Abstract
Spontaneous cerebrospinal fluid (CSF) otorrhea due to tegmen tympani defects can result in hearing impairment and predispose to meningitis. Seizures or neurological deficits are additional risks, particularly when associated with an encephalocele. Surgical repair of the dural defect through a middle cranial fossa (MCF) approach is a treatment option under these circumstances. This series describes eight individuals who presented with CSF otorrhea and MCF encephaloceles associated with conductive hearing loss. Defects in the tegmen tympani were noted in all patients on preoperative cranial imaging, and six of the eight patients had an associated encephalocele. The average age was 57 years (range 26 to 67) with a male:female ratio of 7:1. Most defects occurred on the left side (6 left/2 right). A standard MCF approach and repair of the dural defect with an autologous dural graft (Durepair or DuraGen, Medtronic, Minneapolis, Minnesota, USA) and a synthetic polymer glue (DuraSeal, Covidien, Mansfield, Massachusetts) was performed in each case with universal success. Resolution of the CSF otorrhea was noted in all cases. All cases but one exhibited an improvement in hearing. One patient developed a delayed methicillin-resistant Staphylococcus aureus meningitis 3 months after surgery that resolved with surgical re-exploration and antibiotic therapy. Facial nerve monitoring was standard. All patients exhibited normal facial function postoperatively. Prophylactic lumbar drain placement was only utilized in the first three patients. The MCF approach is an excellent route to effectively repair CSF leaks and encephaloceles due to tegmen tympani and dural defects.
Keywords: middle cranial fossa, tegmen tympani, cerebrospinal fluid leak, otorrhea, encephalocele, hearing loss
Introduction
Defects in the floor of the middle cranial fossa (MCF) are commonly seen in cadaveric studies and encountered in surgical practice.1 Dehiscence of the bone overlying the petrous internal carotid artery (ICA), greater superficial petrosal nerve (GSPN), or geniculate ganglion are reported in 15 to 20% of individuals, placing these structures at risk for potential injury during surgery.1,2,3,4 In addition, bony defects in the tegmen tympani, if accompanied by dural defects, can result in cerebrospinal fluid (CSF) egress into the nasal and/or the middle ear spaces and predispose to the development of an encephalocele (Fig. 1), with a concomitant risk of seizures, hearing dysfunction, and/or meningitis. We report a series of eight individuals (Table 1) who presented with hearing loss, middle ear fluid collections, and temporal encephalocele that were successfully addressed by a MCF craniotomy and repair of tegmen tympani and dural defect(s). We explore the pathogenesis of this condition and describe a simple, yet effective, surgical technique that has provided our patients with a salutary outcome.
Fig. 1.
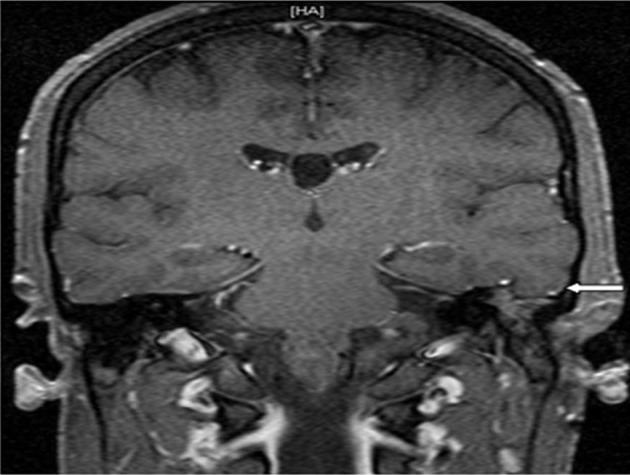
T1-weighted post-gadolinium enhanced coronal magnetic resonance imaging demonstrating a left-sided temporal encephalocele (arrow). An incidental cavum septum pellucidum is noted.
Table 1. Demographics, Presenting Complaints, and Postoperative Outcome in Patients Undergoing Middle Cranial Fossa Approach to Repair Cerebrospinal Fluid Otorrhea Associated with Tegmen Tympani Defects.
| Age | Sex | Presenting complaint | Side involved | Lumbar drain use | Postoperative audiogram | Postoperative facial nerve function | Postoperative CSF leak | Postoperative complications |
|---|---|---|---|---|---|---|---|---|
| 60 | F | CSF drainage in throat, Hearing loss, Mastoiditis | Left | Yes | Not Improved | Normal | None | Delayed wound infection |
| 67 | M | Hearing loss, CSF otorrhea | Left | Yes | Improved | Normal | None | None |
| 62 | M | Hearing loss, CSF otorrhea | Left | Yes | Improved | Normal | None | None |
| 26 | M | Hearing loss, CSF otorrhea | Left | No | Improved | Normal | None | None |
| 64 | M | Hearing loss, CSF otorrhea | Left | No | Improved | Normal | None | None |
| 57 | M | Hearing loss, CSF otorrhea | Left | No | Improved | Normal | None | None |
| 57 | M | Hearing loss, CSF otorrhea | Right | No | Improved | Normal | None | None |
| 63 | M | Hearing loss, CSF otorrhea | Right | No | Improved | Normal | None | None |
Abbreviation: CSF, cerebrospinal fluid.
Methods
The Loyola University Medical Center Institutional Review Board approved this investigation, which consisted of a retrospective chart review of patients who underwent a MCF repair of tegmen tympani defects at our institution by a single neurosurgeon (VCP) and neuro-otologist (SJM). The goal was to perform an outcome analysis of the resolution of CSF leak with preservation of facial nerve function and assessment of hearing preoperatively and postoperatively.
Surgical Procedure
Patients are positioned supine with a shoulder roll underneath the ipsilateral shoulder and the head gently turned 60 degrees toward the contralateral side. Lumbar drain placement was not universally employed; avoiding lumbar CSF drainage allows CSF to remain in the cranial subarachnoid space, providing a cushion for the temporal lobe and protecting it during surgery. Prophylactic antibiotics, a 0.5-g/kg bolus dose of intravenous mannitol, and an antiepileptic medication are routinely administered. Ipsilateral facial nerve monitoring is standard.
A horseshoe-shaped incision is made beginning within 1 cm anterior to the tragus and arcing superiorly approximately 3 to 4 cm above the pinna of the ear, extending down to the asterion posteriorly. The base of the incision is wider than the height of the incision to ensure perfusion of the scalp flap. The temporalis muscle is elevated from inferior to superior and from posterior to anterior, with preservation of its underlying fascial sheath as previously described.5 This critical maneuver helps preserve its neurovascular supply. Three to four burr holes are placed to achieve a craniotomy bone flap measuring approximately 4 to 5 cm across with exposure that extends two thirds anterior to the external auditory meatus (EAM) and one third posterior. The anterior burr hole is located anterior and superior to the posterior root of the zygoma, and the posterior burr hole is located just above and anterior to the asterion. The squamous temporal bone is then drilled flush to the floor of the MCF.
Under microscopic visualization and with careful microdissection, the dura is elevated in a posterior-to-anterior direction to prevent avulsion of the GSPN.6 The dural elevation is centered over the tegmen tympani. The key landmarks are the middle meningeal artery anteriorly, the GSPN medially, the arcuate eminence posteriorly, and the lateral margin of the craniotomy. These delineate the area of the tegmen tympani and MCF floor where these defects are encountered and can be repaired. With the dura elevated and the tegmen tympani exposed, the dural and bony defects are identified. The defects tend to be multiple, irregular areas of dehiscent bone measuring 2 to 5 mm with associated defects in the dura in relative proximity. Encephaloceles herniating through openings in the dura are reduced or amputated with bipolar electrocautery until they recess behind the dural margin. In elderly patients, the dura is thin and friable and must be carefully elevated or the tear may expose underlying temporal cortex. The dural defects are covered with Surgicel Fibrillar (Ethicon, Neuchatel, Switzerland) and repaired either via primary suture approximation or with a Durepair or DuraGen graft (Medtronic, Minneapolis, Minnesota, USA). The bony defects are sometimes carefully covered with pieces of Gelfoam (Pharmacia and Upjohn Company, Kalamazoo, Michigan, USA) that overlap the edges and reinforced with Surgicel Fibrillar. We avoid placing muscle plugs in this location to circumvent migration of remnants of tissue into the middle ear, which could result in hearing loss. The bone defect in the tegmen tympani is not spanned with any material. It is also critical to avoid injury to the vein of Labbé, particularly on the left side, which drains the temporal lobe and perisylvian cortex into the transverse sinus. Tearing or excessive pressure that can compromise this important structure may result in a venous infarction within the temporal lobe and perisylvian cortex, which can have significant functional consequences. The temporal lobe is then allowed to rest back over the repair, adequately securing it. The bone flap is resecured with titanium plates. The temporalis muscle is reattached with absorbable suture to chevron-style holes in the cranium along the superior temporal line. The scalp is meticulously closed in layers to ensure a watertight closure.
Results
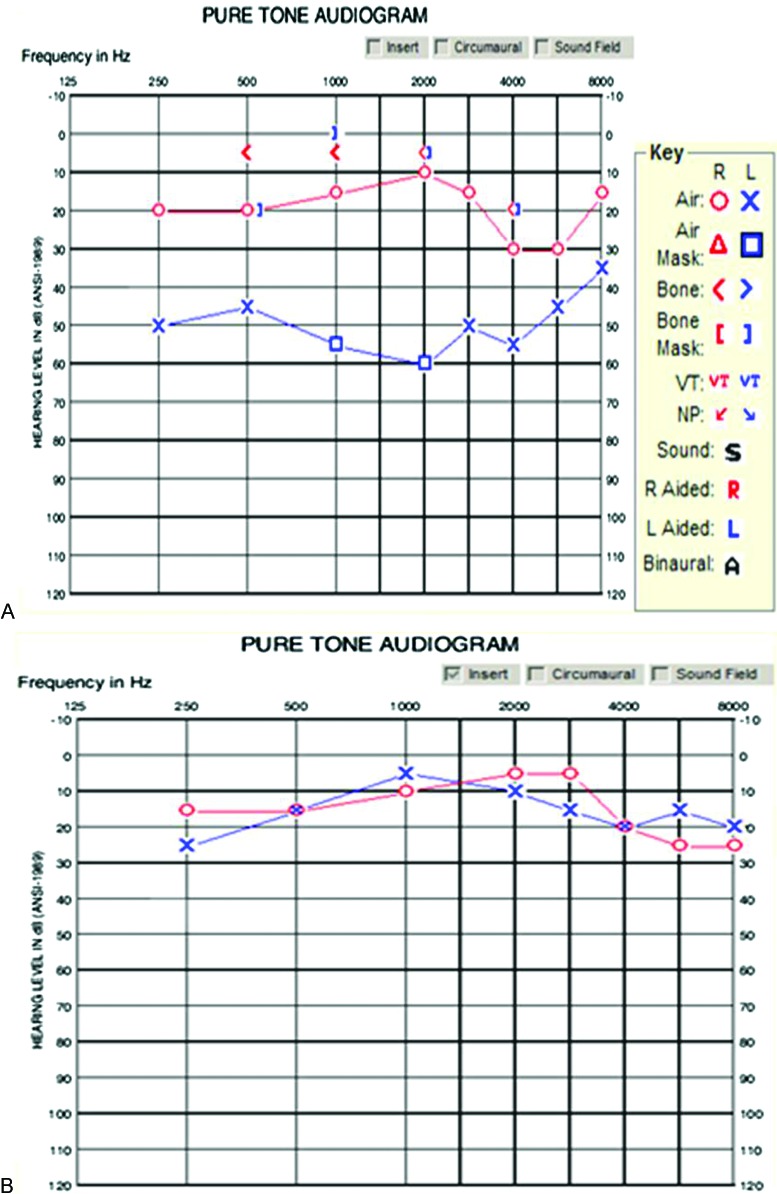
Eight patients with tegmen tympani defects were reviewed in this series, seven men and one woman (Table 1). The average age was 57 years. The most common presenting complaints were ipsilateral subjective hearing loss and ipsilateral otorrhea. All but one patient presented with spontaneous symptoms and had no history of head trauma. The youngest patient (26 years old) in the series suffered a motor vehicle collision, from which he had multiple skull fractures and developed delayed otorrhea. All patients had preoperative and postoperative (4 to 6 months) audiograms (Fig. 2A, B). Subjective hearing improvement was noted in all patients, but objective hearing improvement was documented in seven of the eight patients. Intraoperative facial nerve monitoring was employed in all patients and all patients had intact facial nerve function following surgery. Lumbar drains were employed in three of eight patients. No immediate postoperative CSF leaks were encountered, and CSF otorrhea resolved in all patients. One patient presented 3 months after surgery with meningeal signs and wound erythema. A lumbar drain was placed and she was taken to the operating room for a surgical re-exploration. The dural repair appeared intact and no CSF leak was noted under microscopic inspection. No purulence was observed but the wound was washed out with an antibiotic solution and the dura reinforced with Surgicel Fibrillar. Cultures from the wound and CSF revealed methicillin-resistant Staphylococcus aureus, and she was treated with intravenous antibiotics for 6 weeks. The patient recovered completely with successful resolution of the infection. Although this patient subjectively reported improved hearing, the postoperative audiogram did not confirm that.
Fig. 2.
(A) Preoperative and (B) postoperative audiograms demonstrating improved left-sided hearing following left middle cranial fossa cerebrospinal fluid otorrhea repair.
Discussion
The MCF, which houses the temporal lobe, is largely formed by the greater wing of the sphenoid bone and the squamous and petrous portions of the temporal bone. It transmits numerous important vessels and nerves, in particular the second division of the trigeminal nerve through the foramen rotundum and the third division of the trigeminal nerve through the foramen ovale, both of which are contained within the greater wing of the sphenoid bone. Near the junction of the greater wing of the sphenoid and the petrous portion of the temporal bone is the foramen spinosum that transmits the middle meningeal artery.
The tympanic cavity is an air-filled irregular space within the middle ear in the temporal bone that contains three auditory ossicles (malleus, incus, and stapes) along with their attached muscles. The roof of the tympanic cavity, formed by the tegmen tympani, separates the tympanic cavity from the MCF contents. The tegmen tympani is formed by the petrous and squamous portions of the temporal bone. The suture line between these two portions, the petrosquamous suture, is unossified in young individuals and does not close until adult life. Through this suture, veins from the middle ear pass through to the superior petrosal sinus. The tegmen tympani extends posteriorly to roof the tympanic antrum and anteriorly to cover the semicircular canals.4 Its lateral edge corresponds with the remnants of the petrosquamous suture.
The medial part of the tegmen tympani develops form the otic capsule during chondral ossification, and the lateral portion of the tegmen tympani develops by way of membranous ossification.7 Congenital defects of the tegmen tympani develop ventral to the geniculate ganglion and may be due to incomplete ossification of the tegmental process of the otic capsule.7 Inadequate closure of the petrosquamous suture may be a factor as well.8 Defects in the tegmen tympani may be accompanied by defects in the overlying dura, with resultant egress of CSF or cortical tissue forming an encephalocele. Trauma or infection involving the middle ear and temporal bone are likely considerations, but often the otorrhea accompanying a tegmen tympani defect is spontaneous in nature.9 Regardless of etiology, the consequence of CSF otorrhea or encephalocele formation is hearing loss, seizures, or meningitis. It is hence imperative to address these problems in a timely fashion.
The procedure described above is similar to the MCF approach to the internal auditory canal for removal of an intracanalicular vestibular schwanomma.10 However, the exposure does not need to extend medial to the arcuate eminence and requires less retraction of the temporal lobe. Early in the series, we employed a lumbar drain to assist the process of dural healing via CSF diversion and empirically decrease the risk of recurrent CSF leakage through the repaired dural defect. Later in the series, we found that this step was generally not required. Intraoperatively, the retained CSF within the subarachnoid space provided a protective cushion for the undersurface of the temporal lobe and allowed for the maintenance of fullness of the temporal lobe dura. The fullness of the temporal lobe was found to aid in tightly sealing the tegmen tympani defect. However, the option of lumbar CSF drainage may lessen the degree of temporal lobe retraction and is utilized very effectively in MCF approaches. Careful elevation of the dura from a posterior-to-anterior direction and complete avoidance of bipolar cautery on the MCF floor are essential to preserve facial nerve function.6 A meticulous reconstruction of the dural defect is essential for a good outcome. The eight patients that received this operation had good outcomes with complete resolution of preoperative symptoms, durable cessation of CSF otorrhea, and preservation of facial function in all patients. The one patient who had a delayed onset of meningitis and a wound infection ultimately recovered well but did not have objective improvement in hearing.
Conclusion
The MCF approach allows for optimal exposure and treatment of CSF leaks and encephaloceles due to tegmen tympani defects. It is a practical and effective option with minimal morbidity that can provide complete relief of the patient's symptoms and clinical presenting signs.
Acknowledgment
Administrative Assistant: Lauren Nagle lnagle@lumc.edu.
References
- 1.Arìstegui M, Cokkeser Y, Saleh E. et al. Surgical anatomy of the extended middle cranial fossa approach. Skull Base Surg. 1994;4:181–188. doi: 10.1055/s-2008-1058953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lang D V. Macroscopic bony deficiency of the tegmen tympani in adult temporal bones. J Laryngol Otol. 1983;97:685–688. doi: 10.1017/s0022215100094834. [DOI] [PubMed] [Google Scholar]
- 3.Maina R, Ducati A, Lanzino G. The middle cranial fossa: morphometric study and surgical considerations. Skull Base. 2007;17:395–403. doi: 10.1055/s-2007-991117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parisier S C The middle cranial fossa approach to the internal auditory canal: An anatomic study stressing critical distances between surgical landmarks Laryngosope 197787(suppl):1–20. [DOI] [PubMed] [Google Scholar]
- 5.Kadri P A, Al-Mefty O. The anatomical basis for surgical preservation of temporal muscle. J Neurosurg. 2004;100:517–522. doi: 10.3171/jns.2004.100.3.0517. [DOI] [PubMed] [Google Scholar]
- 6.Tanriover N Sanus G Z Ulu M O et al. Middle fossa approach: microsurgical anatomy and surgical technique from the neurosurgical perspective Surg Neurol 200971586–596., discussion 596 [DOI] [PubMed] [Google Scholar]
- 7.Tóth M, Helling K, Baksa G, Mann W. Localization of congenital tegmen tympani defects. Otol Neurotol. 2007;28:1120–1123. doi: 10.1097/MAO.0b013e31815aee0c. [DOI] [PubMed] [Google Scholar]
- 8.Wetmore S J, Herrmann P, Fisch U. Spontaneous cerebrospinal fluid otorrhea. Am J Otol. 1987;8:96–102. [PubMed] [Google Scholar]
- 9.Brodie H A, Thompson T C. Management of complications from 820 temporal bone fractures. Am J Otol. 1997;18:188–197. [PubMed] [Google Scholar]
- 10.House W F. Surgical exposure of the internal auditory canal and its contents through the middle, cranial fossa. Laryngoscope. 1961:1363–1385. doi: 10.1288/00005537-196111000-00004. [DOI] [PubMed] [Google Scholar]