Abstract
The classical features of superior orbital fissure syndrome arise due to compression of all or some anatomical structures passing through the fissure. A conservative approach is advocated in this condition unless there is a bony impingement of the neuronal structure and/or simultaneous compression of optic nerve leading to blindness or diminished vision. This paper reports three cases of this rare complex and also presents a review of literature.
Keywords: Ophthalmoplegia, orbital trauma, proptosis, ptosis, superior orbital fissure
INTRODUCTION
The superior orbital fissure syndrome (SOFS) is a complex of impaired function of the cranial nerves (III, IV, V, and VI) that enter the orbit through the superior orbital fissure (SOF). Three major precipitating factors for SOFS are trauma, tumor, and inflammation. SOFS of traumatic origin was first described by Herschfeld in 1858.[1] In 1896, Rochon-Duvignaud reported the syndrome as a pathological entity in four syphilis patients,[2] and Lakke defined the complete syndrome in 1962.[3] Any unnatural narrowing of SOF due to trauma of high impact to the upper and midface (frontobasal skull, Le Fort II, III, and zygomatic complex fractures) can precipitate this condition.[4,5,6] Direct bony compression of the contents of the SOF and/or a compression hematoma may cause the signs and symptoms of the syndrome which are either complete or partial depending upon the degree of compression of its related anatomical structure [Table 1]. The syndrome can precipitate itself after reduction of a midface fracture where it was absent previously.[7] The purpose of this paper is to present three new cases managed with megadose steroid therapy and review the literature of this rare complex.
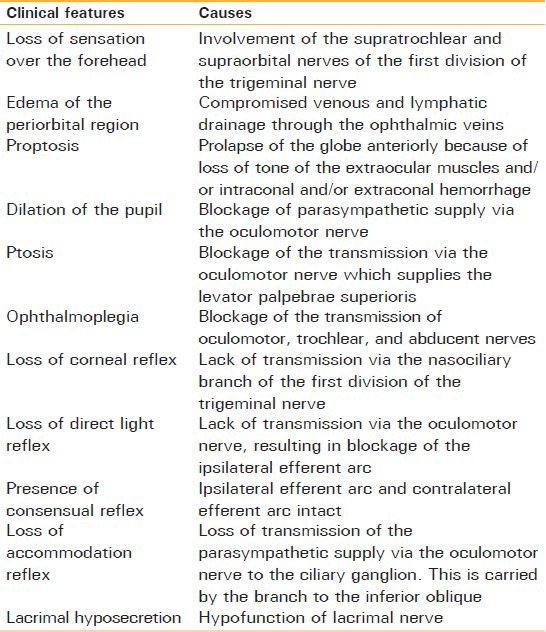
Table 1.
Clinical features of superior orbital fissure syndrome with their causes
CASE REPORTS
Case 1
A 26-year-old male suffered injury due to road traffic accident and reported to the maxillofacial unit after 5 days with the complaint of pain and tenderness over the left cheek region, inability to move the left eye, and numbness over the left forehead. On examination, there was mild swelling on the left half of the face with partial ptosis of the left eye. There was mild proptosis and periorbital edema but marked subconjunctival hemorrhage in left eye [Figure 1a]. Pupil was dilated with vision intact and there was complete absence of movement of eyeball in all the gazes. On ophthalmic examination, there was loss of corneal reflex, loss of direct light reflex, presence of consensual reflex, and loss of accommodation reflex. An ophthalmologic consultation revealed normal fundoscopic findings. On palpation, there was tenderness at the left fronto-zygomatic suture and infraorbital rim. His mouth opening was normal. A computerized tomography (CT) scan showed proptosis of the left eye with no intraconal or extraconal hemorrhage. There was fracture of the lateral wall of the orbit with obvious bony impingement on the lateral rectus. The medial wall and the ethmoidal sinuses were uninvolved [Figure 1b]. A diagnosis of fracture of left zygomatic bone with SOFS was made. The patient was managed with megadose steroid (loading with 30 mg/kg methylprednisolone followed by 15 mg/kg every 6 h for 3 days) and anti-inflammatory drugs. There was partial improvement in the ptosis, proptosis, and ophthalmoplegia after 2 weeks. At the end of 6 weeks, there was complete recovery of ptosis and ophthalmoplegia [Figure 1c].
Figure 1.
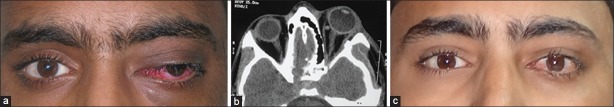
(a) Case 1. Frontal view depicting partial proptosis and ptosis with fixed gaze. (b) Axial CT scan depicting proptosis in left eye. (c) Recovery after the end of 8 weeks
Case 2
A 20-year-old female reported with a chief complaint of pain and swelling on the left half of the face and inability to open her left eye. She had suffered injury few hours back when a rotatory machine belt reportedly broke and directly hit the left side of her face with high impact. Her left half of the face was swollen with complete ptosis of the left eye [Figure 2a]. There was proptosis, periorbital edema, and ecchymosis, but no subconjunctival hemorrhage. The left pupil was fixed and dilated with vision intact and there was complete absence of movement of eyeball in all the gazes [Figure 2b]. On further ophthalmic examination, there was loss of corneal reflex, loss of direct light reflex, presence of consensual reflex, and loss of accommodation reflex. Ophthalmic consultation was done and fundoscopic findings were normal. On palpation, there was depression and tenderness over the zygomatic arch region with tenderness at the fronto-zygomatic suture and the infraorbital rim. There was paresthesia over the left forehead, but sensation over the left infraorbital nerve distribution was normal. Her mouth opening was reduced (2.0 cm) with tenderness at the zygomatic buttress region intraorally. An occipito-mental view of skull showed generalized opacification of the left maxillary sinus with fracture of the zygomatic bone. A CT scan showed marked proptosis of the left eye with no intraconal or extraconal hemorrhage. There was fracture and mild buckling in of the lateral wall of the orbit. The medial wall and the ethmoidal sinuses were uninvolved [Figure 2c]. A diagnosis of fracture of left zygomatic bone with SOFS was made. The patient was managed conservatively with megadose steroid and anti-inflammatory drugs. There was partial improvement in the ptosis, proptosis, and ophthalmoplegia after 2 weeks, after which reduction of the fracture without fixation was done intraorally under local anesthesia. Intraoperative check was maintained for any aggravation of signs and symptoms (e.g., an acute pain in retrobulbar region). The mouth opening improved intraoperatively. The patient was followed at regular interval and her condition improved over the period with mild ptosis still persistent at the end of 8 weeks. The patient was lost to further follow-ups.
Figure 2.

(a) Case 2. Frontal view showing complete ptosis and periorbital edema. (b) Dilated and fixed pupil with complete absence of movement of eyeball on left side. (c) Axial CT scan showing marked proptosis and fracture of the lateral wall of orbit on left side
Case 3
A 38-year-old male suffered facial injury due to road traffic accident 12 days back. He was managed conservatively in a peripheral health center for head injury and was referred to the ophthalmology unit at our hospital. The diagnosis of SOFS was made by the ophthalmologist and the patient was further referred to the maxillofacial unit for opinion regarding facial fractures. On examination, there was bilateral circumorbital ecchymosis and subconjunctival hemorrhage. There was marked proptosis in the right eye [Figure 3a]. The eyeball was fixed in a lateral gaze. Pupil was dilated with vision intact and there was complete absence of movement of eyeball in all the gazes [Figure 3b]. Ophthalmic examination revealed loss of corneal reflex, loss of direct light reflex, presence of consensual reflex, and loss of accommodation reflex. On palpation, there was depression and tenderness over the zygomatic arch region with tenderness at the fronto-zygomatic suture and the infraorbital rim. A CT scan showed marked proptosis of the right eye with no intraconal or extraconal hemorrhage [Figure 3c]. The patient was already on the regimen of megadose steroids prescribed by the ophthalmologist. There was partial improvement in the ptosis, proptosis, and ophthalmoplegia after 4 weeks. The patient was lost to further follow-up.
Figure 3.

(a) Case 3. Partial ptosis, circumorbital edema, ecchymosis and subconjunctival hemorrhage. (b) Marked proptosis, wide pupil, and fixed lateral gaze in right eye. (c) Axial CT scan showing proptosis in right eye
DISCUSSION
The SOF separates the lateral wall and the roof of the orbit and also the greater and the lesser wing of sphenoid. It serves as a pathway between the orbit and the middle cranial fossa. The shape of SOF is like a pear with the long axis extending upward at an angle of 45° from the broad base medially to the apex laterally [Figure 4]. Reymond, et al. in their cadaveric study on 100 skulls concluded that SOF had mainly two morphological variants: Type “a” with characteristic narrowing within the fissure and type “b” which lacked such narrowing and was significantly shorter. The morphological types of the SOF did not present any statistical variation correlating with gender and body type. The size of the SOF in an adult is around 22 mm in length, 2-3 mm in width at the apex, and 7-8 mm at the base.[8] The tendon of the lateral rectus muscle divides the fissure into two parts: The superior part contains trochlear nerve (IV), frontal and lacrimal branches of the ophthalmic division of the trigeminal nerve (V), and the superior branch of ophthalmic vein; and the inferior part which is confined within the tendinous ring contains superior and inferior branches of the oculomotor nerve (III), abducens nerve (VI), nasociliary nerves (V), and the inferior branch of ophthalmic vein, making them more susceptible to shearing injury during craniofacial trauma.
Figure 4.

Diagrammatic representation of right superior orbital fissure with its content (1. lacrimal nerve; 2. frontal nerve; 3. trochlear nerve; 4. superior branch of ophthalmic vein; 5. superior branch of oculomotor nerve; 6. nasociliary nerve; 7. inferior branch of oculomotor nerve; 8. abducens nerve; 9. inferior branch of ophthalmic vein)
In a review of 11,284 patients of craniofacial fractures, Chen and Chen found 33 cases of SOFS (0.3%).[9] Similar studies of large sample size of maxillofacial trauma patients have shown the incidence to be less than 1%.[10,11] It is a complex consisting of periorbital swelling, proptosis, ptosis, numbness of forehead, and paralysis of extraocular muscles due to impairment of III, IV, VI, and the first division of V cranial nerve. An SOFS does not involve the optic nerve and the vision is unaffected. With involvement of the optic nerve and a subsequent compromised vision, the condition is known as orbital apex syndrome where orbital exploration may be recommended on an emergency basis.[11,12] Cranial nerve IV is the least severely injured and achieves the highest level of functional outcomes. In contrast, cranial nerve VI is the most severely injured. This can be the result of its passage through the common tendinous ring and close proximity to the greater wing of sphenoid bone and its long intracranial course.[13]
The rationale behind the treatment of SOFS of traumatic origin lies primarily in minimizing further irreparable damage to the neuronal structures. Fracture repair and restoration of the bony anatomy come secondary. Because of relatively small number of cases reported, no specific guidelines have been clearly defined. But a general consensus lies toward initial observation period of 10-14 days before any surgical manipulation of fracture segments is done.[14] This prevents any hazard of further hemorrhage, involvement of the orbital apex (optic nerve), or injury to the other nerves.
Initial steroid therapy has shown to affect the prognosis of the condition. Postma, et al. (1982) first reported the short-term use of dexamethasone (4 mg every 6 h) in patients with traumatic SOFS. Neurologic sign and ocular symptoms recovered at the 3-month follow-up.[15] Rohrich, et al. showed similar encouraging results with loading dose of 1 mg/kg dexamethasone followed by 0.5 mg/kg every 6 h to treat SOFS in addition to the reduction of associated facial fracture.[16] Recently, Acarturk, et al. reported excellent outcome in five patients with traumatic SOFS using megadose steroid of 30 mg/kg methylprednisolone followed by 5.4 mg/kg/h for 48 h.[17] The literature on steroid treatment of traumatic SOFS shows that the patients treated with steroids have a better chance of neurologic recovery than those with observation alone.[9] Reduction in swelling and edema helps decompress the contents of the fissure and restoration of neuronal function. The current regimen of steroid therapy is methylprednisolone 30 mg/kg loading dose followed by 15 mg/kg every 6 hourly for 3 days. This parentral therapy is followed by regular tapering of oral steroid. Improvement reaches its plateau by the end of 6 months.[9,13]
Surgical intervention is considered when there is an obvious retrobulbar hematoma showing no signs to resolve. An exploration of the orbital apex through a lateral transconjunctival orbitotomy to evacuate the blood can be successful in such situation. A CT scan depicting an evident bony compression from a displaced sphenoid fracture or an orbital blow-in fracture with narrowing of SOF should prompt for a surgical decompression to reduce intraorbital pressure. Chen and Chen propose direct decompression of SOF through the coronal approach and zygomatic osteotomy. This is followed by reduction of sphenoid bone under direct vision.[9]
In summary, SOFS is a rare complication of craniofacial injury. Diagnosis is based on clinical presentation which can be confirmed by radiological examination. In the absence of compression by the fracture fragments, conservative approach with megadose steroids should be the first line of treatment. The prognosis may not be as good if symptoms are caused by displaced bony fragments. With an evident bony compression, a surgical decompression should be planned. The associated facial fractures, especially orbital blow-in fracture, should be reduced early to relieve intraorbital pressure, if the general condition is stable. Partial to complete recovery of cranial nerve function can be expected after proper treatment and improvement reaches its plateau by the end of 6 months.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Hirschfeld DL. Epanchement de Sang dans le Sinus Caverneux de Cote Gauche Diagnostique Pendant la Vie. Comptes Rendus de Societe Biologique. 1858:138. [Google Scholar]
- 2.Rochon-Duvignaud A. Quelques cas de paralysis de tous les nerfs orbitaires (ophthalmoplegia totale avec amaurose et anesthesia dans le domaine de l’ophthalmique), d’originesyphilitique. Arch Ophthalmol (0aris) 1896;16:746–60. [Google Scholar]
- 3.Lakke JP. Superior orbital fissure syndrome: Report of a case caused by local pachymeningitis. Arch Neurol. 1962;7:289–300. doi: 10.1001/archneur.1962.04210040041004. [DOI] [PubMed] [Google Scholar]
- 4.Banks P. The superior orbital fissure syndrome. Oral Surg Oral Med Oral Pathol. 1967;24:455–8. doi: 10.1016/0030-4220(67)90418-5. [DOI] [PubMed] [Google Scholar]
- 5.Pogrel MA. The superior orbital fissure syndrome: Report of a case. J Oral Surg. 1980;38:215–7. [PubMed] [Google Scholar]
- 6.Llorente Pendas S, Albertos Castro JM. Traumatic superior orbital fissure syndrome: Report of a case. J Oral Maxilofac Surg. 1995;53:934–6. doi: 10.1016/0278-2391(95)90285-6. [DOI] [PubMed] [Google Scholar]
- 7.Fujiwara T, Matsuda K, Kubo T, Tomita K, Yano K, Hosokawa K. Superior orbital fissure syndrome after repair of maxillary and naso-orbito-ethmoid Fractures: A Case Study. J Plast Reconstr Aesthet Surg. 2009;62:565–9. doi: 10.1016/j.bjps.2008.11.052. [DOI] [PubMed] [Google Scholar]
- 8.Reymond J, Kwiatkowski J, Wysocki J. Clinical anatomy of the superior orbital fissure and the orbital apex. J Craniomaxillofac Surg. 2008;36:346–53. doi: 10.1016/j.jcms.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 9.Chen C, Chen Y. Traumatic superior orbital fissure syndrome: Current management. Craniomaxillofac Trauma Reconstr. 2010;3:9–16. doi: 10.1055/s-0030-1249369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Antonyshyn O, Gruss JS, Kassel EE. Blow-in fractures of the orbit. Plast Reconstr Surg. 1989;84:10–20. doi: 10.1097/00006534-198907000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Zachariades N, Vairaktaris E, Papavassiliou D, Triantafyllou K, Mezitis M. Orbital apex syndrome. Int J Oral Maxillofac Surg. 1987;16:352–4. doi: 10.1016/s0901-5027(87)80158-3. [DOI] [PubMed] [Google Scholar]
- 12.Kjoer I. A case of orbital apex syndrome in collateral pansinusitis. Acta Ophthalmol. 1945;23:357. [Google Scholar]
- 13.Chen C, Wang T, Tsay P, Huang F, Lai J, Chen Y. Traumatic superior orbital fissure syndrome: Assessment of cranial nerve recovery in 33 cases. Plast Reconstr Surg. 2010;126:205–12. doi: 10.1097/PRS.0b013e3181dab658. [DOI] [PubMed] [Google Scholar]
- 14.Zachariades N. The superior orbital fissure syndrome: Review of the literature and report of a case. Oral Surg Oral Med Oral Pathol. 1982;53:237–40. doi: 10.1016/0030-4220(82)90296-1. [DOI] [PubMed] [Google Scholar]
- 15.Postma MP, Seldomridge GW, Vines FS. Superior orbital fissure syndrome and bilateral internal carotid pseudoaneurysms. J Oral Maxillofac Surg. 1982;48:503–8. doi: 10.1016/0278-2391(90)90241-s. [DOI] [PubMed] [Google Scholar]
- 16.Rohrich RJ, Hackney FL, Parikh RS. Superior orbital fissure syndrome: Current management concepts. J Craniomaxillofac Trauma. 1995;1:44–8. [PubMed] [Google Scholar]
- 17.Acarturk S, Sekucoglu T, Kesiktas E. Mega dose corticosteroid treatment for traumatic superior orbital fissure and orbital apex syndromes. Ann Plast Surg. 2004;53:60–4. doi: 10.1097/01.sap.0000106424.54415.dc. [DOI] [PubMed] [Google Scholar]


