Abstract
Background:
Cesarean section is one of the common surgeries of women. Acute post-operative pain is one of the recognized post-operative complications.
Aims:
This study was planned to compare the effects of suppositories, indomethacin, diclofenac and acetaminophen, on post-operative pain and opioid usage after cesarean section.
Materials and Methods:
In this double-blind clinical trial study, 120 candidates of cesarean with spinal anesthesia and American Society of Anesthesiologists (ASA) I-II were randomly divided into four groups. Acetaminophen, indomethacin, diclofenac, and placebo suppositories were used in groups, respectively, after operation and the dosage was repeated every 6 h and pain score and opioid usage were compared 24 h after the surgery. The severity of pain was recorded on the basis of Visual Analog Scale (VAS) and if severe pain (VAS > 5) was observed, 0.5 mg/kg intramuscular pethidine had been used.
Statistical Analysis Used:
The data were analyzed in SPSS software version 15 and analytical statistics such as ANOVA, Chi-square, and Tukey's honestly significant difference (HSD) post-hoc.
Results:
Pain score was significantly higher in control group than other groups, and also pain score in acetaminophen group was higher than indomethacin and diclofenac. The three intervention groups received the first dose of pethidine far more than control group and the distance for diclofenac and indomethacin were significantly longer (P < 0.001). The use of indomethacin, diclofenac, and acetaminophen significantly reduces the amount of pethidine usage in 24 h after the surgery relation to control group.
Conclusions:
Considering the significant decreasing pain score and opioid usage especially in indomethacin and diclofenac groups rather than control group, it is suggested using of indomethacin and diclofenac suppositories for post-cesarean section analgesia.
Keywords: Acetaminophen, cesarean section, diclofenac, indomethacin, opioid
INTRODUCTION
Pain is an unpleasant emotional and sensory experience along with active or potential tissue damage. For pain relief after cesarean operation, various drugs such as opioids and non-steroidal anti-inflammatory drugs (NSAIDs) are used. Due to complications of opioids, particular attention has been paid to NSAIDs, and the physicians use these drugs as useful analgesics in controlling different types of pain.[1,2] Salicylate and other similar drugs, which are used in treatment of rheumatic diseases, are able to prevent symptoms and signs of inflammation. These drugs also have analgesic and antipyretic effects but their anti-inflammatory properties control some disorders in which pain has directly correlations with the severity of inflammation.
Opiates are very effective for treating acute and chronic pain, although they may also be cases of abuse. When opiates are prescribed, make rapid and potential analgesia. The most common intravenous opioids used in pain relief after gynecological surgeries are morphine, hydromorphone, and fentanyl.[3] All opioids could cause common side effects that include depression in respiratory stimulation center in the brainstem, the hypotension (which is more common in hypovolemic patients), and vomiting. Morphine often causes histamine releasing and may cause flashing, tachycardia, hypotension, itch, and bronchospasm. Long-term administration of opioids slows gastrointestinal transit and causes ileus and constipation in many patients. This condition is likely created by binding opioids to opioids’ receptors in the gastrointestinal tract.[4]
Considering the importance of maternal care in the first hours after birth and the necessity of relaxation for her to communicate with the infant and start feeding, reducing pain after cesarean section is of high importance.[5] A study performed in January 2008 on reducing pain after cesarean section with paracetamol, diclofenac, or their combination declared that morphine has been used 38% less in the combination of diclofenac and paracetamol than paracetamol group. Nevertheless, there was no significant difference in diclofenac group than paracetamol–diclofenac group.[6] Another study conducted in Lebanon in July 2001, investigating the effects of diclofenac or propacetamol in reducing pain after caesarean section in patients receiving morphine, indicated that diclofenac improved analgesia after cesarean section (according to Visual Analog Scale, VAS) and reduced morphine consumption rate significantly.[7] As to the administration of opioids, in addition to the fear of the occurrence of respiratory complications following the injection of these drugs, fear of addiction to opioids are the main reasons to reduce the amount of these drugs to pain control. The complex rules and regulations concerning opioids prescription actually have imposed some limitations on the consumption of these pain-relieving drugs.[8] Currently, as for offering a variety of NSAIDs in the forms of oral, injectable, and suppository medications, particular attention has been paid to these drugs. diclofenac and indomethacin are among those drugs that are effective in controlling post-operative pain. In addition, acetaminophen is an analgesic with minimal side effects that can be effective in controlling post-operative pain. Therefore, with regard to the restrictions in prescribing opioids and little complications of acetaminophen and NSAIDs, this study was conducted with the aim of comparing the effects of three suppositories of acetaminophen, indomethacin, and diclofenac on reducing post-operative pain and reduction of opioid consumption after cesarean section in Alavi Hospital of Ardabil City in Iran.
MATERIALS AND METHODS
This study is a randomized, double-blind clinical trial. The study population included pregnant patients volunteered to cesarean surgery with ASA class I or II referred to Alavi Hospital. They entered into the plan after submitting a written agreement. This study was conducted in 2007 to compare the effects of indomethacin, diclofenac, and acetaminophen suppositories on cesarean post-operative pain severity and opioids consumption rate in Ardebil Alavi Hospital following the approval of Ethics Committee of Ardebil University of Medical Sciences. In order to collect data, a check list was designed.
Inclusion criteria were patients with ASA class I or II, voluntary for cesarean section with spinal anesthesia, and exclusion criteria included kidney diseases, pregnancy hypertension, active peptic ulcers, a history of abdominal surgery, history of cardiovascular disease, and twin pregnancy.
Based on a 30% cesarean post-operative pain reduction in previous studies, to achieve a 30% reduction with a power of 0.80 and a <0.05, 30 women in each group and totally 120 people were required. Sampling method has been a non-random, conventional method and then using randomized blocks, 120 patients were categorized into four groups of A, B, C, and D each including 30 people [Figure 1]. All surgeries were performed by one gynecologist and spinal anesthesia for all patients was performed by injection of the standard amount of hyperbaric 5% Lidocaine (75-100 mg) into the cerebrospinal fluid. None of the patients was administered opioid or sedative drug during the operation.
Figure 1.
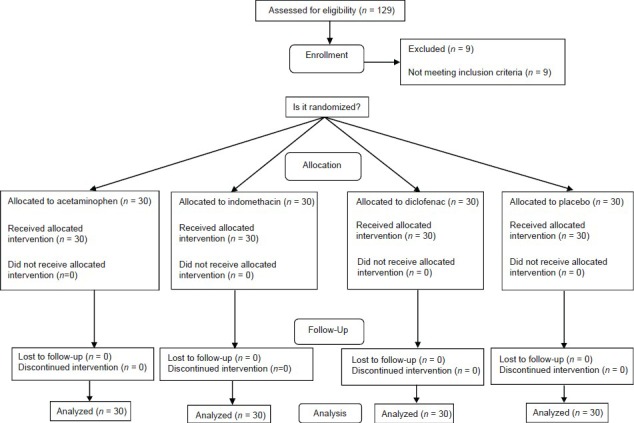
Methodology flowchart
During surgery, patients were monitored in terms of heart rate and arterial oxygen saturation continuously as well as the systolic and diastolic blood pressure once every 5 min.
At the end of surgery, the anesthesia nurse administered 50 mg indomethacin suppository to group A, 50 mg diclofenac suppository to group B, 325 mg acetaminophen suppositories to group C, and placebo suppositories to group D. This was repeated every 6 h (until 24 h) and none of the patients was informed of the type of drug prescribed. The pain severity was recorded by a trained anesthesia nurse using VAS. Pethidine was used in case of severe pain (VAS > 5) as intramuscular 0.5 mg/kg. Intramuscular injection of pethidine (to avoid respiratory complications resulting from the rapid uptake of intravenous injection) has already been used by gynecologists as a routine post-operative analgesic drug, and this is the reason why we used this drug for pain relief in this research. VAS is a measurement instrument of pain severity using horizontal line, 10 cm in length, anchored by word descriptors at each end that no pain is at one end and the very severe pain is indicated at the other end. The patient marks on the line the point that they feel represents their perception of their current state. This method can be used to evaluate the effect of drugs on relieving pain.[4] Frequency and dosage of opioids injection in 24 h after surgery were obtained from the patient records and the nurses report forms and was recorded on the patients’ check list. The information-recording anesthesia nurse, the nurse prescribing medicine, and the data analyzer had no information about the kind of prescribed medication. All the variables in groups were collected in a check list and analyzed by SPSS version 15. ANOVA, Chi-square, and Tukey's honestly significant difference (HSD) post-hoc were used for data analysis in the study. P < 0.05 was considered significant.
RESULTS
There was no difference between the study and control groups in age and duration of surgery [Table 1]. The pain after surgery started in the four groups in the range of 39.46 ± 8.75 min to 43.32 ± 9.33 min, and statistically there was no significant difference between the groups (P = 0.084) [Table 2]. The first dose of pethidine was administered in the range of 46.36 ± 29.45 min to 54.46 ± 31.28 min, that this time was significantly different in four groups (P < 0.001) [Table 2]. In total, the lowest and highest times of pethidine injection have been 0 and 4, respectively. Most patients in the control group (43.3%) had three times pethidine injection and most patients in acetaminophen group (50%) had one pethidine injection. In indomethacin and diclofenac groups, the lowest numbers of pethidine injections have been zero and one time, respectively, and most patients (70% in indomethacin and 80% in diclofenac group) received no opioids. Using “ANOVA” statistical test, considering the number of pethidine injections, there has been statistically significant difference among the four mentioned groups (P < 0.001).
Table 1.
Mean and standard deviation of age and duration of operation of patients in the studied groups
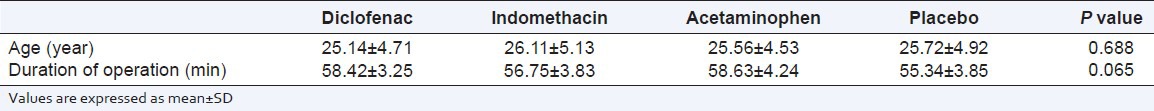
Table 2.
Pain after surgery starting time and first dose of pethidine administrating time in the studied groups
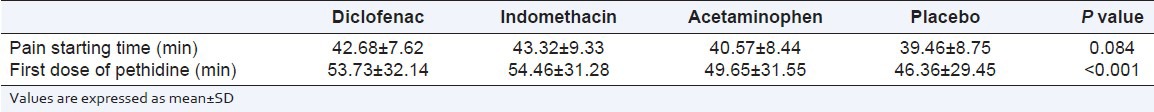
Average dose of pethidine in the placebo group was 138.33 mg, in acetaminophen group 42.21 mg, in indomethacin group 17.32 mg, and in diclofenac group, it was 9.81 mg. There has been statistically significant difference among the four mentioned groups (P < 0.001) [Table 3]. There had been a significant difference between acetaminophen and the two other groups (indomethacin and diclofenac) in terms of the first injection of pethidine (P < 0.001), number of pethidine injections in 24 h (P < 0.01) and the dose of pethidine in 24 h (P = 0.005). The mean pain intensity at 1, 12, and 24 h after surgery was significantly different among the four groups [Table 4]. Using the Tukey's HSD test, there had been a significant difference in pain severity during 12 h (P = 0.002) and 24 h after surgery (P = 0.014) among acetaminophen group and the two other groups (indomethacin and diclofenac).
Table 3.
Average dose of pethidine injected in 24 h in the studied groups
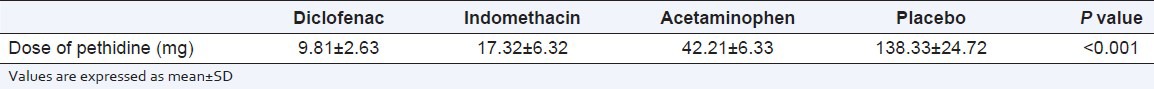
Table 4.
Mean and standard deviation of pain intensity based on visual analog scale criteria in studied groups at different hours after surgery

In total, only seven patients had suffered from some complications, six patients vomiting, and one itching. Most complications have been reported in the control group (three patients) and the least in acetaminophen and diclofenac group (each only one case). Since the number of patients suffering from side effects was less, using statistical tests were not possible.
DISCUSSION
According to this study results, the use of indomethacin, diclofenac, and acetaminophen in comparison with the control group significantly reduced pain intensity at different hours after surgery, and decreased the use of pethidine in 24 h after surgery. Moreover, it was found that acetaminophen suppositories were less effective than other two drugs in reducing the pain intensity and the dose of pethidine injection. Considering the injection time of the first dose of pethidine, compared with the control group, all three groups received drugs with more time intervals, and this time interval was significantly longer for both suppositories of NSAID (diclofenac and indomethacin). Most complications resulting from opioid injection after surgery were also observed in the control group.
In all measured parameters, there was no significant difference between the two groups of indomethacin and diclofenac.
Several studies about the efficacy of various drugs affecting pain relief after cesarean section have been performed. In our study, there was a significant difference in terms of pain intensity in 1, 12, and 24 h after surgery between the control (placebo) and intervention groups. This result was similar to the results of some other studies,[2,7,9,10,11,12,13] whereas in other studies this difference has not been significant.[4,5,14,15,16] For example, in a study conducted by Siddik et al,[7] on 80 patients’ candidate for elective cesarean section in 2001, the patients were divided into four groups of placebo, rectal diclofenac, intravenous propacetamol, and combination of diclofenac and propacetamol. VAS showed that analgesia resulted from diclofenac has been very effective and reduced morphine consumption significantly and the results have been very similar to our study. In many previous studies, considering the dosage of opioid use after surgery with NSAID, there has been significantly reduction in opioid consumption.[7,10,12,13,15,16,17] Some other studies have also shown that acetaminophen use has also significantly decreased opioid consumption, but this reduction has not been equal to NSAID group.[6,7] This study also confirmed the same result.
In a double-blind clinical trial study conducted by Munishankar et al., in 2008 on 78 candidates for elective cesarean section, the patients were divided into three groups of “diclofenac, paracetamol, and diclofenac–paracetamol,” and it was found that the combination of diclofenac and paracetamol compared with paracetamol group alone less morphine had been used and this difference was significant. However, in diclofenac group compared with diclofenac–paracetamol group, there was no significant difference, and this indicates diclofenac to be more effective than paracetamol in reducing opioid consumption.[6] In another study conducted by Montgomery, et al,[16] in 1996 on 60 patient candidates for non-emergency abdominal gynecological surgery, the first group of patients received 1.5 g rectal paracetamol, the second group 100 mg rectal diclofenac, and the third group a combination of these two drugs before the surgery. It was observed that morphine consumption dose in the paracetamol was significantly more than the other two groups (P < 0.05), but there was no significant difference between the three groups of drugs in terms of the side effect. In our study also, there was a significant difference compared with the control group in terms of both pain intensity and opioid consumption rate in both diclofenac and acetaminophen groups.
In a series of studies, it has been shown that the side effects of opioid in comparison with other drugs such as paracetamol and NSAID groups have had significant difference,[5,18] but in some studies, this difference has not been significant.[14,16] In general, the number of patients with side effects has also been lower in our research, although clinically the number of patients with drug side effects was higher in the opioid group.
In 2001, a study was conducted by Ambrose on 297 candidates of elective cesarean section undergoing spinal anesthesia with standard methods using hyperbaric bupivacaine. In this research, the patients were divided into two groups of “placebo and indomethacin suppository 50 mg.” According to VAS criteria, the pain intensity was assessed and the side effects were evaluated. They concluded that the pain intensity and morphine consumption rate and frequency after surgery have significantly been lower in the indomethacin group.[11] The results of that study correlated with our study.
The limitation of our investigation is that this study has only been conducted on candidates for cesarean section so the results may not be generalizable to other surgical procedures, also the future investigations might useful with larger sample size to approve the effects of non-steroidal anti-inflammatory suppositories.
CONCLUSION
According to the results of this study and other studies, we can say that in terms of relieving pain after surgery, NSAIDs are more effective than opioids and acetaminophen. Due to the complicated rules and restrictions on the use of opioids and the high rate of side effects related to opioids, we could suggest prescribing NSAIDs particularly in the form of suppositories, which has no side effects such as gastrointestinal bleeding, as a suitable alternative for relieving opioid after the operation. Acetaminophen was also more effective than opioids, but it could not be as effective as NSAIDs. Thus, regarding the existed situation, it would be better if we use NSAIDs to relieve pain after cesarean section.
Footnotes
Source of Support: Ardabil University of Medical Sciences, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.Trevor A, Katzung B, Masters S. 6th ed. New York: Lange Medical Books/McGraw-Hill; 2002. Katzung and Trevor's Pharmacology; pp. 322–30. [Google Scholar]
- 2.Elyasi H, Heidari M, Shahbeigi S. Comparative effects of indomethacin suppository and pethidine on pain after cesarean section. Pajoohandeh J. 2000;5:9–15. [Google Scholar]
- 3.Liu SS, Wu CL. The effect of analgesic technique on postoperative patient-reported outcomes including analgesia: A systematic review. Anesth Analg. 2007;105:789–808. doi: 10.1213/01.ane.0000278089.16848.1e. [DOI] [PubMed] [Google Scholar]
- 4.Chestnut DH. 4th ed. Philadelphia: Mosby; 2009. Chestnut's obstetric anesthesia principles and practice; pp. 576–86. [Google Scholar]
- 5.Pakar Tadbiri SH, Rahimi E. Comparison of morphine and piroxicam in decreasing post cesarean pain. Scientif J Kurdistan Uni Med Sci. 2001;19:10–14. [Google Scholar]
- 6.Munishankar B, Fettes P, Moore C, Mcload GA. A double-blind randomized controlled trial of paracetamol, diclofenac or their combination for pain relief after cesarean section. Int J Obstet Anesth. 2008;17:9–14. doi: 10.1016/j.ijoa.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Siddik SM, Aouad MT, Jalbout MI, Rizk LB, Kamar GH, Baraka AS. Diclofenac and/or propacetamol for postoperative pain management after cesarean delivery in patients receiving patient controlled analgesia morphine. Reg Anesth Pain Med. 2001;26:310–5. doi: 10.1053/rapm.2001.21828. [DOI] [PubMed] [Google Scholar]
- 8.Abdollahi AA, Arya B, Golalipour MJ, Vakili MA. Comparison of analgesic effects of intramuscular pethedine to diclofenac Na suppository among postoperative inguinal hernioplasty patients. J Gorgan Uni Med Sci. 2001;3:25–29. [Google Scholar]
- 9.Cobby TF, Crighton IM, Kyriakides K, Hobbs GJ. Rectal paracetamol has a significant morphine-sparing effect after hysterectomy. Br J Anaesth. 1999;83:253–6. doi: 10.1093/bja/83.2.253. [DOI] [PubMed] [Google Scholar]
- 10.Rashid M, Jaruidi HM. The use of rectal diclofenac for post-cesarean analgesia. Saudi Med J. 2000;21:145–9. [PubMed] [Google Scholar]
- 11.Ambrose FP. A retrospective study of the effect of postoperative indomethacin rectal suppositories on the need for narcotic analgesia in patients who had a cesarean delivery while they were under regional anesthesia. Am J Obstet Gynecol. 2001;184:1544–7. doi: 10.1067/mob.2001.114920. [DOI] [PubMed] [Google Scholar]
- 12.Lowder L, Danald P, Don H, Todd M. A randomized, controlled trial to compare ketorolac tromethamine versus placebo after cesarean section to reduce pain and narcotic usage. Am J Obst Gyn. 2003;189:1559–62. doi: 10.1016/j.ajog.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 13.Sayadi Z. Effect of indomethacin suppositories on pain relief after cesarean section and to prescribe narcotics in hospitals and Qods maternity ward in 2002-2003. Zahedan J Research in Med Sciences. 2004;6:9–15. [Google Scholar]
- 14.Arya B, Abdollahi AA, Golalipour MJ, Kazemnezhad K, Mohammadi MR. Evaluation of post-operative analgesic efficacy of intramuscular pethidine, compared to indomethacin and diclofenac Na suppositories in unilateral Inguinal hernioplasty patients. J Med Sci. 2007;7:311–4. [Google Scholar]
- 15.Dahl V, Hagen IE, Sveen AM, Norseng H, Koss KS, Steen T. High-dose diclofenac for postoperative analgesia after elective caesarean section in regional anaesthesia. Int J Obstet Anesth. 2002;11:91–4. doi: 10.1054/ijoa.2001.0931. [DOI] [PubMed] [Google Scholar]
- 16.Montgomery JE, Sutherland CJ, Kestin IG, Sneyd JR. Morphine consumption in patients receiving rectal paracetamol and diclofenac alone and in combination. Br J Anaesth. 1996;77:445–7. doi: 10.1093/bja/77.4.445. [DOI] [PubMed] [Google Scholar]
- 17.Yildizhan R, Yildizhan B, Sahin S, Suer N. Comparison of the efficacy of diclofenac and indomethacin suppositories in treating perineal pain after episiotomy or laceration: A prospective, randomized, double-blind clinical trial. Arch Gynecol Obstet. 2009;280:735–8. doi: 10.1007/s00404-009-1006-3. [DOI] [PubMed] [Google Scholar]
- 18.Pluim MA, Wegener JT, Rupreht J, Vulto AG. Tramadol suppositories are less suitable for post-operative pain relief than rectal acetaminophen/codeine. Eur J Anaesthesiol. 1999;16:473–8. doi: 10.1046/j.1365-2346.1999.00520.x. [DOI] [PubMed] [Google Scholar]


