Abstract
Purpose: There is growing recognition that many physician–patient encounters do not require face-to-face contact. The availability of secure Internet portals creates the opportunity for online eVisits. Increasing numbers of health systems provide eVisits, and many health plans reimburse for eVisits. However, little is known on who chooses to seek care via an eVisit. Materials and Methods: At four primary care practices, we used the electronic medical record to identify all eVisits and office visits for sinusitis and urinary tract infections (UTIs) between January 2010 and May 2011. From the electronic medical record we abstracted the necessary information on patient demographics. The population studied included 5,165 sinusitis visits (9% of which were eVisits) and 2,954 UTI visits (3% eVisits). Results: In multivariate models controlling for other patient factors, the variables most strongly associated with a patient initiating an eVisit versus an office visit were age (18–44 years of age versus 65 years of age and older: sinusitis, odds ratio 1.65 [0.97–2.81]; UTI, 2.97 [1.03–8.62]) and longer travel distance to clinic (>10 miles from patient home to clinic versus 0–5 miles: sinusitis, odds ratio 6.54 [4.68–9.16]; UTI, odds ratio 3.25 [1.74–6.07]). Higher income was not associated with higher eVisit use. Conclusions: At these four primary care practices, eVisits accounted for almost 7% of visits for sinusitis and UTI. eVisits attract a younger patient population who might use eVisits for convenience reasons.
Key words: health services research, primary care delivery/access
Introduction
There is a growing recognition that many patient encounters do not require face-to-face contact. The increasing use of the Internet creates the opportunity for eVisits, where the interaction between physician and patient is completely virtual. The distinction between an eVisit and simple patient messaging or e-mail is that an eVisit must include history taking, diagnosis, and intervention.1,2 Some eVisits use real-time video linkage with the patient and might be considered a form of telemedicine. More commonly, eVisits are done in an asynchronous manner. A patient logs onto a secure Internet portal and answers a series of questions about his or her condition. This written information is sent to the physician, who uses this information, along with the patient's electronic medical record (EMR), makes a diagnosis, orders necessary care, and replies to the patient via the portal within several hours. The focus of eVisits, to date, has been primarily on acute problems such as acute respiratory illnesses.
Numerous large integrated medical systems, physician groups, and private companies, are now providing eVisits.1–8 Using a new current procedural terminology code (99444) for eVisits, many health plans now also reimburse eVisits.2 Despite this growing interest, little is known about eVisits. One study found that from the perspective of a health plan, eVisits are cheaper than in-office visits.9 To our knowledge, no prior study has examined who seeks care via an eVisit instead of an in-person office visit.
To fill this gap in knowledge, we compared eVisit and office visit users at four primary care practices for two conditions: sinusitis and urinary tract infection (UTI). We chose these because they are common reasons for eVisits. We had several hypotheses on who might be attracted to eVisits. eVisits are more convenient as there is no travel, and the patient can seek care when physician offices are often closed, such as evenings and weekends. Therefore, we thought eVisits might be particularly attractive to those who live far away from the office and those who are employed. Furthermore, eVisits might be more attractive to those who are more familiar with the Internet, such as the young and those with a higher income. Lastly, our hypothesis was that eVisits would be attractive to those with fewer visits to the office as their relationship with their primary care physician was likely weaker.
Materials and Methods
Study Sites
We studied eVisits and office visits at four practices in the Pittsburgh, PA, region. Although eVisits are now offered at all primary care practices in the UPMC system, these practices were the first to offer eVisits and currently have the highest monthly volume of patients using eVisits. The practices began offering eVisits between August 1, 2008 and April 1, 2009. The four practices have a total of 63 internal medicine and family practice physicians.
How Evisits are Provided
To initiate an eVisit, patients must have a secure patient portal account (MyChart; Epic, Verona, WI), where they can click on a link to eVisits. This triggers a structured questionnaire that confirms their past medical history, medication allergies, and their usual pharmacy. It then includes both close-ended and open-ended questions relevant to the condition. For example, the questionnaire for urinary symptoms asks, “Do you have pain in your back, belly, or on your side below your ribs?” The written answers are sent to a physician in the patient's practice.
Which physician addresses eVisits varies across the clinics and depends on time of day. The physician reviews the answers and patient's EMR and makes a diagnosis and decides on treatment. A note is put into the EMR, and the physician communicates with the patient via the patient portal. Any necessary prescriptions are sent electronically to the patient's pharmacy. If the physician orders tests, the patient generally picks up the order at the clinic, although some labs now accept electronic orders. The care provided in an eVisit is not in real-time. The average response time by a physician is approximately 2 h, but varies by day of the week and time of day.
There are no screening questions that automatically signal that the eVisit is inappropriate. If a physician reviews the eVisit and decides the patient should be seen in the office, the eVisit is still included in the EMR (and captured in our data), although the patient is not charged for both the eVsit and office visit.
Patient Population and Conditions Examined
We identified all office visits and eVisits for sinusitis and UTIs provided at these four practices between January 1, 2010 and May 1, 2011. These visits were termed “index visits.” Consistent with prior literature,10–13 we identified the conditions by the following ICD-9 diagnosis codes: UTI, 595.0, 595.9, 788.1, and 599.0; sinusitis, 461, 461.01, 461.1,461.2, 461.3, 461.8, and 461.9. We looked at all diagnosis codes coded, as the order of diagnoses is typically not clinically important in outpatient visits in the system.
For each patient with an index visit, we obtained data on all encounters in the EMR from January 1, 2009 through May 1, 2011. This provided at least 1 year of data prior to the index visit. We excluded children (eVisits are not currently offered for children) and those with a non-Pennsylvania zip code (fewer than 10 patients). Our goal was to identify first visits for the condition. Therefore, we further excluded index visits if there was an office visit or eVisit for a similar diagnosis in the prior 21 days. Our unit of observation was episodes of sinusitis and UTI, and a single patient could contribute more than one episode.
Data Collected
For each episode we obtained information on the age, gender, race, diagnoses, whether the patient had a patient portal account, and zip code. Data on the race, patient's employment, and marital status are captured and/or confirmed during the registration process. Based on the patient's zip code we obtained U.S. Census data on the median income in the zip code. Visits from December through March were labeled as winter visits. Distance was the number of miles between the centroid of the patient's zip code and the patient's primary care clinic. Our hypotheses were during the winter and as distance increases, eVisit use would increase.
We calculated the number of office visits for any reason in the prior year. We looked at any type of visit in the 12 months prior to the index visit.
Statistical Analyses
For both sinusitis and UTI visits, we compared the characteristics of patients who had an eVisit and an office visit. For our bivariate analyses we used the chi-squared test. We also created a multivariate model to predict eVisit use. For this analysis we limited our sample to only those visits where the patient had a patient portal account. To initiate an eVisit, a patient must have an active account. Limiting our analyses to those with a patient portal allowed us to disentangle what patient characteristics are associated with having a portal account versus, among those with an account, what patient characteristics were associated with using an eVisit. We thought the latter was the more relevant question for this study. For the UTI visits, we further limited the analytic sample to women. The UTI eVisit is designed for women as it is generally recommended that men receive testing.
Results
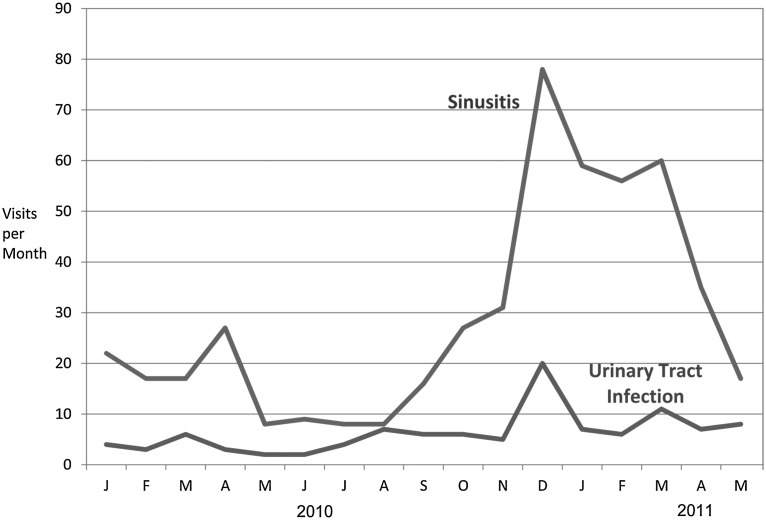
Of the 5,165 visits for sinusitis, 465 (9%) were eVisits. Of the 2,954 visits for UTIs at the four practices, 99 were via an eVisit (3%). The number of eVisits increased slowly over time (Fig. 1), with notable seasonal variation for sinusitis.
Fig. 1.
Increase in number of eVisits with time for sinusitis and urinary tract infections.
Comparison of Patient Characteristics of Evisit Patients Versus Office Visit Patients
In our bivariate analysis, there were notable differences between eVisit and office visit patients across many characteristics (Table 1). Women were more likely to use an eVisit: sinusitis, 77% eVisits versus 69% office visits; UTI, 98% eVisits versus 78% office visits (p<0.001 for both). Older (≥65 years of age) patients were less likely to use an eVisit: sinusitis, 6% eVisits versus 13% office visits; UTI, 9% eVisits versus 27% office visits (p<0.001 for both). Patients with more visits (three or more visits for any reasons) in the prior year were more likely to use an eVisit: sinusitis, 85% eVisits versus 76% office visits; UTI, 87% eVisits versus 74% office visits (p<0.01 for differences). Employed patients were more likely to use an eVisit: sinusitis, 75% eVisits versus 62% office visits; UTI, 60% eVisits versus 46% office visits (p<0.01 for both).
Table 1.
Comparison of Patient Characteristics Among Patients with eVisits and Office Visits
| |
SINUSITIS |
URINARY TRACT INFECTION |
||||
|---|---|---|---|---|---|---|
| PATIENT CHARACTERISTIC | EVISITS (N=475) | OFFICE VISITS (N=4,690) | P VALUE | EVISITS (N=99) | OFFICE VISITS (N=2,855) | P VALUE |
| Gender | ||||||
| Female | 368 (77) | 3,252 (69) | <0.001 | 97 (98) | 2,220 (78) | <0.001 |
| Male | 107 (23) | 1,438 (31) | 2 (2) | 635 (22) | ||
| Age (years) | ||||||
| 18–44 | 213 (45) | 2,062 (44) | <0.001 | 50 (51) | 953 (33) | <0.001 |
| 45–64 | 234 (49) | 2,008 (43) | 40 (40) | 1,128 (40) | ||
| >65 | 28 (6) | 620 (13) | 9 (9) | 774 (27) | ||
| Marital status | ||||||
| Married | 319 (67) | 2,900 (62) | 0.02 | 60 (61) | 1,596 (56) | 0.35 |
| Unmarried | 156 (33) | 1,790 (38) | 39 (39) | 1,259 (44) | ||
| Account with patient portala | ||||||
| Active account | 469 (99) | 2,289 (49) | <0.001 | 98 (99) | 1,209 (42) | <0.001 |
| Not active account | 6 (1) | 1,738 (37) | 1 (1) | 1,134 (40) | ||
| Employment status | ||||||
| Working | 355 (75) | 2,924 (62) | <0.001 | 59 (60) | 1,320 (46) | 0.004 |
| Unemployed/unknown | 83 (17) | 996 (21) | 25 (25) | 742 (26) | ||
| Retired | 26 (5) | 555 (12) | 9 (9) | 672 (24) | ||
| Student | 11 (2) | 215 (5) | 6 (6) | 118 (4) | ||
| Race | ||||||
| White | 458 (96) | 4,346 (93) | 0.003 | 91 (92) | 2,425 (85) | 0.02 |
| Black/African American | 4 (1) | 176 (4) | 2 (2) | 304 (11) | ||
| Other | 13 (3) | 168 (4) | 6 (4) | 126 (4) | ||
| Zip code median household income | ||||||
| <$30,000 | 59 (12) | 477 (10) | 0.18 | 10 (10) | 537 (19) | 0.02 |
| $30,000–45,000 | 298 (63) | 2,914 (62) | 69 (70) | 1,614 (57) | ||
| >$45,000 | 118 (25) | 1,299 (28) | 20 (20) | 704 (25) | ||
| Distance from home to clinic | ||||||
| 0–5 miles | 50 (11) | 1,425 (34) | <0.001 | 16 (16) | 899 (36) | <0.001 |
| 6–10 miles | 172 (37) | 1,056 (25) | 29 (29) | 851 (34) | ||
| >10 miles | 249 (53) | 1,713 (41) | 54 (55) | 750 (30) | ||
| Season of visit | ||||||
| Winter | 305 (64) | 2,541 (54) | <0.001 | 57 (58) | 1,218 (43) | 0.003 |
| Non-winter | 170 (36) | 2,149 (46) | 42 (42) | 1,637 (57) | ||
| Utilization | ||||||
| 3 or more visits in prior year | 405 (85) | 3,578 (76) | <0.001 | 86 (87) | 2,116 (74) | 0.004 |
Data are number (%).
An active account is necessary to receive an eVisit. An account is no longer active when the patient dies or a patient requests deactivation. Patient portal status was captured as of September 2011, which was later than the end of the study.
The differences in patient characteristics observed in bivariate analyses were largely confirmed in multivariate models (Table 2). The exception is employed patients were not more likely to use an eVisit. Average income in the patient's zip code was not associated with eVisit use.
Table 2.
Among Patients with an Account to the Patient Portal, Patient Characteristics Associated with eVisit Use in a Multivariate Model
| |
ODDS RATIO (95% CI) |
|
|---|---|---|
| PATIENT CHARACTERISTIC | SINUSITIS (N=2,484)a | UTI (N=932)a |
| Sex | ||
| Men | 1 (Reference) | Not applicable |
| Women | 1.35 (1.05–1.73) | |
| Age (years) | ||
| 18–44 | 1.65 (0.97–2.81) | 2.97 (1.03–8.62) |
| 45–64 | 1.46 (0.88–2.44) | 1.93 (0.69–5.38) |
| 65+ | 1 (Reference) | 1 (Reference) |
| Marital status | ||
| Married | 1.06 (0.84–1.33) | 1.04 (0.65–1.66) |
| Unmarried | 1 (Reference) | 1 (Reference) |
| Race | ||
| White | 2.76 (0.98–7.79) | 2.66 (0.61–11.63) |
| Other | 3.29 (0.98–11.03) | 4.91 (0.88–27.48) |
| Black | 1 (Reference) | 1 (Reference) |
| Employment status | ||
| Employed | 1.20 (0.91–1.59) | 1.39 (0.82–2.35) |
| Student | 0.62 (0.30–1.29) | 1.15 (0.39–3.43) |
| Retired | 0.82 (0.47–1.45) | 1.16 (0.39–3.43) |
| Unemployed | 1 (Reference) | 1 (Reference) |
| Utilization pattern in prior year | ||
| Less than 3 visits | 1 (Reference) | 1 (Reference) |
| 3 or more visits | 1.50 (1.11–2.02) | 2.54 (1.25–4.44) |
| Average income in zip code | ||
| <$30,000 | 1 (Reference) | 1 (Reference) |
| $30,000–45,000 | 0.62 (0.44–0.88) | 1.40 (0.82–2.35) |
| >$45,000 | 0.74 (0.50–1.08) | 0.91 (0.39–2.11) |
| Season of year | ||
| Winter | 1.48 (1.19–1.85) | 1.80 (1.15–2.81) |
| Other season | 1 (Reference) | 1 (Reference) |
| Distance from home to clinic | ||
| 0–5 miles | 1 (Reference) | 1 (Reference) |
| 6–10 miles | 2.80 (1.99–2.02) | 1.62 (0.82–3.17) |
| >10 miles | 6.54 (4.68–9.16) | 3.25 (1.74–6.07) |
The multivariate model included all variables listed. As noted in the text, men excluded were from the model for urinary tract infection (UTI) as the UTI eVisit module is tailored for women, and therefore eVisit not a good option for men.
Sample size smaller than in Table 1 because limited analyses in this model to those patients with an active patient portal account and have a zip code in data.
CI, confidence interval.
Discussion
Given the perceived advantages of eVisits and demographics of those who use the Internet,14 we expected eVisit users to be younger, wealthier patients who live farther away and do not regularly seek care. This was only partially supported by our results. Convenience appears to be critical as distance and the winter season were associated with greater eVisit use. However, patients who regularly sought care were more likely to use eVisits. Others have described a “digital divide” where lower income people are less likely to use Internet-based health resources.15,16 It is surprising that we saw no digital divide with eVisits as employment status and income were not associated with eVisits use.
The patterns we observe likely relate to how patients learn about eVisits. Patients who regularly use the patient portal frequently for other care are both more aware of eVisits and likely trust their physician enough to use this novel method of receiving care. Patients who see their physician frequently are likely to have a patient portal account.
Some health systems view eVisits as a means of increasing revenue17,18 and combatting the loss of visits to retail clinics and urgent care centers.19,20 Although eVisits make up approximately 5% of visits for these two conditions at these four clinics, given the current growth of eVisits, it will take some time for eVisits to be a viable alternative source of revenue. This is consistent with other studies in which uptake of patient portals and eVisits has been slow.2,17 We believe the slow growth reflects both a lack of awareness among patients17 and a wariness of primary care providers with eVisits.
There are numerous limitations of our analyses. Our analyses are based on diagnosis codes and not the patient's presenting symptoms. For example, among patients who initiated a sinusitis eVisit on the patient portal, only 80% were given a diagnosis of sinusitis. We compared eVisits with office visits. However, this may not be the best comparison. Many physicians provide phone care for these conditions.21 Other alternatives such as urgent care centers and retail clinics are becoming more popular. In the future, it might be useful to compare the patient characteristics of those who receive care at these other care sites.
Increasing numbers of health systems are offering eVisits. In a comparison of eVisits with office visits at primary care practices, eVisits accounted for approximately 5% of visits for sinusitis and UTI. Contrary to our expectations, we saw no digital divide in who used an eVisit, and users of eVisits were higher utilizers of the healthcare system. There is growing interest in eVisits, and our results highlight which patients might be attracted to this new alternative to care.
Acknowledgments
This study was supported by grant 1R21AI097759-01 from the National Institutes of Health, Career Development Award KL2-TR000146 from the National Institutes of Health to A.M., and internal funding by UPMC. We thank Gerald Hunter and Cynthia Carbine for their support pulling the data and analyses. G.D.M., S.P., and G.J.S. were involved in the development of eVisits and have advised other health systems on how to implement them.
Disclosure Statement
No competing financial interests exist.
References
- 1.Adamson SC. Bachman JW. Pilot study of providing online care in a primary care setting. Mayo Clin Proc. 2010;85:704–710. doi: 10.4065/mcp.2010.0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mettner J. The doctor is in (your inbox) 2009. www.minnesotamedicine.com/PastIssues/PastIssues2009/January2009/PulseInboxJanuary2009.aspx. [Aug 2;2012 ]. www.minnesotamedicine.com/PastIssues/PastIssues2009/January2009/PulseInboxJanuary2009.aspx [PubMed]
- 3.Allina Health System. E-Visits: Connect with a clinician online. www.allina.com/ahs/medicalservices.nsf/page/evisits_MyChart. [Mar 29;2012 ]. www.allina.com/ahs/medicalservices.nsf/page/evisits_MyChart
- 4.Albert SM. Shevchik GJ. Paone S. Martich GD. Internet-based medical visit and diagnosis for common medical problems: Experience of first user cohort. Telemed J E Health. 2011;17:304–308. doi: 10.1089/tmj.2010.0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bell A. What's next? Medicine catching up with practical uses of technology. 2012. www.pressandguide.com/articles/2012/03/14/news/doc4f6104e396847656235090.txt. [Mar 29;2012 ]. www.pressandguide.com/articles/2012/03/14/news/doc4f6104e396847656235090.txt
- 6.Berry E. Health plans look to save on each patient visit. 2011. www.ama-assn.org/amednews/2011/12/26/bisc1226.htm. [Mar 29;2012 ]. www.ama-assn.org/amednews/2011/12/26/bisc1226.htm
- 7.Bershow B. The doctor is in (your inbox) 2009. www.minnesotamedicine.com/PastIssues/PastIssues2009/January2009/PulseInboxJanuary2009.aspx. [Mar 29;2012 ]. www.minnesotamedicine.com/PastIssues/PastIssues2009/January2009/PulseInboxJanuary2009.aspx
- 8.Saurage-Altenloh S. Online doctor consultations: Is medicine going remote? 2011. http://blog.chron.com/factistics/2012/03/online-doctor-consultations-is-medicine-going-remote/ [Mar 29;2012 ]. http://blog.chron.com/factistics/2012/03/online-doctor-consultations-is-medicine-going-remote/
- 9.Rohrer JE. Angstman KB. Adamson SC. Bernard ME. Bachman JW. Morgan ME. Impact of online primary care visits on standard costs: A pilot study. Popul Health Manag. 2010;13:59–63. doi: 10.1089/pop.2009.0018. [DOI] [PubMed] [Google Scholar]
- 10.Steinman MA. Gonzales R. Linder JA. Landefeld CS. Changing use of antibiotics in community-based outpatient practice, 1991–1999. Ann Intern Med. 2003;138:525–533. doi: 10.7326/0003-4819-138-7-200304010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Kahan NR. Friedman NL. Lomnicky Y, et al. Physician speciality and adherence to guidelines for the treatment of unsubstantiated uncomplicated urinary tract infection among women. Pharmacoepidemiol Drug Saf. 2005;14:357–361. doi: 10.1002/pds.1044. [DOI] [PubMed] [Google Scholar]
- 12.Kallen AJ. Welch HG. Sirovich BE. Current antibiotic therapy for isolated urinary tract infections in women. Arch Intern Med. 2006;166:635–639. doi: 10.1001/archinte.166.6.635. [DOI] [PubMed] [Google Scholar]
- 13.Piccirillo JF. Mager DE. Frisse ME. Brophy RH. Goggin A. Impact of first-line vs second-line antibiotics for the treatment of acute uncomplicated sinusitis. JAMA. 2001;286:1849–1856. doi: 10.1001/jama.286.15.1849. [DOI] [PubMed] [Google Scholar]
- 14.Pew Internet & American Life Project. Demographics of Internet users. 2012. www.pewInternet.org/Trend-Data-%28Adults%29/Whos-Online.aspx. [Mar 29;2012 ]. www.pewInternet.org/Trend-Data-%28Adults%29/Whos-Online.aspx
- 15.Yamin CK. Emani S. Williams DH, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171:568–574. doi: 10.1001/archinternmed.2011.34. [DOI] [PubMed] [Google Scholar]
- 16.Brodie M. Flournoy RE. Altman DE. Blendon RJ. Benson JM. Rosenbaum MD. Health information, the Internet, and the digital divide. Health Aff (Millwood) 2000;19:255–265. doi: 10.1377/hlthaff.19.6.255. [DOI] [PubMed] [Google Scholar]
- 17.Whitten P. Buis L. Love B. Physician-patient e-visit programs: Implementation and appropriateness. Dis Manag Health Out. 2007;15:207–214. [Google Scholar]
- 18.Adler KG. Web portals in primary care: An evaluation of patient readiness and willingness to pay for online services. J Med Internet Res. 2006;8:e26. doi: 10.2196/jmir.8.4.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashwood JS. Reid RO. Setodji CM. Weber E. Gaynor M. Mehrotra A. Trends in retail clinic use among the commercially insured. Am J Manag Care. 2011;17:e443–e448. [PMC free article] [PubMed] [Google Scholar]
- 20.Weinick RM. Bristol SJ. DesRoches CM. Urgent care centers in the U.S.: Findings from a national survey. BMC Health Serv Res. 2009;9:79. doi: 10.1186/1472-6963-9-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barry HC. Hickner J. Ebell MH. Ettenhofer T. A randomized controlled trial of telephone management of suspected urinary tract infections in women. J Fam Pract. 2001;50:589–594. [PubMed] [Google Scholar]