Abstract
Introduction:
We have evaluated efficacy of diclofenac sodium as pre-emptive analgesia agent in a prospective triple blind placebo controlled randomized clinical trial in a patients undergoing third molar impaction surgery.
Materials and Methods:
Randomization of groups was done by randomization software and two groups were constituted one group receiving placebo pre operatively and then the drug for next five days while the other group was given diclofenac sodium pre operatively and then for five days.
Results:
Results were achieved with help of measurement of outcome variables like postoperative tenderness, swelling and trismus on a visual analogous scale (VAS) and other personalized scale. Collected data shows that there is a significant reduction in the score of postop tenderness in experimental group (P = 0.00), while there is a minimal difference between score of postoperative swelling and tenderness (P > 0.04).
Conclusion:
So, we can conclude that use of diclofenac sodium as a preemptive analgesic agent is beneficial for better pain control in third molar impaction surgery.
Keywords: Diclofenac sodium, pain control, preemptive analgesia, third molar impaction surgery
INTRODUCTION
Effective postoperative pain control is very important factor in our day to day practice. Effective pain control with the help of diclofenac sodium as preemptive analgesic agent in third molar impaction surgery provides better patient compliance following surgery, and prevents occurrence of chronic postoperative pain experience.[1]
For ideal postoperative pain management we need to eliminate or minimize pain and discomfort to the patient. This should be achieved with simple, easily available and economical measure which has very minimum or no adverse effect.
Effective postoperative pain control is achieved by
Preventing the initial neural cascade which leads to hypersensitivity produced by noxious stimuli.[2,3,4,5]
Efficient analgesic agent before the onset of the noxious stimulus to prevent central sensitization and preventing typically painless sensations to be experienced as pain (allodynia).[2,3,4,5]
Various preemptive agents can be used for effective pain control.[6,7,8,9,10,11] We have used oral tablet of diclofenac sodium in 50 mg dose one hour before surgery which is given as a preemptive analgesic agent in experimental group. While in control group placebo it is given one hour before surgery.
With the help of our prospective randomized triple blind placebo-controlled clinical trial, we have evaluated efficacy of diclofenac sodium as preemptive agent in cases of third molar impaction surgery. We have measured postoperative tenderness, swelling and trismus for five postoperative days.
MATERIALS AND METHODS
Sixty patient, both male and female attending the Dept. of of Oral and Maxillofacial Surgery, for removal of impacted third molars had been enrolled in this study. All patients were explained about the study in detail, and the possible complications of the surgery and the drug were discussed with the patient. informed consent was obtained from all patients included for the study. Ethical committee clearance was obtained before starting of study.
The study comprise of two groups of 30 patients each. One group (control group) consist of patients receiving placebo in the preoperative setting (one hour prior to surgery) followed by diclofenac sodium in the postoperative setting three times daily for a period of five days. Second group (experimental group) Had patients receiving diclofenac sodium in the preoperative (one hour prior to surgery) and postoperative settings. Allocation of patients to each group was done by randomization using the software.
The patient, the operating surgeon as well as the evaluating surgeon, all were blinded during the study process.
All patients, were evaluated by the principal investigator. Each patient was assessed at 1 hour postoperatively followed by 3rd and 5th days for swelling, tenderness, trismus and any other complications like nerve injury, infection etc, these findings were recorded on separate form and taken for evaluation after the suture removal.
Criteria for measurement
Pain on a scale of 0 to 10, 0 being absence of pain and 10 being severe pain (VAS).[12]
Swelling, recorded as a following scale: absence of swelling - 0, mild swelling - 1, moderate swelling - 2 and severe swelling - 3.
Trismus, recorded as following scale: absence of trismus - 0, mouth opening >76% - 1, <75% mouth opening >51% - 2, <50% mouth opening >26% - 3 and mouth opening <25% - 4.
Observations and results
At each stage, tenderness, trismus and swelling (Figures 3, 4, 5) were compared between experimental and control group, (Figures 1, 2). Table 1 gives the mean and SD values of these variables for both groups. To compare the tenderness, trismus and swelling between experimental and control groups, non-parametric test “Mann-Whitney” was applied and its P-value was obtained. Throughout the discussion, the level of significance was fixed at 5%.
Figure 3.
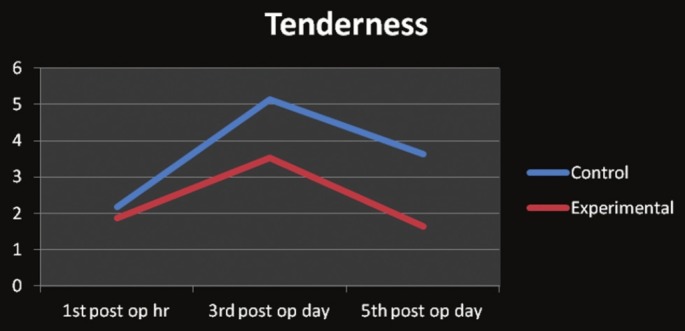
Comparison of rank of tenderness of control and experimental groups
Figure 4.
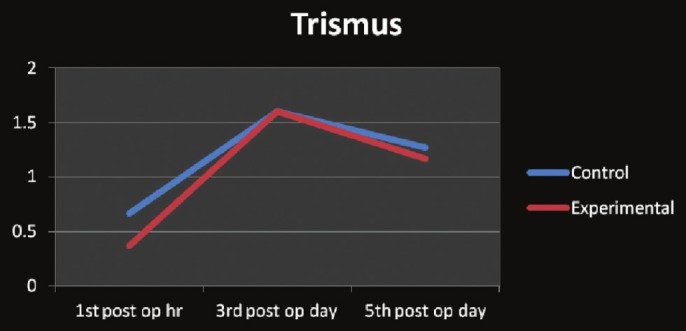
Comparison of rank of trismus of control and experimental groups
Figure 5.
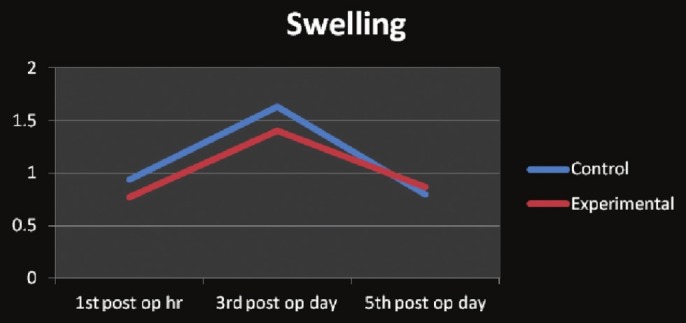
Comparison of rank of swelling of control and experimental groups
Figure 1.
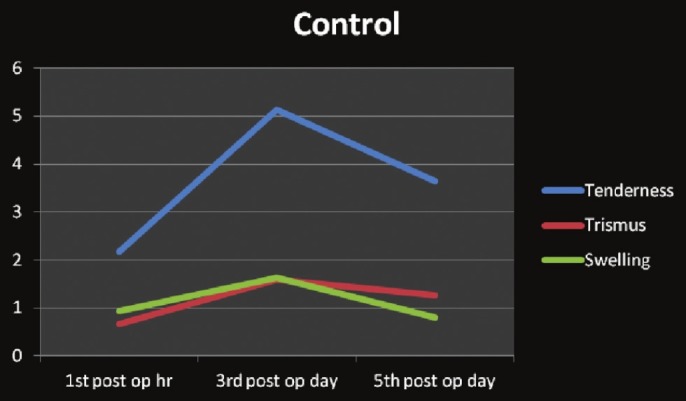
Mean rank of outcomes in control group
Figure 2.
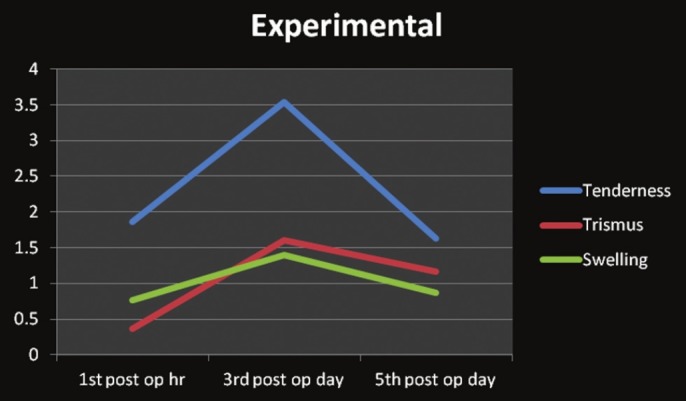
Mean rank of outcomes in experimental group
Table 1.
Comparison between experimental and control groups using Mann-Whitney test
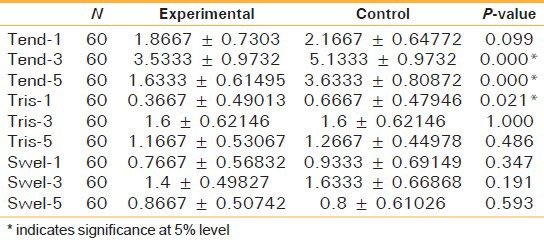
Table 1 shows significant difference in tenderness at 3rd and 5th post operative day between experimental and control groups (P-value <0.05). Trismus and swelling, at any stage, did not see any difference between experimental and control groups (P-value >0.05).
Table 2 shows the comparison of tenderness, trismus and swelling between consecutive two post-operative follow ups at the 3rd and 5th day of surgery. Wilcoxon signed - rank test was used.
Table 2.
Comparison between consecutive two follow-ups: Wilcoxon Signed-Rank Test
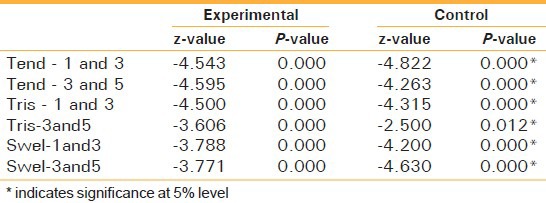
Tables 1 and 2 give the comparison between 1st post-operative hour and 3rd post-operative day as well between 3rd and 5th post-operative day. Tenderness, trismus and swelling shows significant difference between two post-operative follow-ups (P-values are less than 0.05).
DISCUSSION
Results of the derived data is suggestive of better pain control in experimental group. Post-operative score of tenderness shows highly significant difference, between both the groups (P = 0.00) with suggestive low score in the experimental group. Derived data were also suggestive of no significant change (P > 0.04) in both the swelling and trismus.
Definitions of preemptive analgesia
Three different definitions have been used as the basis for the recent clinical trials. Preemptive analgesia has been defined as treatment that: (1) starts before surgery; (2) prevents the establishment of central sensitization caused by incisional injury (covers only the period of surgery) and (3) prevents the establishment of central sensitization caused by incisional and inflammatory injuries (covers the period of surgery and the initial post-operative period).[13]
Prospective study design is a valid method for this kind of research work, so we have designed this study accordingly. There might be chances of biased results from patients as well as from investigator's side if they are aware of time period of consumption of diclofenac sodium but, in this study we have minimized all such bias by making patient, surgeon and investigator blinded and also with and with use of randomization of the patient was done to minimize bias using a software.
Diclofenac sodium is used as preemptive analgesic agent because of its easy ability, economic effective pain control and and relatively safe drug with minimal reported allergy. The plasma half-life of diclofenac sodium is also 1–2 hours, so we can achieve ideal optimal concentration if we provide it in 1-hour preoperatively.
visual analogue scale (VAS) scale is an accepted method for assessment of post-operative pain.[14] Comfort level of the patients are also superior in experimental group than control group as shown with help of derived VAS score.
The mean scores of tenderness in our study at 1-hour post-operatively in the experimental group and control group are 1.86 and 2.16, respectively, with P-value of 0.099 which is less significant; however, the mean scores for 3 days post-operatively for the experimental group and control group are 3.5 and 5.1, respectively, with P-value of 0.001 which is highly significant. Score mean of tenderness on the 6th post-operative day for experimental group is 1.6 and for control group is 3.6 with P value of 0.001 which shows a highly significant difference. And for trismus mean score at 1-hour post-operatively for experimental group is 0.36 and control group 0.66 with P value of 0.02, which shows a significant difference. All other findings show no significance difference.
These achieved results are correlative to the previous studies. Ong, et al.[7] in 2004 conducted a double-blind, randomized, placebo-controlled study where 34 patients had each of their identical-impacted mandibular third molars removed under local anesthesia on two occasions. Throughout the 12-h investigation period, patients reported significantly lower pain intensity scores in the ketorolac pre-treated sides when compared with the post-treated sides. Aoki et al.[11] in 2006 compared the efficacy of the selective cyclooxygenase-2 (COX-2) inhibitor meloxicam for treatment of postoperative oral surgical pain by assessing in a randomized-controlled trial. Patients undergoing unilateral mandibular 3rd molar extraction surgery were allocated to 3 groups, A, B and C. After oral premedication of meloxicam 10 mg in group A, ampiroxicam 27 mg in group B and placebo in group C., post-operative pain was evaluated at the clinic on the 1st, 7th and 14th postoperative day (POD) using a VAS and concluded that COX-2 inhibitor, meloxicam 10 mg, used for premedication reduced post-operative pain compared with control in oral surgery. Pozos-Guillen, et al.[15] in 2007 compared the efficacy of tramadol given before or immediately after surgical extraction of an impacted mandibular third molar under local anesthesia. In this prospective, randomized-controlled, double-blind pilot study, 3 groups of 20 patients each were included: tramadol preoperative, 100 mg intramuscularly (IM) 1 hour before surgery (group A); tramadol postoperative, 100 mg IM immediately after surgery (group B); and saline (group C). This study suggests the preemptive use of tramadol as an alternative for the acute pain treatment after the removal of an impacted mandibular third molar that is carried out under local anesthesia.
Whereas some of the studies show contradictory results from our study. Sisk, et al.,[6] in 1990 conducted a clinical trial for comparison of preoperative and postoperative naproxen sodium for suppression of pain in dental surgery cases. In their trial, they had given naproxen sodium 550 mg 30 min postop in control group while in preemptive group naproxen sodium 550 mg 30 min preop was given. Results are not supportive of the use of preemptive analgesia. Kaczmarzyk, et al.[12] in 2010 conducted a prospective, randomized, double-blinded clinical trial preemptive effect of ketoprofen on postoperative pain following third molar surgery. Ninety six patients were placed into three groups: pre-group (ketoprofen 60 min preoperatively); post-group (ketoprofen 60 min postoperatively); and no-group (placebo) and resulted that initial onset of pain was significantly delayed only in the post-group. Ketoprofen administered after third molar surgery provides more effective pain control than ketoprofen administered before the surgery or placebo.
CONCLUSION
Use of diclofenac sodium orally in 50 mg dose one hour preoperatively as preemptive analgesic agent is economical, effective, easy and safe method of postoperative pain control in mandibular third molar impaction surgery cases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Dickenson AH, Sullivan AF. Subcutaneous formal-ininduced activity of dorsal horn neurons in the rat: Differential response to an intrathecal opiate administered pre or post formalin. Pain. 1987;30:349–60. doi: 10.1016/0304-3959(87)90023-6. [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez-Darder JM, Barbera J, Abellan MJ. Effects of prior anaesthesia on autotomy following sciatic transection in rats. Pain. 1986;24:87–91. doi: 10.1016/0304-3959(86)90029-1. [DOI] [PubMed] [Google Scholar]
- 3.McQuay HJ. Pre-emptive analgesia. Br J Anaesth. 1992;69:1–3. doi: 10.1093/bja/69.1.1. [DOI] [PubMed] [Google Scholar]
- 4.Woolf CJ, Chong MS. Preemptive analgesia—treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993;77:362–79. doi: 10.1213/00000539-199377020-00026. [DOI] [PubMed] [Google Scholar]
- 5.Kelly DJ, Ahmad M, Brull SJ. Preemptive analgesia I: physiological pathways and pharmacological modalities. Can J Anaesth. 2001;48:1000–10. doi: 10.1007/BF03016591. [DOI] [PubMed] [Google Scholar]
- 6.Sisk AL, Grover BJ. A comparison of preoperative and postoperative naproxen sodium for suppression of postoperative pain. J Oral Maxillofac Surg. 1990;48:674–8. doi: 10.1016/0278-2391(90)90048-7. [DOI] [PubMed] [Google Scholar]
- 7.Ong KS, Seymour RA, Chen FG. Preoperative ketorolac has a preemptive effect for postoperative third molar surgical pain. Int J Oral Maxillofac Surg. 2004;33:771–6. doi: 10.1016/j.ijom.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 8.Ong KS, Tan JM. Preoperative intravenous tramadol versus ketorolac for preventing postoperative pain after third molar surgery. Int J Oral Maxillofac Surg. 2004;33:274–8. doi: 10.1006/ijom.2003.0515. [DOI] [PubMed] [Google Scholar]
- 9.Ong KS, Lirk P, Tan JM, Sow BW. The analgesic efficacy of intravenous versus oral tramadol for preventing postoperative pain after third molar surgery. J Oral Maxillofac Surg. 2005;63:1162–8. doi: 10.1016/j.joms.2005.04.028. [DOI] [PubMed] [Google Scholar]
- 10.Pektas ZO, Sener M, Bayram B, Eroglu T, Bozdogan N, Donmez A, et al. A comparison of pre-emptive analgesic efficacy of diflunisal and lornoxicam for postoperative pain management: a prospective, randomized, single-blind, crossover study. Int J Oral Maxillofac Surg. 2007;36:123–7. doi: 10.1016/j.ijom.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Aoki T, Yamaguchi H, Naito H, Shiiki K, Izawa K, Ota Y, et al. Premedication with cyclooxygenase-2 inhibitor meloxicam reduced postoperative pain in patients after oral surgery. Int J Oral Maxillofac Surg. 2006;35:613–7. doi: 10.1016/j.ijom.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 12.Kaczmarzyk T, Wichlinski J, Stypulkowska J, Zaleska M, Woron J. Preemptive effect of ketoprofen on postoperative pain following third molar surgery. A prospective, randomized, double-blinded clinical trial. Int J Oral Maxillofac Surg. 2010;39:647–52. doi: 10.1016/j.ijom.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 13.Kissin I. Preemptive analgesia. Anesthesiology. 2000;93:1138–43. doi: 10.1097/00000542-200010000-00040. [DOI] [PubMed] [Google Scholar]
- 14.Myles PS, Troedel S, Boquest M, Reeves M. The Pain Visual Analog Scale: Is it linear or nonlinear? Anesth Analg. 1999;89:1517–20. doi: 10.1097/00000539-199912000-00038. [DOI] [PubMed] [Google Scholar]
- 15.Pozos-Guillen A, Martinez-Rider R, Aguirre-Banuelos P, Perez-Urizar J. Pre-Emptive analgesic effect of tramadol after mandibular third molar extraction: A pilot study. J Oral Maxillofac Surg. 2007;65:1315–20. doi: 10.1016/j.joms.2006.10.079. [DOI] [PubMed] [Google Scholar]


