Abstract
Background:
Fixed Dose Combinations (FDCs) improve patient compliance and decrease pill burden. However, irrational prescribing of FDCs is a major health concern. As resident doctors are primarily involved in patient management at tertiary care hospitals, knowledge about prescribing FDCs is of paramount importance.
Objective:
To evaluate knowledge, attitude and practice, regarding use of FDCs by resident doctors at a tertiary care teaching hospital.
Materials and Methods:
The study was carried out among resident doctors working at Civil Hospital, Ahmedabad, a tertiary care teaching hospital. One hundred resident doctors from the departments of medicine, obstetrics and gynaecology, surgery, paediatrics, skin and psychiatry, who gave their informed consent, were enrolled. A prevalidated questionnaire regarding knowledge, attitude and prescribing practice of fixed dose combinations was filled up. Data was analyzed with suitable statistical tests.
Results:
Out of the 100 residents recruited for the study, 34, 33 and 33 residents were selected from the 1st, 2nd and 3rd year respectively. The resident doctors were not aware about all of the advantages and disadvantages of FDCs. On an average, only 31% of the residents (lowest 16% among 1st year residents) had knowledge about the Essential Medicine List (EML). Knowledge about rationality of given FDCs was lacking in 81% of the residents. Only 47% could name a single banned FDC in India. Common sources of information about FDCs were medical representatives, colleagues/peers, the Monthly Index of Medical Specialities (MIMS) and Continuous Medical Education (CMEs). A majority of residents (96%) agreed that FDCs should be allowed to be marketed. The residents opined that most commonly prescribed FDCs were of antimicrobial drugs, amongst which amoxicillin + clavulanic acid was the most frequent.
Conclusion:
There is need to improve knowledge about rationality, EML, usage and banned FDCs in post graduate medical students to promote the rational use of drugs.
Keywords: Essential medicine list, fixed dose combinations, knowledge attitude and practice, resident doctors
INTRODUCTION
A Fixed dose combination (FDC) comprises of two or more active drugs in a single dosage form.[1] FDCs enhance the efficacy of individual drugs, decrease the chances of drug resistance (e.g. antimicrobial drugs), improve patient compliance and also decrease the pill burden on the patients. However, there are some disadvantages associated with the use of FDCs like, irrational prescription of FDCs, ineffective and unsafe treatment, exacerbation or prolongation of illness, and higher treatment cost.[2]
The Seventeenth WHO Model List of essential medicines (March 2011) contains only 25 approved FDCs, while in India, irrational drug combinations are easily available and many of them available as over the counter (OTC) drugs.[3] Most of the pharmaceutical companies manufacture a wide number of FDCs as novel products. FDCs are available for the treatment of various disorders e.g. cardiovascular diseases, diabetes, infectious diseases (bacterial infections), gastro intestinal infections, orthopedic conditions, cough and cold, HIV infection, tuberculosis, psychiatric disorders and respiratory diseases.[4]
A study of knowledge, attitude and practice is the most important tool to assess the benefits and lacunae about a subject in the community, so that effective steps can be taken in that direction to improve the outcome. A large number of FDCs are manufactured every year and hence the knowledge about prescribing fixed dose combinations is becoming increasingly important for better health outcomes. Tertiary care teaching hospitals have a dual role to play in terms of educating medical students and providing health care facilities to the patients. Resident doctors are primarily involved in patient management at tertiary care teaching hospitals, so their awareness about prescribing medicines is of prime importance for the treatment of patients. Thus, the present study was conducted to evaluate the knowledge, attitude and practices about prescribing fixed dose combinations among resident doctors at a tertiary care teaching hospital in Ahmedabad city.
Aim of the study
To evaluate knowledge, attitude and practice regarding FDCs among resident doctors at tertiary care teaching hospital.
MATERIALS AND METHODS
The present study was carried out with first, second and third year resident doctors working in medicine, surgery, paediatrics, obstetrics and gynaecology, skin and venereal diseases as well as the psychiatry departments of Civil hospital, Ahmedabad (CHA). A total of 100 resident doctors out of 216 were selected for the study. Prior to this survey, Institutional Ethics Committee (IEC) approval and written informed consent from resident doctors of various departments of the tertiary care teaching hospital, Ahmedabad was taken. A prevalidated questionnaire, with details such as the resident's information about their respective department, year of study and questions regarding knowledge, attitude and prescribing practice of fixed dose combinations was used as a tool, administrated to all the resident doctors and the collected data was analyzed.
RESULTS
The present study was carried out in resident doctors of various departments of tertiary care teaching hospital, Ahmedabad. A total of 100 resident doctors, which included 34, 1st year, 33, 2nd year and 33, 3rd year resident doctors were involved. An analysis of their knowledge revealed that 87% of the residents were aware about FDCs. Improved patient compliance (85%) and less cost (36%) were the major advantages, while difficulty in dosage adjustments was the common disadvantage of prescribing FDCs mentioned by the study population [Table 1]. The knowledge about WHO Essential Medicine List (EML) showed that 80% of the resident doctors knew about its availability. Year wise knowledge about FDCs included in WHO EML is mentioned in Figure 1. It was observed that 44.12% of the 1st year, 27% of 2nd year and 24% of 3rd year resident doctors did not know even a single FDC included in WHO EML [Figure 1]. Only 19% of the resident doctors were able to mention the rationality of given FDCs. Among them 16% were 1st year, 31% were 2nd year while 53% were 3rd year resident doctors [Figure 2]. Similarly, only 43% residents were able to mention a single banned FDC in India. Antimicrobials were the most commonly prescribed FDCs (45%). Out of these, Amoxicillin + Clavulanic acid was the most commonly prescribed antimicrobial FDC. It was prescribed by (31%) of the resident doctors [Table 2]. Other most commonly prescribed FDCs are also mentioned in Table 2. Amoxicillin + Clavulanic acid was the most commonly prescribed FDCs by resident doctors of paediatrics (61.11%), skin and venereal diseases (60%), surgery (42.11%), obstetrics and gynaecology (29.41%) and medicine (19.23%), except psychiatry, where Olanzapine + Fluoxetine (60%) was prescribed more frequently [Table 3]. According to resident doctors, the most common conditions for prescribing FDCs were infections in obstetrics and gynaecology (47.06%), pediatrics (61.11%) and surgery (52.63%). Hypertension (50%), depression (50%) and pyoderma (50%) were the most common condition in medicine, psychiatry and skin and venereal diseases respectively for prescribing FDCs. The detailed results about most commonly prescribed FDCs and the conditions in various departments are mentioned in Table 4. More than ninety percent (96%) of resident doctors opined that FDCs should be allowed to be marketed. Medical representatives (MRs) (71%), colleagues/peers (58%), Monthly Index of Medical specialities (MIMS) (51%), Continuous Medical Education (CMEs) (45%), were the most common sources of information of FDCs, Followed by others which included textbooks (42%), journals (29%), internet (19%), Essential Medicine List (10%) and newspapers (5%) [Figure 3].
Table 1.
Knowledge of advantages and disadvantages about FDCs (n=100)
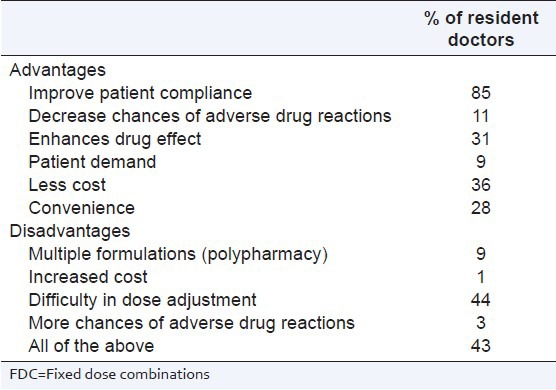
Figure 1.
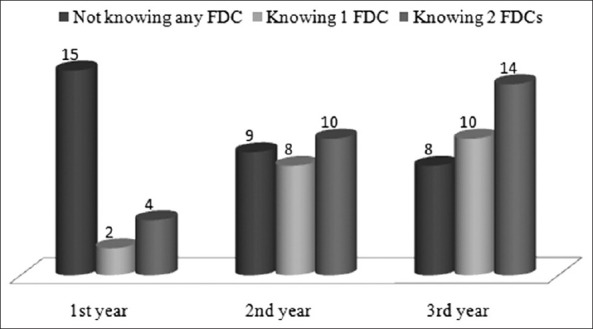
Knowledge about FDCs included in WHO EML (n = 80)
Figure 2.
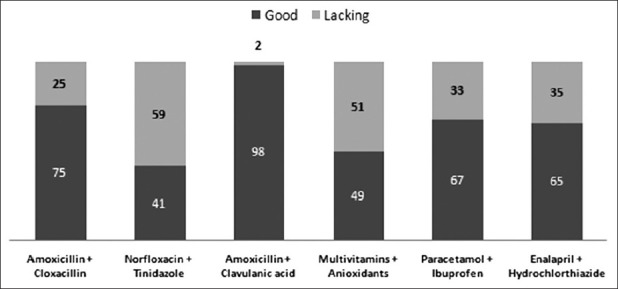
Analysis of knowledge about given FDCs
Table 2.
Commonly prescribed FDCs by resident doctors
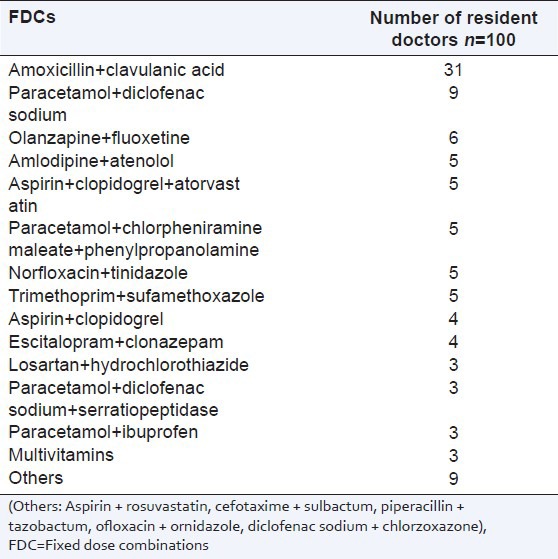
Table 3.
Commonly prescribed FDCs in various departments (n=100)
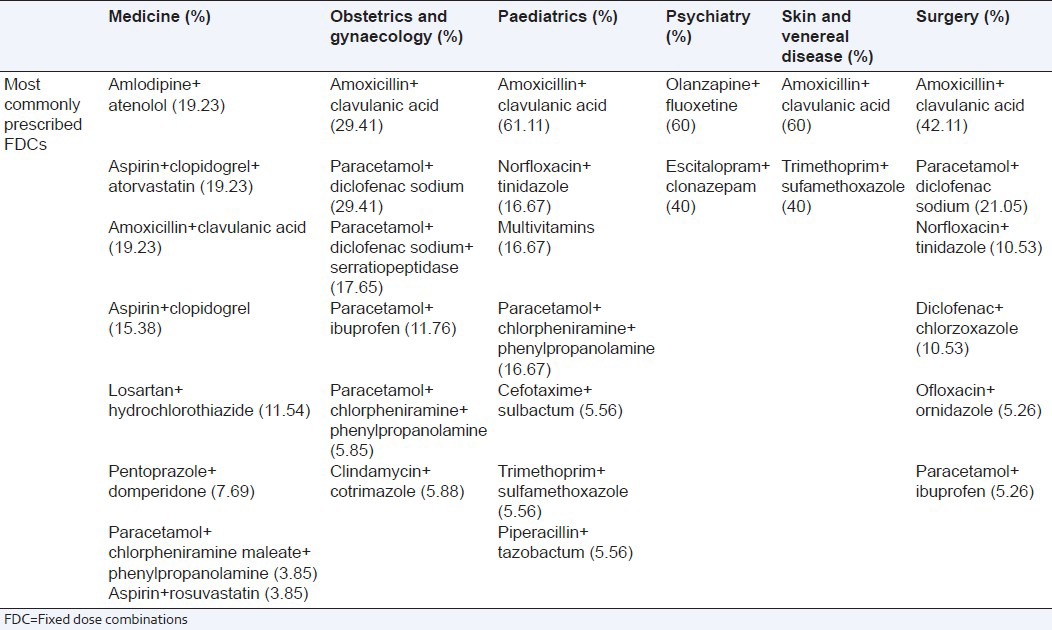
Table 4.
Common conditions for prescribing FDCs in various departments (n=100)
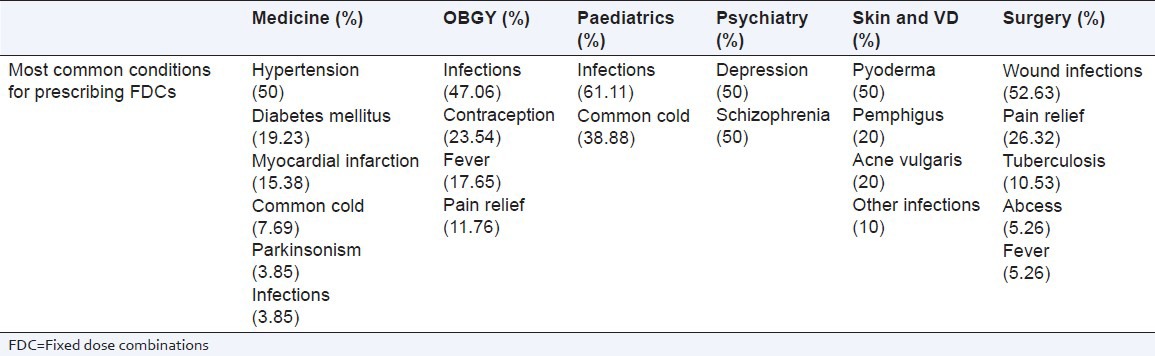
Figure 3.
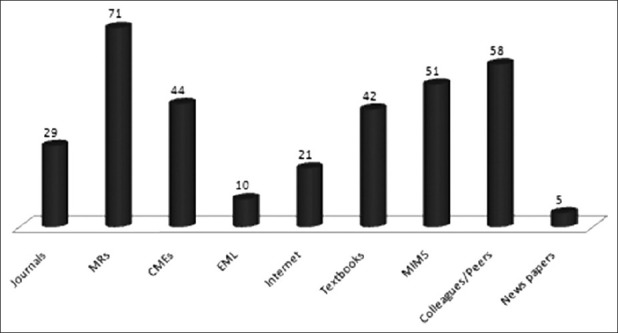
Sources of information about FDCs
DISCUSSION
The knowledge possessed by a community is indicative of their understanding of the given subject. Attitude refers to their feelings towards this subject, as well as any preconceived ideas that they may have towards it. Practice refers to the ways in which they demonstrate their knowledge and attitude through their actions.[5] The levels of knowledge, attitude and practice will enable a more efficient process of understanding the present situation as well as the reasons for it. The triad of knowledge, attitude and practice can also be useful for finding the areas where deficiencies are present. Working in those areas helps in awareness creation, as it will allow the survey to be carried out more appropriately to the needs of the community.
The trend of prescribing fixed dose combinations (FDCs) is increasing in clinical practice[6,7] There are number of advantages associated with the use of FDCs, but inappropriate and indiscriminate use of FDCs due to poor knowledge may lead to irrational prescription.[8,9] Irrational prescribing of FDCs lead to increase risk of adverse drug reactions, higher treatment cost, emergence of resistant organisms and for some time, treatment failure.[10,11] A number of studies have been carried out to evaluate the prescribing pattern of FDCs in India, but a survey about knowledge and practice for prescribing FDCs among resident doctors is lacking. As resident doctors play a major role in prescribing medicines at tertiary care teaching hospitals, the present study was carried out to evaluate knowledge, attitude and practice about prescribing FDCs among resident doctors.
It was observed from the study that improved patient compliance and less cost were the most common advantages, while difficulty in dosage adjustment was the most common disadvantage of FDCs mentioned by resident doctors. But, according to WHO guidelines, there are a number of other advantages like decreased chances of ADRs, enhanced drug effects, simplified management and handling of drug convenience of prescribing. Incompatible pharmacokinetics, drug interactions, potential quality problems are the other disadvantages of using FDCs.
Knowledge about the availability of the WHO Essential Medicine List was lacking in resident doctors. Twenty percent of them were unaware about the existence of EML, out of which 65, 30 and 5% were 1st, 2nd and 3rd year residents respectively. Results also showed that 44.12% of the 1st year, 27.27% of 2nd year and 24.24% of 3rd year resident doctors were not aware of even a single FDC included in the WHO EML. This shows that the knowledge about FDCs was lacking in 1st year resident doctors itself. Only 1/3rd of the most commonly prescribed FDCs by residents were in accordance with WHO EML, Indian EML, and the Gujarat state EML. WHO introduced the concept of essential drug list in 1977 and updates the model list every year. The government of India, under the Ministry of Health and Family Welfare has also recommended the list of essential medicines in India. Knowledge about EML and its updates helps the prescribers to select the drugs and use them rationally for better treatment outcome. The lack of knowledge about EML may be due to lack of sensitization of the residents and may be one of the important causal factors for prescribing errors.
The knowledge about rationality of given FDCs was lacking in 81% of resident doctors. On asking the resident doctors to mention about the rationality of most commonly used FDCs (amoxicillin + cloxacillin, norfloxacin + tinidazole, amoxicillin + clavulanic acid, multivitamins + antioxidants, paracetamol + ibuprofen, enalapril + hydroclorthiazide), most of the resident doctors could not do so. A variety of NSAID combinations are available as over the counter products. Thus, combining two NSAIDs or NSAID with analgesics like paracetamol does not improve the efficacy or potency of treatment and only adds to cost of therapy and risk of the adverse drug reactions.[12,13] As per WHO guidelines, the combination of vitamins are part of nutrition, and vitamin combinations should not be used indiscriminately. The cough mixtures contain expectorants, cough suppressants, antihistamines, sympathomimetics, alcohol and other CNS depressants without any rational basis.[14] All the cough remedies may not need all the ingredients at the same time. Moreover, they also contain certain drugs which have low therapeutic margin. There are number of FDCs which are not rational and still available in the market. Hence, there is need to educate resident doctors about the basis of rationality of each component of the FDCs.[15,16,17]
In our study, we observed that out of the commonly prescribed FDCs, 46% were rational, while more than 50% of them were non justifiable on the basis of their rationality. Some of these combinations were analgesics (Paracetamol + Diclofenac sodium, Paracetamol + Ibuprofen), antimicrobials (Norfloxacin + Tinidazole, Ofloxacin + Ornidazole), combination of antipsychotic and antidepressant drugs (Olanzapine + Fluoxetine) and various cough and cold mixtures in our study. Amoxicillin + Clavulanic acid was the most commonly (31%) prescribed FDC followed by Sulfamethoxazole + Trimethoprim, Amlodipin + Atenolol and losartan + Hydrochlorothiazide, which do have a rational basis of prescribing. Some of the FDCs are not included in the WHO EML, but could still be justifiable. Some of these examples are combination of more than one antihypertensive agents like amlodipine and atenolol, potassium sparing and potassium losing diuretics for the successful control of moderate to severe hypertension. Other combinations include combinations of beta - lactam antibiotics with beta - lactamase inhibitors, piperacillin and tazobactam, antacids containing a mixture of aluminium and magnesium salts, combination of theophylline and β adrenergic agonist for synergistic effect in asthma.[18,19]
Knowledge of banned FDCs was also lacking in resident doctors. More than half (58%) of the resident doctors were not able to mention a single banned FDC in India. The government of India has banned a total of 69 drugs and their combinations with other drugs for manufacturing and marketing in India.[20] Knowledge about the banned drugs/FDCs is very important as lack of this knowledge and prescribing of these agents may lead to serious, adverse drug reactions. Resident doctors were in favour of marketing of FDCs, which may be due to the convenience of prescribing, decreased pill burden of the patient and better patient compliance. In the present study, we observed that medical representatives, MIMS/CIMS and peers were the most common sources for information about FDCs while use of EML, journals and CMEs was very less, which shows that the use of authentic sources of drug information was less and could also be a factor for lack of knowledge and irrational/unjustifiable FDC prescription.
CONCLUSION
We observed that knowledge about FDCs was lacking in resident doctors. They were not able to point out the actual advantages and disadvantages of FDCs. Knowledge about rational/irrational, banned FDCs and availability of WHO EML was also lacking. Poor knowledge about FDCs leads to irrational prescriptions. Lack of utilization of authentic sources of drug information could be the most common cause of poor knowledge. Other factors which may be responsible for the present status could be increased patient load, lack of sensitization during undergraduate training, lack of education sessions about FDCs during post graduation training, sparse number of CMEs stressing upon rational use of medicine, and authentic sources of information about FDCs. As patient's health lies in the hands of healthcare professionals, awareness in resident doctors about advantages, disadvantages and rational prescribing of FDCs is essential, and it can be started from the undergraduate level of teaching. Sensitization towards authentic sources of information like EML, education programmes about FDCs as well as day to day updates regarding banned FDCs are quite necessary to promote rational use of drugs.[21,22]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Office of Combination Products. Food and Drug Administration, USA. [Last accessed on 2012 Feb 16]. Available from: http://www.fda.gov/CombinationProducts/GuidanceRegulatoryInformation/ucm109108.htm .
- 2.Kastury N, Singh S, Ansari KU. An audit of prescription for rational use of fixed dose drug combinations. Indian J Pharmacol. 1999;31:367–9. [Google Scholar]
- 3.World Health Organisation. Essential drugs: 17th updated WHO Model List 2011. [Last accessed on 2012 Aug 9]. Available from: http://www.who.int/medicines/publications/essentialmedicines/en .
- 4.Panda J, Tiwari P, Uppal R. Evaluation of rationality of some FDC: Focus on antihypertensive drugs. Indian J Pharm Sci. 2006;68:649–52. [Google Scholar]
- 5.Badran IG. Knowledge, attitude and practice the three pillars of excellence and wisdom: A place in the medical profession. Eastern Mediterranean Health Journal. 1995;1:8–16. [Google Scholar]
- 6.Anand S, Asha AN, Bhosale U, Suresh S. Emergence of irrationality in fixed dose combinations. Pharma Times. 2008;40:17–21. [Google Scholar]
- 7.Kumar SP. Fixed dose combinations (FDCs) Ration Drugs. 2008;32:1–3. [Google Scholar]
- 8.Sen A. Indian market's fixation with fixed dose combinations. Ration Drug Bull. 2002;12:1–2. [Google Scholar]
- 9.Sarkar C, Das B. Prescribing trends of fixed dose combinations in a tertiary care hospital in Nepal. J Inst Med. 2000;22:53–8. [Google Scholar]
- 10.Shewade D, Pradhan S. Auditing of prescriptions in a government teaching hospital and four retail medical stores in Pondicherry. Indian J Pharmacol. 1998;30:408–10. [Google Scholar]
- 11.Sreedhar D, Subramanian G, Udupa N. Combination drugs: Are they rational? Curr Sci. 2006;91:24–5. [Google Scholar]
- 12.Ratnakar UP, Shenoy A, Ullal SD, Sheetal D, Shivaprakash, Pemminati S, et al. Prescribing patterns of fixed dose combinations in hypertension, diabetes mellitus and dyslipidemia among patients attending a cardiology clinic in a tertiary care teaching hospital in India. Int J Compr Pharm. 2011;6:1–3. [Google Scholar]
- 13.Hogerzeil HV. Promoting rational prescribing: An international prospective. Br J Clin Pharmacol. 1995;39:1–6. doi: 10.1111/j.1365-2125.1995.tb04402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenhalgh T. Drug prescription and self-medication in India: An exploratory survey. Soc Sci Med. 1987;25:307–18. doi: 10.1016/0277-9536(87)90233-4. [DOI] [PubMed] [Google Scholar]
- 15.Patel V, Vaidya R, Nalik D, Borker P. Irrational drug use in India: A prescription survey from Goa. J Postgrad Med. 2005;51:9–12. [PubMed] [Google Scholar]
- 16.Anand S, Asha AN, Bhosale U, Suresh S. Emergence of irrationality in fixed dose combinations. Pharma Times. 2008;40:17–21. [Google Scholar]
- 17.Thomas M, Cherian AM, Mathai D. Measuring the impact of focused workshops on rational drug use. Trop Doct. 1997;27:206–10. doi: 10.1177/004947559702700407. [DOI] [PubMed] [Google Scholar]
- 18.Panda J, Tiwari P, Uppal R. Evaluation of rationality of some FDC: Focus on antihypertensive drugs. Indian J Pharm Sci. 2006;68:649–52. [Google Scholar]
- 19.Poudel A, Palaian S, Shankar PR, Jayasekera J, Izham MI. Irrational fixed dose combinations in Nepal: Need for intervention. Kathmandu Univ Med J. 2008;6:399–405. doi: 10.3126/kumj.v6i3.1723. [DOI] [PubMed] [Google Scholar]
- 20.Central drugs standard control organization. Drugs banned in India. 2012. [Last accessed on 2012 Jan 12]. Available from: http://cdsco.nic.in/html/drugsbanned.html .
- 21.Gautam CS, Aditya S. Irrational drug combinations: Need to sensitize undergraduates. Indian J Pharmacol. 2006;38:169–70. [Google Scholar]
- 22.Bapna JS, Shewade DG, Pradhan SC. Training medical professionals on the concepts of essential drugs and rational drug use. Br J Clin Pharmacol. 1994;37:399–400. doi: 10.1111/j.1365-2125.1994.tb04297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


