Abstract
Objectives:
Study included 20 patients with diagnosis of fascial space infections of odontogenic origin to assess efficacy of serum CRP levels as monitoring tools for determining severity of infections, hospital stay and efficacy of treatment.
Materials and Methods:
Blood samples taken on Day 0, 4 and 8 for measuring serum levels of marker. Simultaneously clinical parameters like swelling size, pain etc. were also recorded on Day 0, 4 and 8 and appropriate treatment given to each patient. Correlation between markers and parameters was found using regression and paired t-test.
Results:
Statistical analysis found strong correlation between lab. values of markes and parameters used to measure severity of infection. Also CRP is significant marker for hospital stay (P<.01).
Interpretation and Conclusion:
Prospective analysis indicates CRP can be effective marker for determining severity of infection, treatment efficacy and hospital stay. Duration of antibiotic usage, intensive unit care, use of nutritional supplements becomes more rationale. Markers also make treatment cost effective and help protecting patients from side effects of excess drug usage.
Keywords: C-reactive protein, odontogenic infection, paired t-test
INTRODUCTION
Patients with fascial space infections of odontogenic origin are at utmost risk for life-threatening situations due to anatomical connectivity of potential spaces to one another. Lethal complications may become inevitable making vigilant scrutiny and monitoring of such patients a necessity.
Although conventional measures to estimate infections such as White Blood Count (WBC) count and Erythrocyte Sedimentation Rate ESR values are valuable in determining state of patient at testing time, the predictability of these is worth limited.[1] The desirability of serum-derived surrogate predictor behavior and outcome cannot be under estimated, arousing interest in identifying substances which could function as prospective monitor of disease progression. Thus, various inflammatory markers came into existence.[1,2,3,4]
C-reactive protein (CRP) was discovered in 1930 in pneumococcal pneumonia patients.[1] CRP is present only in small amounts in normal healthy individuals and is involved in process of innate immune system with functions of compliment activation, antigen clearance, and mediation of phagocytosis by activation of neutrophills.[1,2,5,6] In severe infections or inflammatory reactions, striking rise in serum concentration of CRP is seen up to 1000 fold within few hours of clinical symptoms.[3,6]
CRP concentration raises with infection making it a positive acute phase reactant with a very short half-life of 5–7 h.[1,2,6] Thus, advantage of having short half lives makes serum CRP levels as sensitive indicators of infection.[3,5,6]
So in the present study, we assessed the efficacy of serum CRP levels as monitoring tools in 20 patients with fascial space infections of odontogenic origin, for determining severity of infections, length of hospital stay, and efficacy of treatment regime.
MATERIALS AND METHODS
This randomized prospective study was conducted on patients visiting Department of Oral and Maxillofacial Surgery, with diagnosis of fascial space infections of odontogenic origin. All the patients were treated on in-patient basis. Inclusion criteria was patients with in age group of 17 to 57, any carious or periodontally involved tooth correlated as foci of infection on clinical examination, and radiographic evidence of periapical changes. Exclusion criteria was that the patients who were medically compromised,[2,7] pregnant, chronic alcoholics, on steroid therapy, and on contraceptives. All patients were treated and observed by the same surgeon.[2] Routine laboratory investigations were done along with airway assessment.
At the onset of treatment, discharge samples from infectious site were collected and sent for culture sensitivity and blood sample for assessing values of CRP. Blood samples of all the patients were taken as, T1 – before starting any treatment, T2 – 4th day of treatment, and T3 – 8th day of treatment.
Empirical antibiotic regime was started to control infection and appropriate analgesics were given for pain relief.
Extraction of offending tooth was done if indicated. Incisions were placed keeping facial esthetics, vital structures, and dependent part of swelling into consideration. Infected spaces were explored, locules were broken if present, and decompression done. Irrigation with antibiotic solution was done and continued daily. Penrose drain was placed until discharge stopped. If infection subsided, no further surgical intervention was done and empirical antibiotic therapy continued. But if infection increase or failed to subside, further surgical intervention was done and antibiotic regime changed according to culture and sensitivity reports.
Assessment of patients was done based on various clinical parameters on every 4th day and correlated with laboratory values of serum CRP. Clinical parameters to assess infection were divided into signs and symptoms. Signs used were change in size of swelling (using thread and scale), mouth opening (measuring central incisor distance), active discharge (1 if present and 0 if absent), and number of spaces involved (using clinical observation and CT scan). Symptoms recorded were pain (visual analogue scale), dysphagia (1 if present and 0 if absent), and hoarseness of voice (1 if present 0 if absent).
Serum CRP levels above 11 mg per dl depict definite infection. Treatment regime was considered effective if laboratory values of both inflammatory markers and clinical parameters showed improved condition of patients. Patients were followed up for a period of 1 month.
RESULTS
This was a randomized prospective study conducted on 20 patients with diagnosis of fascial space infections of odontogenic origin. Statistical package used in this study was paired t-test and regression analysis.
The patients were within age group of 17 to 57 years with 90% males and 10% females. The mean age of males was 40.78 ± 8.41 and that of females was 40 ± 15.56 years. Mandible was involved in 16 patients (80%) and 4 patients (20%) had infection of maxillary origin. The most prevalent microorganism isolated was streptococcus (85%).
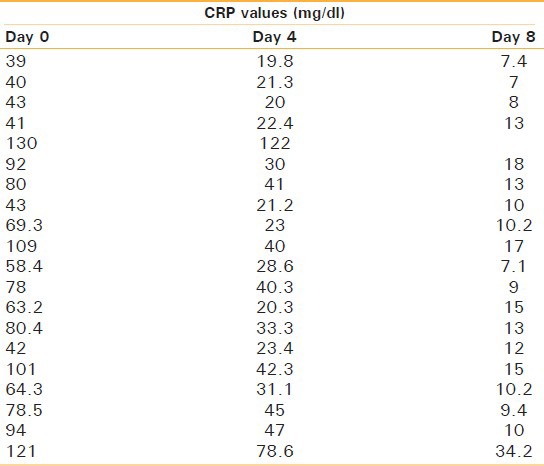
The severity of infection and effectiveness of treatment regime were determined using correlation between clinical parameters and laboratory values of serum CRP [Table 1] using regression test.
Table 1.
CRP levels of patients on day 0, 4, and 8
The relation of CRP with the clinical signs and symptoms was also evaluated using the same method. On first day, the regression equation explained the direct and linear relation between CRP and size of swelling with CRP being significant predictor of size of swelling (P < 0.01). The data for mouth opening explained an inverse relation between CRP and mouth opening. Regression also proved CRP being a significant predictor of mouth opening (P < 0.01). Number of fascial spaces involved was directly proportional to CRP values. The regression equation implied that for every one unit increase in CRP, there was an increase of 0.04 units in number of spaces and 56.2% of the variation in number of fascial spaces was explained by CRP values. Similarly regression equation for pain showed direct relationship with CRP. With every one unit increase in CRP, there was an increase of 0.01 units in pain and 12.03% of the variation in pain could be explained by CRP values. The analyzed data also showed that 20 patients (100%) included in study had discharge present on day 1. Dysphagia was seen in 13 patients (65%) and 8 patients (40%) had hoarseness of voice.
Day 4: The values obtained on day 4 were again evaluated using the same method.
The regression equation explained the direct and linear relation between CRP and size of swelling, CRP being significant predictor of size of swelling (P < 0.01) having R values of 35.94%. The data for mouth opening explained an inverse relation between CRP and mouth opening. Equation proved that CRP was a significant predictor of mouth opening (P < 0.01) having R values of 47.71%. Contrary to mouth opening the number of fascial spaces involved was directly proportional to CRP values. The regression equation for number of spaces implied that for every one unit increase in CRP, there was an increase of 0.04 units in number of spaces and 53.28% of the variation in number of spaces was explained by CRP values. Similarly, regression equation for pain showed direct relationship with CRP. With every one unit increase in CRP, there was an increase of 0.03 units in pain and 4.73% of the variation in pain could be explained by CRP values. The data also showed that 75% of patients included in study had discharge present on day 4. Dysphagia was seen in 30% of patients and 15% of patient had hoarseness of voice. Day 8: The regression equation explained direct and linear relation between CRP and size of swelling, but CRP was not a significant predictor of size of swelling (P > 0.05) having R values of 17.9%. The data for mouth opening explained an inverse relation between CRP and like swelling size CRP was also not a significant predictor of mouth opening (P > 0.05) having R values of 19.2%. Number of spaces involved was directly proportional to CRP values. The regression equation implied that for every one unit increase in CRP, there was an increase of 0.10 units in number of spaces and 49.82% of the variation in number of spaces was explained by CRP values. Similarly, regression equation for pain showed direct relationship with CRP. With every one unit increase in CRP, there was an increase of 0.05 units in pain and 8.1% of the variation in pain could be explained by CRP values. The data showed that none of patients included in study had discharge present on day 8. Dysphagia was seen in four patients (20%) and one patient (5%) had hoarseness of voice.
The above statistical analysis finds strong correlation between laboratory values of marker with clinical parameters used to measure severity of infection. The analysis also proved that values of marker significantly changed and moved toward normal as the condition of patient improved with effective treatment. On the other hand, there was minimal change in the values of markers for a patient whose condition did not improve and patient died (fifth patient) on 6th day. Thus, study proved that CRP is significant predictors of severity of infection and effectiveness of treatment regime.
Analysis of hospital stay
We noticed that CRP was also a significant predictor for hospital stay (P < 0.001). The regression equation shows that there was a linear relationship between CRP and hospital stay, i.e., higher the CRP level, higher was the hospital stay. R2 = 0.4011 implies that 40.11% of variation in hospital stay was explained by CRP [Figure 1].
Figure 1.
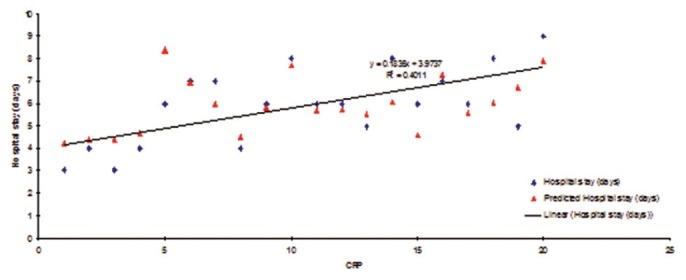
Relationship between CRP and hospital stay
DISCUSSION
The acute phase response is a complex set of systemic and metabolic reactions elicited by infections or other causes of injury. Besides other physiological, metabolic, and biochemical changes, the acute phase response is characterized by alterations in the hepatic synthesis and serum levels of some proteins. Thus, while the levels of positive acute phase proteins like CRP, complement 3, serum amyloid A, alpha-1, and glycoprotein, etc., increase due to stimulation of hepatic synthesis, depression of hepatic production of visceral transport proteins (negative acute phase proteins) like albumin, transferring, thyroxin binding prealbumin (TBPA), and retinol binding proteins (RBP), etc., occurs.[8,9]
Several reports have indicated that visceral transport proteins, mainly those with a low turnover rate, like TBPA, RBP are useful to evaluate protein and protein energy under nutrition as well as to monitor nutritional recovery during nutrient repletion. However, the presence of infection results in depression of their hepatic production as well as increased passage to the extra vascular space, consequently diminishing their serum levels making them markers for acute phase conditions.[9,10]
Similarly CRP, which is present in only small amounts in healthy individuals, is involved in several processes of the unspecific immunologic defense. In severe infections or inflammatory reactions, a striking rise in the serum concentration is often seen. This suggests the possibility that rise of CRP is sufficiently rapid and specific to serve as a definitive aid in the early diagnosis of septicemia.[6] Thus, based on these properties of the markers attempt has been made to use them in patients with fascial space infections.[2,4]
In the present study, we found that CRP had a high degree of correlation with severity of infection having P value < 0.01 from day 0 and day 4. These results were similar to study conducted by Pinilla et al., where they found statistically significant correlation between prealbumin and CRP at 2nd day (r = 0.45, P < 0.01) and 5th day (r = 0.53, P < 0.01) in infection patients.[9] CRP levels were found to be significantly high (P < 0.01) in most of patients of space infections of odontogenic origin. Similar results were obtained by Ren et al.[2] and Ylijoki et al.[1] where CRP levels declined significantly when effective treatment was given to the patient.
In this study, CRP was also a significant predictor for hospital stay (P < 0.001). The regression equation shows that there was a linear relationship between CRP and hospital stay, i.e., higher the CRP level, more was the hospital stay. These results go well in accordance with study of Ylijoki et al.[1] They also found CRP to be a significant predictor for hospital stay (P < 0.001).
CONCLUSION
The findings of this prospective analysis indicate that CRP is effective markers for determining severity of infection, efficacy of treatment regime, and length of hospital stay for patients with fascial space infections of odontogenic origin. Serum CRP reflects immediate effect of the treatment. The duration of antibiotic usage, need for intensive care, and use of additional nutritional supplements become more rationale if these measurements are incorporated in clinical decisions. Thus, we conclude that CRP should be incorporated as monitoring tools for managing patients with fascial space infections of odontogenic origin.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ylijoki S, Suuronen R, Jousimies-Somer H, Meurman JH, Lindqvist C. Differences between patients with or without the need for intensive care due to severe odontogenic infections. J Oral Maxillofac Surg. 2001;59:867–72. doi: 10.1053/joms.2001.25017. [DOI] [PubMed] [Google Scholar]
- 2.Ren YF, Malmstrom HS. Rapid quantitative determination of C-reactive protein at chair side in dental emergency patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:49–55. doi: 10.1016/j.tripleo.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Sganga, et al. Hepatic protein repriosation after trauma and sepsis. J Surg. 1985;120:189–99. [Google Scholar]
- 4.Cunningham LL, Jr, Madsen MJ, van Sickels JE. Using prealbumin as an inflammatory marker for patients with deep space infections of odontogenic origin. J Oral Maxillofac. 2006;64:375–8. doi: 10.1016/j.joms.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Sann L, Bienvenu F, Bienvenu J, Bourgeois J, Bethenod M. Evolution of serum prealbumin, C-reactive protein, and orosomucoid in neonates with bacterial infection. J Pediatr. 1984;105:977–81. doi: 10.1016/s0022-3476(84)80094-3. [DOI] [PubMed] [Google Scholar]
- 6.Sabel KG, Wadsworth C. C-reactive protein (CRP) in early diagnosis of neonatal septicemia. Acta Paediatr Scand. 1979;68:825–31. doi: 10.1111/j.1651-2227.1979.tb08219.x. [DOI] [PubMed] [Google Scholar]
- 7.Stahl WM. Acute phase protein response to tissue injury. Crit Care Med. 1987;15:545–50. doi: 10.1097/00003246-198706000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Malavé I, Vethencourt MA, Pirela M, Cordero R. Serum levels of thyroxine binding prealbumin, C-reactive protein and IL-6 in protein-energy undernourished children and normal controls without or with associated clinical infections. J Trop Pediatr. 1998;44:256–62. doi: 10.1093/tropej/44.5.256. [DOI] [PubMed] [Google Scholar]
- 9.Pinilla JC, Hayes P, Laverty W, Arnold C, Laxdal V. The C-reactive protein to prealbumin ratio correlates with the severity of multiple organ dysfunction. Surgery. 1998;124:799–805. doi: 10.1067/msy.1998.91365. [DOI] [PubMed] [Google Scholar]
- 10.Bárány P. Inflammation, serum C-reactive protein and erythropoietin resistance. Nephrol Dial Transplant. 2001;16:224–7. doi: 10.1093/ndt/16.2.224. [DOI] [PubMed] [Google Scholar]


