Abstract
Calf muscle pump is the motive force enhancing return of venous blood from the lower extremity to the heart. It causes displacement of venous blood in both vertical and horizontal directions, generates ambulatory pressure gradient between thigh and lower leg veins, and bidirectional streaming within calf perforators. Ambulatory pressure gradient triggers venous reflux in incompetent veins, which induces ambulatory venous hypertension in the lower leg and foot. Bidirectional flow in calf perforators enables quick pressure equalization between deep and superficial veins of the lower leg; the outward (into the superficial veins) oriented component of the bidirectional flow taking place during calf muscle contraction is no pathological reflux but a physiological centripetal flow streaming via great saphenous vein into the femoral vein. Calf perforators are communicating channels between both systems making them conjoined vessels; they are not involved in the generation of pathological hemodynamic situations, nor do they cause ambulatory venous hypertension. The real cause why recurrences develop has not as yet been cleared. Pressure gradient arising during calf pump activity between the femoral vein and the saphenous remnant after abolition of saphenous reflux triggers biophysical and biochemical events, which might induce recurrence. Thus, abolition of saphenous reflux removes the hemodynamic disturbance, but at the same time it generates precondition for reflux recurrence and for the comeback of the previous pathological situation; this chain of events has been called hemodynamic paradox.
Keywords: venous hemodynamics, calf perforators, venous hypertension, hemodynamic paradox
Although flow in the arterial system constitutes essentially an uncomplicated pulsing streaming in one direction from the heart to the periphery, venous return from the lower extremity to the heart in upright position is directed against the gravitation force and displays a more complex pattern; this field of the venous circulation and pathophysiology continues to be an insufficiently understood sphere with controversial perceptions concerning pressure and flow interactions in three different parts of venous circulation in the lower extremity: in deep and superficial veins, and in communicating channels between them. Moreover, several hemodynamic phenomena of the venous circulation have not so far been unequivocally apprehended or precisely defined, which provides for misunderstanding and misinterpretations, and deforms results presented after surgical and nonsurgical treatment of varicose veins.
In this article, proven evidences pertaining to the influence of calf pump activity on pressure and flow changes that affect venous return to the heart were gathered from the references. Special point of view was concentrated on the hemodynamic significance of ambulatory venous hypertension, and on confusing opinions concerning incompetent calf perforators and reflux recurrence.
Effect of the Hydrostatic Pressure
During quiet standing with relaxed calf muscles, gravitation force induces hydrostatic hypertension in the veins of the lower extremity. The zero line lies at the level of the right atrium; beneath that point the pressure rises by 0.8 mm Hg/cm and reaches approximately 90 mm Hg at the ankle, depending on body height. The pressure is equal in deep and superficial veins at the same hydrostatic level.1 There is no reflux in incompetent veins of the lower limb during quiet standing with relaxed calf muscles, as verified by direct flow measurements.2 The venous flow toward the heart at rest is provided mainly by vis a tergo, that is, by the resting heart energy beyond the capillaries; pressure difference between venules and right atrium attains approximately 15 mm Hg.
The hydrostatic pressure is a physical factor inducing dilatation of veins, but it is not the motive force evoking venous reflux. Different levels of hydrostatic pressure do not provoke flow. Flow in the veins of the lower extremity is induced by pressure difference related to the same hydrostatic level.
Effect of Increased Intra-abdominal Pressure
Transmission of increased intra-abdominal pressure into the veins of the lower extremity is another important factor: it can produce values exceeding 200 mm Hg, which significantly surpass values of the hydrostatic pressure and have a corresponding veno-dilating effect. The transmission is facilitated by the circumstance that in varicose vein patients there is no competent valve between the saphenofemoral junction (SFJ) and the inferior caval vein in the overwhelming majority of cases.3 4 The consequence is progressive dilatation of the great saphenous vein (GSV) beginning from the SFJ with ensuing incompetence. This is an argument supporting the descending theory and explaining the development of saphenous vein incompetence.
Interestingly, small saphenous vein (SSV) incompetence occurs three to four times less frequently than GSV incompetence, although the hydrostatic pressure at the saphenopopliteal junction is higher than at the SFJ; that is at odds with the ascending theory. The possible explanation is that the SSV is protected against the effect of the increased intra-abdominal pressure by competent valves in the superficial femoral vein. This assumption is corroborated by the fact that in most cases of SSV incompetence, the deep venous axis (femoral, popliteal) above the saphenopopliteal junction is also incompetent,5 6 so that the SSV is exposed to the impact of the intra-abdominal pressure.
Thus, the dilating effect of increased intra-abdominal pressure contributes to the development of incompetent venous conduits and increases the dilating effect of the hydrostatic pressure in the veins of the lower extremity in varicose vein disease.
Activation of Venous Flow
Activity of the calf muscle pump is the motive force that significantly affects venous circulation in the lower extremity. It produces streaming of venous blood in both vertical and horizontal directions.
The vertical flow has two components: a centripetal flow during calf muscle contraction and a centrifugal flow during muscle relaxation. Pressure changes are generated in deep lower leg veins. Calf muscle contraction elevates the pressure to approximately 140 mm Hg and expels venous blood into the popliteal and femoral vein; the pressure difference between the posterior tibial vein (PTV) and popliteal vein amounts in average to 51 mm Hg.1 The centrifugal component during muscle relaxation lasts in competent veins approximately 200 to 300 milliseconds and represents the physiological centrifugal flow7; in incompetent veins, it produces reflux of variant intensity and a duration exceeding 0.5 second.
The horizontal flow takes place in communicating channels between deep and superficial veins of the lower leg. The increased pressure arising during calf muscle contractions is transmitted from deep lower leg veins into the saphenous system through calf perforating veins. Simultaneous pressure measurements in the PTV and GSV in varicose vein patients detected that the peak systolic pressure in the PTV was higher than in the GSV; the average difference was 13 mm Hg. Saphenous reflux did not influence the systolic pressure difference. During muscle relaxation the pressure situation turned round, the peak pressure in the GSV was higher than in the PTV; saphenous reflux significantly increased the pressure difference8 9 10 (Fig. 1).
Fig. 1.
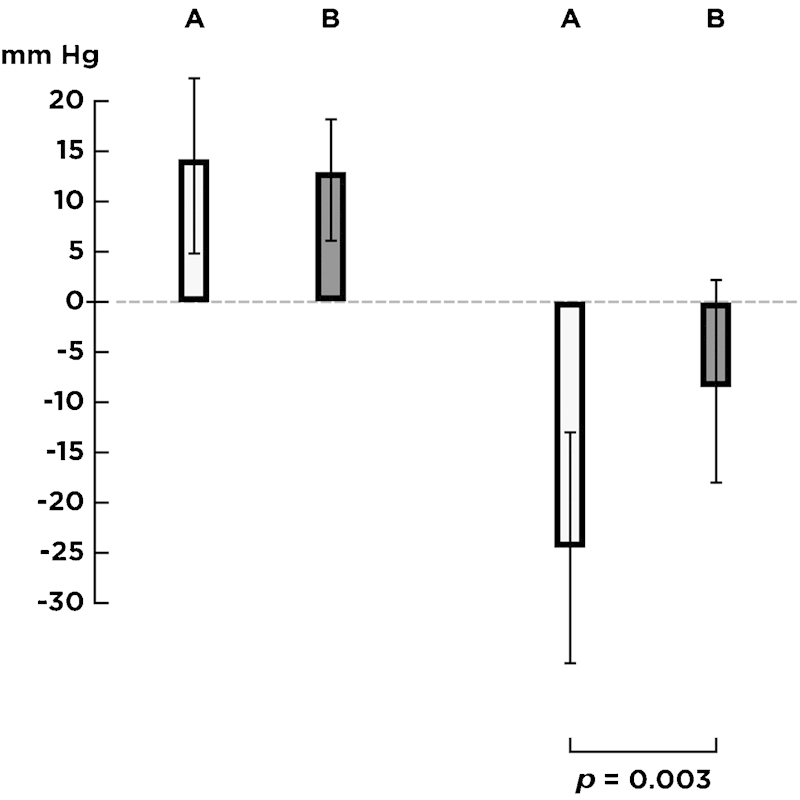
Peak pressure differences between posterior tibial vein and great saphenous vein. Left: during muscle contraction, right: during muscle relaxation. A: with reflux, B: without reflux. Saphenous reflux significantly increased the pressure difference during muscle relaxation.
Hence, the blood is expressed during muscle contraction from the PTV into the GSV via lower leg perforators and increases the pressure in the GSV; the blood afflux taking place through lower leg perforators is no pathological reflux, but a physiological centripetal flow of venous blood streaming further through the GSV into the femoral vein, as documented by duplex ultrasonography. It causes neither ambulatory venous hypertension nor another pathological situation.
During muscle relaxation, the blood returns back from the GSV into the PTV; this bidirectional streaming was documented by duplex ultrasonography in healthy persons11 and by electromagnetic flow measurements in varicose vein patients.2 The vector of the bidirectional flow is oriented inward into the PTV: larger amount of blood flows from the superficial into the deep veins of the lower leg than in the opposite direction during calf pump activity, especially if saphenous reflux is present.2
Simultaneous recordings of the mean (damped) pressure in the PTV and GSM revealed that the pressure curves were very similar, nearly identical, both in healthy persons and in varicose vein patients10 12 13 (Figs. 2 and 3). This documents that lower leg perforators allow unhindered quick pressure transmission and equalization between deep and superficial veins; deep and superficial veins in the lower leg form conjoined vessels.
Fig. 2.
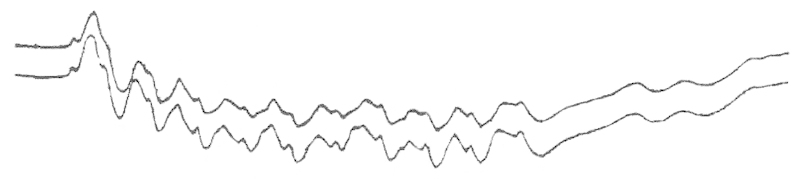
Simultaneous recordings of the mean pressure in the posterior tibial vein (lower curve) and great saphenous vein (upper curve) in a varicose vein patient after temporary occlusion of the saphenous reflux. Physiological decrease in pressure during calf pump activity. Pressure curves in both veins are nearly identical.
Fig. 3.
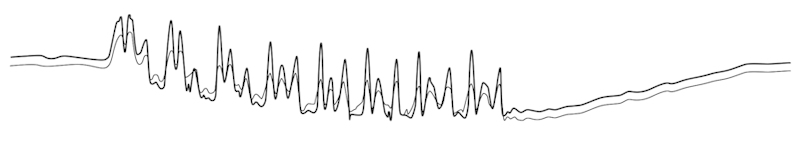
Simultaneous recordings of the factual pressure in the posterior tibial vein (upper curve) and great saphenous vein (lower curve) in a patient with severe chronic venous insufficiency. After interruption of saphenous reflux, physiological decrease in pressure was recorded both in posterior tibial and in great saphenous vein during calf pump activity; slow return to the starting level during the following recovery period. Both curves are nearly identical demonstrating pressure behavior typical of conjoined vessels.
Ambulatory Pressure Gradient: Ambulatory Venous Hypertension
Calf pump activity evokes physiological decrease in pressure to approximately 25 mm Hg in the veins of the lower leg and foot. In contrast, the pressure in the thigh veins (popliteal and femoral veins) does not decrease: it exhibits fluctuations during calf pump activity, but the mean pressure keeps the starting level of the quiet standing up. As a consequence, pressure difference between thigh and lower leg veins arises1 8 12 (Fig. 4); it was called ambulatory pressure gradient and yielded the value of 37.4 ± 6.4 mm Hg13 (Fig. 5).
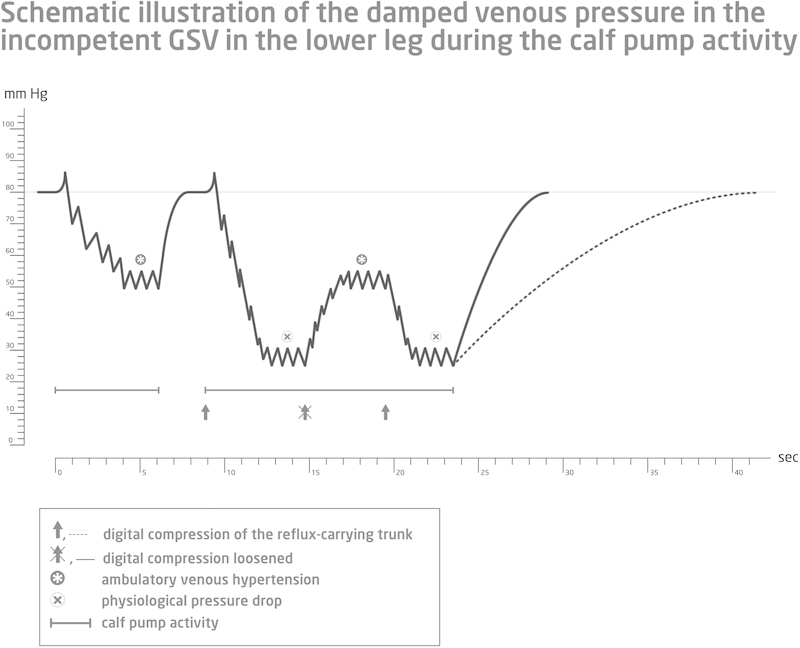
Fig. 4.
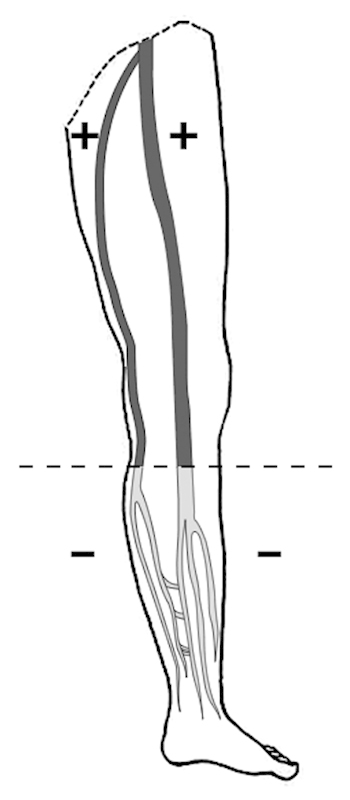
Calf pump activity generates pressure difference between thigh and lower leg veins, which has been called ambulatory pressure gradient. The dashed line indicates the boundary of the ambulatory pressure gradient. The sign + means higher pressure, the sign − means lower pressure.
Fig. 5.
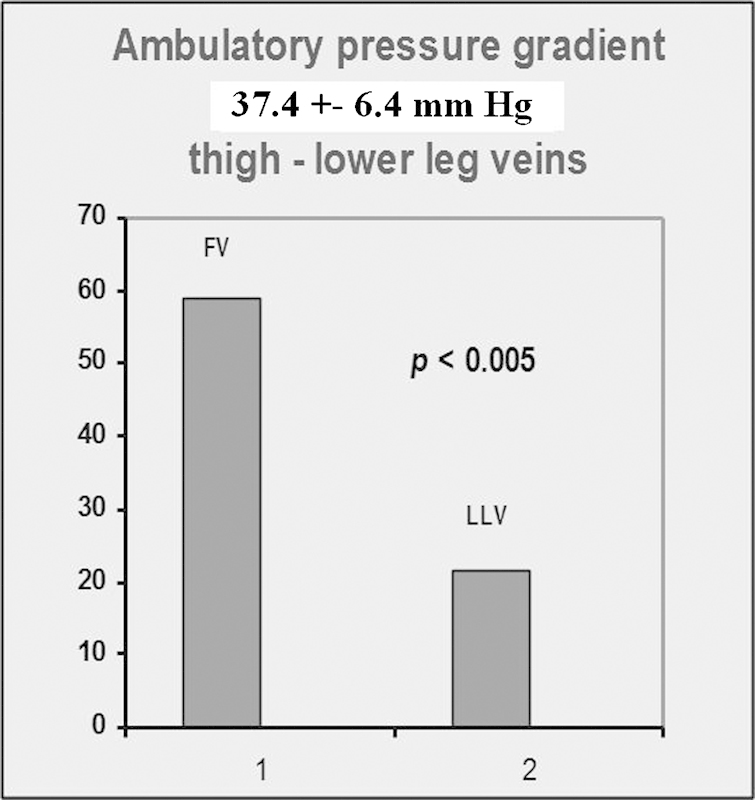
Ambulatory pressure gradient: statistical evaluation yielded the value of 37.4 ± 6.4 mm Hg. The pressure difference between thigh and lower leg veins was highly significant.
Ambulatory pressure gradient sets off venous reflux in incompetent veins. Venous reflux can be defined as a centrifugal flow of blood within an incompetent venous channel connecting both poles of the ambulatory pressure gradient. The higher pole lies in the femoral or iliac vein and the lower pole in the lower leg vein. Reflux takes place during relaxation of calf muscles and stops as soon as the ambulatory pressure gradient is equalized. It causes ambulatory venous hypertension, the severity of which depends on the intensity of the centrifugal flow expressed in mL/s.
Ambulatory venous hypertension can be defined as a deviation from the physiological decrease in pressure to higher values. The severity of ambulatory venous hypertension is determined by the difference between calf pump output (analogous to cardiac output—the calf pump has been called “peripheral heart”) and the inflow into the venous system, which is the sum of flow coming through capillaries plus the amount of reflux. It is irrelevant whether reflux takes place in superficial or deep veins; reflux intensity is the decisive factor. When the expelled and refluxing blood volumes equilibrate, no decrease in pressure occurs during calf pump activity. This severe hemodynamic disturbance in varicose vein disease develops due to reflux, not due to failure of the calf muscle venous pump, as demonstrated in Figs. 3 and 6.
Fig. 6.
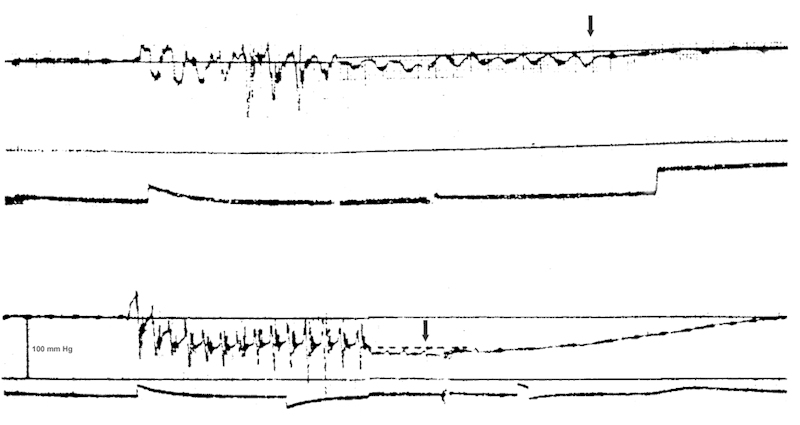
Pressure recordings from the great saphenous vein above the ankle in a patient with chronic venous insufficiency and varicose ulcer. Factual pressure followed by damped pressure. Top: the gravest form of ambulatory venous hypertension; no decrease in pressure during calf pump activity. Bottom: restoration of physiological pressure conditions after temporary occlusion of the refluxing great saphenous vein. Arrow marks the end of muscle contractions. Ambulatory venous hypertension was caused by venous reflux, not by calf pump failure.
Thus, it must be discriminated between hydrostatic and ambulatory venous hypertension: hydrostatic hypertension is caused by gravitation force, whereas ambulatory hypertension is caused by venous reflux. The situation is schematically illustrated in Fig. 7. The starting level corresponds to hydrostatic venous hypertension. In a case with saphenous reflux, the pressure drops to the level of ambulatory venous hypertension. Abolition of saphenous reflux entails pressure drop right up to the level of physiological decrease in pressure; release of saphenous reflux retrieves pressure rise back to ambulatory venous hypertension. After cessation of calf pump activity, the pressure returns either quickly (under the influence of reflux) or slowly (without reflux) to the starting level.
Fig. 7.
Schematic illustration of the hydrostatic venous hypertension, ambulatory venous hypertension, and physiological decrease in pressure. For more details, see text. GSV, great saphenous vein.
Hence, ambulatory pressure gradient triggers venous reflux, and moreover it sets off biophysical and biochemical events inducing recurrent reflux after therapeutic elimination of saphenous reflux, as discussed in sections “Tendency of Varicose Veins to Recur” and “The Hemodynamic Paradox.”
The Role of Incompetent Lower Leg Perforating Veins
The hemodynamic significance of calf perforating veins continues to be the point of controversy. The conception that incompetent calf perforating veins cause hemodynamic disturbance and that they are responsible for the formation of leg ulcerations is still widely accepted. However, there are some evidences that rebut this opinion. Pressure measurement in the PTV and GSV in varicose vein patients with severe chronic venous insufficiency and large incompetent lower leg perforators showed that there was a physiological decrease in pressure in both the PTV and the GSV during calf pump activity, once the saphenous reflux was abolished by digital compression.2 8 9 10 14
Furthermore, direct pressure measurement in incompetent lower leg perforator found out a physiological decrease in pressure after saphenous reflux was abolished by digital compression,2 which is exactly the contrary of what the theory of incompetent perforators asserts. Flow recordings with electromagnetic flow meter in incompetent calf perforator revealed a bidirectional streaming, the vector of which was oriented inward not outward (again in contradiction to the theory of incompetent calf perforators). Saphenous reflux enhanced the inward-oriented component.2
Another proof was gained by plethysmographic measurements. Strain gauge plethysmography evaluating refill times t-90, t-50, and refill volume confirmed very grave forms of chronic venous insufficiency before surgery. Reestablishment of physiological hemodynamic conditions was achieved 1 week after pure crossectomy in the presence of large incompetent lower leg perforating veins15 (Fig. 8, I, II).
Fig. 8.
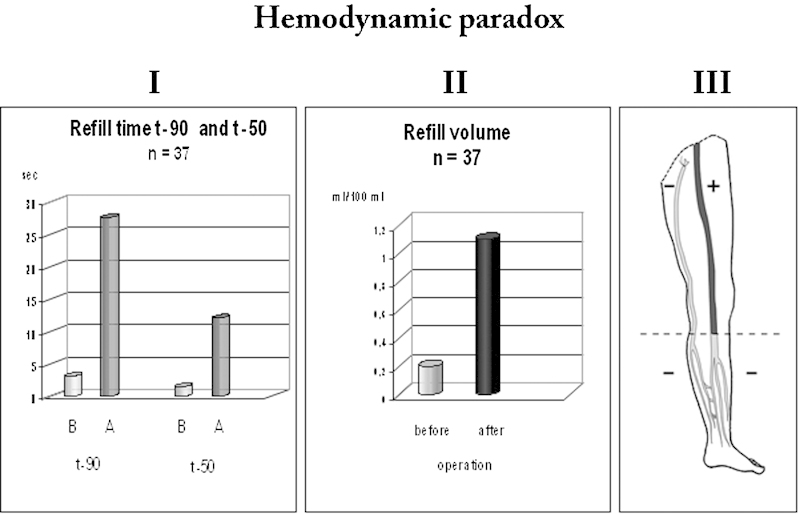
Hemodynamic paradox. Elimination of saphenous reflux in the groin restored physiological hemodynamic conditions (I, II), but at the same time it generated prerequisite for the comeback of previous pathological situation with recurrent reflux (III). Strain-gauge plethysmography evaluating refill time t-90, t-50, and refill volume in patients with very severe chronic venous insufficiency displayed the gravest form of hemodynamic disturbance before operation (B); reestablishment of physiological hemodynamic conditions was achieved in the presence of large incompetent calf perforators 1 week after pure crossectomy without any additional measure (A). However, abolition of saphenous reflux generated pressure difference between the femoral vein and the saphenous remnant, which set off biophysical and biochemical events evoking recurrent reflux. For more details, see text.
The mentioned evidences rebut the theory of incompetent perforating veins. Calf perforators enlarge with increasing saphenous reflux and diminish after saphenous reflux has been abolished by a therapeutic measure.16 17 Even if incompetent, they are not involved in the generation of hemodynamic disturbance. They do not cause ambulatory venous hypertension.
The conception that calf perforating veins in healthy persons were competent was formulated many years ago on the basis of freely contrived speculations, without any objective proof; nevertheless, that assertion has been widely accepted. Modern duplex ultrasonography cannot unambiguously resolve this issue: it is able to assess particular calf perforators, but not the system as a whole. On the other hand, simultaneous pressure recordings in deep and superficial veins of the lower leg are a more suitable assessment tool to evaluate this issue and to disclose the reality.
Pressure curves recorded from the PTV and GSV in healthy persons were quite similar, nearly identical, with steep increases in pressure during each calf muscle contraction both in deep and in superficial veins1 12; that is, a pressure pattern typical of conjoined vessels demonstrating unhindered pressure transmission and a persuasive proof excluding competency of the calf perforating system. Moreover, centripetal flow in the GSV, which can be recorded as a result of calf muscle contraction or manual calf squeezing, must come from deep lower leg veins via calf perforators. So, as long as no conclusive proof will be presented confirming complete competence of the calf perforating systems, we are not entitled to assert that calf perforating veins as a whole in healthy persons are competent and preclude evasion of venous blood from deep into superficial veins.
Simultaneous pressure recordings from the PTV and GSV in varicose vein patients yielded similar results8 10 14 (Figs. 2 and 3), and confirmed the conclusion that calf perforating veins enable quick pressure transmission and equalization together with bidirectional flow within them. Deep and superficial veins of the lower leg form conjoined vessels, as mentioned earlier.
Tendency of Varicose Veins to Recur
Recurrence after varicose vein surgery is a common event with a wide range depending on the length of follow-up, applied therapeutic procedure, and method used to diagnose recurrence. Apart from disease progression, inadequate surgery has been blamed to cause recurrences.18 19 20 Nevertheless, recurrences arose after correctly performed crossectomy and stripping as well.21 22 The groin region is the most common site where recurrent reflux occurs. Neovascularization, that is, formation of new venous channels after surgical closure of refluxing SFJ, was considered to be the most significant cause of recurrent varicose veins, and the surgical procedure itself has been blamed to trigger neovascularization.23 24 25 Attempts to prevent recurrences in the groin by inserting diverse sorts of barriers over the ligated SFJ were disappointing26 27 28 29; mechanical barriers either moderately reduced reflux recurrence rate in the groin in some studies or were ineffective in others, but in all they did not preclude development of recurrent reflux. Some authors expressed the opinion that recurrent reflux in varicose vein disease was unavoidable, no matter how careful and painstaking the primary procedure might be,28 30 and postulated that some unspecified hemodynamic factors might be responsible for recurrences.31 32
The Hemodynamic Paradox
A recent article dealt with that issue.33 In short, abolition of saphenous reflux is able to remove the gravest hemodynamic disturbance and to reestablish physiological pressure values, but simultaneously it creates preconditions for recurrent reflux and for the comeback of the previous pathological situation. During calf pump activity, venous blood is drained from the incompetent remnant of the GSV into the deep lower leg veins, which results in pressure decrease in this vein. Thus, once saphenous reflux has been abolished, pressure difference of 37.4 ± 6.4 mm Hg is generated during calf pump activity between the femoral vein and the GSV remnant in the thigh, which stimulates reappearance of reflux (Fig. 8, III). The pressure difference enhances flow rate through preexisting minor communicating channels, which increases fluid shear stress on the endothelium and sets off release of vasodilating agents34 35 36 37 38; the result is a progressive dilatation of preformed tiny communicating channels between the femoral vein and the incompetent GSV remnant, and ultimately recurrent reflux.
Ambulatory pressure gradient arising in healthy persons between thigh and lower leg veins is transmitted in varicose vein disease into the thigh; the boundary lies now between the femoral vein and incompetent superficial veins of the thigh.
Pressure difference between the femoral vein and superficial veins in the thigh does not appear in healthy persons where competent valves preclude drainage of venous blood from the thigh into the lower leg. Hence, no pressure difference develops between the femoral vein and competent superficial veins in the thigh in healthy persons; no impulse for the development of centrifugal flow emerges. Neovascularization does not take place after harvesting GSV for bypass graft. Surgery itself does not trigger the development of recurrent reflux in varicose vein disease.
The propensity to restore centrifugal flow in incompetent veins is the consequence of the process induced by pressure difference between two vascular segments. That biological process is salutary in arterial system: it induces creation of collateral circulation in arterial occlusions.34 35 36 Unfortunately, in varicose vein disease, it causes harm: because the flow direction in incompetent GSV is predominantly centrifugal, the tendency to restore reflux is the logical outcome once an obstacle to centrifugal flow has been created by the therapeutic measure abolishing reflux. Thus, the process can be considered as a derailment of the natural recovery abilities.
The same mechanism is obviously active in veins with centripetal flow, too. Thrombosis of the venous outflow tract also evokes pressure gradient, which might trigger the same biophysical and biochemical events generating venous collateral circulation with restored centripetal flow.
Conclusion
Ambulatory pressure gradient arises between thigh and lower leg veins during calf pump activity and triggers venous reflux in varicose vein disease. Venous reflux causes ambulatory venous hypertension in the lower leg and foot, the severity of which depends on the intensity of centrifugal flow expressed in mL/s. Bidirectional flow within calf perforators equalizes pressure differences between superficial and deep veins of the lower leg and makes them conjoined vessels. Incompetent lower leg perforating veins are not involved in the generation of hemodynamic disturbances, and they do not cause ambulatory venous hypertension. Pressure difference occurring between the femoral vein and the saphenous remnant after interruption of saphenous reflux triggers biophysical and biochemical events that lead to recurrent reflux. The propensity to restore centrifugal flow improves impaired arterial circulation in arterial occlusions, but causes harm in incompetent veins, evoking recurrent reflux. The effect of the mentioned hemodynamic factors may explain the tenacious tendency of varicose vein disease to recur.
There is a curious chain of events in varicose vein disease, the hemodynamic paradox: therapeutic procedure that removes saphenous reflux, the most important pathological factor causing hemodynamic disturbance in varicose vein disease, simultaneously generates hemodynamic preconditions for recurrent reflux and for progressive comeback of the previous pathological situation. From this point of view, abolition of saphenous reflux should be considered as a very important, nevertheless just a palliative, therapeutic measure, because the propensity for reflux recurrence progressively attenuates and ultimately thwarts the excellent immediate therapeutic result (Fig. 9). Hypothetically, only a therapeutic procedure that would be able to completely preclude drainage of blood from superficial thigh veins into the lower leg, that means which would reinstall conditions distinctive of healthy persons, would be able to heal varicose vein disease.
Fig. 9.
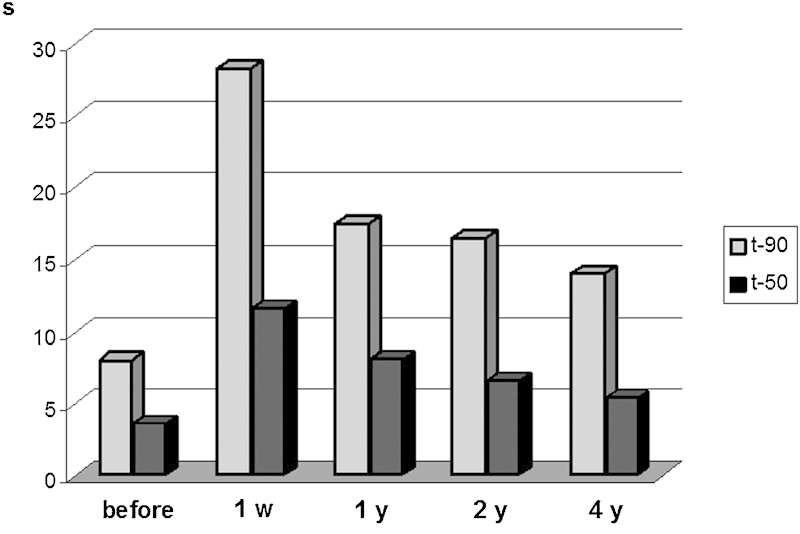
Progressive deterioration of the hemodynamic situation after crossectomy caused by recurrent reflux, evaluated by strain gauge plethysmographic parameters refill time t-90 and t-50 during 4 years follow-up. 1 w, 1 week after crossectomy, y, year(s).
References
- 1.Arnoldi C C. Venous pressure in the legs of healthy human subjects at rest and during muscular exercise in nearly erect position. Acta Chir Scand. 1965;130:530–583. [PubMed] [Google Scholar]
- 2.Bjordal R. Simultaneous pressure and flow recordings in varicose veins of the lower extremity. A haemodynamic study of venous dysfunction. Acta Chir Scand. 1970;136(4):309–317. [PubMed] [Google Scholar]
- 3.Trendelenburg F. Ligation of the great saphenous vein in lower leg varicose veins [in German] Beitr Klin Chir. 1891;7:195–210. [Google Scholar]
- 4.Ludbrook J, Beale G. Femoral venous valves in relation to varicose veins. Lancet. 1962;1(7220):79–81. doi: 10.1016/s0140-6736(62)91724-5. [DOI] [PubMed] [Google Scholar]
- 5.Hauser H Brunner U New pathophysiological and functional aspects concerning incompetence of small saphenous vein [in German] Vasa 199322338–341.8310773 [Google Scholar]
- 6.Recek C, Hammerschlag A. Incompetence of the femoral vein and small saphenous vein: Is there any a causal relationship? [in German] Phlebologie. 1997;26:115–119. [Google Scholar]
- 7.Jeanneret C, Labs K H, Aschwanden M, Bollinger A, Hoffmann U, Jäger K. Physiological reflux and venous diameter change in the proximal lower limb veins during a standardised Valsalva manoeuvre. Eur J Vasc Endovasc Surg. 1999;17(5):398–403. doi: 10.1053/ejvs.1998.0797. [DOI] [PubMed] [Google Scholar]
- 8.Arnoldi C C. Venous pressure in patients with valvular incompetence of the veins of the lower limb. Acta Chir Scand. 1966;132:628–645. [Google Scholar]
- 9.Recek C, Koudelka V. Effet circulatoire du reflux saphénien dans la varicose essentielle. Phlebologie. 1979;32(4):407–414. [PubMed] [Google Scholar]
- 10.Recek C, Koudelka V. Perforating veins of the leg and their role in the pathogenesis of varicose veins. Rozhl Chir. 1973;52(1):14–20. [PubMed] [Google Scholar]
- 11.Sarin S, Scurr J H, Smith P D. Medial calf perforators in venous disease: the significance of outward flow. J Vasc Surg. 1992;16(1):40–46. [PubMed] [Google Scholar]
- 12.Höjensgard I C, Stürup H. Static and dynamic pressures in superficial and deep veins of the lower extremity in man. Acta Physiol Scand. 1952;27(1):49–67. doi: 10.1111/j.1748-1716.1953.tb00923.x. [DOI] [PubMed] [Google Scholar]
- 13.Recek C, Pojer H. Ambulatory pressure gradient in the veins of the lower extremity. Vasa. 2000;29(3):187–190. doi: 10.1024/0301-1526.29.3.187. [DOI] [PubMed] [Google Scholar]
- 14.Recek C. A critical appraisal of the role of ankle perforators for the genesis of venous ulcers in the lower leg. J Cardiovasc Surg (Torino) 1971;12(1):45–49. [PubMed] [Google Scholar]
- 15.Recek C. Saphenous reflux as a cause of severe hemodynamic disturbance in chronic venous insufficiency [in German] Acta Chir Austriaca. 1998;30:76–77. [Google Scholar]
- 16.Recek C, Karisch E, Gruber J. Diameter changes in calf perforators and deep veins of the lower leg after abolition of the saphenous reflux [in German] Phlebologie. 2000;29:37–40. [Google Scholar]
- 17.Gohel M S, Barwell J R, Wakely C. et al. The influence of superficial venous surgery and compression on incompetent calf perforators in chronic venous leg ulceration. Eur J Vasc Endovasc Surg. 2005;29(1):78–82. doi: 10.1016/j.ejvs.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 18.Geier B, Stücker M, Hummel T. et al. Residual stumps associated with inguinal varicose vein recurrences: a multicenter study. Eur J Vasc Endovasc Surg. 2008;36(2):207–210. doi: 10.1016/j.ejvs.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 19.Dwerryhouse S, Davies B, Harradine K, Earnshaw J J. Stripping the long saphenous vein reduces the rate of reoperation for recurrent varicose veins: five-year results of a randomized trial. J Vasc Surg. 1999;29(4):589–592. doi: 10.1016/s0741-5214(99)70302-2. [DOI] [PubMed] [Google Scholar]
- 20.Joshi D, Sinclair A, Tsui J, Sarin S. Incomplete removal of great saphenous vein is the most common cause for recurrent varicose veins. Angiology. 2011;62(2):198–201. doi: 10.1177/0003319710375090. [DOI] [PubMed] [Google Scholar]
- 21.Fischer R, Linde N, Duff C, Jeanneret C, Chandler J G, Seeber P. Late recurrent saphenofemoral junction reflux after ligation and stripping of the greater saphenous vein. J Vasc Surg. 2001;34(2):236–240. doi: 10.1067/mva.2001.115802. [DOI] [PubMed] [Google Scholar]
- 22.Allegra C, Antignani P L, Carlizza A. Recurrent varicose veins following surgical treatment: our experience with five years follow-up. Eur J Vasc Endovasc Surg. 2007;33(6):751–756. doi: 10.1016/j.ejvs.2006.12.020. [DOI] [PubMed] [Google Scholar]
- 23.Glass G M. Neovascularization in recurrence of varices of the great saphenous vein in the groin: phlebography. Angiology. 1988;39(7, Pt 1):577–582. doi: 10.1177/000331978803900704. [DOI] [PubMed] [Google Scholar]
- 24.Jones L, Braithwaite B D, Selwyn D, Cooke S, Earnshaw J J. Neovascularisation is the principal cause of varicose vein recurrence: results of a randomised trial of stripping the long saphenous vein. Eur J Vasc Endovasc Surg. 1996;12(4):442–445. doi: 10.1016/s1078-5884(96)80011-6. [DOI] [PubMed] [Google Scholar]
- 25.Nyamekye I, Shephard N A, Davies B, Heather B P, Earnshaw J J. Clinicopathological evidence that neovascularisation is a cause of recurrent varicose veins. Eur J Vasc Endovasc Surg. 1998;15(5):412–415. doi: 10.1016/s1078-5884(98)80202-5. [DOI] [PubMed] [Google Scholar]
- 26.Winterborn R J, Earnshaw J J. Randomised trial of polytetrafluoroethylene patch insertion for recurrent great saphenous varicose veins. Eur J Vasc Endovasc Surg. 2007;34(3):367–373. doi: 10.1016/j.ejvs.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 27.Bhatti T S, Whitman B, Harradine K, Cooke S G, Heather B P, Earnshaw J J. Causes of re-recurrence after polytetrafluoroethylene patch saphenoplasty for recurrent varicose veins. Br J Surg. 2000;87(10):1356–1360. doi: 10.1046/j.1365-2168.2000.01602.x. [DOI] [PubMed] [Google Scholar]
- 28.Earnshaw J J, Davies B, Harradine K, Heather B P. Preliminary results of PTFE patch saphenoplasty to prevent neovascularization leading to recurrent varicose veins. Phlebology. 1998;13:10–13. [Google Scholar]
- 29.Gibbs P J, Foy D M, Darke S G. Reoperation for recurrent saphenofemoral incompetence: a prospective randomised trial using a reflected flap of pectineus fascia. Eur J Vasc Endovasc Surg. 1999;18(6):494–498. doi: 10.1053/ejvs.1999.0906. [DOI] [PubMed] [Google Scholar]
- 30.Frings N, Nelle A, Tran V TP. et al. Unavoidable recurrence and neoreflux after correctly performed ligation of the saphenofemoral junction: neovascularization? [in German] Phlebologie. 2003;32:96–100. [Google Scholar]
- 31.Turton E P, Scott D J, Richards S P. et al. Duplex-derived evidence of reflux after varicose vein surgery: neoreflux or neovascularisation? Eur J Vasc Endovasc Surg. 1999;17(3):230–233. doi: 10.1053/ejvs.1998.0719. [DOI] [PubMed] [Google Scholar]
- 32.El Wajeh Y, Giannoukas A D, Gulliford C J, Suvarna S K, Chan P. Saphenofemoral venous channels associated with recurrent varicose veins are not neovascular. Eur J Vasc Endovasc Surg. 2004;28(6):590–594. doi: 10.1016/j.ejvs.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 33.Recek C. The hemodynamic paradox as a phenomenon triggering recurrent reflux in varicose vein disease. Int J Angiol. 2012;21(3):181–185. doi: 10.1055/s-0032-1325168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schaper W. Collateral circulation: past and present. Basic Res Cardiol. 2009;104(1):5–21. doi: 10.1007/s00395-008-0760-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pipp F, Boehm S, Cai W J. et al. Elevated fluid shear stress enhances postocclusive collateral artery growth and gene expression in the pig hind limb. Arterioscler Thromb Vasc Biol. 2004;24(9):1664–1668. doi: 10.1161/01.ATV.0000138028.14390.e4. [DOI] [PubMed] [Google Scholar]
- 36.Schaper W, Scholz D. Factors regulating arteriogenesis. Arterioscler Thromb Vasc Biol. 2003;23(7):1143–1151. doi: 10.1161/01.ATV.0000069625.11230.96. [DOI] [PubMed] [Google Scholar]
- 37.Resnick N, Gimbrone M A Jr. Hemodynamic forces are complex regulators of endothelial gene expression. FASEB J. 1995;9(10):874–882. doi: 10.1096/fasebj.9.10.7615157. [DOI] [PubMed] [Google Scholar]
- 38.Schierling W, Troidl K, Troidl C, Schmitz-Rixen T, Schaper W, Eitenmüller I K. The role of angiogenic growth factors in arteriogenesis. J Vasc Res. 2009;46(4):365–374. doi: 10.1159/000189797. [DOI] [PubMed] [Google Scholar]


