Abstract
Nasopharyngeal branchial cysts (NBCs) have been discussed in the literature in only a limited number of publications. Differing from Tornwaldt cysts, NBCs present laterally and arise from the fossa of Rosenmuller and may track superiorly within the bony confines of the Eustachian tube. Initially patients are asymptomatic but may present with aural fullness, unilateral conductive hearing loss, and serous otitis media as the cyst mass grows. Two of our three patients had the lesion incidentally identified at the time of assessment for another diagnosis. In this case series, imaging characteristics and response to treatment are reviewed. A literature search was performed to summarize the management options for this entity.
Keywords: nasopharyngeal branchial cysts, skull base, Tornwaldt cysts, mucus retention cysts, nasopharyngeal cysts, marsupialization
Introduction
Cystic lesions of the nasopharynx are typically benign. However, care must be taken to distinguish these presentations from neoplasms that may also arise in this region. Cystic masses of the nasopharynx are often found incidentally,1 either by nasal endoscopy or imaging. As these lesions grow they can produce local compressive symptoms of nasal obstruction, aural fullness, conductive hearing loss, or cranial nerve dysfunction.
Cysts arising from the nasopharynx are classified into midline and lateral types.2 These are further grouped into congenital and acquired. Tornwaldt cysts are a congenital midline nasopharyngeal cyst. They originate deep to the pharyngobasilar fascia and are a persistent embryonic communication between the anterior or caudal notochord in the nasopharynx. The most common midline nasopharyngeal cysts are mucus retention cysts, which are an acquired lesion. They are distinguished from Tornwaldt cysts in that they originate superficial to the pharyngobasilar fascia. Intra-adenoid cysts are an additional cause of midline acquired nasopharyngeal cysts. The most common cause of lateral nasopharyngeal cysts are branchiogenic cysts. These are distinguished from mucus retention cysts by arising deep to the pharyngobasilar fascia. Nasopharyngeal branchial cysts (NBCs) are lined with stratified squamous epithelium, pseudostratified squamous epithelium, or both. Lymphoid aggregation may be found in the subepithelial connective tissue.3 Mucus retention cysts also arise in the lateral nasopharynx but are much less common than NBCs. Oncocytic cysts (Warthin's tumor) are a rare cause of acquired lateral nasopharyngeal cysts.4,5
Total excision has previously been described as the standard treatment method for NBCs.6 Total excision of these cysts is often challenging and carries with it the risk of potential vascular injury at the level of the skull base. Marsupialization of these lesions has also been reported to be effective.7 We report three cases of NBCs that were managed effectively with endoscopic marsupialization.
Patients and Methods
We retrospectively reviewed three consecutive patients from 2007 to 2011 with NBCs treated at Tufts Medical Center. The patients underwent preoperative imaging with magnetic resonance imaging (MRI) and subsequent endoscopic transnasal marsupialization. At the time of surgery, tissue specimens from the approach and cyst lining were sent for histopathologic evaluation, and the cavity's contents were evacuated. All patients underwent postsurgical evaluation with endoscopic examination for varying time periods (ranging from 1 to 4 years). No recurrences have been encountered in the series.
Cases
Case 1
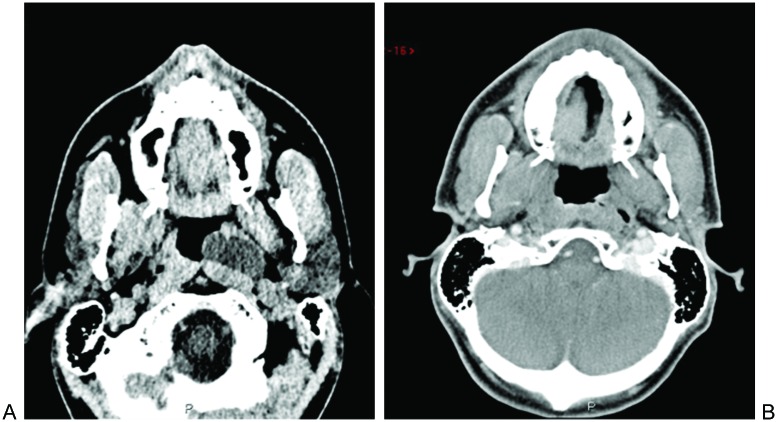
A 25-year-old man presented with a right-sided lateral rectus palsy, and an MRI of the head demonstrated a left-sided cystic mass of the nasopharynx (Fig. 1A). The dumbbell-shaped mass extended from the medial aspect of the Eustachian tube toward the middle cranial fossa. The patient had no nasal or otologic symptoms. On nasal endoscopy a submucosal mass medial to the left torus tubarius was noted. The patient underwent successful endoscopic transnasal marsupialization of the cystic lesion. A postoperative computed tomography (CT) showed resolution of the cystic mass (Fig. 1B). Subsequently, he was diagnosed with multiple sclerosis, explaining his initial presentation of diplopia and lateral rectus palsy. He has had no evidence of recurrence for 2 years following surgery.
Fig. 1.
Hypointense T1 signal on magnetic resonance imaging (MRI; A). Postoperative computed tomography (CT) after marsupialization of nasopharyngeal cyst (B).
Case 2
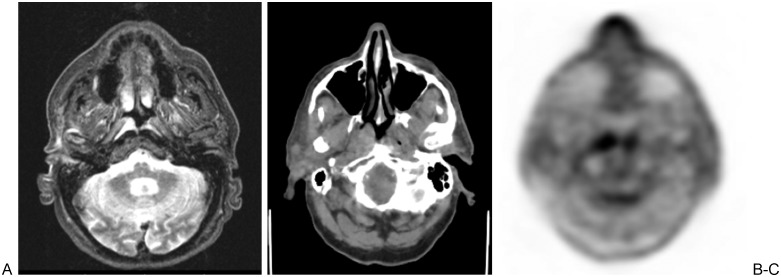
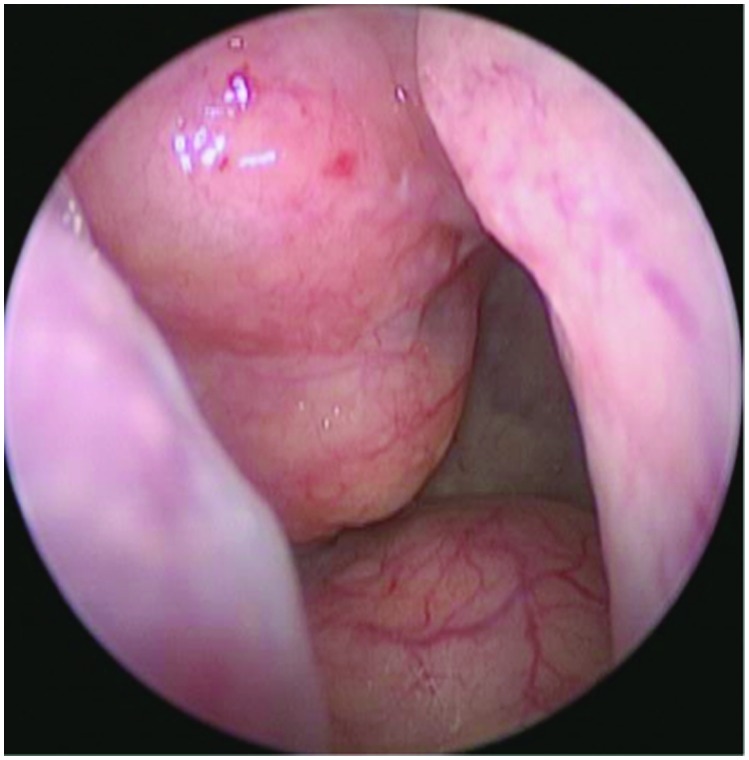
A 78-year-old man with a history of recurrent temporal skin squamous cell carcinoma metastatic to the parotid gland, status postsurgery and adjuvant radiation therapy, was found on MRI to have asymmetric mass lesion in the right nasopharynx (Fig. 2A). It showed increased T2 and fluid-attenuated inversion-recovery (FLAIR) signal intensity. Positron emission tomography–computed tomography (PET-CT) imaging demonstrated increased uptake within the cystic mass that was initially interpreted as a potential skull base metastasis from the prior skin cancer (Figs. 2B and 2C). On nasal endoscopy, a submucosal mass in the right fossa of Rosenmuller was present (Fig. 3). The patient had symptoms of an ipsilateral conductive hearing loss and aural fullness. He underwent an endoscopic transnasal marsupialization of the cystic lesion and 1 year after surgery has had no evidence of recurrence.
Fig. 2.
T2 hyperintense signal in right lateral nasopharynx on magnetic resonance imaging (MRI; A). Asymmetry of nasopharynx on computed tomography (CT; B). Increased uptake in right lateral nasopharynx on positron emission tomography (PET; C).
Fig. 3.
Right nasopharyngeal submucosal mass obstructing the view of the Eustachian tube.
Case 3
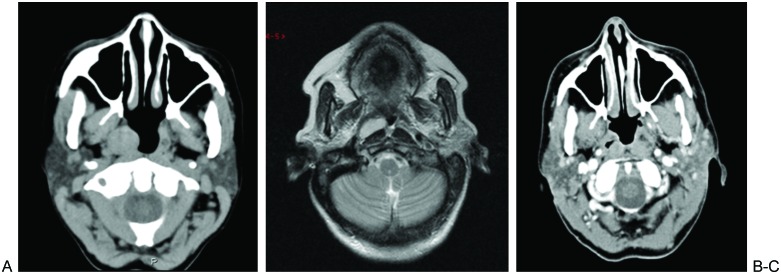
A 50-year-old woman presented with right-sided otalgia and bilateral aural fullness. On sinus CT, a 1.5 × 1.7 cm soft tissue mass in the right fossa of Rosenmuller was noted (Fig. 4A). A submucosal nasopharyngeal mass was seen on subsequent nasal endoscopy. Additional imaging with MRI showed a well circumscribed T1 and T2 hyperintense cystic lesion (Fig. 4B). The patient underwent transnasal endoscopic drainage and marsupialization of the mass and has had no evidence of recurrence for 4 years following surgery. A postoperative CT confirmed decompression of the cystic mass (Fig. 4C).
Fig. 4.
Computed tomography (CT) showing soft tissue mass in right fossa of Rosenmuller (A). Hyperintense on T2 magnetic resonance imaging (MRI; B). Postoperative CT after marsupialization (C).
Discussion
MRI with contrast is superior to CT in the radiologic evaluation of NBCs. Although CT shows excellent relation of the lesions to bony structures, MRI has the capacity to better demonstrate the precise relationship of the lesion to the great vessels. Additionally, signal characteristics on MRI help distinguish lesions of the nasopharynx. NBCs are usually slightly hypointense on T1-weighted MRI and hyperintense on T2-weighted MRI. CT typically shows a low density mass.5
The standard accepted treatment of NBCs is surgery. Multiple surgical approaches to NBCs have been described. Complete extirpation of the cyst either by transcervical, transpalatal, or transmandibular approaches have been considered the mainstays of management.8 Each approach has its own relative advantages and disadvantages in terms of exposure and associated morbidity. Aspiration of cysts has also been described; however, this was likely to result in recurrence. More recently, transoral marsupialization has been described as an effective method of managing NBCs. In the case series of three patients, with a follow-up ranging from 8 to 40 months, no recurrences were reported. When compared with complete excision, the authors considered this technique to offer benefits of being less invasive, requiring decreased OR time, offering less functional loss and cosmetic deformity to the patients, and being associated with a shorter hospitalization.7
The three cases of NBC at our institution were surgically managed via an endoscopic transnasal marsupialization. There was no recurrence of disease in a follow-up period that ranged from 1 to 4 years. The surgery was performed as an outpatient procedure and was associated with no significant complications.
Conclusion
NBCs are lateral cystic lesions of the nasopharynx that are found deep to the pharyngobasilar fascia. An understanding of the differential diagnosis of cystic lesions of the nasopharynx is important in excluding these lesions from other processes. Our series, in addition to established literature, suggests that these lesions can be effectively managed with biopsy and marsupialization.
References
- 1.Ali M Y. Pathogenesis of cysts and crypts in the nasopharynx. J Laryngol Otol. 1965;79:391–402. doi: 10.1017/s0022215100063854. [DOI] [PubMed] [Google Scholar]
- 2.Nicolai P, Luzzago F, Maroldi R, Falchetti M, Antonelli A R. Nasopharyngeal cysts. Report of seven cases with review of the literature. Arch Otolaryngol Head Neck Surg. 1989;115:860–864. doi: 10.1001/archotol.1989.01860310098032. [DOI] [PubMed] [Google Scholar]
- 3.Little J W, Rickles N H. The histogenesis of the branchial cyst. Am J Pathol. 1967;50:533–547. [PMC free article] [PubMed] [Google Scholar]
- 4.Guggenheim P. Cysts of the nasopharynx. Laryngoscope. 1967;77:2147–2168. doi: 10.1288/00005537-196712000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Ben Salem D, Duvillard C, Assous D, Ballester M, Krausé D, Ricolfi F. Imaging of nasopharyngeal cysts and bursae. Eur Radiol. 2006;16:2249–2258. doi: 10.1007/s00330-006-0238-x. [DOI] [PubMed] [Google Scholar]
- 6.Verma A Sohail M A al-Khabori M Moosa M Nasopharyngeal cyst of branchiogenic origin: report of a case and review of the literature Ear Nose Throat J 200079722–724., 726, 730–731 [PubMed] [Google Scholar]
- 7.Tsai T Y, Su C Y. Surgical technique of transoral marsupialization for the treatment of nasopharyngeal branchial cysts. Ann Otol Rhinol Laryngol. 2010;119:336–341. doi: 10.1177/000348941011900511. [DOI] [PubMed] [Google Scholar]
- 8.Carrau R L, Myers E N, Johnson J T. Management of tumors arising in the parapharyngeal space. Laryngoscope. 1990;100:583–589. doi: 10.1288/00005537-199006000-00006. [DOI] [PubMed] [Google Scholar]