Abstract
Objectives:
To demonstrate the feasibility of GafChromic® XR-QA2 (ISP Corp., Wayne, NJ) as a dosemeter when performing measurements of the effective dose from three cone beam CT (CBCT) units and to compare the doses from examinations of three common dental clinical situations. A second aim was to compare the radiation doses for three digital panoramic units with the doses for the CBCT units.
Methods:
The CBCT units used were Veraviewepocs 3De® (J Morita MFG Corp., Kyoto, Japan), ProMax® 3D (Planmeca, Helsinki, Finland) and NewTom VGi® (Quantitative Radiology, Verona, Italy). GafChromic XR-QA2 films were placed between the selected layers of the head and neck of a tissue-equivalent human skull (RANDO® phantom; The Phantom Laboratory, Salem, NY). The exposure parameters were set using the automatic exposure control function of the units. Depending on the availability, medium and smaller field of view (FOV) scanning modes were used. The effective dose was estimated using the 2007 International Commission on Radiological Protection formalism.
Results:
The lowest effective dose of a CBCT unit was observed for ProMax 3D, FOV 4 × 5 cm (10 μSv), the highest for NewTom VGi, FOV 8 × 8 cm—high resolution (129 μSv). The range of effective doses for digital panoramic machines measured was 8–14 μSv.
Conclusions:
This study demonstrates the feasibility of using radiochromic films for dental CBCT and panoramic dosimetry.
Keywords: radiation dosage, cone beam computed tomography, film dosimetry
Introduction
Panoramic radiography has long been a common diagnostic imaging technique in dentistry owing to its low dose and large area for evaluation, which includes bone and teeth in the same image.1 Cone beam CT (CBCT) is a more recent technology that has significant potential for a number of clinical situations requiring CBCT imaging.2 Although CBCT provides additional information, it may result in higher radiation doses than conventional imaging procedures, such as intraoral and panoramic.2,3 Although the absorbed doses from oral and maxillofacial radiology procedures are usually low, no exposure to radiographs can be regarded as completely free of risk. The measurement of absorbed organ doses is needed to estimate the effective dose associated with diagnostic radiographic imaging. The traditional way of determining the effective dose in oral and maxillofacial radiology is by measuring the organ doses using thermoluminescent dosemeters (TLDs) and head phantoms.3–6
In rotating irradiation geometry with collimated radiation fields, the dose distribution will show more or less steep dose gradients. This is a major problem if you want to map or sample the dose distribution with a reasonable degree of accuracy using TLDs. The geometry drawback encouraged us to choose a method with higher spatial resolution for mapping the dose distributions in a phantom. The GafChromic® XR-QA film (ISP Corp., Wayne, NJ) is designed specifically as a quality assurance (QA) tool for radiology and dosimetry applications. In combination with flatbed document scanners,7 it has been used for measuring medical8 and dental9 CBCT doses and CT doses.10,11 Some of the characteristics of this film have been studied: energy dependence8 and angular dependence.10 One of the advantages of this film is that it provides a high-resolution image with no chemical processing.12 The film is not sensitive to visual light and can therefore be handled in ambient light. Ionizing radiation induces polymerization within the active layer of the film, changing its reflectance and making it appear darker. The darkening of the film is dependent on the radiation exposure received. The darkening of the film occurs instantaneously as the reaction immediately creates a polymer dye complex within the active layer of the film.13
The aim of this study was to demonstrate the feasibility of the GafChromic film as a dosemeter for use in rotating dental radiography and apply this technique for estimation of the effective doses from three CBCT units and three panoramic units.
Materials and methods
Cone beam CT units
The CBCT units selected for this study were Veraviewepocs 3De® (J Morita MFG Corp., Kyoto, Japan), ProMax® 3D (Planmeca, Helsinki, Finland) and NewTom VGi® (Quantitative Radiology, Verona, Italy). All CBCT units used flat panel detectors (FPDs) based on similar principles, i.e. a scintillating CsI layer and a light-sensitive silicon photodiode matrix. Exposure parameters and protocols used are given in Table 1.
Table 1.
Technical parameters of selected CBCT and panoramic exposure protocols and sites in which GafChromic® XR-QA2 films were placed in the phantom
| CBCT units | Protocol | FOV sizes (d) × (h) cm | kV | mA | s | Phantom levels | Number of exposures |
| Veraviewepocs 3De® | Upper jaw impacted canine region | 4 × 4 | 80 | 5.0 | 9.5, NP | 3-4-5-6 | 10 |
| Lower jaw molar region | 4 × 4 | 80 | 5.0 | 9.4, NP | 5-6-7-8 | 10 | |
| NewTom VGi® | TMJ, bl: normal resolution | 12 × 8 | 110 | 5.3 | 3.6, P | 4-5-6-7-8 | 30 |
| TMJ, ul: normal resolution | 8 × 8 | 110 | 6.1 | 3.6, P | 4-5-6-7-8 | 30 | |
| TMJ, ul: high resolution | 8 × 8 | 110 | 17.2 | P5.4, P | 4-5-6-7-8 | 20 | |
| ProMax® 3D | Upper jaw impacted canine region | 4 × 5 | 84 | 10.0 | 12, P | 3-4-5-6 | 50 |
| Panoramic units | |||||||
| Veraviewepocs 3De | Panorama, standard, level 3 | — | 78 | 10.0 | 7.4, NP | 5-6-7-8 | 20 |
| ProMax 3D | Panorama, standard, level 3 | — | 66 | 9.0 | 16, P | 5-6-7-8 | 30 |
| ProMax | Panorama, standard | — | 74 | 12.0 | 16, NP | 5-6-7-8 | 20 |
bl, bilateral; CBCT, cone beam CT; FOV, field of view; Level 3, level 3 of autoexposure used for adults; NP, not pulsed radiation; P, pulsed radiation; TMJ, temporomandibular joint; ul, unilateral.
GafChromic XR-QA2 film is manufactured by ISP Corp., Wayne, NJ; Veraviewepocs 3De units by J Morita MFG Corp., Kyoto, Japan; NewTom VGi by Quantitative Radiology, Verona, Italy; and Promax 3D and Promax by Planmeca, Helsinki, Finland.
Panoramic units
The panoramic machines selected for this study were Veraviewepocs 3De (J Morita MFG Corp., Kyoto, Japan), ProMax 3D and ProMax (Planmeca) ProMax was used with a photostimulable phosphor plate system (PSP) (DX-S digitizer; Agfa HealthCare, Mortsel, Belgium), ProMax 3D was used with a charge coupled device detector (CCD) and Veraviewepocs 3De was used with the same FPD as for the CBCT mode. The parameters of voltage (kV), tube current (mA) and exposure time (s) for each scan of the CBCT and panoramic units were fixed at the units’ manufacturer-recommended settings for an average adult patient (Table 1).
Phantom and the GafChromic film XR-QA2
The phantom (RANDO®; The Phantom Laboratory, Salem, NY) was a small adult skull surrounded by soft tissue-equivalent material (Figure 1). Using the positioning aid provided for the scanner, the phantom was positioned mimicking a typical patient examination.
Figure 1.

RANDO® phantom head (The Phantom Laboratory, Salem, NY)
GafChromic films were placed between four selected levels in the head and neck of the phantom for each radiographic technique to record the distribution of the absorbed radiation dose. For detailed information regarding placement of the films, see Table 1.
Measurements were performed using GafChromic XR-QA2 films that were scanned with an Epson® Perfection 4990 Photo flatbed scanner (Seiko Epson Corp., Nagano, Japan). To be able to translate the blackening of the film to absorbed dose, the film has to be calibrated before dosimetric application. The dose–response curve of the GafChromic film was determined using an ionization chamber (Radcal 10X6-6®, a Radcal model 9660 ion chamber digitizer and a Radcal model 2186 electrometer; Radcal Corp., Monrovia, CA). A standard X-ray tube for medical radiology (A-196®; Varian Medical Systems, Inc., Salt Lake City, UT) with a standard collimating device (Svendx SX100-MF; Santax Medico A/S, Aarhus, Denmark) was used for irradiation. The ionization chamber was placed on top of a 255-cm-thick styrofoam slab to minimize the backscatter. A Raysafe® (Unfors Raysafe AB, Billdal, Sweden) semi-conducting detector was placed adjacent to the ionization chamber for use as an exposure monitor when the film was irradiated. The detector was connected to a Raysafe Xi electrometer.
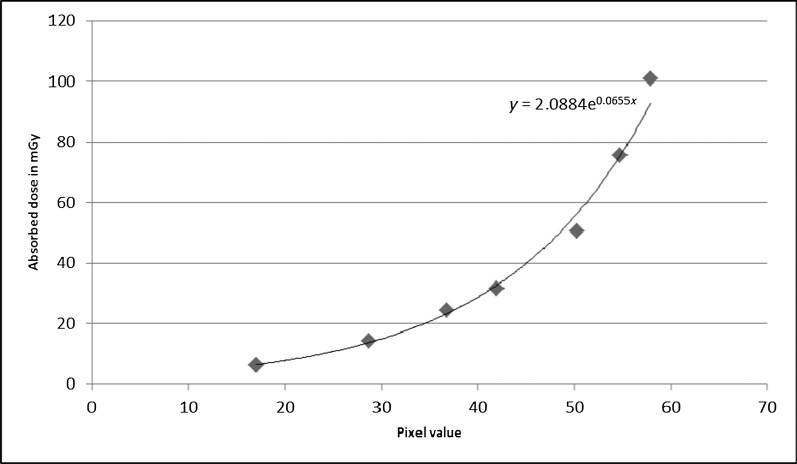
The output (mGy/mAs) of the X-ray tube was determined using 60 kV, 80 kV and 120 kV X-ray tube potentials. The ionization chamber was thereafter removed and replaced with pieces of the GafChromic film that were irradiated with absorbed doses (in air) up to 200 mGy. It was found that the dose–response curve for 60 kV, 80 kV and 120 kV coincided. Owing to the very small spectral dependence of the ion chamber used for the output measurements, the calibration was not sensitive to tube potential, and the same calibration curve could thus be used for all three CBCT units. This is in agreement with what was found for the GafChromic XR-CT film.14 This film has identical physical properties and an identical calibration curve to the GafChromic XR-QA film. The film used in this study is a new version, XR-QA2, which has a slightly higher sensitivity. According to our results, there is no reason to believe that the spectral dependence should differ from that of the XR-CT film, indicating that their atomic compositions are very similar. A piece of film that did not undergo any irradiations was scanned together with the other films and used for background subtraction. The pieces of films were scanned to an ordinary 24-bit red–green–blue (RGB) image; a 24-bit RGB image was used for simplicity reasons to train inexperienced operators. No colour channel selection or suppression was used, and images were stored as 24-bit RGB images. These images were read with Image J® (see http://rsbweb.nih.gov/ij/), following background subtraction, and converted to black-and-white 8‐bit images. The mean pixel values were measured in each film square using rectangular regions of interest (ROIs). The mean pixel values were used to construct a dose–response diagram. The equation of the dose–response curve (Figure 2) was used for converting the net pixel value distributions found in the phantom measurements to the absorbed dose distribution.
Figure 2.
Dose–response calibration curve. The x-axis is the film response represented by the net pixel value change and the y-axis is the corresponding absorbed dose
Before the GafChromic films were positioned for the CBCT scans, a scout image was taken to ensure correct positioning of the phantom and that the field of view (FOV) included the whole anatomical ROI. The dose measurements did not include the scout images. After loading with GafChromic XR-QA2 films, the phantom was exposed several times (Table 1) to provide a reliable measurement. Later, these values were divided by the number of exposures to provide one individual value for each region.
For the skin (entrance) dose measurements, TLDs were used. The TLDs were calibrated using a secondary standard 60Co beam and a pre-defined, reproducible geometric set-up with a plexiglass phantom containing the dosemeters. Prior to the dose measurements in the clinical situation, the dosemeters were annealed at 400 °C for 10 min. For every group of 20 dosemeters, 4 were used for reference irradiation in the 60Co beam and 2 were used for background correction, leaving 14 dosemeters available for clinical dosimetry. The dosemeters were read in a Thermo Scientific Harshaw 5500 TLD® reader (Thermo Fisher Scientific Inc., Reading, UK). The signal was corrected for the dosemeter’s higher sensitivity to diagnostic X-ray energies, and was thereafter converted to the absorbed dose.
Scanning system
An Epson Perfection 4990 PHOTO scanner was used. Warming up the scanner provided a more stable light source and more consistent optical density readings.15 The films were scanned in the same orientation, and within the region of the scanner, which had been previously determined to be the most uniform in sensitivity. The Image J programme was used for converting the net pixel value distributions found in the phantom measurements to the absorbed dose distributions.
Dose estimations
The mean absorbed dose to organs (parotid gland, oral mucosa, extrathoracic airways, bone surfaces, red bone marrow, skin, brain and thyroid gland) and tissue types that were irradiated were estimated by superimposing ROIs on the dose distribution matrices (Figure 3) and calculating the mean value inside each ROI. This was repeated for all film sheets in the phantom.
Figure 3.

Region of interests on the dose distribution matrices; (a) vertebra, (b) parotid gland and (c) mandible
The equivalent dose for an organ/tissue was calculated as the product of the mean absorbed dose to that organ/tissue and the fraction of that organ/tissue that was irradiated. For the skin surface of the exposed head and neck, we used a simple model. The irradiated area in CBCT imaging, which represented the irradiated skin surface of the head and neck area, was Y (cm²) and the total skin surface area was 1.9 m² (19 000 cm²).16 The fraction of the skin area was assumed to be Y/19 000. The estimation of fraction of the irradiated bone surface was based on the total bone area (100 000 cm2)17 and bone area irradiated for each protocol. Owing to higher attenuation in the bone, a conversion factor for Dbone/Dsoft-tissue of 4 was used. The fraction of the red bone marrow irradiated (cervical vertebrae and the mandibular ramus) was assumed to be 2% for the temporomandibular joint (TMJ) lower jaw and panoramic protocol and <1% for the upper jaw scan.16 The brain fraction estimation is just a crude estimation depending on the radiation geometry of each protocol. The fractions of organs irradiated in each protocol are shown in Table 2. The effective dose was then estimated as the sum of the organ/tissues’ equivalent dose multiplied by their tissue-weighting factor according to the International Commission on Radiological Protection (ICRP) 2007 recommendations.18
Table 2.
Estimated fraction of tissue irradiated by primary and scattered radiation for CBCT and panoramic scan protocols
| Fraction irradiated |
|||||
| Upper jaw impacted canine region 4 × 4 | Lower jaw molar region 4 × 4 | TMJ: normal resolution 12 × 8 |
Upper jaw impacted canine region 4 × 5 | Standard panoramic | |
| TMJ: normal resolution 8 × 8 |
|||||
| TMJ: high resolution 8 × 8 |
|||||
| Tissue | Primary/scattered | Primary/scattered | Primary/scattered | Primary/scattered | Primary/scattered |
| Parotid glands | 0.70/0.30 | 1.00/0.00 | 1.00/0.00 | 0.70/0.30 | 1.00/0.00 |
| Oral mucosa + extrathoracic airways | 1.00/0.00 | 1.00/0.00 | 1.00/0.00 | 1.00/0.00 | 1.00/0.00 |
| Brain | 0.10/0.90 | 0.00/1.00 | 0.20/0.80 | 0.10/0.90 | 0.10/0.90 |
| Bone surfaces | 0.01/0.99 | 0.02/0.98 | 0.02/0.98 | 0.01/0.99 | 0.02/0.98 |
| RBM | <0.01/>0.99 | 0.02/0.98 | 0.02/0.98 | <0.01/>0.99 | 0.02/0.98 |
| Skin | 0.01/0.99 | 0.01/0.99 | 0.03/0.97 | 0.02/0.98 | 0.02/0.98 |
| Thyroid | 0.00/1.00 | 0.00/1.00 | 0.00/1.00 | 0.00/1.00 | 0.00/1.00 |
CBCT, cone beam CT; RBM, red bone marrow; TMJ, temporomandibular joint.
Result
For CBCT units, the results were split up by dividing the units into two categories: medium FOV (used for TMJ) and small FOV (used for maxillary impacted canine and mandibular molar area). This allows for a better comparison between protocols, as different FOV sizes are used for different subsets of patients.
Table 3 gives the absorbed organ doses and effective doses for medium FOV (TMJ) protocols. The effective dose ranged between 45 μSv and 129 μSv. The highest absorbed dose was in the parotid salivary gland. The effective dose of the examination with high resolution was nearly three times higher than that for normal resolution with the same FOV (8 × 8 cm). Table 3 also shows the results for the small FOV protocols. The effective dose ranged between 10 μSv and 22 μSv.
Table 3.
Absorbed organ dose (mGy) and effective dose (µSv) for CBCT and panoramic scan protocols
| CBCT-small FOV |
CBCT-medium FOV |
Panorama |
|||||||
| Veraviewepocs® 3De |
Veraviewepocs 3De |
ProMax® 3D |
NewTom VGi® |
NewTom VGi |
NewTom VGi |
Veraviewepocs 3De |
ProMax 3D |
ProMax |
|
| Tissue | Upper jaw (4 × 4) | Lower jaw (4 × 4) | Upper jaw (4 × 5) | TMJ NR (12 × 8) | TMJ NR (8 × 8) | TMJ HR (8 × 8) | Standard | Standard | Standard |
| Parotid glands | 1.890 | 0.900 | 0.840 | 2.400 | 2.130 | 5.700 | 0.700 | 0.650 | 1.000 |
| Oral mucosa + extrathoracic airways | 0.120 | 0.600 | 0.070 | 2.300 | 1.800 | 5.200 | 0.240 | 0.156 | 0.240 |
| Brain | 0.001 | NS | 0.001 | 0.230 | 0.150 | 0.420 | 0.002 | 0.001 | 0.002 |
| Bone surfaces | 0.065 | 0.108 | 0.040 | 0.122 | 0.102 | 0.306 | 0.017 | 0.009 | 0.014 |
| RBM | NS | 0.036 | NS | 0.048 | 0.040 | 0.120 | 0.005 | 0.003 | 0.004 |
| Skin | 0.017 | 0.015 | 0.012 | 0.074 | 0.062 | 0.186 | 0.001 | 0.001 | 0.001 |
| Thyroid | 0.001 | 0.050 | 0.001 | 0.020 | 0.020 | 0.040 | 0.020 | 0.013 | 0.020 |
| Effective dose | 21 | 22 | 10 | 56 | 45 | 129 | 11 | 8 | 14 |
CBCT, cone beam CT; FOV, field of view; HR, high resolution; NR, normal resolution; NS, not significant; RBM, red bone marrow; TMJ, temporomandibular joint.
Veraviewepocs 3De units are manufactured by J Morita MFG Corp., Kyoto, Japan; NewTom VGi by Quantitative Radiology, Verona, Italy; and Promax 3D and Promax by Planmeca, Helsinki, Finland.
The dosimetric results of panoramic imaging are shown in Table 3. The highest absorbed doses were found in the parotid salivary glands (0.65–1.0 mGy). Effective doses range between 8 μSv and 14 μSv. The unit with the highest effective dose is the ProMax using a PSP as a receptor; the unit with the lowest effective dose is the ProMax 3D.The effective dose was 1.8 times higher in ProMax than in ProMax 3D.
For comparison purposes, the effective doses were also calculated as multiples of the average dose of panoramic radiograph of the same study and as a percentage of the average annual dose of 760 µSv in Sweden from natural background radiation.19 Moreover, the excess cases of fatal cancer in 1 million people irradiated was calculated using a risk coefficient of 5.5 × 10−2 Sv−11 (Table 4).
Table 4.
Effective dose and risk as multiple of average panoramic images, days of natural background dose in Sweden and risk of cancer
| Unit/protocol | Effective dose (µSv) | Dose as multiple of average panoramic radiographa | Days of per capita natural background (2.08 µSv per day) | Excess cases of fatal cancer in 1 million peopleb |
| Veraviewepocs 3De®/upper jaw | 21 | 1.9 | 10 | 1.2 |
| Veraviewepocs 3De/lower jaw | 22 | 2.0 | 11 | 1.2 |
| ProMax® 3D/upper jaw | 10 | 0.9 | 5 | 0.6 |
| NewTom VGi®/TMJ, NR (12 × 8) | 56 | 5.1 | 27 | 3.9 |
| NewTom VGi/TMJ, NR (8 × 8) | 45 | 4.1 | 22 | 2.5 |
| NewTom VGi/TMJ, HR (8 × 8) | 129 | 11.7 | 62 | 7.1 |
| Veraviewepocs 3De/panorama | 11 | 1.0 | 5 | 0.6 |
| ProMax 3D/panorama | 8 | 0.7 | 4 | 0.4 |
| ProMax/panorama | 14 | 1.3 | 7 | 0.8 |
Veraviewepocs 3De units are manufactured by J Morita MFG Corp., Kyoto, Japan; NewTom VGi by Quantitative Radiology, Verona, Italy; and Promax 3D and Promax by Planmeca, Helsinki, Finland.
HR, high resolution; NR, normal resolution; TMJ, temporomandibular joint.
Average of three units: ProMax, ProMax 3D, Veraviewepocs 3De (11 µSv).
Based on the same study—calculated by using a risk coefficient of 5.5 × 10−2 Sv−1.
The highest excess cases were associated with the scan protocol used for the TMJ—high resolution, whose effective dose is about 62 days of exposure to background radiation. The lowest fatal cancer excess cases of the CBCT scans were associated with the ProMax 3D upper impacted canine protocol. Its effective dose corresponds to approximately 5 days of exposure to natural background radiation. On the other hand, the effective dose of panoramic radiography was between 4 and 7 days of natural exposure.
Discussion
The results of this study should be interpreted with care owing to the complex relationship between image quality, size of the scanned volume and absorbed dose to different tissues. The main purpose of this study was to develop and test GafChromic film dosimetry rather than to compare the clinical performance of imaging devices.
There are a number of ways to estimate the effective dose. All of them include assumptions, which result in limitations and uncertainties.20
The effective dose corresponds to the risk that also a uniformly distributed dose with the same value in the whole body would represent. It gives a general indication of the level of risk for the X-ray examination in question. It takes into account different organs’ sensitivities to induction of severe late effects and is the preferred quantity for comparing the detrimental effects from different exposure situations to large populations.18
Most studies of dose distribution measurements in oral and maxillofacial radiography are based on TLDs.3–6 The dosemeters are placed inside a phantom in small cavities, which have been drilled in a regular pattern in every slice of the phantom. TLDs have the advantage of being rather sensitive and can measure the absorbed dose down to at least 0.5 mGy with sufficient accuracy. They also have some major drawbacks, namely:
They must be handled with extreme care, and the whole dose measuring procedure, including calibration, is very time-consuming.
Their energy dependence in the diagnostic energy range will result in their response being dependent on the amount of scatter at the measurement point. As the amount of scatter varies within the phantom, the uncertainty of the dose values will increase.
The dosemeters are 3 × 3 × 1 mm3. In an irradiation geometry, where the dose gradients are as steep as 25% per mm, it is obvious that the positioning of the radiation field in relation to the dosemeters can heavily affect the dose values measured.
Radiochromic films, initially intended for dose measurement in radiotherapy, are now also available with higher sensitivity for X-ray diagnostic purposes as GafChromic XR-QA, XR-QA2 and XR-CT. There are some advantages of GafChromic films compared with TLDs, such as easy preparation and adjustable size of the film. The reading process and the digitization procedure for a set of three film sheets take a few seconds, whereas around 1 min or more is necessary for reading one TLD. Furthermore, the GafChromic film will present a continuous “analog”-like dose distribution, where the limit for spatial resolution is set by the pixel size when digitizing the image in the flatbed scanner.
Recent studies have shown that it is possible to use ordinary office flatbed document scanners for radiochromic film scanning.7,21 The film response depends on the film type, batch number and scanning parameters. As for any radiation dosimetry system, uncertainties exist.12
The attenuation of the film was determined experimentally and was found to be two times higher than that of the soft tissue. Thus, the film thickness of 25 μm corresponds to 50 μm of soft tissue, which is negligible for the dose measurement geometry. However, one situation that can occur and can affect the dose measurements is when the central beam of the X-ray field coincides with the film plane. Here, there exist primary photon paths directed along the film plane, which will lead to underestimation of the absorbed dose because of the higher attenuation in the film. We have experimentally determined the underestimation to be in the order of 10%. This will, however, only occur if the central axis of the radiation field coincides with the film plane. We have deliberately avoided this in all measurement situations.
In all settings of different units, the salivary gland tissue received the highest amount of radiation exposure. The salivary gland tissue tends to be in the centre of the imaging field and receives nearly constant exposure during the rotation of the gantry. This is a major reason for the increased effective dose seen when using the newest ICRP 2007 guidelines,18 as the salivary gland tissue had not been previously included in the calculations.
The effective doses of the ProMax 3D-CBCT estimated in the present study were lower than those previously reported.2–4 However, the main explanation for the lower measured doses is likely to be the increase in copper filtration of the X-ray beam and the difference in FOV. A study by Ludlow and Ivanovic22 was based on an early version of the ProMax 3D-CBCT unit. Beginning in 2008, those units were equipped with an additional 0.5 mm of copper filtration to reduce the dose. We also found that the effective dose for Veraviewepocs 3De-CBCT (21 μSv) is higher than that for the ProMax 3D-CBCT (10 μSv) for upper jaw at small FOV. Again, the greatest contribution to the lower measured doses is probably an increase in the copper filtration of the X-ray beam for the ProMax 3D unit and a short exposure time of 2.8–8.3 s, combined with a pulsed output. The ProMax 3D unit used was an upgraded unit of the version that was manufactured in 2011. In the newest model, manufactured in 2012, some parameters are changed for three-dimensional exposure; however, the mAs is constant and the dose should not be affected.
From the results, the effect of FOV positioning can be observed. Comparing an upper jaw canine region with a lower jaw molar region scan from the Veraviewepocs 3De-CBCT, it is clear that there were large differences regarding the absorbed dose for the parotid salivary glands and oral mucosa. On the other hand, the dose to the thyroid was very low because it was outside of the primary beam for all protocols.
The NewTom VGi provides two levels of resolution of the same FOV (8 × 8): high and normal. When the high resolution was selected, the calculated effective dose was 129 μSv. If the normal resolution is chosen, the present study shows that the effective dose can be reduced to about 35% of that with high resolution. When comparing the effective dose from a study by Ludlow,23 it can be seen that a higher effective dose for high resolution (172 μSv) and a normal resolution (51 μSv) of the same FOV were found than those in this study (129–45 μSv). Also, the effective dose of FOV (12 × 8) normal resolution (56 µSv) is lower when compared with the study by Ludlow (69 µSv).23 Difference in dosimetry and variation in phantom position can again account for these differences.
The absorbed dose produced by a CBCT unit is dependent on the imaging parameters used (tube potential, mAs); pulsed beam vs continuous beam; amount, type, and shape of beam filter; full 360° rotation vs partial rotation; limited vs full FOV; and resolution setting. Some of these factors, such as type of beam and filtration, are unique to a specific unit, whereas other factors, such as FOV, are under the control of the operator. In general, smaller FOV, lower radiation dose5 and a shorter scanning time all result in a lower total dose of radiation. Also, the dose levels are lower in a CBCT scan when compared with multislice (CT) scanners.22
We measured the absorbed dose during panoramic exposure with three digital panoramic units equipped with different detectors. Effective doses ranged between 8 μSv and 14 μSv. When PSP, CCD and FPD units were compared, the effective dose of the panoramic unit using the PSP receptor (14 μSv) was higher than those of the CCD and FPD units (8–11 μSv).
When the exposure settings are considered, the panoramic machine (ProMax) with the highest dose uses 74 kV, the highest tube current (12 mA) and the longest exposure time (16 s). The ProMax 3D-Panoramic, yielding the lowest dose, operates at the lowest tube current (9 mA). Differences in the doses measured depend not only on the tube potential, mA and filter but also on the actual exposure time, i.e. if the X-rays are continuous or pulse. The sizes of the radiation field also play a significant role.
Ludlow et al3 evaluated a ProMax (CCD based) panoramic machine operated at 68 kV and 13 mA with a 16 s exposure time and found an effective dose of 24.3 μSv using the ICRP 2007 tissue weights. In our study, an effective dose of 14 μSv was found. Difference in the type of dosimetry, variation in exposure settings and phantom composition and position can account for these differences.
The use of CBCT for diagnosis, dental implant planning and orthodontic treatment is a subject of intense discussion among dental practitioners. The risk associated with exposing a patient to higher levels of radiation must be weighed against the improvements in patient care and the information that is gained through the use of CBCT. This issue must be carefully considered.
In conclusion, GafChromic film can be utilised to map the dose distribution and measure the absorbed organ/tissue dose of CBCT and panoramic radiography. The use of small FOV and standard resolution reduces the dose when compared with larger FOVs of the same ROI or higher resolution.
References
- 1.White SC, Pharoah MJ. The evolution and application of dental maxillofacial imaging modalities. Dent Clin North Am 2008; 52: 689–705, v. 10.1016/j.cden.2008.05.006 [DOI] [PubMed] [Google Scholar]
- 2.European Commission Cone beam CT for dental and maxillofacial Radiology: evidence based guidelines. Radiation Protection Publication 172. Luxembourg, Germany: European Commission; 2012. (accessed 27 June 2012). Available from: http:/ec.europa.eu/energy/nuclear/radiation_protection/doc/publication/172.pdf [Google Scholar]
- 3.Ludlow JB, Davies-Ludlow LE, White SC. Patient risk related to common dental radiographic examinations: the impact of 2007 International Commission on Radiological Protection recommendations regarding dose calculation. J Am Dent Assoc 2008; 139: 1237–1243 [DOI] [PubMed] [Google Scholar]
- 4.Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 2012; 81: 267–271. 10.1016/j.ejrad.2010.11.028 [DOI] [PubMed] [Google Scholar]
- 5.Qu XM, Li G, Ludlow JB, Zhang ZY, Ma XC. Effective radiation dose of ProMax 3D cone beam computerized tomography scanner with different dental protocols. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 110: 770–776. 10.1016/j.tripleo.2010.06.013 [DOI] [PubMed] [Google Scholar]
- 6.Ludlow J, Davies-Ludlow L, Brooks S, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol 2006; 35: 219–226. 10.1259/dmfr/14340323 [DOI] [PubMed] [Google Scholar]
- 7.Boivin J, Tomic N, Fadlallah B, Deblois F, Devic S. Reference dosimetry during diagnostic CT examination using XR-QA radiochromic film model. Med Phys 2011; 38: 5119–5129. 10.1118/1.3622607 [DOI] [PubMed] [Google Scholar]
- 8.Tomic N, Devic S, DeBlois F, Seuntjens J. Reference radiochromic film dosimetry in kilovoltage photon beams during CBCT image acquisition. Med Phys 2010; 37: 1083–1092 [DOI] [PubMed] [Google Scholar]
- 9.Rampado O, Bianchi SD, Peruzzo Cornetto A, Rossetti V, Ropolo R. Radiochromic films for dental CT dosimetry: a feasibility study. Phys Med 2012. 10.1016/j.ejmp.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 10.Brady S, Yoshizumi T, Toncheva G, Frush D. Implementation of radiochromic film dosimetry protocol for volumetric dose assessments to various organs during diagnostic CT procedures. Med Phys 2010; 37: 4782–4792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rampado O, Garelli E, Ropolo R. Computed tomography dose measurements with radiochromic films and a flatbed scanner. Med Phys 2010; 37: 189–196 [DOI] [PubMed] [Google Scholar]
- 12.Devic S. Radiochromic film dosimetry: past, present, and future. Phys Med 2011; 27: 122–134. 10.1016/j.ejmp.2010.10.001 [DOI] [PubMed] [Google Scholar]
- 13.Rink A, Vitkin IA, Jaffray DA. Suitability of radiochromic medium for real-time optical measurements of ionizing radiation dose. Med Phys 2005; 32: 1140. [DOI] [PubMed] [Google Scholar]
- 14.Butson MJ, Cheung T, Yu PK. Measurement of energy dependence for XRCT radiochromic film. Med Phys 2006; 33: 2923–2925 [DOI] [PubMed] [Google Scholar]
- 15.Paelinck L, De Neve W, De Wagter C. Precautions and strategies in using a commercial flatbed scanner for radiochromic film dosimetry. Phys Med Biol 2007; 52: 231. 10.1088/0031-9155/52/1/015 [DOI] [PubMed] [Google Scholar]
- 16.International Commission on Radiation Protection Basic anatomical and physiological data for use in radiological protection: reference values. ICRP publication 89. Ann ICRP 2002; 32: 1–277 [PubMed] [Google Scholar]
- 17.Jee WSS. The skeletal tissues. In: Weiss L. (ed). Histology: cell and tissue biology. 5th edn Kidlington, UK: Elsevier Science Ltd.; 1983. pp. 206–254 [Google Scholar]
- 18.International Commission on Radiation Protection Recommendations of the International Commission on Radiation Protection. ICRP publication 103. Ann ICRP 2007; 37: 1–332. 10.1016/j.icrp.2007.10.003 [DOI] [PubMed] [Google Scholar]
- 19.Vattenfall. Radiation. Reference to Vattenfall AB Environmental Product Declarations S-P-00021 and S-P-00026. 2010 [accessed 15 March 2012]. Available from: http://www.vattenfall.com/en/file/Radiation_12808068.pdf
- 20.Thilander-Klang A, Helmrot E. Methods of determining the effective dose in dental radiology. Radiat Prot Dosimetry 2010; 139: 306–309. 10.1093/rpd/ncq081 [DOI] [PubMed] [Google Scholar]
- 21.Thomas G, Chu R, Rabe F. A study of GafChromic XR Type R film response with reflective-type densitometers and economical flatbed scanners. J Appl Clin Med Phys 2003; 4: 307–314. 10.1120/1.1621373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 106–114. 10.1016/j.tripleo.2008.03.018 [DOI] [PubMed] [Google Scholar]
- 23.Ludlow JB. Effective doses of NewTom VGi variable volume dental CBCT unit. Annual meeting of the American Association of Dental Research (AADR). Tampa, FL: (cited 21–24 March 2012). Available from: http://iadr.confex.com/iadr/2012tampa/webprogram/Paper1570 [Google Scholar]