Abstract
Purpose
Mathematical and simulation models are increasingly used to plan for and evaluate health sector responses to disasters, yet no clear consensus exists regarding best practices for the design, conduct, and reporting of such models. We examined a large selection of published health sector disaster response models to generate a set of best practice guidelines for such models.
Methods
We reviewed a spectrum of published disaster response models addressing public health or healthcare delivery, focusing in particular on the type of disaster and response decisions considered, decision makers targeted, choice of outcomes evaluated, modeling methodology, and reporting format. We developed initial recommendations for best practices for creating and reporting such models and refined these guidelines after soliciting feedback from response modeling experts and from members of the Society for Medical Decision Making.
Results
We propose six recommendations for model construction and reporting, inspired by the most exemplary models: Health sector disaster response models should address real-world problems; be designed for maximum usability by response planners; strike the appropriate balance between simplicity and complexity; include appropriate outcomes, which extend beyond those considered in traditional cost-effectiveness analyses; and be designed to evaluate the many uncertainties inherent in disaster response. Finally, good model reporting is particularly critical for disaster response models.
Conclusions
Quantitative models are critical tools for planning effective health sector responses to disasters. The recommendations we propose can increase the applicability and interpretability of future models, thereby improving strategic, tactical, and operational aspects of preparedness planning and response.
MeSH/Keywords: Disaster Planning, Mass Casualty Incidents, Computer Simulation, Cost-benefit Analysis, Guideline
1. BACKGROUND
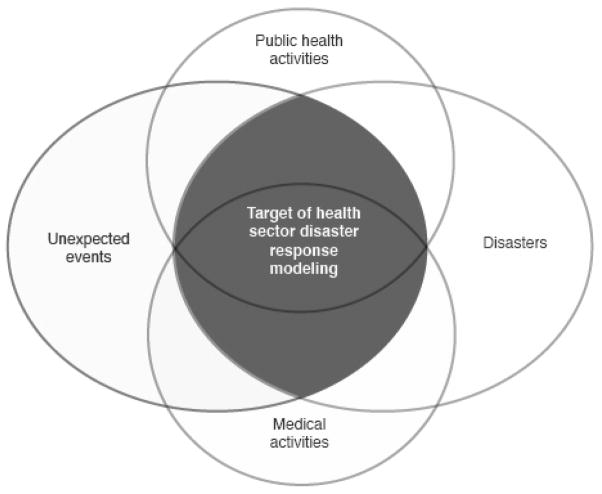
Disasters such as the 2001 U.S. terrorist attacks, Hurricane Katrina, and the 2008 Chengdu earthquake have highlighted the need for improved public health and medical disaster response capabilities at local, regional, national, and international levels. Disasters are commonly defined as events whose consequences exceed the capability of local or regional medical and public health systems to provide necessary responses in a timely manner (Figure 1). We use the term “health sector disaster response” to encompass all activities of medical and public health systems affected by a disaster, including treatment of existing casualties and prevention and treatment of future casualties. Major unresolved issues remain at all levels of disaster response decision making, including long-range strategic planning, tactical response planning, and real-time operational support.* For example, how should the logistical systems for response to various types of public health disasters be organized? How much hospital-based surge capacity might be needed for potential mass casualty events? What is the most efficient and effective way to rapidly dispense medications or vaccines to large numbers of individuals?
Figure 1. Health System Disaster Response Modeling.
This figure presents the target of health system disaster response modeling. We distinguish between unexpected events and disasters. An unexpected event (e.g., hurricane, earthquake) may not necessarily result in a disaster. A disaster (e.g., war, famine) may not necessarily be an unexpected event. Similarly, public health activities include a broad range of activities, including some (e.g., asthma prevention) that are not relevant to health sector disaster responses. Medical activities, likewise, include a broad range of activities (e.g., routine patient care) that are not relevant to disaster responses. The focus of this paper is models of public health and medical activities that address unexpected disasters.
Increasingly, simulation and mathematical modeling are being used to explore the capabilities, costs, and consequences of public health and medical disaster response plans. Members of the Society for Medical Decision Making and its journal have been active in this nascent field, publishing a variety of models including those that address the epidemiological and medical consequences of bioterrorism-related illness and pandemic influenza, logistical challenges during disaster responses, and the cost-effectiveness of specific disaster response strategies.1–5 Recently, the U.S. Department of Health and Human Services and the Centers for Disease Control and Prevention created initiatives to support modeling projects of relevance to their missions. However, the field of health sector disaster response modeling lacks a coherent thematological or methodological organization. Such organization could assist modelers in understanding and addressing the requirements of end users, facilitate consistent and systematic reporting of model inputs and results, and promote the development of standardized methodological approaches -- just as the Report from the Panel on Cost Effectiveness in Health and Medicine provides guidance for the field of cost-effectiveness analysis.6
This paper describes the range of models that have been developed for public health and medical responses to disasters and proposes a set of recommendations for developing and reporting the results of these models—something that has been lacking in the literature. This paper addresses three questions: 1) What kinds of health sector disaster response models have been developed? We describe exemplary and representative articles from the literature on applied decision support modeling for health sector disaster response, paying particular attention to the ways in which these articles differ from classic cost-effectiveness studies. 2) What methodologies have been and might be used for such models? We discuss the use of a range of modeling techniques for a variety of decision problems. 3) What are best practices for modeling and reporting of health sector disaster responses? We provide recommendations that we hope will serve as guides for the development of models focused on public health and medical responses to disasters; for funders of relevant modeling efforts; and for journals interested in publishing the findings of these models.
2. METHODS
We sought to identify best practices in modeling health sector disaster responses and the reporting of such models. We focused on models that can support informed decision making about responses to public health disasters. We did not perform a systematic review; instead, we sought to identify a range of articles that used a variety of modeling methodologies to address a broad range of disasters and response decisions. The focus of our analysis was on modeling methodologies, model quality, and the reporting of model analysis and results—but not on the specific planning insights from the models. Thus, we do not present detailed results of analyses performed with the included models.
2.1. Literature Search
We searched for published models from relevant sources including MEDLINE, International Abstracts in Operations Research, content experts, and the authors of included models. We also searched the tables of contents of relevant journals in such diverse fields as economics, industrial engineering, operations research, nuclear technology, and risk analysis (e.g., Operations Research, Management Science, Risk Analysis, European Journal of Operational Research, Interfaces, Journal of Intelligent Transportation Systems, Nuclear Technology, Decision Analysis). From recent U.S. National Preparedness Guidelines,7 we identified a variety of disasters that could have a significant effect on public health.
We identified 567 potentially relevant articles, reviewed 120, and included 67 articles describing 55 models. The models we selected for inclusion are representative of the literature and are not intended to be exhaustive; however, they directly inform our recommendations. We included only articles that describe a quantitative model designed to support informed decision making about public health or medical responses to disasters. We excluded highly stylized mathematical models that have little immediate practical application (e.g., those focused on the mathematics of infectious disease progression), non-peer reviewed models and those presented in abstracts only, and articles not written in English.
From each included article, we collected information about the purpose of the model, type of disaster considered, aspect of response the model was designed to address, modeling approach, model setting, decision makers included in the model, decisions modeled, and model outputs. We also collected information about the quality of each model and its reporting based in part on established criteria for the evaluation of healthcare models (e.g., whether all relevant model inputs and their sources were described, whether all assumptions of the model were explained).6
2.2. Development of Recommendations
As a team, we developed criteria for characterizing high quality modeling and model reporting and then developed a set of recommendations addressing the design, conduct, and reporting of such models. During these detailed discussions, we drafted and then revised the recommendations in an iterative manner. There were no significant disagreements among the writing team regarding model classification or resulting recommendations.
2.3. Critical Review by Content Experts and Members of the Society for Medical Decision Making
We sought critical feedback from content experts and members of the Society for Medical Decision Making (SMDM) on drafts of this position paper. We presented our results at the 2008 SMDM Annual Meeting in Philadelphia and the 2008 INFORMS conference in Washington, DC, and posted a draft of this paper on the SMDM website for additional comments. The final paper incorporates these comments.
3. RESULTS
3.1. Response Models
Table 1 describes the included studies and outlines the purpose of each model, the disaster considered, the model design, and outputs. Included models address a variety of decision makers (e.g., first responders, hospital officials, planners, public health officials), geographic settings (e.g., local, regional, national), decisions modeled (e.g., dispensing, inventory/stockpiling, supply chain network design, prevention or mitigation of disaster effects, treatment, health care work force staffing, transportation), and outcomes evaluated (e.g., costs, morbidity, mortality, quality-adjusted life years, hospital utilization measures, logistical outcomes), and use a range of modeling methodologies. The quality of modeling methodology and model reporting was variable (Figure 2). The following sections provide an overview of response decisions modeled, outcomes evaluated, and modeling methodologies used in these selected papers.
Table 1.
Description of Selected Health Sector Disaster Response Models
| Author (Reference) |
Purpose of Model/Study | Modeling Methodology |
Disaster Evaluated† |
Decision Makers Considered* |
Geographic Setting |
Decisions Modeled§ |
Outcomes¶ |
|---|---|---|---|---|---|---|---|
| Disease Outbreaks | |||||||
| Braithwaite, Fridsma, Roberts1 | To assess the cost-effectiveness of pre-exposure anthrax vaccination vs. an emergency surveillance and response system | Dynamic compartmental model | Anthrax | P | Local and Regional | Rx, P | $, QALY, M |
| Hupert, Mushlin, Callahan3, 9 | To determine staffing levels necessary to maintain throughput requirements for antibiotic dispensing centers in the aftermath of a bioterrorism attack | Simulation (Discrete event) | Anthrax | P, PH | Local | D, S | L |
| Lee and others34, 35 | To construct and implement a real-time decision support system for planning antibiotic dispensing in response to a large-scale disease outbreak | Simulation, Optimization | Anthrax | P, PH | Local (Urban setting) | D, S | L |
| Brookmeyer, Johnson, Bollinger11, 79 | To assess the optimum duration of antibiotic prophylaxis and evaluate varying prophylactic strategies (pre or post-exposure vaccination, antibiotic prophylaxis) for anthrax response | Competing risks, probability/mathematical model | Anthrax | P, PH | Local | Rx, P | M |
| Wein, Craft, and others66–68 | To evaluate the effectiveness of several response strategies for anthrax (pre-exposure vaccination, achievable levels of distributed antibiotic prophylaxis, biosensor efficacy) | Multi-tiered mathematical model | Anthrax | P | Local (A large city) | I, ND, Rx, P | L, M |
| Fowler and others62 | To assess the cost-effectiveness of vaccination (pre- or post-exposure) vs. post-exposure antibiotic prophylaxis response strategies for anthrax | Simulation (Decision analytic) | Anthrax | P | Local (A large US metropolitan area) | Rx, P | $, QALY, M |
| Schmitt and others63 | To evaluate the cost-effectiveness of vaccination (pre- or post-exposure) vs. post-exposure antibiotic prophylaxis response strategies for anthrax response | Simulation (Markov model) | Anthrax | P | Regional (Attack via US Postal Service) | Rx, P | $, QALY, M |
| Zaric, Bravata, Brandeau, and others5, 41, 52 | To evaluate the cost-effectiveness of alternative strategies for maintaining and dispensing antibiotic inventories (local vs. regional) and communication with the public during an anthrax response | Dynamic compartmental model | Anthrax | P | Local (A large US metropolitan area) | I, ND, P | $, QALY, M |
| Whitworth40 | To evaluate plans for anthrax response (e.g., number and location of dispensing centers, dispensing strategies, staffing plans, and traffic-management plans) | Simulation (Discrete event) | Anthrax | P | Local | D, S | L |
| Medema and others60 | To evaluate health and economic outcomes of interventions for pandemic influenza (e.g., increasing the vaccine supply through egg-based or cell culture, provision of antivirals) | Simulation | Pandemic influenza | P, O | National | Rx | $, L, M |
| van Genugten, Heijnen, Jager54 | To estimate (using FluSurge4) hospitalizations and deaths in the Netherlands from pandemic influenza, as a function of response strategy (no intervention, vaccinate high-risk individuals, vaccinate all, treat symptomatic people with antiviral drugs) | Spreadsheet | Pandemic influenza | PH | National (Netherlands) | P, Rx | M, H |
| Longini and others56 | To investigate the effectiveness of targeted use of antivirals to contain the first wave of an influenza pandemic in the United States (before a vaccine can be developed) | Simulation (Stochastic, discrete time, network of 2000 individuals) | Pandemic influenza | PH | “A typical American community” | P, Rx | O |
| Meltzer, Cox, Fukuda57 | To estimate outcomes of pandemic influenza (illnesses, deaths, etc.) and the effects of potential vaccination strategies, and to determine how much should be spent each year to plan/prepare for mass vaccination | Simulation (Monte Carlo) | Pandemic influenza | P | National (US) | P | $, M, H |
| Eichner and others53 | To evaluate the impact of three types of interventions on pandemic influenza outcomes: antivirals, social distancing, and contact reduction | Compartmental epidemic model (Deterministic) | Pandemic influenza | P | National, Regional, or Local | P | M, L, H |
| Wilson, Mansoor, Baker26 | To estimate population health and economic impacts of the next influenza pandemic in New Zealand | Deterministic model | Pandemic influenza | P | National (New Zealand) | P | $, H |
| Zhang, Meltzer, Wortley4 | To estimate the impact of pandemic influenza on hospital services | Spreadsheet | Pandemic influenza | H, P | Regional | Rx | H, M |
| Soberiaj and others25 | To estimate the impact of pandemic influenza on hospital services at the William Beaumont Army Medical Center in El Paso, Texas | Spreadsheet | Pandemic influenza | H, P | Local | Rx | M |
| Siddiqui and Edmonds59 | To evaluate the cost-effectiveness of antiviral stockpiling and near-patient testing (rapid diagnostic tests at point of care) for an influenza pandemic in the United Kingdom | Spreadsheet (Incorporates a decision tree; allows for probabilistic and other sensitivity analyses) | Pandemic influenza | P, PH | National (UK) | I, Rx | $, QALY |
| Balicer and others58 | To evaluate the cost-benefit of three different strategies for the use of stockpiled antiviral drugs during an influenza pandemic: therapeutic; long-term pre-exposure prophylaxis (PrEP), and short-term PrEP | Spreadsheet | Pandemic influenza | P, PH | National | I, Rx | $ |
| Germann and others36 | To simulate pandemic influenza in the United States and evaluate the effect of potential mitigation strategies, including antivirals, vaccines, and modified social mobility (travel restrictions, school closures) | Simulation (Microsimulation of 281 million individuals in 2000-person subgroups) | Pandemic influenza | P | National (US) | P | M |
| Khazeni and others61 | To estimate the cost-effectiveness of two control strategies for pandemic influenza: antiviral prophylaxis and prime-boost vaccination | Compartmental epidemic model (Deterministic) | Pandemic influenza | P, PH | Local (A large US metropolitan city) | P | $, QALY |
| Colizza and others80 | To evaluate the effect of international travel restrictions and antiviral treatment on the worldwide spread of pandemic influenza | Compartmental epidemic model (Stochastic; linked models, one for each of 3100 cities/airports) | Pandemic influenza | P, PH | Global | P | M |
| Gupta, Moyer, and Stern64 | To evaluate the cost-benefit of quarantine in controlling SARS | Mathematical (Deterministic) | SARS | PH | Local (Toronto) | P | $, M |
| Lloyd-Smith, Galvani, and Getz81 | To evaluate the effects on SARS transmission within a hospital and a community of hospital-based contact precautions, quarantine, and isolation | Compartmental epidemic model (Stochastic) | SARS | H, PH | Local (Hospital and community) | P | M, O |
| Lipsitch and others82 | To evaluate the effects on SARS transmission of quarantine and isolation measures | Compartmental epidemic model (Deterministic) | SARS | PH | Local | P | M, L, O |
| Massin and others55 | To evaluate interventions for controlling a pneumonic plague outbreak: masks, quarantine, prophylaxis, travel restrictions | Compartmental epidemic model (Deterministic) | Plague | P | National, Regional | P | M |
| Kaplan, Craft, Wein83 | To compare mass vaccination vs. ring vaccination for responding to a smallpox attack in a major US city | Compartmental epidemic model (deterministic) | Smallpox | PH | Regional | P | M |
| Meltzer and others70 | To evaluate the amount of quarantine and vaccination (alone or in combination) that would be required to control a smallpox outbreak caused by bioterrorists, and to estimate the number of vaccine doses needed | Markov model (Spreadsheet) | Smallpox | P | Local | P | M |
| Miller, Randolph, Patterson84 | To evaluate the effects on health and the healthcare system of strategies for responding to a smallpox attack, including vaccination (mass vaccination or ring vaccination), social distancing measures, and quarantine | Simulation (Discrete event, modeling individual people) | Smallpox | P | Local | P | M, H |
| Glasser and others71 | To evaluate the effects of a variety of smallpox control strategies, including isolation of infectives, vaccination of healthcare workers, general vaccination, ring vaccination, and school closure | Compartmental epidemic model (Deterministic) | Smallpox | P | Local | P | M |
| Porco and others85 | To evaluate the effects of contact tracing and ring vaccination in controlling smallpox | Simulation (Discrete event, network of households and workplaces/social groups) | Smallpox | P, PH | Local (A community with households, workplaces, social groups) | P | M |
| Riley and Ferguson86 | To assess the efficacy of symptomatic case isolation, contact tracing with vaccination, and mass vaccination in controlling a smallpox outbreak | Simulation (Individual-based, incorporates spatial factors) | Smallpox | P | National (Great Britain) | P | M |
| Natural Disasters | |||||||
| Barbarosoğlu and Arda48 | To determine the most efficient flow of relief supplies in a transportation network in the aftermath of a rapid-onset disaster | Optimization (Stochastic programming) | Earthquake | P, FR | Local (Urban setting) | ND, T | L |
| Balcik and Beamon39 | To determine the number and location of global distribution centers for stockpiled relief items, as well as the quantity of those items to be maintained, in order to improve disaster response | Optimization (Linear and dynamic programming) | Earthquake | P | Global | ND, T | L |
| Fawcett and Oliveira15 | To estimate the impact of health facility damage, rescue time, and out-of-region transportation on overall mortality from an earthquake | Simulation | Earthquake | H, P, PH, O | Local (Lisbon, Portugal) | T, Rx | L, M,O |
| Paul and others16 | To estimate the transient patient surge at regional hospitals resulting from an earthquake | Simulation (Discrete event with regression-based parameters) | Earthquake | H, P, PH, O | Regional | ND, S, T, Rx | L, H |
| Regnier17 | To determine, for specific locations in the United States, the relationship between hurricane track prediction accuracy and lead time for evacuations | Simulation (Markov model) | Hurricane | P | Local (Four U.S. coastal cities) | T | L, $ |
| Özdamar, Ekinci, Küçükyazici47 | To apply vehicle routing and multi-commodity network flow techniques to develop an algorithm for efficiently dispatching relief supplies to a community affected by a rapid-onset disaster | Optimization | General natural disaster | P | Regional | T | L |
| Manmade Disasters | |||||||
| Beamon and Kotleba18, 19 | To develop inventory management models (order quantities and reorder points) to aid sustained humanitarian response to complex emergencies | Optimization (Simulation used to test model in a case study) | Conventional warfare | P | Regional | I | L |
| Papazoglou and Christou21 | To determine the best short-term emergency response to a nuclear accident, considering the tradeoff between adverse health effects and costs | Optimization (Multiobjective) | Nuclear | P | Regional | P | M, $ |
| Feng and Keller22 | To evaluate different plans for distribution of potassium iodide after release of radioactive iodine caused by a nuclear accident or terrorism | Optimization (Multiobjective decision analysis) | Nuclear | P, PH | Regional | D, I, P | O |
| Dombroski and Fischbeck49, 50 | To evaluate strategies (e.g., caring for patients at the bomb site vs. evacuation) for response to a “dirty bomb” (a conventional explosive wrapped in radioactive material) | Dispersion Model | Radiologic | FR, PH, O | Local | P, O | M, O |
| Georgopoulos and others51 | To evaluate key parameters affecting the exposure of healthcare workers to hazardous materials from contaminated patients | Simulation | Chemical | H, P, FR | Local | P | M, O |
| Inoue, Yanagisawa, Kamae20 | To determine how to increase patient survival rates after a large-scale disaster through improvements in triage and transport procedures | Simulation | Airport accident | FR, PH | Local (Urban airport) | T, O | M |
| Christie and Levary45 | To develop a scenario planning tool for use in the event of a manmade rapid-onset disaster to effectively assign and transport patients for treatment | Simulation | Airplane crash in urban area | FR, PH | Local (Urban setting) | T, O | L |
| Hospital Planning | |||||||
| Levi and others27– 29, 53 | To evaluate Israeli hospitals’ disaster capacity and plans, train decision makers, and assist in managing real situations by identifying bottlenecks and evaluating a variety of response strategies | Simulation | Mass casualty events (e.g., conventional warfare) | H | Hospital | S, Rx, P, O | L, M, H |
| Kanter30, 31 | To evaluate tradeoffs in pediatric hospital strategies that involve altering the standard of care and increasing ICU surge capacity | Simulation | Mass casualty events | H | Hospital | O | H |
| Earnest and others32 | To predict the number of available isolation beds | Autoregressive moving average model | SARS | H | Hospital | O | H |
| Hupert and others33 | To estimate overcrowding of emergency departments due to adverse events from rapid mass prophylaxis campaigns | Spreadsheet model | Smallpox, Anthrax | PH | Hospital | P | M,H |
| Other Types of Models | |||||||
| Han and others46 | To determine efficient route and destination assignments for public evacuation after a large-scale disaster | Simulation | Large-scale disaster requiring evacuation of large urban area | P | Local (Urban setting) | T | L |
| Narzisi and others73 | To analyze hospital capacity, public health preparedness and response, and behavior of the public during a rapid-onset urban disaster | Simulation (Agent-based) | General disaster (distributed or point-source) | P | Local (Urban setting) | H | L |
| Dekle and others38 | To apply facility location techniques to identify potential disaster recovery centers for a local planning authority | Optimization (Integer programming) | General large-scale disaster | P | Local (County) | ND, T | L |
| Balcik, Beamon, and Smilowitz42 | To determine the allocation of relief supplies and scheduling and routing of vehicles for the “last mile” distribution of supplies in response to a disaster | Optimization (Mixed integer programming) | General disaster | P | Local | T, O | $, O |
| Barbarosoğlu, Özdamar, Çevik43 | To evaluate operational routing and loading decisions for helicopter dispatch during the aftermath of a disaster | Optimization (Mixed integer programming) | General disaster | P | Local (Urban setting) | T | L |
| Jotshi, Gong, Batta44 | To develop efficient emergency vehicle routing strategies in the aftermath of a major disaster using available real-time data | Optimization | General disaster | P | Local (Urban setting) | ND, T | H, L |
Disaster evaluated: Some of the included models apply to general disasters but for illustrative purposes used data from specific disaster types. Here, we have categorized them according to the specific type of disaster considered.
Decision makers considered: FR=first responders; H=hospital officials; P=planners (e.g., military planners, national-level emergency response planners); PH=public health officials; O=others (e.g., vaccine manufacturers)
Decisions modeled: D=dispensing; I=inventory/stockpiling; ND=supply chain network design; P=prevention or mitigation of the disaster effects (e.g., vaccination strategies, quarantine, isolation, prophylaxis); Rx=treatment; S=healthcare workforce staffing; T=transportation; O=others (e.g., financing, traffic management)
Outcomes: $=costs; H=hospital utilization measures (e.g., bed capacity); L=logistical outcomes such as inventory levels or queue lengths; M=morbidity or mortality; QALY=quality-adjusted life years; O=others (e.g., probability of containment).
Figure 2. Model and Reporting Quality.
This figure presents the summary assessment of the key quality criteria applied to the included models and the reports describing them.
3.1.1. Response Decisions Modeled
We identified models that address the following broad categories of response decisions: treatment and control of disease outbreaks, response to natural disasters, response to manmade disasters, hospital planning, and disaster response logistics. These categories are not mutually exclusive (for example, a model examining response to a natural disaster could focus on logistical issues). Also, models that focus on treatment and control of disease outbreaks are, of necessity, significantly different from models that focus on responses to natural and manmade disasters; however, all of these disasters require public health and medical responses.
Treatment and control of disease outbreaks
A variety of models have addressed preparation for and response to noncommunicable diseases such as anthrax or communicable diseases such as pandemic influenza, bioterrorist smallpox, and SARS. These models assess the impact of a variety of mitigation strategies, including vaccination, prophylaxis and treatment with antimicrobials, social distancing measures (e.g., masks, school closures), quarantine, travel restrictions, and vaccine development. Several notable models of disease outbreaks have been validated with available data from relevant prior outbreaks in humans3, 8, 9 and animal experiments.10, 11 In one study, researchers from three different groups compared the results of their pandemic influenza simulation models.12 They noted that, “the results need to be viewed more as helping structure thinking about pandemic planning, rather than being predictive of the precise effectiveness of different policies.”12
Responses to natural disasters
Despite the frequency and potentially catastrophic health consequences of natural disasters (e.g., in 2007, 406 natural disasters killed 17,000 people and affected another 201 million people13; and in 2004, the Boxing Day tsunami killed more than 200,000 people14), remarkably few published models have focused on the public health and medical responses to such events. Several of the included models focused on earthquakes,15, 16 including one that is geographically customizable and allows the user to estimate the impact of health facility damage, rescue time, and out-of-region transportation on overall mortality.15 One study of evacuation timing in response to the threat of a hurricane presented receiver operating characteristic curves for four coastal U.S. cities comparing the probability of correct landfall prediction against the probability of a false alarm.17
Response to manmade disasters
Relatively few models have addressed response to manmade disasters such as conventional warfare, radiologic and chemical accidents, acts of terrorism, and large-scale industrial accidents. Some manmade disasters such as war and famine have a slow onset, and may require sustained responses in which relief demands may have occasional spikes.18, 19 One model of famine in Sudan used data from the ongoing crisis there to determine the optimal reorder points and order quantities for relief supplies.18 The authors used simulation to evaluate the interdependence of critical response variables, and reported key insights that humanitarian agencies can use to improve disaster response.19 A study of a hypothetical airport accident used historical data and interviews with responders to simulate the relationships among transport time, triage classification, and patient survival rates.20
Several models have evaluated public health responses to nuclear incidents.21, 22 In general, these models evaluate tradeoffs among different accident mitigation objectives (e.g., minimize adverse health effects, minimize costs). One study of competing plans for distribution of potassium iodide after the release of radioactive iodine from a nuclear accident or terrorism showed how the preferred distribution plan changes as a function of the weights associated with different objectives.22
Hospital planning
Hospital planning models for public health disasters have estimated demand for health care, evaluated triage strategies, planned hospital capacity, and developed appropriate protocols for decontamination and the use of personal protective equipment. Some of these models have been made publicly available in easy-to-use spreadsheets for use by planners for estimating demand for both inpatient and outpatient hospital services,4, 23 and have been used to estimate response capability in a variety of specific settings.24–26
Several models investigate hospital capacity during disasters and, importantly, evaluate potential response bottlenecks at key sites (e.g., emergency departments, operating rooms) and for key resources (e.g., specialized staff). 27–33 One model has been used to evaluate a hospital’s disaster plan, train decision makers, and assist in managing real situations by identifying bottlenecks and evaluating a variety of response strategies.27–29 One model evaluates tradeoffs in hospital strategies that involve altering the standard of care and increasing ICU surge capacity.30, 31 Another model estimates expected overcrowding of emergency departments due to adverse events from rapid vaccination campaigns.33
Response logistics
Logistical decisions are integral to many aspects of disaster response. These include decisions about procurement, transport, stockpiling, and maintenance of needed supplies; mass vaccination, prophylaxis and treatment; transportation and evacuation; and assignment of response personnel.
For many disasters, needed supplies must be rapidly dispensed to large populations. Several models evaluate the location, design, and operation of mass dispensing centers and other supply facilities (e.g., staffing, facility layout).3, 9 One publicly available model has been widely utilized by public health officials to plan dispensing of antibiotics, vaccines, and other disaster supplies in response to anthrax bioterrorism.3, 9, 34, 35 Another model, a decision support system that evaluates facility layout and staffing allocations for emergency mass dispensing, was tested in a field exercise conducted in Georgia.34, 35
Dispensing antimicrobials, vaccines, and other materials during a large-scale disaster response places enormous strain on local health sector infrastructure; conversely, the limits of that infrastructure may influence the course of the disaster. Thus, it is critical that models examining such scenarios evaluate the feasibility of modeled interventions. One pandemic influenza planning model considered the impact of vaccinating 10 million U.S. residents per week over the course of a multi-month pandemic response.36 An unresolved issue is how or whether such vaccination would be feasible given the public health and medical infrastructure, vaccine supply chains, and other aspects of current response logistics in the U.S.
Other important logistical decisions relate to the design and management of the disaster response supply chain including, for example, the location of supply centers, disaster recovery centers, and dispensing sites.37–39 Two notable models incorporate multiple components of the anthrax response supply chain: one considers local level components (e.g., dispensing points, dispensing processes, staffing and traffic management plans)40; the other considers national, regional, and local components.5, 41 Integrated models such as these can help identify the critical elements needed for efficient performance of a disaster response supply chain.
A variety of routing and transportation problems arise in response logistics planning. Models have been developed to determine the allocation of relief supplies and scheduling and routing of vehicles for the “last mile” distribution of supplies in response to a disaster,42 evaluate operational routing and loading decisions for helicopter dispatch in the aftermath of a disaster,43 optimize the transportation of triaged casualties to local hospitals for treatment,44 determine efficient ways to transport patients to hospitals, and model the evacuation of a populated area in anticipation of a disaster.20, 45, 46 Some studies investigate alternative routing of supplies after disaster-related damage to local infrastructure (e.g., bridge destruction after earthquakes), notably using real-world data to inform model inputs.44, 47, 48 A critical factor that can affect disaster response logistics is the behavior of the public and first responders. Several included models have considered such behavioral factors: for example, radiologic exposure after a dirty bomb and timeliness of care to patients as a function of use of cumbersome personal protective equipment;49, 50 contamination risk after chemical terrorism as a function of the behavior of the public and first responders;51 and costs and benefits of alternative communication strategies during an anthrax response as a function of the behavior of the public in response to public health instructions.52
3.1.2. Response Outcomes Evaluated
The included models considered a wide variety of outcomes. For example, in addition to disease incidence and prevalence,53 the included models of infectious disease response considered outcomes such as hospitalizations,54 outpatient visits,53 deaths,54, 55 number of doses of drugs or vaccines required,55 and chance that a pandemic is averted.56 Hospital planning models typically evaluate the demand for various hospital services28, 29, 57 and patient waiting times,16 and often attempt to identify potential bottlenecks in the response.30, 31
Some analyses include costs and attempt to measure the cost-effectiveness of various planning and response strategies. For example, researchers have evaluated the cost-effectiveness (or cost-benefit) of strategies for preparation for and response to influenza pandemics,57–61 anthrax attacks,5, 52, 62, 63 and SARS.64 One study estimated the financial burden of incorrect evacuation decisions in response to hurricanes.17 Comparing estimated health outcomes and costs associated with different disaster response strategies may promote the effective and efficient use of limited public health resources.65
A number of the included response models did not consider intervention costs, sometimes as a result of direct proscription of such analyses by funding sources. In one analysis of the effectiveness of several response strategies for reducing inhalational anthrax mortality (e.g., pre-attack vaccination, antibiotic prophylaxis), the authors noted that their funders discouraged them from considering costs.66–68 They concluded that they had “mixed success” influencing policymakers, partly because one of their key findings was perceived as “too expensive and logistically difficult to achieve.”68
3.1.3. Modeling Methodologies
A variety of modeling methodologies have been applied to analyze disaster response decisions, with considerable variation in the type and complexity of mathematical and analytical techniques used. These include statistical analyses,32, 69 simple spreadsheet calculations,4, 54, 58 Markov models,17, 63, 70 epidemiological models,4, 53–55, 58, 61, 71, 72 supply chain and inventory management models,5, 18, 19, 41 facility location models,38, 39 and vehicle routing and network flow techniques.43, 44, 46–48 Some of the models are quite simple, and consider a relatively small number of entities (e.g., groups of individuals categorized by disease stage, or patients in a single emergency room),32, 55, 61, 71 whereas others simulate complex systems with thousands or even millions of individuals.36, 73
Because of the inherent uncertainty and complexity of disasters and disaster response, many researchers have used computer simulation to model potential outcomes of a disaster under different scenarios: for example, to determine staffing requirements at dispensing centers3 and plan dispensing strategies34, 35 after a bioterror attack, to determine effective routes and assignments for evacuating a population,46 and to evaluate strategies for transporting of victims of an airport disaster to hospitals.20, 45 One large-scale agent-based simulation models all individuals in a dynamically interacting urban population after a disaster such as that caused by biological, radiological, or chemical hazards.73 Such a model can be used to investigate a variety of logistical and operational decisions, but must be interpreted in light of the large number of input assumptions required.
Some researchers have made extensive efforts when developing models to incorporate input from disaster response planners, and to build models that planners can use. For example, one spreadsheet model for planning mass dispensing and vaccination clinics was developed in collaboration with county health officials74 and made available as a tool that emergency response planners can use to automatically generate spreadsheets customized for their own needs.75, 76
3.2. Recommendations
Based on our evaluation of the included models, we propose six recommendations for best practices for modeling and reporting of public health and medical responses to disasters. Clearly, models for any purpose, disaster responses or otherwise, should be rigorous in their design, execution, and reporting. The leaders in the field of modeling health sector responses to disasters come from a wide array of disciplines (e.g., clinical medicine, public health, medical informatics, operations research). Typically, their analyses follow established guidelines for best practices in modeling and model reporting from their relevant disciplines (e.g., 6, 77). The following recommendations identify specific additional features needed for modeling health sector responses to disasters that are not always included in other standards, and represent an effort to enunciate best practices for this new field of research and action.
Health sector disaster response models differ from many models in that they are designed to support ongoing planning endeavors. These range from long-term strategic decisions to immediate-term operational decisions. Thus, they might be used at one point for pre-event planning and later for decision making during an actual response. Moreover, in contrast to published reports of cost-effectiveness analyses that provide insights into a decision problem, disaster response models often need to be used for ongoing decision making by planners who must customize models for their own needs. To complicate matters, these planners typically do not have any particular modeling expertise—a fact that has critical implications for the design and reporting of such models.
Recommendation 1. Health sector disaster response models should be designed with stakeholder input to effectively address the spectrum of relevant real-world planning and response problems
A critical aspect of any disaster response model is that it be useful for addressing the practical planning problems faced by clinicians, first responders, and public health officials. Thus, such models should be able to realistically assess the health effects of disasters and the response capabilities of the public health and health care systems. To do so, these models should be designed to address realistic scenarios with inputs based on real-world data. Where data are not available, other related data from related disasters, drills and tabletop exercises, or expert opinion could be incorporated. For such models to be useful, their results should be validated to the extent possible—for example, by comparing model outputs to observed data from relevant disasters. Disaster response models should evaluate the feasibility (e.g., implementation logistics) of alternative response strategies proposed. We advocate the early involvement of key stakeholders as part of an iterative process to support the design of realistic and useful models.
Recommendation 2. Health sector disaster response models intended for use by response planners should include a user-friendly interface, capacity to customize model inputs to suit local needs, ability to quickly and easily perform sensitivity analyses, and ongoing user support
Some highly stylized mathematical models can provide critical insights into disaster response planning; however, for many disaster response planning endeavors, ongoing decision making by end users is needed. In this case, they must be designed so that they (or appropriate end-user versions of them) can be readily used by response planners. Health sector disaster response models can play an important role in ongoing decision making, in local settings by response professionals (e.g., public health officials, physicians, emergency responders, hospital management, military planners, vaccine and pharmaceutical manufacturers, among many others) who may not be analytically trained but have considerable ground-level expertise. Thus, the input data and assumptions of models need to be clear so that planners can evaluate the relevance of model results. Models must provide results quickly and allow users to easily perform sensitivity analyses on different response scenarios. Good models will also allow users to evaluate tradeoffs in strategies (e.g., evaluating the tradeoffs between investment in local stockpiles versus the development of local dispensing capacity, or downgrading the standard of care in hospitals versus enhancing hospital surge capacity for the critically ill). Finally, the usefulness of such models is greatly enhanced when they are publicly available for use by planners, who can customize them for their own situations.
Recommendation 3. Health sector disaster response models should strike the appropriate balance between simplicity and complexity so that they adequately represent real-world scenarios, but are still useable and interpretable by intended end-users
The appropriate level of complexity is difficult to define a priori; it is a function of the planning decision being addressed and the desired level of detail of the results. For example, models designed to consider dispensing center operations may need to provide detailed results, whereas models designed to evaluate broader strategic decisions such as comparisons of treatment options may reasonably provide less detailed results. Good models will be complex enough to provide credible insights into the planning problems they were designed to address while remaining as simple and tractable as possible, thus supporting the use of such models for decision making by planners.
Recommendation 4. Health sector disaster response models should include relevant outcomes which may extend beyond those typically considered in cost-effectiveness analyses; these may include timeliness and efficiency of response, resource utilization, evacuation timing, and/or measures related to behavior of responders and the public
Unlike traditional cost-effectiveness analyses, outcomes other than morbidity, mortality, and costs may also be important in the design or evaluation of a disaster response plan. Critical outcomes of disaster response may include resource utilization (e.g., hospital capacity usage, emergency department closure rates, and transportation network congestion) and other logistical measures (e.g., bottlenecks, evacuating timing); and measures related to behavior of responders and the public (e.g., patient adherence to prophylaxis and treatment, patient self-referral patterns). Unfortunately, few well-validated metrics exist for many of these key outcomes (this is an important area of active research). It may also be important to consider longer term outcomes such as the capacity for sustained response and long-term health effects (e.g., mental health effects) since plans for sustained responses may differ from those for rapid responses. Costs may not be particularly relevant for every decision that is analyzed. Modelers should carefully consider the appropriate outcome measures to include, as well as means for validating those metrics.
Recommendation 5. Health sector disaster response models should address the fundamental uncertainties in disaster scenarios including the likelihood and magnitude of an event, operational response capabilities, supply chain capacity and robustness, behavior of responders and the public, and counter-measure effectiveness
Public health disasters are rare events that may unfold in unpredictable ways. Thus, disaster response models must be designed to allow for comprehensive sensitivity analyses of uncertain model parameters and uncertain event scenarios. A notable feature of all preparedness activity is that plans must be made and paid for now in order to improve response to a wide range of possible future events, most of which will never occur. The cost-effectiveness of a disaster response plan is often critically dependent on the probability that the disaster occurs as well as its possible magnitude. One way to evaluate the effectiveness of a specific response plan under a variety of potential disaster conditions is with scenario planning.78 Scenario planning can highlight critical aspects of disaster response plans (e.g., bottlenecks) and can assist in designing response plans with adequate capacity and redundancy. As appropriate, good response models will incorporate the uncertainties associated with human and behavioral factors. For example, it may be important to evaluate a variety of assumptions about the behavior of both the public and first responders during an event (e.g., willingness of first responders to come to work in a dangerous environment, selection of treatment facilities by the public, adherence to recommended treatment/prophylaxis, behaviors in response to evacuation orders).
Recommendation 6. Good reporting is particularly critical for health sector disaster response models. In this context, good reporting consists of, at a minimum: addressing the impetus for the study; defining critical assumptions; explaining modeling methodology; discussing key sensitivity analyses; making available public-use versions of the model; and identifying all relevant partners in model creation
Given the rarity of most disasters, the uncertainties involved in both the events and their response, and the considerable societal importance placed on effective disaster response, detailed reporting of modeling methodologies, assumptions, and data sources is essential. Good model reporting will enable planners to customize analyses for their own purposes and compare the results of different models. A flow chart describing the event sequence may be helpful for planners who are interested in implementing the model. Good reporting of disaster models also includes the presentation of sensitivity analyses that identify key uncertainties, and the development of policy statements around these results. Additionally, reports of disaster response models should include specific insights for planners, describe how the model could be applied to response scenarios other than those specifically considered, and identify model limitations and key needs for future data collection.
4. DISCUSSION
Recent large-scale disasters in the U.S. and internationally have underscored the need for effective and efficient public health and medical responses. Partly as a result of these events, the field of disaster response modeling has emerged. The growing literature of disaster response modeling includes a number of exemplary models which we present in this paper. This field differs in key ways from traditional cost-effectiveness and healthcare modeling, leading to specialized requirements for model design and reporting. These informed our six recommendations: disaster response models should 1) be designed to address real-world disaster response problems, 2) be made available (in some form) for use by planners, 3) strike an appropriate balance between computational complexity and usability, 4) evaluate relevant disaster response outcomes, which often extend beyond those considered in traditional cost-effectiveness analyses, 5) explore critical uncertainties, and 6) be presented in sufficient detail that their results can be fully interpreted.
These recommendations are intended to increase the usefulness of disaster response models. Some of these recommendations are similar to those in established standards for modeling in some areas. For example, in medical cost-effectiveness analysis, it is standard practice to explore the effects of critical uncertainties on the results of the analysis. However, this is not necessarily the case in other modeling disciplines such as logistics or operations research. Other recommendations, such as making models available for use by planners, are not widely included in any published guidelines for public health or medical modeling.
The nascent field of modeling public health responses to disasters is reminiscent of the state of medical cost-effectiveness modeling in the 1970s and 1980s: It is highly heterogeneous in terms of methodologic approaches, outcomes evaluated, and quality of presentation. This has led to different approaches in framing and analyzing the research questions. As a consequence, it is typically not possible to compare results across models—even across models that evaluate related problems (such as treatment strategies for inhalational anthrax). Just as standard guidelines have facilitated the comparison of medical cost-effectiveness models by encouraging modelers to adhere to a set of principles (e.g., the adoption of the societal perspective when appropriate, discounting both costs and benefits, etc.),6 we hope that our recommendations will similarly help to standardize approaches adopted by modelers of public health responses to disasters.
Quantitative models are essential to planning effective health sector responses to disasters. The recommendations we propose should increase the applicability and interpretability of future models, thereby improving strategic, tactical, and operational aspects of preparedness planning and response.
Acknowledgments
Grant Support: This project received no funding support.
We thank the members of the Society for Medical Decision Making for their thoughtful comments on an earlier draft of this position paper. We thank Wei Xiong and Helen-Ann Brown from Weill Medical College of Cornell University and Mary Hill-Harmon and Peter Highnam from the Biomedical Advanced Research and Development Authority of the U.S. Department of Health and Human Services for their assistance with our literature review. The authors received no funding support for this project. Margaret Brandeau is supported by grant R01-DA15612 from the National Institute on Drug Abuse.
Footnotes
Decision making can be considered strategic, tactical, or operational based on the spatial and temporal range of the decisions. For example, state officials make strategic decisions during the development of pandemic influenza response plans; county health officials make tactical decisions when procuring influenza response stockpiles based on those plans; and, during an actual response to an influenza pandemic, local health officials face the operational decisions of determining how to utilize staff and resources to most effectively respond to the emergency.
References
- 1.Braithwaite RS, Fridsma D, Roberts MS. The cost-effectiveness of strategies to reduce mortality from an intentional release of aerosolized anthrax spores. Med Decis Making. 2006 Mar-Apr;26(2):182–93. doi: 10.1177/0272989X06286794. [DOI] [PubMed] [Google Scholar]
- 2.Bravata D, McDonald K, Szeto H, et al. A conceptual framework for evaluating information technologies and decision support systems for bioterrorism preparedness and response. Med Decis Making. 2004;24(2):192–206. doi: 10.1177/0272989X04263254. [DOI] [PubMed] [Google Scholar]
- 3.Hupert N, Mushlin AI, Callahan MA. Modeling the public health response to bioterrorism: using discrete event simulation to design antibiotic distribution centers. Med Decis Making. 2002 Sep-Oct;22(5 Suppl):S17–25. doi: 10.1177/027298902237709. [DOI] [PubMed] [Google Scholar]
- 4.Zhang X, Meltzer MI, Wortley PM. FluSurge--a tool to estimate demand for hospital services during the next pandemic influenza. Med Decis Making. 2006 Nov-Dec;26(6):617–23. doi: 10.1177/0272989X06295359. [DOI] [PubMed] [Google Scholar]
- 5.Zaric GS, Bravata DM, Holty J-EC, et al. Modeling the logistics of response to anthrax bioterrorism. Med Decis Making. 2008;28:332–50. doi: 10.1177/0272989X07312721. [DOI] [PubMed] [Google Scholar]
- 6.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 7.US Department of Homeland Security. National preparedness guidelines. 2007 [cited April 3, 2008]; Available from: http://www.dhs.gov/xlibrary/assets/National_Preparedness_Guidelines.pdf.
- 8.Wilkening DA. Sverdlovsk revisited: modeling human inhalation anthrax. Proc Natl Acad Sci U S A. 2006 May 16;103(20):7589–94. doi: 10.1073/pnas.0509551103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hupert N, Cuomo J, Callahan MA, Mushlin AI, Morse SS. Prepared by Weill Medical College of Cornell University, Department of Public Health under Contract No 290-02-0013-3. Rockville, MD: Agency for Healthcare Research and Quality; Community-based mass prophylaxis: a planning guide for public health preparedness. AHRQ Pub No. 04-0044;2004. [Google Scholar]
- 10.Brookmeyer R, Johnson E, Barry S. Modelling the incubation period of anthrax. Stat Med. 2005 Feb 28;24(4):531–42. doi: 10.1002/sim.2033. [DOI] [PubMed] [Google Scholar]
- 11.Brookmeyer R, Johnson E, Bollinger R. Modeling the optimum duration of antibiotic prophylaxis in an anthrax outbreak. Proc Natl Acad Sci U S A. 2003 Aug 19;100(17):10129–32. doi: 10.1073/pnas.1631983100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halloran ME, Ferguson NM, Eubank S, et al. Modeling targeted layered containment of an influenza pandemic in the United States. Proc Natl Acad Sci U S A. 2008;105(12):4639–44. doi: 10.1073/pnas.0706849105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Federation of Red Cross and Red Crescent Societies. World Disasters Report 2008: Focus on HIV and AIDS. Geneva: International Federation of Red Cross and Red Crescent Societies; 2008. [Google Scholar]
- 14.British Red Cross. [Accessed July 8, 2008];Boxing Day tsunami, 2004: background information. 2005 http://www.redcross.org.uk/standard.asp?id=46361.
- 15.Fawcett W, Oliveira CS. Casualty treatment after earthquake disasters: development of a regional simulation model. Disasters. 2000 Sep;24(3):271–87. doi: 10.1111/1467-7717.00148. [DOI] [PubMed] [Google Scholar]
- 16.Paul JA, George SK, Yi P, Lin L. Transient modeling in simulation of hospital operations for emergency response. Prehosp Disast Med. 2006;21(3):223–36. doi: 10.1017/s1049023x00003757. [DOI] [PubMed] [Google Scholar]
- 17.Regnier E. Public evacuation decisions and hurricane track uncertainty. Manage Sci. 2008;54(1):16–28. [Google Scholar]
- 18.Beamon BM, Kotleba SA. Inventory modeling for complex emergencies in humanitarian relief operations. Int J Logistics: Res App. 2006;9(1):1–18. [Google Scholar]
- 19.Beamon BM, Kotleba SA. Inventory management support systems for emergency humanitarian relief operations in South Sudan. Int J Logistics Manage. 2006;17(2):187–212. [Google Scholar]
- 20.Inoue H, Yanagisawa S, Kamae I. Computer-simulated assessment of methods of transporting severely injured individuals in disaster--case study of an airport accident. Comput Methods Programs Biomed. 2006 Mar;81(3):256–65. doi: 10.1016/j.cmpb.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 21.Papazoglou IA, Christou MD. A decision support system for emergency response to major nuclear accidents. Nucl Technol. 1997;118(2):97–122. [Google Scholar]
- 22.Feng T, Keller LR. A multiple-objective decision analysis for terrorism protection: potassium iodide distribution in nuclear incidents. Dec Anal. 2006;3(2):76–93. [Google Scholar]
- 23.Centers for Disease Control and Prevention. FluAid 2.0. 2000 [cited April 13, 2009]; Available from: www.cdc.gov/flu/tools/fluaid.
- 24.Menon DK, Taylor BL, Ridley SA. Modelling the impact of an influenza pandemic on critical care services in England. Anaesthesia. 2005 Oct;60(10):952–4. doi: 10.1111/j.1365-2044.2005.04372.x. [DOI] [PubMed] [Google Scholar]
- 25.Sobieraj JA, Reyes J, Dunemn KN, et al. Modeling hospital response to mild and severe influenza pandemic scenarios under normal and expanded capacities. Mil Med. 2007 May;172(5):486–90. doi: 10.7205/milmed.172.5.486. [DOI] [PubMed] [Google Scholar]
- 26.Wilson N, Mansoor O, Baker M. Estimating the impact of the next influenza pandemic on population health and health sector capacity in New Zealand. N Z Med J. 2005 Mar 11;118(1211):U1346. [PubMed] [Google Scholar]
- 27.Levi L, Bregman D. Simulation and management games for training command and control in emergencies. Stud Health Technol Inform. 2003;95:783–7. [PubMed] [Google Scholar]
- 28.Levi L, Bregman D, Geva H, Revach M. Hospital disaster management simulation system. Prehosp Disaster Med. 1998 Jan-Mar;13(1):29–34. [PubMed] [Google Scholar]
- 29.Levi L, Bregman D, Geva H, Revah M. Does number of beds reflect the surgical capability of hospitals in wartime and disaster? The use of a simulation technique at a national level. Prehosp Disaster Med. 1997 Oct-Dec;12(4):300–4. [PubMed] [Google Scholar]
- 30.Kanter RK. Strategies to improve pediatric disaster surge response: potential mortality reduction and tradeoffs. Crit Care Med. 2007 Dec;35(12):2837–42. doi: 10.1097/01.CCM.0000287579.10746.43. [DOI] [PubMed] [Google Scholar]
- 31.Kanter RK, Moran JR. Pediatric hospital and intensive care unit capacity in regional disasters: expanding capacity by altering standards of care. Pediatrics. 2007 Jan;119(1):94–100. doi: 10.1542/peds.2006-1586. [DOI] [PubMed] [Google Scholar]
- 32.Earnest A, Chen MI, Ng D, Sin LY. Using autoregressive integrated moving average (ARIMA) models to predict and monitor the number of beds occupied during a SARS outbreak in a tertiary hospital in Singapore. BMC Health Serv Res. 2005 May 11;5(1):36. doi: 10.1186/1472-6963-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hupert N, Wattson D, Cuomo J, Benson S. Anticipating demand for emergency health services due to medication-related adverse events after rapid mass prophylaxis campaigns. Acad Emerg Med. 2007 Mar;14(3):268–74. doi: 10.1197/j.aem.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 34.Lee EK, Maheshwary S, Mason J, Glisson W. Decision support system for mass dispensing of medications for infectious disease outbreaks and bioterrorist attacks. Ann Oper Res. 2006;148(1):25–53. [Google Scholar]
- 35.Lee EK, Maheshwary S, Mason J, Glisson W. Large-scale dispensing for emergency response to bioterrorism and infectious-disease outbreak. Interfaces. 2006;36(6):591–607. [Google Scholar]
- 36.Germann TC, Kadau K, Longini IM, Jr, Macken CA. Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci U S A. 2006 Apr 11;103(15):5935–40. doi: 10.1073/pnas.0601266103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brandeau ML, Hutton DW, Owens DK, Bravata DM. Planning the bioterrorism response supply chain: learn and live. Am J Disaster Med. 2007;2:231–48. [PubMed] [Google Scholar]
- 38.Dekle J, Lavieri MS, Martin E, Emir-Farinas H, Francis RL. A Florida county locates disaster recovery centers. Interfaces. 2005;35(2) [Google Scholar]
- 39.Balcik B, Beamon BM. Facility location in humanitarian relief. Int J Logistics: Res App. 2008;11(2):101–21. [Google Scholar]
- 40.Whitworth MH. Designing the response to an anthrax attack. Interfaces. 2006;36(6):562–8. [Google Scholar]
- 41.Bravata DM, Zaric GS, Holty JE, et al. Reducing mortality from anthrax bioterrorism: strategies for stockpiling and dispensing medical and pharmaceutical supplies. Biosecur Bioterror. 2006;4(3):244–62. doi: 10.1089/bsp.2006.4.244. [DOI] [PubMed] [Google Scholar]
- 42.Balcik B, Beamon BA, Smilowitz K. Last mile distribution in humanitarian relief. J Intell Transp Sys. 2008;12(2):51–63. [Google Scholar]
- 43.Barbarosoğlu G, Özdamar L, Çevik A. An interactive approach for hierarchical analysis of helicopter logistics in disaster relief operations. Eur J Oper Res. 2002;140:118–33. [Google Scholar]
- 44.Jotshi A, Gong Q, Batta R. Dispatching/routing of emergency vehicles in disaster mitigation using data fusion concepts. Socioecon Plann Sci. 2008 doi: 10.1016/j.seps.2008.02.005. [DOI] [Google Scholar]
- 45.Christie PM, Levary RR. The use of simulation in planning the transportation of patients to hospitals following a disaster. J Med Syst. 1998 Oct;22(5):289–300. doi: 10.1023/a:1020521909778. [DOI] [PubMed] [Google Scholar]
- 46.Han LD, Yuan F, Chin S-M, Hwang H. Global optimization of emergency evacuation assignments. Interfaces. 2006;36(6):502–13. [Google Scholar]
- 47.Özdamar L, Ekinci E, Küçükyazici B. Emergency logistics planning in natural disasters. Ann Oper Res. 2004;129:217–45. [Google Scholar]
- 48.Barbarosoğlu G, Arda Y. A two-stage stochastic programming framework for transportation planning in disaster response. J Oper Res Soc. 2004;55:43–53. [Google Scholar]
- 49.Dombroski MJ, Fischhoff B, Fischbeck PS. Predicting emergency evacuation and sheltering behavior: a structured analytical approach. Risk Anal. 2006 Dec;26(6):1675–88. doi: 10.1111/j.1539-6924.2006.00833.x. [DOI] [PubMed] [Google Scholar]
- 50.Dombroski MJ, Fischbeck PS. An integrated physical dispersion and behavioral response model for risk assessment of radiological dispersion device (RDD) events. Risk Anal. 2006 Apr;26(2):501–14. doi: 10.1111/j.1539-6924.2006.00742.x. [DOI] [PubMed] [Google Scholar]
- 51.Georgopoulos PG, Fedele P, Shade P, et al. Hospital response to chemical terrorism: personal protective equipment, training, and operations planning. Am J Ind Med. 2004 Nov;46(5):432–45. doi: 10.1002/ajim.20075. [DOI] [PubMed] [Google Scholar]
- 52.Brandeau ML, Zaric GS, Freiesleben J, Edwards FL, Bravata DM. An ounce of prevention is worth a pound of cure: Improving communication to reduce mortality during bioterrorism responses. Am J Disaster Med. 2008;2:65–78. [PubMed] [Google Scholar]
- 53.Eichner M, Schwehm M, Duerr HP, Brockmann SO. The influenza pandemic preparedness planning tool InfluSim. BMC Infect Dis. 2007;7:17. doi: 10.1186/1471-2334-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van Genugten ML, Heijnen ML, Jager JC. Pandemic influenza and healthcare demand in the Netherlands: scenario analysis. Emerg Infect Dis. 2003 May;9(5):531–8. doi: 10.3201/eid0905.020321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Massin L, Legrand J, Valleron AJ, Flahault A. Modelling outbreak control for pneumonic plague. Epidemiol Infect. 2007 Jul;135(5):733–9. doi: 10.1017/S0950268806007345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Longini IM, Jr, Halloran ME, Nizam A, Yang Y. Containing pandemic influenza with antiviral agents. Am J Epidemiol. 2004 Apr 1;159(7):623–33. doi: 10.1093/aje/kwh092. [DOI] [PubMed] [Google Scholar]
- 57.Meltzer MI, Cox NJ, Fukuda K. The economic impact of pandemic influenza in the United States: priorities for intervention. Emerg Infect Dis. 1999 Sep-Oct;5(5):659–71. doi: 10.3201/eid0505.990507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Balicer RD, Huerta M, Davidovitch N, Grotto I. Cost-benefit of stockpiling drugs for influenza pandemic. Emerg Infect Dis. 2005 Aug;11(8):1280–2. doi: 10.3201/eid1108.041156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Siddiqui MR, Edmunds WJ. Cost-effectiveness of antiviral stockpiling and near-patient testing for potential influenza pandemic. Emerg Infect Dis. 2008;14(2):267–74. doi: 10.3201/eid1402.070478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Medema JK, Zoellner YF, Ryan J, Palache AM. Modeling pandemic preparedness scenarios: health economic implications of enhanced pandemic vaccine supply. Virus Res. 2004 Jul;103(1–2):9–15. doi: 10.1016/j.virusres.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 61.Khazeni N, Hutton DW, Garber AG, Owens DK. Working Paper. Stanford University; Stanford, CA: 2008. Cost effectiveness of antiviral prophylaxis and prime boost vaccine strategies for an influenza pandemic. [Google Scholar]
- 62.Fowler RA, Sanders GD, Bravata DM, et al. Cost-effectiveness of defending against bioterrorism: a comparison of vaccination and antibiotic prophylaxis against anthrax. Ann Intern Med. 2005 Apr 19;142(8):601–10. doi: 10.7326/0003-4819-142-8-200504190-00008. [DOI] [PubMed] [Google Scholar]
- 63.Schmitt B, Dobrez D, Parada JP, et al. Responding to a small-scale bioterrorist anthrax attack: cost-effectiveness analysis comparing preattack vaccination with postattack antibiotic treatment and vaccination. Arch Intern Med. 2007 Apr 9;167(7):655–62. doi: 10.1001/archinte.167.7.655. [DOI] [PubMed] [Google Scholar]
- 64.Gupta AG, Moyer CA, Stern DT. The economic impact of quarantine: SARS in Toronto as a case study. J Infect. 2005 Jun;50(5):386–93. doi: 10.1016/j.jinf.2004.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.American College of Physicians. Information on cost-effectiveness: An essential product of a national comparative effectiveness program. Ann Intern Med. 2008;148:956–61. doi: 10.7326/0003-4819-148-12-200806170-00222. [DOI] [PubMed] [Google Scholar]
- 66.Wein LM, Craft DL, Kaplan EH. Emergency response to an anthrax attack. Proc Natl Acad Sci U S A. 2003 Apr 1;100(7):4346–51. doi: 10.1073/pnas.0636861100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wein LM, Craft DL. Evaluation of public health interventions for Anthrax: a report to the secretary’s council on Public Health Preparedness. Biosecur Bioterror. 2005;3(4):348–56. doi: 10.1089/bsp.2005.3.348. [DOI] [PubMed] [Google Scholar]
- 68.Craft DL, Wein LM, Wilkins AH. Analyzing bioterror response logistics: the case of anthrax. Manage Sci. 2005;51(5):679–92. [Google Scholar]
- 69.Talmor D, Jones AE, Rubinson L, Howell MD, Shapiro NI. Simple triage scoring system predicting death and the need for critical care resources for use during epidemics. Crit Care Med. 2007 May;35(5):1251–6. doi: 10.1097/01.CCM.0000262385.95721.CC. [DOI] [PubMed] [Google Scholar]
- 70.Meltzer MI, Damon I, LeDuc JW, Millar JD. Modeling potential responses to smallpox as a bioterrorist weapon. Emerg Infect Dis. 2001 Nov-Dec;7(6):959–69. doi: 10.3201/eid0706.010607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Glasser JW, Foster SO, Millar JD, Lane JM. Evaluating public health responses to reintroduced smallpox via dynamic, socially structured, and spatially distributed metapopulation models. Clin Inf Dis. 2008;46(Suppl 3):S182–94. doi: 10.1086/524382. [DOI] [PubMed] [Google Scholar]
- 72.Kaplan EH, Craft DL, Wein LM. Analyzing bioterror response logistics: the case of smallpox. Math Biosci. 2003 Sep;185(1):33–72. doi: 10.1016/s0025-5564(03)00090-7. [DOI] [PubMed] [Google Scholar]
- 73.Narzisi G, Mincer JS, Smith S, Mishra B. Resilience in the face of disaster: Accounting for varying disaster magnitudes, resource topologies, and (sub)population distributions in the PLAN C emergency planning tool. In: Marik V, Vyatkin V, Colombo AW, editors. Holonic and Multiagent Systems for Manufacturing 2007, LNAI 4569. Berlin: Springer-Verlag; 2007. pp. 433–46. [Google Scholar]
- 74.Aaby K, Herrmann JW, Jordan CS, Treadwell M, Wood K. Montgomery County’s public health service uses operations research to plan emergency mass dispensing and vaccination clinics. Interfaces. 2006;36(6):569–79. [Google Scholar]
- 75.Herrmann JW. Disseminating emergency preparedness planning models as automatically generated custom spreadsheets. Interfaces. 2008;38(4):263–70. [Google Scholar]
- 76.University of Maryland and the Advanced Practice Center for Public Health Emergency Preparedness and Response of Montgomery County M. Software for improving mass dispensing and vaccination clinic operations. 2008 [cited April 13, 2009]; Available from: http://www.isr.umd.edu/Labs/CIM/projects/clinic/software.html.
- 77.Hillier FS, Lieberman GJ. Introduction to operations research. 8. New York: McGraw-Hill; 2005. [Google Scholar]
- 78.Wilson I, Ralston WK., Jr . Scenario planning handbook: Developing strategies in uncertain times. Boston, MA: South-Western Educational Publishing; 2006. [Google Scholar]
- 79.Brookmeyer R, Johnson E, Bollinger R. Public health vaccination policies for containing an anthrax outbreak. Nature. 2004 Dec 16;432(7019):901–4. doi: 10.1038/nature03087. [DOI] [PubMed] [Google Scholar]
- 80.Colizza V, Barrat A, Barthelemy M, Valleron AJ, Vespignani A. Modeling the worldwide spread of pandemic influenza: baseline case and containment interventions. PLoS Med. 2007 Jan;4(1):e13. doi: 10.1371/journal.pmed.0040013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lloyd-Smith JO, Galvani AP, Getz WM. Curtailing transmission of severe acute respiratory syndrome within a community and its hospital. Proc Biol Sci. 2003 Oct 7;270(1528):1979–89. doi: 10.1098/rspb.2003.2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lipsitch M, Cohen T, Cooper B, et al. Transmission dynamics and control of severe acute respiratory syndrome. Science. 2003 Jun 20;300(5627):1966–70. doi: 10.1126/science.1086616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kaplan EH, Craft DL, Wein LM. Emergency response to a smallpox attack: the case for mass vaccination. Proc Natl Acad Sci U S A. 2002 Aug 6;99(16):10935–40. doi: 10.1073/pnas.162282799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Miller G, Randolph S, Patterson JE. Responding to bioterrorist smallpox in San Antonio. Interfaces. 2006;36(6):580–90. [Google Scholar]
- 85.Porco TC, Holbrook KA, Fernyak SE, et al. Logistics of community smallpox control through contact tracing and ring vaccination: a stochastic network model. BMC Public Health. 2004 Aug 6;4:34. doi: 10.1186/1471-2458-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Riley S, Ferguson NM. Smallpox transmission and control: spatial dynamics in Great Britain. Proc Natl Acad Sci U S A. 2006 Aug 15;103(33):12637–42. doi: 10.1073/pnas.0510873103. [DOI] [PMC free article] [PubMed] [Google Scholar]