Abstract
Suicide prevention must be transformed by integrating injury prevention and mental health perspectives to develop a mosaic of common risk public health interventions that address the diversity of populations and individuals whose mortality and morbidity contribute to the burdens of suicide and attempted suicide. Emphasizing distal preventive interventions, strategies must focus on people and places—and on related interpersonal factors and social contexts—to alter the life trajectories of people before they become suicidal. Attention also must be paid to those in the middle years—the age with the greatest overall burden. We need scientific and social processes that define priorities and assess their potential for reducing what has been a steadily increasing rate of suicide during the past decade.
Preventing suicide is very challenging, especially when seeking to shift the modal behaviors of large populations.1,2 Talented, dedicated people have made extraordinary efforts to reduce suicide in the United States during these first years of the 21st century, but the overall rate has risen steadily. The 1990s was a decade of decline; the crude suicide rate was 10.46 per 100 000 people in 1999, with an age-adjusted rate of 10.48.3 In 2008 suicide became the 10th leading cause of death in our nation, up from its long-held position of 11th. In 2010 suicide accounted for 38,364 deaths, with a crude rate of 12.43 and an age-adjusted rate of 12.08 per 100 000, respectively,4 the latter being 15.26% higher than the comparable 1999 figure. Preliminary reports indicate 38,235 deaths in 2011. By comparison, there were 37,233 lives lost in 2010 from transportation accidents.5 Suicide far surpasses more publically noted challenges, such as homicide—the 16th leading cause of death—which took 16 259 lives in 2010.
In 2010 suicide was the third leading cause of death for those aged 15 to 24 years (4600), after unintentional injury (12 341) and homicide (4678); second among those aged 25 to 34 years (5735), between unintentional injury (14 573) and homicide (4258); and fourth (6571) among those aged 35 to 44 years. For those aged 35 to 64 years, there have been steady annual increases in age-adjusted rates from 1999 to 2010: men climbed from 21.48 to 27.64 suicides per 100 000 and women from 6.19 to 8.21, for a combined change in those ages from 13.70 to 17.75 per 100 000, an increase of nearly 30%.3
This far outweighed all other changes in rates during the same period. For those aged 10 to 24 years, rates tended to remain relatively stable during the first decade of the 21st century: males had an age-adjusted rate of 11.64 in 1999 and 11.56 in 2010, whereas females had rates of 2.17 and 2.83, respectively. Among those aged 25 to 34 years, males had rates of 20.74 in 1999 and 22.50 in 2010, an increase of 8.5%, with comparable rates for females of 4.58 and 5.34 (16.6% more). The age-adjusted suicide rate for those aged 65 years and older declined from 15.81 in 1999 (33.80 for men; 4.34 for women) to 14.89 per 100 000 in 2010 (29.00 for men; 4.19 for women), a drop of 5.8%.3 Although the use of firearms as a method of suicide remained relatively stable from 1999 to 2010 (age-adjusted rates of 5.96 in 1999 and 6.06 in 2010, with a brief dip in mid-decade), the rate of poisoning suicides grew steadily (1.76 in 1999 and 2.06 in 2010), with the greatest increase in the middle years.
Taken together, these statistics only hint at the devastation wreaked by suicide on the lives of families, friends, coworkers, and communities. Between 2000 and 2010,3 suicide was the fifth leading cause of years of potential life lost (YPLL) for those younger than 65 years in the United States (5.9% of the total; nearly 8.23 million YPLL), more than homicide (5.0%; 6.94 million), and following unintentional injury (18.9%), malignant neoplasms (16.2%), heart disease (12.1%), and deaths during the perinatal period (7.9%). By 2010, suicide accounted for 6.9% of YPLL (764,776 of 11,043,870) for those younger than 65 years whereas homicide was 4.7% (522,701) of YPLL, reflecting the continued changes in the distribution of these premature deaths. Furthermore, fundamental factors that contribute to the contexts for suicide, especially during the early and middle years of life, also relate to unintentional deaths owing to alcohol poisoning, drug overdose, and motor vehicle accidents as well as to interpersonal violence and homicide.2 Identifying and mitigating or preventing such common risks potentially serve as the foundation for public health and injury prevention approaches to preventing suicide and attempted suicide.
The costs of suicide and attempted suicide are economic as well as personal and social. For 2005, the estimated cost of suicide was more than $34.6 billion arising from 32 637 deaths and including medical costs and inferred lost work3; by comparison, that same year 18 124 homicides were projected to cost about $25.3 billion. Since then, suicides have risen by nearly 6000 and homicides have declined by nearly 2000, obviously altering the cost projections further toward a greater burden from the less-attended problem. The hospitalization and emergency department costs arising from self-harm in 2005 were nearly $6.4 billion. Thus, suicide and attempted suicide, in addition to involving deaths, damaged lives, and broad ramifications for family and friends, damage our collective economic well-being.
THE GULF BETWEEN ASPIRATIONS, ACTIONS, AND OUTCOMES
When US Surgeon General David Satcher issued his Call to Action in 1999 and commissioned the development of the 2001 National Strategy for Suicide Prevention (NSSP 1.0),6,7 he asserted that preventing suicide and attempted suicide was a winnable battle, a battle that reflected priorities of the Senate8 and the House of Representatives.9 But the overall burdens of suicide and attempted suicide have grown during the 21st century, not declined. How do we understand the gulf between the aspirations of the surgeon general and the Congress, the expectations of the NSSP 1.0, and the reality of suicide that we face today?
A diverse set of factors contributes to the formation and maintenance of the gaps that separate aspirations from effective outcomes.
Despite the progress derived from the Centers for Disease Control and Prevention’s National Violent Death Reporting System and the increase of data access through the WISQARS and WONDER reporting systems, the United States continues to experience a fundamental data gap because of slow reporting, a lack of basic surveillance information for suicide, and very few systematic or detailed data for attempted suicide. As a nation, we do not have the essential, timely information feedback loop regarding suicide that is central to any large-scale public health process of problem identification, program development and implementation, evaluation, dissemination, and program modification–adjustment.
At the community and state levels, fundamental challenges range from inadequate and variable determination of manner of death to long-held fears that rapid reporting of suicide attempts to facilitate treatment referrals will intrude on personal privacy. Without timely data it will be very challenging to know what interventions actually make a difference in national or regional rates of suicide and medically serious suicide attempts.
NSSP 1.0 was a panoply of broadly framed recommendations that were sensitive to the needs of diverse constituencies but not truly a strategic plan that set explicit priorities, expectations for timely implementation, and measurable outcomes. There were no specifically allocated governmental funds to achieve its goals and no clearly defined entity that was accountable for its implementation. In part, this reflected the decentralized nature of responsibility for health services across the nation. Although NSSP 1.0 espoused a “public health approach,” many interpreted this as equivalent to case finding of imminently suicidal individuals through deploying screening programs and gatekeeper training programs in high schools and universities—although neither has ever demonstrated any impact on rates of suicide or attempted suicide. For example, the single published randomized trial of gatekeeper training did not support its premise that brief training either changed the skills or behaviors of recipients or increased referrals of vulnerable persons to needed services.10
In a related vein, the priorities expressed in the landmark Garrett Lee Smith Act, which has funded many suicide prevention programs in the United States since its passage in 2004, have been devoted to youths and young adults aged 24 years and younger, particularly those in schools, universities, and tribal communities. Driven largely by the understandable efforts of surviving family members—particularly parents—these have focused on the portion of the population, in terms of its age range, that contributes relatively less to overall deaths. To date, there are no comparable efforts that focus on suicide in the middle years of life and little if any coherent discussion nationally about how one would design, develop, implement, or evaluate such programs.
Overall, there has been a pervasive emphasis on high-risk individuals. This raises 2 concerns. Individuals in such groups, in fact, constitute a relatively small percentage of the population; thus, if we had effective programs for reducing suicides among them, the overall contribution to the burden of deaths would be relatively small.11 Rose’s theorem is as pertinent to suicide as it is to heart disease2,12–14; most suicides come from the general population rather than the much smaller groups of people who are disabled by severe mental disorders, despite the higher rates in those groups. Also, risk factors for suicide and related warning signs have been derived from studies comparing suicides with community controls, general population data, or attempters with comparison participants; however, they have not represented prospectively collected samples in which it has been possible to follow people until death.15–19
Although relatively small group studies and meta-analyses have shown statistically significant differences, these factors have not been found to have predictive validity when used in the context of screening programs,20 and many people who go on to die by suicide fail to be detected while in care,21 even in health systems such as the Veterans Administration in which resources have been heavily deployed to detect known risks.22 Although it may be reasonable to define these as clinical features, it is another matter to consider them as risk factors that have discriminating value. Common features cannot predict rare events. It is essential to avoid the ecological fallacy of simply applying characteristics of a population to individual members and assuming that these will predict outcomes.
It could be argued that suicide rates would be higher if current high-risk programs did not exist. This assertion may be true but has not been demonstrated or supported inferentially. To support such assertions, one would need to fulfill criterion (a) conduct carefully designed and analyzed large-scale naturalistic studies to demonstrate a high diversion rate of newly identified at-risk individuals into care alternatives, with related positive outcomes that sustainably alter life trajectories; or (b) perform large-scale collaborative trials (ideally, randomized in an appropriate fashion) that have the potential to aggregate sufficient numbers to demonstrate less suicide or meaningful proxy outcomes (e.g., reduction in medically serious suicide attempts); plus (c) show that these evidence-based measures have been applied widely enough in the real world with sufficient program fidelity to have a discernible regional or national impact on the rates of suicide or serious attempts.
Colleagues and I have noted 5 challenges for suicide prevention that have yet to be addressed.1,2 Challenge 1 is an inability to discriminate the relatively few true cases from the large numbers of false-positive cases. Suicide is a relatively rare event—thankfully—but the clinical and social risks are common. This relates directly to the dilemma of using commonly occurring risk factors as the guide for designing interventions. To illustrate the dilemma, let’s assume that the suicide rate for individuals suffering major depression is 50 times greater than is the national average—about 600 per 100 000, that is, 600 dying in a year among 100 000 having a major depression diagnosis. How will one reasonably distinguish those relatively few from the 99 400 who will not die by suicide in the coming year? Alternatively stated, when seeing any person with a diagnosis of major depression, there is a greater than 99% chance that she or he will not die from suicide in the coming year. No doubt, a great many people suffering risks require active treatment and sometimes emergency interventions because we do not know how to distinguish those who might die from those who will not. Essential treatment should not be conflated with suicide prevention as a public health preventive intervention.
Challenge 2 is the large number of false-negative cases that escape preventive detection.21–23 No matter how vigilant we may be, many lethally intent individuals are not identified. Despite the high frequency of psychopathological findings revealed by using postmortem psychological autopsy methods, those features are often not sufficiently compelling in life to raise alarms or foretell death. Indeed, this quandary serves as a compelling rationale for means-oriented interventions that do not depend on identifying specific individuals at times when they are suicidal.
Challenge 3 is the inability of clinical services to reach many individuals who have suicidal intent. It is clear that most people in the midst of a life-ending crisis do not come to the attention of service providers and that the growth of crisis services during the past decade has not stemmed the rising tide. This requires attention to what we have defined as the social geography of our communities and the social ecology of groups who could benefit from selective or indicated interventions.2 Social geography refers to the diverse settings of every community, with each offering unique sampling (recruiting) biases—“potential points of capture”2—in which one might array preventive interventions and engage those who reside or pass through (e.g., schools and universities, the courts, large corporations, and primary care, detoxification, and mental health clinics). An example of a social geography perspective asks: Which target populations for preventive interventions do we encounter in courts awaiting trial? Who do we miss?
Defining social ecology offers a complementary perspective; I use it to denote a process of defining and listing the multiple settings in which one might engage specific groups (e.g., alcoholic men). Where are the community sites in which we can find alcoholic men who may be vulnerable, distressed, or depressed?
Challenge 4 is a continuing paucity of knowledge about fundamental biological, psychological, social, and cultural factors that contribute to apparent risk among diverse populations and groups. Such factors vary by age, race, gender, sexual orientation, residential geography, and sociocultural and economic status. Our limited understanding of how best to define and mobilize protective factors that may diminish the impact of risk factors widens this knowledge gap further.
Challenge 5 is the lack of coordinated strategies for suicide prevention to deal effectively with myriad local, regional, state, and national agencies and organizations that could, in theory, play a role in preventing suicide.
These challenges argue for broadly based public health approaches that reach beyond the current methods of finding individuals deemed to be at imminent risk to die. Public health approaches are required that foster distal preventive interventions for populations and selective groups at a time when those individuals who are potentially vulnerable among them are not at imminent risk.
But it has been difficult to enlist either the public health community or the mental health community in such approaches. Members of the mental health community tend to say that such distal preventive interventions are not suicide prevention programs; their goal is to treat suicidal individuals as the target, with the implication that this will result in a reduction in the number of suicides. To date, that has not proven to be true. Focusing efforts on reducing the overall suicide rate opens doors to a broad range of approaches; focusing primarily on detected suicidal individuals limits perspectives and suffers from the conundrum that most suicidal people, or people who have attempted suicide and survived their first attempt, do not die from suicide.2
Despite the surgeon general’s Call to Action more than a decade ago,6 it is apparent that the public health community has not fully embraced suicide prevention in the way that it has prioritized preventing motor vehicle accidents, falls among elderly individuals, and youth violence. For example, (1) the Centers for Disease Control and Prevention has not yet formally listed suicide as one of its key priorities despite its heavy burdens (although it did recently fund an injury control research center that focuses on suicide prevention), (2) New York State’s Department of Health injury prevention Web site does not list suicide among its topics,24 and (3) a possible reflection of the diminished importance of suicide prevention in the public health arena is found in the recent State of the States: 2009 Report from the Safe States Alliance.25 Participating states ranked suicide attempts as their top programmatic priority area in 2005 and 2007; the 2009 report revealed that suicide and self-inflicted injury were the sixth priority and suicide attempts the seventh. These changes have come at a time when the suicide rate has been increasing steadily.
Our country will see a transformation only when we have programs that deal with the fundamental factors that precede becoming suicidal—such as family turmoil, early life abuse, alcohol and substance misuse, partner violence, employment adversity, and encroaching medical comorbidities associated with poorly treated pain and functional decline. We must pay as much attention to context as we do to person. Put another way, we must reduce the prevalence of adversities that drive human vulnerabilities toward distress and disease; at the same time we must strengthen community support and increase people’s willingness to accept help. Success requires bridging the gaps and building on values and ideas from public health and injury prevention, mental health, law and policy, and survivors, communities, states, and regions.
At the heart of the challenge posed by suicide, attempted suicide, and related interpersonal violence is the question of whether suicide really is preventable. Without doubt, the basis of my argument is that prevention is possible.26 To date, the major effective public health initiatives have involved means restriction or control.27 However, the potential impact of such interventions is limited by ecological factors (e.g., pertinent to hanging or jumping from high places) and by social forces (e.g., firearm access). Although there are important examples of effective population-oriented interventions that involve actively engaging groups and individuals,28–31 these have yet to be broadly applied or generalized in any systematic fashion. Without sufficient optimism and aspirational goals—the necessary basis of social commitment and political will—it will be impossible to muster the needed energy, resources, and sustained effort to implement needed initiatives and programs.
RESHAPING THE FIELD OF SUICIDE PREVENTION
To forge new approaches to preventing suicide, attempted suicide, and their antecedents, it is crucial to bridge the gaps that separate key elements in our field and develop novel action coalitions. There are 2 fundamental barriers, one conceptual and the other collaborative.
Creating a Compelling Vision
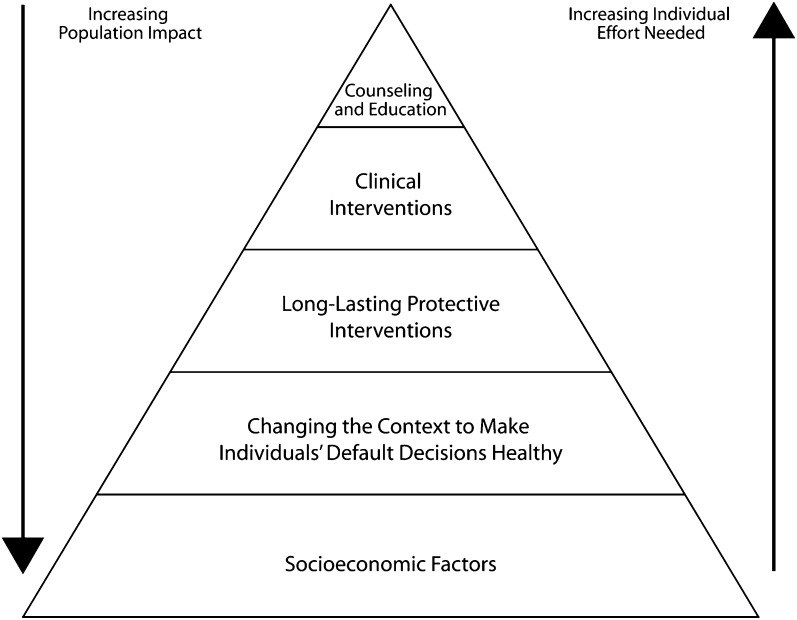
Reducing the burden of suicide and attempted suicide in the United States requires a fundamental reconsideration of current approaches. If one uses Frieden’s recently presented impact on health model (Figure 1),32 it is apparent that nearly all the suicide prevention efforts put forth since the release of NSSP 1.0 have been confined to the uppermost 2 tiers—clinical interventions and counseling and education—which essentially depend on changing the behavior of suicidal individuals themselves, family members, and care providers.
FIGURE 1—
The Health Impact Pyramid.
Source. Frieden.32
Frieden emphasizes that these top tier programs are much less likely to succeed than are more broadly based initiatives. Current programs have tended to concentrate on detecting imminently at-risk individuals with the aim of referring them to care, and none have measured reductions in suicides as a key outcome. As noted, Garrett Lee Smith grants often have supported educational programs for gatekeepers in communities and schools. Although these are laudable, they have been evaluated most often on the basis of process indicators (e.g., number of people trained) rather than changes in behaviors (e.g., increased contact with target populations that lead to more frequent referrals for services) or improved outcomes (fewer suicide attempts and suicides). Thus, it is unclear whether such efforts change or save lives. Future approaches require a clear understanding of desired outcomes and how they fit into guiding conceptual frameworks.
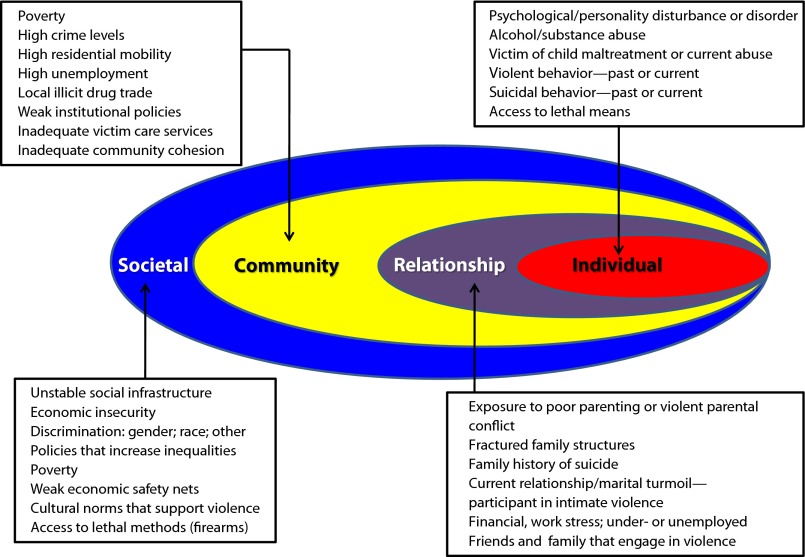
Violence prevention programs have adopted ecological models. Figure 2 presents a modification of the diagram presented by Butchart et al.33 It offers one view of the diverse array of factors that can influence suicide. Although it can serve as a transactional model to investigate interactions across layers, it may not explain where to begin prevention initiatives. Nonetheless, it challenges us to deal with the central issue of relating individual-level actions and outcomes to family and community factors, that is, linking persons to contexts. Understanding suicide requires such integration.
FIGURE 2—
Ecological model of shared risks for suicide and interpersonal violence.
Source. Adapted from Butchart et al.33
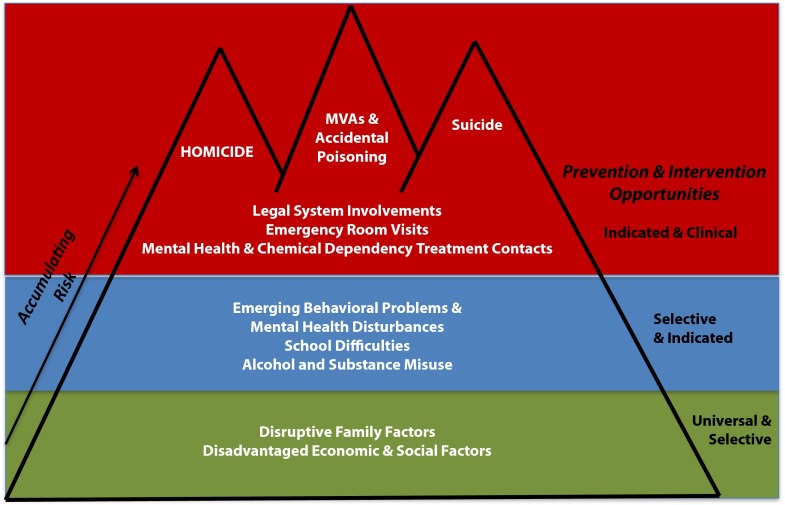
Another approach seeks to depict developmental ecological frameworks or models.2 Figure 3 points to areas for early preventive interventions and highlights what we see as common risks for developmentally related adverse outcomes in early middle adulthood—accidental death, suicide, and homicide.2 Colleagues and I were drawn to this view in light of our initial work with the US Air Force. Its suicide prevention program actually served as a violent death and violence prevention program, helping to reduce suicide, accidental death, homicide, violent offenses, and moderate to severe family violence.28
FIGURE 3—
Common developmental contexts for different adverse outcomes of premature death in early adulthood.
Note. MVA = motor vehicle accident.
Source. Caine et al.2
Substantial effort was devoted in the US Air Force to increasing early interventions with families in which there was impending or early stages of intimate partner violence. Also, data from psychological autopsies34 and the US National Mortality Followback Survey35 have pointed to interpersonal violence as a key common risk area for suicide and other adverse outcomes, which are supported by findings from complementary perspectives.36–39 Among suicides recorded in the National Violent Death Reporting System,39 participation in intimate partner violence was the leading factor identified in 10% to 11% of the suicides during the years of study, 2003 to 2008, and contributed heavily to several other latent classes that were identified. Additionally, other types of interpersonal violence contributed principally to another 6% or more.
There also are high rates of suicide attempts (12%) among respondents to petitions for orders of protection—that is, the presumed perpetrators of intimate violence—in civil courts40 and comparable levels (15%) among people awaiting trial in criminal court.41 Thus, preventing and mitigating interpersonal violence has benefits in its own right and stands as a prime example of targeting both contexts and behaviors that can change the trajectories of people’s lives. The same potential holds for accidental deaths and suicide.42
To integrate public health and mental health perspectives, specific programmatic initiatives must find a balance that considers social geography (a community view) and social ecology (a group and person view). For each potential intervention site in a community it should be possible to determine systematically who is encountered and who will be missed. The complementary perspective tracks the ecology of the many groups for whom we seek to promote mental health, lessen adversity, and ultimately prevent suicide. We need to establish where we would most productively encounter and engage them in their physical locations in communities and perhaps their social networks on the Internet.
As a practical means of integrating context and person, it is essential to outline an on-the-ground frame into which we can assemble the pieces of the mosaic of preventive interventions that are both locally specific and conceptually grounded. In these parameters planners can begin to assess the potential reach of each effort and its likely impact on suicide and attempted suicide rates. Indeed, use of simulation models and other quantitative approaches can offer targets or benchmarks against which to judge the effects of initiative in the action mosaic if there are timely data available for such studies.
Considering Socially and Politically Sensitive Topics
Although content issues are essential for developing farsighted, compelling strategies, they are insufficient without a broadly shared willingness to engage in difficult discussions that lead to definitive actions. Efforts to reduce suicide in the United States are unlikely to succeed unless the nation forthrightly deals with socially and politically sensitive key issues. An essential step for any national- or state-level initiative entails realistically assessing the potential impact of each interventional component of any proposed prevention mosaic. This involves identifying the target populations, measuring their respective contributions to the overall burden of suicide, defining how much of a reduction of suicide and serious suicide attempts will result from such efforts, and establishing a priori how those outcomes will be measured. In 2010, for example, there were 1933 suicides of youths aged 19 years and younger. If their deaths were reduced by 50.0% (i.e., 967 fewer), the national burden would be reduced by 2.5%. When viewed as the lost, loved child of a family, there is no question about priorities; when viewed in the context of establishing national priorities, there is much room for vigorous, well-informed, constructive discussion.
Such discussion must lead to social negotiations that form the substrate for collective actions. Without candid, scientifically based appraisal and frank consideration and respect for fundamental differences, it is unlikely that prevention efforts can achieve much headway. I present 3 issues as potential focal points around which collaborative solutions must be developed.
Issue 1.
Death during the middle years of life, involving people from middle adulthood to the early 60s, has served as the impetus for the past decade’s increases in suicide, both in terms of increasing rates and in overall number of deaths.3 There are no well-conceived, tested, or off-the-shelf programs on which to build prevention efforts for people in the middle years, and to date, there have been few processes that seek to bring together the diverse constituencies and communities necessary to confront the challenges suicide in the middle years poses.
One reason for the lack of attention to suicide in the middle years is the understandable nature of survivor-guided advocacy in the United States; another may be the nature of many middle years suicides. Most are men, although this also is the portion of the life span when women in the United States have their highest suicide rates. Many reflect long-standing problems that snowball over the course of time, involving persistent or recurrent drinking or drug use, family turmoil and violence, problems with employment, emerging or worsening depression, and gradual social and functional decline.15 Often decedents have not seen mental health or medical providers, or they had dropped out of care during the months or years before their suicides. Although absent from the clinical arena, they frequently have been encountered by the police and in courts and assessed by social service agencies, or they have come to the attention of their employer for inadequate work performance. Many do not elicit sympathetic responses from their families, spouses, or children: they burn their bridges and have disruptive life experiences not long before death.43
Including interpersonal violence is key, given its repeated presence as one of the most important, distal presuicidal factors that can be identified and addressed effectively. Addressing other exacerbating factors—for example, chronic drinking and declining work performance—requires that these too be seen at the population level as common risks for suicide and for other adverse outcomes. This invites the formation of prevention alliances that seek to mitigate or intercede with fundamental factors that potentially lead to a diverse array of adverse outcomes.2
Issue 2.
The major method of suicide in the United States remains firearms, although the use of other means has been increasing. Any discussion that examines the role of firearms in suicide involves a sensitive and complex topic, given constitutional concerns and the evident political polarization.
Discussion of restricting individual ownership of firearms would not be productive in our country, any more than discussion of restricting access to tall buildings would be productive for suicide prevention in Hong Kong, where jumping from heights is the most common cause of death. But discussions of firearm safety and public awareness of suicide prevention can be a topic for common consideration—if public health professionals and gun enthusiasts develop a collaborative dialogue outside the more hotly politicized topics of the day. We must create a scientific forum that respects all viewpoints.
Issue 3.
Some will surely view preventing suicide, addressing interpersonal violence, talking about firearm safety, and dealing with depression and other mental health concerns at a community and public health level as invasions of individual privacy and as fraught with concerns about stigma.
Public health traditions recognize ethical demands for population needs that may supersede individual-level concerns.44,45 This perspective may seem to diverge from the intensely individual focus of mental health professionals and related privacy advocates, who are especially mindful of stigma and the need for confidentiality of information and communication.
Taiwan, for example, has now mandated reporting all suicide attempts. Taiwan’s government, commentators, and public health and medical communities view this mandate in the same light as reporting serious infectious diseases; they see suicide as a dire public health urgency. Although some sites have reported spotty compliance, others have a near 100% registration rate. Data show that more than 80% of more than 50 000 reported cases received aftercare services; studies that link the attempter files with Taiwan’s version of the National Death Index reveal that, among all attempters who have been followed for 1 to 3 years, those who had aftercare had a 22% lower suicide rate than did those who did not have contact.46 Although this naturalistic appraisal may have many shortcomings (sample bias being a great concern), it points to the potential benefit of creating more comprehensive surveillance, reporting, and aftercare, similar to the situation in Denmark that has been central to its fundamental suicide research47 and important prevention initiatives.48
Many voices in the United States would undoubtedly describe as intrusive, unethical, and unacceptable any broadly applied registration of suicide attempts that clinicians or case managers routinely followed—no matter the degree of public health concern. How one views the inevitable debate likely will depend on values related to personal privacy and confidentiality, public responsibility for deaths in local communities, and whether suicide and attempted suicide truly are public health problems.
Suicide was historically seen as a social concern and more recently as a medical and personal problem.49,50 Accepting the premise that distal preventive interventions are intended to change the trajectories of people’s lives suggests a willingness to embrace broader social responsibilities. Yet it remains uncertain whether such a stance would gain wide acceptance across the nation. Without thoughtful and open discussion, we will have insufficient guidance to develop needed programs.
CONCLUSIONS
I would recommend that any person, group, community, or agency that is contemplating the design, development, and implementation of suicide prevention initiatives ask themselves a series of questions:
What are the broad goals and specific objectives of the intervention and the program?
Where does this program fit in an overall framework (i.e., mosaic, schema, model) of suicide prevention interventions?
Who do we expect to reach with this effort?
Who will we miss?
What will we be changing?
How will we measure those changes and use the information to rigorously evaluate and modify (or disseminate or eliminate) the program as indicated?
Will these changes affect local, regional, and national suicide rates?
How confident are we in our findings?
Can the program and its results be exported widely?
Can the program be sustained after its ardent founders have moved on?
It certainly is fair to argue that we have no data as yet, beyond the impact of means control in some countries, to ensure that public health approaches to preventing suicide actually will alter powerful antecedents and in turn lower death rates. However, if such approaches include safer communities, less domestic abuse and trauma, reduced misuse of alcohol and drugs, greater recognition and access to care for those with mental health concerns, and efforts to prevent school dropout or employment insecurity, the likely benefits will be measurable and meaningful. Economic supports can save lives.51 Some may not label this as suicide prevention; I see such reductions in premature death as a gain.
The experiences of this decade since the publication of NSSP 1.0 have taught us crucial, often sobering lessons. Many of these have served as guidance for the newly released version of the national strategy (NSSP 2.0). Gleaning the most from these experiences—successes and failures both—requires honesty, vision, energy, and dedication. Most important, there is a critical need for continuing candid debate and deliberation, even as many visionary and well-intentioned people persist in efforts to engage communities and individuals to save lives. Preventing suicide is a winnable battle, a battle that requires leadership, cohesion, and sustained support and commitment to planning, action, evaluation, and constructive change.
Acknowledgments
This work was supported in part by the US Centers for Disease Control and Prevention (grant R49 CE002093).
Many concepts and ideas in this piece have been informed and shaped by working with colleagues, particularly Yeates Conwell, Kerry Knox, Catherine Cerulli, Kenneth Connor, Wendi Cross, Paul Duberstein, Robert Bossarte, Peter Wyman, and Jerry Reed.
Human Participant Protection
No protocol approval was necessary because all data were obtained from publicly available secondary sources.
References
- 1.Caine ED. Preventing suicide is hard to do! Psychiatr Serv. 2010;61(12):1171. [DOI] [PubMed] [Google Scholar]
- 2.Caine ED, Knox KL, Conwell Y. Public health and population approaches for suicide prevention. In: Cohen NL, Galea S, eds. Population Mental Health: Evidence, Policy, & Public Health Practice. London, UK: Routledge; 2011:303–338 [Google Scholar]
- 3.Centers for Disease Control and Prevention Web-Based Injury Statistics Query and Reporting System. Available at: http://webappa.cdc.gov/sasweb/ncipc/mortrate10_us.html. Accessed February 4, 2013 [Google Scholar]
- 4.Kochanek KD, Xu J, Murphy SL, Miniño AM, Kung H-C. Deaths: final data for 2009. Natl Vital Stat Rep. 2011;60(3):1–116 DHHS publication PHS 2012–1120 [PubMed] [Google Scholar]
- 5.Hoyert DL, Xu JQ. Deaths: preliminary data for 2011. Natl Vital Stat Rep. 2012;61(6):1–51 [PubMed] [Google Scholar]
- 6.Satcher D. The Surgeon General’s Call to Action to Prevent Suicide. Washington, DC: Department of Health and Human Services; 1999 [Google Scholar]
- 7.Satcher D. National Strategy for Suicide Prevention: Goals and Objectives for Action. Rockville, MD: Department of Health and Human Services; 2001 [PubMed] [Google Scholar]
- 8.143 Cong. Rec. S3995—Suicide in America—Senate; May 6. Washington, DC: US Government Printing Office; 1997 [Google Scholar]
- 9.House of Representatives. HRes. 212; 105th Congress. October 10, 1998 [Google Scholar]
- 10.Wyman PA, Brown CH, Inman Jet al. Randomized trial of a gatekeeper program for suicide prevention: 1-year impact on secondary school staff. J Consult Clin Psychol. 2008;76(1):104–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis G, Hawton K, Jones P. Strategies for preventing suicide. Br J Psychiatry. 1997;171:351–354 [PubMed] [Google Scholar]
- 12.Knox KL, Conwell Y, Caine ED. If suicide is a public health problem, what are we doing to prevent it? Am J Public Health. 2004;94(1):37–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14(1):32–38 [DOI] [PubMed] [Google Scholar]
- 14.Rose G. The Strategy of Preventive Medicine. Oxford, UK: Oxford University Press; 1992 [Google Scholar]
- 15.Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry. 1996;153(8):1001–1008 [DOI] [PubMed] [Google Scholar]
- 16.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405 [DOI] [PubMed] [Google Scholar]
- 17.Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BMC Psychiatry. 2004;4:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Arch Gen Psychiatry. 1997;54(4):337–343 [DOI] [PubMed] [Google Scholar]
- 19.Kraemer HC. Current concepts of risk in psychiatric disorders. Curr Opin Psychiatry. 2003;16:421–430 [Google Scholar]
- 20.Peña JB, Caine ED. Screening as an approach for adolescent suicide prevention. Suicide Life Threat Behav. 2006;36(6):614–637 [DOI] [PubMed] [Google Scholar]
- 21.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159(6):909–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ilgen MA, Bohnert AS, Ignacio RVet al. Psychiatric diagnoses and risk of suicide in veterans. Arch Gen Psychiatry. 2010;67(11):1152–1158 [DOI] [PubMed] [Google Scholar]
- 23.Conwell Y, Duberstein P, DiGiorno A, Cox C, Forbes NT, Caine ED. Risk Factors for Suicide in Later Life. Lorne, Australia: International Psychogeriatric Association; 2001 [Google Scholar]
- 24.New York State Department of Health. Injury Prevention in New York State. Available at: http://www.health.state.ny.us/prevention/injury_prevention. Accessed November 12, 2012. [Google Scholar]
- 25.State of the States: 2009 Report. Atlanta, GA; Safe States Alliance; 2011 [Google Scholar]
- 26.Caine ED. Suicide prevention is a winnable battle. Am J Public Health. 2012;102(suppl 1):S1–S6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yip PS, Caine E, Yousuf S, Change SS, Su KC, Chen YY. Means restriction for suicide prevention. Lancet. 2012;379(9834):2393–2399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Knox KL, Litts DA, Talcott GW, Feig JC, Caine ED. Risk of suicide and related adverse outcomes after exposure to a suicide prevention programme in the US Air Force: cohort study. BMJ. 2003;327(7428):1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knox KL, Pflanz S, Talcott GWet al. The US Air Force suicide prevention program: implications for public health policy. Am J Public Health. 2010;100(12):2457–2463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coffey CE. Building a system of perfect depression care in behavioral health. Jt Comm J Qual Patient Saf. 2007;33(4):193–199 [DOI] [PubMed] [Google Scholar]
- 31.Fleischmann A, Bertolote JM, Wasserman Det al. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bull World Health Organ. 2008;86(9):703–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100(4):590–595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Butchart A, Phinney A, Check P, Villaveces A. Preventing Violence: a Guide to Implementing the Recommendations of the World Report on Violence and Health. Geneva, Switzerland: World Health Organization; 2004 [Google Scholar]
- 34.Conner KR, Duberstein PR, Conwell Y. Domestic violence, separation, and suicide in young men with early onset alcoholism: reanalyses of Murphy’s data. Suicide Life Threat Behav. 2000;30(4):354–359 [PubMed] [Google Scholar]
- 35.Conner KR, Cox C, Duberstein PR, Tian L, Nisbet PA, Conwell Y. Violence, alcohol, and completed suicide: a case–control study. Am J Psychiatry. 2001;158(10):1701–1705 [DOI] [PubMed] [Google Scholar]
- 36.Hiroeh U, Appleby L, Mortensen PB, Dunn G. Death by homicide, suicide, and other unnatural causes in people with mental illness: a population-based study. Lancet. 2001;358(9299):2110–2112 [DOI] [PubMed] [Google Scholar]
- 37.Webb RT, Qin P, Stevens H, Mortensen PB, Appleby L, Shaw L. National study of suicide in all people with a criminal justice history. Arch Gen Psychiatry. 2011;68(6):591–599 [DOI] [PubMed] [Google Scholar]
- 38.Webb RT, Qin P, Stevens L, Appleby L, Shaw J, Mortensen PB. Combined influence of serious mental illness and criminal offending on suicide risk in younger adults. Soc Psychiatry Psychiatr Epidemiol. 2012; Epub ahead of print [DOI] [PubMed] [Google Scholar]
- 39.Logan J, Hall J, Karch D. Suicide categories by patterns of known risk factors: a latent class analysis. Arch Gen Psychiatry. 2011;68(9):935–941 [DOI] [PubMed] [Google Scholar]
- 40.Conner KR, Cerulli C, Caine ED. Threatened and attempted suicide by partner—violent male respondents petitioned to family violence court. Violence Vict. 2002;17(2):115–125 [DOI] [PubMed] [Google Scholar]
- 41.Swogger MT, You S, Cashman-Brown S, Conner KR. Childhood physical abuse, aggression, and suicide attempts among criminal offenders. Psychiatry Res. 2011;185(3):363–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bergen H, Hawton K, Kapur Net al. Shared characteristics of suicides and other unnatural deaths following nonnonfatal self-harm? A multicentre study of risk factors. Psychol Med. 2012;42(4):727–741 [DOI] [PubMed] [Google Scholar]
- 43.Duberstein PR, Conwell Y, Caine ED. Interpersonal stressors, substance abuse, and suicide. J Nerv Ment Dis. 1993;181(2):80–85 [DOI] [PubMed] [Google Scholar]
- 44.Khan MM, Mian AI. The one truly serious philosophical problem: ethical aspects of suicide. Int Rev Psychiatry. 2010;22(3):288–293 [DOI] [PubMed] [Google Scholar]
- 45.Leeder SR. Ethics and public health. Intern Med J. 2004;34(7):435–439 [DOI] [PubMed] [Google Scholar]
- 46.Pan YJ, Chang WH, Lee MB, Chen CH, Liao SC, Caine ED. Effectiveness of a nationwide aftercare program for suicide attempters. Psychol Med. 2012; Epub ahead of print [DOI] [PubMed] [Google Scholar]
- 47.Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Arch Gen Psychiatry. 2011;68(10):1058–1064 [DOI] [PubMed] [Google Scholar]
- 48.Nordentoft M. Crucial elements in suicide prevention strategies. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(4):848–853 [DOI] [PubMed] [Google Scholar]
- 49.Kushner HI. Self-Destruction in the Promised Land: A Psychocultural Biology of American Suicide. New Brunswick, NJ: Rutgers University Press; 1989 [Google Scholar]
- 50.Minois G. History of Suicide: Voluntary Death in Western Culture. Baltimore, MD: Johns Hopkins University Press; 1999 [Google Scholar]
- 51.Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet. 2009;374(9686):315–323 [DOI] [PubMed] [Google Scholar]