Abstract
Aims/hypothesis
The aim of our study was to identify subgroups of patients attending the Scottish Diabetic Retinopathy Screening (DRS) programme who might safely move from annual to two yearly retinopathy screening.
Methods
This was a retrospective cohort study of screening data from the DRS programme collected between 2005 and 2011 for people aged ≥12 years with type 1 or type 2 diabetes in Scotland. We used hidden Markov models to calculate the probabilities of transitions to referable diabetic retinopathy (referable background or proliferative retinopathy) or referable maculopathy.
Results
The study included 155,114 individuals with no referable diabetic retinopathy or maculopathy at their first DRS examination and with one or more further DRS examinations. There were 11,275 incident cases of referable diabetic eye disease (9,204 referable maculopathy, 2,071 referable background or proliferative retinopathy). The observed transitions to referable background or proliferative retinopathy were lower for people with no visible retinopathy vs mild background retinopathy at their prior examination (respectively, 1.2% vs 8.1% for type 1 diabetes and 0.6% vs 5.1% for type 2 diabetes). The lowest probability for transitioning to referable background or proliferative retinopathy was among people with two consecutive screens showing no visible retinopathy, where the probability was <0.3% for type 1 and <0.2% for type 2 diabetes at 2 years.
Conclusions/interpretation
Transition rates to referable diabetic eye disease were lowest among people with type 2 diabetes and two consecutive screens showing no visible retinopathy. If such people had been offered two yearly screening the DRS service would have needed to screen 40% fewer people in 2009.
Electronic supplementary material
The online version of this article (doi:10.1007/s00125-013-2928-7) contains peer reviewed but unedited supplementary material, which is available to authorised users.
Keywords: Diabetes, Diabetic retinopathy, Maculopathy, Retinal screening, Screening intervals
Introduction
Regular screening for proliferative retinopathy is recommended for people with diabetes, as laser treatment can prevent vision loss [1]. The Scottish Diabetic Retinopathy Screening (DRS) programme achieved national coverage in 2006 with the goal of annual screening of all people aged ≥12 years with diabetes [2]. The key objective of the service is to allow intervention with laser in patients with proliferative retinopathy before sight is affected by vitreous haemorrhage or retinal detachment. Retinal photographs are not discriminatory for proliferative retinopathy or its precursors and so will also reveal signs of maculopathy. The economic case for screening for diabetic macular oedema, however, has not to date met the WHO criteria for systematic screening [3]. Despite this, more patients are referred from the DRS to specialist ophthalmology care with suspected diabetic macular oedema (maculopathy) than with suspected proliferative retinopathy. Furthermore, the two groups of patients are managed differently. Patients with proliferative retinopathy, even those with normal vision, are offered laser treatment, whereas patients with macular oedema are increasingly only offered treatment if they have symptomatic visual loss. This is because laser cannot restore vision but, and perhaps equally important, once treatment for proliferative retinopathy has been completed it does not need repeating, whereas emerging treatment for macular oedema will restore vision in many, but at the cost of indefinite monthly intraocular injections [4, 5].
In the year April 2010 to March 2011 the DRS programme examined 174,582 people (85% of the eligible population) [6]. However, the prevalence of diabetes is continuing to increase in Scotland (as in other parts of the world) by an average of 4.2% per annum [7]. This increasing demand requires a greater efficiency of current screening practices including, amongst others, an optimal screening interval for attendees.
Other groups have published on the subject of retinal screening intervals. Iceland [8] and Sweden [9] have both reported on their positive experiences of switching individuals without evidence of retinopathy to longer screening intervals. Recent publications from Iceland and Denmark using modelling approaches to determine individualised screening intervals suggested screening intervals incorporating a variety of measures beyond type and duration, such as HbA1c, blood pressure and diabetes treatment ranging from 6 months to 5 years [8, 10]. Data from the Welsh [11] and English [12–14] diabetic retinopathy screening programmes also support a move to lengthening the screening interval for individuals without retinopathy.
The aim of this study was to use DRS programme data to model the 1 and 2 year transition rates between the various states of retinopathy, to establish the transition rates for specific subgroups of the population screened according to sex, diabetes duration and type of diabetes, and to establish whether there are subgroups of the population at very low risk of transition to the referable state of retinopathy in a 2 year interval.
Methods
The data used were from a pseudo-anonymised extract from May 2008 of the Scottish Care Information–Diabetes Collaboration (SCI-DC), a clinical diabetes information system which automatically collates clinical data from people diagnosed with diabetes in Scotland [15] and which has a current estimated coverage of >99%. Ethical approval was obtained from the Scotland A Research Ethics Committee, the Caldicott (data privacy) Guardians for the 14 Scottish health boards, and the National Health Service Information Services Division Privacy Advisory Committee.
Eligible individuals (aged ≥12 years with a diagnosis of diabetes and without suspensions) registered on SCI-DC are invited either 6 monthly or annually to participate in the DRS programme depending on the results at their previous screening examination as described previously [16]. Since 2008, the DRS programme has consistently screened >80% of the eligible population each year [6].
The Scottish grading system [17] classifies background diabetic retinopathy, and thus the risk of progressing to proliferative retinopathy, separately from the presence of maculopathy. There are four possible outcomes from grading: (1) recall for a slit-lamp examination as the photographs are ungradable; (2) recall in 12 months if the patient has no visible retinopathy or only mild background retinopathy; (3) recall in 6 months if the patient has observable background retinopathy or observable background maculopathy; and (4) referral to ophthalmology if the patient has proliferative retinopathy, referable background retinopathy or referable maculopathy. Actions are determined by the finding in the worst eye. For this analysis we excluded examinations which resulted in ungradable images. Slit-lamp examination outcomes were not available for all health boards for the whole time course of the study, but where slit-lamp data were available they were included in the results.
The primary interest in the study was defined as transition rate to any referable disease (which includes referable background and proliferative retinopathy, and those with referable maculopathy). We performed subanalyses according to the primary aim of retinal screening (the early detection of people who have, or who are at risk of developing, proliferative retinopathy), i.e. referable background or proliferative retinopathy (‘referable retinopathy’).
Study population
This study was restricted to individuals with type 1 or type 2 diabetes diagnosed prior to 31 May 2008. Individuals were included only if they had an initial DRS examination which showed that the worst eye had no visible retinopathy, mild background retinopathy, observable background retinopathy or observable maculopathy, and at least one subsequent DRS examination. For baseline covariate data, to describe the included population, we selected the measure from SCI-DC taken nearest to the initial screening examination for BMI (kg/m2), HbA1c (% and mmol/mol), systolic and diastolic blood pressure (mmHg). In order to limit missing covariate data while retaining a temporal relationship between measure and screening we used a series of cut-points for time between screening and covariate measure (HbA1c ±180 days, blood pressure ±90 days and BMI ±1,085 days.)
Statistical methods
For comparison of baseline variables we used multiple linear and logistic regression models. All statistical analyses were undertaken using the R statistical package [18].
Multi-state modelling
The DRS data consist of observations of a continuous-time process (the progression of retinopathy) at arbitrary times (i.e. at screening visits) and with measurements that may not always perfectly reflect the underlying pathology at the retina (i.e. disease may be invisible to the naked eye/photography or misgraded by retinal photography). Our objective was to model the so-called transition intensity between the four observed states of no visible retinopathy, mild background retinopathy, observable disease and referable disease as defined above. We therefore fitted a hidden Markov model with misclassification to the data using the msm package for R [19] and examined the effect of individual level covariates on the transition intensities between states. We then reported the model-based probabilities of observing a transition to referable disease states in the ensuing 1 and 2 year periods according to diabetes type, sex, diabetes duration and observed retinal photograph grade at the current screening examination, as all these characteristics were shown to influence transition intensities and were available to the DRS at the time of screening. The electronic supplementary material (ESM) gives more information on msm model methods. From the fitted model, the probabilities of the reported retinopathy states at screening after any specified time interval can be calculated for any individual, given the observations so far and the covariates for that individual. We repeated the analysis of this four-state model with a five-state model in which we further separated out referable background or proliferative retinopathy and referable maculopathy into two states.
Results
There were 184,621 people with at least one successful DRS examination between October 2005 and November 2011 (the latest date for which data were available). From these we selected those who did not have referable disease at their first screening and who were evaluable for progression (n = 155,114; 84.0%). The median number (interquartile range [IQR]) of examinations included in this study was four (IQR three to five), with a median interval between successful examinations of 12.7 months (IQR 12.1–13.9 months) (ESM Table 1).
Among those included in the analysis, the degree of retinopathy at the initial DRS examination was related to a number of factors including sex, age, diabetes duration, glycaemia and blood pressure (Table 1). Median time between screening and measures of blood pressure, HbA1c and BMI were 32, 51 and 148 days, respectively. Overall, relationships shown were not affected by time between screening and measurement of covariates, though if the interval was limited to within 30 days associations between blood pressure and retinopathy grades were no longer statistically significantly different.
Table 1.
Baseline demographics by initial retinopathy grade and diabetes type
| Variable | No visible retinopathy | Mild background retinopathy | Observable retinopathy or maculopathy | p value* (no visible retinopathy vs mild background retinopathy) | p value* (no visible retinopathy vs observable retinopathy or maculopathy) |
|---|---|---|---|---|---|
| Type 1 | 7,869 (40.7%) | 7,427 (38.4%) | 784 (4.1%) | ||
| Male sex | 4,131 (52.5%) | 4,150 (55.9%) | 442 (56.4%) | <0.0001 | 0.0415 |
| Age (years) | 33.7 ± 17.1 | 41.7 ± 14.8 | 43.4 ± 13.1 | <0.0001 | <0.0001 |
| Diabetes duration (years) | 7.1 (3.0–13.5) | 18.8 (11.5–28.6) | 20.8 (15.3–27.4) | <0.0001 | <0.0001 |
| HbA1c | <0.0001 | <0.0001 | |||
| % | 8.6 ± 1.8 | 8.7 ± 1.6 | 9.2 ± 1.6 | ||
| mmol/mol | 70.4 ± 19.6 | 71.8 ± 17.3 | 76.8 ± 17.4 | ||
| Systolic blood pressure (mmHg) | 126.5 ± 17.2 | 130.2 ± 17.2 | 132.4 ± 17.9 | <0.0001 | <0.0001 |
| Diastolic blood pressure (mmHg) | 73.8 ± 10.4 | 74.6 ± 9.9 | 76.3 ± 10.4 | 0.0048 | <0.0001 |
| BMI (kg/m2) | 25.7 ± 5.5 | 27.0 ± 5.0 | 27.6 ±5.2 | <0.0001 | <0.0001 |
| Type 2 | 101,539 (68.5%) | 35,227 (23.8%) | 2,268 (1.5%) | ||
| Male sex | 55,172 (54.3%) | 20,407 (57.9%) | 1,298 (57.2%) | <0.0001 | 0.0066 |
| Age (years) | 64.4 ± 11.8 | 64.6 ± 11.6 | 65.1 ± 11.2 | 0.0008 | 0.0024 |
| Diabetes duration (years) | 4.1 (1.6–7.5) | 6.9 (3.2–12.0) | 11.4 (6.4–16.5) | <0.0001 | <0.0001 |
| HbA1c | <0.0001 | <0.0001 | |||
| % | 7.3 ± 1.5 | 7.6 ± 1.6 | 8.1 ± 1.8 | ||
| mmol/mol | 56.7 ± 16.1 | 59.9 ± 17.3 | 64.8 ± 19.5 | ||
| Systolic blood pressure (mmHg) | 135.0 ± 16.2 | 137.0 ± 17.3 | 138.6 ± 18.5 | <0.0001 | <0.0001 |
| Diastolic blood pressure (mmHg) | 76.3 ± 9.9 | 76.0 ± 10.2 | 75.6 ± 10.5 | 0.0003 | 0.0184 |
| BMI (kg/m2) | 31.6 ± 6.4 | 31.4 ± 6.3 | 31.4 ± 6.2 | 0.1744 | 0.6282 |
Data are means ± SD except for sex (n with percentage) and diabetes duration (median with IQR)
*p values computed by multiple logistic regression and controlled for sex and age, except for sex where p value was calculated using χ 2 test
Observed transitions
Overall, there were 11,275 cases of incident referable disease in the study, of which 2,071 (18.4%) were due to the presence of referable retinopathy; the remaining 9,204 (81.6%) were due to referable maculopathy. Of the cases of referable maculopathy, 526 (5.7%) were associated with the observable background retinopathy grade, whereas the rest had either no visible retinopathy or mild background retinopathy.
ESM Table 2 shows the frequency of the various states by year of screening examination. There was a slightly higher yield of referable cases in year 1, but in subsequent years the percentage with referable disease was stable year on year at ∼5% for people with type 1 diabetes and ∼2% for people with type 2 diabetes.
We calculated progression for both the ‘any referable disease’ and ‘referable retinopathy’ endpoints. As referable maculopathy accounted for the majority of the cases of referable disease, the risk of progression to referable retinopathy was always substantially lower for any given diabetes type, sex and duration. The percentage of those transitioning between all possible consecutive examination pairs during the entire follow-up period is summarised in Table 2. As expected, the proportion transitioning to referable disease from no visible retinopathy was far lower than for those with mild background diabetic retinopathy (0.6% vs 5.1% for any referable disease in type 2 diabetes), whereas >20% of individuals with observable retinopathy or maculopathy transitioned to any referable disease at their next examination. Of note, there was also a striking amount of regression, particularly at lower degrees of retinopathy. For example, 18.2% of people with type 1 diabetes and 36.4% of people with type 2 diabetes transitioned from mild background retinopathy to no visible retinopathy at their subsequent examination.
Table 2.
Observed transitions between states of retinopathy among diabetic patients undergoing retinal screening in the DRS programme
| State at prior assessment | State at next assessment | Total pairs | ||||
|---|---|---|---|---|---|---|
| No visible retinopathy n (%) | Mild background retinopathy n (%) | Observable retinopathy or maculopathy n (%) | Referable maculopathy n (%) | Referable background or proliferative retinopathy n (%) | ||
| Type 1 | ||||||
| No visible retinopathy | 17,112 (76.5) | 4,852 (21.7) | 127 (0.6) | 200 (0.9) | 66 (0.3) | 22,357 (100) |
| Mild background retinopathy | 3,950 (18.2) | 14,912 (68.8) | 1,059 (4.9) | 1,374 (6.3) | 386 (1.8) | 21,681 (100) |
| Observable retinopathy or maculopathy | 78 (3.0) | 834 (32.1) | 1,056 (40.7) | 483 (18.6) | 144 (5.5) | 2,595 (100) |
| Total | 21,140 (45.3) | 20,598 (44.2) | 2,242 (4.8) | 2,057 (4.4) | 596 (1.3) | |
| Type 2 | ||||||
| No visible retinopathy | 258,326 (85.9) | 39,888 (13.3) | 716 (0.2) | 1,605 (0.5) | 282 (0.1) | 300,817 (100) |
| Mild background retinopathy | 37,912 (36.4) | 58,339 (56.0) | 2,617 (2.5) | 4,457 (4.3) | 808 (0.8) | 104,133 (100) |
| Observable retinopathy or maculopathy | 773 (11.7) | 2,367 (35.7) | 2,024 (30.5) | 1,085 (16.4) | 385 (5.8) | 6,634 (100) |
| Total | 297,011 (72.2) | 100,594 (24.4) | 5,357 (1.3) | 7,147 (1.7) | 1,475 (0.4) | |
Distribution of observed results from pairs of consecutive examinations
To allow a simple graphical presentation of transitions, the percentages transitioning to various states from a given state over just the first three consecutive examinations are shown in ESM Fig. 1a–f.
Probability of progression
Fitting the hidden Markov model yielded estimates of the rates at which the underlying disease states and the observed states differed, and the rates at which these states regressed, given the modelling assumption that transitions between these states arose from a Markov process and that the ‘referable’ states did not regress. The transition intensity matrix and emission matrix from the model are shown in ESM Tables 3 and 4 for type 1 diabetes and ESM Tables 5 and 6 for type 2 diabetes. The relationship between the retinopathy grades and the hidden states in the Markov model is detailed in the ESM data file.
For both type 1 and type 2 diabetes, the risk of progression increased with the degree of retinopathy at last screening (Table 3 for type 1 diabetes and Table 4 for type 2 diabetes). The risk of progression at any given duration and retinopathy grade was also consistently higher for people with type 1 diabetes than for people with type 2 diabetes. For type 1 diabetes, men had a higher risk than women at each duration and retinopathy category, but for type 2 diabetes the risk estimates were similar for men and women. For type 1 diabetes, the effect of duration was marked for up to 10 years, after which duration had little effect on risk estimates. People with a state of no visible retinopathy at their last screening represented a group at low risk of 2 year progression to any referable disease or referable retinopathy in a 2 year interval. For example, at a duration of 10 years men with no visible retinopathy and type 2 diabetes had a risk of progression to any referable disease of 0.27% at 1 year and 0.91% at 2 years, with the corresponding risks for referable retinopathy of 0.05% and 0.16%.
Table 3.
Probability of referable disease and referable background retinopathy or proliferative retinopathy at screening intervals of 1 or 2 years, by sex, diabetes duration and current retinopathy grade in those with type 1 diabetes
| Current grading | Type 1 diabetes duration (years) | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Probability of any referable disease (%) | Probability of referable retinopathy (%) | Probability of any referable disease (%) | Probability of referable retinopathy (%) | ||||||
| 1 year interval | 2 year interval | 1 year interval | 2 year interval | 1 year interval | 2 year interval | 1 year interval | 2 year interval | ||
| No visible retinopathy | 0 | – | – | – | – | – | – | – | – |
| 5 | 0.43 | 1.34 | 0.09 | 0.30 | 0.33 | 0.96 | 0.07 | 0.21 | |
| 10 | 0.51 | 1.88 | 0.11 | 0.42 | 0.44 | 1.59 | 0.10 | 0.36 | |
| 15 | 0.51 | 1.94 | 0.11 | 0.43 | 0.45 | 1.71 | 0.10 | 0.39 | |
| Mild background retinopathy | 0 | – | – | – | – | – | – | – | – |
| 5 | 5.92 | 10.00 | 1.31 | 2.22 | 4.84 | 7.56 | 1.08 | 1.68 | |
| 10 | 7.32 | 14.40 | 1.64 | 3.23 | 6.66 | 12.90 | 1.50 | 2.90 | |
| 15 | 7.49 | 15.30 | 1.68 | 3.43 | 6.97 | 14.20 | 1.57 | 3.21 | |
Referable disease: referable maculopathy, referable background retinopathy and proliferative retinopathy; referable retinopathy: referable background retinopathy and proliferative retinopathy
Table 4.
Probability of referable disease and referable background retinopathy or proliferative retinopathy at screening intervals of 1 or 2 years, by sex, diabetes duration and current retinopathy grade in those with type 2 diabetes
| Current grading | Type 2 diabetes duration (years) | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Probability of any referable disease (%) | Probability of referable retinopathy (%) | Probability of any referable disease (%) | Probability of referable retinopathy (%) | ||||||
| 1 year interval | 2 year interval | 1 year interval | 2 year interval | 1 year interval | 2 year interval | 1 year interval | 2 year interval | ||
| No visible retinopathy | 0 | 0.15 | 0.40 | 0.03 | 0.07 | 0.15 | 0.37 | 0.03 | 0.06 |
| 5 | 0.21 | 0.67 | 0.04 | 0.11 | 0.24 | 0.70 | 0.04 | 0.12 | |
| 10 | 0.27 | 0.91 | 0.05 | 0.16 | 0.31 | 1.03 | 0.05 | 0.18 | |
| 15 | 0.30 | 1.10 | 0.05 | 0.19 | 0.37 | 1.31 | 0.06 | 0.22 | |
| Mild background retinopathy | 0 | 2.79 | 4.43 | 0.47 | 0.75 | 2.52 | 5.59 | 0.43 | 0.63 |
| 5 | 4.08 | 7.41 | 0.69 | 1.26 | 4.06 | 6.96 | 0.69 | 1.19 | |
| 10 | 5.10 | 10.20 | 0.87 | 1.74 | 5.43 | 10.40 | 0.93 | 1.78 | |
| 15 | 5.80 | 12.20 | 0.99 | 2.08 | 6.43 | 13.20 | 1.09 | 2.25 | |
Referable disease: referable maculopathy, referable background retinopathy and proliferative retinopathy; referable retinopathy: referable background retinopathy and proliferative retinopathy
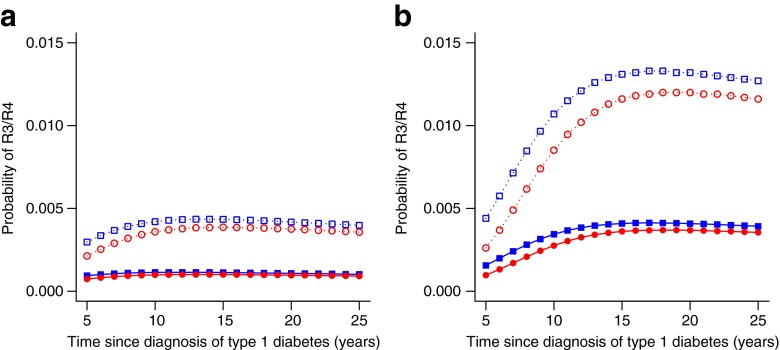
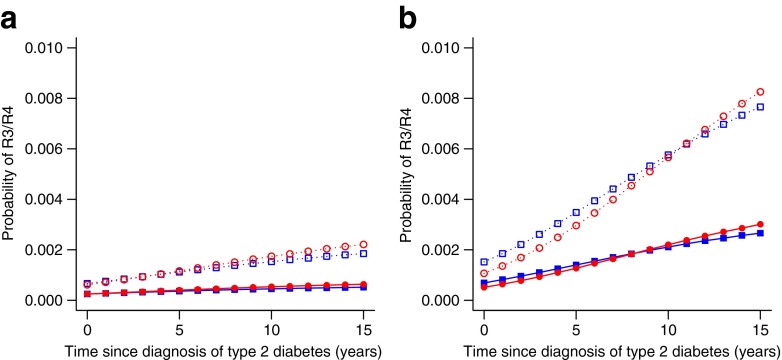
Figure 1a shows the probabilities of developing referable retinopathy at either 1 or 2 year screening intervals by sex for people with type 1 diabetes over a range of diabetes durations if the current state was no visible retinopathy. By contrast, the risks for the subset who had mild background retinopathy at the examination prior to a grade of no visible retinopathy are shown in Fig. 1b and were clearly greater at all diabetes durations. The same was true for type 2 diabetes (Fig. 2a,b). The probabilities of progression for those with no visible retinopathy at the current and previous examination are shown in Table 5 for type 1 diabetes and Table 6 for type 2 diabetes. The lowest risk stratum for both types of diabetes was those with a current and previous state of no visible retinopathy. These patients had a very low probability of referable disease or referable retinopathy in a 2 year interval regardless of diabetes duration.
Fig. 1.
Transition probabilities to referable background retinopathy (R3) or proliferative retinopathy (R4) from no visible retinopathy by sex and diabetes duration in type 1 diabetes for 1 or 2 yearly screening intervals when last screening showed no visible retinopathy (a) and when last screening showed no visible retinopathy but previous screening showed mild background retinopathy (b). Blue filled squares, men with 1 year screening interval; blue open squares, men with 2 year screening interval; red filled circles, women with 1 year screening interval; red open circles, women with 2 year screening interval
Fig. 2.
Transition probabilities to referable background retinopathy (R3) or proliferative retinopathy (R4) from no visible retinopathy by sex and diabetes duration in type 2 diabetes for 1 or 2 yearly screening intervals when last screening showed no visible retinopathy (a) and when last screening showed no visible retinopathy but previous screening showed mild background retinopathy (b). Blue filled squares, men with 1 year screening interval; blue open squares, men with 2 year screening interval; red filled circles, women with 1 year screening interval; red open circles, women with 2 year screening interval
Table 5.
Probability of referable disease and referable background retinopathy or proliferative retinopathy at screening intervals of 1 or 2 years, by sex, diabetes duration and previous and current retinopathy grade in those with type 1 diabetes
| Previous and current grading | Type 1 diabetes duration (years) | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Probability of any referable disease (%) | Probability of referable retinopathy (%) | Probability of any referable disease (%) | Probability of referable retinopathy (%) | ||||||
| 1 year interval | 2 year interval | 1 year interval | 2 year interval | 1 year interval | 2 year interval | 1 year interval | 2 year interval | ||
| No visible retinopathy, no visible retinopathy | 0 | – | – | – | – | – | – | – | – |
| 5 | 0.19 | 0.81 | 0.04 | 0.18 | 0.14 | 0.56 | 0.03 | 0.13 | |
| 10 | 0.24 | 1.13 | 0.05 | 0.25 | 0.20 | 0.93 | 0.04 | 0.21 | |
| 15 | 0.24 | 1.16 | 0.05 | 0.26 | 0.21 | 0.99 | 0.05 | 0.22 | |
| Mild background retinopathy, no visible retinopathy | 0 | – | – | – | – | – | – | – | – |
| 5 | 0.70 | 1.98 | 0.16 | 0.44 | 0.43 | 1.17 | 0.10 | 0.26 | |
| 10 | 1.54 | 4.75 | 0.34 | 1.07 | 1.22 | 3.75 | 0.28 | 0.85 | |
| 15 | 1.84 | 5.84 | 0.41 | 1.31 | 1.60 | 5.13 | 0.36 | 1.16 | |
Referable disease: referable maculopathy, referable background retinopathy and proliferative retinopathy; referable retinopathy: referable background retinopathy and proliferative retinopathy
Table 6.
Probability of referable disease and referable background retinopathy or proliferative retinopathy at screening intervals of 1 or 2 years, by sex, diabetes duration and previous and current retinopathy grade in those with type 2 diabetes
| Previous and current grading | Type 2 diabetes duration (years) | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Probability of any referable disease (%) | Probability of referable retinopathy (%) | Probability of any referable disease (%) | Probability of referable retinopathy (%) | ||||||
| 1 year interval | 2 year interval | 1 year interval | 2 year interval | 1 year interval | 2 year interval | 1 year interval | 2 year interval | ||
| No visible retinopathy, no visible retinopathy | 0 | 0.07 | 0.24 | 0.01 | 0.04 | 0.07 | 0.24 | 0.01 | 0.04 |
| 5 | 0.11 | 0.41 | 0.02 | 0.07 | 0.12 | 0.45 | 0.02 | 0.08 | |
| 10 | 0.13 | 0.57 | 0.02 | 0.10 | 0.17 | 0.68 | 0.03 | 0.12 | |
| 15 | 0.16 | 0.69 | 0.03 | 0.12 | 0.20 | 0.87 | 0.03 | 0.15 | |
| Mild background retinopathy, no visible retinopathy | 0 | 0.40 | 0.91 | 0.07 | 0.15 | 0.30 | 0.64 | 0.05 | 0.11 |
| 5 | 0.82 | 2.08 | 0.14 | 0.35 | 0.75 | 1.78 | 0.13 | 0.30 | |
| 10 | 1.23 | 3.42 | 0.21 | 0.58 | 1.29 | 3.38 | 0.22 | 0.57 | |
| 15 | 1.55 | 4.55 | 0.27 | 0.77 | 1.76 | 4.92 | 0.30 | 0.83 | |
Referable disease: referable maculopathy, referable background retinopathy and proliferative retinopathy; referable retinopathy: referable background retinopathy and proliferative retinopathy
Discussion
Potential loss of vision remains a major concern for people with diabetes. Retinal screening programmes aim to enable ophthalmic assessment and treatment to be focused on those most at risk of future sight loss. This is particularly important for proliferative retinopathy, which is asymptomatic until vitreous haemorrhage or retinal detachment occur. At the outset of retinal screening programmes in the UK a 12 monthly screening interval was selected empirically [2, 20, 21], reflecting the hospital diabetes clinic tradition of annual review for people with diabetes. Contemporary data derived from screening programmes have been used to define more optimal/individualised screening intervals [8–14, 22, 23]. Here we report the largest and most comprehensive study to date. We show that men and women with type 2 diabetes and no visible retinopathy at their last screening have a low risk of developing referable retinopathy within a 1 year (≤0.06%) or 2 year screening interval (≤0.22%). If two consecutive screenings showed no visible retinopathy, the risks were even lower (≤0.03% after a 1 year interval and ≤0.15% after a 2 year interval even with a diabetes duration of 15 years). For a given screen finding of no visible retinopathy, prior evidence of any retinopathy increased the rate of transition to referable disease in a 2 year interval approximately sixfold, although it remained low in absolute terms. This is not surprising as, although discrepancies between the observed and underlying true state may occur through confusion with photographic artefacts and the variability of human performance, the changes in the retina that can be captured on photograph will not always show the damage occurring within the retina. For instance, capillary occlusion will cause microaneurysms to thrombose followed by resorption of local haemorrhage or exudate, and while capillary occlusion is visible on fluorescein angiography it is not visible on retinal photographs or to the naked eye. Transition to referable disease in a 2 year interval was higher in those with longer duration of type 2 diabetes and in those with type 1 diabetes.
The primary strength of this study is that it uses data from a national diabetic retinopathy screening service which includes longitudinal screening data for 155,114 people with type 1 or type 2 diabetes. This makes it the largest study to address the interval rates of disease to date. The DRS also uses a centralised quality-controlled grading system, and the criteria for referable disease have not altered over the course of the programme. The choice of the hidden Markov model approach used here was also flexible enough to allow for inevitable imperfections inherent in using retinal photographs to assess retinopathy and maculopathy, and for covariate effects on the rate of progression of retinopathy. We believe this is a better approach than use of life tables, Cox proportional hazards models or interval censored survival analysis because it captures both up and down transitions of disease states which our data show are clearly occurring. The modelling approach was also flexible enough to allow for misclassified observations and covariate effects on the rate of progression of retinopathy. For this analysis we excluded examinations which resulted in an ungraded image: over the course of the study 9,585 individuals had an ungraded image (6.2% of study participants with ungraded images), accounting for only 1.6% of screening episodes in the study period. Thus, we do not think that excluding these examinations greatly affected our findings.
Weaknesses of the study are that we do not as yet have sufficient follow-up in the national programme to fully examine the implications of extending screening intervals beyond 2 years. Another potential weakness is that we do not know the retinal status of patients prior to the first screening episode within the DRS programme, which, as we show, may influence subsequent risk. The msm package also has some limitations. The fitting algorithm converges only to a local mode of the likelihood: with different starting values slightly different solutions are obtained. We specified starting values that allowed the model to find a solution that could be interpreted as a ‘misclassification’ model, in which the observed scores roughly corresponded to the hidden states with error. In practice, however, different starting values gave similar risk predictions even though the underlying model variables were different.
We have chosen initially to provide results based on a limited set of clinical data available to the DRS programme. It is possible that further refinements of risk of progression and thus safe screening interval can be determined by adding additional clinical data, for example on diabetes control, treatment regimen and other comorbidities such as hypertension. Use of additional covariate data could allow us to determine more ‘personalised’ screening intervals but would not be possible to implement without direct connectivity of the DRS programme database to the clinical diabetes database, which is not currently feasible.
One of the key questions to address when determining an optimal screening window is what level of interval disease is acceptable and this is to some extent arbitrary. The mean grading sensitivity of the DRS programme in 2010 was 91.1% (SD 4.3) [24]. The annual referral rate for eye clinic review is between 3.5% and 4.0% [25, 26]. Estimates of annual screening rates for sight-threatening retinopathy from elsewhere in the UK among individuals without retinopathy at baseline are low, ranging from 0.01% [14] to 0.3% [12, 13]. We have shown here that in a group with no visible disease at their two most recent screenings the probability of referable disease (both maculopathy and retinopathy) in a 2 year screening interval is low. Our findings suggest that those with no visible retinopathy in both their current and previous screening could be considered for extending to 2 year screening intervals. Implementing a rule of requiring two consecutive examinations with no visible retinopathy before switching to a 2 year interval would mean that 40% of all people screened in 2008 would have been eligible to shift, with a reduction of 51,278 screening examinations in 2009 and thus more efficient use of resources. If we use the less stringent rule of having only the last screening examination finding of no visible retinopathy, 63% of people screened in 2008 would have switched to 2 yearly screening, with a reduction of 81,230 screening examinations in 2009. However, whilst overall rates of incident disease in this subgroup are low, the rates at 2 years are higher than at annual screening and alteration in the screening interval will ultimately require consideration of the ‘acceptable’ absolute rate of interval disease, especially for proliferative retinopathy, as well as other factors such as cost–benefits. In particular we should consider the possible impact of reduced clinical contact and opportunities to use detection of non-referable retinopathy and maculopathy for improving overall diabetic control.
One striking element of the data is that there was a considerable degree of regression in visible retinopathy state especially in people with type 2 diabetes and lower grades of retinopathy. This is likely in part to reflect progression of capillary occlusion leading to ‘disappearance’ of microaneurysms followed by resorption of local exudate and haemorrhage, rather than a true return to normal retinal perfusion. However, the lack of newly forming microaneurysms to replace those previously noted also suggests that in some individuals the underlying disease process had improved. We cannot tell at this stage if the level of regression seen here was a result of improvements in the management of people with diabetes particularly with regard to glycaemia and blood pressure. Models that did not allow for regression had higher deviance (poorer fit to the data).
This study shows that the increased risk of extending the screening intervals for diabetic retinopathy for patients with type 2 diabetes and no visible retinopathy after two successive annual screening examinations is small. Possible benefits of two yearly intervals include screening a greater number of patients and/or enabling high-risk patients to be screened more frequently. This work should help inform policy-makers as to whether the benefits of two yearly screening for this group of patients outweigh the risks.
Electronic supplementary material
Below is the link to the electronic supplementary material.
a–f Observed Transitions by Diabetes Type and Initial DRS Grading. a) Type 1 Diabetes and no visible retinopathy at Initial DRS Exam. b) Type 1 Diabetes and mild background retinopathy at Initial DRS Exam. c) Type 1 Diabetes and Observable Retinopathy at Initial DRS Exam. d) Type 2 Diabetes and no visible retinopathy at Initial DRS Exam. e) Type 2 Diabetes and mild background retinopathy at Initial DRS Exam. f) Type 2 Diabetes and Observable Retinopathy at Initial DRS Exam. Obs = observable retinopathy and observable maculopathy grades. Ref = referable retinopathy including referable background retinopathy, proliferative retinopathy and referable maculopathy. All individuals had a minimum of two exams and data has been limited to first three exams for graphical purposes only (PDF 220 kb)
(PDF 26 kb)
(PDF 23 kb)
(PDF 18 kb)
(PDF 11 kb)
(PDF 18 kb)
(PDF 11 kb)
(PDF 20 kb)
Acknowledgements
We wish to acknowledge the work of all involved in the Scottish Diabetes Retinopathy Screening Service and the Scottish Diabetes Research Network.
Funding
This work was supported by the Wellcome Trust through a Scottish Health Informatics Programme (SHIP) grant (ref. WT086113). SHIP is a collaboration between the universities of Aberdeen, Dundee, Edinburgh, Glasgow and St Andrews and the Information Services Division of NHS Scotland.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
HCL was involved in the conception of the study, analysis of the data and drafted the manuscript. SON was involved in the design of the study—specifically the selection of the modelling approach—and undertook analysis of the data and revised the manuscript. HMC conceived and designed the study, interpreted the data and revised the manuscript. PM undertook the hidden Markov model analysis and was integral to the interpretation of the data and the revision of the manuscript. DTC, GPL JAO and SP were involved in the conception of the study, interpretation of the data and critically revising the manuscript. MWB, AB, JD, EJH, NL, RSL, JAM, ADM, DWMP, NAS and SHW were involved in interpretation of the data and critically revising the manuscript. All authors approved the final version of the manuscript.
Abbreviations
- DRS
Scottish diabetic retinopathy screening
- IQR
Interquartile range
- SCI-DC
Scottish Care Information–Diabetes Collaboration
Footnotes
H. C. Looker and S. O. Nyangoma contributed equally to this study.
P. McKeigue and H. M. Colhoun contributed equally to this study.
Members of the SDRN Epidemiology Group beyond the authors listed:
I. Brady, Population Health Sciences, University of Dundee; S. Livingstone, Population Health Sciences, University of Dundee; J. Chalmers, Victoria Hospital, Kirkcaldy; S. Cunningham, Clinical Technology Centre, University of Dundee; R. Elder, Information Services Division, NHS Scotland; A. Emslie-Smith, Arthurstone Medical Centre, Dundee; B. Guthrie, Population Health Sciences, University of Dundee; L. Govan, Institute of Health and Wellbeing, University of Glasgow; D. Levin, Medical Research Institute, University of Dundee; R. McAlpine, Diabetes Managed Clinical Network, NHS Tayside; J. Petrie, University of Glasgow; C. Fischbacher, National Services Scotland, NHS Scotland
References
- 1.Kohner EM. Diabetic retinopathy. BMJ. 1993;307:1195–1199. doi: 10.1136/bmj.307.6913.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National diabetes retinopathy screening (2011). Available from www.ndrs.scot.nhs.uk/, accessed 6 October 2011
- 3.Facey K, Cummins E, Macpherson K, Morris K, Reay L, Slattery J. Organisation of services for diabetic retinopathy screening. Glasgow: Health Technology Assessment Report 1. Health Technology Board for Scotland; 2002. [Google Scholar]
- 4.Mitchell P, Bandello F, Schmidt-Erfurth U, et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118:615–625. doi: 10.1016/j.ophtha.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 5.Elman MJ, Aiello LP, Beck RW, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117(1064–1077):e1035. doi: 10.1016/j.ophtha.2010.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scottish Diabetic Retinopathy Screening Programme annual report 2010–2011. Available from www.ndrs.scot.nhs.uk/ExecGrp/Docs/DRSP%20Annual%20Report%202010-2011.pdf, accessed 30 July 2012
- 7.Scottish Diabetes Survey 2011. Available from www.diabetesinscotland.org.uk/Publications/SDS%202011.pdf, accessed 1 October 2012
- 8.Aspelund T, Thornorisdottir O, Olafsdottir E, et al. Individual risk assessment and information technology to optimise screening frequency for diabetic retinopathy. Diabetologia. 2011;54:2525–2532. doi: 10.1007/s00125-011-2257-7. [DOI] [PubMed] [Google Scholar]
- 9.Agardh E, Tababat-Khani P. Adopting 3-year screening intervals for sight-threatening retinal vascular lesions in type 2 diabetic subjects without retinopathy. Diabetes Care. 2011;34:1318–1319. doi: 10.2337/dc10-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehlsen J, Erlandsen M, Poulsen PL, Bek T. Individualized optimization of the screening interval for diabetic retinopathy: a new model. Acta Ophthalmol. 2012;90:109–114. doi: 10.1111/j.1755-3768.2010.01882.x. [DOI] [PubMed] [Google Scholar]
- 11.Thomas RL, Dunstan F, Luzio SD, et al. Incidence of diabetic retinopathy in people with type 2 diabetes mellitus attending the Diabetic Retinopathy Screening Service for Wales: retrospective analysis. BMJ. 2012;344:e874. doi: 10.1136/bmj.e874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Younis N, Broadbent DM, Harding SP, Vora JP. Incidence of sight-threatening retinopathy in type 1 diabetes in a systematic screening programme. Diabet Med. 2003;20:758–765. doi: 10.1046/j.1464-5491.2003.01035.x. [DOI] [PubMed] [Google Scholar]
- 13.Younis N, Broadbent DM, Vora JP, Harding SP. Incidence of sight-threatening retinopathy in patients with type 2 diabetes in the Liverpool Diabetic Eye Study: a cohort study. Lancet. 2003;361:195–200. doi: 10.1016/S0140-6736(03)12267-2. [DOI] [PubMed] [Google Scholar]
- 14.Jones CD, Greenwood RH, Misra A, Bachmann MO. Incidence and progression of diabetic retinopathy during 17 years of a population-based screening program in England. Diabetes Care. 2012;35:592–596. doi: 10.2337/dc11-0943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Livingstone SJ, Looker HC, Hothersall EJ, et al. Risk of cardiovascular disease and total mortality in adults with type 1 diabetes: Scottish Registry Linkage Study. PLoS Med. 2012;9:e1001321. doi: 10.1371/journal.pmed.1001321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Looker HC, Nyangoma SO, Cromie D, et al. Diabetic retinopathy at diagnosis of type 2 diabetes in Scotland. Diabetologia. 2012;55:2335–2342. doi: 10.1007/s00125-012-2596-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DRS (2007) The Scottish Diabetic Retinopathy Grading Scheme 2007 v1.1. Available from www.ndrs.scot.nhs.uk/ClinGrp/Docs/Grading%20Scheme%202007%20v1.1.pdf, accessed 30 July 2012
- 18.Development Core Team R. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2009. [Google Scholar]
- 19.Jackson C. Multi-state models for panel data: the msm package for R. Journal of Statistical Software. 2011;38:1–28. [Google Scholar]
- 20.Welcome to the English National Screening Programme for Diabetic Retinopathy (2012). Available from www.retinalscreening.nhs.uk/pages/, accessed 10 January 2012
- 21.Diabetic Retinopathy Screening Service for Wales (2012). Available from www.cardiffandvaleuhb.wales.nhs.uk/drssw, accessed 10 January 2012
- 22.Olafsdottir E, Stefansson E. Biennial eye screening in patients with diabetes without retinopathy: 10-year experience. Br J Ophthalmol. 2007;91:1599–1601. doi: 10.1136/bjo.2007.123810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chalk D, Pitt M, Vaidya B, Stein K. Can the retinal screening interval be safely increased to 2 years for type 2 diabetic patients without retinopathy? Diabetes Care. 2012;35:1663–1668. doi: 10.2337/dc11-2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goatman KA, Philip S, Fleming AD, et al. External quality assurance for image grading in the Scottish Diabetic Retinopathy Screening Programme. Diabet Med. 2012;29:776–783. doi: 10.1111/j.1464-5491.2011.03504.x. [DOI] [PubMed] [Google Scholar]
- 25.Leese GP, Morris AD, Swaminathan K, et al. Implementation of national diabetes retinal screening programme is associated with a lower proportion of patients referred to ophthalmology. Diabet Med. 2005;22:1112–1115. doi: 10.1111/j.1464-5491.2005.01603.x. [DOI] [PubMed] [Google Scholar]
- 26.Philip S, Cowie LM, Olson JA. The impact of the Health Technology Board for Scotland's grading model on referrals to ophthalmology services. Br J Ophthalmol. 2005;89:891–896. doi: 10.1136/bjo.2004.051334. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
a–f Observed Transitions by Diabetes Type and Initial DRS Grading. a) Type 1 Diabetes and no visible retinopathy at Initial DRS Exam. b) Type 1 Diabetes and mild background retinopathy at Initial DRS Exam. c) Type 1 Diabetes and Observable Retinopathy at Initial DRS Exam. d) Type 2 Diabetes and no visible retinopathy at Initial DRS Exam. e) Type 2 Diabetes and mild background retinopathy at Initial DRS Exam. f) Type 2 Diabetes and Observable Retinopathy at Initial DRS Exam. Obs = observable retinopathy and observable maculopathy grades. Ref = referable retinopathy including referable background retinopathy, proliferative retinopathy and referable maculopathy. All individuals had a minimum of two exams and data has been limited to first three exams for graphical purposes only (PDF 220 kb)
(PDF 26 kb)
(PDF 23 kb)
(PDF 18 kb)
(PDF 11 kb)
(PDF 18 kb)
(PDF 11 kb)
(PDF 20 kb)