Abstract
Wrist arthroscopy plays a valuable role in the management of scapholunate instability. A spectrum of injuries can occur to the scapholunate interosseous ligament, which may be difficult to detect with imaging studies. Wrist arthroscopy enables detection and management of injury to the scapholunate ligament under bright light and magnified conditions, in both acute and chronic situations.
Keywords: wrist arthroscopy, carpal instability
The development of wrist arthroscopy is a natural evolution from the successful application to larger joints. The wrist continues to challenge clinicians with an array of potential diagnoses in management. Wrist arthroscopy allows direct visualization of the cartilage surfaces, synovial tissue, and particularly the interosseous ligaments under magnification and bright light. Wrist arthroscopy has been shown to be a useful adjunct in the management of both acute and chronic injuries to the scapholunate interosseous ligament.
The majority of acute sprains of the wrist with normal radiographic findings resolve after temporary immobilization. The method of choice to further evaluate the patient who does not improve continues to be controversial. Tricompartmental wrist arthrography has historically been the gold standard for the detection of interosseous ligament tears.1 Magnetic resonance imaging (MRI) has certainly improved the sensitivity in detection of complete and partial tears to the interosseous ligament. However, wrist arthroscopy's ability to simultaneously detect and treat injuries of the scapholunate interosseous ligament (SLIL) is a major advance. Particularly, a partial tear of the SLIL that continues to be symptomatic is difficult to detect with imaging studies alone but is readily identifiable arthroscopically.2
The purpose of this article is to discuss the arthroscopic management of acute and chronic injuries to the SLIL.
Anatomy
The scapholunate ligament complex involves both extrinsic and intrinsic ligamentous components. The intrinsic portion of the SLIL includes the palmar, midsubstance, and dorsal portions. Berger and Landsmeer have shown that the dorsal portion appears to be the primary biomechanical functioning portion to the interosseous ligament.3 It is composed of stout transverse fibers to resist rotation. The volar portion of the interosseous ligament is composed of longer oblique fibers that allow rotation in the sagittal plane. The central fibromembranous portion of the ligament is frequently perforated, usually in older individuals. Dye from wrist arthrography may leak through this perforation, suggesting a tear of the interosseous ligament, although biomechanically the functioning thicker volar and dorsal portions of the ligament are still intact and provide stability.4,5 Thus, a positive arthrogram may cloud the clinical picture. The extrinsic components include the volar radioscaphocapitate ligament, long radiolunate ligament, and short radiolunate ligament. The extent of injury required to disrupt the normal kinematics of the scapholunate interval is not well understood and is controversial.
The SLIL has been shown to stretch and eventually tear. Mayfield et al have shown that the elongation to failure may be up to 225% its length.6 An isolated injury to the SLIL itself may not yield disassociation and widening on plain or stress radiographs. However, a combined injury to both the intrinsic and extrinsic ligaments may result in scapholunate diastasis.7 Plain radiograph abnormalities may not be seen initially until gradual attenuation of the extrinsic ligaments occurs. A spectrum of injury to the SLIL is seen. This spectrum of injury is readily identifiable arthroscopically and may be managed based on the severity of the injury and chronicity.8
Management
The management of scapholunate instability is relatively straightforward when radiographic signs of scapholunate instability are present in acute injuries. The management of a patient who is clinically suspected of having scapholunate instability, yet whose plain radiographs are normal, is controversial. Patients who are clinically suspected of having a SLIL tear but whose radiographs are normal are immobilized, and repeat evaluations are performed at 1 and 3 weeks in an acute injury. If the patient continues to be symptomatic on evaluation at the 4-week interval, further ancillary imaging may be performed. While MRI is surpassing arthrography as the imaging study of choice, satisfactory evaluation requires a sufficiently strong magnet and an experienced radiologist. In the patient who continues to be symptomatic at the 4–5 week interval and whose history and clinical examination is strongly consistent with an injury to the SLIL, we generally perform a “Mississippi MRI”: to proceed directly with arthroscopic evaluation to the wrist. The key to remember is that the window of opportunity for healing in acute injury to the interosseous ligament is fairly limited.
Arthroscopic Evaluation
The crucial key to arthroscopic management of carpal instability is recognition of what is normal and what is abnormal. Both the radiocarpal and midcarpal spaces should be evaluated arthroscopically when carpal instability is suspected. Wrist arthroscopy is not considered complete if the radiocarpal and mid carpal spaces have not both been evaluated.
The wrist is arthroscopically evaluated with standard techniques. The 3–4 and 6R portals are made by pulling the skin against the tip of a no. 11 blade. Blunt dissection is performed with a hemostat to the level of the capsule. The arthroscope with a blunt trocar is introduced into the 3–4 portal. Inflow is provided through the 6U portal. Outflow is provided through the arthroscopic cannula to limit fluid extravasation of the wrist. The SLIL is best seen with the arthroscope in the 3–4 portal (Fig. 1). Following arthroscopic evaluation of the radiocarpal space, the arthroscope is then placed into the midcarpal radial (MCR) portal. This portal is ∼1 cm distal to the 3–4 portal in line with the radial border of the long finger. In some patients, it may be difficult to enter into the MCR portal. There is more space available in the midcarpal ulnar (MCU) portal, and if difficulty arises, the MCU portal may be initially used to improve visualization. It is important to have separate inflow and outflow to the midcarpal space. In the midcarpal space, inflow is traditionally provided through the arthroscopic cannula and a separate outflow is provided through a needle placed in the MCU portal.
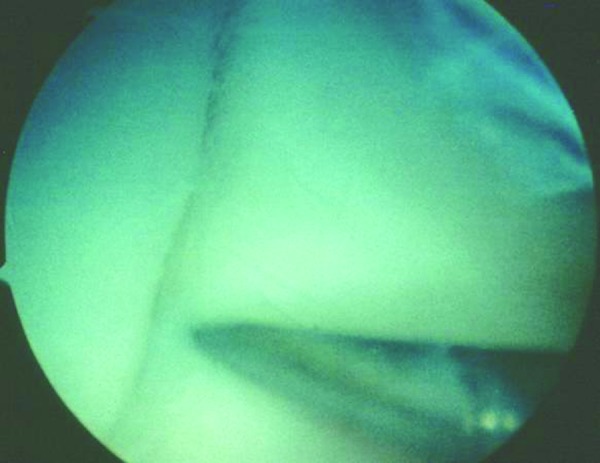
Fig. 1.
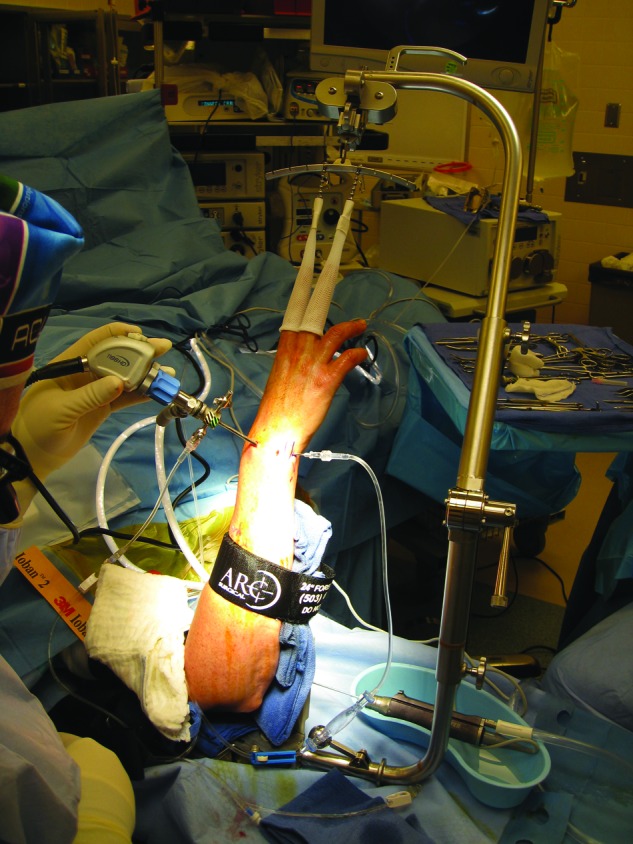
The wrist is suspended in a traction tower in a slightly flexed position. The standard 3–4 portal is used for visualization of the SLIL.
The SLIL is best visualized with the arthroscope in the 3–4 portal. It should have a concave appearance as viewed from the radiocarpal space. In the midcarpal space, the scapholunate interval should be tight and congruent without any step-off. This is in contrast to the lunotriquetral carpal interval, in which a 1-mm step-off is usually seen.
As noted before, a spectrum of injury to the SLIL is seen as it starts to stretch and eventually tear. The appearance of the carpal bones converts from the normal concave to convex. As the SLIL tears, it hangs down and blocks visualization with the arthroscope in the radiocarpal space.9 As the severity of the injury increases, the degree of rotation between the scaphoid and lunate increases and is best evaluated with the arthroscope in the midcarpal space.
Geissler devised an arthroscopic classification of carpal instability and suggested management of acute injuries to the SLIL (Table 1).10 In grade I injuries, there is loss of the normal concave appearance of the interosseous ligament from the scaphoid and the lunate as the ligament bulges with a convex appearance, as seen with the arthroscope in the radiocarpal space. In the mid carpal space, the scapholunate interval is still tight and congruent. It is thought these are minor wrist sprains and usually will resolve with simple immobilization.
Table 1. Geissler arthroscopic classification of carpal instability.
| Grade | Description | Management |
|---|---|---|
| I | Attenuation/hemorrhage of interosseous ligament as seen from the radiocarpal joint. No incongruency of carpal alignment in the midcarpal space. | Immobilization |
| II | Attenuation/hemorrhage of interosseous ligament as seen from the radiocarpal joint. Incongruency/step-off as seen from midcarpal space. A slight gap (less than width of a probe) between carpals may be present. | Arthroscopic reduction and pinning |
| III | Incongruency/step-off of carpal alignment is seen in both the radiocarpal and midcarpal spaces. The probe may be passed through the gap between carpals. | Arthroscopic/open reduction and pinning |
| IV | Incongruency/step-off of carpal alignment is seen in both the radiocarpal and midcarpal spaces. Gross instability with manipulation is noted. A 2.7-mm arthroscope may be passed through the gap between carpals. | Open reduction and repair |
In Geissler grade II injuries, the interosseous ligament continues to stretch and a convex appearance is seen between the scaphoid and the lunate with the arthroscope in the radiocarpal space. In the midcarpal space, the scapholunate interval is no longer congruent. The scaphoid starts to flex palmarly and its dorsal lip is rotated distal to the level of the lunate. This is best appreciated with the arthroscope in the MCU portal looking across the wrist to detect the amount of rotation between the scaphoid and the lunate.
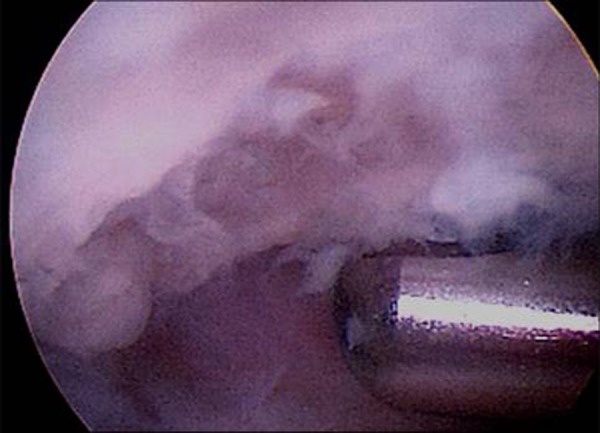
In Geissler grade III injuries, the interosseous ligament tear has progressed from a stretch to a tear and a gap is seen between the scaphoid and the lunate with the arthroscope in the radiocarpal and midcarpal spaces. The tear usually progresses from a volar to dorsal direction. This gap can be appreciated from both the radiocarpal and the midcarpal space. In the midcarpal space, a 1-mm probe may be passed through the gap and twisted between the scaphoid and the lunate (Fig. 2). Sometimes the gap between the scaphoid and the lunate is not immediately seen until a probe is used to push the scaphoid away from the lunate. A portion of the dorsal portion of the SLIL is still attached.
Fig. 2.
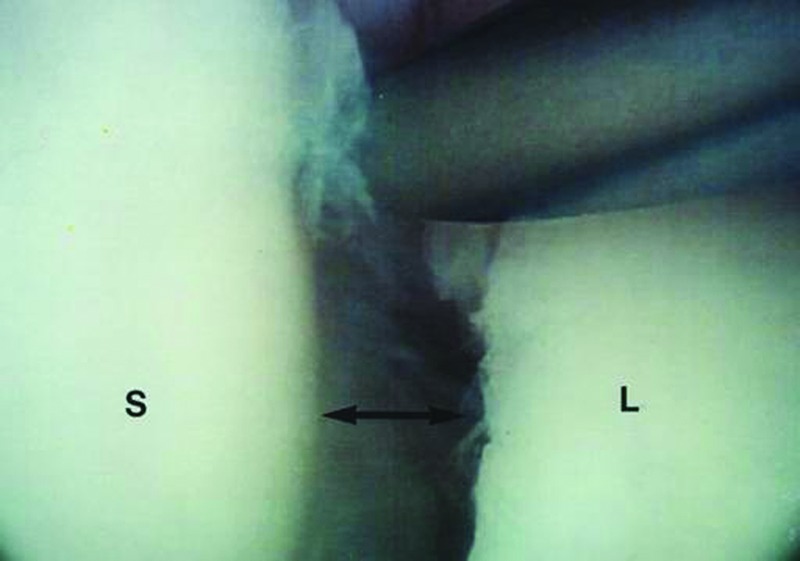
Arthroscopic view with the arthroscope in the radial midcarpal space. Note the probe being inserted through the MCU portal, palpating and demonstrating a gap between the scaphoid and the lunate.
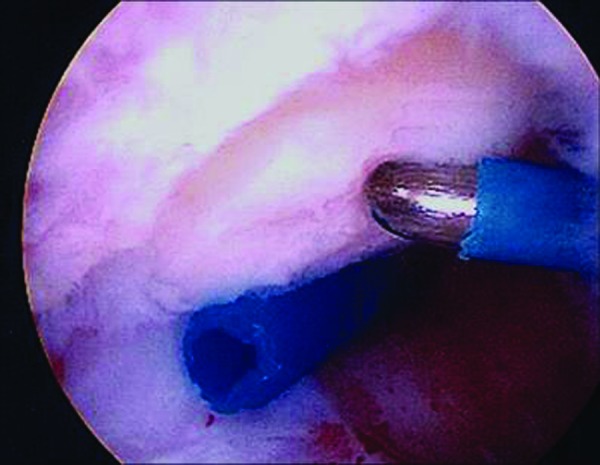
In Geissler grade IV injuries, there is a complete tear to the SLIL. The arthroscope can be freely translated between the radiocarpal and midcarpal spaces (drivethrough sign) (Fig. 3).
Fig. 3.

Arthroscopic view of a Geissler grade IV tear of the SLIL with the “drivethrough sign.” The capitate is easily seen between the interval of the scapholunate, and the arthroscope can be easily transferred back and forth between the radiocarpal and midcarpal spaces through the tear.
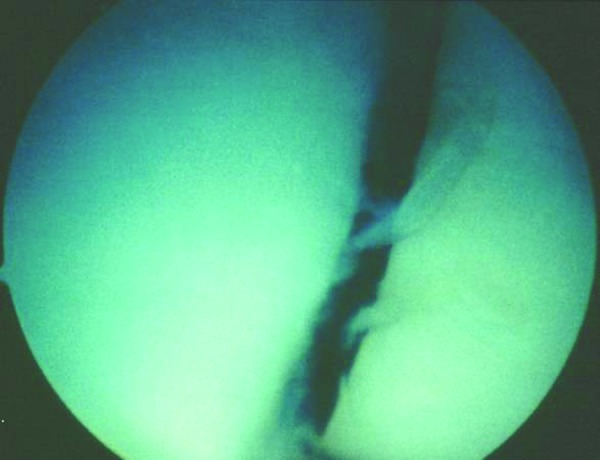
A “poor man's arthrogram” can be performed. In this technique, inflow is provided through the 6U portal and a needle is placed in the midcarpal space. A free flow of fluid between the radiocarpal and midcarpal spaces is consistent with an interosseous ligament tear (Fig. 4).
Fig. 4.

A “poor man's arthrogram.” Inflow is maintained in the 6U portal, and an 18-gauge needle is placed in the midcarpal space. Note the free flow of fluid between the radiocarpal and midcarpal spaces, signifying a tear to the interosseous ligament.
Patients with an acute Geissler grade II or grade III injuries most ideally are suited for arthroscopically assisted reduction and pinning. The arthroscope is placed in the 3–4 portal after the wrist has been evaluated from both the radiocarpal and midcarpal spaces. A 1.1-mm (0.045-in) Kirschner wire (K-wire) is inserted either through a soft tissue protector or in oscillation mode dorsally in the anatomic snuffbox to the scaphoid. It is important to use some type of soft tissue protector to avoid injury to dorsal sensory branches of the radial nerve. A small incision is made and blunt dissection is carried down with a hemostat to the level of the capsule and scaphoid. The K-wire can be seen as it enters into the scaphoid with the arthroscope in the radial gutter in the radiocarpal space. In this technique, the lunate has been marked out by the 3–4, 4–5, MCR, and MCU portals. The K-wire is aimed into the center of the square marked by these four portals.
In an alternative, easier technique, the wrist is taken out of traction and, under fluoroscopic control; the surgeon may insert the K-wires in the scaphoid, aiming toward the lunate (Fig. 5). Fluoroscopy confirms the position of the K-wires in the scaphoid as they are aimed toward the lunate.
Fig. 5.
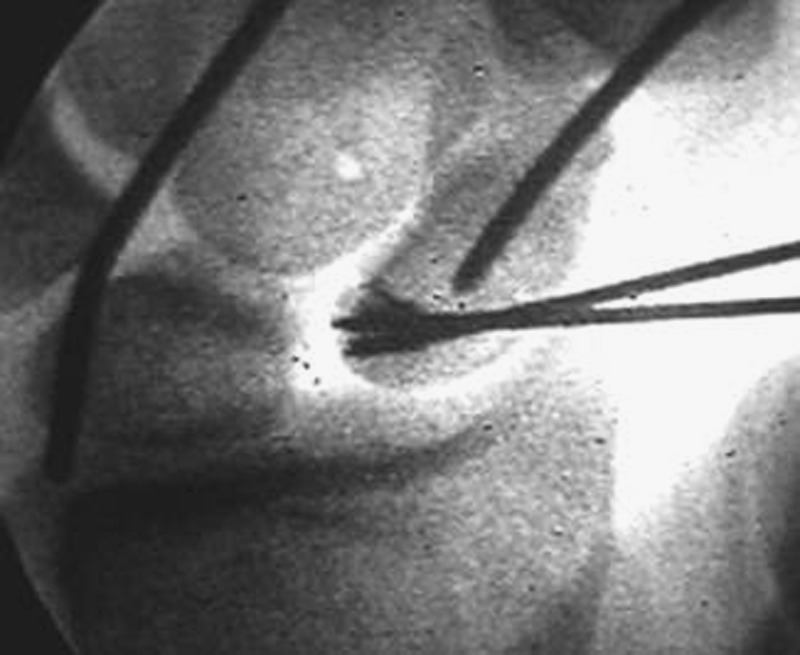
Multiple K-wires are initially placed into the scaphoid toward the lunate prior to arthroscopic reduction of the scapholunate interval.
Once the K-wires are placed into the scaphoid, the wrist is then resuspended in the traction tower. The arthroscope is then placed in the MCU portal. This allows the surgeon to look across the wrist to better judge the rotation and reduction of the scapholunate interval as the K-wires are advanced. The scapholunate interval is then anatomically reduced, as viewed arthroscopically from the mid carpal space (Fig. 6). This may be done by several mechanisms. The wrist may be extended and ulnarly deviated in the traction tower to reduce the palmar flexion of the scaphoid further. Alternatively, K-wires are inserted into the dorsum of the scaphoid and lunate and used as joysticks to control rotation of the scapholunate interval. This is particularly useful in grade III injuries, where a gap exists between the scaphoid and the lunate. The surgeon then advances the K-wires across the scapholunate interval, aiming for the lunate, after the interval has been anatomically reduced. Fat droplets are usually seen exiting between the scaphoid and the lunate in the midcarpal space as the K-wires are driven across the carpal bones. Three or four K-wires are placed in this manner (Fig. 7). In an acute injury, no wires are placed from the scaphoid into the capitate, so as to avoid injury to the pristine articular cartilage of that interval.
Fig. 6.
The arthroscope is placed in the MCU portal and the scapholunate interval is viewed arthroscopically.
Fig. 7.

The K-wires are then advanced across the scapholunate interval after confirming reduction from the midcarpal space.
The wires are left protruding from the skin, and the wrist is immobilized in a below-elbow cast. The pin tracks are evaluated every 2 weeks. The K-wires are then removed in the office at the 8-week interval, and the wrist is immobilized an additional 4 weeks. Digital range of motion (ROM) exercise is initiated immediately. ROM and grip-strengthening exercises of the wrist are started at the 3-month interval.
Patients with acute grade IV injuries to the SLIL are felt to be best reduced through a small dorsal incision to obtain primary repair of the dorsal portion of the SLIL. Prior to this arthrotomy, the wrist is evaluated arthroscopically for any additional injuries, including potential cartilaginous loose bodies and additional injury to the lunotriquetral interosseous ligament, the triangular fibrocartilage complex, or both (Figs. 8, 9). Following repair to the scapholunate interosseous ligament, a SLIC screw (Acumed, Hillsboro, OR) is placed across the scapholunate interval. This screw freely rotates at its midsection and also toggles at its midsection. The screw allows continued compression at the scapholunate interval while the SLIL heals (Fig. 10). The screw allows early ROM as compared with protruding K-wires. The screw may be removed following healing of the SLIL. The use of the screw in Geissler grade II and grade III acute interosseous ligament injuries is currently being evaluated as well.
Fig. 8.

Posteroanterior radiograph of a 19-year-old college football player with a complete avulsion of SLIL.
Fig. 9.
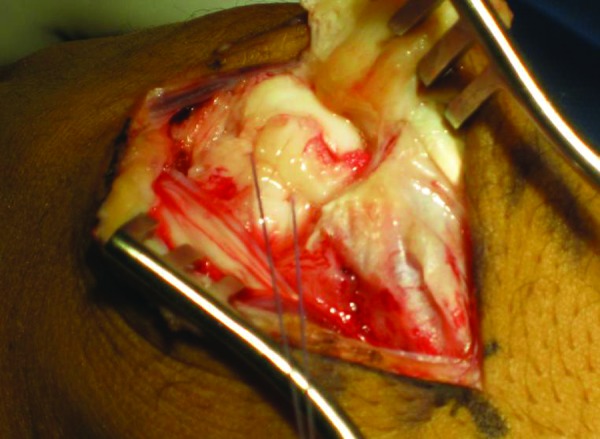
With the patient in Fig. 8 having a complete tear, an open repair of the interosseous ligament is performed.
Fig. 10.

A SLIC screw is placed across the scapholunate interval to stabilize the tear as the ligament heals. The patient in Fig. 8 returned to competition in approximately 3 months.
Whipple reviewed the results of arthroscopic management of scapholunate instability using the previously described technique, and patients were followed for a duration of 1–3 years.11 In his series, patients were divided into two distinct groups of 40 patients each according to duration of symptoms and the scapholunate gap seen on radiographs. Of patients who had a history of scapholunate instability for 3 months or less and had less than a 3-mm side-to-side difference in the scapholunate interval, 83% had maintenance of the reduction and symptomatic relief. Conversely, only 53% of patients had symptomatic relief following arthroscopic reduction and pinning when they had been symptomatic for greater than 3 months and had more than a 3-mm side-to-side scapholunate gap. Patients with less than 3 months symptom duration and 3-mm side-to-side scapholunate gap were followed up for 2–7 years, and it was found that 85% continued to maintain their stability in this series. This series emphasized the need for early diagnosis and management for acute scapholunate instability, and the scapholunate ligament has a diminished capacity for healing after the injury becomes chronic.
Management of Chronic Tears
Chronic tears of the SLIL lose their intrinsic ability to heal, as previously shown by the work of Whipple.11 The management of chronic injury to the SLIL is controversial and depends on the severity of the tear. Possible treatment options include simple arthroscopic débridement, ligamentous reconstruction, proximal row carpectomy, intercarpal fusion, and, potentially, wrist fusion as a salvage procedure when secondary degenerative changes are present.
The arthroscopic technique for débridement of partial chronic tears of the SLIL is straightforward.12 The interosseous ligament is assessed from both the interosseous ligament injury and the radiocarpal and midcarpal spaces. Grade I chronic injuries may or may not be symptomatic. Arthroscopic débridement would be indicated primarily for chronic Geissler grade II or grade III injuries to the SLIL. Following arthroscopic evaluation of the wrist, the arthroscope is transferred into the 6R portal. The shaver is brought in through the 3–4 portal to debride the torn fibers of the SLIL (Fig. 11). The goal of management is to debride the unstable tissue back to stable tissue similar to débridement of a tear to the articular disk of the triangular fibrocartilage complex. The primary access is to the membranous portion of the SLIL with the shaver in the 3–4 portal and a partial débridement of the volar and dorsal portions of the interosseous ligament is possible.
Fig. 11.
Arthroscopic view with the arthroscope in the 6R portal demonstrating débridement of a partial tear to the SLIL with the shaver in the 3–4 portal.
Weiss et al examined the role of arthroscopic débridement for both partial and complete tears to the interosseous ligament.13 They noted that at an average of 27 months following débridement, 19 of 29 patients who had a complete tear of the SLIL and 31 of 36 patients who had a partial tear had resolution or decrease in wrist symptoms following arthroscopic débridement. They noted that arthroscopic débridement of complete tears of the SLIL had a lower success rate, and other surgical options may need to be considered.
Electrothermal shrinkage may play a role in the management of chronic partial tears of the SLIL. Electrothermal shrinkage is controversial, and most studies have had a short follow-up. Electrothermal shrinkage is based on the theory that heating the collagen matrix results in shrinkage of the collagen as the structure denatures. Fibroblasts then grow into the shrunken collagen tissue. Several questions still remain unanswered, such as what the stability of this disorganized collagen matrix is over time and whether the shrunken tissue will act similarly to a normal ligament.
Similar to arthroscopic débridement, the technique is relatively straightforward. The wrist is initially evaluated from both the radiocarpal and mid carpal spaces. The arthroscope is placed in the 4–5 or 6R portal. A monopolar or bipolar thermal probe is used in the 3–4 portal. A monopolar probe has deeper penetration of the heat into the tissue than a bipolar probe does. Following mechanical débridement of the interosseous ligament tear, an electrothermal probe is used to shrink the remaining portion of the interosseous ligament (Fig. 12). Transverse passes appear to be more effective than longitudinal passes in contracting the interosseous ligament. It is important not to paint the ligament but to make transverse passes so that normal uninvolved tissue may then grow into the shrunken portion of the interosseous ligament. The thermal probe is then used to continue along both the dorsal and volar capsule. Next, the arthroscope is placed in the MCU portal, and shrinkage may continue into the midcarpal space with the probe in the MCR portal.
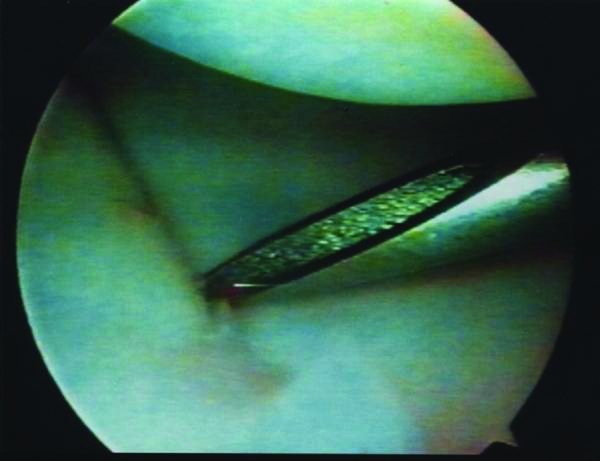
Fig. 12.
Arthroscopic view with the arthroscope in the 6R portal, demonstrating electrothermal shrinkage of a partial tear to the SLIL with the electrothermal probe in the 3–4 portal.
It is important that the probe is continuously moving so as not to concentrate all the heat in one particular spot. It is extremely important to increase the flow of the irrigation fluid when using an electrothermal probe. Inflow is provided through the 6U portal and outflow is maintained through the arthroscope. The purpose of increasing the flow is to disseminate the heat from the probe. The temperature of the irrigation fluid as it leaves the wrist should be monitored. The wattage of the probe may be turned down, and the temperature of the monopolar probe should not exceed 68°C. It is important to remember that the volume of irrigation fluid of the wrist is quite small and the fluid may rapidly heat up with the use of a thermal probe. Following shrinkage of the interosseous ligament, the arthroscope is placed back in the MCR portal to assess the stability of the scapholunate interval (Figs. 13, 14).
Fig. 13.
Arthroscopic view of a gap between the scaphoid and lunate as seen with the arthroscope in the MCR portal.
Fig. 14.
Arthroscopic view demonstrating reduction of the gap between the scaphoid and the lunate with the arthroscope in the MCR portal following shrinkage of the interosseous ligament.
Postoperative management of electrothermal shrinkage for chronic partial tears of the SLIL is controversial. Limited protocols are available. Some authors believe that immobilization alone is sufficient, while others believe in temporary K-wire stabilization. Patients are typically immobilized for 6–8 weeks following thermal shrinkage. ROM and grip-strengthening exercises are initiated at 3 months from surgery.
Geissler reviewed his results in 19 patients with isolated chronic tears to the scapholunate or lunotriquetral interosseous ligament.14 A chronic injury was defined as symptoms present for longer than 6 months in his study. He noted that grade II tears of the SLIL did significantly better than grade III or grade IV tears. Of the six patients with grade II tears, there were four excellent and two good results. In the four patients who had a grade III tear, there was one excellent, one good, one fair, and one poor result.
Wrist arthroscopy plays a limited salvage role in patients with complete chronic tears of the SLIL. Wrist arthroscopy can be used to evaluate the degree and extent of articular cartilage degeneration in patients with scapholunate advanced collapse (SLAC) of the wrist.15 The status of the articular cartilage, as determined arthroscopically, helps to determine whether a reconstructive procedure, such as ligament reconstruction or capsulodesis, would be indicated as compared with a salvage procedure (four-corner fusion, proximal carpectomy).
Arthroscopic evaluation of the status of the articular cartilage of the head of the capitate is extremely useful in determining the indications for four-corner fusion versus proximal row carpectomy. Patients who have significant chondromalacia changes of the capitate, as viewed arthroscopically, would be better candidates for four-corner fusion or limited wrist fusion than for proximal row carpectomy.
In patients who have point tenderness over the radial styloid and want a minimally invasive procedure, arthroscopic radial styloidectomy is an option. It is important that the patient realizes that this is a temporary procedure and further surgery may be indicated in the future. In this technique, the arthroscope is placed in the 3–4 portal and a burr is placed through the 1–2 portal. The amount of chondromalacia on the scaphoid facet of the distal radius marks the area of bone to be resected. Approximately 4 mm of bone may be excised utilizing this technique. It is important to protect the origin of the radioscaphocapitate ligament in performing this procedure.
Wrist arthroscopy continues to grow in popularity as a valuable adjunct to the management of wrist disorders. It enables the evaluation of intracarpal structures under bright light and magnified conditions with minimal morbidity as compared with an arthrotomy. It is extremely sensitive for detecting the spectrum of injury that occurs to the SLIL as it stretches and eventually tears. Improved techniques will continue to emerge as more surgeons are instructed in the use of wrist arthroscopy and better instrumentation is developed.
Footnotes
Conflict of Interest None
References
- 1.Weiss A PC, Akelman E, Lambiase R. Comparison of the findings of triple injection cinearthrography of the wrist with those of arthroscopy. J Bone Joint Surg Am. 1996;78(3):348–356. doi: 10.2106/00004623-199603000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Whipple T L, Marotta J J, Powell J H III. Techniques of wrist arthroscopy. Arthroscopy. 1986;2(4):244–252. doi: 10.1016/s0749-8063(86)80079-2. [DOI] [PubMed] [Google Scholar]
- 3.Berger R A, Landsmeer J MF. The palmar radiocarpal ligaments: a study of adult and fetal human wrist joints. J Hand Surg Am. 1990;15(6):847–854. doi: 10.1016/0363-5023(90)90002-9. [DOI] [PubMed] [Google Scholar]
- 4.Cooney W P. Evaluation of chronic wrist pain by arthrography, arthroscopy, and arthrotomy. J Hand Surg Am. 1993;18(5):815–822. doi: 10.1016/0363-5023(93)90047-7. [DOI] [PubMed] [Google Scholar]
- 5.Chung K C, Zimmerman N B, Travis M T. Wrist arthrography versus arthroscopy: a comparative study of 150 cases. J Hand Surg Am. 1996;21(4):591–594. doi: 10.1016/S0363-5023(96)80008-6. [DOI] [PubMed] [Google Scholar]
- 6.Mayfield J K. Wrist ligamentous anatomy and pathogenesis of carpal instability. Orthop Clin North Am. 1984;15(2):209–216. [PubMed] [Google Scholar]
- 7.Meade T D, Schneider L H, Cherry K. Radiographic analysis of selective ligament sectioning at the carpal scaphoid: a cadaver study. J Hand Surg Am. 1990;15(6):855–862. doi: 10.1016/0363-5023(90)90003-a. [DOI] [PubMed] [Google Scholar]
- 8.Johnstone D J, Thorogood S, Smith W H, Scott T D. A comparison of magnetic resonance imaging and arthroscopy in the investigation of chronic wrist pain. J Hand Surg [Br] 1997;22(6):714–718. doi: 10.1016/s0266-7681(97)80431-7. [DOI] [PubMed] [Google Scholar]
- 9.Adolfsson L. Arthroscopic diagnosis of ligament lesions of the wrist. J Hand Surg [Br] 1994;19(4):505–512. doi: 10.1016/0266-7681(94)90217-8. [DOI] [PubMed] [Google Scholar]
- 10.Geissler W B, Freeland A E, Savoie F H, McIntyre L W, Whipple T L. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78(3):357–365. doi: 10.2106/00004623-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Whipple T L. The role of arthroscopy in the treatment of scapholunate instability. Hand Clin. 1995;11(1):37–40. [PubMed] [Google Scholar]
- 12.Ruch D S, Poehling G G. Arthroscopic management of partial scapholunate and lunotriquetral injuries of the wrist. J Hand Surg Am. 1996;21(3):412–417. doi: 10.1016/S0363-5023(96)80354-6. [DOI] [PubMed] [Google Scholar]
- 13.Weiss A PC, Sachar K, Glowacki K A. Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg Am. 1997;22(2):344–349. doi: 10.1016/S0363-5023(97)80176-1. [DOI] [PubMed] [Google Scholar]
- 14.Geissler W B, Haley T. Arthroscopic management of scapholunate instability. Atlas Hand Clin. 2001;6:253–274. [Google Scholar]
- 15.Watson H K, Ballet F L. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9(3):358–365. doi: 10.1016/s0363-5023(84)80223-3. [DOI] [PubMed] [Google Scholar]


