Abstract
Objectives. We examined differences in self-reported mental health (SRMH) between US-born and Somalia-born Black Americans compared with White Americans. We tested how SRMH was affected by stigma toward seeing a mental health provider, discrimination in the health care setting, or symptoms of depression.
Methods. Data were from a 2008 survey of adults in Minnesota and were limited to US-born and Somalia-born Black and White Americans (n = 938).
Results. Somalia-born adults were more likely to report better SRMH than either US-born Black or White Americans. They also reported lower levels of discrimination (18.6%) than US-born Black Americans (33.4%), higher levels of stigma (23.6% vs 4.7%), and lower levels of depressive symptoms (9.1% vs 31.6%). Controlling for stigma, discrimination, and symptomatology, Somalia-born Black Americans reported better SRMH than White and Black Americans (odds ratio = 4.76).
Conclusions. Mental health programming and health care providers who focus on Black Americans’ mental health might be missing important sources of heterogeneity. It is essential to consider the role of race and ethnicity, but also of nativity, in mental health policy and programming.
Black Americans are at lower risk than White Americans for common mental disorders, such as anxiety and mood disorders, and substance use.1 Evidence is less clear that there are differences for rates of psychological distress or depressive symptoms,2 with some research indicating that Black Americans may fare worse on these measures,3,4 and other studies showing that they may do better.5 Recent research examined diversity within the Black American population and highlighted important differences in mental health outcomes by nativity.5 For example, Williams et al.,6 using data from the National Survey of American Life, found that Caribbean-born Black males had higher risk of 12-month psychiatric disorders than did US-born Black men, whereas the opposite pattern held for women. The study by Williams7 in 1986 described the historical development of epidemiological studies of mental illness in this population. Using data from the National Institute of Mental Health Epidemiological Catchment Area study, he concluded that there was a paucity of studies that documented the variation in mental illness among Black Americans of different backgrounds.7
These studies illustrated the need for research to differentiate between the experiences of US-born and foreign-born Black individuals. To date, no large studies have focused exclusively on immigrants from Africa, who made up about 4% of the total foreign-born population and 49% of the foreign-born Black population in the United States in 2010.8 This study provided an opportunity to examine mental health among Somalia-born Black adults compared with US-born Black and White adults. Data were from a representative sample of adults enrolled in public health care programs in Minnesota, thereby focusing on primarily low-income adults.
Studies generally found that foreign-born adults had lower rates of mental illness and psychological distress than US-born adults.5,9 One explanation was that having strong social ties and a strong sense of belonging to a particular ethnic group might protect against mental illness.10 An alternative explanation was that healthy people were more likely to take on the challenge of immigrating (the “healthy migrant” effect).11
Although most research on the healthy immigrant paradox has focused on Hispanic or Latino populations, important differences exist between such populations and the Somalia-born population. Most Somalia-born individuals immigrated in the midst of civil war. In their study of Somali and Oromo (Ethiopian) immigrants to the United States, Jaranson et al.12 found that 25% to 69% had experienced torture before immigrating. Because exposure to conflict leads to vulnerability toward mental health problems, Somalia-born individuals might be expected to report worse mental health than their US-born counterparts. Specifically, exposure to trauma and stress that accompany leaving conflict zones could be expected to predict higher rates of posttraumatic stress disorder and depression. Many refugee populations do exhibit higher rates of such disorders.12,13
Some studies indicated that foreign-born Black immigrants had better mental and physical health than their US-born counterparts.14,15 Furthermore, foreign-born Black adults demonstrated lower rates of chronic disease16 and fewer risk factors than US-born Black adults.17 However, these studies largely focused on Caribbean-born Black immigrants and not their Somalia-born counterparts, who might have markedly different immigration experiences. Additionally, these populations might hold different attitudes toward mental illness and have different experiences within the health care arena. To better understand differences between groups, we investigated the role of stigma, discrimination, and symptomatology.
Stigma can lead to understated self-reports of mental illness and might prevent people with mental illness from seeking, engaging in, or following through with treatment.18,19 Previous work suggested that Black Americans in the United States hold less stigmatized attitudes toward mental health care than do White Americans,20 but research has not explored this issue in as much depth in the immigrant population. Qualitative research suggested that some Somali immigrants might be reluctant to admit to mental health problems and might experience shame, guilt, or even suicidal ideation in response to experiencing mental illness.21 Such stigma and reticence to admit to mental illness might manifest itself as embarrassment to see a mental health provider.22
Although the mental health of Somalia-born individuals might be closely tied to immigration and acculturation, US-born Black adults face prolonged exposure to racism that negatively affects mental health.23 The link between discrimination toward US-born Black Americans and physical and mental health outcomes has been well documented,24 including myriad studies that documented the association between self-reports of discrimination and mental health.25 Yet, there is a paucity of research that has sought to understand the role that discrimination plays in the mental health of foreign-born Black immigrants.23
International studies suggested that African immigrant populations outside of the United States experience social exclusion, which might contribute to poor mental health. Although UK and US ethnic minority groups have different cultural and social contexts and histories of migration, they share experiences of social exclusion that can potentially contribute to mental disorders. There are also similarities in the pattern of interaction and experiences of mental health services by ethnic minority groups in the United Kingdom and the United States.26–28 For example, the existence of inequalities in diagnosis and treatment of Afro-Caribbeans in the United Kingdom is well-established. Studies found that perceptions of discriminatory treatment by health services deterred Afro-Caribbeans from accessing such services.29,30
In the United States, there is evidence that foreign-born Black adults report experiencing less discrimination than their counterparts born in the United States. A 2009 study, for example, found that of pregnant US-born and foreign-born Black Americans, the US-born cohort was significantly more likely to report experiencing racial discrimination.31 In addition to discrimination and racism generally, it is important to understand the role of unfair treatment within the health care setting. If individuals do not feel that they are given fair treatment, it may lead to reticence to seek help or follow treatment recommendations.
An alternative explanation for differences in self-reported mental health (SRMH) is that groups experience different symptoms of mental illness and that SRMH is an accurate reflection of mental health status. The Patient Health Questionnaire-2 (PHQ-2) has proved effective in detecting mental illness symptomatology in clinical settings32,33 and can be compared with SRMH to gain a more complete picture of mental health status. Some research found that despite experiencing discrimination, Black Americans demonstrated lower rates of many common mental illnesses than did White Americans.25 The healthy immigrant paradox found that, despite low socioeconomic and social standing, some immigrants had better health outcomes than more advantaged groups.14,15 However, much of this research focused on this effect among Hispanic populations.34 Research among Somalia-born immigrants found that mental illness was often somaticized, with symptoms of physical, rather than mental, ailments.21
This article addressed the following research questions. (1) Do US-born and Somalia-born Black Americans differ from White Americans in SRMH? (2) Do stigma, discrimination in a health care setting, and symptoms of mental illness explain differences in SRMH? (3) Do interactions between race or nativity and stigma, discrimination, and symptomatology mediate these relationships? Answering these questions will allow us to develop a richer understanding of the mental health experiences of these populations while gaining a better understanding of how stigma around mental health and experiences within the health care system might affect individuals’ perceptions of their mental health.
METHODS
Data were from a random sample of enrollees in Minnesota Health Care Programs. The 2008 survey focused on health care experiences and barriers to access. Hmong, Somali, African American, American Indian, and Hispanic individuals were oversampled, and only 1 person per household was included in the sample.
Data were collected with a mixed mode design (mail and telephone). Eligible respondents were first sent a mail survey conducted in English, with a telephone follow-up of persons who did not respond to the second mailing in English, Spanish, Hmong, or Somali as needed. Twenty-eight percent of Somali respondents completed the survey by mail (n = 82), significantly less than White or US-born Black respondents (78% and 67%, respectively.) Of those Somalis who responded by mail, 41% reported having assistance in filling out the survey. By definition, those who completed the survey by telephone responded for themselves, not with assistance from a friend or relative. The response rate (defined by the American Association for Public Opinion Research, AAPOR-4) was 44.3%, consistent with response rates for other publicly insured populations.35
Administrative and some claims data were available for all eligible respondents, allowing us to compare nonrespondents with respondents. Respondents were significantly older and more likely to be female, White, or Asian than were nonrespondents. They were also less likely to be Black and American Indian. There was no difference between respondents and nonrespondents in the percentage who spoke Somali. However, nonrespondents were significantly more likely to list their nationality as Somali than were respondents (12.5% vs 10.3%). Poststratification weights adjusted for these differences. There were few differences in service use associated with mental health. Rates of outpatient visits with a mental health diagnosis were similar, as were the percentages of respondents and nonrespondents who had a first-listed diagnosis of depression or had a claim for an antidepressant. Nonrespondents were more likely to have a first-listed diagnosis of any mental health problem (International Classification of Diseases-Ninth Revision36 codes 290–319), although the difference was substantively small (30.5% vs 28.6%).
Community researchers from the Hispanic, US-born Black, Somali, Hmong, American Indian, and European American communities partnered with University researchers using a community-based participatory research model.37,38 The translation process from English to Somali was overseen by a community organization, with the assistance of a paid translator from the Somali community. Community members were involved in rewriting questions that did not resonate during the pilot, resulting in improved understanding and increased response rates from the Somalia-born community.
Measures
Dependent variable.
We assessed mental health with a measure of current self-reported emotional health. SRMH was significantly associated with physical and mental health outcomes. Beyond providing an understanding of respondents’ acknowledgment of emotional problems, SRMH was associated with use of mental health services and predicted physical decline and mortality.39 Respondents were asked, “Overall, how would you rate your emotional health?” with 5 response options, from “poor” to “excellent” emotional health.
Independent variables.
Discrimination in health care settings was measured with 2 items.40 First, respondents were asked how often they thought their race, ethnicity, or nationality caused health care providers to treat them unfairly on a scale of “never” to “always.” Second, they were asked if they experienced discrimination because of their race or skin color during a health care visit in the past year. Respondents who answered positively that they had been treated unfairly or discriminated against were coded as 1 for the combined measure and 0 otherwise.
Stigma was assessed using a measure from the National Comorbidity Surveys.41 Respondents were asked: “How embarrassed would you be if your friends knew you were getting professional help for an emotional problem?” Four response options ranged from 1 for “not at all embarrassed” to 4 for “very embarrassed.” A dichotomous measure was coded as 1 if the respondent answered, “very embarrassed,” and 0 otherwise.
Symptomatology was measured using the PHQ-2 screener.33 The items asked respondents how often in the last 2 weeks they were bothered by (1) having little interest or pleasure in doing things, or (2) feeling down, depressed or hopeless. The original response categories included “not at all,” “several days,” “more than half,” and “nearly every day,” and a summed score of greater than or equal to 3 had excellent specificity and sensitivity for detecting potential clinical depression.33 However, pretests indicated that respondents had difficulty with choosing a response option if they thought the symptom described just a few, but not “several days”; consequently, the response options were modified to include “not at all,” “some days,” “several days,” “more than half the days,” or “nearly every day.” In the analysis, some days and not at all were combined to mirror the original response categories, and a summed score of 3 or greater was used to indicate a positive depression screener. To control for comorbidity,42,43 self-rated physical health was included with depressive symptomatology in the models (coded 1–5; with 5 representing excellent health).
Controls.
Full models included the following controls: age, gender (1 = female), education (1 = high school graduate), employment (employed, unemployed, or not in the labor force), and being married or in a marriage-like relationship (vs single, divorced, or widowed).
Race and ethnicity were measured consistent with Office of Management and Budget standards,44 with ethnicity (including Latino/Hispanic, Somali, or Hmong) asked first followed by race. Persons could identify as more than 1 race, and were assigned to 1 racial category using the Office of Management and Budget’s “whole assignment, smallest group” method.44 Where race was missing from the survey data (in less than 3% of cases), race from administrative data was used. For the present study, the sample was limited to adult respondents (n = 2194) and was further restricted to US-born Black adults (n = 242) and Somalia-born adults (n = 288), with White adults as the reference group (n = 408). The total analytic sample consisted of 938 respondents, which was comparable to or exceeded the sample size of this population in similar studies.13,23
Analyses
First, we examined whether the 3 groups (White, US-born Black, and Somalia-born Black) differed on the independent variables by using the Pearson χ2 test for significance. Next, because SRMH was an ordinal variable, we used ordered logistic regression to obtain odds ratios of reporting better mental health. We used a series of nested models to understand the individual effects of stigma, discrimination, and symptomatology on SRMH.
Data were weighted to account for the stratified sampling design and nonresponse to represent the population of enrollees in Minnesota’s public health programs. All estimates presented were based on the weighted data. Standard errors were adjusted in the analysis to account for the complex survey design. After we removed individuals with missing data points, the total study sample was 799 participants, accounting for a decrease of approximately 15% of responses over the 5 nested models.
RESULTS
Table 1 includes descriptive statistics. Notably, Somalia-born respondents were younger, more likely to be married, and more likely to be employed than were their US-born Black counterparts. However, they were less likely to have graduated from high school. Overall, White respondents were the most advantaged in terms of being the most likely to have graduated high school and to be employed.
TABLE 1—
Demographic Differences by Race/Ethnicity and Nativity: Minnesota, 2008
| Independent Variables | Range | White, Mean | US-Born Black, Mean | Somalia-Born Black, Mean |
| Female | 0/1 | 0.63 | 0.67 | 0.67 |
| Age, y | 18–89 | 43.66 | 43.21 | 40.11* |
| US-born | 0/1 | 0.97 | 1.00 | 0.00*** |
| Married | 0/1 | 0.40 | 0.23 | 0.50*** |
| Employed (1 = full or part-time) | 0/1 | 0.41 | 0.23 | 0.30*** |
| Unemployed | 0/1 | 0.15 | 0.20 | 0.20*** |
| Not in labor force | 0/1 | 0.44 | 0.57 | 0.51*** |
| High school graduate | 0/1 | 0.82 | 0.67 | 0.37*** |
| Self-rated physical health (1 = poor) | 1–5 | 3.11 | 2.95 | 3.71*** |
Note. White respondents are the reference category. Statistics calculated using the weighted sample: White (n = 408), US-born Black (n = 242), and Somalia-born Black (n = 288).
*P < .05; ***P < .001.
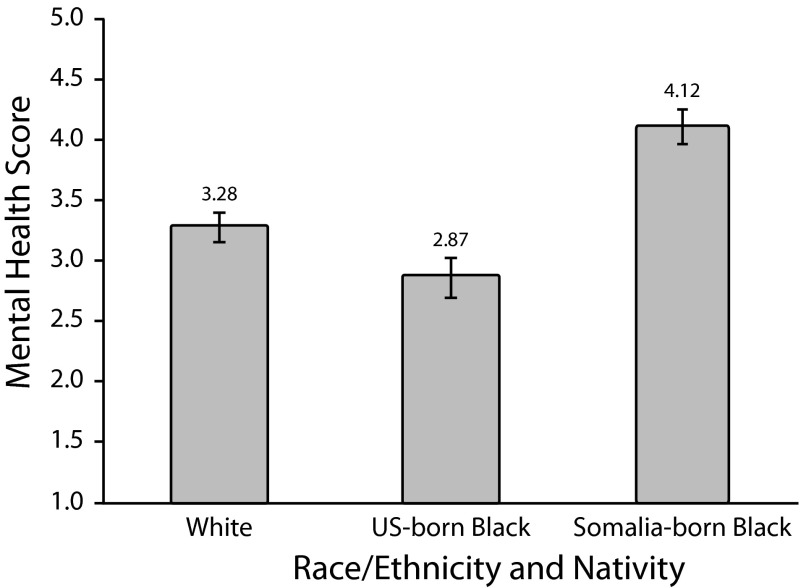
As shown in Figure 1, Somalia-born adults reported significantly better mental health than did White adults, whereas US-born Black adults reported worse mental health. The mean difference between Somalia-born and US-born Black adults was 1.25 (on a 5-point scale), which was significant at P < .001.
FIGURE 1—
Average self-reported mental health score among adult respondents by race/ethnicity and nativity: Minnesota, 2008.
Note. 1 = poor mental health; 5 = excellent mental health. Percentages are based on the weighted sample. Reference category = White respondents. Whiskers indicate 95% confidence intervals. All differences were significant at P < .001.
Figure 2 demonstrates that US-born Black adults were the most likely and White adults were the least likely to have experienced discrimination in a health care setting. Meanwhile, Somalia-born respondents reported more embarrassment about seeing a mental health provider than did US-born Black and White respondents. Nearly 24% of Somalia-born respondents reported that they would be “very embarrassed” if their friends knew that they were seeking health care for a mental health problem. By contrast, fewer than 5% of US-born Black respondents reported such stigma. Finally, US-born Black respondents were more than twice as likely as White respondents and more than 3 times as likely as Somalia-born respondents to screen positive for depression. Differences between US-born and Somalia-born Black respondents were statistically significant at P < .001 for all 3 measures.
FIGURE 2—
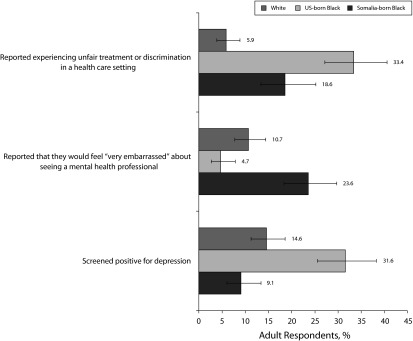
Discrimination, stigma, and symptomatology among adult respondents by race/ethnicity and nativity: Minnesota, 2008.
Note. Percentages are based on the weighted sample. Reference category = White respondents. Whiskers indicate 95% confidence intervals. All differences between US-born and Somalia-born Black adults were significant at P < .001.
Results of the ordered logistic regressions are shown in Table 2. Model 1 included demographic characteristics as controls. In this model, US-born Black adults had 34% lower odds of better SRMH compared with White adults. Conversely, Somalia-born adults had an odds ratio of 5.86 for better SRMH. Model 2 added stigma, which was not significantly associated with SRMH and did not substantially change the coefficients for racial groups. Model 3 added the composite measure of discrimination, at which point the odds for US-born Black adults were no longer significant. Subsequent tests for mediation, using the 4-step approach of Baron and Kenny,45 indicated a partial mediating effect of discrimination on SRMH. The odds of reporting better mental health for Somalia-born adults remained highly significant (P < .001) and increased to 6.54. Model 4 added physical health and depressive symptomatology, both significant predictors of SRMH. The odds of reporting better mental health for Somalia-born adults remained highly significant, but decreased slightly. Model 5 included all independent variables and showed an enduring positive effect of Somali nativity on SRMH. We also explored whether the effects of discrimination, stigma, or symptoms on SRMH varied by cultural group by adding separate interaction terms into the regression shown in model 5. None of these were significant.
TABLE 2—
Odds Ratios for Reporting Excellent Emotional Health: Minnesota, 2008
| Variable | Model 1, OR (95% CI) | Model 2, OR (95% CI) | Model 3, OR (95% CI) | Model 4, OR (95% CI) | Model 5, OR (95% CI) |
| US-born Blacka | 0.66* (0.46, 0.95) | 0.61* (0.42, 0.89) | 0.79 (0.53, 1.16) | 0.93 (0.63, 1.38) | 1.02 (0.66, 1.55) |
| Somalia-born Blacka | 5.86*** (3.75, 9.15) | 5.96*** (3.81, 9.33) | 6.54*** (4.10, 10.43) | 4.30*** (2.72, 6.80) | 4.76*** (2.96, 7.65) |
| Age | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 1.01 (1.00, 1.02) | 1.01 (1.00, 1.02) |
| Female | 0.91 (0.63, 1.32) | 0.88 (0.61, 1.27) | 0.87 (0.60, 1.26) | 0.81 (0.55, 1.18) | 0.75 (0.51, 1.10) |
| High school graduateb | 1.31 (0.88, 1.97) | 1.31 (0.88, 1.97) | 1.32 (0.88, 1.98) | 1.13 (0.74, 1.72) | 1.13 (0.73, 1.75) |
| Unemployedc | 0.62 (0.37, 1.05) | 0.62 (0.38, 1.03) | 0.61 (0.36, 1.02) | 0.57* (0.34, 0.94) | 0.55* (0.33, 0.91) |
| Not in labor forcecd | 0.61* (0.40, 0.93) | 0.61* (0.40, 0.93) | 0.61* (0.40, 0.93) | 1.10 (0.71, 1.71) | 1.10 (0.71, 1.71) |
| Married | 1.25 (0.86, 1.81) | 1.23 (0.85, 1.78) | 1.24 (0.86, 1.79) | 1.34 (0.91, 1.96) | 1.31 (0.90, 1.92) |
| Embarrassmente | 0.86 (0.71, 1.03) | 0.87 (0.73, 1.05) | |||
| Discriminationf | 0.47* (0.25, 0.88) | 0.53 (0.28, 1.02) | |||
| Physical healthg | 2.20*** (1.73, 2.79) | 2.25*** (1.77, 2.87) | |||
| Depressionh | 0.05*** (0.03, 0.11) | 0.06*** (0.03, 0.11) |
Note. CI = confidence interval; OR = odds ratio; n = 799. Statistics calculated using weighted sample. Interaction terms between race/nativity and embarrassment, race/nativity and discrimination, and race/nativity and depression were tested for each model. None produced significant results. (Results available upon request.) In preliminary models, we tested the effect of years lived in the United States on outcomes of interest. Because of collinearity with nativity in multivariate models, these results are not presented here, but are available on request.
Reference category is White.
Compared with less than a high school education.
Reference category is employed.
Includes retired, disabled, and student.
4 = very embarrassed; 1 = not at all.
1 = experienced.
5 = excellent; 1 = poor.
1 = screened positive on Patient Health Questionnaire-2.
*P < .05; ***P < .001.
DISCUSSION
This study showed the importance of examining differences by race/ethnicity and nativity status to understand mental health. Despite a history of experiencing conflict, the Somalia-born respondents in this study demonstrated better mental health than their US-born counterparts. This could be indicative of a different frame of reference: after relocating, they might report relatively better mental health compared with past circumstances. Unlike other research,46,47 we found that US-born Black adults had worse SRMH than did White adults. Our findings speak to the heterogeneity within the Black American population; we focused on a low-income group. Racial differences in psychological distress might be more pronounced among persons facing socioeconomic disadvantage.48
This study had important limitations. First, our sample was state-specific, limited to publicly insured adults in Minnesota. Therefore, caution should be used in making generalizations to other contexts. Despite this limitation, this study was unique in its sample of Somalia-born adults largely because of its Minnesota context. A number of studies that examined racial/ethnic differences in care drew on state-specific Medicaid samples, in part because of considerable variation in the completeness and reliability of race data across states (e.g., Shields et al.49) Many studies that examined the role of discrimination among minority groups also utilized samples from 1 city or state.13,23,50
Second, caution should be used in interpreting results, given the 44.3% survey response rate. However, this rate was not surprising in the lower-income diverse Medicaid population sample. Studies showed that Medicaid enrollees often had lower response rates than those not on Medicaid.35,51,52 Overall, response rates for Medicaid and low-income populations varied widely depending on follow-up efforts, with examples ranging between 38%47 and 50%.53 In this study, there were few differences between respondents and nonrespondents in mental health services use. However, there was a 2 percentage point difference on having a past claim associated with a mental health diagnosis, suggesting that the analysis might underrepresent the sickest enrollees, although given the size of the difference, any bias was modest.
Third, social desirability might have had an impact on respondents’ answers, especially for Somalia-born respondents, because of the high levels of stigma they reported. However, the majority (72%) of Somali respondents in our study completed the survey by telephone, reducing the potential for embarrassment about reporting low SRMH in a face-to-face situation or with the help of a friend or relative. Furthermore, only 12% of all Somali respondents reported having assistance in completing the survey.
Finally, our measure of discrimination was limited to health care settings and might not capture the full experience and associated mental health consequences of discrimination in a range of contexts. The measure might especially underestimate the impact of discrimination for US-born Black adults, who might have experienced a lifetime of discrimination within and beyond the US health care system.
Despite its limitations, the findings pointed to important variations within broad racial/ethnic groups. Somalia-born adults in this study reported the highest levels of stigma related to mental health. It was possible that cultural differences in willingness to admit to emotional problems during an interview meant that this population overestimated their mental health and underreported symptoms of depression. Although stigma did not appear to be related to SRMH, we were limited to 1 measure. Further attention to the meaning and measurement of stigma in diverse cultural groups is needed.
Understanding the mental health care needs for Somali immigrants and their US-born counterparts is an important task. Mental health programming that targets minority populations broadly may be missing important heterogeneity. For mental health programs to be successful, they must address potential cultural stigma. Increasing efforts to support the certification of Somali-trained physicians and generally increasing diversity in the medical workforce may foster comfort for Somalia-born adults who feel embarrassed to seek mental health help. If Somalia-born adults are embarrassed about seeing a mental health provider, it may also be appropriate for primary care physicians to offer limited services or for care to be provided in an integrated setting.
These findings had important policy implications. Despite theoretically having access to care, publicly insured adults reported different amounts of unfair treatment and discrimination in the health care system, depending on race, ethnicity, and nationality. This was an important reminder that although the Patient Protection and Affordable Care Act of 2010 will improve access to care, there are other factors that contribute to disparate health outcomes, such as unfair treatment and discrimination. Attention must also be paid to persisting disparities in insurance status for immigrant groups that may limit access to mental health care.54,55
Acknowledgments
This research was supported by the Minnesota Department of Human Services. An earlier version of this study was presented at the 2012 Midwest Sociological Society Annual Meeting in Minneapolis, Minnesota, and as a poster at the 2011 Agency for Healthcare Research and Quality 17th Annual National Research Service Award Trainee Research Conference in Seattle, Washington.
Note. The content of this article is solely the responsibility of the authors and does not necessarily represent the official position of the Department of Human Services.
Human Participant Protection
Data collection for this study received institutional review board approval from the Minnesota Department of Human Services and the University of Minnesota.
References
- 1.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2005;62(6):593–602 [DOI] [PubMed] [Google Scholar]
- 2.Lincoln KD, Chatters LM, Taylor RJ. Psychological distress among black and white Americans: differential effects of social support, negative interaction and personal control. J Health Soc Behav. 2003;44(3):390–407 [PMC free article] [PubMed] [Google Scholar]
- 3.Myers HF, Lesser I, Rodriguez Net al. Ethnic differences in clinical presentation of depression in adult women. Cultur Divers Ethnic Minor Psychol. 2002;8(2):138–156 [DOI] [PubMed] [Google Scholar]
- 4.Emslie GJ, Weinberg WA, Rush AJ, Adams RM, Rintelmann JW. Depressive symptoms by self-report in adolescence: phase I of the development of a questionnaire for depression by self-report. J Child Neurol. 1990;5(2):114–121 [DOI] [PubMed] [Google Scholar]
- 5.Bratter JL, Eschbach K. Race/ethnic differences in nonspecific psychological distress: evidence from the National Health Interview Survey (NHIS). Soc Sci Q. 2005;86(3):620–644 [Google Scholar]
- 6.Williams DR, Haile R, Gonzalez HM, Neighbors H, Baser R, Jackson JS. The mental health of black Caribbean immigrants: results from the National Survey of American Life. Am J Public Health. 2007;97(1):52–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams DH. The epidemiology of mental illness in Afro-Americans. Hosp Community Psychiatry. 1986;37(1):42–49 [DOI] [PubMed] [Google Scholar]
- 8.US Census Bureau American FactFinder 2010 American Community Survey. Available at: http://www.census.gov Accessed October 15, 2010. [Google Scholar]
- 9.Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(12):1226–1233 [DOI] [PubMed] [Google Scholar]
- 10.Mossakowski KN. Coping with perceived discrimination: does ethnic identity protect mental health? J Health Soc Behav. 2003;44(3):318–331 [PubMed] [Google Scholar]
- 11.Dey AN, Lucas JW. Physical and mental health characteristics of U.S.- and foreign-born adults: United States, 1998-2003. Adv Data. 2006;(369):1–19 [PubMed] [Google Scholar]
- 12.Jaranson JM, Butcher J, Halcon Let al. Somali and Oromo refugees: correlates of torture and trauma history. Am J Public Health. 2004;94(4):591–598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ellis BH, MacDonald HZ, Lincoln AK, Cabral HJ. Mental health of Somali adolescent refugees: the role of trauma, stress, and perceived discrimination. J Consult Clin Psychol. 2008;76(2):184–193 [DOI] [PubMed] [Google Scholar]
- 14.Read JG, Emerson MO, Tarlov A. Implications of black immigrant health for U.S. racial disparities in health. J Immigr Health. 2005;7(3):205–212 [DOI] [PubMed] [Google Scholar]
- 15.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol. 2002;74(1):83–109 [DOI] [PubMed] [Google Scholar]
- 16.Venters H, Gany F. African immigrant health. J Immigr Minor Health. 2011;13(2):333–344 [DOI] [PubMed] [Google Scholar]
- 17.Lucas JW, Barr-Anderson DJ, Kington RS. Health status of non-Hispanic U.S.-born and foreign-born black and white persons: United States, 1992-95. Vital Health Stat 10. 2005;(226):1–20 [PubMed] [Google Scholar]
- 18.Corrigan P. How stigma interferes with mental health care. Am Psychol. 2004;59(7):614–625 [DOI] [PubMed] [Google Scholar]
- 19.Sirey JA, Bruce ML, Alexopoulos GSet al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiatry. 2001;158(3):479–481 [DOI] [PubMed] [Google Scholar]
- 20.Shim RS, Compton MT, Rust G, Druss BG, Kaslow NJ. Race-ethnicity as a predictor of attitudes toward mental health treatment seeking. Psychiatr Serv. 2009;60(10):1336–1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scuglik DL, Alarcon RD, Lapeyre AC, 3rd, Williams MD, Logan KM. When the poetry no longer rhymes: mental health issues among Somali immigrants in the USA. Transcult Psychiatry. 2007;44(4):581–595 [DOI] [PubMed] [Google Scholar]
- 22.Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophr Bull. 2004;30(3):511–541 [DOI] [PubMed] [Google Scholar]
- 23.Krieger N, Kosheleva A, Waterman PD, Chen JT, Koenen K. Racial discrimination, psychological distress, and self-rated health among US-born and foreign-born black Americans. Am J Public Health. 2011;101(9):1704–1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams DR. Race, socioeconomic status, and health: the added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896(1):173–188 [DOI] [PubMed] [Google Scholar]
- 25.Williams DR, Earl TR. Commentary: race and mental health–more questions than answers. Int J Epidemiol. 2007;36(4):758–760 [DOI] [PubMed] [Google Scholar]
- 26.Bhui KS, McKenzie K. Rates and risk factors by ethnic group for suicides within a year of contact with mental health services in England and Wales. Psychiatr Serv. 2008;59(4):414–420 [DOI] [PubMed] [Google Scholar]
- 27.Department of Health and Human Services (DHHS) Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. 2001. Rockville, MD: US Substance Abuse and Mental Health Services Administration [PubMed] [Google Scholar]
- 28.Bhui K, Christie Y, Bhugra D. The essential elements of culturally sensitive psychiatric services. Int J Soc Psychiatry. 1995;41(4):242–256 [DOI] [PubMed] [Google Scholar]
- 29.Mclean C, Campbell C, Cornish F. African-Caribbean interactions with mental health services in the UK: experiences and expectations of exclusion as (re)productive of health inequalities. Soc Sci Med. 2003;56(3):657–669 [DOI] [PubMed] [Google Scholar]
- 30.Campling P. Race, culture, and psychotherapy. Psychiatrist. 1989;13(10):550–551 [Google Scholar]
- 31.Dominguez TP, Strong EF, Krieger N, Gillman MW, Rich-Edwards JW. Differences in the self-reported racism experiences of US-born and foreign-born black pregnant women. Soc Sci Med. 2009;69(2):258–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Löwe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58(2):163–171 [DOI] [PubMed] [Google Scholar]
- 33.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292 [DOI] [PubMed] [Google Scholar]
- 34.Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60(Spec No 2):S68–S75 [DOI] [PubMed] [Google Scholar]
- 35.Gallagher PM, Fowler FJ. Don’t forget about in-person interviews. Paper presented at Eighth Conference on Health Survey Research Methods. Feb. 20-23, 2004. Peachtree City, GA [Google Scholar]
- 36.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 37.Israel BA, Coombe CM, Cheezum RRet al. Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health. 2010;100(11):2094–2102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Israel BA, Schulz AJ, Parker EA, Becker AB, Community-Campus Partnerships for Health Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Educ Health (Abingdon). 2001;14(2):182–197 [DOI] [PubMed] [Google Scholar]
- 39.Lee Y. The predictive value of self assessed general, physical, and mental health on functional decline and mortality in older adults. J Epidemiol Community Health. 2000;54(2):123–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krieger N, Sidney S. Racial discrimination and blood pressure: The CARDIA study of young black and white adults. Am J Public Health. 1996;86(10):1370–1378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mojtabai R. Americans’ attitudes toward mental health treatment seeking: 1990-2003. Psychiatr Serv. 2007;58(5):642–651 [DOI] [PubMed] [Google Scholar]
- 42.Buist-Bouwman MA, de Graaf R, Vollebergh WA, Ormel J. Comorbidity of physical and mental disorders and the effect on work-loss days. Acta Psychiatr Scand. 2005;111(6):436–443 [DOI] [PubMed] [Google Scholar]
- 43.Scott KM, Bruffaerts R, Tsang Aet al. Depression-anxiety relationships with chronic physical conditions: results from the world mental health surveys. J Affect Disord. 2007;103(1-3):113–120 [DOI] [PubMed] [Google Scholar]
- 44. Office of Management and Budget. Standards for the classification of federal data on race and ethnicity. Updated 2010. Available at: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=172. Accessed February 13, 2011.
- 45.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182 [DOI] [PubMed] [Google Scholar]
- 46.Zuvekas SH, Fleishman JA. Self-rated mental health and racial/ethnic disparities in mental health service use. Med Care. 2008;46(9):915–923 [DOI] [PubMed] [Google Scholar]
- 47.Weech-Maldonado R, Morales LS, Elliott M, Spritzer K, Marshall G, Hays RD. Race/ethnicity, language, and patients’ assessments of care in Medicaid managed care. Health Serv Res. 2003;38(3):789–808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams DR, Costa M, Leavell JP. Race and mental health: patterns and challenges. In: Scheid TL, Brown TN, eds. A Handbook for the Study of Mental Health – Social Contexts, Theories and Systems. 2nd ed. New York, NY: Cambridge University Press; 2010:268–290 [Google Scholar]
- 49.Shields AE, Comstock C, Weiss KB. Variations in asthma care by race/ethnicity among children enrolled in a state Medicaid program. Pediatrics. 2004;113(3 Pt 1):496–504 [DOI] [PubMed] [Google Scholar]
- 50.Spencer MS, Chen J. Effect of discrimination on mental health service utilization among Chinese Americans. Am J Public Health. 2004;94(5):809–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Beebe TJ, Davern ME, McAlpine DD, Call KT, Rockwood TH. Increasing response rates in a survey of Medicaid enrollees: the effect of a prepaid monetary incentive and mixed modes (mail and telephone). Med Care. 2005;43(4):411–414 [DOI] [PubMed] [Google Scholar]
- 52.Gallagher PM, Fowler FJ, Stringfellow VL. Notes from the field: experiments influencing response rates from Medicaid enrollees. Paper presented at the 55th Annual Conference of the American Association for Public Opinion Research. May 18-21, 2000. Portland, OR [Google Scholar]
- 53.Gibson PJ, Koepsell TD, Diehr P, Hale C. Increasing response rates for mailed surveys of Medicaid clients and other low-income populations. Am J Epidemiol. 1999;149(11):1057–1062 [DOI] [PubMed] [Google Scholar]
- 54.Ku L, Matani S. Left out: immigrants’ access to health care and insurance. Health Aff (Millwood). 2001;20(1):247–256 [DOI] [PubMed] [Google Scholar]
- 55.Derose KP, Escarce JJ, Lurie N. Immigrants and health care: sources of vulnerability. Health Aff (Millwood). 2007;26(5):1258–1268 [DOI] [PubMed] [Google Scholar]