Abstract
Objectives. We assessed expected ethics competencies of public health professionals in codes and competencies, reviewed ethics instruction at schools of public health, and recommended ways to bridge the gap between them.
Methods. We reviewed the code of ethics and 3 sets of competencies, separating ethics-related competencies into 3 domains: professional, research, and public health. We reviewed ethics course requirements in 2010–2011 on the Internet sites of 46 graduate schools of public health and categorized courses as required, not required, or undetermined.
Results. Half of schools (n = 23) required an ethics course for graduation (master’s or doctoral level), 21 did not, and 2 had no information. Sixteen of 23 required courses were 3-credit courses. Course content varied from 1 ethics topic to many topics addressing multiple ethics domains.
Conclusions. Consistent ethics education and competency evaluation can be accomplished through a combination of a required course addressing the 3 domains, integration of ethics topics in other courses, and “booster” trainings. Enhancing ethics competence of public health professionals is important to address the ethical questions that arise in public health research, surveillance, practice, and policy.
Public health as a profession has a long history of expecting ethical behavior by its providers, scientists, and decision-makers. With early influences from medicine and nursing, laboratory science, and epidemiology, to more contemporary disciplines (e.g., behavioral science and engineering), public health consists of diverse professions,1 each of which contributes unique training, expectations of professional behavior, and discipline-specific codes of ethics. The common link that brings these disparate professionals together is the need for collective effort to improve health through a population focus.2
Public health’s population focus presents unique ethics considerations that differ from those reflected in biomedicine and clinical care. Interactions between health care providers and patients emphasize the clinician’s obligation to the patient and the patient’s autonomy. Emphasis on the individual presents a challenge to public health professionals whose “patient” is the community or population. Since the early 2000s, at least a dozen public health ethics frameworks offered by scholars and practitioners have discussed the tensions that occur between autonomy and community responsibility.3 Public health professionals, many of whom are trained in medicine and allied health, understand that ethical challenges arise in the population setting, in public health practice, and public health research. The purpose of this assessment was to assess the expected ethical competencies of public health professionals as reflected in published codes and competencies, review current ethics instruction at schools of public health (SPH), and recommend ways to bridge the gap between what is expected and what is currently taught in graduate level courses.
PUBLISHED COMPETENCIES FOR PUBLIC HEALTH PROFESSIONALS
Public health professionals have 1 code of ethics4 that applies to all disciplines and 3 sets of published competencies5–8 that outline multiple skills and behaviors deemed necessary for proficient ethical practice of public health. The first document, the Public Health Code of Ethics,4 promulgated by the Public Health Leadership Society and adopted by the American Public Health Association in 2002, describes 12 principles for the ethical behavior of public health professionals and agencies. Its accompanying document outlining the ethical skills required to fulfill this code,9 published in 2004, built on competencies generated from an Institute of Medicine report on the future of public health.2 The second document, which is the first of the 3 sets of competencies, is the Association for Schools of Public Health (ASPH) Core Competencies.5,6 These competencies were developed for MPH and DrPH degree programs by ASPH, which in 2011 represented 46 accredited SPH in North America.
The second of 3 sets of competencies, published by the Centers for Disease Control and Prevention (CDC) and the Council of State and Territorial Epidemiologists (CSTE), are the Competencies for Applied Epidemiologists in Governmental Public Health Agencies.7 These represent a set of tiered competencies that vary by skill and experience levels for epidemiologists working in public sector agencies at all levels of government. Competencies are outlined at 4 performance levels, including entry level, midlevel, senior supervisory, and senior scientist or subject matter expert. The third set of competencies, from the Public Health Foundation’s Council on Linkages between Academia and Public Health Practice (PHF COL) Core Competencies for Public Health Professionals,8 outline a tiered set of skills for all public health practitioners. The 3 tiers include entry-level professionals, mid-level personnel with supervisory or management responsibilities, and senior-level managers and leaders in public health organizations.
Each of these 4 sets of expectations for professional knowledge and skills includes ethics-related competencies, which we categorized into 3 domains. The first domain, professional ethics, reflects how we ought to act as public health professionals, and is defined as “the principles of proper conduct concerning the rights and duties of the professional, relations with patients or consumers and fellow practitioners, as well as actions of the professional and interpersonal relations with patient or consumer families.”10 The second domain, public health ethics, or how we apply ethical thinking to our decision-making in public health practice, is defined as “the philosophical knowledge and analytic reasoning necessary for careful thinking and decision making in creating and implementing public health policy.”11(p12) The third domain, public health research ethics, includes research integrity, and refers to how we conduct research responsibly at 2 levels, the individual level and the institutional level. For the first level, research integrity is “the individual’s commitment to intellectual honesty and personal responsibility.”12(p5) At the institutional level, research integrity, is
a commitment to creating an environment that promotes responsible conduct [of research] by embracing standards of excellence, trustworthiness, and lawfulness and then assessing whether researchers and administrators perceive that an environment with high levels of integrity has been created.12(p5)
The sets of competencies do not specify how public health professionals gain ethics competencies in each of the 3 domains, although their acquisition is expected as a competency at graduation or as a practicing professional.
Few studies examined the frequency and nature of ethics training among SPH in the United States or other western schools of public health. In the United Kingdom, Kessel13 reported that 12 of 23 (52%) public health graduate programs reported that they include public health ethics topics in their curricula and that ethics was a fully or partially required course in 43% of programs. Content and nature of the courses were inconsistent. Coughlin et al.14 surveyed US SPH in 1996 and reported that 1 of 24 SPH accredited at that time required an ethics course for all students. Seven other SPH required a course for MPH or doctoral students. A total of 13 of 24 (54%) SPH required ethics instruction for graduation (9 for MPH students and 4 for doctoral students). Elective courses in ethics were offered in 14 (58%) SPH. The authors recommended developing model curricula in public health ethics.
In 2002, Callahan and Jennings15 proposed advancing ethics in public health and encouraged SPH to give priority to ethics in their curriculum development. In 2003, the Institute of Medicine recommended that ethics be an integral part of graduate public health curricula.2 Accordingly, we examined the extent to which accredited SPH adopted ethics courses in their curricula in the academic year 2010–2011.
METHODS
We reviewed the published public health code of ethics and 3 sets of published competencies for public health professionals to identify the formal expectations of ethical competence. We categorized each ethics-related competency into 1 or more of the 3 ethics domains (professional, public health, or research as previously defined). These 3 domains reflect the comprehensive set of expectations related to ethics knowledge and competency for public health professionals. We categorized competencies that contained expectations in more than 1 of these domains into both (or all 3) domains. When investigators categorized competencies differently (in 8 instances), we reexamined the categorization and determined whether the competency fit in more than 1 domain.
We also reviewed the 2010–2011 course requirements of the 46 North American graduate SPH accredited by the Council of Education on Public Health as reported on each school’s Internet site during February 2011. We categorized each school’s ethics training requirement into “required” if an ethics course was required for any student (master’s or doctoral level) for graduation, “not required” if an ethics course was not required for graduation, and “undetermined” if we were unable to ascertain this information. We also attempted to ascertain whether elective ethics courses were offered at schools that did not require an ethics course for graduation. We ascertained the topics covered by reviewing course titles and brief course descriptions when that information was available on the school’s Internet site.
RESULTS
We determined that 8 principles from the Code of Ethics fit into the ethics domains we defined (Table 1), 3 of which mapped to more than 1 domain. In addition, we identified 9 ASPH MPH competencies and 9 ASPH DrPH competencies related to ethics (5 of which mapped to more than 1 domain), as well as 5 of the CDC and CSTE competencies (2 of which mapped to more than 1 domain), and 16 of the PHF COL competencies that fit into the ethics domains (Table 1), 1 of which mapped to more than 1 domain.
TABLE 1—
Number of Ethics Competencies by Domain as Expected for 2010–2011 Graduates of Accredited Schools of Public Health, North America
| Domain |
|||
| Ethics Competencies | Professional Ethics | Research Ethics | Public Health Ethics |
| Code of public health ethics4 | 5 | NA | 6 |
| ASPH competencies for MPH and DrPH5,6 | 9 | 4 | 10 |
| CDC/CSTE competencies for applied epidemiologists7 | 2 | 4 | 1 |
| Council on Linkages between Academia and Public Health Practice8 | 15 | 1 | 1 |
Note. ASPH = Association for Schools of Public Health; CDC = Centers for Disease Control and Prevention; CSTE = Council of State and Territorial Epidemiologists; NA = not applicable. Reported numbers indicate the number of competencies categorized into each domain; 11 competencies fit into more than 1 domain.
For the 2010–2011 academic year, we determined that 23 of 46 (50%) accredited SPH required a course in ethics for graduation from either a master’s or doctoral program. Fewer schools (21; 45.7%) did not require a course, and we were unable to determine this requirement for 2 (4.3%) schools. Of the 23 schools with required courses, 1 school required all graduate students (master’s and doctoral level) to complete 1 ethics course to graduate, 4 schools required all MPH students to complete an ethics course, 2 schools required all DrPH students to complete an ethics course, and 1 school required all doctoral-level students (e.g., PhD, ScD, or DrPH) to complete an ethics course. The remaining 15 schools required completion of an ethics course as required by the students’ departmental affiliation, usually departments of health policy.
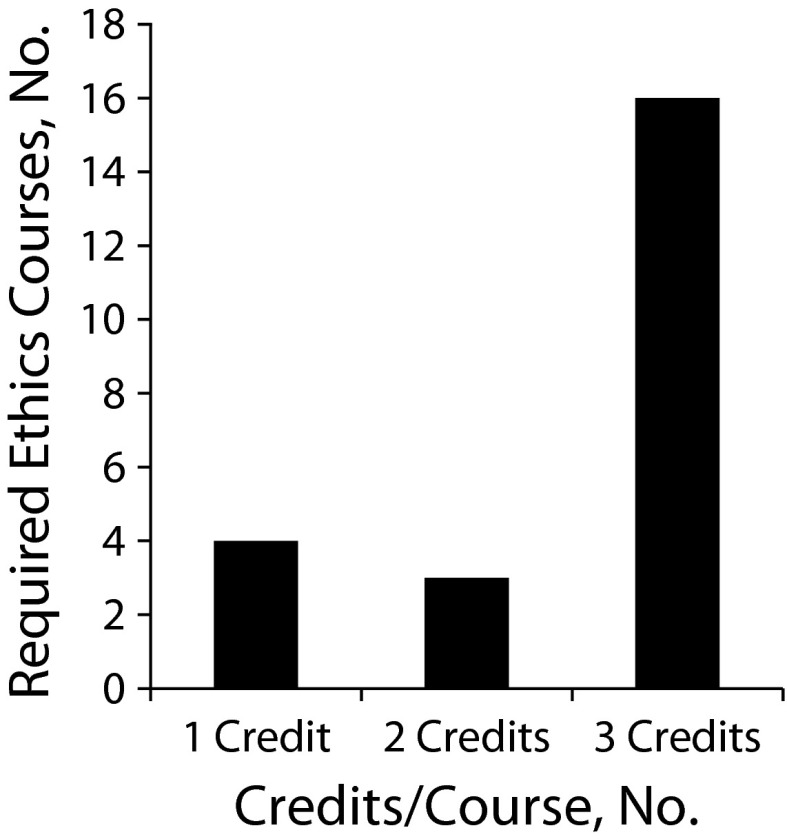
Credit hours of required ethics courses varied from 1 to 3 (Figure 1), with the majority of schools requiring 3-credit hour courses. Topics covered in the ethics courses, which we inferred from course titles and descriptions, included professional ethics, public health ethics, research ethics, general ethics, law and ethics, health and human rights, and bioethics. Certain courses appeared to cover a single topic or domain (e.g., a course labeled Research Ethics), whereas others appeared to address multiple domains (e.g., a course labeled Issues in Public Health Ethics).
FIGURE 1—
Number of credit hours for required ethics courses in 23 of 46 accredited graduate schools of public health, 2010–2011, North America.
Note. Twenty-one schools of public health do not require an ethics course; 2 schools’ data were unavailable.
DISCUSSION
There are documented expectations that public health professionals be proficient in professional, research, and public health ethics, yet only half of accredited SPH require coursework in this area. Although the number of accredited SPH in North America approximately doubled since 1996,14 the proportion of schools that require ethics courses for all students in 2010–2011 remained stable or decreased slightly compared with the mid-1990s.
As a result of these findings, we reviewed and discussed existing literature on ethics instruction to create our recommendations. Practitioner proficiency in ethics in public health requires training similar to the acquisition of other skills—didactic courses, practical training in applying classroom lessons to actual cases, and cultivating interest in developing expertise in ethical decision-making. Improving proficiency will improve our ability to identify, discuss, and address ethics problem so we can implement ethical public health solutions. The first step in this process, including our study, is to identify gaps between expectations of practitioner performance and graduate level course content in SPH.
Limitations
One limitation of our study was that we collected data from SPH Internet sites without confirming with school representatives that courses were being taught as described online. Although we had no reason to believe that the posted information was inaccurate, validation of the fidelity of course implementation was beyond the scope of this study. Posted requirements reflected the academic year (2010–2011); therefore, the data were recent. We were unable to ascertain whether an ethics course was required for 2 schools on the basis of information posted on the school’s Internet site or upon follow-up by telephone. We were unable to determine by our Internet search the extent to which ethics instruction was integrated into other courses, which might replace a focused ethics course, but no mention of this type of “ethics across the curriculum” was apparent on any of the sites. Also, we were unable to determine whether the courses were offered by full-time or part-time adjunct faculty, which might indicate the extent to which ethics courses or topics were infused throughout the curriculum. The nature of our approach provided a useful initial look into existing ethics courses, but we were unable to ascertain detailed information about the content or quality of instruction. Further research on this topic is needed. We examined only accredited graduate SPH to keep our analysis comparable with previous work on this topic,14 leaving out undergraduate programs for which competencies are not fully developed, as well as graduate programs that are not within an SPH. Finally, although this type of review cannot evaluate the value of teaching the existing ethics competencies, or if in fact the various codes of ethics are being taught, it can provide information on whether the infrastructure exists currently in SPH for public health ethics education.
Recommendations
Training and skill building are critical for preparing public health professionals with the skills they need to navigate the complex ethical decision-making process encountered in public health. We recommend an integrated, 3-pronged approach to developing skills in ethical analysis and the habit of ethical conduct: first, a standalone ethics course; second, integration of ethics across the curriculum; and third, ethics “boosters” during employment, in places where public health scientists and practitioners work. First, to build foundational skills, we recommend a standalone course that covers the 3 ethics domains and develops essential skills that students will use to identify and evaluate ethical dilemmas in other courses. An analogy is the fundamental mathematics course that is essential for learning mathematics as well as for succeeding in other courses, including epidemiology and statistics. Second, we recommend the foundational course be paired with an integration of ethics into other courses in the public health curriculum, revealing authentic ethical dimensions of public health in, for example, epidemiology, biostatistics, and environmental health. Integrating ethics training into students’ practicum requirements reflects ASPH’s recommendation for practical learning of competencies through practicum experiences.16 Similar to how students apply their newly acquired epidemiology skills in a real-world setting, for example, practicum and field experiences in master’s and doctoral programs should provide opportunities for students to use their ethics decision-making skills in confronting current ethics debates. Third, we recommend that booster lessons in ethics be integrated with other in-service training where public health scientists and practitioners work, whether at the local, state, tribal, federal, or global levels, in government, as well as in other organizations. This postgraduate continuing education in ethics might include seminars, journal clubs, or partnership with a university-based ethics institute. It is our hope that both sets of instruction (formal coursework and booster lessons in the practice world) would inform each other to create practical and useful instruction. Additionally, ethics instruction in SPH could be bolstered greatly by ethical behavior of faculty and supervisors who model positive attitudes toward ethics requirements and apply the ethics instruction to assess and resolve ethical concerns in academia, research, and practice.17 Finally, it would be helpful for an accrediting or other central educational organization to routinely monitor the requirements and content of public health ethics instruction.
Our recommendations can be debated and evaluated in terms of their effectiveness in enhancing ethical competence of public health professionals. Debate exists regarding whether a standalone course is a wise approach for ethics education.18 Adding another required course that competes for time in an already densely packed curriculum can be challenging. A single course might give students the impression that ethics is a separable, distinct topic about which one can learn in a 3-credit hour course and is otherwise unrelated to other professional aspects. A fully integrated approach to ethics instruction requires coordination and commitment from faculty in all SPH departments to address an area in which they likely have little training or expertise.18 A combination of a foundational course and a coordinated effort to identify and address ethics aspects in all areas of the curriculum with continuing education in the real-world setting of public health research, surveillance, practice, or policy can enhance ethical competence of public health professionals. This competency is critical, whether to address historical implementation of public health projects,19 or to address current ethics questions in public health research,20 surveillance,21 practice,22 or policy.23
To evaluate the effectiveness of our 3-pronged approach to develop the ethical competence of public health professionals, we have the opportunity for a natural experiment as schools without a required course begin to implement the requirement. A 4-component model for developing basic ethical dimensions that are amenable to measurement and evaluation has been proposed24 and could be applied in a pre- and postgraduate program study design. This model outlines 4 essential processes, which could be adapted to examine ethical skills—including recognizing ethical concerns, judging ethically right actions, prioritizing ethical values, and demonstrating courage and conviction to implement ethical behavior—that must be fostered to develop comprehensive ethical judgment.19 These ethical skills could be measured for each of the 3 prongs in our approach to reveal the additional skills each adds. Also, evaluating these essential ethical skills among persons who received their ethics training on the job after their graduate programs and those exposed to the ethics booster training would be helpful. Empirical evidence gathered from public health professionals who have and have not received academic or in-service training can provide information on which to base curriculum development for both academic and practice-based ethics training.
Conclusions
The code of ethics and sets of competencies for public health professionals include clear expectations for proficiency in professional ethics, research ethics, and public health ethics, but do not prescribe how one acquires these skills. Graduate training in public health provides an opportunity for exposure to ethics concepts and development of foundational skills in the 3 ethics domains. Half of the accredited SPH require at least some students, depending on program and departmental affiliation, to take an ethics course, leaving half of the schools not requiring an ethics course. Our study also showed that course content varied substantially, from a single topic (e.g., research ethics in courses entitled “Regulations in Human Subjects Research”) to broad topics (e.g., courses entitled “Issues in Public Health Ethics”). Courses appearing to cover all 3 ethics domains mentioned in the competencies were rare. Our study results also showed that modest progress has been made in public health instruction since the surveys of the past 2 decades. Public health practitioners must be competent in public health ethics to assess and address the ethical dimensions that are intertwined in public health research, surveillance, practice, and policy. Fully integrating ethics instruction through formal coursework, infusion across curricula, and providing ethics boosters in the workplace can move us closer toward improving the ethics education of the public health workforce. Our 3-pronged practical recommendations are intended to enhance ethical competence of public health professionals.
Human Participant Protection
No protocol review was necessary because this project did not involve human research participants.
References
- 1.Centers for Disease Control and Prevention 60 years of public health science at CDC. MMWR Morb Mortal Wkly Rep. 2006;55(1):1–516410759 [Google Scholar]
- 2.Institute of Medicine Who Will Keep the Public Healthy? Washington, DC: The National Academies Press; 2003 [Google Scholar]
- 3.Lee LM. Public health ethical theory: review and path to convergence. J Law Med Ethics. 2012;40(1):85–98 [DOI] [PubMed] [Google Scholar]
- 4.Thomas JC, Sage M, Dillenberg J, Guillory VJ. A code of ethics for public health. Am J Public Health. 2002;92(7):1057–1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calhoun JG, Ramiah K, Weist EM, Shortell SM. Development of a core competency model for the master of public health degree. Am J Public Health. 2008;98(9):1598–1607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Association for Schools of Public Health (ASPH). Doctor of public health (DrPH) core competency model. Washington, DC: ASPH; 2010. Available at: http://www.asph.org/document.cfm?page=1004. Accessed August 15, 2011.
- 7. Centers for Disease Control and Prevention (CDC), Council of State and Territorial Epidemiologists (CSTE). Competencies for applied epidemiologists in governmental public health agencies. Atlanta, GA: US Department of Health and Human Services, CDC; 2008. Available at: http://www.cdc.gov/AppliedEpiCompetencies. Accessed August 16, 2011.
- 8. Council on Linkages Between Academia and Public Health Practice. Core competencies for public health professionals. Washington, DC: Public Health Foundation; 2010. Available at: http://www.phf.org/resourcestools/pages/core_public_health_competencies.aspx. Accessed July 26, 2012.
- 9.Thomas J. Skills for the ethical practice of public health. Washington DC: Public Health Leadership Society; 2004; Available at: http://phls.org/CMSuploads/Skills-for-the-Ethical-Practice-of-Public-Health-68547.pdf. Accessed August 16, 2011 [DOI] [PubMed] [Google Scholar]
- 10.Hensyl WR, Stedman’s Medical Dictionary. 25th ed Baltimore, MD: Williams & Wilkins; 1990 [Google Scholar]
- 11.Gostin LO. Public health law, ethics, and human rights: mapping the issues. : Gostin LO, Public Health Law and Ethics: A Reader. Berkeley, CA: University of California Press; 2002:12:1–22 [Google Scholar]
- 12.Institute of Medicine Integrity in Scientific Research: Creating an Environment That Promotes Responsible Conduct. Washington, DC: The National Academies Press; 2002 [PubMed] [Google Scholar]
- 13.Kessel AS. Public health ethics: teaching survey and critical review. Soc Sci Med. 2003;56(7):1439–1445 [DOI] [PubMed] [Google Scholar]
- 14.Coughlin SS, Katz WH, Mattison DR. Ethics instruction at schools of public health in the United States. Am J Public Health. 1999;89(5):768–770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Callahan D, Jennings B. Ethics and public health: forging a strong relationship. Am J Public Health. 2002;92(2):169–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Association of Schools of Public Health (ASPH), Centers for Disease Control and Prevention (CDC), Council for State and Territorial Epidemiologists (CSTE). Applied epidemiology competencies curriculum and practicum project. Task Force Report. Washington DC: ASPH, CDC, CSTE; 2008. Available at: http://www.asph.org/userfiles/AEC-Task-Force-Rpt-08-FINAL.pdf. Accessed August 16, 2011.
- 17.Hyder AA. Ethics and schools of public health [letter]. Am J Public Health. 2000;90(4):639–640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas JC. Teaching ethics in schools of public health. Public Health Rep. 2003;118(3):279–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frieden TR, Collins FS. Intentional infection of vulnerable populations in 1946-1948: another tragic history lesson. JAMA. 2010;304(18):2063–2064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Semaan S, Santibanez S, Garfein R, Heckathorn D, Des Jarlais DC. Ethical and regulatory considerations in HIV prevention studies employing respondent-driven sampling. Int J Drug Policy. 2009;20:14–27 [DOI] [PubMed] [Google Scholar]
- 21.Lee LM, Heilig CM, White A. Ethical justification for conducting public health surveillance without patient consent. Am J Public Health. 2012;102(1):38–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Semaan S, Leinhos M. The ethics of public health practice for the prevention and control of sexually transmitted diseases. : Aral S, Douglas J, Lipshutz J, Behavioral Interventions for Prevention and Control of Sexually Transmitted Diseases. New York, NY: Springer-SBM; 2007:517–548 [Google Scholar]
- 23.Branson B, Semaan S. HIV screening in health care settings in the United States. Virtual Mentor. 2009;11(12):974–979 [DOI] [PubMed] [Google Scholar]
- 24.Bebeau MJ, Rest JR, Narvaez D. Beyond the promise: a perspective on research in moral education. Educ Res. 1999;28(4):18–26 [Google Scholar]