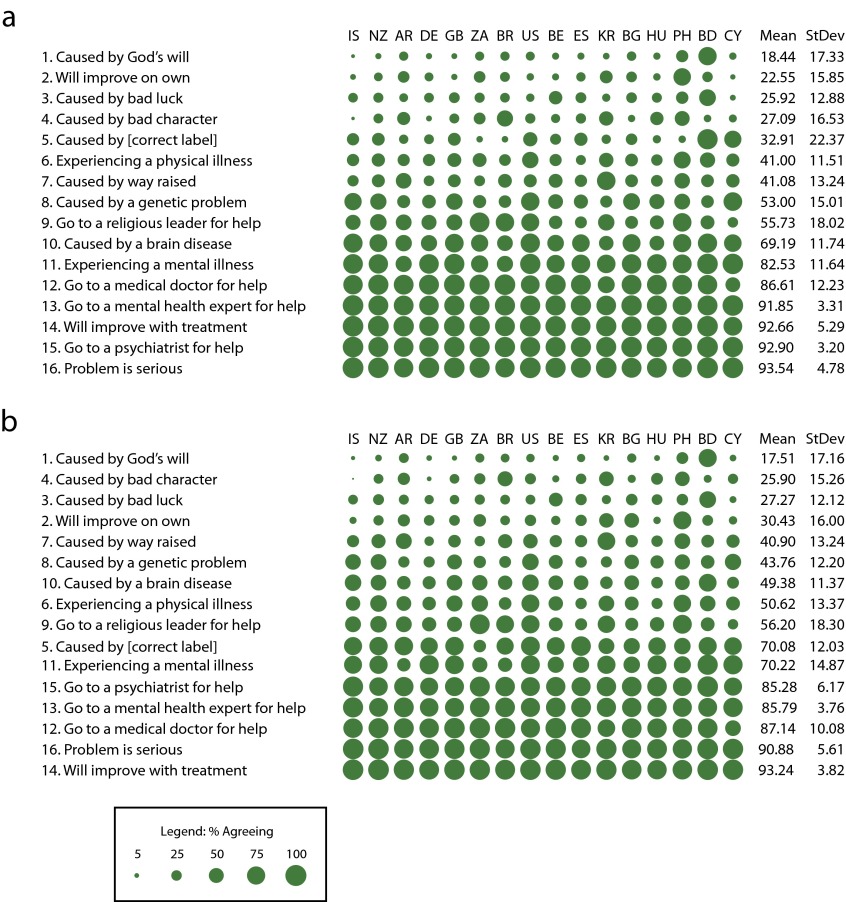
FIGURE 1—
Public response on mental health knowledge, beliefs, and treatment endorsements for (a) schizophrenia and (b) depression: Stigma in Global Context–Mental Health Study, 2004–2012.
Note. AR = Argentina (South America; n = 1420); BD = Bangladesh (Asia; n = 1501); BE = Belgium (Europe; n = 1166); BG = Bulgaria (Europe n = 1121); BR = Brazil (South America; n = 1522); CY = Cyprus (Europe; n = 804); DE = Germany (Europe; n = 1255); ES = Spain (Europe; n = 1206); GB = Great Britain (Europe; n = 1030); HU = Hungary (Europe; n = 1252); IS = Iceland (Europe; n = 1033); KO = South Korea (Asia; n = 1003); NZ = New Zealand (Australia; n = 1020); PH = Philippines (Asia; n = 1200); US = United States (North America; n = 1425); ZA = South Africa (Africa; n = 1550). Area of circle corresponds to percentage agreeing on each item in each country. Items are ordered from low to high according to across-country mean percentage agreeing (second-to-last column) and countries are ordered from low to high according to across-item mean percentage stigmatizing. The sample sizes were n = 6542 for schizophrenia and n = 6539 for depression.
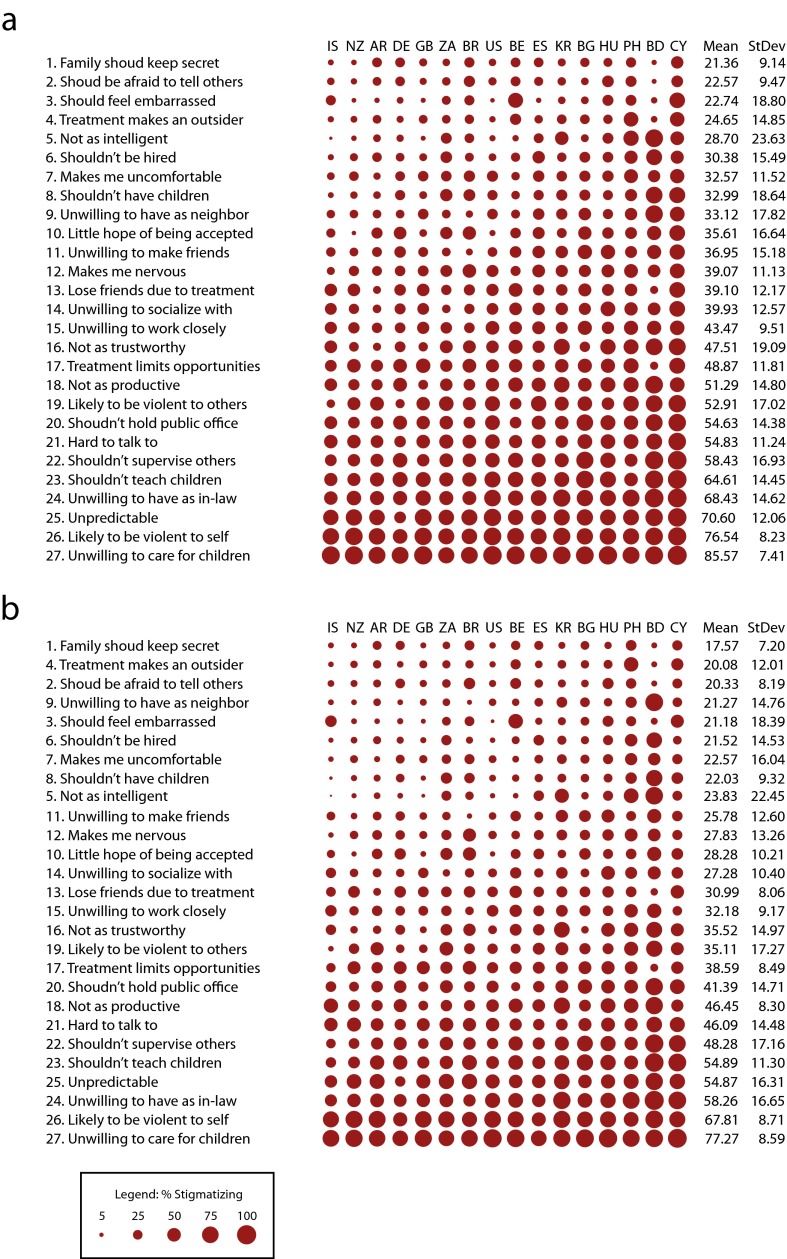
FIGURE 2—
Public response to stigma items for (a) schizophrenia and (b) depression: Stigma in Global Context–Mental Health Study, 2004–2012.
Note. AR = Argentina (South America; n = 1420); BD = Bangladesh (Asia; n = 1501); BE = Belgium (Europe; n = 1166); BG = Bulgaria (Europe n = 1121); BR = Brazil (South America; n = 1522); CY = Cyprus (Europe; n = 804); DE = Germany (Europe; n = 1255); ES = Spain (Europe; n = 1206); GB = Great Britain (Europe; n = 1030); HU = Hungary (Europe; n = 1252); IS = Iceland (Europe; n = 1033); KO = South Korea (Asia; n = 1003); NZ = New Zealand (Australia; n = 1020); PH = Philippines (Asia; n = 1200); US = United States (North America; n = 1425); ZA = South Africa (Africa; n = 1550). Area of circle corresponds to percentage stigmatizing on each item in each country. The sample sizes were n = 6542 for schizophrenia and n = 6539 for depression.
We measured all individual items via a Likert-type strategy (i.e., strongly agree, agree, disagree, strongly disagree), and collapsed them into dichotomies (endorsement of a stigmatizing response coded as 1; rejection coded as 0).
Analysis
We used an exploratory data analysis42 approach. For each stigma variant, we calculated the percentage of respondents agreeing within each country. A grand mean and standard deviation for each item averaged item scores and are presented as column marginals. Values are represented graphically by circles, where the circle size (i.e., area) varies in direct proportion to the percentage agreeing with the statement. Thus, larger circles indicate stigmatizing items with greater cultural prevalence (Raw percentages can be found in in a supplement to the online version of this article at http://www.ajph.org).
Scatter plots with Pearson correlation (r) examined the similarity and differences in the public’s assessment of schizophrenia and depression. We based correlations on the level of correspondence between the 2 cases for each knowledge item and prejudice item (n = 16 and 27, respectively).
RESULTS
In Figures 1a and 2a, items are sorted and numbered from low to high by the grand mean. The same item numbers are used in Figures 1b and 2b to facilitate comparison. In all figures, countries are presented left to right, by increasing overall level of stigmatizing response for depression and schizophrenia combined.
Stigma as Ignorance and Misinformation
For schizophrenia, Figure 1a reveals 4 items (items 13–16) with the greatest public endorsement, measured by highest percentage endorsing the items, coupled with the lowest overall variation. Across countries, recognition of severity, endorsement of psychiatry, acknowledged efficacy of treatment, and endorsement of mental health professionals (e.g., counselors, psychologists) were widely embraced. A second set of 3 items (items 10–12: use of general physicians, identification of a “mental illness,” and endorsing a disease attribution) were reported with somewhat lower endorsement, greater variability, or both. This total set of 7 items, associated with “modern” or “scientific” assessments, was endorsed by more than two thirds of the population in each country, even where general education levels are relatively low.
Furthermore, there was low or variable endorsement of traditional stigmatizing attributions (e.g., bad character, bad luck, God’s will; see Bangladesh and the Philippines as exceptions). A major problem appears in the public’s inability to recognize the vignette (item 5) as “schizophrenia” (i.e., greater differences in the percentage and variance providing a correct “label”). Fewer than half of respondents endorsed this item; however, Bangladesh, along with Cyprus, stand out as exceptions.
For depression (Figure 1b), the same 6 items received endorsement from the highest percentage of individuals across all countries, though the ordering differs slightly in rank (in order: items 14, 16, 12, 13, 15, 11). Unlike schizophrenia, endorsement of a “general medical doctor” (item 12) elicited a positive response from a large percentage of respondents but with greater variability. Each item drew endorsements from more than two thirds of respondents.
Two differences stand out for depression compared with schizophrenia. First, relatively more respondents could correctly identify depression (item 5; grand mean = 70.08% vs 32.91% for schizophrenia); and attribution to a “brain disease or disorder” (item 10) received less support (grand mean = 49.38% vs 69.19% for schizophrenia). The least endorsed items were, again, those attributions reflecting stigmatizing attitudes (see Bangladesh as an outlier).
Stigma as Social Rejection and Devaluation
Figure 2a reveals that the highest levels of stigmatizing responses were concentrated in 5 items endorsed by nearly two thirds or more of respondents (items 27–23): child care provider, potential for violence (self-directed), unpredictability, marry into family, and teach children. The next 5, with more than half of respondents endorsing, targeted authority, civic responsibility, and perceived life chances (supervise at work, public office, productivity), as well as interactional barriers or concerns (difficult to talk to, violent to others). The lowest levels of public stigma were associated with disclosure (secrecy, afraid to tell, embarrassment), treatment carryover (outsider), basic civil rights (hire if qualified), and intelligence.
Figure 2b, on depression, provides evidence of notably lower levels of stigmatizing responses. However, with some switching in rank ordering, the 7 most widely held items in terms of stigma of rejection and devaluation are the same as for schizophrenia. However, only 2 items—unwillingness to have the vignette person as a childcare provider, or to believe that an individual described with symptoms consistent with clinical depression is likely to self-harm—reached the two thirds of the population mark (items 26 and 27). Unpredictability and rejection in the family sphere through intermarriage were also lower on average, as with schizophrenia. The data also revealed fairly similar low stigmatizing responses on issues of disclosure, treatment carryover, and inclusion (in order: items 1, 4, 2, 3, 6). In addition, the unwillingness to have the vignette person as a neighbor did not elicit a negative response at the same place in rank ordering as schizophrenia (position 4 vs 9, respectively).
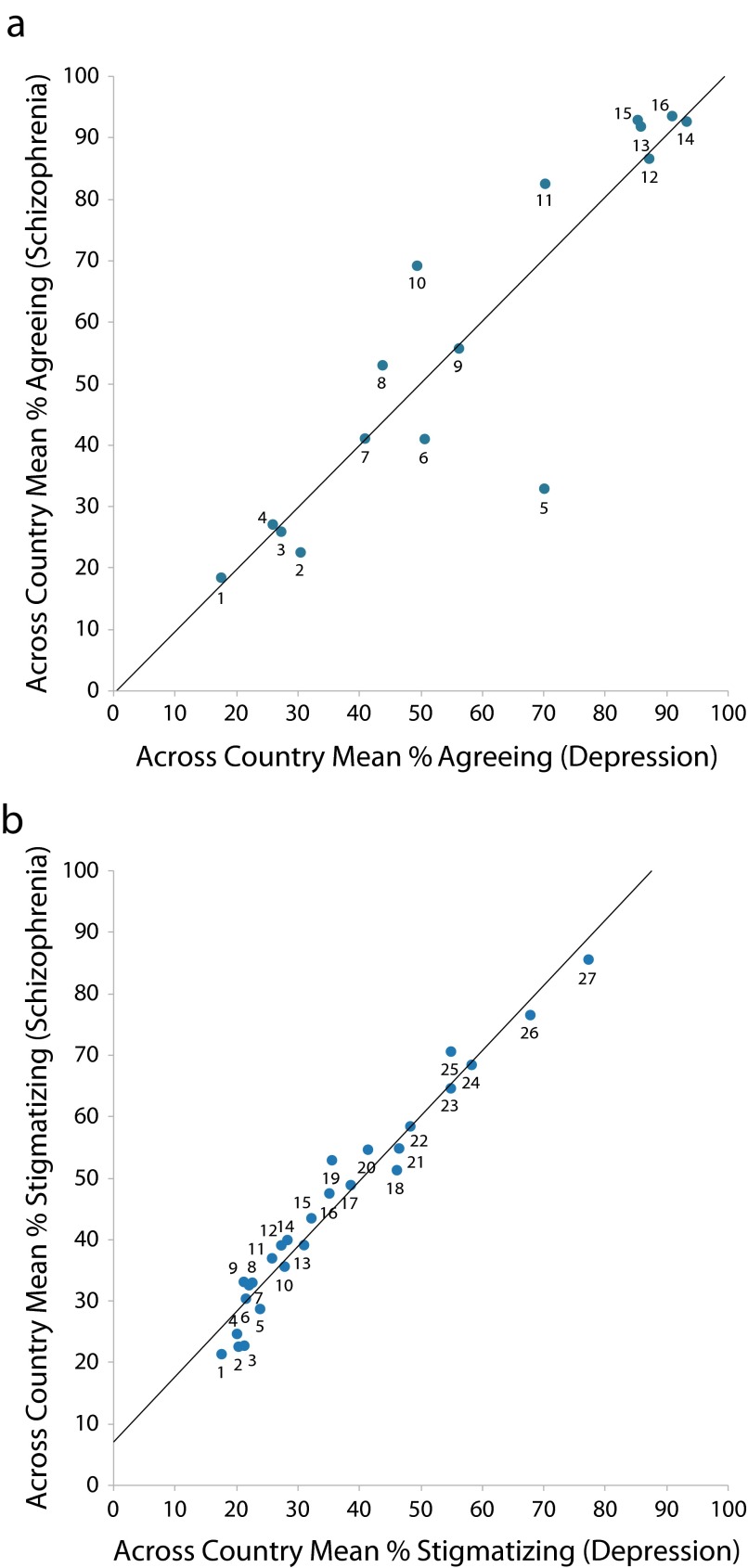
Public Response to Schizophrenia vs Depression
Figure 3 reinforces the similarity of ranking results. Scatterplots of stigma items tapping ignorance (Figure 3a; r = 0.90; df = 14; P < .001) and rejection or devaluation issues (Figure 3b; r = 0.98; df = 25; P < .001) show remarkable correspondence for schizophrenia and depression. Differences appear to be on knowledge, rather than prejudice issues. The correct identification of depression was significantly higher than for schizophrenia (item 5). Yet, the public was more likely to see schizophrenia as a mental illness and as caused by a brain disease (items 11 and 10; Figure 3a).
FIGURE 3—
Correlation of schizophrenia and depression across country item means for (a) knowledge, beliefs, and treatment endorsement items and (b) stigma items: Stigma in Global Context–Mental Health Study, 2004–2012.
Note. The sample sizes were n = 16 for knowledge, beliefs, and treatment endorsement items and n = 27 for stigma items.
Figure 3b reveals very small differences in the public response to prejudice and devaluation for these 2 scenarios except for respondents endorsing stigma items for depression. Because respondents did not receive both vignettes, but only 1 randomly, these results do not reflect acquiescence bias or other methodological confounds.
DISCUSSION
Because large-scale, representative population-based studies on public stigma tap into the cultural climate in which individuals experience and respond to mental health problems, they offer one scientific foundation to recalibrate community targets and messages of change. The SGC-MHS provides a global analysis of the nature of public stigma. The SGC-MHS does not represent a randomly selected set of countries, nor do the vignettes incorporate the spectrum of symptoms within mental health disorders. However, when we focused on schizophrenia and depression, we aimed to (1) examine the robustness of previous findings, (2) reconfigure our understanding of the backbone or core sentiments underlying stigma, and (3) provide new directions for change. The focus here was on similarities and differences in the public response to many dimensions of stigma and did not focus on cross-national differences in any detailed manner.
Thus, though not without limitations, our descriptive, cross-national findings reinforce and generalize recent past research while offering novel insights. Essentially, stepping back to reconsider the dimensions of culture that have been used to measure stigma, we divided issues into 2 types to reflect the division between mental health knowledge (ignorance, misinformation) and prejudice (rejection, devaluation). We did not use these indicators as traditional summative scales; rather, we employed them as single items to search for the backbone of stigma across societies. Four basic findings stand out.
First, in line with other recent studies that focused on a smaller scale or a single country, the majority of the public has received, and at least tacitly endorses, ideas about the severity of mental illness and accepts its underlying causes as located in the same realm as other illnesses. They reject old etiological notions of individual weakness, secrecy, and moral failure, reporting that treatment should be sought.
Second, there does appear to be a backbone of stigma. Even in countries with more accepting cultural climates, issues that deal primarily with intimate settings (the family), vulnerable groups (children), or self-harm elicit the greatest amount of negative response. A secondary core targets the unwillingness to see individuals with mental illness in positions of authority or power (work supervisors, public officials) and uneasiness about how to interact with or whether to fear violence from individuals with mental health problems. What seems to draw concern from a smaller segment of the public are issues of disclosure (secrecy, embarrassment), basic civil rights (hire if qualified), competence (intelligence), and less intimate social venues (neighbor).
Third, the public responds differently to schizophrenia and depression, but this appears to be in terms of level rather than rank. The same issues, with some slight rearrangement, elicit negative or positive responses from the most, the moderate, and the least percentage of respondents. A few differences on recognition indicate that schizophrenia is likely to be seen by more people as mental illness or a brain disorder, yet less likely to be correctly identified as a specific disorder.
Fourth, although not explored in depth, and despite the existence of core sentiments, there is cross-national variability. Responses on both literacy and prejudice call for greater examination for overall country profiles and also for specific outliers (e.g., God’s will in Bangladesh).43,44
We agree with our Canadian and British colleagues18,22: the main challenge that lies ahead is to identify the interventions that will produce behavior changes in individuals, families, and societies to decrease discrimination against people with mental illness. However, we reassert that, without a scientific base of evaluation, novel assessment, and routine monitoring, these efforts, like stigma itself, are based on assumptions, beliefs, and hopes. Even the best and most well-intentioned efforts may be a poor fit with the actual challenges faced by individuals, families, medical providers, and public health practitioners. Efforts may use messages or approaches that do not target, let alone break the backbone of, core sentiments underlying rejection and intolerance.
Our findings reinforce recent conclusions that individuals endorse the “modern” understandings of the etiology of mental illness, making traditional educational campaigns focusing on mental illness as a “real” disease a low priority.11,13,15 If the public understands that mental illnesses are medical problems but still reject individuals with mental illness, then educational campaigns directed toward ensuring inclusion become more salient. Although legal prescriptions that bar exclusion coupled with legal proscriptions to prevent or punish those who violate them may be in order, our results indicate that traditional civil rights targets (e.g., hire if qualified) already translate into fewer individuals endorsing rejection. The more difficult targets tap into deeper dimensions of recovery. That is, concerns with trust in work and family settings may signal a rejection of the fundamental idea that individuals with mental illness can get better, living full and complete lives in spite of their illness.45
Although a long tradition of research has indicated that attitudes do not necessarily translate into behaviors, we have 2 important pieces of recent scientific information that support a continued focus on cultural context. First, individuals are more willing to express stigma than to act on it, setting cultural expressions as the litmus test for marking challenges and crafting public health interventions.46,47 Second, path-breaking work that connects larger cultural climates to individually held attitudes, experiences, and self-stigmatizing profiles provides a clear direction for multilevel efforts.16,48 Unless we attack stigma at the cultural level, the prospects for changing the lives of those affected by mental illness is unlikely. A focus on small-scale individual-level efforts, even if successful, will continually confront negative reinforcement from the larger culture. As one component among many, addressing efforts to influence larger cultural contexts of misunderstanding, inclusion or rejection, and tolerance or intolerance is essential.
The public health implications of the backbone of stigma hold promise for redirecting stigma reduction efforts toward novel messages and approaches. Because the public holds a tacit understanding of the etiology of mental illness, our efforts need to move past this message. To consider messaging that targets core sentiments that elicit negative responses from the public must be at the heart of new campaigns. Our analyses did not point to one “correct” approach or another, but rather emphasized the penetrating and damaging nature of prejudice, the complexity of hard-core targets, and the resulting multifaceted response that needs to be mounted. Only coordinated and sustained efforts are likely to improve the mental health of populations.
Acknowledgments
This research was supported by grants from the Fogarty International Center, the National Institute of Mental Health, the Office of Behavioral and Social Science Research (grant R01TW006374-01), the Icelandic Centre for Research, Ghent University, and the National Science Foundation (to the US General Social Survey). B. A. Pescosolido holds a career award from the National Institute of Drug Abuse (grant K18DA031462-01). Additional support was provided by Indiana University’s College of Arts and Sciences Infrastructural Grant to the Indiana Consortium for Mental Health Services Research, and Indiana University’s Clinical and Translational Sciences Institute through support for Indiana University’s Network Science Initiative.
Thanks also to Karen Kafadar, chair of the Department of Statistics, Indiana University Bloomington, for her advice on the analytic strategy.
Human Participant Protection
This research has been approved by the Indiana University Institutional Review Board (protocol 04-9051).
References
- 1.Pescosolido BA. Stigma: what do we think; what do we know; what can we prove? J Health Soc Behav. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Link BG, Yang L, Phelan JC, Collins P. Measuring mental illness stigma. Schizophr Bull. 2004;30(3):511–541 [DOI] [PubMed] [Google Scholar]
- 3.Martin JK, Pescosolido BA, Olafsdottir S, McLeod JD. The construction of fear: modeling Americans’ preferences for social distance from children and adolescents with mental health problems. J Health Soc Behav. 2007;48(1):50–67 [DOI] [PubMed] [Google Scholar]
- 4.Pescosolido BA, Martin JK, Lang A, Olafsdottir S. Rethinking theoretical approaches to stigma: a framework integrating normative influences on stigma (FINIS). Soc Sci Med. 2008;67(3):431–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S. The public’s view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. Am J Public Health. 1999;89(9):1339–1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pescosolido BA, McLeod JD, Avison WR. Through the looking glass: the fortunes of the sociology of mental health. In: Avison WR, McLeod JD, Pescosolido BA, eds. Mental Health, Social Mirror. New York, NY: Springer; 2007: 3–32 [Google Scholar]
- 7.Phelan JC, Link BG, Dovidio JF. Stigma and prejudice: one animal or two? Soc Sci Med. 2008;67(3):358–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Evans-Lacko S, Rose D, Henderson C, Thornicroft G. Comment on the evaluation of the time to change anti-stigma campaign. The Psychiatrist. 2010;34:541–542 [Google Scholar]
- 9.Sartorius N, Schulze H. Reducing the Stigma of Mental Illness: A Report From a Global Association. New York, NY: Cambridge University Press; 2005 [Google Scholar]
- 10.Couture S, Penn DL. Interpersonal contact and the stigma of mental illness: a review of the literature. J Ment Health. 2003;12:291–305 [Google Scholar]
- 11.Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. “A disease like any other?” A decade of change in public reactions to schizophrenia, depression and alcohol dependence. Am J Psychiatry. 2010;167(11):1321–1330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Phelan JC, Link BG, Stueve A, Pescosolido BA. Public conceptions of mental illness in 1950 and 1996: what is mental illness and is it to be feared? J Health Soc Behav. 2000;41(2):188–207 [Google Scholar]
- 13.Schomerus G, Schwahn C, Holzinger Aet al. Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand. 2012;125(6):440–452 [DOI] [PubMed] [Google Scholar]
- 14.Swindle R, Heller K, Pescosolido BA, Kikuzawa S. Responses to “nervous breakdowns” in America over a 40-year period: mental health policy implications. Am Psychol. 2000;55(7):740–749 [DOI] [PubMed] [Google Scholar]
- 15.Read J, Haslam N, Sayce L, Davies E. Prejudice and schizophrenia: a review of the “mental illness is an illness like any other” approach. Acta Psychiatr Scand. 2006;114(5):303–318 [DOI] [PubMed] [Google Scholar]
- 16.Mojtabai R. Mental illness stigma and willingness to seek mental health care in the European Union. Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):705–712 [DOI] [PubMed] [Google Scholar]
- 17.Corrigan PW. Where is the evidence supporting public service announcements to eliminate mental illness stigma? Psychiatr Serv. 2012;63(1):79–82 [DOI] [PubMed] [Google Scholar]
- 18.Stuart H, Arboleda-Florez J, Sartorius N. Paradigms Lost: Fighting Stigma and the Lessons Learned. New York, NY: Oxford University; 2012 [Google Scholar]
- 19.Link BG, Phelan JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: labels, causes, dangerousness and social distance. Am J Public Health. 1999;89(9):1328–1333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatization of people with mental illness. Br J Psychiatry. 2000;177(1):4–7 [DOI] [PubMed] [Google Scholar]
- 21.Stuart H, Arboleda-Florez J. Community attitudes toward persons with schizophrenia. Can J Psychiatry. 2001;46(3):245–252 [DOI] [PubMed] [Google Scholar]
- 22.Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: ignorance, prejudice, or discrimination? Br J Psychiatry. 2007;190:192–193 [DOI] [PubMed] [Google Scholar]
- 23.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington DC: American Psychiatric Association; 1994 [Google Scholar]
- 24.Pescosolido BA, Martin JK, Link BG, Kikuzawa S, Burgos G, Swindle R. Americans’ Views of Mental Illness and Health at Century’s End: Continuity and Change. Public Report on the MacArthur Mental Health Module, 1996 General Social Survey. Bloomington, IN: Indiana Consortium for Mental Health Services Research; 2000 [Google Scholar]
- 25.Boyer CA, Pescosolido BA, Medina TR. Issues in understanding mental illness and its measurement: global problems, local manifestations and the issue of labeling. Presented at the International Conference on Survey Methods in Multinational, Multiregional, and Multicultural Contexts; June 25–29, 2008; Berlin, Germany [Google Scholar]
- 26.Pescosolido BA, Martin JK. The challenges of international survey collaboration. An introduction to the Stigma in Global Context–Mental Health Study (SGC-MHS). Presented at the International Conference on Survey Methods in Multinational, Multiregional, and Multicultural Contexts; June 25–29, 2008; Berlin, Germany [Google Scholar]
- 27.Pescosolido BA, Olafsdottir S. The logistics of survey implementation in a comparative study of mental illness: issues and resolutions in translation across cultural boundaries. Presented at the International Conference on Survey Methods in Multinational, Multiregional, and Multicultural Contexts; June 25–29, 2008; Berlin, Germany [Google Scholar]
- 28.International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. Vol. 2 Geneva, Switzerland: World Health Organization; 2011 [PubMed] [Google Scholar]
- 29.Bogardus ES. Social Distance. Yellow Springs, OH: The Antioch Press; 1959 [Google Scholar]
- 30.Martin JK, Pescosolido BA, Tuch SA. Of fear and loathing: the role of disturbing behavior, labels and causal attributions in shaping public attitudes toward persons with mental illness. J Health Soc Behav. 2000;41(2):208–233 [Google Scholar]
- 31.Bobo L, Kluegel JR, Smith RA. Laissez faire racism: the crystallization of a “kinder, gentler” anti-Black ideology. In: Tuch SA, Martin JK, eds. Racial Attitudes in the 1990s: Continuity and Change. Greenwood, CT: Praeger; 1997:15–44 [Google Scholar]
- 32.Hyman HH, Sheatsley PB. Attitudes on integration. Sci Am. 1956;195:35–39 [Google Scholar]
- 33.Schuman HS, Steeh C, Bobo L. Racial Attitudes in America: Trends and Interpretations. Cambridge, MA: Harvard University Press; 1985 [Google Scholar]
- 34.Cohen J, Struening E. Opinions about mental illness in the personnel of two large hospitals. J Abnorm Soc Psychol. 1962;64:349–360 [DOI] [PubMed] [Google Scholar]
- 35.Link BG, Cullen FT, Struening EL, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: an empirical assessment. Am Sociol Rev. 1989;54:400–423 [Google Scholar]
- 36.Angermeyer MC, Matschinger H. The effect of personal experience with mental illness and attitude toward individuals suffering from mental disorders. Soc Psychiatry Psychiatr Epidemiol. 1996;31(6):321–326 [DOI] [PubMed] [Google Scholar]
- 37.Corrigan PW, Matthews AK. Stigma and disclosure: implications for coming out of the closet. J Ment Health. 2003;12(3):235–248 [Google Scholar]
- 38.Phelan JC, Link BC. Fear of people with mental illnesses: the role of personal and impersonal contact and exposure to threat or harm. J Health Soc Behav. 2004;45(1):68–80 [DOI] [PubMed] [Google Scholar]
- 39.Slovic P, Monahan J. Probability, danger, and coercion: a study of risk perception and decision-making in mental health law. Law Hum Behav. 1995;19(1):49–65 [Google Scholar]
- 40.Borinstein AB. Public attitudes toward persons with mental illness. Health Aff (Millwood). 1992;11(3):186–196 [DOI] [PubMed] [Google Scholar]
- 41.Roman PM, Floyd HH. Social acceptance of psychiatric illness and psychiatric treatment. Soc Psychiatry. 1981;16:21–29 [Google Scholar]
- 42.Tukey JW. Exploratory Data Analysis. Reading, MA: Addison-Wesley; 1977 [Google Scholar]
- 43.Olafsdottir S, Pescosolido BA. Constructing illness: how the public in eight Western nations respond to a clinical description of “schizophrenia.” Soc Sci Med. 2011;73(6):929–938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pescosolido BA, Olafsdottir S, Martin JK, Long JS. Cross-cultural aspects of the stigma of mental illness. In: Arboleda-Florez J, Sartorius N, eds. Understanding the Stigma of Mental Illness: Theory and Interventions. London, UK: John Wiley & Sons Ltd; 2008 [Google Scholar]
- 45.McCranie A. Recovery in mental illness: the roots, meanings, and implementations of a “new” services movement. In: Pilgrim D, Rogers A, Pescosolido BA, eds. The Sage Handbook of Mental Health and Illness. London, UK: Sage Publications; 2010:471–489 [Google Scholar]
- 46.Jones EG, Mendell LM. Assessing the decade of the brain. Science. 1999;284(5415):739. [DOI] [PubMed] [Google Scholar]
- 47.Smith ER, Mackie DM. Surprising emotions. Science. 2009;323(5911):215–216 [DOI] [PubMed] [Google Scholar]
- 48.Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychol Med. 2012;42(8):1741–1752 [DOI] [PubMed] [Google Scholar]