Abstract
Influenza viruses pose a major public health burden to communities around the world by causing respiratory infections that can be highly contagious and spread rapidly through the population. Despite extensive research on influenza viruses, the modes of transmission occurring most often among humans are not entirely clear. Contributing to this knowledge gap is the lack of an understanding of the levels of infectious virus present in respirable aerosols exhaled from infected hosts. Here, we used the ferret model to evaluate aerosol shedding patterns and measure the amount of infectious virus present in exhaled respirable aerosols. By comparing these parameters among a panel of human and avian influenza viruses exhibiting diverse respiratory droplet transmission efficiencies, we are able to report that ferrets infected by highly transmissible influenza viruses exhale a greater number of aerosol particles and more infectious virus within respirable aerosols than ferrets infected by influenza viruses that do not readily transmit. Our findings improve our understanding of the ferret transmission model and provide support for the potential for influenza virus aerosol transmission.
INTRODUCTION
Influenza A viruses are capable of spreading rapidly among immunologically vulnerable populations, causing annual epidemics and global pandemics. The ability of influenza viruses to transmit between hosts is dependent on multiple host, viral, and environmental factors, and transmission does not always occur in the same manner. Three modes of influenza virus transmission have been described (1). Contact transmission includes direct contact between infected individuals and indirect contact with fomites. Droplet transmission occurs when large particles that are typically sprayed from a cough or sneeze contact someone's respiratory mucosa or conjunctiva. Aerosol (AR) transmission (also called airborne or droplet nucleus transmission) occurs when small particles that have a slower settling velocity and can remain suspended in the air for prolonged periods of time are inhaled by susceptible hosts. Aerosol transmission may occur in a close range, where virus-containing aerosols are more concentrated and a higher infectious dose may be inhaled, or over a long range, where the virus has become more dilute, resulting in a lower infectious dose. Much debate surrounds the relative predominance of each mode of transmission among people, and a universal cutoff aerodynamic diameter to distinguish the size of droplets from that of droplet nuclei has not been agreed upon. For the purposes of this study, we use a cutoff of 5 μm because particles of this size can be respired and reach alveolar tissues of the lower respiratory tract; nevertheless, attention should also be given to particles of larger size (up to 10 μm) that can be inhaled and deposited in the upper airways (2).
Despite continued debate over the mode of transmission responsible for the majority of transmission events among humans, the importance of aerosols to indoor transmission has found considerable support (3, 4) although the incidence of long-range aerosol transmission continues to be questioned (5). A recent proof-of-concept study confirmed the potential benefits of human challenge studies in identifying secondary attack rates in controlled social settings representing various levels of exposure (6). Additionally, recent reports of the size distribution of aerosols exhaled by people during coughing after influenza virus infection and the detection of infectious virus in respirable aerosols exhaled by infected individuals highlight the need for a better understanding of the potential role of aerosols in influenza virus transmission (7, 8).
Because of the inherent limitations of human studies, mammalian models have been developed to study influenza virus transmission. The ferret has become a popular model for this purpose because of its natural susceptibility to influenza viruses and because it recapitulates the general disease and transmissibility phenotypes observed in human influenza virus infection (9). Ferrets are often used to characterize the ability of emerging influenza viruses to transmit through the air to assess their pandemic potential (10, 11). We recently evaluated differences in influenza virus infections in ferrets inoculated intranasally (IN) or by aerosol (AR) inhalation and found that AR inoculations can result in disease that more closely resembles naturally acquired infections (12); however, questions remain about how these differences may affect virus transmission. Due to the limited information that has been reported on the aerosol shedding patterns of influenza virus-infected ferrets (12, 13) and the need for improved techniques of sampling infectious influenza virus in aerosols, we set out to analyze the aerosol shedding patterns of ferrets inoculated IN or by AR and determine the level of infectious virus present in respirable aerosols (<5 μm). By comparing these parameters among a panel of human and avian influenza viruses exhibiting diverse transmissibility efficiencies in ferrets, we found that animals infected by highly transmissible viruses exhale more aerosol particles and more infectious virus within aerosol particles than those infected by influenza viruses that do not readily transmit among ferrets. These findings have important implications in our understanding of the ferret transmission model and the potential for influenza virus aerosol transmission.
MATERIALS AND METHODS
Viruses.
A panel of five human and avian influenza A viruses was evaluated, including two seasonal influenza viruses, A/Panama/2007/99 (H3N2; PN99) and A/Solomon Islands/03/06 (H1N1; SI06), influenza A H1N1 pdm09 virus A/Mexico/4482/09 (MX09), and two highly pathogenic avian influenza (HPAI) H5N1 viruses, A/Thailand/16/04 (TH04; clade 1) and A/Bangladesh/5487/11 (BD11; clade 2.2.2). Virus stocks of PN99, SI06, and TH04 were propagated in the allantoic cavities of 10-day-old embryonated hens' eggs as previously described (14). Virus stocks for MX09 and BD11 were grown in Madin-Darby canine kidney (MDCK) cells as previously described, and all virus stock titers were determined by standard plaque assay in MDCK cells. HPAI viruses were handled in biosafety level 3 containment, including enhancements required by the U.S. Department of Agriculture and the National Select Agent Program (15–17).
Ferret inoculations and morbidity and transmission experiments.
Ferrets that were 6 to 9 months old (Triple F Farms) and serologically negative against currently circulating influenza viruses and the viruses included here were used in this study and were housed in cages within a Duo-Flo Bioclean mobile clean room (Lab Products). For each virus, at least four ferrets (n = 4 [SI06, MX09, and BD11], 5 [PN99], and 6 [TH04]) were sedated with a ketamine hydrochloride cocktail and inoculated, two ferrets IN with 106 or 107 PFU of virus in a 1-ml volume and two to four ferrets by AR with a presented dose of 102.7 to 105.6 PFU of virus using the AeroMP aerosol exposure system (Biaera) as previously described (12). Both methods of inoculation have been shown to deliver virus to the upper and lower respiratory tracts. IN delivered inoculum doses should be considered estimations of the amount of virus reaching the respiratory tract because some of the inoculum is swallowed during inoculation (12). The presented dose constitutes the amount of virus inhaled by the animal but not necessarily the amount that is deposited within the respiratory tract and is based on the time of exposure, minute volume (MV) of respiration, and the aerosolized virus concentrations achieved during inoculation. Therefore, the precise presented dose is determined subsequent to the inoculation procedure and is unique to each animal. Immediately prior to inoculation, the MV of respiration was measured for all animals while sedated using whole-body plethysmography (Buxco Research Systems). Ferrets were monitored daily for 6 days for morbidity as measured by weight loss and at 2, 4, and 6 days postinoculation (dpi) for changes in MV of respiration. Nasal washes were collected (18) for virus titration at 1, 3, and 5 dpi after aerosol sampling was completed for that day.
Transmissibility of BD11 virus was assessed as previously described (14) using both the direct-contact transmission (DCT) experiment and the respiratory droplet transmission (RDT) experiment. For each experiment, three ferrets were presented with 105.0 to 105.2 PFU of virus by AR inhalation. One day after inoculation, a naive ferret was placed either in the same cage as each inoculated ferret (for the DCT experiment) or in an adjacent cage with perforated side walls (for the RDT experiment, which allows transmission to occur through the air while preventing direct or indirect contact between the animal pairs). Nasal washes were collected every other day for at least 7 dpi or 7 days postcontact (dpc) for virus titration. Convalescent-phase serum samples were tested for the presence of BD11 virus-specific antibodies by hemagglutination inhibition assay as described previously (14). Transmission was noted by virus detection in nasal washes or seroconversion.
Aerosol analyses.
Exhaled aerosols from sedated ferrets were analyzed for size distribution using an aerodynamic particle sizer (APS) (TSI Inc.) for 30 min of closed-mouth, normal breathing followed by 5 min of sneezing stimulation in uninfected animals and in infected animals at 2, 4, and 6 dpi. Sneezing was induced in ferrets by vellication of the nares using the tip of a catheter, similar to the nasal wash collection procedure but without the use of nasal wash solution (18). During the 5-min collection period, the number of times that ferrets sneezed varied greatly but was approximately 30 to 100 times; TH04 virus-infected ferrets sneezed the least, <50 times, due to severe illness. Size distribution data are reported as total particle counts or volume collected for aerodynamic diameters in the range of 0.5 to 20 μm measured during the aerosol collection period. Count median aerodynamic diameters (CMAD) and total volumes were calculated using the DistFit software package (Chimera Technologies, Forest Lake, MN).
Exhaled aerosols were also evaluated for the presence of infectious virus using a viable two-stage cascade impactor (Tisch Environmental) as described previously (12) at 1, 3, and 5 dpi. Multiple time points were selected so that the peak time of shedding would be captured for all animals. Aerosols were collected for 30 min of normal, closed-mouth breathing and 5 min of sneezing stimulation, followed by collection of nasal wash samples. The cascade impactor was operated so that aerosols were separated onto two stages containing a thin sheet of gelatin; the top stage collected particles >4.7 μm and the bottom stage collected particles 0.65 to 4.7 μm in size. Immediately following sample collection, the gelatin was melted at 37°C and subjected to plaque assay without dilution and to RNA extraction for real-time reverse transcription-PCR (RT-PCR) as described previously (12). Viral RNA copy numbers were extrapolated using a standard curve based on samples of known virus titers (PFU/ml).
To determine the effect of the aerosol collection procedure on the viability of virus, rates of recovery of infectious virus were assessed by spiking the collection medium on impactor plates with known concentrations of virus (101 to 105 PFU) and then passing sterile air through the impactor for 30 or 5 min to represent the normal breathing or sneezing collection times, respectively. The gelatin medium on each plate was immediately melted at 37°C and subjected to plaque assay without dilution. All aerosol samples were collected under ambient laboratory conditions that were monitored daily (21 ± 1°C and 30% ± 10% relative humidity).
Statistics.
Areas under the curve (AUCs) were determined whenever serial measurements were collected; exceptions include data from uninfected animals. Significance of differences in morbidity, exhaled aerosol counts, volumes, and infectious virus between influenza virus groups (n = 4 to 6 each group) were determined using the Kruskal-Wallis test. The same parameters were evaluated for significant differences between human and avian influenza virus groups (n = 13 or 10, respectively) using the Mann-Whitney test. A P value of <0.05 was considered significant.
RESULTS
Comparison of disease in ferrets caused by influenza viruses after i.n. or AR inoculation.
Five influenza A viruses were selected for this study based on their diverse virulence and transmissibility phenotypes following i.n. inoculation in ferrets as reported elsewhere or here (Table 1). Two seasonal influenza viruses (H3N2 and H1N1) that transmit readily through the air and cause mild, transient disease in ferrets, with frequent sneezing observed (14, 19), were included. A 2009 pandemic H1N1 virus that was previously shown to cause more substantial disease and slightly reduced transmission in our RDT experiment (10) was included, plus two HPAI viruses exhibiting distinct virulence phenotypes, with less frequent sneezing observed and both lacking the ability to transmit among ferrets in our RDT experiment (20). BD11 virus transmissibility was evaluated in both DCT and RDT experiments. When ferrets were housed in the same cage, 2 of 3 contact ferrets seroconverted but none shed detectable virus in nasal washes, and during the RDT experiment, no transmission was observed (Table 1).
Table 1.
Virulence and transmissibility phenotypes of influenza viruses
| Virus | Subtype | Wt lossa (%) | Lethality (%) | Sneezing | Transmissionb |
Reference | |
|---|---|---|---|---|---|---|---|
| DC | RD | ||||||
| A/Panama/2007/99 | H3N2 | 7.9 | 0 | 3/3 | NTc | 3/3 | 14 |
| A/Solomon Islands/03/06 | H1N1 | 7.8 | 0 | 3/3 | NT | 3/3 | 19 |
| A/Mexico/4482/09 | H1N1 | 17.5 | 50 | 3/6 | 3/3 | 2/3 | 10 |
| A/Thailand/16/04 | H5N1 | 14.4 | 100 | 1/6 | 0/3 | 0/3 | 20, 21 |
| A/Bangladesh/5487/11 | H5N1 | 14.2 | 17 | 0/6 | 2/3 | 0/3 | This study |
Mean maximum weight loss for inoculated ferrets as described in the indicated reference.
DC, direct-contact transmission experiment; RD, respiratory droplet transmission experiment.
NT, not tested.
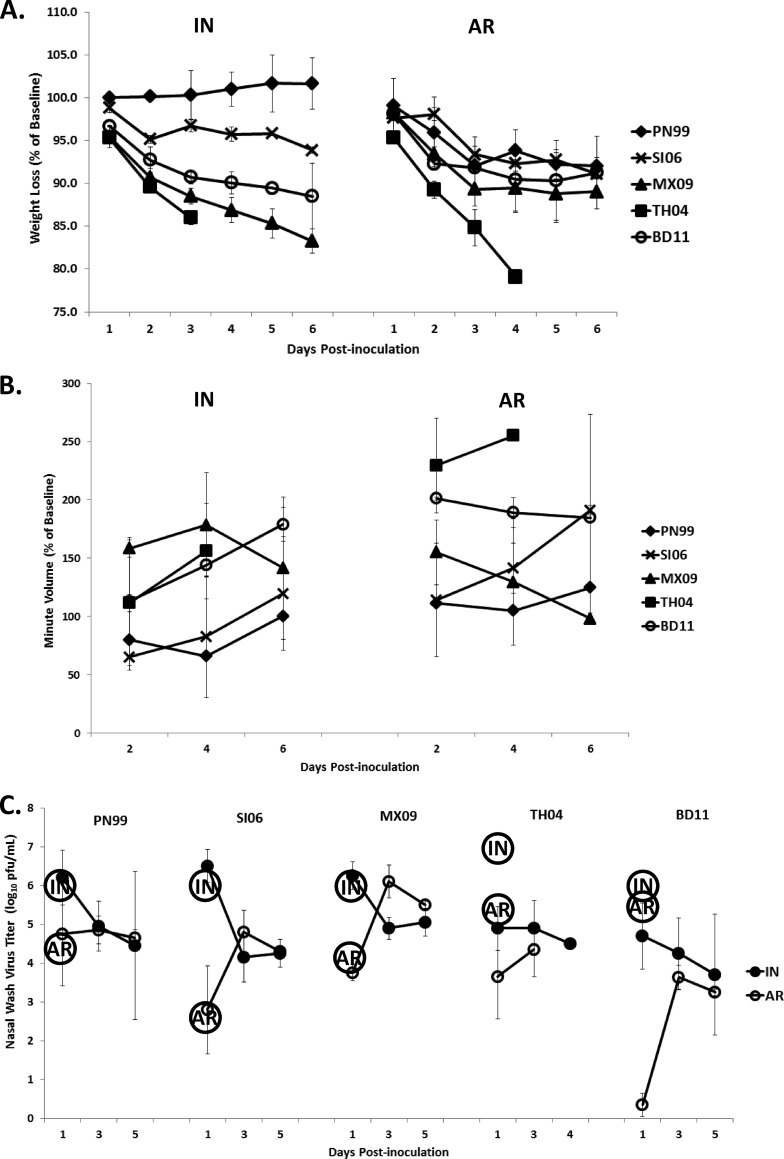
Once a panel of viruses was selected, four or more ferrets were each inoculated with influenza virus, two of them IN and two to four via AR, and were observed for 6 days for signs of disease and virus shedding. i.n. inoculated ferrets received a dose of 106 to 107 PFU, while AR-inoculated ferrets received a presented dose of 102.7 to 105.6 PFU (Fig. 1C). Morbidity was most severe in ferrets infected by the HPAI TH04 virus, with mean maximum weight loss of 21% and 100% lethality by 4 dpi (Fig. 1A). The least severe disease was observed in ferrets infected by seasonal influenza viruses (PN99 or SI06), which resulted in 0 to 9% mean maximum weight loss regardless of the method of inoculation. No significant differences in weight loss were observed between the two methods of inoculation for any of the viruses tested. When the MV of respiration was measured, values derived from AR-inoculated ferrets were generally higher (with the exception of MX09 virus) than those from i.n. inoculated ferrets (Fig. 1B). TH04 virus-infected ferrets' mean MV values peaked at 156 and 255% of baseline (IN and AR, respectively) before all ferrets succumbed to infection. No significant differences were observed among ferrets IN inoculated, but when human and avian influenza virus groups were compared among those inoculated by AR, ferrets infected by H5N1 avian influenza viruses exhibited significantly higher MV values (P = 0.0040). These findings demonstrate that assessment of respiration changes in infected animals may be a useful clinical parameter to include when comparing the disease characteristics caused by influenza viruses.
Fig 1.
Comparison of morbidity and influenza virus titers in ferret nasal washes. Ferrets were inoculated intranasally (IN) or by aerosol (AR) inhalation with 102.7 to 107 PFU of virus and were monitored daily for 6 days (n = 4 [SI06, MX09, and BD11], 5 [PN99], and 6 [TH04]). (A) Mean weight loss ± standard deviation (SD) is shown as the percentage of baseline for each virus group. (B) Mean minute volume of respiration ± SD was measured on alternating days in sedated animals by whole-body plethysmography and is shown as the percentage of baseline for each virus group. (C) Mean virus titers ± SD in nasal wash samples collected on alternating days are shown. No TH04-infected ferrets survived past day 4. Circles containing “IN” or “AR” represent the amount of inoculum administered to ferrets by the respective method of inoculation.
Nasal wash samples were collected from infected ferrets at 1, 3, and 5 dpi, and virus titers were measured by standard plaque assay (Fig. 1C). For the human influenza viruses, the virus titers measured at 1 dpi were very similar to inoculum doses for both IN and AR-inoculated groups. For avian influenza viruses, the virus titers measured at 1 dpi were reduced by 1 to 2 logs for TH04 and 1 to 5 logs for BD11 virus compared to inoculum doses. Therefore, regardless of the method of inoculation, inoculum titers were maintained within the first 24 h following infection only in animals inoculated with human influenza viruses, but by 3 dpi virus titers were similar for the different methods of inoculation for all virus groups, despite the diverse transmission efficiencies. Overall, virus shedding in nasal washes of animals IN inoculated peaked at 1 dpi, while AR-inoculated virus titers peaked on 3 dpi, establishing differences in virus shedding kinetics measured in nasal washes between these two methods of inoculation.
Size distribution of aerosols exhaled by ferrets.
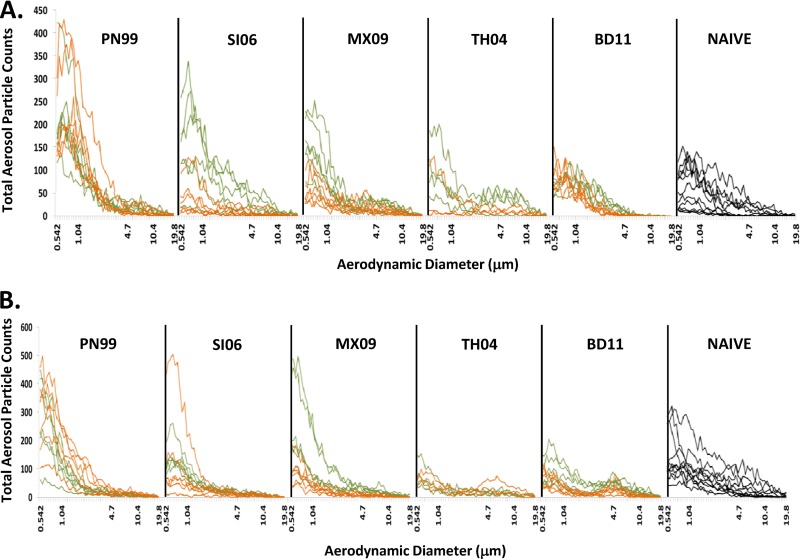
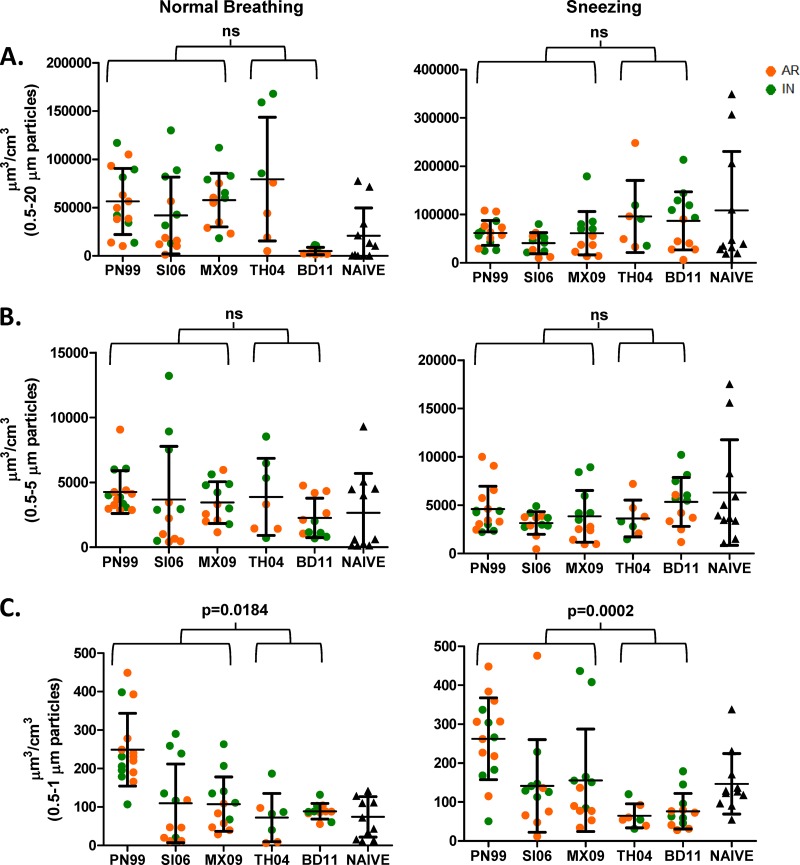
Little is known about the aerosols shed from infected hosts that may contribute to transmission events and how this may differ among infections caused by viruses exhibiting diverse transmissibility phenotypes. Therefore, we analyzed the size distribution of exhaled aerosols from individual uninfected and infected ferrets at 2, 4, and 6 dpi during 30 min of normal breathing followed by 5 min of sneezing stimulation. An APS spectrometer was used for this analysis, and the aerodynamic diameters of aerosol particles ranging in size from 0.5 to 20 μm were measured. Despite substantial variability among samples, ferrets infected by the human influenza viruses combined exhaled a greater number of aerosol particles during normal breathing (16 to 64% more) than uninfected animals (P = 0.0279) or those infected by avian influenza viruses (P = 0.0341), and no consistent difference was observed between the two methods of inoculation or among the time points of collection (Fig. 2A; Table 2). The majority of the aerosols were in the respirable size range (>93% for naive animals, >75% for avian virus-infected animals, and > 85% for human influenza virus-infected animals). Sneezing samples showed greater variability, but again, those collected from human influenza virus-infected ferrets contained 53 to 85% more particles of 0.5 to 20 μm in size than those collected from ferrets infected by TH04 or BD11 viruses (P = 0.0075), while comparisons to naive animals was not significant (P = 0.5055) (Fig. 2B; Table 2). The majority of particles generated during sneezing were <5 μm (>80% for naive animals, >66% for avian virus-infected animals, and >77% for human influenza virus-infected animals), which are capable of prolonged suspension in the air and are more readily inhaled. To have an idea of the total amount of respiratory secretions being exhaled, the total volume of aerosol particles (not the volume of air) was calculated within various size ranges for each animal (Fig. 3). No significant difference was observed when the human and avian influenza virus groups were compared in the 0.5- to 20-μm or 0.5-to 5-μm size range, but in the <1-μm, submicrometer size range, ferrets infected by human influenza viruses exhaled significantly greater volumes of aerosols during normal breathing (P = 0.0184) and sneezing (P = 0.0002) than those infected by avian influenza viruses (Fig. 3C). When the virus groups were compared individually, PN99 virus-infected ferrets shed the greatest volumes of aerosol particles in the submicrometer size range during both normal breathing and sneezing, 46 to 75% more than all other virus groups. Although certain virus groups showed significant differences between i.n. and AR inoculation (MX09 and BD11 viruses), no consistent differences in exhaled volumes were observed between the two methods of inoculation (Fig. 3). In addition to size distribution analysis, exhaled aerosols from infected ferrets were also evaluated for the presence of infectious virus.
Fig 2.
Analysis of aerosols exhaled by individual influenza virus-infected or uninfected ferrets. Particle size distributions of aerosols exhaled by ferrets inoculated with 102.7 to 107 PFU of virus IN (green lines) or by AR inhalation (orange lines) or by naive animals (black lines) during normal breathing (A) or sneezing stimulation (B) are shown (n = 4 [SI06, MX09, and BD11], 5 [PN99], 6 [TH04], and 11 [naive]). Collection procedures were performed at 2, 4, and 6 days after inoculation, but these time points are not distinguished. Total particle counts in the aerodynamic diameter range of 0.5 to 20 μm are shown, but due to space constraints, selected sizes are noted on the x axis.
Table 2.
Size distribution of exhaled aerosol particles from infected or naive ferrets
| Type of sample | Virusa | CMAD rangeb (μm) |
Total countsc |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 0.5–20 μm |
0.5–5 μm |
0.5–1 μm |
|||||||
| Median | GSD | Avg | SD | Avg | SD | Avg | SD | ||
| Normal breathing (30 min) | PN99 | 0.70–0.95 | 1.67–2.35 | 3,434 | 1,384 | 3,250 | 1,309 | 1,925 | 818 |
| SI06 | 0.68–1.74 | 1.58–2.59 | 1,750 | 1,589 | 1,602 | 1,466 | 846 | 790 | |
| MX09 | 0.74–1.85 | 1.70–2.84 | 1,689 | 855 | 1,486 | 824 | 865 | 557 | |
| TH04 | 0.71–3.20 | 1.69–1.85 | 1,425 | 1,051 | 1,144 | 885 | 599 | 509 | |
| BD11 | 0.68–1.08 | 1.56–1.85 | 1,379 | 360 | 1,355 | 348 | 671 | 158 | |
| Naive | 0.71–1.16 | 1.5–2.38 | 1,234 | 1,010 | 1,154 | 928 | 556 | 392 | |
| Sneezing (5 min) | PN99 | 0.64–0.86 | 1.66–2.63 | 3,648 | 1,668 | 3,471 | 1,646 | 2,164 | 947 |
| SI06 | 0.66–1.28 | 1.69–2.59 | 1,996 | 1,292 | 1,860 | 1,292 | 1,119 | 968 | |
| MX09 | 0.68–0.91 | 1.98–2.53 | 1,304 | 1,880 | 2,137 | 1,770 | 1,304 | 1,089 | |
| TH04 | 0.76–2.16 | 2.4–2.97 | 537 | 542 | 1,030 | 415 | 537 | 256 | |
| BD11 | 0.69–2.62 | 1.87–2.75 | 609 | 891 | 1,276 | 740 | 609 | 350 | |
| Naive | 0.80–2.24 | 1.82–2.66 | 3,073 | 1,840 | 2,738 | 1,619 | 1,345 | 883 | |
Shading indicates avian influenza viruses.
The count median aerodynamic diameter (CMAD) and geometric standard deviation (GSD) for each sample were determined, and the range is shown for each virus group.
Total counts for each sample were determined, and the average and standard deviation (SD) are shown for each virus group.
Fig 3.
Analysis of aerosol volumes exhaled by influenza virus-infected and uninfected ferrets. The total aerosol volume exhaled (not the volume of air) from naive ferrets (triangles) or from ferrets inoculated with 102.7 to 107 PFU of virus IN (green) or by AR inhalation (orange) during normal breathing or sneezing (n = 4 [SI06, MX09, and BD11], 5 [PN99], 6 [TH04], and 11 [naive]) is shown. Total volumes were determined for aerosols 0.5 to 20 μm (A), 0.5 to 5 μm (B), and 0.5 to 1 μm (C) in size exhaled from individual animals. Collection procedures were performed at 2, 4, and 6 days after inoculation, but these time points are not distinguished. Mean values ± SDs are shown. The statistical significance of comparisons between human and avian influenza virus groups is shown; ns, not significant.
Virus detection in aerosols exhaled by ferrets.
Detection of influenza virus in aerosols has largely been reported as the amplification of viral genetic material via PCR. We established a method for the collection of exhaled aerosols from infected ferrets designed to preserve the viability of virus in the aerosols (12). For this study, aerosols exhaled by ferrets were segregated into two size categories (>4.7 μm and 0.65 to 4.7 μm) and captured on collection medium at 1, 3 and 5 dpi for 30 min of normal breathing and 5 min of sneezing stimulation. To have a better idea of the impact of the aerosol collection procedure on the viability of virus, diluted virus stocks were used to the spike collection medium applied to each impactor plate, and after sterile air was pulled through the impactor for 30 or 5 min, the medium was harvested and subjected to plaque assay. This procedure was repeated with a range of virus titers (101 to 105 PFU) for each virus to obtain a general idea of the virus recovery rates. Infectious virus was recovered at rates that on average ranged from 7 to 35% of the original amount (Fig. 4). These recovery rates were considered while interpreting data acquired during aerosol collection from infected animals.
Fig 4.
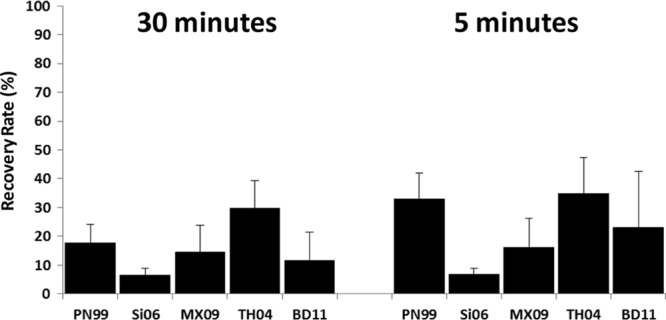
Rates of recovery of influenza virus. The rates of recovery of infectious influenza virus using the viable cascade impactor were assessed by spiking the collection medium on impactor plates with virus (101 to 105 PFU) and then passing sterile air through the impactor for 30 or 5 min. Virus titers in collection medium were determined by plaque assay without dilution and compared to the amount used to spike the plate. The mean percentage (+SD) of recovery for each virus is shown.
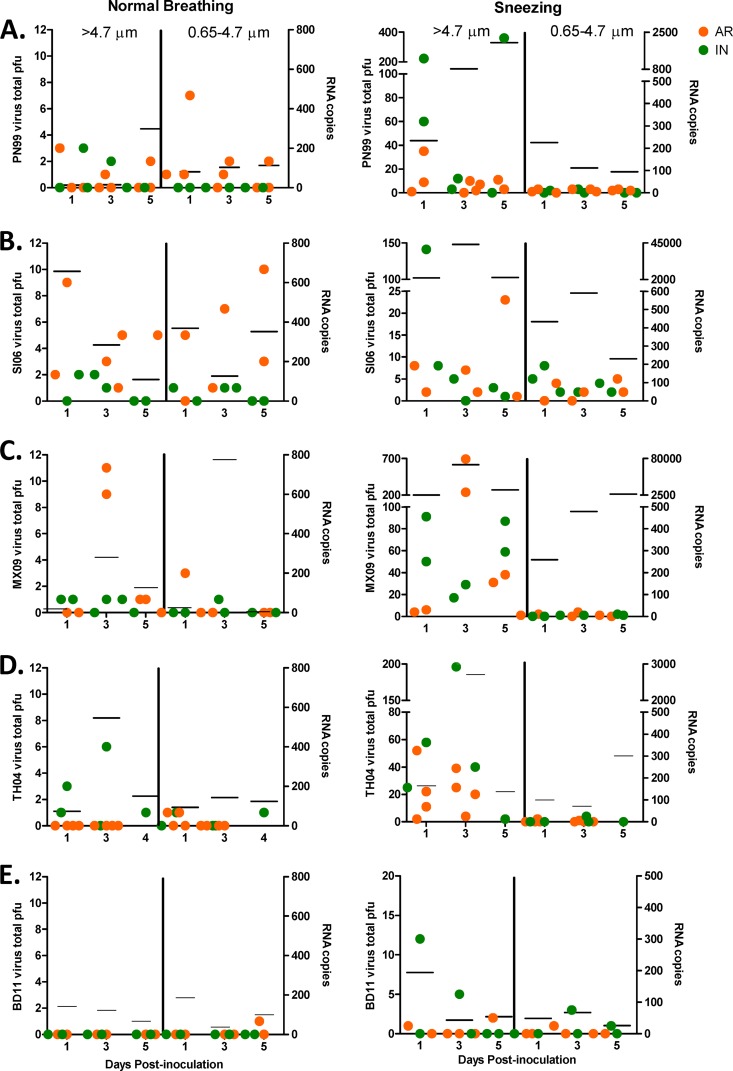
Infectious virus was detected in exhaled aerosols from all ferrets to various degrees and at different dpi during normal breathing or sneezing regardless of virus group. During 30 min of normal breathing, virus levels were highest in ferrets infected by human influenza viruses, with peak levels ranging from 3 to 11 PFU in particles within either size group, but ferrets infected with PN99 and SI06 viruses actually exhaled more virus in the respirable size range of aerosols than in the >4.7-μm range (Fig. 5A and B). In contrast, ferrets infected by avian influenza viruses exhaled 0 to 6 and 1 PFU in the >4.7-μm and 0.65- to 4.7-μm size groups, respectively (Fig. 5D and E). Comparison of the shedding patterns of all the animals revealed that ferrets in the human influenza virus group exhaled significantly higher levels of infectious virus in aerosols than those in the avian influenza virus group (overall, P = 0.0008; 0.65 to 4.7 μm, P = 0.0318; >4.7 μm, P = 0.0150). When the recovery rates from spiked-virus experiments were incorporated into these findings, differences between the human and avian influenza virus groups were still significant (overall, P = 0.0011; 0.65 to 4.7 μm, P = 0.0234; >4.7 μm, P = 0.0064). Overall, ferrets infected by a human influenza virus exhaled infectious virus at rates of 1 to 4 PFU/min and approximately 8 to 28 PFU/liter of air exhaled. Those animals infected by avian influenza viruses exhaled infectious virus at rates of <1 PFU/min and 1 to 3 PFU/liter of air exhaled. Infectious human influenza viruses were shed at levels 3- to 20-fold higher than those detected for avian influenza viruses. Viral RNA detected in air exhaled during normal breathing was also greater in ferrets infected by human versus avian influenza viruses (Fig. 5). Peak levels in either size group after 30 min ranged from 298 to 791 copies for human influenza viruses, up to 4 times greater than for avian influenza viruses, which ranged from 199 to 546 copies.
Fig 5.
Infectious virus present in aerosols exhaled from influenza virus-infected ferrets. Aerosols were collected from ferrets inoculated with 102.7 to 107 PFU of PN99 (A), SI06 (B), MX09 (C), TH04 (D), or BD11 (E) virus IN (green) or by AR inhalation (orange) during normal breathing or sneezing using a viable cascade impactor (n = 4 [SI06, MX09, and BD11], 5 [PN99], and 6 [TH04]). Virus titers collected on impactor plates on alternating days after inoculation were determined by plaque assay without dilution, and total PFU is shown for each ferret on the left y axis. Viral RNA levels in the same samples from combined IN and AR experiments were estimated by real-time RT-PCR and are shown as lines on the right y axis.
Because ferrets infected by influenza viruses have a tendency to sneeze at different rates and at different time points after infection (21), we wanted to analyze the amount of virus being expelled into the air during sneezing. Virus levels in the respirable size range (<5 μm) detected by our assays during 5 min of sneezing stimulation were significantly higher (P = 0.0058) in ferrets infected by human influenza viruses combined (up to 8 PFU) than in those infected by avian influenza viruses (up to 4 PFU) (Fig. 5). When the recovery rates from spiked samples were considered, differences between the two virus groups were still significant (P = 0.0044). Peak viral RNA in respirable particles was less defined and ranged from 225 to 4539 copies for human influenza viruses and 67 to 313 copies for avian influenza viruses. Particles >5 μm were also analyzed; these include the very large particles of mucus that settle on surfaces immediately after being expelled (2) and are expected to exhibit the greatest variability. Significance was not found when the virus levels directly measured were compared for human and avian influenza virus groups (P = 0.0673), but after the data were normalized to the virus recovery rates, the differences were found to be significant (P = 0.0143). Peak titers measured in this size range were 141 to 692 PFU for the human influenza virus group and 12 to 196 PFU for the avian influenza virus group, while viral RNA was measured at levels as high as 104.8 and 103.4 copies, respectively. No consistent difference was measured among any of the viruses tested in the levels of infectious virus in exhaled aerosols between those ferrets IN inoculated and those inoculated by AR. However, distinct differences have been shown here between the amounts of highly transmissible, human influenza virus being exhaled into the air by infected animals and those of less transmissible, avian influenza viruses. The findings we report here provide the opportunity for a greater understanding of the influenza virus ferret transmission model, which will enhance our ability to assess the potential for emerging influenza viruses to transmit readily through the air and pose a risk to public health.
DISCUSSION
Influenza viruses responsible for epidemics and pandemics have the ability to spread rapidly among susceptible individuals by contact (direct or indirect) or through the air via close-range or long-range transmission (1). The relative predominances of these modes of transmission have been debated for some time. A key determinant of whether a particular virus can successfully transmit through the air from one host to cause infection in another is whether the virus maintains viability as it passes through the air. Here, we selected a panel of influenza viruses that exhibit a range of transmissibility phenotypes and, using the ferret model, evaluated morbidity and the aerosol shedding profiles during normal breathing and sneezing of animals infected IN or by AR. We found that overall, ferrets infected by transmissible human influenza viruses exhale more aerosolized respiratory secretions and higher levels of infectious virus in aerosols than animals with avian influenza virus infections. Although there are additional determinants of influenza virus transmission, these results show that highly transmissible influenza viruses maintain viability in exhaled aerosols of the size capable of prolonged suspension in the air.
Comparison of morbidities observed in animals inoculated IN or by AR inhalation revealed no significant differences in weight loss in ferrets regardless of the method of inoculation; a similar finding was previously reported for PN99 virus (12). MV of respiration values in AR-inoculated animals were higher (with the exception of MX09 virus) than those in i.n. inoculated animals, with a high degree of variability among animals. Increases in MV of respiration due to lower airway obstruction after i.n. inoculation of influenza virus have also been reported in cotton rats, but only in young animals, which exhibit greater lung elasticity than their older counterparts (22). Others have shown increased morbidity in mice after AR inoculation of an H3N2 influenza virus than after IN delivery of virus, but the MV of respiration was not measured (23). We also observed differences between the virus shedding kinetics in nasal washes of animals based on the method of inoculation; peak virus shedding was delayed in AR-inoculated compared to IN inoculated ferrets. Similar kinetics were previously shown in AR-inoculated ferrets and in those naturally infected by exposure to other infected ferrets (12). We also observed a ≥1-log drop in virus nasal wash titers at 1 day after inoculation but only with the avian influenza viruses. Nasal wash sampling in these animals may represent secretions primarily from the upper respiratory tract, which has been shown to better support the replication of human influenza viruses than that of avian influenza viruses, and this may account for the drop in virus titers observed on the first day after infection (24, 25). Collectively, our findings highlight differences in morbidity and virus shedding kinetics in nasal washes between IN and AR-inoculated ferrets, but characterization of the aerosols exhaled from infected animals is essential to understanding the factors affecting influenza virus transmission.
A number of studies have characterized the aerosol shedding patterns of people during aerosol-generating activities such as breathing, coughing, sneezing, and talking (26), but until recently, little was known about the effect of influenza virus infection on aerosol production in people. Lindsley et al. (7) reported increases in the number and volume of aerosol particles exhaled by infected patients during coughing, with a great degree of variability among samples and with the majority of particles in the respirable size range. Similarly, we found that ferrets also shed more respirable aerosols after infection with human influenza viruses, and with substantial variability among samples. These findings are corroborated by previous studies showing a greater incidence of rhinorrhea among ferrets during the first few days after infection by highly transmissible influenza viruses than after infection by poorly transmissible strains and correlations with local proinflammatory cytokine responses (21). The majority of the aerosols measured in the current study during normal breathing were in the respirable size range, but when the volumes were compared, a greater difference between the two groups of infected animals was revealed at the submicrometer particle size range (<1 μm), albeit with substantial variability. Others have measured the size distribution of aerosols in air exhausted from cages housing ferrets infected by influenza virus and have reported the greatest concentrations of particles in the submicrometer size range (13). Submicrometer aerosols may remain suspended in still air for 12 hours or more, increasing the opportunity for aerosols of this size to be inhaled (27).
The potential of respirable aerosols to carry infectious influenza virus from one host to another has remained uncertain, primarily because published reports are, for the most part, limited to the detection of influenza virus RNA and not infectious virus. Multiple laboratories have reported the detection of the majority of influenza virus RNA in exhaled aerosols from humans in the respirable size range (8, 28–31) and that infected patients exhaled up to 20 copies/min (32). Infectious virus has been detected in aerosol particles exhaled by humans (8, 28), but, with limited preservation of virus viability, quantitative analyses have not been reported. Infectious virus has been detected in air samples collected from guinea pigs infected by human influenza virus, and although droplets in air samples were not segregated by size, an average of 40 PFU/liter of air sampled was measured (33). Using ferrets infected by human influenza viruses in the current study, we measured not only viral RNA in exhaled aerosols during normal breathing (up to 26 copies/min) but also infectious virus (up to 4 PFU/min). When similar experiments were performed with poorly transmissible, avian influenza viruses, <1 PFU/min and up to 18 copies/min were detected, with the most striking differences observed in the respirable size range of aerosols. The 50% ferret infectious dose (FID50) for aerosol delivery of human influenza virus (PN99) is 1.9 PFU, while the FID50 for avian influenza virus (TH04) is 4 PFU (12). For comparison, the 50% human infectious dose of influenza virus delivered in 1- to 3-μm-size aerosols is reported as 0.6 to 3 50% tissue culture infectious doses (34). Additional factors affecting transmission are certainly involved here, including differences between human and avian influenza virus receptor binding preferences and tissue tropisms (24), but the amount of infectious virus in aerosols being exhaled by infected hosts is also an important consideration.
Because the ferret transmission model is such a valuable tool in the risk assessment of emerging influenza viruses, it is important that we have a good understanding of how transmission is occurring for each virus evaluated using this model. During a DCT experiment, transmission may occur by direct or indirect contact, large droplets, or aerosols, while during an RDT experiment, transmission may occur by large droplets or aerosols. The detection of infectious influenza virus in respirable aerosols highlights the potential for a role of respirable aerosols in transmission events occurring during RDT experiments. Others have shown that influenza virus present in particles <15 μm is responsible for transmission of virus between ferrets, although only viral RNA was detected in these studies (13, 35). It is also plausible that aerosols play a role in transmission experiments in which animals are housed in direct contact; the contribution of close-range aerosol transmission cannot be ruled out in these scenarios (36). The improved techniques and information derived from our current study will enhance the utility of the ferret influenza transmission model by providing a more comprehensive understanding of the virus and aerosol shedding profiles of infected animals.
There are a number of limitations to this study that warrant mention. Many of the data reported are dependent on instrumentation that has certain functional restraints. Size distribution data included only particles of 0.5 to 20 μm in size, and infectious virus in aerosols of <0.65 μm was not collected. The rates of recovery of infectious influenza virus were 7 to 35%, depending on the virus and collection time. Similar recovery rates (15 to 34%) were reported using a different collection device (37), but nevertheless, improvements in recovery rates would provide a more accurate account of the amounts of infectious virus present in exhaled aerosols and would allow us to better represent the kinetics of viable virus shedding in aerosols, which may not be possible with the sensitivity of the current assay. All experiments reported here were conducted under ambient laboratory conditions. The aerosol and virus shedding profiles observed under diverse environmental conditions (temperature and humidity) are not known, but such knowledge may improve our understanding of the seasonality of influenza viruses. Lastly, data extrapolated from animal model studies will never exactly represent the human situation, but the amount of information that can be obtained from animal studies, most of which could never be performed in human volunteers, makes the ferret model an invaluable tool in influenza research and in our mission to improve global public health. The findings reported here using the ferret model do not unequivocally prove that transmission occurs via respirable aerosols; however, they do confirm the need for a continued focus on the potential for short-range and long-range aerosol transmission of influenza viruses. Data obtained from further research using the ferret model as well as epidemiological reports and, when possible, human challenge studies will bring us closer to fully understanding the mechanisms of influenza virus transmission.
ACKNOWLEDGMENTS
K. M. Gustin is supported by the Oak Ridge Institute for Science and Education.
We are grateful to the Ministry of Public Health in Thailand and the People's Republic of Bangladesh for providing highly pathogenic avian influenza viruses. We thank Vic Veguilla for statistical expertise, Shannon Emery for assistance with real-time RT-PCR analyses, and the CDC Animal Resources Branch for exceptional animal care.
We declare that we have no competing financial interests. The findings and conclusions in this report are those of the authors and do not necessarily reflect the views of the funding agency.
Footnotes
Published ahead of print 8 May 2013
REFERENCES
- 1. Weber TP, Stilianakis NI. 2008. Inactivation of influenza A viruses in the environment and modes of transmission: a critical review. J. Infect. 57:361–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hinds W. 1999. Aerosol technology: properties, behavior, and measurement of airborne particles, 2nd ed, p 233–259 John Wiley & Sons, New York, NY [Google Scholar]
- 3. Moser MR, Bender TR, Margolis HS, Noble GR, Kendal AP, Ritter DG. 1979. An outbreak of influenza aboard a commercial airliner. Am. J. Epidemiol. 110:1–6 [DOI] [PubMed] [Google Scholar]
- 4. Tellier R. 2009. Aerosol transmission of influenza A virus: a review of new studies. J. R Soc. Interface 6(Suppl 6):S783–S790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brankston G, Gitterman L, Hirji Z, Lemieux C, Gardam M. 2007. Transmission of influenza A in human beings. Lancet Infect. Dis. 7:257–265 [DOI] [PubMed] [Google Scholar]
- 6. Killingley B, Enstone JE, Greatorex J, Gilbert AS, Lambkin-Williams R, Cauchemez S, Katz JM, Booy R, Hayward A, Oxford J, Bridges CB, Ferguson NM, Nguyen Van-Tam JS. 2012. Use of a human influenza challenge model to assess person-to-person transmission: proof-of-concept study. J. Infect. Dis. 205:35–43 [DOI] [PubMed] [Google Scholar]
- 7. Lindsley WG, Pearce TA, Hudnall JB, Davis KA, Davis SM, Fisher MA, Khakoo R, Palmer JE, Clark KE, Celik I, Coffey CC, Blachere FM, Beezhold DH. 2012. Quantity and size distribution of cough-generated aerosol particles produced by influenza patients during and after illness. J. Occup. Environ. Hyg. 9:443–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ. 2013. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 9(3):e1003205. 10.1371/journal.ppat.1003205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Belser JA, Katz JM, Tumpey TM. 2011. The ferret as a model organism to study influenza A virus infection. Dis. Model Mech. 4:575–579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maines TR, Jayaraman A, Belser JA, Wadford DA, Pappas C, Zeng H, Gustin KM, Pearce MB, Viswanathan K, Shriver ZH, Raman R, Cox NJ, Sasisekharan R, Katz JM, Tumpey TM. 2009. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science 325:484–487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Munster VJ, de Wit E, van den Brand JM, Herfst S, Schrauwen EJ, Bestebroer TM, van de Vijver D, Boucher CA, Koopmans M, Rimmelzwaan GF, Kuiken T, Osterhaus AD, Fouchier RA. 2009. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science 325:481–483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gustin KM, Belser JA, Wadford DA, Pearce MB, Katz JM, Tumpey TM, Maines TR. 2011. Influenza virus aerosol exposure and analytical system for ferrets. Proc. Natl. Acad. Sci. U. S. A. 108:8432–8437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Koster F, Gouveia K, Zhou Y, Lowery K, Russell R, MacInnes H, Pollock Z, Layton RC, Cromwell J, Toleno D, Pyle J, Zubelewicz M, Harrod K, Sampath R, Hofstadler S, Gao P, Liu Y, Cheng YS. 2012. Exhaled aerosol transmission of pandemic and seasonal H1N1 influenza viruses in the ferret. PLoS One 7:e33118. 10.1371/journal.pone.0033118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Maines TR, Chen LM, Matsuoka Y, Chen H, Rowe T, Ortin J, Falcon A, Nguyen TH, Mai le Q, Sedyaningsih ER, Harun S, Tumpey TM, Donis RO, Cox NJ, Subbarao K, Katz JM. 2006. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc. Natl. Acad. Sci. U. S. A. 103:12121–12126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. HHS 2009. Biosafety in microbiological and biomedical laboratories, 5th ed, vol CDC 21–1112 HHS Publications, Atlanta, GA [Google Scholar]
- 16. USDA 2013, posting date U.S. Department of Agriculture, Animal and Plant Health Inspection Service. http://www.aphis.usda.gov/programs/ag_selectagent
- 17. National Select Agent Registry 2012, posting date. http://www.selectagents.gov
- 18. Zitzow LA, Rowe T, Morken T, Shieh WJ, Zaki S, Katz JM. 2002. Pathogenesis of avian influenza A (H5N1) viruses in ferrets. J. Virol. 76:4420–4429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Van Hoeven N, Pappas C, Belser JA, Maines TR, Zeng H, Garcia-Sastre A, Sasisekharan R, Katz JM, Tumpey TM. 2009. Human HA and polymerase subunit PB2 proteins confer transmission of an avian influenza virus through the air. Proc. Natl. Acad. Sci. U. S. A. 106:3366–3371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jackson S, Van Hoeven N, Chen LM, Maines TR, Cox NJ, Katz JM, Donis RO. 2009. Reassortment between avian H5N1 and human H3N2 influenza viruses in ferrets: a public health risk assessment. J. Virol. 83:8131–8140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Maines TR, Belser JA, Gustin KM, van Hoeven N, Zeng H, Svitek N, von Messling V, Katz JM, Tumpey TM. 2012. Local innate immune responses and influenza virus transmission and virulence in ferrets. J. Infect. Dis. 205:474–485 [DOI] [PubMed] [Google Scholar]
- 22. Trias EL, Hassantoufighi A, Prince GA, Eichelberger MC. 2009. Comparison of airway measurements during influenza-induced tachypnea in infant and adult cotton rats. BMC Pulm. Med. 9:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Smith JH, Nagy T, Barber J, Brooks P, Tompkins SM, Tripp RA. 2011. Aerosol inoculation with a sub-lethal influenza virus leads to exacerbated morbidity and pulmonary disease pathogenesis. Viral Immunol. 24:131–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Belser JA, Maines TR, Tumpey TM, Katz JM. 2010. Influenza A virus transmission: contributing factors and clinical implications. Expert Rev. Mol. Med. 12:e39. [DOI] [PubMed] [Google Scholar]
- 25. Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440:435–436 [DOI] [PubMed] [Google Scholar]
- 26. Gralton J, Tovey E, McLaws ML, Rawlinson WD. 2011. The role of particle size in aerosolised pathogen transmission: a review. J. Infect. 62:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hinds W. 1999. Aerosol technology: properties, behavior, and measurement of airborne particles, 2nd ed, p 42–74 John Wiley & Sons, New York, NY [Google Scholar]
- 28. Lindsley WG, Blachere FM, Thewlis RE, Vishnu A, Davis KA, Cao G, Palmer JE, Clark KE, Fisher MA, Khakoo R, Beezhold DH. 2010. Measurements of airborne influenza virus in aerosol particles from human coughs. PLoS One 5:e15100. 10.1371/journal.pone.0015100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Blachere FM, Lindsley WG, Pearce TA, Anderson SE, Fisher M, Khakoo R, Meade BJ, Lander O, Davis S, Thewlis RE, Celik I, Chen BT, Beezhold DH. 2009. Measurement of airborne influenza virus in a hospital emergency department. Clin. Infect. Dis. 48:438–440 [DOI] [PubMed] [Google Scholar]
- 30. Lindsley WG, Blachere FM, Davis KA, Pearce TA, Fisher MA, Khakoo R, Davis SM, Rogers ME, Thewlis RE, Posada JA, Redrow JB, Celik IB, Chen BT, Beezhold DH. 2010. Distribution of airborne influenza virus and respiratory syncytial virus in an urgent care medical clinic. Clin. Infect. Dis. 50:693–698 [DOI] [PubMed] [Google Scholar]
- 31. Bischoff WE, Swett K, Leng I, Peters TR. 2013. Exposure to influenza virus aerosols during routine patient care. J. Infect. Dis. 207:1037–1046 [DOI] [PubMed] [Google Scholar]
- 32. Fabian P, McDevitt JJ, DeHaan WH, Fung RO, Cowling BJ, Chan KH, Leung GM, Milton DK. 2008. Influenza virus in human exhaled breath: an observational study. PLoS One 3:e2691. 10.1371/journal.pone.0002691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mubareka S, Lowen AC, Steel J, Coates AL, Garcia-Sastre A, Palese P. 2009. Transmission of influenza virus via aerosols and fomites in the guinea pig model. J. Infect. Dis. 199:858–865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Alford RH, Kasel JA, Gerone PJ, Knight V. 1966. Human influenza resulting from aerosol inhalation. Proc. Soc. Exp. Biol. Med. 122:800–804 [DOI] [PubMed] [Google Scholar]
- 35. Lakdawala SS, Lamirande EW, Suguitan AL, Jr, Wang W, Santos CP, Vogel L, Matsuoka Y, Lindsley WG, Jin H, Subbarao K. 2011. Eurasian-origin gene segments contribute to the transmissibility, aerosol release, and morphology of the 2009 pandemic H1N1 influenza virus. PLoS Pathog 7:e1002443. 10.1371/journal.ppat.1002443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Edenborough KM, Gilbertson BP, Brown LE. 2012. A mouse model for the study of contact-dependent transmission of influenza a virus and the factors that govern transmissibility. J. Virol. 86:12544–12551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cao G, Noti JD, Blachere FM, Lindsley WG, Beezhold DH. 2011. Development of an improved methodology to detect infectious airborne influenza virus using the NIOSH bioaerosol sampler. J. Environ. Monit. 13:3321–3328 [DOI] [PMC free article] [PubMed] [Google Scholar]