Abstract
Purpose The sphenoid sinus is a complex structure with key variations that are important for endoscopic parasellar approaches. In this study, high-resolution computed tomography (HRCT) scans were analyzed for the frequency of these variations.
Methods A retrospective radiographic analysis was conducted on patients undergoing HRCT between July 2008 and September 2010.
Results Sphenoid sinus pneumatization was defined as conchal, presellar, sellar, and postsellar based on pneumatization relative to the anterior and posterior face of the sella. The distribution ranged from 1.8%, 7.3%, 47.6%, and 43.3%, respectively. We found a greater preponderance of sellar and postsellar variation than previously reported. No differences were found in regard to age, gender, and ethnicity (African American, Caucasian, Asian, and Hispanic) (p > 0.05). The prevalence of optic nerve, maxillary nerve, and internal carotid artery protrusion was 26.1%, 25.9%, and 28.2%, respectively, and dehiscence was 2.1%, 7.4%, and 2.9%, respectively. Accessory septae were present in 43.5% of cases. A lateral recess was identified in 72.4% and clinoid pneumatization in 20% of patients.
Conclusion This study demonstrates a greater prevalence of sphenoid sinus pneumatization and variations than previously reported. This has important implications in terms of preparation and anticipation of possible variations to avoid complications.
Keywords: congdon classification, sphenoid sinus pneumatization, parasellar anatomy, endoscopic sinus surgery, sphenoid sinus, computed tomography, endoscopic skull base surgery, optic nerve, internal carotid artery, transsphenoidal surgery
Introduction
The sphenoid sinus is a highly variable anatomic structure. Individual differences can be attributed to the extent of sphenoid sinus pneumatization, varying number and position of septa, and the relationship with surrounding structures. Congdon was among the first to meticulously study the sphenoid sinus and classified it into three types based on the degree of pneumatization relative to the sella turcica: conchal, presellar, and sellar.1 These extremes of pneumatization are important to understand, as they present their own challenges to surgeons performing endoscopic endonasal transsphenoidal approach (EETSA) to the skull base and parasellar region.2,3,4,5 Awareness of the exact configuration of a particular individual's sphenoid sinuses before surgery is vital to avoid complications.
There have been several studies analyzing the sphenoid sinus anatomy through both cadaveric dissection and computed tomography (CT) analysis. The results have been varied and data have ranged from 2 to 28% conchal, 17 to 21% presellar, 54 to 85% sellar, and 22% postsellar.6,7,8,9,10,11,12 The great variation is in part due to the lack of a standardized definition of these classes, partly due to the approach to analyzing the specimens, and—in some studies—the smaller power.
Through anecdotal evidence during endoscopic sinus and skull base surgery, the senior author (JAE) has encountered a greater number of well-pneumatized specimens. In this study, we aim to define the prevalence of these various degrees of pneumatization, explore the different anatomical variations of the sphenoid sinuses, and describe their incidence according to gender and ethnicity.
Materials and Methods
Experimental Design
The protocol for this study was reviewed and approved by the Institutional Review Board of the University of Medicine and Dentistry of New Jersey – New Jersey Medical School in Newark, New Jersey. High-resolution computed tomography (HRCT) maxillofacial and paranasal sinus scans of 170 patients (a subset of a previously described cohort13) who underwent diagnostic imaging for rhinosinusitis or facial trauma were reviewed by two independent observers (an otolaryngologist and a radiologist). Patients who had trauma or prior surgery of the ethmoid or sphenoid sinuses, or tumor causing distortion of the anatomy, were excluded from this study. All scans were performed using Centricity Enterprise™ Picture Archiving and Communication Systems (PACS, General Electric Healthcare, Piscataway, New Jersey, USA) at the University Hospital in Newark, New Jersey between July 2008 and September 2010. HRCT scans were analyzed for the degree of sphenoid sinus pneumatization and the listed anatomic variations by each observer for a total of 2,204 data points. Sphenoid sinus pneumatization was defined relative to the vertical plane of the anteriormost and posteriormost extent of the sella (Fig. 1). Further anatomic variations were identified and graded as described below.
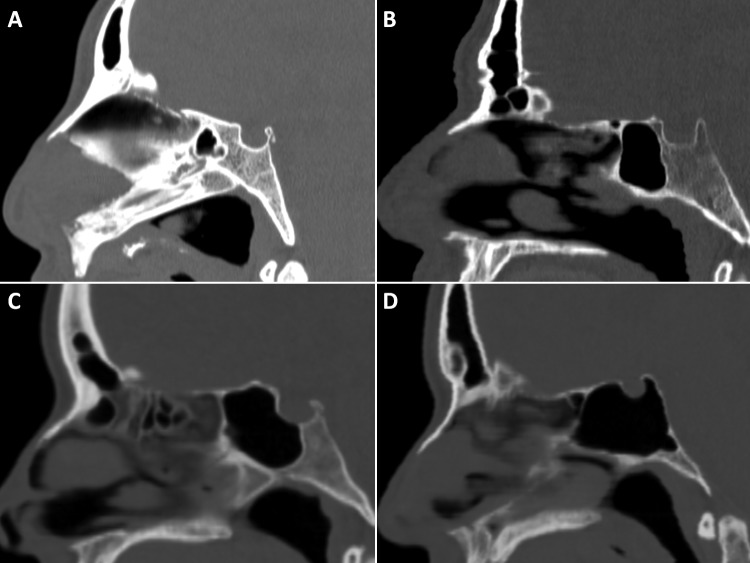
Fig. 1.
Sagittal high-resolution computed tomography scans of the different type of sphenoid pneumatizations: (A) conchal, (B) presellar, (C) sellar, and (D) postsellar.
Septation
This referred to accessory septum, not the single intersinus septum, and could best be identified on axial and coronal views.
Lateral Sphenoid Recess
This was defined as the lateral pneumatization of the sphenoid sinus into the greater wing of the sphenoid and pterygoid processes. This was best viewed on the axial and coronal images (Fig. 2).
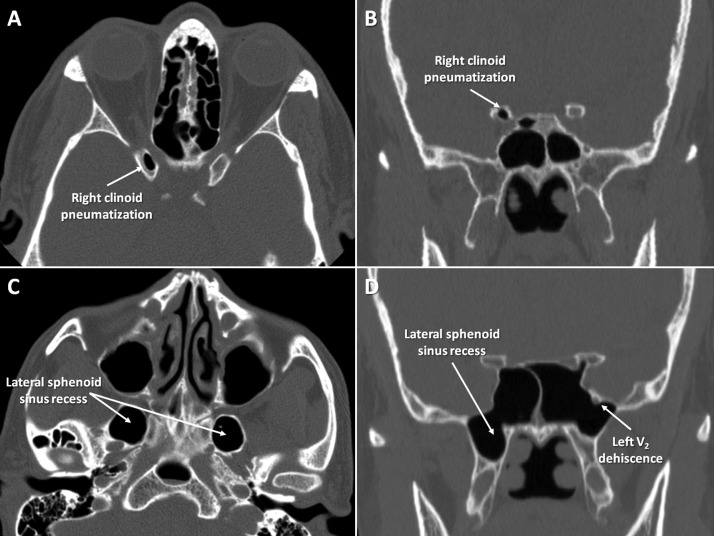
Fig. 2.
(A) Axial and (B) coronal high-resolution computed tomography (HRCT) scans depicting a pneumatized right clinoid process. (C) Axial and (D) coronal HRCT scans demonstrating the lateral sphenoid sinus recess and a left V2 dehiscence.
Clinoid Process Pneumatization
The pneumatization of the anterior or posterior clinoid processes was noted. This was best seen on axial, coronal, or sagittal views (Fig. 2).
Internal Carotid Artery, Optic Nerve, and Maxillary Division of the Trigeminal Nerve (V2) Protrusion
This was defined as 50% or more of the noted structure projecting into the pneumatized space of the sphenoid sinus but with an intact bony covering. This was better evaluated on axial imaging for the internal carotid artery and coronal imaging for the optic nerve and V2 (Figs. 2 and 3).
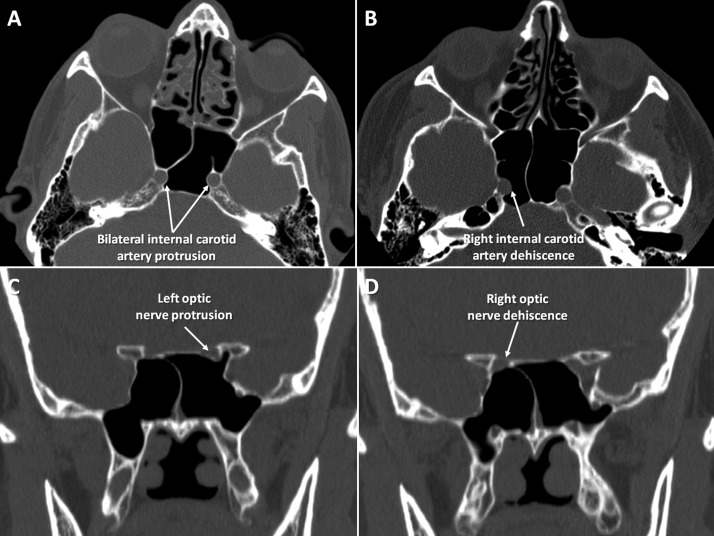
Fig. 3.
Axial high-resolution computed tomography (HRCT) scans demonstrating (A) bilateral internal carotid artery protrusion and (B) a right internal carotid artery dehiscence. Coronal HRCT scans demonstrating (C) a left optic nerve protrusion and (D) a right optic nerve dehiscence.
Internal Carotid Artery, Optic Nerve, and V2 Dehiscence
This was noted if there was a lack of bony margin around these structures (Fig. 3).
Study Population
A total of 170 patients who met the study inclusion criteria are included in this analysis. The mean patient age was 44.7 (range, 19 to 81 years). The study group consisted of 96 (56.5%) women and 74 (43.5%) men. Based on the documented demographics, there were 65 (38.2%) African American, 55 (32.4%) Hispanic, 26 (15.3%) Caucasian, 6 (3.5%) Asian patients, and 18 (10.6%) were racially undefined. No significant age difference was found amongst the different ethnic groups (p > 0.05). There was no difference in age between men and women (p > 0.05).
Statistical Methods
Statistical analysis was performed using Fisher's exact test for categorical variables and ANOVA for continuous variables. Two-tailed tests were performed for each scenario and significance level was set at p < 0.05. All analyses were performed using Microsoft Office Excel 2007 (Microsoft Corp., Redmond, Washington, USA).
Results
The data were analyzed by two independent observers, averaged, and compared with respect to variations in the anatomical configuration of the surrounding structures, including the protrusion or dehiscence of the internal carotid artery, optic nerve, and V2 (Table 1); the presence of clinoid pneumatization, accessory septae, and lateral recesses (Table 2); and Congdon pneumatization (Table 3). The data were also stratified according to ethnicity (Table 4) and gender (Table 5). The percent agreement between the two observers was 94.4% with a Cohen's kappa coefficient of 0.89.
Table 1. Averaged Data from Two Observers of the Rates of Protrusion and Dehiscence of the Internal Carotid Artery, Optic Nerve and V2 into the Sphenoid Sinus.
| No protrusion | 50% protrusion | Dehiscence | ||||
|---|---|---|---|---|---|---|
| Number | Percent (%) | Number | Percent (%) | Number | Percent (%) | |
| Internal carotid a. | 234 | 68.8 | 96 | 28.2 | 10 | 2.9 |
| African American | 92 | 70.8 | 32 | 24.6 | 6 | 4.6 |
| Hispanic | 79 | 71.2 | 29 | 26.1 | 3 | 2.7 |
| Caucasian | 27 | 50.9 | 26 | 49.1 | 0 | 0 |
| Asian | 5 | 41.7 | 6 | 50 | 1 | 8.3 |
| Male | 87 | 58 | 58 | 38.7 | 5 | 3.3 |
| Female | 146 | 75.3 | 42 | 21.7 | 6 | 3.1 |
| Optic nerve | 245 | 71.9 | 89 | 26.1 | 7 | 2.1 |
| African American | 96 | 73.9 | 32 | 24.6 | 2 | 1.5 |
| Hispanic | 87 | 78.4 | 22 | 19.8 | 2 | 1.8 |
| Caucasian | 28 | 51.9 | 22 | 40.7 | 4 | 7.4 |
| Asian | 4 | 30.8 | 8 | 61.5 | 1 | 7.7 |
| Male | 104 | 69.3 | 40 | 26.7 | 6 | 4 |
| Female | 140 | 72.5 | 50 | 25.9 | 3 | 1.6 |
| V2 nerve | 227 | 66.8 | 88 | 25.9 | 25 | 7.4 |
| African American | 79 | 60.3 | 38 | 29 | 14 | 10.7 |
| Hispanic | 72 | 65.5 | 31 | 28.2 | 7 | 6.4 |
| Caucasian | 35 | 66 | 15 | 28.3 | 3 | 5.7 |
| Asian | 10 | 83.3 | 1 | 8.3 | 1 | 8.3 |
| Male | 94 | 63.1 | 42 | 28.2 | 13 | 8.7 |
| Female | 133 | 68.9 | 47 | 24.4 | 13 | 6.7 |
Table 2. Averaged Data from Two Observers of the Rates of Clinoid Pneumatization, Accessory Septation, and Lateral Recess of the Sphenoid Sinus.
| Number | Percent (%) | |
|---|---|---|
| Clinoid pneumatization | 34 | 20 |
| African American | 11 | 16.9 |
| Hispanic | 9 | 16.4 |
| Caucasian | 7 | 26.9 |
| Asian | 4 | 66.7 |
| Male | 20 | 27 |
| Female | 15 | 15.6 |
| Accessory septation | 74 | 43.5 |
| African American | 32 | 49.2 |
| Hispanic | 20 | 36.4 |
| Caucasian | 13 | 50 |
| Asian | 3 | 50 |
| Male | 34 | 46 |
| Female | 39 | 40.6 |
| Lateral recess pneumatization | 123 | 72.4 |
| African American | 55 | 84.6 |
| Hispanic | 32 | 58.2 |
| Caucasian | 21 | 80.8 |
| Asian | 4 | 66.7 |
| Male | 54 | 73 |
| Female | 70 | 72.9 |
Table 3. Averaged Data from Two Observers of Sphenoid Sinus Pneumatization.
| Conchal | Presellar | Sellar | Postsellar | |||||
|---|---|---|---|---|---|---|---|---|
| Number | Percentage (%) | Number | Percentage (%) | Number | Percentage (%) | Number | Percentage (%) | |
| Overall | 3 | 1.8 | 12 | 7.3 | 78 | 47.6 | 71 | 43.3 |
| African American | 1 | 1.5 | 4 | 6.2 | 35 | 53.9 | 25 | 38.5 |
| Hispanic | 2 | 3.7 | 6 | 11.1 | 21 | 38.9 | 26 | 48.2 |
| Caucasian | 0 | 0 | 1 | 4 | 10 | 40 | 14 | 56 |
| Asian | 0 | 0 | 0 | 0 | 3 | 50 | 3 | 50 |
| Male | 1 | 1.4 | 6 | 8.1 | 34 | 36.2 | 34 | 36.2 |
| Female | 2 | 2.1 | 7 | 7.5 | 46 | 48.9 | 41 | 43.6 |
Table 4. Subgroup Analysis by Ethnic Group.
| P values | ||||
|---|---|---|---|---|
| Race | Asian | Hispanic | Caucasian | |
| Conchal | African American | 1.0 | 0.6 | 1.0 |
| Asian | – | 1.0 | 1.0 | |
| Hispanic | – | – | 1.0 | |
| Presellar | African American | 1.0 | 0.5 | 1.0 |
| Asian | – | 1.0 | 1.0 | |
| Hispanic | – | – | 0.4 | |
| Sellar | African American | 1.0 | 0.1 | 0.3 |
| Asian | – | 0.7 | 0.7 | |
| Hispanic | – | – | 1.0 | |
| Postsellar | African American | 0.7 | 0.4 | 0.2 |
| Asian | – | 1.0 | 1.0 | |
| Hispanic | – | – | 0.6 | |
| Internal carotid artery protrusion | African American | 0.08 | 0.9 | a 0.002 |
| Asian | – | 0.1 | 1.0 | |
| Hispanic | – | – | a 0.005 | |
| Internal carotid artery dehiscence | African American | 0.5 | 0.5 | 0.2 |
| Asian | – | 0.3 | 0.2 | |
| Hispanic | – | – | 0.6 | |
| Optic nerve protrusion | African American | a 0.002 | 0.4 | a 0.03 |
| Asian | – | *0.003 | 0.22 | |
| Hispanic | – | – | a 0.008 | |
| Optic nerve dehiscence | African American | 0.3 | 1.0 | ‡0.06 |
| Asian | – | 0.3 | 1.0 | |
| Hispanic | – | – | 0.1 | |
| V2 protrusion | African American | 0.2 | 1.0 | 1.0 |
| Asian | – | 0.2 | 0.3 | |
| Hispanic | – | – | 1.0 | |
| V2 dehiscence | African American | 1.0 | 0.3 | 0.7 |
| Asian | – | 0.6 | 0.6 | |
| Hispanic | – | – | 1.0 | |
| Clinoid pneumatization | African American | *0.02 | 1.0 | 0.4 |
| Asian | – | a 0.02 | 0.1 | |
| Hispanic | – | – | 0.5 | |
| Accessory septae | African American | 1.0 | 0.2 | 1.0 |
| Asian | – | 0.7 | 1.0 | |
| Hispanic | – | – | 0.3 | |
| Lateral recess | African American | 0.3 | a 0.002 | 0.8 |
| Asian | – | 1.0 | 0.6 | |
| Hispanic | – | – | 0.5 | |
Indicates significance at the 0.05 level,
indicates near significance.
Table 5. Subgroup Analysis by Gender.
| P value | |
|---|---|
| Conchal | 1.0 |
| Presellar | 1.0 |
| Sellar | 0.8 |
| Postsellar | 0.8 |
| Internal carotid artery protrusion | 0.0008a |
| Internal carotid artery dehiscence | 1.0 |
| Optic nerve protrusion | 0.9 |
| Optic nerve dehiscence | 0.2 |
| Maxillary nerve protrusion | 0.5 |
| Maxillary nerve dehiscence | 0.5 |
| Clinoid pneumatization | 0.1 |
| Accessory septae | 0.5 |
| Lateral recess | 1.0 |
Indicates significance at the 0.05 level.
Internal Carotid Artery, Optic Nerve, and V2
Internal carotid artery protrusion overall was 28.2% and dehiscence was 2.9%. The rate of dehiscence was 4.6% in African Americans, 2.7% in Hispanics, 8.3% in Asians, and 0% in Caucasians. There was no statistically significant difference between the groups with respect to internal carotid artery dehiscence (p > 0.05) (Tables 4 and 5). There was a higher instance of internal carotid artery protrusion in men, which was statistically significant (p = 0.008) (Table 1 and 5). The rate of protrusion was 24.6% in African Americans, 26.1% in Hispanics, 50.0% in Asians, and 49.1% in Caucasians. The difference in internal carotid artery protrusion was statistically significantly higher in Caucasians compared with African Americans (p = 0.002) and Hispanics (p = 0.005) (Tables 1 and 4).
Optic nerve dehiscence overall was 2.1%, with the greatest prevalence among Asians at 7.7%, followed by Caucasians at 7.4%, then Hispanics at 1.8%, and African Americans at 1.5%. There was no statistical difference in optic nerve dehiscence in regard to ethnicity (p > 0.05) (Tables 1 and 4). In addition, Asians and Caucasians also had the greatest instance of optic nerve protrusion at 61.4% and 40.7%, respectively, whereas the rates in Hispanics and African Americans were 19.8% and 24.6%, respectively. The difference in optic nerve protrusion was statistically higher in Caucasians as compared with African Americans (p = 0.03) and Hispanics (p = 0.008). Similarly, optic nerve protrusion rates were significantly higher in Asians than in African Americans (p = 0.002) and Hispanics (p = 0.003) (Tables 1 and 4). Optic nerve dehiscence amongst men was twice the rate found in women (4% and 1.6%, respectively) (Table 1). However, optic nerve dehiscence and protrusion displayed no statistically significant difference in gender types (p > 0.05) (Table 5).
Analysis of V2 showed an overall dehiscence rate of 7.4%. This was greatest in African Americans at 10.7%, followed by Asians at 8.3%, Hispanics at 6.4%, and Caucasians at 2.7%. The rate of protrusion was 29% in African Americans, 28.2% in Hispanics, 28.3% in Caucasians, and 8.3% in Asians. There was a slight male predominance, with a rate of 8.7% in men compared with 6.7% in women. However, there was no statistically significant difference in gender or ethnicity (p > 0.05) (Tables 4 and 5).
Clinoid Process, Accessory Septae, and Lateral Recess
Clinoid process pneumatization occurred in 20% of the population, most commonly among Asians at 66.7%. Clinoid process pneumatization occurred in 26.9% of Caucasians, 16.9% of African Americans, and 16.4% of Hispanics. There was a statistically higher prevalence amongst Asians when compared with African Americans (p = 0.02), and Hispanics (p = 0.02) (Table 4). Clinoid process pneumatization was more prevalent in men than women, 27% versus 15.6% without reaching statistical significance (p > 0.05) (Table 5).
Accessory sphenoid sinus septation was noted in 43.5% of the population, with an equal prevalence among Asians and Caucasians at 50%. The rates in Hispanics and African Americans were 36.4% and 49.2%, respectively. This data showed no statistical difference between the different ethnic groups and men and women (p > 0.05) (Table 4 and 5).
Lateral sphenoid recess was found in 72.4% of the population, with a higher percentage among African Americans and Caucasians (84.6% and 80.8%, respectively). The prevalence in Hispanics and Asians was 58.2% and 66.7%, respectively. There was a higher prevalence of lateral sphenoid recess in African Americans when compared with Hispanics (p = 0.002) (Table 4). There was no difference in prevalence rates between men and women and the other ethnic groups (Table 4 and 5).
Sphenoid Sinus Pneumatization
The overall prevalence of sphenoid sinus pneumatization was 1.8% conchal, 7.3% presellar, 47.6% sellar, and 43.3% postsellar. In subgroup analysis by gender and ethnicity (African American, Hispanic, Caucasian, Asian), we noted that among African Americans the sellar type was most common at 53.8%; in Hispanics and Caucasians the postsellar type was most common at 48.2% and 56%, respectively; and in Asians the sellar and postsellar configurations were the only types at 50% each. Conchal and presellar types were most common among Hispanics at 3.7% and 6%, respectively. Men had an equal number of sellar and postsellar types at 36.2% each, and women had a sellar predominance at 48.9% (Table 3). However, there were no statistical differences in gender and ethnicity between groups (p > 0.05) (Table 4).
The data were further analyzed to determine any age influence in the pattern of pneumatization. Nonetheless, there was no significant difference found in ages between the different sphenoid pneumatization configuration (p > 0.05).
Discussion
The anatomy of the sphenoid sinus can be quite complex. The great amount of anatomic variation is attributed to the extent of sphenoid sinus pneumatization, varying number and position of septae, and the relationship with surrounding structures. The sphenoid sinus can be seen on computed tomography (CT) scan as early as 2 years of age and is usually fully developed by the age of 14.8 The direction of pneumatization is normally inferoposterolateral. However, the actual degree of pneumatization varies greatly in each individual.8 Congdon originally classified the sphenoid sinus into three types based on the level of pneumatization.1 The conchal type is described as pneumatization in which the posterior wall of the sinus lies anterior to the sella turcica (Fig. 1A). In the presellar type, the posterior limit of the sinus extends into the anterior portion of the sella (Fig. 1B). The sellar type has pneumatization past the anterior border of the sella such that the sella bulges into the sinus (Fig. 1C). Other classifications of sphenoid pneumatization exist; consequently, a uniform standard is not currently in use.14 In this study we included the postsellar type to identify those sinuses with pneumatization completely surrounding the sella (Fig. 1D).
It is important to evaluate the extent of pneumatization prior to undertaking surgical approaches to the parasellar region. Each type of sphenoid pneumatization configuration presents the surgeon attempting an EETSA with a different situation that can hinder or facilitate access to the sellar and parasellar region. Most patients with a sellar or parasellar lesion such as a pituitary adenoma or craniopharyngioma undergoing planned resection have a HRCT and/or magnetic resonance imaging (MRI) scans. Surgeons must meticulously study the preoperative imaging to become familiar with the nuances and variations unique to each case and proceed accordingly to decrease the risk of complications.
The EETSA to the sella turcica and adjacent structures has garnered increasing popularity because of its lower morbidity and mortality as compared with the transcranial approach.15,16,17 This approach provides the least traumatic route, avoids brain retraction, and allows for excellent visualization for resection of lesions.8 Associated complication rate of the EETSA is low but not negligible and can be life threatening. The potential complications of this technique include epistaxis, hyposmia, anosmia, sinusitis, headache, dizziness, cerebrospinal fluid leakage, subarachnoid hemorrhage, intracavernous carotid artery aneurysm, and blindness.18
Anatomic studies have been conducted to better understand the variability of the structures encountered during EETSA to minimize complications.8,9 The sphenoid ostia vary in shape, location, and distance to the midline.9,19,20,21 The sphenoid sinus also differs in degree of pneumatization, number and position of septa, and relation to adjacent structures. This current study aims to further characterize the prevalence of the different types of sphenoid sinus pneumatization and other anatomic variations, as they relate to age, gender, and ethnicity.
The conchal type of sphenoid sinus is thought to exist mostly in children because sphenoid sinus pneumatization begins at 6 months to 4 years of age and usually is completed by 18 years of age. It is usually found to be the least common of the three configurations initially described by Congdon, often around 2% in most studies dealing with adult radiologic studies or specimens.6,8,22,23 However, Tan and Ong's study of adult Asian cadavers exhibited a much higher proportion of conchal types of sphenoid sinuses pneumatization, with 28% of their specimens showing this variation.7 Our study found an overall prevalence of 1.8%, which is more in accordance with previously reported data. There were no statistically significant differences for ethnicity or gender for the conchal pneumatization type (p > 0.05). The conchal type of sphenoid sinus pneumatization increases the difficulty of the EETSA because of the amount of bone present between the sphenoid face and the sellar/parasellar region.7 This type of sphenoid configuration precluded the use of the EETSA in the past.8 However, with the improvements in surgical instrumentation, optical devices, and more accurate navigation systems, this sphenoid configuration is no longer a contraindication for EETSA.
The presellar type of pneumatization is usually intermediate in frequency in studies conducted thus far. We found an overall percentage of presellar sphenoid pneumatization in 7.3% of our patients. There were no statistically significant differences for ethnicity or gender for the presellar pneumatization type (p > 0.05). This configuration presents less of a challenge than the conchal type during EETSA because there is less bone between the anterior wall of the sella and the sphenoid sinus. However, there is a lack of sellar bulge since the sinus only extends up to a plane perpendicular to the anterior face of the sella turcica. A sellar bulge, when present, serves as an important landmark and facilitates surgery.8
The sellar configuration has been the most prevalent of the pneumatization types in previous studies.1,6,7,8,9,24 Our study showed similar results and further subdivided this configuration into sellar and postsellar types. Overall, this was the most prevalent configuration in all groups, without statistically significant differences between ethnicities and genders (p > 0.05). The sellar and postsellar configurations are most amenable to EETSA. However, if the degree of pneumatization is too extensive and a state of hyperpneumatization exists, the anatomy can be distorted with protrusion or dehiscence of the optic nerves and internal carotid arteries. Hence, the lateral walls of the sphenoid sinus are often less than 0.5 mm in thickness.22 Protrusions and dehiscence of the walls of the optic nerve, internal carotid artery, V2, and the vidian nerve are not uncommon.24 A hyperpneumatized sphenoid sinus increases the risk of inadvertent perforation and damage to those adjacent structures.8 The increased pneumatization can also cause the floor of the middle cranial fossa to be mistaken for the sella and lead to unwarranted intracranial entry.8 Additionally, penetration of the posterior wall of the sphenoid sinus and clivus and subsequent cerebrospinal fluid leakage can take place when one is not cognizant of extensive pneumatization involving the dorsum sellae and clival recess.8
Anatomic variations in sphenoid pneumatization between Asians and Caucasians have previously been reported.25 This study was unique in that it analyzed the anatomic variations in various ethnic groups and amongst genders. Interestingly, it showed an overall higher prevalence of many anatomic variations including pneumatization, as determined by Congdon; the presence of lateral sphenoid recesses; and clinoid pneumatization among Asians than previously reported. The remainder of the groups varied, though not to the same degree. Importantly, we found a statistically higher prevalence of internal carotid artery protrusion in Caucasians compared with Africans Americans and Hispanics, as well as statistically higher prevalence of optic nerve protrusion in Caucasians and Asians when compared with African Americans and Hispanics. These findings may have interesting implications when considering the ease of EETSA and complication rates among different ethnic groups.
The limitations of this study include the smaller representation of some of the ethnic groups (i.e., Asians). In addition, there are no confirmatory endoscopic correlations with the HRCT scans. However, Shin et al compared the presence of Onodi cells on CT and then endoscopically and found a good correlation between the two modalities.26 Clearly this is an area that needs further research, but certainly the usefulness of CT scans in determining anatomical variations and in preoperative planning is apparent.
Conclusion
Knowledge of the distinctive anatomy of an individual patient's sphenoid sinus is essential in planning EETSA. HRCT scans allow for adequate identification of the different sphenoid sinus configurations. Although previous studies have helped define the anatomic complexities of the sphenoid sinus, our study advances the knowledge of this region by further defining the relationship between pneumatization and age, gender, and ethnicity. Enrichment of the knowledge of the sphenoid sinus anatomic variation will aid in reducing complications associated with EETSA. Adequate knowledge and preoperative planning must be accompanied by sufficient experience to effectively reduce complications.
Financial Disclosures None Conflicts of Interest None
Note
Presented at the 22nd North American Skull Base Society Meeting, Las Vegas, Nevada, February 17–19, 2012.
References
- 1.Congdon E D. The distribution and mode of origin of septa and walls of the sphenoid sinus. Anat Rec. 1920;18:97–123. [Google Scholar]
- 2.Liu J K, Christiano L D, Patel S K, Eloy J A. Surgical nuances for removal of retrochiasmatic craniopharyngioma via the endoscopic endonasal extended transsphenoidal transplanum transtuberculum approach. Neurosurg Focus. 2011;30:E14. doi: 10.3171/2011.1.FOCUS10297. [DOI] [PubMed] [Google Scholar]
- 3.Liu J K, Christiano L D, Patel S K, Tubbs R S, Eloy J A. Surgical nuances for removal of tuberculum sellae meningiomas with optic canal involvement using the endoscopic endonasal extended transsphenoidal transplanum transtuberculum approach. Neurosurg Focus. 2011;30:E2. doi: 10.3171/2011.3.FOCUS115. [DOI] [PubMed] [Google Scholar]
- 4.Liu J K Eloy J A Endoscopic endonasal transplanum transtuberculum approach for resection of retrochiasmatic craniopharyngioma J Neurosurg 201232(Suppl):E2. [PubMed] [Google Scholar]
- 5.Schmidt R F, Choudhry O J, Raviv J. et al. Surgical nuances for the endoscopic endonasal transpterygoid approach to lateral sphenoid sinus encephaloceles. Neurosurg Focus. 2012;32:E5. doi: 10.3171/2012.3.FOCUS1267. [DOI] [PubMed] [Google Scholar]
- 6.Banna M, Olutola P S. Patterns of pneumatization and septation of the sphenoidal sinus. J Can Assoc Radiol. 1983;34:291–293. [PubMed] [Google Scholar]
- 7.Tan H K, Ong Y K. Sphenoid sinus: an anatomic and endoscopic study in Asian cadavers. Clin Anat. 2007;20:745–750. doi: 10.1002/ca.20507. [DOI] [PubMed] [Google Scholar]
- 8.Hamid O, El Fiky L, Hassan O, Kotb A, El Fiky S. Anatomic Variations of the Sphenoid Sinus and Their Impact on Trans-sphenoid Pituitary Surgery. Skull Base. 2008;18:9–15. doi: 10.1055/s-2007-992764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abuzayed B, Tanriöver N, Ozlen F. et al. Endoscopic endonasal transsphenoidal approach to the sellar region: results of endoscopic dissection on 30 cadavers. Turk Neurosurg. 2009;19:237–244. [PubMed] [Google Scholar]
- 10.Batra P S, Citardi M J, Gallivan R P, Roh H J, Lanza D C. Software-enabled computed tomography analysis of the carotid artery and sphenoid sinus pneumatization patterns. Am J Rhinol. 2004;18:203–208. [PubMed] [Google Scholar]
- 11.Batra P S, Citardi M J, Gallivan R P, Roh H J, Lanza D C. Software-enabled CT analysis of optic nerve position and paranasal sinus pneumatization patterns. Otolaryngol Head Neck Surg. 2004;131:940–945. doi: 10.1016/j.otohns.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Citardi M J, Gallivan R P, Batra P S. et al. Quantitative computer-aided computed tomography analysis of sphenoid sinus anatomical relationships. Am J Rhinol. 2004;18:173–178. [PubMed] [Google Scholar]
- 13.Tomovic S, Esmaeili A, Chan N J. et al. High-resolution computed tomography analysis of the prevalence of Onodi cells. Laryngoscope. 2012;122:1470–1473. doi: 10.1002/lary.23346. [DOI] [PubMed] [Google Scholar]
- 14.Elwany S, Yacout Y M, Talaat M, El-Nahass M, Gunied A, Talaat M. Surgical anatomy of the sphenoid sinus. J Laryngol Otol. 1983;97:227–241. doi: 10.1017/s0022215100094056. [DOI] [PubMed] [Google Scholar]
- 15.Jho H D Carrau R L McLaughlin M R Somaza S C Endoscopic transsphenoidal resection of a large chordoma in the posterior fossa Acta Neurochir (Wien) 1997139343–347., discussion 347–348 [PubMed] [Google Scholar]
- 16.Divitiis E D, Cappabianca P. Springer-Verlag/Wien, Austria; 2003. Endoscopic Endonasal Transsphenoidal Surgery. [Google Scholar]
- 17.Frank G, Pasquini E, Farneti G. et al. The endoscopic versus the traditional approach in pituitary surgery. Neuroendocrinology. 2006;83:240–248. doi: 10.1159/000095534. [DOI] [PubMed] [Google Scholar]
- 18.Charalampaki P, Ayyad A, Kockro R A, Perneczky A. Surgical complications after endoscopic transsphenoidal pituitary surgery. J Clin Neurosci. 2009;16:786–789. doi: 10.1016/j.jocn.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Campero A, Emmerich J, Socolovsky M. et al. Microsurgical anatomy of the sphenoid ostia. J Clin Neurosci. 2010;17:1298–1300. doi: 10.1016/j.jocn.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 20.Idowu O E, Balogun B O, Okoli C A. Dimensions, septation, and pattern of pneumatization of the sphenoidal sinus. Folia Morphol (Warsz) 2009;68:228–232. [PubMed] [Google Scholar]
- 21.Filho B C, Pinheiro-Neto C D, Weber R, Voegels R L. Sphenoid sinus symmetry and differences between sexes. Rhinology. 2008;46:195–199. [PubMed] [Google Scholar]
- 22.Fujii K, Chambers S M, Rhoton A L Jr. Neurovascular relationships of the sphenoid sinus. A microsurgical study. J Neurosurg. 1979;50:31–39. doi: 10.3171/jns.1979.50.1.0031. [DOI] [PubMed] [Google Scholar]
- 23.Szolar D, Preidler K, Ranner G. et al. The sphenoid sinus during childhood: establishment of normal developmental standards by MRI. Surg Radiol Anat. 1994;16:193–198. doi: 10.1007/BF01627594. [DOI] [PubMed] [Google Scholar]
- 24.Unal B, Bademci G, Bilgili Y K, Batay F, Avci E. Risky anatomic variations of sphenoid sinus for surgery. Surg Radiol Anat. 2006;28:195–201. doi: 10.1007/s00276-005-0073-9. [DOI] [PubMed] [Google Scholar]
- 25.Lu Y, Pan J, Qi S, Shi J, Zhang X, Wu K. Pneumatization of the sphenoid sinus in Chinese: the differences from Caucasian and its application in the extended transsphenoidal approach. J Anat. 2011;219:132–142. doi: 10.1111/j.1469-7580.2011.01380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shin J H, Kim S W, Hong Y K. et al. The Onodi cell: an obstacle to sellar lesions with a transsphenoidal approach. Otolaryngol Head Neck Surg. 2011;145:1040–1042. doi: 10.1177/0194599811418040. [DOI] [PubMed] [Google Scholar]