Abstract
Potential items to be included in an HIV Treatment Optimism scale were reviewed by 17 HIV-positive gay and bisexual men (GBM), resulting in a 21-item test instrument. After pilot testing, data were collected from a multi-city sample of high-risk HIV-positive GBM (n = 346), who were currently on treatment and were recruited to attend a two-day sexual health seminar. The scale items were analyzed utilizing Principal Components Analysis and reliability testing. The factor analysis resulted in the development of three separate scales. The Susceptibility scale contained 10 items associated with a belief that HIV is less transmissible while on HIV treatment. The Condom Motivation scale contained five items addressing a decreased motivation to use condoms while on treatment and the Severity scale contained four items associated with a decreased sense of the severity of an HIV diagnosis. Reliability coefficients (α ) and mean inter-item correlations (M) for the three scales were acceptable (Susceptibility, α = 0.86, M = 0.39; Condom Motivation, α = 0.84, M = 0.50; Severity, α = 0.71, M = 0.37). Combined as one scale, the reliability coefficient was respectable (α = 0.76), but the mean inter-item correlation was 0.14. Based on this analysis, use of a single measure was not supported and three separate scales were developed. The scales were equivalent across racial groups except White men were more like to report a decreased motivation to use condoms compared to Black or Latino men. Three separate scales addressing beliefs about the transmissibility of HIV while on treatment (Susceptibility), the quality of life while on HIV treatment (Severity) and the motivation to use condoms consistently while on treatment (Condom Motivation) may be better markers for assessing optimistic beliefs about HIV treatment among HIV-positive GBM.
Keywords: HIV optimism, gay men, HIV, scale development
Introduction
Since the successful introduction of protease inhibitors as primary HIV treatment was reported in 1996 (Hammer, 1996), researchers and HIV prevention specialists have speculated about the possible role that HIV treatment optimism might play in the continuing sexual risk and HIV transmission among men who have sex with men (MSM; Kelly, Otto-Salaj, Sikkema, Pinkerton, & Bloom, 1998; Rabkin & Ferrando, 1997).
Among HIV-positive MSM, research that has focussed on the association between treatment optimism and sexual risk has been inconclusive. While several studies found an association (Dukers et al., 2001; Ostrow et al., 2002; Vanable, Ostrow, McKirnan, Taywaditep, & Hope, 2000), other evidence exists that increased optimism was not associated with risk (Cox, Beauchemin, & Allard, 2004; Remien, Halkitis, O’Leary, Wolitski, & Gomez, 2005) and that being on HIV treatment may actually be associated with an increase in preventive health behaviors (Nollen et al., 2002; Vanable, Ostrow, & McKirnan, 2003). A recent meta-analysis of treatment optimism studies also found no increase in sexual risk among HIV-positive persons who were on HIV treatment (Crepaz, Hart, & Marks, 2004), when compared with those who were not HIV-positive.
One potential reason for the divergent reported findings may be the vastly different measurements used to assess for HIV treatment optimism. Previous measurement instruments have had several limitations. For instance, some initial research was focussed solely on the association between a lower viral load and sexual risk (Dukers et al., 2001). This limits our understanding of any actual beliefs associated with a lowered viral load or the actual risk behavior.
Most measurement research on treatment optimism utilized components of the Health Belief Model (Rosenstock, Strecher, & Becker, 1994) to test for optimistic beliefs about HIV (International Collaboration on HIV Optimism, 2003). Specifically, concepts utilized are severity, which is based on the notion that having HIV is seen as less grave than it was prior to the advent of these treatments, and susceptibility which is the concept that if one is on treatment and one’s viral load is lowered or “undetectable” one is less susceptible to transmit HIV to sexual partners.
There currently exists no scale to assess for treatment optimism among HIV-positive MSM. The lack of a scale for HIV-positive MSM may account for some of the discrepancies in the findings, as the issue of severity (how severe is living with HIV) is likely to be different for those who are diagnosed with HIV than those who are not. Some scales have used slightly ambiguous terms that may confound the issue of transmission with severity. For example, Elford, Bolding, and Sherr (2002) reported that HIV-positive MSM were more likely to report an increase in optimism. However, items that focussed on severity such as “I am less worried about HIV infection than I used to be” (Elford et al., 2002) could be related to living with HIV (severity) or transmission of HIV (susceptibility). For HIV-positive MSM, being less worried about HIV might be more related to the medical manifestations of untreated HIV disease. Thus, testing for severity among HIV-positive MSM requires the inclusion of one’s perceived health status.
Several studies that reported increased optimistic beliefs among MSM reported acceptable psychometric properties of their scales, such as alpha coefficients (Ostrow et al., 2002; Van de Ven, Crawford, Kippax, Knox, & Prestage, 2000; Vanable et al., 2000), however, none were specific to HIV-positive MSM.
Many previous measures of optimistic HIV treatment beliefs included only two phrases associated with treatment optimism (Huebner, Rebchook, & Kegeles, 2004). It is likely that one or two statements will not adequately encompass all the beliefs associated with treatment optimism, or that these beliefs will endure over time as the novelty of highly active antiretroviral therapy (HAART) diminishes. More detailed scale items may be useful for measuring this construct. In addition to including items that assess HIV-positive MSM’s level of Severity while on treatment, it is essential to ask those who are living with HIV if they perceive any change in their motivation to use condoms, as motivation is a critical component of behavior change. A final concern about the measures of treatment optimism is that they may not measure the construct adequately for ethnic minority populations. The overwhelming majority of the research conducted in this area did not identify the racial make up of their samples (International Collaboration on HIV Optimism, 2003; Ostrow et al., 2002; Van de Ven, Kippax, Knox, Prestage, & Crawford, 1999) and of those that did, the samples were mostly white men (Elford et al., 2002; Huebner & Gerend, 2001; Kalichman, Nachimson, Cherry, & Williams, 1998; Vanable et al., 2000). Since men of color are experiencing disproportionately higher rates of HIV infection, it may be that treatment optimism takes different forms in these populations, and may have more profound impact on risk behavior.
The above literature indicates the need for the development of a robust measure of treatment optimism. In the present study, we are reporting on the development of a treatment optimism scale specifically for HIV-positive MSM. We attempted to mitigate the limitations of previous research in several ways. This scale development study focussed solely on high-risk HIV-positive men in the USA who are currently on treatment. We included items that address the perceived level of severity of living with HIV while on treatment as a component of optimistic beliefs and items that focussed on changes in motivation to use condoms as a result of optimistic beliefs about HIV treatment. We utilized a large multi-city sample to increase the generalizability of the findings and we included large numbers of African American, Latino, and White men to evaluate whether optimism varies by racial/ethnic group. We also analyzed the reliability of the scales using both standard reliability measures and inter-item correlations.
Methods
Qualitative development of study instrument
Seventeen HIV-positive gay and bisexual men (GBM)/MSM participated in a focus group to review potential items to be used in a Treatment Optimism scale that were suggested from previous research, with some modifications to reflect the experience of HIV-positive MSM (Huebner & Gerend, 2001; Van de Ven et al., 1999; Vanable et al., 2000). Participants assisted in assessing the appropriateness, readability, and structural organization of the items, as well as generating other items. The items included in the proposed scale reflect many of the issues brought up by the participants, particularly those related to severity, susceptibility, and motivation to use condoms now that we have treatment. Although, condom use motivation is not a component of the health belief model, it has been reported to be linked to treatment optimism (Nollen et al., 2002; Vanable et al., 2003), and therefore, some items reflecting this concept were included in the scale.
Quantitative instrument development
A 21-item, seven-point Likert scale was utilized to allow for a range of responses (1 = Strongly Disagree; 7 = Strongly Agree).1
Study population
The scale data were collected at baseline from 346 MSM attending a two-day sexual health intervention in Boston, Los Angeles, Houston, and New York, four cities with high HIV incidence. Eligibility criteria included being an HIV-positive male, at least 18 years of age, and having had at least one incident of unprotected anal intercourse in the past year. All protocols and procedures, as well as the content of the study instrument were approved by the Human Subjects Protection Institutional Review Board at the University of Minnesota, as well as community-based partnering agencies (as appropriate).
Treatment optimism scale factor analysis
The analysis was conducted with SPSS (version14) and only those men with complete scale item data were included in the factor analysis (n = 303). Principal Components Analysis (PCA) extraction with a varimax orthogonal rotation was the method utilized because it is known to more likely provide a factor solution (Nunnally & Bernstein, 1994; Preacher & MacCallum, 2003).
Results
Study population characteristics
The sample (Table 1) was racially diverse (48% African American, 25% Latino, 23% White, and 5% Asian, Pacific Islander, Native American, Mixed or other). Participants were well-educated (67% reported at least some college), and most were on disability (53%) with a median annual income of $10,000 (Interquartile Range – IQR; $5000–$20,000). The median age in the sample was 43 (IQR 38–48), and 82% of the sample identified as gay/same gender loving. The median number of years since HIV diagnosis was 12 (IQR 7–16), and the median number of months on treatment was 70 (IQR 30.5–117.5). Of the 539 total participants in the four city trials, 346 (64%) answered all the questions and were included in the analysis.
Table 1.
Demographic characteristics of participants (n = 346).
| Characteristic | n | % |
|---|---|---|
| Age at time of survey (years) | ||
| 21–29 | 13 | 4 |
| 30–39 | 101 | 29 |
| 40–49 | 159 | 46 |
| 50–9 | 72 | 21 |
| Race/ethnicity | ||
| White | 80 | 23 |
| African American | 164 | 48 |
| Latino/Hispanic | 85 | 25 |
| Other (Asian Pacific Islander, Native American, Multiple) | 16 | 5 |
| Education | ||
| High-school graduate or less | 129 | 37 |
| At least some college | 217 | 63 |
| Employment status | ||
| Employed at least part time | 84 | 24 |
| On disability | 183 | 53 |
| Other (retirees, students) | 79 | 23 |
| Income | ||
| $0–$5000 | 72 | 26 |
| $5001–$10,000 | 77 | 28 |
| $10,001–$20,000 | 70 | 25 |
| $20,001–$150,000 | 59 | 21 |
| Sexual orientation | ||
| Gay/same gender loving | 265 | 81 |
| Other (straight, bisexual) | 61 | 19 |
| Comfort with sexual orientation | ||
| Very uncomfortable | 75 | 22 |
| Intermediate | 97 | 28 |
| Very comfortable | 170 | 50 |
| Alcohol frequency over last three months | ||
| Never | 109 | 32 |
| Moderate (<2–3 times a month) | 129 | 38 |
| Regular (1–2 times a week to everyday) | 104 | 30 |
| Drug use frequency over last three months | ||
| Never | 143 | 41 |
| At least once | 203 | 59 |
| Viral load | ||
| <50: undetectable | 205 | 70 |
| >50: detectable | 88 | 30 |
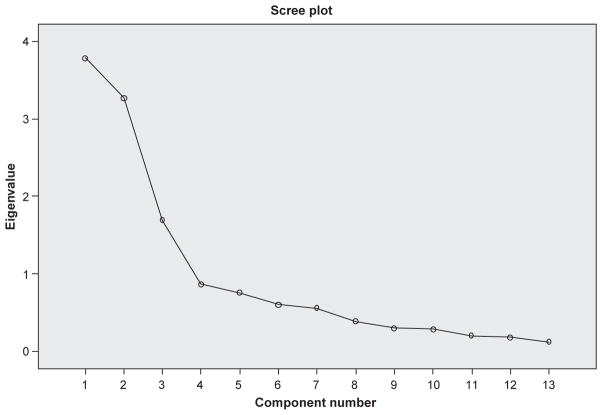
Initial analysis of eigenvalues and scree plot (Figure 1) suggested a 3, 4, or 5 factor solution could all be potentially good fits for the data. The deciding factors were the interpretation based on theory, interpretability of the factors, a minimum of three items loading (>0.35) on each factor, the examination of the scree plot (Figure 1), and the relatively low eigenvalues associated with the fourth and fifth factors. Because it was assumed that the factors would address the concepts of Severity and Susceptibility as well as Condom Motivation while on treatment, the PCA was run using the three-factor model and removing items that did not load highly on any of the three factors. In the final PCA (using orthogonal rotation, forcing a three-factor structure, and eliminating two items which did not load above 0.35 on any factor in the first run), no items loaded higher than 0.35 on more than one factor (Table 2). This summary accounted for 53.5% of the variance.
Figure 1.
Treatment optimism scale scree plot (n = 346).
Table 2.
Summary of items and factor loadings for Varimax orthogonal three-factor solution for the treatment optimism questionnaire (n = 303).
| Component
|
Communality | |||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| 122. On treatment less likely to transmit HIV during RAS | 0.81 | 0.67 | ||
| 125. Treatment makes condom use less important for IAS | 0.80 | 0.65 | ||
| 124. On treatment less likely to transmit HIV for oral sex | 0.78 | 0.61 | ||
| 126. Treatment makes condom use less important for RAS | 0.77 | 0.60 | ||
| 123. On treatment less likely to transmit HIV for IAS | 0.73 | 0.54 | ||
| 117. Condom use for RAS less important | 0.66 | 0.50 | ||
| 116. Condom use for IAS less important | 0.64 | 0.44 | ||
| 121. On treatment less concern about STD transmission | 0.62 | 0.39 | ||
| 110. UVL less likely to transmit | 0.45 | 0.21 | ||
| 112. AIDS nearly cured | 0.37 | 0.24 | ||
| 129. Less motivation to use condoms for RAS-2 partners | 0.87 | 0.77 | ||
| 128. Less motivation to use condoms for IAS-1 partners | 0.85 | 0.74 | ||
| 130. Less motivation to use condoms for IAS-2 partners | 0.83 | 0.71 | ||
| 127. Less motivation to use condoms for RAS-1 partners | 0.81 | 0.67 | ||
| 113. Always using condoms good (reverse coded) | 0.43 | 0.21 | ||
| 136. On treatment, feel healthier | 0.83 | 0.70 | ||
| 139. On treatment, life better | 0.81 | 0.62 | ||
| 137. On treatment, enjoy sex more | 0.76 | 0.61 | ||
| 111. HIV drugs improve lives | 0.46 | 0.23 | ||
Note: Component loadings less than 0.35 have been suppressed. RAS, receptive anal sex; IAS, insertive anal sex; UVL, undetectable viral load.
The items that loaded onto these three factors were more closely scrutinized to assess whether they clustered together in an interpretable manner. The items that loaded onto the second factor, Condom Motivation, all addressed motivation to use condoms now that we have treatment. This concept is consistent with the Theory of Reasoned Action (Fishbein & Middlestadt, 1989). Thus, it appears that these three sub-scales address the two constructs from the Health Belief Modal as well as the motivation construct from the Theory of Reasoned Action.
Internal consistency reliability for this scale and its sub-scales, were assessed with Cronbach’s alpha (Cronbach, 1951) and because alpha values are largely influenced by number of items comprising a scale, the mean inter-item correlations were also examined.
Reliability coefficients for the three scales (Susceptibility, α =.86; Condom Motivation, α = 0.84, and Severity, α = 0.71) were acceptable (see Table 3). The mean inter-item correlations were also considered adequate for the individual scales (Susceptibility, M = 0.39; Condom Motivation, M = 0.50; Severity, M = 0.37). Given that the mean inter-item score for the Susceptibility scale and the Severity scale were similar and the number of items was disparate, the items were considered to have solid reliability. Finally, a reliability analysis was conducted on all three sub-scales together as one scale. The resulting reliability coefficient was respectable (α = 0.76), but with a mean inter-item correlation of 0.14. Based on the results of the PCA, current theory, the obtained alpha coefficients, and the obtained mean inter-item correlations, use of the complete measure without sub-scales was not supported. Therefore, we analyzed the three scales, Susceptibility, Condom Motivation, and Severity, separately.
Table 3.
Summary of factor analysis of treatment optimism scale.
| Factor | # items (score range) | Median (IQRa) | Eigenvalue | % variance | α | Ma |
|---|---|---|---|---|---|---|
| Susceptibility | 10 (7–70) | 24.00 (15.0–36.00) | 4.64 | 24.4 | 0.86 | 0.39 |
| Condom motivation | 5 (5–35) | 24.00 (19.00–31.00) | 3.20 | 16.9 | 0.84 | 0.50 |
| Severity | 4 (4–28) | 12.00 (8.00–16.00) | 2.30 | 12.2 | 0.71 | 0.37 |
| Total | 19 | 53.5 | 0.76 | 0.14 |
IQR, Interquartile range; M, mean inter-item correlation.
These three scales were individually summed to create three separate scale scores for each participant. The data from 346 men were analyzed with these three separate treatment optimism scale scores based on the scales shown in the Appendix 1. Susceptibility is a 10-item scale scored from 7 to 70; Condom Motivation is a five-item scale scored from 5 to 35; and Severity is a four-item scale scored from 4 to 28.
Scale scores were diverse for each of the scales. Susceptibility and Severity were positively skewed. Men tended to cluster with the belief that HIV is not less transmissible while on treatment and that HIV treatment has positively influenced their quality of life. In contrast, Condom Motivation was negatively skewed, such that participants are not less likely to use condoms now that we have treatment. The median scale score (24) for Susceptibility was lower than the scale midpoint (31.5) and the interquartile range was low. The median scale score for Condom Motivation was higher than the potential midpoint (24). The median Severity scale score was exactly at the scale midpoint (12).
There were no significant differences among demographic variables and the scale scores of Susceptibility and Severity. However, utilizing Kruskal–Wallis tests to look at differences among the demographic groups and Condom Motivation found that White men were more likely to report a decreased motivation to use condoms in the era of HAART compared to Black men and Latino men (χ2(2) = 8.02, p = 0.02). In addition, men in the highest quartile income bracket also reported a decrease in motivation compared to the middle-income brackets (χ2(3) = 9.10, p = 0.03). Those with at least some college education also reported a decrease in condom motivation compared to those with no college education (Mann–Whitney U = 11,420.50, p < 0.01).
Discussion
This study endeavored to improve upon the measurement of treatment optimism among HIV-positive MSM, by developing an instrument with detailed concepts associated with beliefs about treatment optimism amongMSM, including areas such as quality of life (severity of living with HIV while on treatment), and normed on a more racially diverse population.
The use of HIV-positive MSM to assist in the drafting of items as well as two pre-tests helped to ensure the scales’ internal and external validity. This analysis used two measures to assess for reliability. If just using the Cronbach’s alpha, this scale would have been thought to be reliable as a total scale, but the limitations of Cronbach’s alpha are important to note when sub-scales have a disparate numbers of items. Although an overall measure was not supported by this analysis, the distinct scales provide rich information regarding the beliefs associated with HIV treatment. The lack of reliability of the overall measure may be related to a number of factors. Perhaps, the constructs of Susceptibility and Severity are distinctly different for HIV-positive MSM when compared to other populations such as HIV-negative men, though this question could not be answered with these data. Condom Motivation was significantly but weakly correlated with Severity (rs = −027, p < 0.001) and Susceptibility (rs = 0.11, p < 0.01). Men who are living with HIV and on treatment did not generally endorse the notion that HIV is less transmissible while on treatment. They did however, generally endorse the notion that HIV is less severe now that we have treatment. In fact, the data were skewed in those very directions. Most participants disagreed that HIV is less transmissible with treatment and agreed that they feel better that we have treatment. Since the men in this study were recruited to participate in a sexual health workshop there may exist some bias toward thinking about condom motivation as part of such a proposed intervention.
This analysis did not support one single scale to address optimism among this sample. It appears that the scales measure slightly different concepts and though correlated, do not altogether work well as a single measurement tool for optimism. Previous research in this area may have oversimplified the analysis and not seen this lack of correlation. By cross validating with two measures we have increased the reliability of our findings. Therefore, the use of three separate scales to assess levels of Susceptibility, Severity, and Condom Motivation is advised.
The skewness of the scales may be a result of a lack of variability among the sample of high-risk highly educated MSM. There appears to be a high rate of belief that HIV is still transmissible while on treatment, that treatment has increased quality of life for those on treatment and that HIV-positive MSM are not less motivated to use condoms now that we have treatment. It would be important to assess for the impact of social norms among this population as these norms may be influencing this tendency to agree that HIV is not less transmissible and that motivation to use condoms has not decreased.
Although, condom motivation was a scale that developed from this study, it is not clear to what degree it is an integral part of treatment optimism. However our data did indicate that condom motivation, when related to anti-retroviral treatment, does differ across racial/ethnic groups and shows differences related to socio-economic status. That is, white, well-educated men in the highest quartile bracket of income tended to report a lower motivation to use condoms now that we have treatment. Evidence exists that African American men in particular do not report lower intent to use condoms nor more sexual risk (Millett, Peterson, Wolitski, & Stall, 2006). Further research is required to understand these differences and whether this decrease in motivation is associated with sexual risk among these various populations. Additional research is necessary to understand the relationship between optimism and behavior based on the context of current scientific knowledge regarding HIV transmission while on treatment.
A strength of this study is its sample composition of urban HIV-positive MSM from diverse racial backgrounds who reported increased risk for serodiscordant unprotected anal intercourse (SDUAI). These findings may not represent other populations who are reporting less risk or who do not live in urban areas. However, due to the limited number of studies looking at racial differences in terms of treatment optimism, this study adds to our understanding of this issue among more racially diverse populations, reflective of epicenters. In addition, the comprehensive scale development process and analysis allows these scales to be utilized to assess for the association between sexual risk and optimistic beliefs about HIV treatment among HIV-positive MSM who are currently on treatment.
Acknowledgments
This study was funded by the National Institute of Mental Health, Office on AIDS Research, grant #MH064412. The Positive Connections Team comprises staff at the University of Minnesota, consultants from AIDS Service Organizations and other universities who provided specialist guidance and direction, and a national leadership team of HIV-positive gay and bisexual men who partnered with this project at every stage from conceptualization to submission of findings. As a multi-site trial, this study was conducted under the oversight of the University of Minnesota Institutional Review Board (IRB), study # 0302S43321, and five other community-based IRBs. We acknowledge with gratitude our community-based partners and staff who included Howard Brown Health Center, Chicago, IL; Gay City Health Project, Seattle, WA; Whitman Walker Clinic, Washington, DC; Fenway Community Health Center, Boston, MA; Gay Men’s Health Crisis, New York, NY; AIDS Project Los Angeles and Black AIDS Institute, Los Angeles, CA; and Legacy Community Health Services, Houston, TX.
Appendix 1. Final 19 items comprising the treatment optimism scale factors
| Item |
| Factor 1: Susceptibility |
| People on combination drug therapy (HAART) are less likely to pass HIV on to an HIV-negative sexual partner through unprotected receptive anal sex (having an HIV-negative sexual partner fuck them without a condom). |
| HIV combination drug therapy (HAART) has made it less important for me to use condoms for insertive anal sex (fucking). |
| People on combination drug therapy (HAART) are less likely to pass HIV on to an HIV-negative sexual partner through unprotected oral sex. |
| HIV combination drug therapy (HAART) has made it less important for me to use condoms for receptive anal sex (getting fucked). |
| People on combination drug therapy (HAART) are less likely to pass HIV on to an HIV-negative sexual partner through unprotected insertive anal sex (fucking an HIV-negative partner without a condom). |
| Because we now have effective treatment for HIV, using condoms every time I have receptive anal sex (being fucked) is less important to me. |
| Because we now have effective treatment for HIV, using condoms every time I have insertive anal sex (fucking) is less important to me. |
| People who are on combination drug therapy (HAART) need to be less concerned about sexually transmitted diseases (such as gonorrhea, or syphilis) than those who are not on combination drug therapy. |
| A person with a viral load that is “undetectable” means that someone with HIV is less likely to transmit HIV to an HIV-negative sexual partner. |
| Having treatments for HIV (like HAART) means that AIDS is very nearly cured. |
| Factor 2: Condom motivation |
| Since we have effective treatment for HIV, I feel more motivated to use condoms with secondary partners each time I have receptive anal sex (getting fucked). |
| Since we have effective treatment for HIV, I feel more motivated to use condoms with my primary partner each time I have insertive anal sex (fucking). |
| Since we have effective treatment for HIV, I feel more motivated to use condoms with secondary partners each time I have insertive anal sex (fucking). |
| Always using condoms for anal sex is good for an HIV-positive person’s health even while on effective therapy. |
| Since we have effective treatment for HIV, I feel more motivated to use condoms with my primary partner each time I have receptive anal sex (getting fucked). |
| Factor 3: Severity |
| Since being on combination drug therapy (HAART) I feel physically healthier. |
| My life is much better now that I am on combination drug therapy (HAART). |
| Since being on combination drug therapy (HAART), I enjoy sex more. |
| HIV effective therapy has made the lives of people living with HIV who take the drugs better. |
Footnotes
A complete listing of original items in the scale is available through the first author.
References
- Cox J, Beauchemin J, Allard R. HIV status of sexual partners is more important than antiretroviral treatment related perceptions for risk taking by HIV positive MSM in Montréal, Canada. Sexually Transmitted Infections. 2004;80(6):518–523. doi: 10.1136/sti.2004.011288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N, Hart TA, Marks G. Highly active antiretroviral therapy and sexual risk behavior. A meta-analytic review. JAMA: Journal of the American Medical Association. 2004;292(2):224–236. doi: 10.1001/jama.292.2.224. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- Dukers NHTM, Goudsmit J, de Wit JBF, Prins M, Weverling G, Countinho RA, et al. Sexual risk behaviour relates to the virologic and immunological improvements during highly active antiretroviral therapy in HIV-1 infection. AIDS. 2001;15(3):369–378. doi: 10.1097/00002030-200102160-00010. [DOI] [PubMed] [Google Scholar]
- Elford J, Bolding G, Sherr L. High-risk sexual behaviour increases among London gay men between 1998 and 2001: What is the role of HIV optimism? AIDS. 2002;16(11):1537–1544. doi: 10.1097/00002030-200207260-00011. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Middlestadt S. Using the theory of reasoned action as a framework for understanding and changing AIDS-related behaviors. In: Mays VM, Albee GW, Schneider SF, editors. Primary prevention of AIDS. Newbury Park: Sage; 1989. pp. 93–110. [Google Scholar]
- Hammer SM. Advances in antiretroviral therapy and viral load monitoring. 11th International AIDS Conference; Vancouver. 1996. Jul, [PubMed] [Google Scholar]
- Huebner DM, Gerend MA. The relation between beliefs about drug treatments for HIV and sexual risk behavior in gay and bisexual men. Annals of Behavioral Medicine. 2001;23(4):304–312. doi: 10.1207/S15324796ABM2304_10. [DOI] [PubMed] [Google Scholar]
- Huebner DM, Rebchook GM, Kegeles SM. A longitudinal study of the association between treatment optimism and sexual risk behavior in young adult gay and bisexual men. Journal of Acquired Immune Deficiency Syndromes. 2004;37(4):1514–1519. doi: 10.1097/01.qai.0000127027.55052.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Collaboration on HIV Optimism. HIV treatments optimism among gay men: An international perspective. Journal of Acquired Immune Deficiency Syndromes. 2003;32:545–550. doi: 10.1097/00126334-200304150-00013. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Nachimson D, Cherry C, Williams E. AIDS treatment advances and behavioral prevention setbacks: Preliminary assessment of reduced perceived threat of HIV-AIDS. Health Psychology. 1998;17(6):546–550. doi: 10.1037//0278-6133.17.6.546. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Otto-Salaj LL, Sikkema KJ, Pinkerton SD, Bloom FR. Implications of HIV treatment advances for behavioral research on AIDS: Protease inhibitors and new challenges in HIV secondary prevention. Health Psychology. 1998;17(4):310–319. doi: 10.1037//0278-6133.17.4.310. [DOI] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Wolitski RJ, Stall RD. Greater risk for HIV infection of black men who have sex with men: A critical literature review. American Journal of Public Health. 2006;96(6):1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nollen NL, Goggin K, Heiland MF, Catley D, Kessler K, Brammer SK, et al. The impact of combination therapy on the health behaviors of HIV+ gay men. AIDS & Behavior. 2002;6(2):131–139. [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric theory. 3. New York: McGraw-Hill; 1994. [Google Scholar]
- Ostrow DG, Fox KJ, Chmiel JS, Silvestre A, Visscher BR, Vanable PA, et al. Attitudes towards highly active antiretroviral therapy are associated with sexual risk taking among HIV-infected and uninfected homosexual men. AIDS. 2002;16(5):775–780. doi: 10.1097/00002030-200203290-00013. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, MacCallum RC. Repairing tom swift’s electric factor analysis machine. Understanding Statistics. 2003;2(1):13–43. [Google Scholar]
- Rabkin JG, Ferrando S. A ‘second life’ agenda: Psychiatric research issues raised by protease inhibitor treatments for people with human immunodeficiency virus or the acquired immunodeficiency syndrome. Archives of General Psychiatry. 1997;54:1049–1053. doi: 10.1001/archpsyc.1997.01830230091013. [DOI] [PubMed] [Google Scholar]
- Remien RH, Halkitis PN, O’Leary A, Wolitski RJ, Gomez CA. Risk perception and sexual risk behaviors among HIV-positive men on antiretroviral therapy. AIDS & Behavior. 2005;9(2):167–176. doi: 10.1007/s10461-005-3898-7. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. The health belief model and HIV risk behavior change. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: Theories and methods of behavioral interventions. AIDS prevention and mental health. New York, NY: Plenum Press; 1994. pp. 5–24. [Google Scholar]
- Van de Ven P, Crawford J, Kippax S, Knox S, Prestage G. A scale of optimism-scepticism in the context of HIV treatments. AIDS Care. 2000;12(2):171–176. doi: 10.1080/09540120050001841. [DOI] [PubMed] [Google Scholar]
- Van de Ven P, Kippax S, Knox S, Prestage G, Crawford J. HIV treatments optimism and sexual behavior among gay men in Sydney and Melbourne. AIDS. 1999;13(16):2289–2294. doi: 10.1097/00002030-199911120-00011. [DOI] [PubMed] [Google Scholar]
- Vanable PA, Ostrow DG, McKirnan DJ. Viral load and HIV treatment attitudes as correlates of sexual risk behavior among HIV-positive gay men. Journal of Psychosomatic Research Special Issue: HIV & Immunology. 2003;54(3):263–269. doi: 10.1016/s0022-3999(02)00483-x. [DOI] [PubMed] [Google Scholar]
- Vanable PA, Ostrow DG, McKirnan DJ, Taywaditep KJ, Hope BA. Impact of combination therapies on HIV risk perceptions and sexual risk among HIV-positive and HIV-negative gay and bisexual men. Health Psychology. 2000;19(2):134–145. doi: 10.1037//0278-6133.19.2.134. [DOI] [PubMed] [Google Scholar]