Abstract
Introduction Scapholunate ligament injuries usually result due to a fall on the outstretched hand leading to scapholunate instability. The natural history of untreated scapholunate instability remains controversial and usually results in late arthritic changes- the so-called “SLAC” wrist. The advent of wrist arthroscopy helps in early diagnosis and treatment of these serious injuries. In selected cases with reducible scapholunate instability (Garcia-Elias stages 2, 3 and 4) we propose a new “all arthroscopic dorsal capsulo- ligamentous repair” with the added advantage of early rehabilitation and prevention of post-operative stiffness.
Material and Methods We report the results of our series of 57 consecutive patients suffering from chronic wrist pain refractory to conservative measures. All patients underwent a thorough clinical examination in addition to a standard set of radiographs and MRI exam; and they were treated by an all-arthroscopic dorsal capsulo-ligamentous repair under loco-regional anesthesia on an ambulatory basis. All patients were available for follow-up at regular intervals during the post-operative period. At follow-up, the wrist ROM in all directions, the grip strength, DASH questionnaire and pain relief based on the VAS were recorded for both- the operated and contra-lateral sides.
Results There were 34 males & 23 females with a mean age of 38.72 ± 11.33 years (range 17–63 years). The dominant side was involved in 52 cases. The mean time since injury was 9.42 ± 6.33 months (range 3–24 months) and the mean follow-up was 30.74 ± 7.05 months (range 18–43 months). The mean range of motion improved in all directions. The mean difference between the post- and pre-operative extension was 14.03° (SEM = 1.27°; p < 0.001); while the mean difference between the post-and pre-operative flexion was 11.14° (SEM = 1.3°; p < 0.0001) with flexion and radial deviation reaching 84.3% and 95.72% respectively of the unaffected wrist. The mean difference for the VAS score was -5.46 (SEM = 0.19; p < 0.0001). The mean post-operative grip strength of the affected side was 38.42 ± 10.27 kg (range 20–60 kg) as compared with mean pre-operative grip strength of 24.07 ± 10.51 kg (range 8–40 kg) (p < 0.0001). The mean post-operative grip strength of the operated side was 93.4% of the unaffected side. The DISI was corrected in all cases on post-operative radiographs. The mean difference between the post-and pre-operative SL angles was −8.95° (SEM = 1.28°; p < 0.0001). The mean post-operative DASH score was 8.3 ± 7.82 as compared with mean pre-operative DASH score of 46.04 ± 16.57 (p < 0.0001). There was a negative co-relation between the overall DASH score and the post-operative correction of the DISI deformity with a lower DASH score associated with increasing SL angles.
Discussion The dorsal portion of the scapholunate ligament is critical for the stability scapholunate articulation, largely due to its attachment to the dorsal capsule. We have recently conducted a multi-centric anatomical study with international collaboration demonstrating the critical importance of this dorsal scapholunate complex. The all arthroscopic capsulo-ligamentous repair technique provides reliable results in addition to avoiding postoperative stiffness. The overall results at a mean follow-up period of more than 2 years in our series of young, active patients appear to be encouraging.
Keywords: scapholunate ligament, chronic scapholunate injury, dorsal capsuloplasty, wrist arthroscopy
Scapholunate ligament injuries usually result from a fall on the outstretched hand. The natural history of untreated scapholunate instability remains controversial and usually results in late arthritic changes- which progress to a scapholunate advanced collapse (SLAC) wrist. Arthroscopy is a valuable tool for the diagnosis and treatment of acute scapholunate dissociation. In chronic lesions, treatment options are more controversial than in the acute cases.
Most forms of treatment recommended in the literature consist of an open repair or alternative reconstruction techniques which can improve pain and grip strength, but very often lead to stiffness in the wrist joint.1 We have therefore developed an all arthroscopic dorsal capsulo-ligamentous repair technique to avoid an open dissection of the wrist capsule.2
Material and Methods
57 consecutive patients with refractory chronic wrist pain due to a partial or complete but reducible scapholunate ligament tear were treated with an all arthroscopic dorsal capsulo- ligamentous repair. Pain and a positive Watson's test on clinical examination associated with radiological signs of scapholunate instability (increased SL interval on PA and increased SL angle on lateral views) were considered as indications for surgical intervention. There were 35 cases with sports-related injuries of which 10 patients were professional athletes. ROM on both sides was measured in all patients preoperatively. Tenderness on palpation in the affected wrist was noted and the Watson test was performed. Standard PA, lateral and oblique radiographs were performed on all patients. The scapholunate gap and the scapholunate angles were measured. All patients also had an MR-arthrogram. All patients were reviewed by the senior author at regular intervals. At final follow-up, patients were evaluated using the DASH outcome questionnaire by an independent reviewer. Wrist range of motion was recorded in flexion, extension and radial/ulnar deviation.
Grip strength was measured using the JAMAR dynamometer (Preston, Cambridge, MA, USA) and compared with the opposite side. Furthermore, patient satisfaction was assessed by asking the patients to grade their postoperative result as excellent, good, fair and poor.
Standard PA, lateral and oblique radiographs were obtained for all patients at 8 weeks after surgery, and then at regular intervals until the last follow-up. The scapholunate angle was determined by the operating surgeon and an independent examiner. An MRI was routinely performed at 6 months post-operatively.
Operative Technique
The procedures were performed on an outpatient basis under regional anesthesia and with an upper arm tourniquet. The elbow was flexed to 90°on an arm table and the hand was suspended by means of a hand holder with traction of 3 to 5 kg.
We used the standard arthroscopic 3–4 and 6R portals for the radio-carpal joint and MCR and MCU for the midcarpal joint. The joints were first insufflated with normal saline. A small transverse incision was made with a 15 number scalpel followed by blunt dissection with a mosquito forceps. The 2.4 mm arthroscope was introduced through the 3–4 portal and the instruments through the 6R portal-these two portals are interchangeable according to need. The midcarpal joint was explored through the MCU portal. Exploration and palpation of the structures in the two joints confirms the lesion and provides the staging.
We graded the degree of the scapholunate instability using the Geissler classification3 (Table 1); and the Classification of Garcia-Elias et al4 (Table 2)
Table 1. Arthroscopic Geissler's classification.
| Geissler classification of cartilage lesions |
| Stage 1 Attenuation/hemorrhage SL in RCJ; no incongruency in MCJ |
| Stage 2 Attenuation/perforation of SL in RCJ; Small incongruency in MCJ |
| Stage 3 Perforation of SL in RCJ/Incongruency and step-off in MCJ (> probe) |
| Stage 4 Incongruency and step-offin RCJ and MCJ: Gross instability with manipulation |
Table 2. Garcia-Elias staging system.
| Stages | I | II | III | IV | V | VI |
|---|---|---|---|---|---|---|
| Dorsal SLL intact? | Yes | No | No | No | No | No |
| Repairable SLL? | Yes | Yes | No | No | No | No |
| Scaphoid alignment normal? | Yes | Yes | Yes | Yes | No | No |
| Carpal malignment reducible? | Yes | Yes | Yes | Yes | No | No |
| Cartilage in RC & MC joints normal? | Yes | Yes | Yes | Yes | Yes | No |
Only Garcia-Elias stages 2, 3 and 4 were treated with this technique. The carpal alignment was noted as either being preserved (stage 2 and 3) or amenable to correction if mal-alignment was seen (stage 4). Usually, the scapholunate ligament is detached from the scaphoid and remains attached to the lunate, but on the dorsal distal aspect, close to the normal insertion of the scapholunate ligament to the capsule, there are remnants of the scapholunate ligament on both- the dorsal horn of the lunate and the scaphoid. It is difficult to visualize the dorsal scapholunate ligament from a 6R portal because, when the wrist is in traction, the dorsal capsule is apposed to the ruptured ligament but releasing the traction allows visualization of the torn ligament. An 18 gauge needle is inserted under direct vision through the 3–4 radiocarpal portal into the radio-carpal joint. Care is taken not to directly enter the open part of the capsule. The needle is inserted through the dorsal capsule up to 1 mm from the capsular hole and then the needle is directed through the radial remnant of the S-L ligament obliquely from dorsal to palmar and proximal to distal, until the tip of the needle is seen in the midcarpal joint. The scope is then switched to the MCU portal and a 3.0 PDS suture is passed through the needle and pulled out through the MCR portal with a hemostat under direct vision from the MCU portal (Fig. 1). A second suture is then passed parallel to the first one in the lunate/ulnar remnant of SL-ligament and brought out through the same portal (Fig. 2). A knot is tied between the two sutures. Following this, distal to proximal traction is applied to the both proximal ends of the sutures to place the first knot into the mid-carpal joint between the scaphoid and the lunate, volar to the dorsal part of SL ligament (Fig. 3). A second knot is tied between the two proximal ends and introduced in the 3–4 portal incision, dorsal to the capsule. This knot lies outside the wrist joint on the dorsal capsule. The net effect of this achieves a capsulo- ligamentous repair between the scapholunate ligament and the dorsal capsule overlying the ligament (Fig. 4). However, it must be borne in mind that if the scapholunate ligament has been completely avulsed off the bone instead of being torn and if there are no remnants, this procedure cannot be performed. The procedure for stage 4 cases is slightly different from that described above. In such instances, the scaphoid must be reduced and stabilized with both- the lunate and capitate. This is done by external and internal maneuvers under fluoroscopic control. Once the reduction is confirmed then the capsulo-ligamentous repair can be performed. The scaphoid is stabilized with 1.2 mm parallel K-wires passed through the scaphoid into the capitate. The final dorsal knot is performed after SL stabilization and fixation with K-wires (Fig. 5). The radiocarpal and midcarpal joints are thoroughly lavaged before instrument retrieval. The portal incisions are not sutured. A bulky dressing and a simple volar splint is applied upon completion of the surgery.
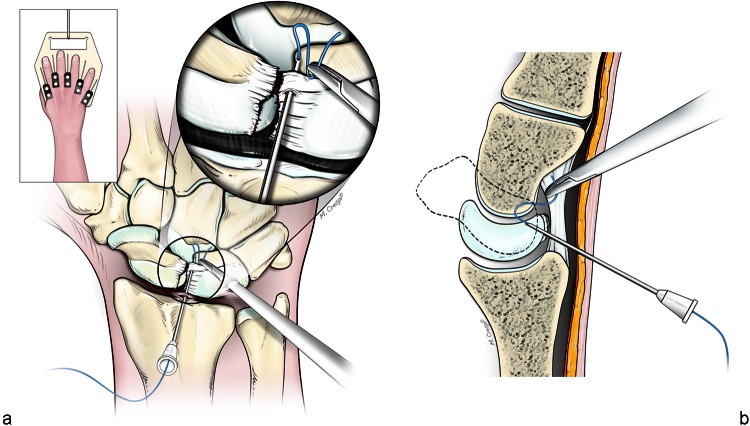
Fig. 1.
(a) Schema representing the passage of the first suture through the dorsal capsule, (b) then a remaining dorsal remnant of the scapholunate ligament attached to the dorsal horn of lunate. The passage is made from the radiocarpal to the midcarpal joint.
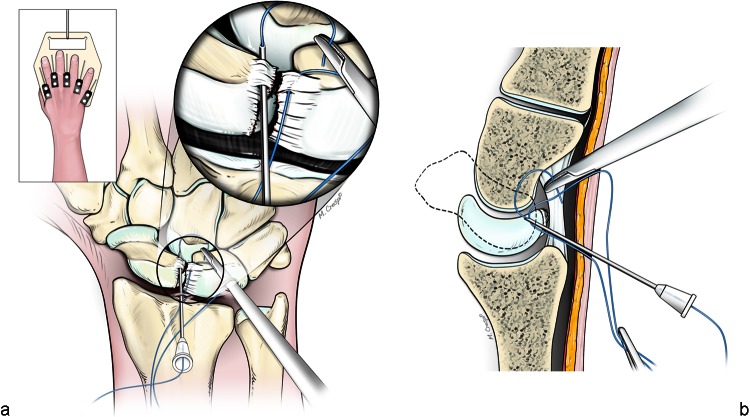
Fig. 2.
(a) Schema representing the passage of the second suture through the dorsal capsule, (b) then a remaining dorsal remnant of the scapholunate ligament attached to the dorsal scaphoid. The passage is made from the radiocarpal to the midcarpal joint.
Fig. 3.
After the first knot has been tied between the two sutures; a distal to proximal traction is applied to the both proximal ends of the sutures to place the first knot into the mid-carpal joint between the scaphoid and the lunate, volar to the dorsal part of SL ligament.
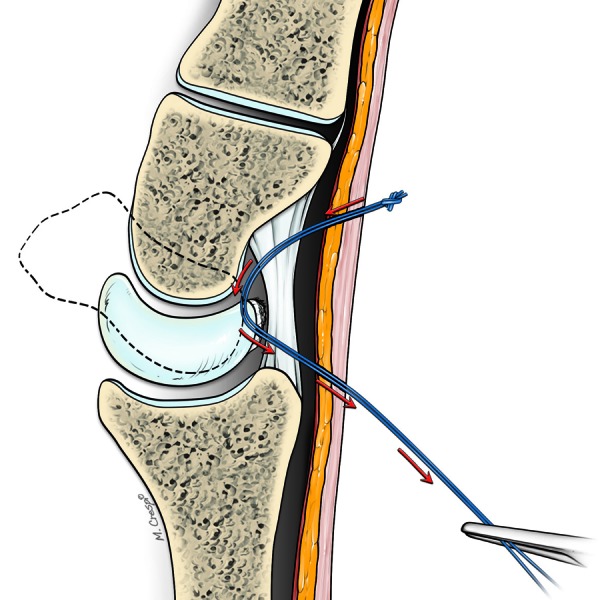
Fig. 4.
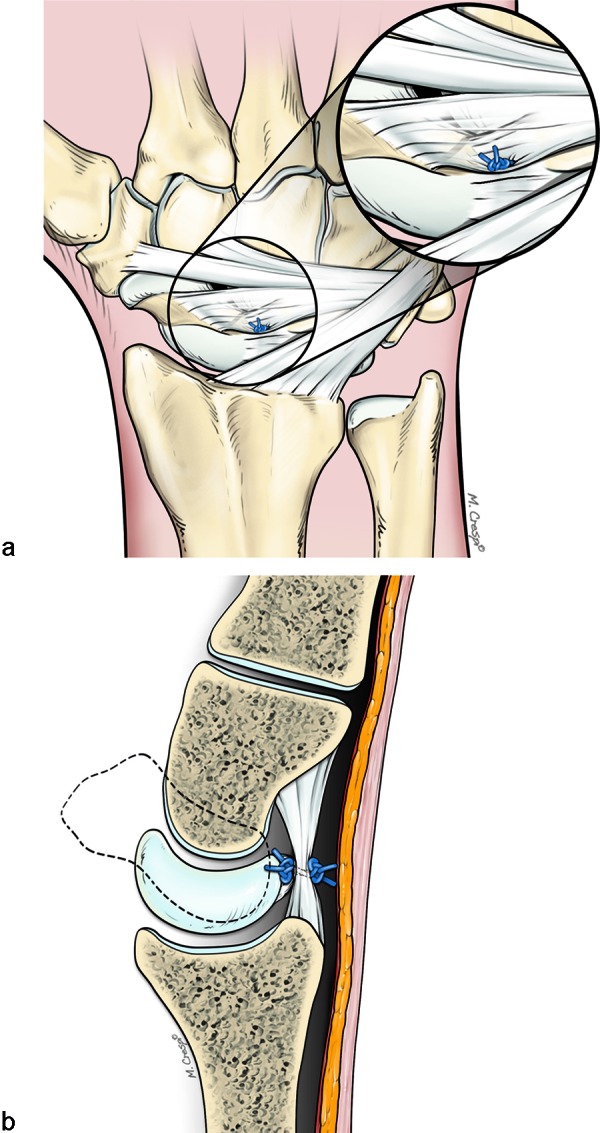
(a) Schema representing the second knot tied between the two proximal ends and introduced in the 3–4 portal incision, dorsal to the capsule. (b) This knot lies outside the wrist joint on the dorsal capsule. The net effect of this achieves a capsuloplasty between the scapholunate ligament and the dorsal capsule overlying the ligament.
Fig. 5.
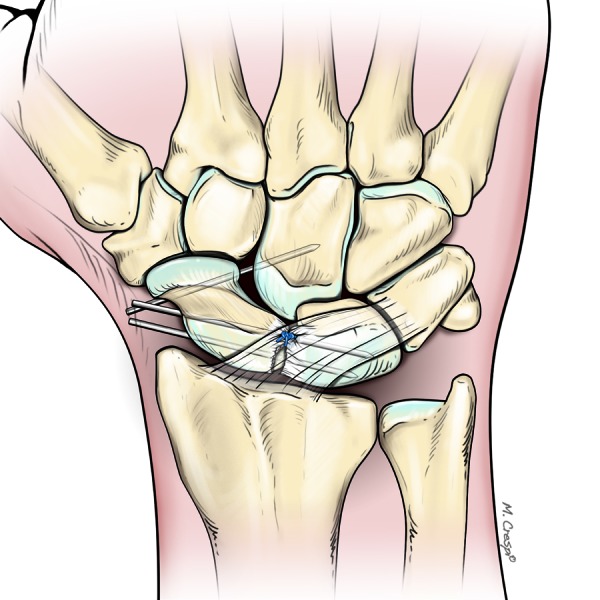
Schema representing the stabilization of the scaphoid by1.2 mm parallel K-wires passed through the scaphoid into the capitate (Garcia-Elias' stage 4 cases only). The final dorsal knot is performed after SL fixation.
Postoperative Protocol
The wrist is immobilized in a splint for two months. After eight weeks passive wrist motion is commenced under the supervision of a physiotherapist. K-wires, when used (i.e., in stage 4), are removed after two months and the patients undergo the same physiotherapy protocol (Fig. 6).
Fig. 6.
(a) Clinical case of scapholunate dissociation 9 months after injury- (Garcia-Elias Stage 4). (b-c) X-Rays showing the correct reduction and stabilization of scapholunate space after arthroscopic dorsal capsuloplasty. (d-e) 12 months of follow-up, recovery of excellent range of motion in both extension and flexion. (f-g) MRI after 12 months showing the correct reduction of lunate, and the reality of the dorsal capsuloplasty with a thickening of the capsule compared with the horn of the lunate and even a tightening of this capsule toward the lunate.
Statistical Analysis
Data analysis was performed bivariate analysis and fit and t-test for matched pairs. Results were considered significant for p < 0.05.
Results
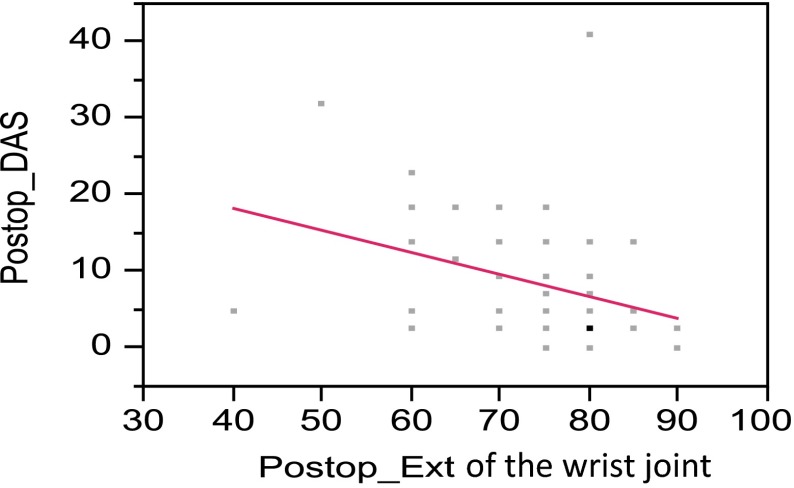
There were 34 males and 23 females with a mean age of 38.7 ± 11.3 years (range 17–63 years). The dominant side was involved in 52 cases. The mean time from the injury was 9.4 ± 6.3 months (range 3–24 months) and the mean follow-up was 30.7 ± 7 months (range 18–43 months). The mean range of motion improved in all directions. The mean difference between the post- and pre-operative extension was 14. ° (Standard Error of Mean-SEM = 1.27°; p < 0.001); while the mean difference between the post-and pre-operative flexion was 11° (SEM = 1.3°; p < 0.0001) with flexion and radial deviation reaching 84.3% and 95.72% respectively of the unaffected wrist. The mean difference for the VAS score was -5.46 (SEM = 0.19; p < 0.0001). The mean post-operative grip strength of the affected side was 38.4 ± 10.2 kg (range 20–60 kg) as compared with mean pre-operative grip strength of 24.1 ± 10.5 kg (range 8–40 kg) (p < 0.0001). The mean post-operative grip strength of the operated side was 93.4% of the unaffected side. The DISI was corrected in all cases on post-operative radiographs (a SL angle greater than 60° on the lateral view was considered as a DISI).(Table 3). The mean difference between the post-and pre-operative SL angles was −8.9° (SEM = 1.28°; p < 0.0001). The mean post-operative DASH score was 8.3 ± 7.8 as compared with mean pre-operative DASH score of 46. ± 16.6 (p < 0.0001). There was a negative correlation between the overall DASH score and the post-operative correction of the DISI deformity with a lower DASH score associated with increasing SL angles (Fig. 7).
Table 3. Pre- and post-operative Scapho-lunate (SL) angles on the lateral X-ray (a SL angle greater than 60° on the lateral view was considered as a DISI pattern-marked with an asterisk).
| Patient number | Pre-op SL angle in degrees | Post-op SL angle in degrees |
|---|---|---|
| 1 | 65* | 50 |
| 2 | 50 | 45 |
| 3 | 55 | 45 |
| 4 | 70* | 50 |
| 5 | 70* | 55 |
| 6 | 45 | 45 |
| 7 | 65* | 55 |
| 8 | 40 | 45 |
| 9 | 45 | 45 |
| 10 | 70* | 50 |
| 11 | 65* | 55 |
| 12 | 50 | 45 |
| 13 | 45 | 45 |
| 14 | 65* | 50 |
| 15 | 65* | 60 |
| 16 | 60 | 55 |
| 17 | 50 | 50 |
| 18 | 90* | 55 |
| 19 | 45 | 45 |
| 20 | 50 | 50 |
| 21 | 45 | 45 |
| 22 | 40 | 40 |
| 23 | 50 | 45 |
| 24 | 50 | 45 |
| 25 | 70* | 65* |
| 26 | 65* | 55 |
| 27 | 45 | 45 |
| 28 | 50 | 50 |
| 29 | 60 | 45 |
| 30 | 65* | 50 |
| 31 | 55 | 50 |
| 32 | 50 | 45 |
| 33 | 60 | 45 |
| 34 | 75* | 70* |
| 35 | 45 | 45 |
| 36 | 50 | 50 |
| 37 | 50 | 45 |
| 38 | 75* | 50 |
| 39 | 75* | 50 |
| 40 | 70* | 50 |
| 41 | 85* | 50 |
| 42 | 55 | 45 |
| 43 | 90* | 55 |
| 44 | 50 | 50 |
| 45 | 70* | 50 |
| 46 | 55 | 50 |
| 47 | 55 | 50 |
| 48 | 70* | 50 |
| 49 | 90* | 80* |
| 50 | 65* | 50 |
| 51 | 55 | 45 |
| 52 | 45 | 45 |
| 53 | 50 | 50 |
| 54 | 50 | 45 |
| 55 | 45 | 45 |
| 56 | 50 | 50 |
| 57 | 65* | 50 |
Fig. 7.
Regression Plot for Postoperative DASH and Postoperative Wrist extension. The post-operative wrist extension in degrees is plotted on the X-axis against the DASH score on the Y-axis.
Using Garcia-Elias's staging system three patients were classified as Stage 2, 25 patients as Stage 3 and 29 patients as Stage 4. Twenty patients required temporary K-wire fixation. 9 patients with Stage 4 did not require SL pinning as adequate and stable reduction of the SL was achieved per-operatively & as determined by intra-operative fluoroscopy. 16 patients had associated TFCC lesions which were treated arthroscopically in the same operative session with a TFCC repair. There was no change in the post-operative protocol for any of these patients. All the patients returned to work in an average period of 9 weeks (range, 1 to 12 weeks) and the all professional level athletes continued their sporting activities at the same level as prior to the injury. 56 patients (98.2%) were very satisfied or satisfied with their result. 1 patient had a fair result and was unsatisfied, mainly due to post-operative wrist stiffness.
Radiographic Results
The mean difference in the means of the preoperative and postoperative SL angle was −8.95° (SEM = 1.28°, p < 0.0001). The DISI remained uncorrected in 11 patients (19%) postoperatively. All post-operative MRI studies demonstrated a reduction in the T2 weighted signal indicating healing.
Discussion
The dorsal portion of the scapholunate ligament is critical for the stability scapholunate articulation, largely due to its attachment of the dorsal capsule. Dissociation of the scapholunate joint occurs after a rupture of the scapholunate ligament and at least one of its secondary capsular restraints.5 The natural history of untreated scapholunate dissociation results in SLAC wrist.6,7 Most procedures described in the literatures are aimed at stabilizing the scapholunate joint.1 The best outcomes of treatment in scapholunate dissociation are obtained with treatment in the acute phase or in the first two months after the lesion, especially with partial tears.3 Direct suture repair of the scapholunate ligament with dorsal capsular augmentation is the most commonly used technique for an acute complete scapholunate ligament tear.
The treatment of chronic SL ligament injuries is still controversial. Numerous techniques have been described such as a dorsal capsulodesis8,9, ligament reconstructions using tendon grafts, and inter-carpal arthrodesis techniques. Most of the techniques are effective for pain-relief but lead to significant wrist stiffness. We therefore developed a minimally invasive technique to stabilize the scapholunate articulation, thus preserving maximum wrist movement.
In a survey article by Zarkadas10 on surgical management of scapholunate instability by 468 hand surgeons of the American and Canadian associations with different soft tissue and/or bone tissue reconstructions, 99% expected a post-operative limitation of wrist motion. 66% expected a recovery of only 40 to 60% of normal wrist motion. Only 1% of the respondents expected a 81 to 100% recovery. Grip strength of over 75% of the normal value was expected by only 18% of the surgeons in patients with chronic lesions. Furthermore 84% considered that patients will end up with occasional pain on moderate use of the injured wrist. Deshmukh et al.11 published a prospective study on 44 cases of SL dissociations treated by Blatt's capsulodesis. Wrist extension was restricted from 60° to 38° (36.7% loss) compared with the unaffected side, flexion reduced from 71° to 40° (43.7%), radial deviation from 17° to 4° (76.5%) and ulnar deviation from 16° to 13° (50%). Post-operative grip strength reached only 75.1% of the unaffected side in their series. Pain relief measured by the Visual Analogue Scale (VAS) improved from 7.9 pre-operatively to 4.1 post-operatively, but only 21 patients (47.7%) had good or excellent pain relief, while 52.3% had only fair to poor relief. Moran et al12 compared a modified Brunelli technique to Berger capsulodesis. 30% loss of motion between the pre and post-operative values was noted in the tenodesis group and 27% loss in the capsulodesis group. Decrease of flexion-extension arc of motion was statistically significant in both groups. There was no difference in the grip strength between the two groups. Links13 compared the Brunelli technique with the four-bone-weave technique in 44 patients and showed better overall results than the four-bone-weave technique. Weiss14 noted loss of wrist motion, improved grip strength and good satisfaction in 14 patients with a bone-retinaculum-bone technique. All of these techniques result in significant wrist stiffness and eventually lead to arthritic changes. However, we observed better ROM and grip strength in our current series.
We conclude that our technique appears to be a reliable method to stabilize Stage 2, 3 and 4 scapholunate dissociations without the issue of wrist stiffness due to extensive open dissection techniques as reported in most of the studies.10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29 Further data in a larger cohort of patients with a longer follow-up is required to determine the effect on SLAC-wrist deterioration.
Footnotes
Conflict of interest None
References
- 1.Kalainov D M, Cohen M S. Treatment of traumatic scapholunate dissociation. J Hand Surg Am. 2009;34(7):1317–1319. doi: 10.1016/j.jhsa.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 2.Mathoulin Ch, Dauphin N. Sallen v. Capsulodèse arthroscopique dorsale dans les lésions chroniques du ligament scapho-lunaire. Chir. Main. 2009;28(6):398. [Google Scholar]
- 3.Geissler W B Haley T Arthroscopy management of scapholu- nate instability Atlas of Hand Clinics 6253–274., 2001 [Google Scholar]
- 4.Garcia-Elias M, Lluch A L, Stanley J K. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am. 2006;31(1):125–134. doi: 10.1016/j.jhsa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 5.Berger R A, Imeada T, Berglund L, An K N. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg Am. 1999;24(5):953–962. doi: 10.1053/jhsu.1999.0953. [DOI] [PubMed] [Google Scholar]
- 6.Watson H K, Ballet F L. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9(3):358–365. doi: 10.1016/s0363-5023(84)80223-3. [DOI] [PubMed] [Google Scholar]
- 7.Pilný J, Kubes J, Hoza P, Sprláková A, Hart R. [Consequennce of nontreatment scapholunate instability of the wrist] Rozhl Chir. 2006;85(12):637–640. [PubMed] [Google Scholar]
- 8.Blatt G. Capsulodesis in reconstructive hand surgery. Dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3(1):81–102. [PubMed] [Google Scholar]
- 9.Busse F, Felderhoff J, Krimmer H, Lanz U. [Scapholunate dissociation: treatment by dorsal capsulodesis] Handchir Mikrochir Plast Chir. 2002;34(3):173–181. doi: 10.1055/s-2002-33690. [DOI] [PubMed] [Google Scholar]
- 10.Zarkadas P C, Gropper P T, White N J, Perey B H. A survey of the surgical management of acute and chronic scapholunate instability. J Hand Surg Am. 2004;29(5):848–857. doi: 10.1016/j.jhsa.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Deshmukh S C, Givissis P, Belloso D, Stanley J K, Trail I A. Blatt's capsulodesis for chronic scapholunate dissociation. J Hand Surg [Br] 1999;24(2):215–220. doi: 10.1054/jhsb.1998.0183. [DOI] [PubMed] [Google Scholar]
- 12.Moran S L, Ford K S, Wulf C A, Cooney W P. Outcomes of dorsal capsulodesis and tenodesis for treatment of scapholunate instability. J Hand Surg Am. 2006;31(9):1438–1446. doi: 10.1016/j.jhsa.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Links A C, Chin S H, Waitayawinyu T, Trumble T E. Scapholunate interosseous ligament reconstruction: results with a modified Brunelli technique versus four-bone weave. J Hand Surg Am. 2008;33(6):850–856. doi: 10.1016/j.jhsa.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Weiss A P. Scapholunate ligament reconstruction using a bone-retinaculum-bone autograft. J Hand Surg Am. 1998;23(2):205–215. doi: 10.1016/S0363-5023(98)80115-9. [DOI] [PubMed] [Google Scholar]
- 15.Slater R R Jr, Szabo R M, Bay B K, Laubach J. Dorsal intercarpal ligament capsulodesis for scapholunate dissociation: biomechanical analysis in a cadaver model. J Hand Surg Am. 1999;24(2):232–239. doi: 10.1053/jhsu.1999.0232. [DOI] [PubMed] [Google Scholar]
- 16.Szabo R M, Slater R R Jr, Palumbo C F, Gerlach T. Dorsal intercarpal ligament capsulodesis for chronic, static scapholunate dissociation: clinical results. J Hand Surg Am. 2002;27(6):978–984. doi: 10.1053/jhsu.2002.36523. [DOI] [PubMed] [Google Scholar]
- 17.Wintman B I, Gelberman R H, Katz J N. Dynamic scapholunate instability: results of operative treatment with dorsal capsulodesis. J Hand Surg Am. 1995;20(6):971–979. doi: 10.1016/S0363-5023(05)80145-5. [DOI] [PubMed] [Google Scholar]
- 18.Gajendran V K, Peterson B, Slater R R Jr, Szabo R M. Long-term outcomes of dorsal intercarpal ligament capsulodesis for chronic scapholunate dissociation. J Hand Surg Am. 2007;32(9):1323–1333. doi: 10.1016/j.jhsa.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 19.Brunelli F, Spalvieri C, Bremner-Smith A, Papalia I, Pivato G. [Dynamic correction of static scapholunate instability using an active tendon transfer of extensor brevi carpi radialis: preliminary report] Chir Main. 2004;23(5):249–253. doi: 10.1016/j.main.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Chabas J F, Gay A, Valenti D, Guinard D, Legre R. Results of the modified Brunelli tenodesis for treatment of scapholunate instability: a retrospective study of 19 patients. J Hand Surg Am. 2008;33(9):1469–1477. doi: 10.1016/j.jhsa.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 21.Talwalkar S C, Edwards A T, Hayton M J, Stilwell J H, Trail I A, Stanley J K. Results of tri-ligament tenodesis: a modified Brunelli procedure in the management of scapholunate instability. J Hand Surg [Br] 2006;31(1):110–117. doi: 10.1016/j.jhsb.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 22.De Smet L, Van Hoonacker P. Treatment of chronic static scapholunate dissociation with the modified Brunelli technique: preliminary results. Acta Orthop Belg. 2007;73(2):188–191. [PubMed] [Google Scholar]
- 23.Harvey E J, Berger R A, Osterman A L, Fernandez D L, Weiss A P. Bone-tissue-bone repairs for scapholunate dissociation. J Hand Surg Am. 2007;32(2):256–264. doi: 10.1016/j.jhsa.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 24.Almquist E E, Bach A W, Sack J T, Fuhs S E, Newman D M. Four-bone ligament reconstruction for treatment of chronic complete scapholunate separation. J Hand Surg Am. 1991;16(2):322–327. doi: 10.1016/s0363-5023(10)80120-0. [DOI] [PubMed] [Google Scholar]
- 25.Bleuler P, Shafighi M, Donati O F, Gurunluoglu R, Constantinescu M A. Dynamic repair of scapholunate dissociation with dorsal extensor carpi radialis longus tenodesis. J Hand Surg Am. 2008;33(2):281–284. doi: 10.1016/j.jhsa.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 26.Ogunro O. Dynamic stabilization of chronic scapholunate dissociation with palmaris longus transfer: a new technique. Tech Hand Up Extrem Surg. 2007;11(4):241–245. doi: 10.1097/bth.0b013e3180a5e97d. [DOI] [PubMed] [Google Scholar]
- 27.Rosenwasser M P, Miyasajsa K C, Strauch R J. The RASL procedure: reduction and association of the scaphoid and lunate using the Herbert screw. Tech Hand Up Extrem Surg. 1997;1(4):263–272. [PubMed] [Google Scholar]
- 28.Siegel J M, Ruby L K. A critical look at intercarpal arthrodesis: review of the literature. J Hand Surg Am. 1996;21(4):717–723. doi: 10.1016/S0363-5023(96)80037-2. [DOI] [PubMed] [Google Scholar]
- 29.Pomerance J. Outcome after repair of the scapholunate interosseous ligament and dorsal capsulodesis for dynamic scapholunate instability due to trauma. J Hand Surg Am. 2006;31(8):1380–1386. doi: 10.1016/j.jhsa.2006.07.005. [DOI] [PubMed] [Google Scholar]