Abstract
Objectives The aim was to optimize the algorithm of operative intervention for trigeminal neuralgia (TN).
Design A multivariate analysis was undertaken to determine factors that had influenced both the initial choice of surgical intervention and the subsequent outcomes.
Setting The study was undertaken with patients who underwent microvascular decompression (MVD) or percutaneous glycerol injection (PGI) for TN between 2007 and 2009.
Participants Seventy-one consecutive patients (43 female) were selected.
Main Outcome Measures Data were prospectively recorded and included demographics, etiology, and presentation of TN, duration of symptoms, neurovascular contact, and the outcomes of surgery.
Results The response rates for MVD and PGI were 96.2% and 87.5%, respectively. The recurrence rates were 9.8% following MVD and 33.3% following PGI. Multivariate analyses confirmed multiple sclerosis and the identification of neurovascular contact as the only factors predictive of the choice of surgical intervention and the risk of recurrence following MVD.
Conclusions Our approach to choosing an operative intervention has been validated. The presence of neurovascular contact and the diagnosis of multiple sclerosis influenced the choice of surgery and were predictive of subsequent outcome. Both MVD and PGI offer effective treatment options for TN. Surgery should be offered early when medical management fails.
Keywords: trigeminal neuralgia, microvascular decompression, percutaneous glycerol injection, neurovascular contact, multiple sclerosis
Introduction
Trigeminal neuralgia (TN) is a relatively rare condition that is prevalent in 1 in 1,000 of the population.1 It is characterized by the abrupt onset of severe lancinating pain along the distribution of the trigeminal nerve. A large proportion of cases are due to neurovascular contact at the root entry zone of the trigeminal nerve,1,2 and magnetic resonance imaging (MRI) is the recommended diagnostic modality.3 The majority of cases are managed conservatively with neuroleptics such as carbamazepine; surgical intervention is reserved for those who fail medical therapy. The two interventions performed at our institution are microvascular decompression (MVD) and percutaneous glycerol injection (PGI) of the trigeminal ganglion.
The aim of this study was to evaluate the factors that influenced the choice of surgical intervention for TN and to investigate their correlation with the factors predictive of success as well as those predictive of the risk of recurrence.
Methods and Materials
Patients
Patients who underwent MVD or PGI for TN were identified from the skull base database and confirmed within the theater registry. Data were prospectively collected into the database and further information was obtained from digital hospital records and from follow-up telephone consultations. Informed consent was obtained from all patients prior to their inclusion in this study. The approval of the local ethics committee was not required due to the nature of this study. The information included patient demographics such as age and sex; characteristics of TN including the duration, distribution, and typical or atypical features of the symptoms; etiology, including the diagnosis of multiple sclerosis (MS); previous therapeutic procedures; radiological and operative findings for MVD; complications; and the outcome.
Definitions
The duration of symptoms was ascertained either from the full history of TN or from the point of recurrence following a previous operative procedure provided there was a period of relief. TN was classified as classical in idiopathic cases or if neurovascular compression was evident or as symptomatic in cases secondary to other pathology such as tumor growth or MS.
Radiological and operative findings were considered in cases of MVD only. Two consultant neuroradiologists (RS & AH), blinded to the affected side and surgical findings, retrospectively interpreted the images separately and reached a consensus regarding (1) the presence of a vessel, (2) whether this was an artery or a vein, and (3) whether the vessel was in contact with the trigeminal nerve. Their findings were analyzed against the “gold standard” of operative findings. Neurovascular contact was defined as the presence of any vessel in contact with the trigeminal nerve (irrespective of the point of contact and whether it distorted the nerve or not). The presence of a vessel specifically at the root entry zone of the trigeminal nerve did not influence the surgical management. In cases of mixed arterial and venous involvement, the comparisons were made to the vessel with the greatest degree of contact with the nerve.
The outcomes of the procedures were divided into the following categories: success, partial success, and failure. The operative procedures were considered to be successful if the patient had complete relief of pain and no longer required analgesia for this purpose. Patients were considered to have had a partial success if there was a reduction in pain such that they were able to reduce the dose of their medication, and failure described the absence of any postoperative relief of pain. Recurrence defined a complete or partial return of symptoms of TN following either a complete or partial success following operative intervention.
Follow-Up
Postoperative follow-up was conducted either by outpatient visits or telephone interviews. Questions were asked regarding the outcome and complications of the procedure.
Interventions for TN
All operative procedures were performed by or under supervision of consultant neurosurgeons SAR and ATK. Microvascular decompression was offered to patients with radiological evidence of a vessel in contact with the trigeminal nerve. Percutaneous glycerol injection of the trigeminal ganglion was considered in the absence of a vessel on MRI or in patients with a diagnosis of MS or comorbidities that might have prevented them from tolerating a major operative procedure.
Microvascular decompression was performed in a standard fashion via a retrosigmoid approach. In the event that no vessel in contact with the trigeminal nerve was identified, a partial rhizotomy was performed in patients with V2 or V3 neuralgia only so as to avoid ocular anesthesia. Percutaneous glycerol injection of the trigeminal ganglion was performed as an ablative procedure under general anesthesia.
Statistical Analysis
We analyzed the data using the software package SPSS 19 (Chicago, Illinois, USA). The results were expressed as mean (± standard deviation [SD] or range) or percentage as appropriate. Comparison between the groups was performed using the Mann-Whitney U test and the χ2 test as appropriate. Cox regression multivariate analysis using the stepwise method was applied to determine independent predictors of the choice of surgery, success of intervention, and recurrence. Significance was accepted at p < 0.05. The sensitivity and specificity (95% confidence intervals [CI]) of MRI in the description of neurovascular anatomy were calculated and compared using MedCalc 6.12 for Windows software (MedCalc Software, Mariakerke, Belgium). Kaplan-Meier survival analysis was undertaken to compare the risk of recurrence of TN following MVD versus PGI.
Results
Patients
Between 2007 and 2009, 71 patients with TN underwent 79 operative procedures (54 MVD and 25 PGI). Forty-nine patients underwent MVD, 18 received PGI, and 4 underwent both procedures. Five of the MVD procedures also included a partial rhizotomy. One patient underwent a repeat MVD, and three patients received a second PGI. The details of the patients are summarized in Table 1. Of the patients with symptomatic TN, eight had MS, one patient experienced neurovascular compression due to the presence of a basilar artery aneurysm, and another experienced neurovascular compression due to a vestibular schwannoma.
Table 1. Summary of Patient Details.
| Number of patients | 71 |
|---|---|
| Age (years)* | 59 (25–83) |
| Male/female: No. (%) | 28 (39)/43 (61) |
| Right/left/bilateral: No. (%) | 35 (49)/30 (42)/6 (8) |
| Classical/symptomatic: No. (%) | 61 (86)/10 (14) |
| Typical/atypical: No. (%) | 45 (63)/26 (37) |
| Duration of symptoms (years)a | 5.2 (0–20) |
| Duration of follow-up (months)a | 16.3 (0–41) |
Data shown represent mean (range).
TN was mainly distributed in V2 and V3 (32%); however, the mandibular branch was solely affected in a similar proportion of patients (31%). No information was available regarding the distribution of TN in six patients. Fifty-five patients (77%) had received no operative treatment prior to their first surgery during the study period. Percutaneous ablative procedures had been performed in 12 patients (17%) and MVD in 4 patients (6%) previously.
Factors Influencing the Choice of Intervention for TN
A univariate analysis was undertaken to determine the factors that influenced the choice of MVD versus PGI. The variables included were age, MS, previous MVD, previous percutaneous ablative procedure and the presence of neurovascular contact on prospective interpretation of MRI. All of the factors, with the exception of age, were found to have a significant influence on the choice of surgery. A Cox linear regression multivariate analysis confirmed previous MVD (relative risk [RR] –0.556, 95% CI –0.847 to –0.266, p < 0.0001), MS (RR –0.434, 95% CI –0.697 to –0.170, p = 0.002), and the presence of neurovascular contact on MRI (RR 0.220, 95% CI 0.014 to 0.426, p = 0.037) to be independent predictors of the choice of operative treatment. Previous percutaneous ablative procedure did not reach significance (p = 0.082).
Preoperative MRI versus Operative Findings
Fifty-three patients with TN received MVD. Forty-nine of these patients underwent preoperative radiological assessment using MRI. This was not undertaken by four patients due to claustrophobia and the presence of metalwork from previous maxillofacial surgery. The images of eight patients could not be retrieved. One patient was excluded from this analysis due to the finding of a tumor within proximity of the trigeminal nerve. The neuroradiologists analyzed the images of the remaining 40 patients.
Out of this group, a vessel was detected at surgery in 38 patients (artery, n = 23; vein, n = 5; artery plus vein, n = 10). The grid for calculating the sensitivity and specificity of MRI in detecting the presence of a vessel, whether this was an artery or a vein, and whether the vessel was in contact with the trigeminal nerve is displayed in Table 2, and the results are displayed in Table 3. Neuroradiologist A was significantly more accurate in the identification of an artery (p = 0.0488). However, the other comparative analyses did not identify any further statistically significant difference in the accuracy between the two neuroradiologists. The greatest accuracy was achieved as a consensus, although the differences did not reach statistical significance.
Table 2. Consensus Radiological Versus Operative Findings.
| Operative Findings | Radiological Findings | ||
|---|---|---|---|
| Present | Absent | ||
| Vessel | Present | 36 | 2 |
| Absent | 2 | 0 | |
| Artery | Present | 25 | 8 |
| Absent | 2 | 5 | |
| Vein | Present | 8 | 7 |
| Absent | 8 | 17 | |
| Artery and vein | Present | 3 | 7 |
| Absent | 2 | 28 | |
| Neurovascular contact | Present | 35 | 3 |
| Absent | 1 | 1 | |
Table 3. Sensitivity and Specificity of the Separate Neuroradiologist Reports and the Consensus.
| Sensitivity | Specificity | |||||
|---|---|---|---|---|---|---|
| A | B | Consensus | A | B | Consensus | |
| Vessel | 94.7 | 94.7 | 94.7 (90.7–100.0) | 0.0 | 0.0 | 0.0 (29.0–96.3) |
| Artery | 78.8 | 63.6 | 75.8 (57.7–88.9) | 71.4 | 71.4 | 71.4 (29.0–96.3) |
| Vein | 46.7 | 73.3 | 53.3 (26.6–78.7) | 76.0 | 64.0 | 68.0 (46.5–85.1) |
| Artery and vein | 20.0 | 20.0 | 30.0 (6.7–65.2) | 93.3 | 90.0 | 93.3 (77.9–99.2) |
| Contact | 92.1 | 89.5 | 92.1 (78.6–98.3) | 50.0 | 0.0 | 50.0 (1.3–98.7) |
Note: Data shown represent percentage (confidence intervals).
Results of Interventions
Microvascular decompression was successful in 48 operative cases (90.6%), partially successful in three cases (5.7%), and failed in only two cases (3.8%). No follow-up could be obtained for one patient. At a mean follow-up of 17.2 (range 2 to 41) months, recurrence occurred in five (9.8%) patients, two of whom had MS, and three underwent further operative treatment. Two patients opted for PGI of the trigeminal ganglion, and one patient underwent a re-exploration with subsequent rhizotomy.
Complications were encountered following 13 MVDs (24%), and these consisted of infections (n = 5), hydrocephalus (n = 2), vestibular dysfunction (n = 2), trigeminal neuropathy (n = 2), and single cases of CSF rhinorrhea and partial trochlear nerve palsy. One patient also experienced trismus in addition to vestibular dysfunction.
Twenty-two patients underwent PGI of the trigeminal ganglion. Trigeminal neuralgia returned in five patients, three of whom received a second PGI before 2010. Two of these patients experienced a further recurrence of their TN, and follow-up was unavailable for the third patient, resulting in exclusion from the analysis. Overall, of the 24 operative cases included in the study, 12 (50%) were successful, 9 (37.5%) were partially successful, and 3 (12.5%) failed to provide any relief of TN. Percutaneous glycerol injection was associated with an overall recurrence rate of 33.3%.
Complications occurred only in three cases and included dysesthesia and hypersensitivity around the ipsilateral eye, medial temporal leptomeningeal enhancement resulting in a seizure, and penetration of the oral mucosa with excessive bleeding.
Factors Predictive of Success of Interventions for TN
A univariate analysis of the factors that could potentially influence the success of either therapeutic intervention for TN is shown in Table 4. The variables included in the analysis were age, sex, previous intervention, the type of operation, and the etiology, features, and duration of TN. Only the type of therapeutic intervention (MVD versus PGI) was associated with a significantly higher chance of success, and this was confirmed by Cox linear regression multivariate analysis to be an independent predictor of success (RR 0.404, 95% CI 0.218 to 0.589, p < 0.0001). A univariate and multivariate analysis of the factors predictive of success of MVD found none to be of significance. Statistical evaluation was not undertaken within the glycerol injection treatment group due to an insufficient number of operative cases. A comparative analysis did not identify a significant difference in the predictive value of an artery as opposed to a vein on the success of MVD.
Table 4. Factors Influencing Success of Intervention for TN: Univariate Analysis.
| Variable | Success | p value |
|---|---|---|
| Age (years)a: successful versus unsuccessful | 59.6 (± 14.8) versus 57.4 (± 15.5) | 0.461 |
| Male versus female | 22/30 (73.3%) versus 38/47 (80.9%) | 0.574 |
| Classical versus symptomatic | 53/65 (81.5%) versus 7/12 (58.3%) | 0.123 |
| Typical versus atypical | 38/47 (80.9%) versus 22/30 (73.3%) | 0.574 |
| Duration of symptoms (month)a: successful versus unsuccessful | 60.5 (± 54.5) versus 58.1 (± 53.5) | 0.525 |
| Previous intervention: yes versus no | 16/23 (69.6%) versus 44/54 (81.5%) | 0.368 |
| MVD versus glycerol injection | 48/53 (90.6%) versus 12/24 (50%) | <0.0001 |
Abbreviations: MVD, microvascular decompression; TN, trigeminal neuralgia.
Data shown represent mean (± SD).
Factors Predictive of Risk of Recurrence of TN
A univariate analysis to evaluate whether any of the above factors were associated with a greater risk of recurrence of TN showed the type of operative intervention (MVD versus PGI) to have a significant influence (Table 5), and this was confirmed to be an independent predictor of recurrence on multivariate analysis (RR –0.233, 95% CI –0.422 to –0.044, p = 0.016). Fig. 1 illustrates the difference in the recurrence rate between the two operative interventions. A univariate analysis of the factors predictive of the risk of recurrence following MVD did not reveal any to be of significance. However, a multivariate analysis of the factors with a p value < 0.2 identified the presence of neurovascular contact at the time of surgery and a history of MS to be independent predictors of the risk of recurrence (RR –0.276, 95% CI –0.751 to –0.096, p < 0.0001; RR 0.628, 95% CI 0.633 to 1.292, p = 0.012 respectively). A comparative analysis failed to identify a significant difference in the influence of an artery as opposed to a vein on the risk of recurrence following MVD.
Table 5. Factors Predictive of Recurrence of TN Following Intervention: Univariate Analysis.
| Variable | Recurrence | p value |
|---|---|---|
| Age (years)a: no recurrence versus recurrence | 55.1 (± 16.7) versus 59.9 (± 14.5) | 0.337 |
| Male versus female | 3/28 (10.7%) versus 9/44 (20.5%) | 0.346 |
| Classical versus symptomatic | 8/61 (13.1%) versus 4/11 (36.4%) | 0.078 |
| Typical versus atypical | 9/46 (19.6%) versus 3/26 (11.5%) | 0.517 |
| Duration of symptoms (month)a: no recurrence versus recurrence | 47.8 (± 34.8) versus 62.5 (± 56.9) | 0.571 |
| Previous intervention | 6/23 (26.1%) versus 7/54 (12.9%) | 0.191 |
| MVD versus glycerol injection | 5/51 (9.8%) versus 7/21 (33.3%) | 0.032 |
Abbreviations: MVD, microvascular decompression; TN, trigeminal neuralgia.
Data shown represent mean (± SD).
Fig. 1.
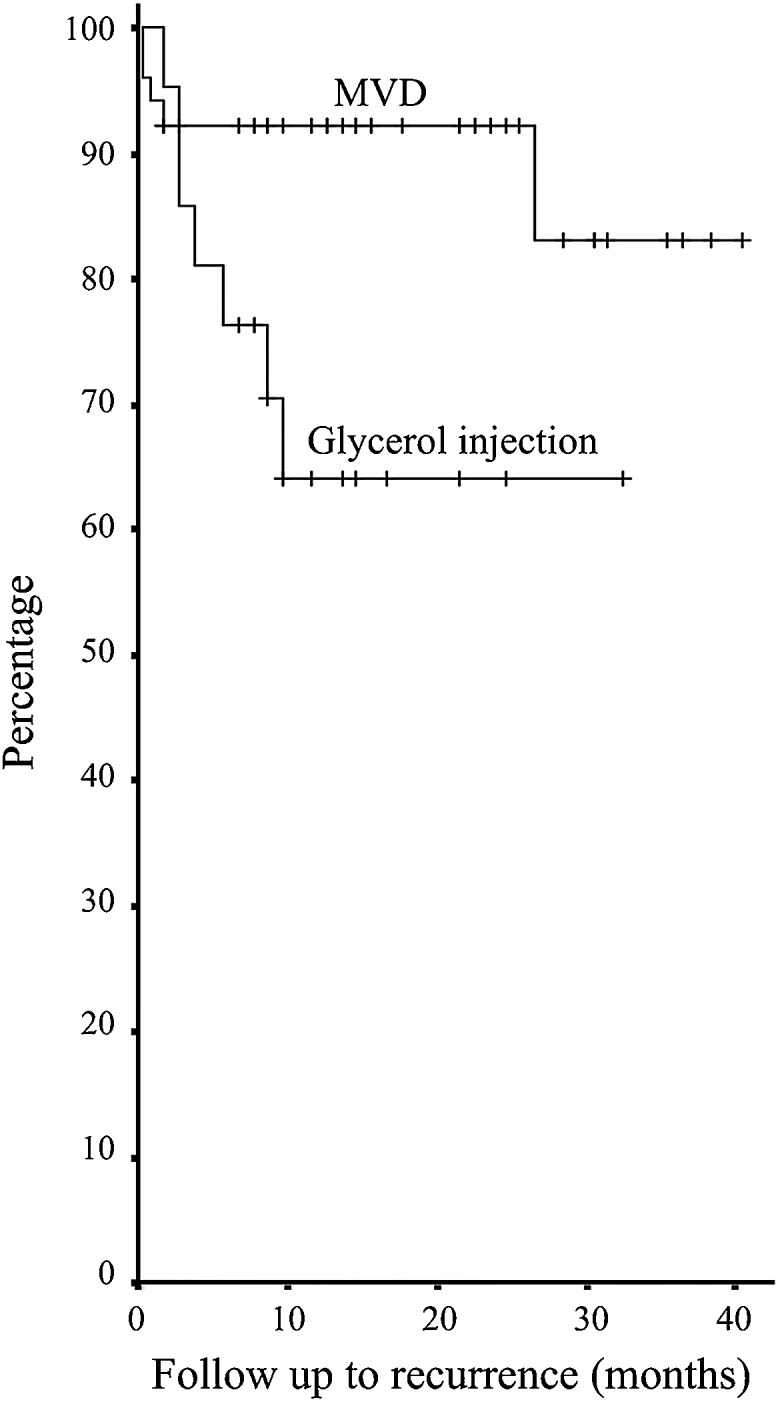
Kaplan-Meier curve demonstrating the recurrence rate for microvascular decompression and percutaneous glycerol injection.
Multiple Sclerosis
Of the eight patients with MS, all but one presented with typical symptoms of TN. Two underwent MVD, and both experienced a return of their symptoms within 2 months. Following this, one of these patients underwent a PGI along with six others who had MS. Out of this group only one patient experienced a recurrence of symptoms.
Discussion
Microvascular decompression was found to be an effective operative intervention for TN with a high success rate (90.6%) and a relatively low recurrence rate (9.8%), whereas PGI was associated with a modest success rate (50%) and a relatively high recurrence rate (33.3%). Multivariate analysis confirmed the type of therapeutic intervention to be an independent predictive factor of success and of recurrence.
A study of posterior fossa surgery including MVD and rhizotomy reported a reduction of TN in 98% of patients with complete resolution in 87%.4 Furthermore, a recent systematic review by Cruccu et al of the American Academy of Neurology and the European Federation of Neurological Societies (AAN-EFNS) that included five published reports identified immediate postoperative relief of TN in 90% of patients who underwent MVD; over 80% of patients remained without pain at 1 year and 73% at 5 years.3 Two further studies identified a similar long-term outcome.4,5 We reported complete relief in 90.6% of patients with a partial reduction of TN in a further 5.7%, and of these under 10% have experienced a return of their symptoms. This demonstrates comparable efficacy for MVD at this institution.
Our overall complication rate appears to be similar to that of the literature. In their systemic review, the AAN-EFNS identified major complications in 4% of patients following MVD for TN, including cerebrospinal fluid leaks, infarctions, or hematomas.3 Aseptic meningitis was found to be the most common complication, affecting a further 11% of patients, and ipsilateral hearing loss was reported as the major long-term problem in up to 10% of patients.3 We reported an overall complication rate of 24%, excluding cutaneous and oral sensory loss. Infection was the most common complication (9.3%).
The operative outcome for PGI has been investigated in several studies.6,7,8 Henson et al reported complete or partial relief of TN in 86% of patients who received PGI.6 However 15 of the 31 successfully treated patients (48.4%) experienced a return of their symptoms within a median time of 5 months.6 A more recent study found that 50% of patients experienced a recurrence of their TN within 16 months following PGI.7 The results of this study demonstrate a reduction of TN in 87.5% of operative cases; a third of these patients experienced recurrence within 9 months. Our morbidity rate with PGI is similar to that reported by others (12% versus 11%).7
Due to the limited duration of follow-up, it is difficult to compare the long-term outcomes of intervention with those of other studies. There are no randomized trials or recent case-matched comparative studies for MVD versus PGI in the treatment of TN. However, the differences between these two interventions with regards to their influence on success and recurrence cannot be ignored. The literature illustrates the advantages that MVD offers over PGI in achieving long-term relief of TN, and the results of our analysis agree with this consensus.3,4,5,6,7,8,9
A multivariate analysis of the factors predictive of recurrence of TN following MVD found the presence of neurovascular contact and a history of MS to be significant. These correlate with the factors we take into account when choosing an operative intervention, validating our approach.
The presence of neurovascular contact at the time of posterior fossa exploration indicated that patients were more likely to remain symptom free. Microvascular decompression was successful even in patients with simple neurovascular contact, in the absence of distortion of the trigeminal nerve or a vessel at the root entry zone. Given the high sensitivity of MRI (92.1%) in the identification of vascular contact, this imaging modality can often be relied upon to accurately inform a surgical decision. Although we found the specificity of MRI rather poor (50%), this result comes from only two reported cases, hence the very wide 95% CI of 1.3 to 98.7. Although this warrants further investigation, the practicality of this is difficult, as MVD is not routinely undertaken if no vessel is seen to be present on MRI.
The reliability of MRI in the preoperative assessment of patients considered for MVD has been subject to debate. The AAN-EFNS encountered a variety of results regarding the sensitivity (52 to 100%) and specificity (29 to 93%) of MRI and suspected this to be a consequence of the differences in the techniques employed.3 We found the routine assessment of scans using three-dimensional (3D) reformats, including sagittal views, assisted in identifying vascular presence. Some centers rely upon magnetic resonance tomographic angiography (MRTA) as an alternative imaging modality.5,10 Two studies reported MRTA to be sensitive in 90 to 96% of cases, with a specificity ranging from 36 to 100%.5,10 From the literature gathered, there does not appear to be strong evidence supporting the benefit of one imaging modality over the other. The latest AAN-EFNS guidelines recommend that patients suitable for MVD undergo high-resolution MRI.3
The etiological mechanism of MS in the pathogenesis of TN does not necessarily involve vascular compression, and therefore the benefits of decompressive surgery in the absence of an ablative procedure may be short-lived. However, one study reported that a large proportion of patients with MS achieved a positive long-term outcome following MVD and argues that this diagnosis should not prevent patients from being offered decompressive surgery.11 Antic et al reported that in patients with MS, partial sensory rhizotomy played a more significant role than MVD in providing relief of TN.12 We favored the choice of a percutaneous ablative procedure for patients with MS and found in cases of MVD they were significantly more likely to experience a return of their symptoms (n = 2).
Previous studies identified other significant predictors of recurrence such as female sex, younger age at the time of surgery, and the preoperative duration of symptoms lasting longer than 8 to 12 years.4,13 Although we have not found these factors to be of significance in the choice or outcome of surgery, some play a role in the decision of an operative intervention. Elderly patients with comorbidities are favored for a PGI due to the less-invasive nature of this procedure and its lower morbidity rate compared with that of MVD (12% versus 28%). Percutaneous glycerol injection is also favored by a history of previous decompressive surgery, as neurovascular contact has already been relieved. The duration of symptoms prior to surgery in our patients was often prolonged, with some patients experiencing symptoms for up to 20 years. This highlights the need for an early referral for consideration of surgery in those who fail medical therapy. In a previous survey of patients who underwent posterior fossa surgery, the majority expressed their desire for earlier intervention.14
Conclusion
The results of this study have validated our approach to choosing a surgical intervention. Factors, which influenced our decisions, were borne out as having significant impact on surgical outcomes. Microvascular decompression is preferred due to its higher success and lower recurrence rate in the majority of patients with the presence of neurovascular contact on MRI. Because of the lower complication rate, percutaneous glycerol injection should be considered in patients who have previously received MVD, have a history of MS, or are elderly with comorbidities. Given the high success of operative intervention and the prolonged duration of symptoms in the majority of patients, surgery should be offered earlier when conservative management fails.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Field E A, Longman L, Tyldesley W R. Oxford: Oxford University Press; 2003. Tyldesley's Oral Medicine. 5th ed. [Google Scholar]
- 2.Scully C, Porter S. Orofacial disease: update for the clinical team: 9. Orofacial pain. Dent Update. 1999;26:410–417. doi: 10.12968/denu.1999.26.9.410. [DOI] [PubMed] [Google Scholar]
- 3.Cruccu G, Gronseth G, Alksne J. et al. American Academy of Neurology Society; European Federation of Neurological Society . AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol. 2008;15:1013–1028. doi: 10.1111/j.1468-1331.2008.02185.x. [DOI] [PubMed] [Google Scholar]
- 4.Theodosopoulos P V, Marco E, Applebury C, Lamborn K R, Wilson C B. Predictive model for pain recurrence after posterior fossa surgery for trigeminal neuralgia. Arch Neurol. 2002;59:1297–1302. doi: 10.1001/archneur.59.8.1297. [DOI] [PubMed] [Google Scholar]
- 5.Sarsam Z, Garcia-Fiñana M, Nurmikko T J, Varma T R, Eldridge P. The long-term outcome of microvascular decompression for trigeminal neuralgia. Br J Neurosurg. 2010;24:18–25. doi: 10.3109/02688690903370289. [DOI] [PubMed] [Google Scholar]
- 6.Henson C F, Goldman H W, Rosenwasser R H. et al. Glycerol rhizotomy versus gamma knife radiosurgery for the treatment of trigeminal neuralgia: an analysis of patients treated at one institution. Int J Radiat Oncol Biol Phys. 2005;63:82–90. doi: 10.1016/j.ijrobp.2005.01.033. [DOI] [PubMed] [Google Scholar]
- 7.Kouzounias K, Lind G, Schechtmann G, Winter J, Linderoth B. Comparison of percutaneous balloon compression and glycerol rhizotomy for the treatment of trigeminal neuralgia. J Neurosurg. 2010;113:486–492. doi: 10.3171/2010.1.JNS091106. [DOI] [PubMed] [Google Scholar]
- 8.Wilkinson H A. Trigeminal nerve peripheral branch phenol/glycerol injections for tic douloureux. J Neurosurg. 1999;90:828–832. doi: 10.3171/jns.1999.90.5.0828. [DOI] [PubMed] [Google Scholar]
- 9.Pagni C A, Fariselli L, Zeme S. Trigeminal neuralgia. Non-invasive techniques versus microvascular decompression. It is really available any further improvement? Acta Neurochir Suppl (Wien) 2008;101:27–33. doi: 10.1007/978-3-211-78205-7_5. [DOI] [PubMed] [Google Scholar]
- 10.Han-Bing S, Wei-Guo Z, Jun Z, Ning L, Jian-Kang S, Yu C. Predicting the outcome of microvascular decompression for trigeminal neuralgia using magnetic resonance tomographic angiography. J Neuroimaging. 2010;20:345–349. doi: 10.1111/j.1552-6569.2009.00378.x. [DOI] [PubMed] [Google Scholar]
- 11.Sandell T Eide P K The effect of microvascular decompression in patients with multiple sclerosis and trigeminal neuralgia Neurosurgery 201067749–753., discussion 753–754 [DOI] [PubMed] [Google Scholar]
- 12.Antic B Peric P Posterior fossa exploration in treatment of trigeminal neuralgia associated with multiple sclerosis Surg Neurol 200971419–423., discussion 423 [DOI] [PubMed] [Google Scholar]
- 13.Barker F G II, Jannetta P J, Bissonette D J, Larkins M V, Jho H D. The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med. 1996;334:1077–1083. doi: 10.1056/NEJM199604253341701. [DOI] [PubMed] [Google Scholar]
- 14.Zakrzewska J M Lopez B C Kim S E Coakham H B Patient reports of satisfaction after microvascular decompression and partial sensory rhizotomy for trigeminal neuralgia Neurosurgery 2005561304–1311., discussion 1311–1312 [DOI] [PubMed] [Google Scholar]


