Abstract
The management of depression and other negative psychological states in cardiac patients has been a focus of multiple treatment trials, though such trials have not led to substantial improvements in cardiac outcomes. In contrast, there has been minimal focus on interventions to increase positive psychological states in cardiac patients, despite the fact that optimism and other positive states have been associated with superior cardiovascular outcomes. Our objective was to develop an 8-week, phone-based positive psychology intervention for patients hospitalized with acute cardiac disease (acute coronary syndrome or decompensated heart failure). Such an intervention would consist of positive psychology exercises adapted for this specific population, and it would need to be feasible for practitioners and patients in real-world settings. By adapting exercises that were previously validated in healthy individuals, we were able to generate a positive psychology telemedicine intervention for cardiac patients that focused on optimism, kindness, and gratitude. In addition, we successfully created a companion treatment manual for subjects to enhance the educational aspects of the intervention and facilitate completion of exercises. Finally, we successfully performed a small pilot trial of this intervention, and found that the positive psychology intervention appeared to be feasible and well-accepted in a cohort of patients with acute cardiac illness. Future studies should further develop this promising intervention and examine its impact on psychological and medical outcomes in this vulnerable population of cardiac patients.
Key words: positive psychology, optimism, cardiovascular disease, acute coronary syndrome, congestive heart failure
Introduction
Negative emotional states are strongly associated with poor outcomes in patients with heart disease. For example, depressive symptoms in cardiac patients are common,1 persistent, 2 and independently associated with negative medical outcomes.3,4 This link between depression and adverse cardiac events appears to be especially strong among patients hospitalized for acute cardiac conditions, such as acute coronary syndrome (ACS) or congestive heart failure (CHF), for whom depression has been repeatedly established as a risk factor for recurrent cardiac events and mortality. 3–5 Other negative psychological states, especially anxiety, have also been associated with the development and progression of cardiac disease,6,7 and anxiety symptoms and disorders have been linked with cardiac-related death.8 However, there have been multiple trials to treat depression and associated conditions in cardiac patients, and depression treatment in heart disease patients has not consistly resulted in improved cardiac outcomes.9–11
In contrast to negative states, positive psychological states, such as optimism, are associated with superior cardiovascular outcomes in those with and without known heart disease. For example, the Women's Health Initiative study of over 97,000 women found that women in the upper quartile of dispositional optimism had a significantly lower incidence of coronary heart disease, cardiac mortality, and all-cause mortality than those in the bottom quartile.12 In patients with known heart disease, optimism, vigor, and well-being have been associated with reduced mortality13 and independently linked with fewer readmissions and increased survival following cardiac surgery.14,15 Indeed, a recent meta-analysis of the relationship between optimism and physical health found that optimism was significantly linked to lower mortality and superior cardiovascular outcomes.16 Other analyses have suggested that a broad range of positive psychological constructs, including positive emotions and subjective well-being, are linked with superior physical health outcomes.17–19 Furthermore, the effects of positive psychological conditions appear to be independent of negative affective states, including depressive symptoms,17,18 suggesting that it is not simply an absence of depression or anxiety that confers the cardiovascular benefit associated with positive emotions.
How might positive psychological states influence cardiac health? First, positive emotions may impact cardiovascular outcomes through health behaviors. Positive psychological states, such as optimism, have been associated with greater adherence to healthy behaviors in persons with and without known heart disease.13,20–22 For example, optimists appear to be more likely to follow a hearthealthy diet,23,24 and less likely to smoke,22 than pessimists. Older adults with higher levels of optimism and/or positive health beliefs also have higher rates of physical activity than those with lower levels.22,24,25 Furthermore, a recent trial found that patients with positive mood prior to cardiac transplant surgery were more likely to adhere to a post-surgical medication regimen at six months.20 In addition to impacting health-related behaviors, these positive emotional and cognitive states may impact physiology. Optimism and related states are associated with healthy autonomic function26 and reduced inflammation.27 Given that autonomic function and inflammation are predictors of adverse cardiac events,27–29 this may also contribute to the link between positive states and cardiac health.
Clearly positive psychological states are important but can they be cultivated or taught? Although a sizeable portion of happiness is explained by static factors (e.g. intrinsic disposition and external life events), it appears that approximately 40% of happiness is directly under one's own control,30 and specific interventions can increase positive emotions and cognitions. In recent years, there has been an emerging focus on positive psychology, a discipline that aims to improve the frequency and intensity of positive emotional experiences. 31,32 Positive psychology interventions have focused on targeted activities in several domains, including altruism (e.g. performing acts of kindness), gratitude (e.g. systematically recalling positive life events), using one's personal strengths in a deliberate manner, and optimism (e.g. imagining positive future outcomes). A recent meta-analysis of over 50 trials of positive psychology interventions in more than 4,000 subjects found that positively-oriented interventions have consistently led to increases in happiness, reductions in depression, and improvements in overall wellbeing. 32 Furthermore, in some cases, such benefits can last months after the intervention. 31,32 Although some resiliency programs in medical patients have included small components of these interventions with good effect,33,34 trials of positive psychology interventions in the medically ill have been exceedingly rare.35
Therefore, there is a clear opportunity to create a novel positive psychology-based treatment for post-ACS and CHF patients with the potential to improve outcomes in a vulnerable population. Positive psychology interventions have not been attempted in this population, and there has been much to learn about the proper composition and feasible delivery of positive psychology interventions when attempting to intervene in medically-ill patients. If an intervention to improve positive emotional experiences were feasible, well-accepted, and successful in improving the intensity and frequency of positive emotions, the intervention could potentially have broad health benefits.
To address this gap in the literature, we had two primary aims. In concert with experts in positive psychology and mind-body medicine, we sought to develop an 8-week telemedicine positive psychology intervention for patients initially hospitalized for ACS or CHF. In addition, our second aim was to create a companion treatment manual that described the rationale and content of the intervention, and that facilitated completion of the intervention exercises. In this paper, we will describe the development of both the intervention and treatment manual that were tailored to the vulnerable population of ACS and CHF patients. We will also briefly describe the results of a small randomized exploratory trial that assessed the feasibility and potential utility of this intervention in ACS and CHF patients.
Materials and Methods
Population for the intervention
The intervention was developed for hospitalized patients with either ACS or CHF. We chose this population and setting for several reasons. First, these two conditions are among the most common causes of admission to cardiac units, and both are associated with poor health-related quality of life, functional impairment, and high rates of hospital readmission and mortality.36,37 Furthermore, a substantial literature links negative emotions (depression) with morbidity and mortality for post-ACS patients and those with CHF,4,5,8 underscoring the high-risk nature of this population and the potential public health benefits of an intervention that could improve emotional states. Finally, hospitalization for an acute medical decompensation can represent a teachable moment during which patients may be more amenable to behavior change and new interventions to improve health status. Therefore, uptake of a new intervention may be more effective in this population versus a cohort with stable disease.
Mode of intervention delivery
To enhance the accessibility of this intervention, we chose to create a phone-based intervention because recently-hospitalized cardiac patients may have significant functional limitations. Interactions by phone (rather than in-person visits) are likely more feasible for such patients. This delivery method also increases our ability to include patients living far from the hospital or those without transportation; any patient with access to a phone can be included. Although internet-based interventions may also be innovative, the telemedicine intervention provides a more personal experience; furthermore, a significant subset of ACS/CHF patients (mean age in our previous studies38,39 was 63 years) will not have ready internet access and thus a phone-based solution would be accessible to a greater number of individuals. This delivery setup also increased feasibility from an interventionalist perspective, as the intervention could be delivered from any private phone rather than a fixed physical setting for which there may be limitations of space or availability.
In addition to the phone-based interaction between study trainer and participant, we created a straightforward written manual that outlined the details of the intervention activities, and their rationale, for participants to review before, during, and after the intervention (see below). We also included supplementary reading for participants who were interested in understanding the broader context of the intervention.
Intervention development team
To ensure that we created an intervention that was grounded in evidence-based interventions yet well-adapted to and feasible for this cardiac population, we established a multidisciplinary team with expertise in several domains. The team included two psychologist researchers (SL, JB) who have substantial experience in positive psychology research in a variety of populations. They ensured that the intervention included well-studied and appropriate positive psychology exercises. Two members of the team (GF, JD) were physician leaders in the Benson Henry Institute for Mind-Body Medicine (BHI) with many years of experience supervising clinical and research behavioral interventions in the medically ill. Finally, two core members of the study team (JH, CM) had considerable experience performing behavioral cardiology research interventions on inpatient cardiac hospital units, including phone-based interventions post-discharge for ACS and CHF patients. This constellation of team members ensured that there would be relevant expertise to carefully develop an appropriate and effective intervention.
Intervention
The intervention was developed to last eight weeks, with weekly exercises and weekly contact between trainer and participant. Each week, participants would complete all aspects of a positive psychology exercise in a single day; the choice of this timing was based on evidence that such clustering of intervention activities is more effective than completing activities over a longer time frame.40 We chose to have participants complete exercises on a weekly basis, rather than more frequently, to make the intervention more feasible for subjects who may have limited energy or time. In addition, some positive psychology trials have found weekly exercises to be more effective than daily exercises in improving positive affect, possibly due to loss of novelty and ‘hedonic adaptation' when tasks are completed every day.30,40
The first session of the intervention, which lasted approximately 45 min, was conducted in-hospital prior to the patient's discharge. During this meeting, the study trainer described the overall procedures of the study, provided the intervention manual, reviewed basic information about positive psychology, and discussed the rationale for the positive psychology intervention. The trainer would then assign the first exercise for the patient to complete, review the exercise, and assign the next week's exercise. After the initial in-hospital session, weekly phone call sessions (approximately 15 min long) were conducted to review the exercise and prepare participants for the next week's exercises. For subjects who were still in hospital at the time of the first scheduled phone call, the session was conducted in person instead of over the phone. Each of the exercises required approximately 20 min of writing about events, acts, goals, and/or feelings, allowing participants to have a physical record of their work.
Selection of the positive psychology exercises to be used in the study was based on several factors. We chose to focus on the positive emotions/cognitions of gratitude, kindness, and optimism in this intervention because of substantial evidence for the efficacy of exercises focusing on these three constructs;30,41–43 we also targeted optimism because this is the positive state most reliably linked to cardiac health.43 Finally, within these parameters, we chose exercises that we thought would be most relevant to patients recently hospitalized with ACS/CHF and those that would be straightforward to complete. The intervention, completed in the same order by all participants, contained four modules (Table 1).
Table 1. Overview of positive psychology exercises.
| Exercise | Brief summary and reason for selection |
|---|---|
| Week 1* (Gratitude): | Subjects recall and record in detail three events in the past week for which they are grateful. |
| Three good things *completed in hospital | Rationale: we chose this as the first exercise to highlight the presence of positive events even during medically stressful times, and because it is straightforward and brief. Cultivating gratitude in similar interventions has been linked to beneficial effects for both mental health (i.e. depression, optimism, well-being, and social engagement)31,40 and physical health/health behaviors (physical complaints, frequency of exercise, amount and quality of sleep).40 |
| Week 2 (Gratitude): | Subjects recall another person's kindness and write a letter that describes their gratitude. |
| Gratitude Letter” | Rationale: this exercise was selected because of its relatively strong effect on mood and well-being. For example, one study found that completing a gratitude letter led to sustained improvement of well-being for up to six months.44 |
| Week 3 (Optimism): | Subjects imagine one's best possible future (over the next five years) with respect to social relationships, and consider how to actualize this future. |
| Best Possible Self (social relationships) | Rationale: this exercise and related exercise is frequently used and is associated with feeling happier, less distressed, and being sick less often; participants have also been found to report interest in continuing this exercise after the intervention is over.42,44,45 |
| Week 4 (Optimism): | Subjects imagine one's best possible self in the future (over the next five years) with regard to mental and physical health and consider how to actualize this future. |
| Best Possible Self (health) | Rationale: same as above. |
| Weeks 5–6 (Altruism): | Subjects perform three kind acts for others within a single day. |
| Three Acts of Kindness | Rationale: prior work has demonstrated that performing and recording one's acts of kindness is associated with improved mood.41 Participants performed all of their kind acts on the same day given the evidence that such clustering is most effective. |
| Weeks 7–8 (Choice): | Subjects repeat exercise of their choice from weeks 1–6, changing specific content of the activity or the recipient of gratitude letter or kind acts. |
| Rationale: prior studies in this area suggest that person-activity fit may moderate the success of psychological interventions and the most effective strategies are those that fit participants' individual needs and areas of weakness.30,40,46 |
Module I (Weeks 1 and 2): Gratitude
Exercise I (Three Good Things), which was completed in hospital, asked patients to recall three good things that had happened that week, despite recent medical events. Participants were instructed to write about three good events and why they happened in as much detail as possible, and to record how the event made them feel at the time and after the event (including while writing about it). This exercise was adapted from successful work previously carried out in other populations that focused on counting blessings and recalling prior good events.30,40–42 It was selected as the first exercise to educate patients about the presence of positive events and emotions in their lives and because it is a simple, relatively brief exercise that could be performed in the context of a single in-hospital, in-person session.
Exercise II (Gratitude Letter) was a letter addressed to a person in the participant's life who did something for which they were grateful. Subjects were asked to describe in specific terms how an individual's behavior had affected their life, why they were grateful, the impact of this act on their current life, and how often the individual's efforts were recalled. Participants were advised that the letter was a private document, not necessarily written to be delivered or shown to anyone (although they were free to do so if they chose). Participants were also asked to note how they felt during and after writing the letter. This activity was selected because of its relatively strong effect on happiness and depression. For example, an internet-based study found that people who completed this exercise were happier and less depressed immediately post intervention compared to a control group, and these improvements were maintained one month later.31 Furthermore, a study that randomly assigned participants to positive activities found that completing a gratitude letter led to sustained improvement of well-being for as long as six months.44
Module II (Weeks 3 and 4): Optimism
Exercise III (Best Possible Self) involved imagining one's best possible future with respect to social relationships. Patients were instructed first to think about their present connection to family members, friends, neighbors, colleagues and other important people in their social network, and then to imagine their ideal life five years in the future in terms of those social relationships. Study participants were next instructed to write, with specific details, about what they had envisioned, and to record how they felt during and after the exercise. The second exercise within this module (Exercise IV) was to imagine one's best possible self in the future with regard to mental and physical health. In this exercise, participants were asked to imagine that everything related to their physical and mental health has gone as well as it possibly could have for the next five years. Again, in as much detail as possible, participants wrote about what they had envisioned and how they felt during and after the exercise. The exercises in this module were selected on the basis of evidence linking optimism and cardiac health,12,43 as well as prior studies using similar interventions to good effect. The Best Possible Self exercise and related exercises in randomized trials has been found to be associated with feeling happier, less distressed, and being sick less often.43,44,46
Module III (Weeks 5 and 6): Kindness
The kindness exercises for this module (Exercises V and VI) used the same activity over both weeks. Specifically, participants were instructed to perform three kind acts for others within a single day because there is evidence that such clustering of acts is most effective.40 They were then asked to record the acts and how they felt during them. We selected this exercise on the basis of experimental work demonstrating that both performing and recording one's acts of kindness is associated with increased happiness.41
Module IV (Weeks 7 and 8): Choice
In the final two weeks of the intervention, participants were allowed to choose and complete exercises from the previous six weeks that they felt best fitted their interests and personality. We allowed patients to choose their own exercises on the basis of evidence that patient-activity match is important to improved well-being and that fit may moderate intervention success.30 Indeed, previous research has shown that the effectiveness of happiness-increasing techniques varies considerably among individuals; the most effective strategies are those that fit participants' individual needs and areas of weakness.30,40,46
Treatment manual
The treatment manual for participants had several sections. In the introductory section, the manual described the overall structure of the 8-week intervention, outlined reasons why positively-oriented exercises may be helpful, explored common myths about the exercises, and prepared participants for the completion of the exercises.
Next, the manual included chapters for each week's exercise. At the beginning of each chapter, a brief educational section described the importance of the positive activity for the corresponding week (e.g. Why does optimistic thinking boost happiness? and Why does doing kind deeds make people happy?). These educational sections were condensed from Dr. Sonja Lyubomirsky's (2008) book The How of Happiness47 and adapted to this specific clinical population. (For sample sections, see Figure 1; the full manual is available from the authors.) The manual then described the specific study exercise for that week, outlined the details of performing and recording the exercise, and provided space to describe the events and feelings it evoked. Finally, the manual ended with a discussion of the value of maintaining positive well-being activities. Evidence for the sustained practice of positive psychology-related interventions has been relatively limited48 but is of clear importance. This section of the manual discussed how participants might develop a structured habit of performing the exercises that would have the greatest impact for them, as well as the best fit with their values, needs, interests, and resources. The manual closed with space to record a plan to complete such exercises over the following month.
Figure 1.
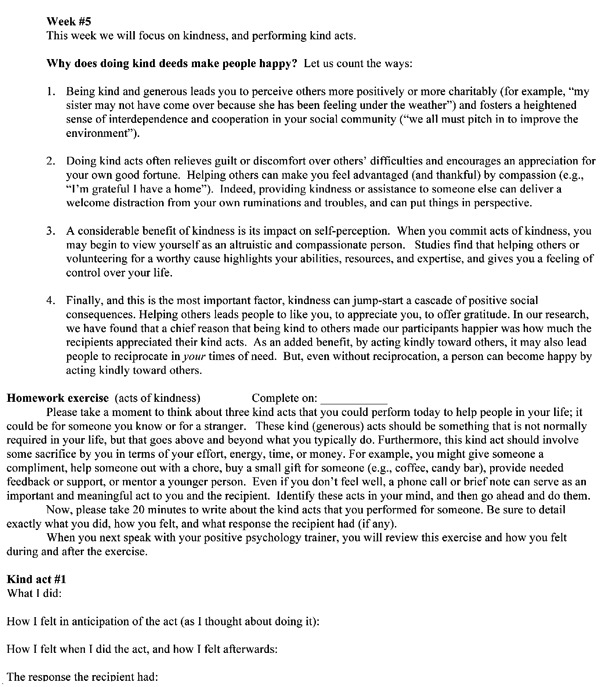
Sample pages from positive psychology treatment manual.
Selection and training of study interventionalist
We chose to utilize a social worker because, as part of their training and practice, most social workers have extensive experience interacting with patients and discussing emotional states in the context of acute stressors, such as medical illness. Because medical social workers are core personnel on cardiac units our intervention would not require the addition of a new care team member, potentially bolstering its feasibility. Finally, social workers are available at a lower cost than registered nurses, physicians, or psychologists, again increasing the intervention's viability and generalizability.
The role of the trainer was not to perform an interpersonal therapeutic intervention, but rather to describe and review exercises performed independently by participants. Thus, the trainer's responsibilities were straightforward and easily learned. The study interventionalist was trained by reading both the treatment manual and book (The How of Happiness) associated with the intervention, attending sessions on positive psychology provided by the BHI, and participating in several meetings with the intervention developers to discuss the book and manual, answer questions, and problem-solve potential issues. Throughout the intervention, the interventionalist was supervised by the principal investigator to discuss patient-specific issues and consulted with the positive psychology experts for clarification of the exercises.
Feasibility trial (exploratory aim)
Once the intervention and manual were created, we assessed its feasibility and potential impact by developing a small, exploratory randomized three-arm trial that included a positive psychology intervention, an active control group, and an attentional control. For each arm, we created treatment manuals that described an 8-week intervention program and listed exercises associated with that program, and compared the three 8-week interventions for patients admitted to one of three inpatient cardiac units for ACS or decompensated heart failure. The trial had a goal recruitment of 30 subjects. Subjects with significant cognitive impairment, medical illness likely to result in death within six months, active suicidal ideation, active substance use disorder, inability to write or use phone, enrollment in similar interventions (e.g. yoga, meditation, positive psychology), or inability to speak English were excluded.
Participants were randomized to one of three arms. The Positive Psychology (PP) intervention was as detailed above. Subjects in this condition were provided with the treatment manual and a copy of The How of Happiness for more information about the rationale and evidence for the interventions they would complete. The Relaxation Response (RR; active control) group utilized a well-validated meditation-based intervention that has led to reduced anxiety and fewer physical symptoms in cardiac patients.49–51 In this group, subjects were initially led through a 20 min relaxation exercise and given a manual describing the exercise and its potential benefits; subjects were then given a CD and instructed to practice daily for 20 min. Weekly calls from the study trainer reviewed progress with completion of the exercises and helped to problem-solve any difficulties in performing the daily exercises. The Recollection (attentional control) intervention, similar to prior control conditions in positive psychology studies,42 had subjects recall and list events that occurred during the previous week without assigning any particular emotion to the events. This intervention had a structure that paralleled the PP intervention with regard to frequency of exercises and review of manual/exercises at weekly calls.
In all three arms, trained study staff met subjects in the hospital, provided the treatment manual specific to their study condition, and completed an exercise. Weekly follow-up exercises were then completed by the participant, recorded in the treatment manual, and discussed by phone with the interventionist (∼20 min) for the remainder of the program.
The primary outcome measures for the pilot study were feasibility (number of weeks during which study exercises were completed in each arm), and global utility (between-group comparison of scores on single-item questions regarding ease of completion, overall utility, increase in optimism, and likelihood of continuing the exercises after eight weeks (all rated on a five-point Likert scale). Subjects also completed secondary outcomes at baseline and eight weeks from study staff who were blinded to the subject's study condition. These measures included measures of depression (Center for Epidemiologic Studies - Depression Scale [CES-D]52), happiness (Subjective Happiness Scale,53 positive affect subscale of CES-D), anxiety (Hospital Anxiety and Depression Scale - Anxiety Subscale54) and mental healthrelated quality of life (Medical Outcomes Study Short-Form 1255 Mental Component Score). The pilot trial was approved by our institution's review board.
Results
In accordance with the primary aim of this investigation, the intervention and treatment manuals for the positive intervention were successfully created. The intervention was then successfully delivered to cardiac inpatients by a trained social worker using the treatment manual. Regarding the feasibility trial (the secondary aim), 30 subjects were recruited and enrolled; 26 completed at least one phone session and 23 of 26 (88%) completed the 8-week follow-up assessment (n=9 positive psychology; n=7 in each of the other arms). Participants in all three groups had relatively high rates of exercise completion, with an overall completion rate of approximately 70% of all exercises over the 8-week period. The completion rate was highest in the PP group (PP, 76.5%; RR, 64.0%; Recollection, 70.9%). At eight weeks, subjects in the PP intervention were more likely to rate the intervention as easy to complete (mean rating 4.22 on a 1–5 Likert scale in the PP group vs 3.86 in other two groups) and globally helpful (mean rating 4.11 on 1–5 Likert scale in PP vs 3.86 and 2.86 in the RR and Recollection groups, respectively). In addition, participants in the PP condition had improved optimism at the 8-week follow up compared with their baseline optimism (PP, 4.00 vs 3.86 and 2.71 in the RR and Recollection groups, respectively). Subjects in the RR group were slightly more likely to report that they would continue the exercises after the study compared to the other groups (PP, 4.22; RR, 4.43; Recollection, 2.14). None of these differences were statistically significant given the very small sample size in this pilot study, but these results show the potential feasibility, acceptability, and utility of the positive psychology intervention in cardiac patients.
For the secondary 8-week outcomes, subjects in the PP intervention had greater improvement in depressive symptoms, anxiety, happiness (CES-D subscale), and health-related quality of life relative to the subjects in the other two groups. The magnitude of differences was greatest between the PP and recollection conditions. RR subjects had greater improvements on happiness assessed with the Subjective Happiness Scale (Table 2).
Table 2. Mean (SD) change score on secondary study outcomes from baseline to eight weeks.
| Measure | Positive psychology (n=9) | Relaxation response (n=7) | Recollection (n=7) | df | F | P | Cohen's d** |
|---|---|---|---|---|---|---|---|
| CES-D | −5.4 (10.7) | −4.7 (7.2) | −2.3 (11.3) | 22 | 0.21 | 0.81 | 0.28 |
| CESD-H | 3.0 (4.0) | 0.9 (2.0) | 0.1 (4.5) | 22 | 1.34 | 0.29 | 0.68 |
| SHS | 1.1 (3.7) | 2.4 (2.2) | −0.5 (2.7) | 22 | 1.53 | 0.24 | 0.49 |
| HADS-A | −2.8 (4.9) | −1.3 (2.0) | −1.7 (6.6) | 22 | 0.20 | 0.82 | 0.19 |
| SF-12 MCS | 5.9 (10.1) | 5.4 (5.9) | −1.3 (13.9) | 22 | 1.10 | 0.35 | 0.59 |
Italics. Denotes the greatest change on each outcome measure.
Comparison of positive psychology versus recollection conditions.
CES-D, Center for Epidemiologic Studies Depression scale; CESD-H, four positive affect (“happiness”) items of the CES-D; HADS-A, Hospital Anxiety and Depression Scale - anxiety subscale; SHS, Subjective Happiness Scale; SF-12 MCS, Mental Component Score of the Short-Form 12.
Discussion
Overall, we successfully developed and implemented a positive psychology-based intervention for individuals with acute cardiovascular disease. We identified empirically-validated exercises to increase positive affective and cognitive experiences that had been used in other populations, and adapted them to create a telemedicine intervention for patients with significant cardiovascular disease. Our multidisciplinary team also created and utilized a companion treatment manual for participants receiving this intervention.
Most previous positive psychology interventions have been conducted in non-clinical populations, or in those without medical illness. To our knowledge, only two interventions using any kind of positive emotion-related interventions in patients with cardiac illness have been studied: a pilot trial aimed at positive affect and self-affirmation in outpatients with hypertension or recent angioplasty35 and a laboratory study of the impact of forgiveness therapy on anger-recall stress-induced changes in myocardial perfusion.56
In contrast to the above interventions, our positive psychology intervention used empirically- validated positive psychology interventions, delivered by phone, in a vulnerable and important population (ACS/CHF patients) with high rates of readmission and mortality. Furthermore, we were careful to create an intervention that could potentially be implemented in clinical settings if found to be efficacious. We also took a more global approach to positive affect and cognitions by targeting several important positive psychology constructs (e.g. gratitude) rather than just happiness or optimism. Given the compelling evidence of the links between positive affect and cardiac outcomes12,16,57 and the ability of positive psychological interventions to improve well-being, this line of work may have substantial clinical and public health relevance.
One additional strength of our approach is that the positive psychology exercises were supervised by a social worker who did not require extensive training. Given that for the most part the intervention consisted of participants independently completing relatively straightforward exercises, the positive psychology trainer was simply required to review the exercises with subjects, discuss material in the treatment manual, and encourage the patient to complete subsequent exercises.
Our small pilot study suggested that the intervention was feasible in this population of patients with recent acute cardiac illness. More than three-quarters of the exercises were completed by subjects in the PP study group, and subjects reported that the exercises were easy to complete, useful, and enhanced optimism. Furthermore, the improvements in mood, anxiety and other outcome measures compared to the other groups were promising.
Limitations
Much remains to be learned about the optimal content, duration, and delivery of this and other positive psychological interventions in cardiac patients. Our positive psychological intervention, which we adapted to the specific population of hospitalized ACS/CHF patients, differs in several ways from previously-tested interventions in non-cardiac populations. Previous positive psychology interventions have typically used a single exercise or content area (compared to our intervention which focused on optimism, kindness, and gratitude), have been substantially briefer than ours (approximately three-quarters have been less than eight weeks32), and have been performed in-person or over the internet. We believe that a broader, longer, and phone-based intervention is more likely to have an impact given that multiple positive states are linked with cardiac outcomes, previously successful interventions in behavioral medicine have included longer treatment durations,58,59 and the telemedicine approach is the most feasible for this set of patients. As this intervention is rigorously tested in future studies, the optimal frequency, duration, and dosing of this treatment design must be considered.
The exploratory feasibility trial also had several limitations, as it was a single-site, very small feasibility trial that was not powered to find significant between-group differences. Moreover, it did not examine other important outcomes such as adherence, physical status, or hospital readmission. It is clear that future studies will need to address these limitations in order to assess the ability of this work to impact outcomes of clinical and public health significance.
Additional refinement and testing of this positive psychology intervention for cardiac patients are required to ensure that the field can develop the best intervention to impact meaningful clinical outcomes. Many questions remain: should positive interventions focus on improving overall well-being or target very specific psychological constructs like optimism, which is associated with superior cardiac health? Should positive psychology interventions serve as a new way to improve negative psychological syndromes like anxiety and depression (which are also associated with adverse cardiac outcomes), or should they be adapted to a broader population of patients than just those with a clinical disorder? Given recent findings that medical outcomes and health behaviors improved among cardiac patients who completed a program that simultaneously focused on psychological and medical factors,60 should positive psychology interventions target health behaviors such as diet or exercise as a way to improve cardiac outcomes? Answers to these questions will have important implications for the adaptation of positive psychology interventions to clinical settings. Although much remains to be learned, this line of work holds much promise in attempts to improve the lives of patients with serious cardiac illness.
Acknowledgments:
this work was supported in part by grant R01-DP00336 from the United States Disease Control and Prevention (CDC) to Dr. Herbert Benson. The authors have no conflicts of interest to report and there were no other funding sources.
References
- 1.Rudisch B, Nemeroff CB. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry. 2003;54:227–40. doi: 10.1016/s0006-3223(03)00587-0. [DOI] [PubMed] [Google Scholar]
- 2.Kaptein KI, de Jonge P, van den Brink RH, et al. Course of depressive symptoms after myocardial infarction and cardiac prognosis: a latent class analysis. Psychosom Med. 2006;68:662–8. doi: 10.1097/01.psy.0000233237.79085.57. [DOI] [PubMed] [Google Scholar]
- 3.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66:802–13. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 4.van Melle JP, de Jonge P, Spijkerman TA, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a metaanalysis. Psychosom Med. 2004;66:814–22. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- 5.Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–37. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 6.Huffman JC, Smith FA, Blais MA, et al. Anxiety, independent of depressive symptoms, is associated with in-hospital cardiac complications after acute myocardial infarction. J Psychosom Res. 2008;65:557–63. doi: 10.1016/j.jpsychores.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Moser DK, Riegel B, McKinley S, et al. Impact of anxiety and perceived control on in-hospital complications after acute myocardial infarction. Psychosom Med. 2007;69:10–6. doi: 10.1097/01.psy.0000245868.43447.d8. [DOI] [PubMed] [Google Scholar]
- 8.Huffman JC, Celano CM, Januzzi JL. The relationship between depression, anxiety, and cardiovascular outcomes in patients with acute coronary syndromes. Neuropsychiatr Dis Treat. 2010;6:123–36. doi: 10.2147/ndt.s6880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glassman AH, O'Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701–9. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 10.Lesperance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367–79. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- 11.Rollman BL, Belnap BH, LeMenager MS, et al. Telephone-delivered collaborative care for treating post-CABG depression: a randomized controlled trial. JAMA. 2009;302:2095–103. doi: 10.1001/jama.2009.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tindle HA, Chang YF, Kuller LH, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women's Health Initiative. Circulation. 2009;120:656–62. doi: 10.1161/CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steptoe A, Dockray S, Wardle J. Positive affect and psychobiological processes relevant to health. J Pers. 2009;77:1747–76. doi: 10.1111/j.1467-6494.2009.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chocron S, Etievent JP, Viel JF, et al. Preoperative quality of life as a predictive factor of 3-year survival after open heart operations. Ann Thorac Surg. 2000;69:722–7. doi: 10.1016/s0003-4975(99)01329-6. [DOI] [PubMed] [Google Scholar]
- 15.Konstam V, Salem D, Pouleur H, et al. Baseline quality of life as a predictor of mortality and hospitalization in 5,025 patients with congestive heart failure. SOLVD Investigations. Studies of Left Ventricular Dysfunction Investigators. Am J Cardiol. 1996;78:890–5. doi: 10.1016/s0002-9149(96)00463-8. [DOI] [PubMed] [Google Scholar]
- 16.Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: a metaanalytic review. Ann Behav Med. 2009;37:239–56. doi: 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70:741–56. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 18.Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: does happiness lead to success? Psychol Bull. 2005;131:803–55. doi: 10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- 19.Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131:925–71. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- 20.Leedham B, Meyerowitz BE, Muirhead J, et al. Positive expectations predict health after heart transplantation. Health Psychol. 1995;14:74–9. doi: 10.1037//0278-6133.14.1.74. [DOI] [PubMed] [Google Scholar]
- 21.Schnohr P, Kristensen TS, Prescott E, et al. Stress and life dissatisfaction are inversely associated with jogging and other types of physical activity in leisure time--The Copenhagen City Heart Study. Scand J Med Sci Sports. 2005;15:107–12. doi: 10.1111/j.1600-0838.2004.00394.x. [DOI] [PubMed] [Google Scholar]
- 22.Steptoe A, Wright C, Kunz-Ebrecht SR, et al. Dispositional optimism and health behaviour in community-dwelling older people: associations with healthy ageing. Br J Health Psychol. 2006;11:71–84. doi: 10.1348/135910705X42850. [DOI] [PubMed] [Google Scholar]
- 23.Kelloniemi H, Ek E, Laitinen J. Optimism, dietary habits, body mass index and smoking among young Finnish adults. Appetite. 2005;45:169–76. doi: 10.1016/j.appet.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Giltay EJ, Geleijnse JM, Zitman FG, et al. Lifestyle and dietary correlates of dispositional optimism in men: The Zutphen Elderly Study. J Psychosom Res. 2007;63:483–90. doi: 10.1016/j.jpsychores.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 25.Browning C, Sims J, Kendig H, et al. Predictors of physical activity behavior in older community-dwelling adults. J Allied Health. 2009;38:8–17. [PubMed] [Google Scholar]
- 26.Oveis C, Cohen AB, Gruber J, et al. Resting respiratory sinus arrhythmia is associated with tonic positive emotionality. Emotion. 2009;9:265–70. doi: 10.1037/a0015383. [DOI] [PubMed] [Google Scholar]
- 27.Roy B, Diez-Roux AV, Seeman T, et al. Association of optimism and pessimism with inflammation and hemostasis in the Multi-Ethnic Study of Atherosclerosis (MESA) Psychosom Med. 2010;72:134–40. doi: 10.1097/PSY.0b013e3181cb981b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prather AA, Marsland AL, Muldoon MF, et al. Positive affective style covaries with stimulated IL-6 and IL-10 production in a middle-aged community sample. Brain Behav Immun. 2007;21:1033–7. doi: 10.1016/j.bbi.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steptoe A, O'Donnell K, Badrick E, et al. Neuroendocrine and inflammatory factors associated with positive affect in healthy men and women: the Whitehall II study. Am J Epidem. 2008;167:96–102. doi: 10.1093/aje/kwm252. [DOI] [PubMed] [Google Scholar]
- 30.Lyubomirsky S, Sheldon KM, Schkade D. Pursuing happiness: the architecture of sustainable change. Rev Gen Psychology. 2005;9:111–31. [Google Scholar]
- 31.Seligman ME, Steen TA, Park N, et al. Positive psychology progress: empirical validation of interventions. Am Psychol. 2005;60:410–21. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- 32.Sin NL, Lyubomirsky S. Enhancing wellbeing and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol. 2009;65:467–87. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- 33.Bradshaw BG, Richardson GE, Kumpfer K, et al. Determining the efficacy of a resiliency training approach in adults with type 2 diabetes. Diabetes Educ. 2007;33:650–9. doi: 10.1177/0145721707303809. [DOI] [PubMed] [Google Scholar]
- 34.Burton NW, Pakenham KI, Brown WJ. Feasibility and effectiveness of psychosocial resilience training: a pilot study of the READY program. Psychol Health Med. 2010;15:266–77. doi: 10.1080/13548501003758710. [DOI] [PubMed] [Google Scholar]
- 35.Charlson ME, Boutin-Foster C, Mancuso CA, et al. Randomized controlled trials of positive affect and self-affirmation to facilitate healthy behaviors in patients with cardiopulmonary diseases: rationale, trial design, and methods. Contemp Clin Trials. 2007;28:748–62. doi: 10.1016/j.cct.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 36.Maddox TM, Reid KJ, Rumsfeld JS, et al. One-year health status outcomes of unstable angina versus myocardial infarction: a prospective, observational cohort study of ACS survivors. BMC Cardiovasc Disord. 2007;7:28–28. doi: 10.1186/1471-2261-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart Disease and Stroke Statistics--2011 Update: A Report From the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huffman JC, Mastromauro CA, Sowden GA, et al. A collaborative care depression management program for cardiac inpatients: depression characteristics and inhospital outcomes. Psychosomatics. 2011;52:26–33. doi: 10.1016/j.psym.2010.11.021. [DOI] [PubMed] [Google Scholar]
- 39.Huffman JC, Smith FA, Blais MA, et al. Preexisting major depression predicts in-hospital cardiac complications after acute myocardial infarction. Psychosomatics. 2008;49:309–16. doi: 10.1176/appi.psy.49.4.309. [DOI] [PubMed] [Google Scholar]
- 40.Emmons RA, McCullough ME. Counting blessings versus burdens: an experimental investigation of gratitude and subjective well-being in daily life. J Pers Soc Psychol. 2003;84:377–89. doi: 10.1037//0022-3514.84.2.377. [DOI] [PubMed] [Google Scholar]
- 41.Otake K, Shimai S, Tanaka-Matsumi J, et al. Happy people become happier through kindness: a counting kindnesses intervention. J Happiness Stud. 2006;7:361–75. doi: 10.1007/s10902-005-3650-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sheldon KM, Lyubomirsky S. How to increase and sustain positive emotion: the effects of expressing gratitude and visualizing best possible selves. J Positive Psychology. 2006;1:73–82. [Google Scholar]
- 43.Tindle H, Davis E, Kuller L. Attitudes and cardiovascular disease. Maturitas. 2010;67:108–13. doi: 10.1016/j.maturitas.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lyubomirsky S, Dickerhoof R, Boehm JK, et al. Becoming happier takes both a will and a proper way: An experimental longitudinal intervention to boost well-being. Emotion. 2011;11:391–402. doi: 10.1037/a0022575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.King LA. The health benefits of writing about life goals. Pers Soc Psychol Bull. 2001;27:10–7. [Google Scholar]
- 46.Brunstein J, Schultheiss O, Grassman R. Personal goals and emotional well-being: the moderating role of motive dispositions. J Pers Soc Psychol. 1998;75:494–508. doi: 10.1037//0022-3514.75.2.494. [DOI] [PubMed] [Google Scholar]
- 47.Lyubomirsky S. The How of Happiness. New York: Penguin Press; 2008. [Google Scholar]
- 48.Cohn MA, Fredrickson BL. In search of durable positive psychology interventions: Predictors and consequences of long-term positive behavior change. Journal of Positive Psychology. 2010;5:355–66. doi: 10.1080/17439760.2010.508883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deckro GR, Ballinger KM, Hoyt M, et al. The evaluation of a mind/body intervention to reduce psychological distress and perceived stress in college students. J Am Coll Health. 2002;50:281–7. doi: 10.1080/07448480209603446. [DOI] [PubMed] [Google Scholar]
- 50.Dusek JA, Hibberd PL, Buczynski B, et al. Stress management versus lifestyle modification on systolic hypertension and medication elimination: a randomized trial. J Altern Complement Med. 2008;14:129–38. doi: 10.1089/acm.2007.0623. [DOI] [PubMed] [Google Scholar]
- 51.Nakao M, Myers P, Fricchione G, et al. Somatization and symptom reduction through a behavioral medicine intervention in a mind/body medicine clinic. Behav Med. 2001;26:169–76. doi: 10.1080/08964280109595764. [DOI] [PubMed] [Google Scholar]
- 52.Roberts RE, Vernon SW. The Center for Epidemiologic Studies Depression Scale: its use in a community sample. Am J Psychiatry. 1983;140:41–6. doi: 10.1176/ajp.140.1.41. [DOI] [PubMed] [Google Scholar]
- 53.Lyubomirsky S, Lepper HS. A measure of subjective happiness: preliminary reliability and construct validation. Social Indicators Research. 1999;46:137–55. [Google Scholar]
- 54.Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 55.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 56.Waltman MA, Russell DC, Coyle CT, et al. The effects of a forgiveness intervention on patients with coronary artery disease. Psychol Health. 2009;24:11–27. doi: 10.1080/08870440903126371. [DOI] [PubMed] [Google Scholar]
- 57.Davidson KW, Mostofsky E, Whang W. Don't worry, be happy: positive affect and reduced 10-year incident coronary heart disease: the Canadian Nova Scotia Health Survey. Eur Heart J. 2010;31:1065–70. doi: 10.1093/eurheartj/ehp603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rohde P, Silva SG, Tonev ST, et al. Achievement and maintenance of sustained response during the Treatment for Adolescents With Depression Study continuation and maintenance therapy. Arch Gen Psychiatry. 2008;65:447–55. doi: 10.1001/archpsyc.65.4.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Roy-Byrne P, Craske MG, Sullivan G, et al. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 2010;303:1921–8. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611–20. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]


