Abstract
Fraud and misconduct in clinical research is widespread. Good clinical practice is a guideline adopted internationally as standard operating procedure for conduct of clinical research. Despite these guidelines being available, unavailability of internationally harmonized framework for managing research fraud and misconduct makes clinical research a highly vulnerable area to commit fraud. Fraud could be of various types and due to various reasons. Whatever the circumstances be, any fraud should be dealt with strictly and regulations should be in place to prevent its occurrence.
Keywords: Clinical research, fraud, misconduct
INTRODUCTION
Scientific fraud reappears with alarming consistency from paleontology to nanotechnology. Several studies have found that more than 40% of surveyed researchers were aware of misconduct but did not report it. Sheehan et al. reported in 2005 that 17% of surveyed authors of clinical drug trials reported that they personally knew of fabrication in research occurring over the previous 10 years.[1] Quality at sites is usually judged by audits and inspections. There has been as high as 23% (official action indicated) for cause inspections conducted by US Food and drug Administration (USFDA) over the last several years.[2] These kinds of results indicate that there exists a substantial problem. Fraud/misconduct can lead to study losing its entire credibility. Moreover, it can lead to ineffective or harmful treatment being available or patients being denied of effective treatment. This article discusses the difference between fraud and misconduct, the possible reasons for the occurrence of the same and explores options, which can possibly help prevent such instances.
IS FRAUD AND MISCONDUCT THE SAME?
Fraud and misconduct are the two terminologies often used interchangeably. However, there is a gross distinction between the two. Scientific misconduct/fraud is a violation of the standard codes of scholarly conduct and ethical behavior in scientific research. Definition of fraud as defined in court is “the knowing breach of the standard of good faith and fair dealing as understood in the community, involving deception or breach of trust, for money.”[1] Fraud is an intentional deception made for personal gain or to damage another individual, for instance, intentionally falsifying and/or fabricating research data, and misleading reporting of the results. Misconduct may not be an intentional action, rather an act of poor management. It also includes failure to follow established protocols if this failure results in unreasonable risk or harm to humans.[3] Fraud should have an element of deliberate action, which is not the case with misconduct.
The Medical Research Council (MRC) definition of misconduct and fraud (or a variation of the MRC code) is widely used. This code states the following definition:
The fabrication, falsification, plagiarism or deception in proposing, carrying out or reporting results of research or deliberate, dangerous or negligent deviations from accepted practices in carrying out research. It includes failure to follow established protocols if this failure results in unreasonable risk or harm to humans, other vertebrates or the environment and facilitating of misconduct in research by collusion in, or concealment of, such actions by others. It also includes intentional, unauthorised use, disclosure or removal of, or damage to, research-related property of another, including apparatus, materials, writings or devices used in or produced by the conduct of research. It does not include honest error or honest differences in the design, execution, interpretation or judgement in evaluating research methods or results or misconduct unrelated to the research process. Similarly it does not include poor research unless this encompasses the “intention to deceive” (MRC, 1997).[4]
WHY DOES ANYONE COMMIT FRAUD/MISCONDUCT?
Reasons for fraud/misconduct in clinical Research could vary from personal to professional. Fraud could be a result of professional over ambition to become famous, a gain in prestige by being a part of international clinical trials or for financial interests. At times it could be due to laziness of the researcher or site staff for complex studies needing repeat assessments e.g., repeat blood pressure measurements, Blood pressure rounded off to nearest 5 mm, timed spirometry assessments. At times, misconduct also results when an investigator strongly believes intuitively in the “right” answer despite the available evidence being contrary.[5] Misconduct could also be due to innocent ignorance like backdating the subject's signature on a consent form because the subject forgot to date the form initially or discarding source documents after accurate transcription or even creating source documents from case record forms. Pressures for promotion and tenure, competition amongst investigators, need for recognition, ego, personality factors and conflicting personal and professional obligations are some factors, which can influence certain individuals to involve in fraud/misconduct. There could also be associated environmental factors such as amount of oversight of the study, existence of explicit versus implicit rules, penalties and rewards attached to such rules, extent of training imparted, regulations involved and insufficient mentoring.[6]
ARE THERE DIFFERENT TYPES OF FRAUD/MISCONDUCT?
Fraud can be fabrication, falsification, and plagiarism of data or even deception in conduct. Fabricating data involves creating a new record of data or results. Most commonly fabricated documents are Informed consent Forms and Patient diaries. Falsifying data means altering the existing records. It is the deliberate distortion or omission of undesired data or results. Plagiarism on the other hand is an unacknowledged presentation or exploitation of work and ideas of others’ as one's own. Deception in clinical research is the deliberate concealment of a conflict of interest or inclusion of deliberately misleading statements in research proposals or other documents.
The most common types of misconduct in clinical research are: Failure to follow an investigational plan; inadequate and inaccurate records; inadequate drug accountability; inadequate completion of informed consent forms; failure to report adverse drug reactions; failure to obtain and/or document subject consent; failure to notify an Institutional Review Board (IRB)/Ethics Committee (EC) of changes/progress reports; failure to obtain or document IRB approval.[3,7]
CAN RESEARCH FRAUD BE PICKED UP EARLY?
Red flags or warning signals, during the conduct of a clinical trial should prompt the monitor to be more vigilant and look at the data with a magnifying glass. For example, for patients seen at a given medical center or by a particular doctor, excessive instances of perfect attendance on the scheduled day could be a hallmark of falsified data.[1] The most important identifiers include implausible trends, e.g., 100% drug compliance, identical lab on electrocardiogram results, no serious adverse events reported, subjects adhering perfectly to a visit schedule.[3] Furthermore, certain practices or behavior at the site or by site personnel should raise suspicion in the mind of the monitor though they may not definitely indicate any kind of fraud. Major differences in trends at a particular site from other sites, unusually fast recruitment, very few withdrawals, very few adverse events being reported, all drugs being dispensed in a similar manner (e.g., all tubes of cream dispensed being pressed at the same point), repeat postponement of meetings or same pen used throughout the study are some of the indicators for a monitor to look at the site more closely.[8]
WHAT COULD BE THE IMPACT OF FRAUD?
The impact on affected individuals and the research community can be profound. Such incidents result in huge cost to the sponsor in terms of additional resource for investigating fraud and cost of possibly repeating those aspects of research, which were fraudulent. It can also leads to disciplinary action for researchers. Such a researcher may not be allowed to be a part of any advisory committee or peer review board. Any article published by such a researcher might be re-reviewed and retracted if required. Fraudulent clinical research also affects the validity of data and impacts the core of good clinical practice adversely, i.e., rights, safety and well-being of research participants. On a broader scale of impact on health-care, it can lead to wrong or ineffective or harmful molecules being brought in the market.[9,10]
HOW CAN WE STRENGTHEN RESEARCH MISCONDUCT AND FRAUD DETECTION?
Role of IRBs/ECs should be strengthened in safeguarding interest of research participants. They should have internal control and review mechanisms for monitoring the ethical and quality aspects of ongoing studies. Existing regulations if any must be simplified and made more effective. Should there be no existing regulations, they must be put in place to manage fraudulent issues. All organizations who are involved in clinical research should have clear operational policies and procedures for approach to research misconduct and fraud. Whistle blowers should be cultivated and there should be guidelines agreed upon internationally to safeguard them.
WHAT ARE VARIOUS COUNTRIES DOING TO MANAGE RESEARCH FRAUD?
Despite fraud being recognized as a criminal act by all nations there are no international rules, which harmonize the management and regulation of clinical research dishonesty or misconduct. Most countries do not have laws specific to manage fraud in clinical research and have adopted their own approaches. Table 1 mentions the agencies relevant to research fraud.
Table 1.
Agencies relevant to research fraud (adapted from Sheehan[1])
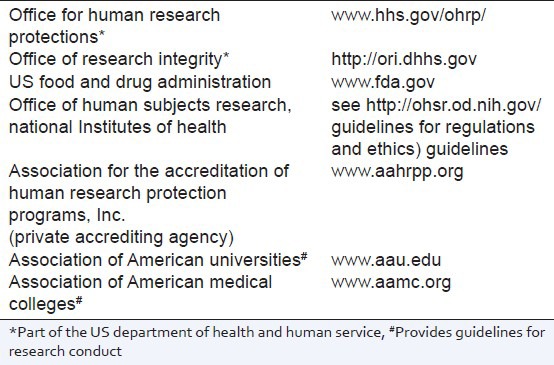
In United States, there are different bodies like Office for Human Research Protections which provides guidance, education and clarification on human research subject protection. Another body Office of Research Integrity promotes integrity in biomedical and behavioral research. FDA plays a major role in prevention and detection of fraud. If the site has not complied with regulatory requirements or has engaged in fraudulent activity, FDA has the power to disqualify the investigator from taking part in further research. National Research Ethical Council of Finland produces guidelines for prevention and investigations of alleged scientific dishonesty. However, responsibility of taking actions against those found guilty remains with universities and research institutes. In Denmark, Danish Committee on Scientific Dishonesty, which was split into three groups often sit together to consider cases and can recommend sanctions to be taken in cases of fraud. National Committee for the Evaluation of Dishonesty in Health Research in Norway since 1994 reports findings to the institution and the involved parties, but again leaves any sanctions up to the employers. In Sweden, the institutions conduct their own investigations, with an expert advisory group, linked to the Swedish MRC (MFR, providing guidance. Every institution in Germany also has its own committee to investigate and suggest actions in cases of suspected research misconduct. The Committee of Inquiry on Allegations of Scientific Misconduct investigates allegations of scientific misconduct carried out by those who receive deutsche forschungsgemeinschaft- an academic research funding agency funding. If scientific misconduct is established, the committee's findings are forwarded to the central steering Joint Committee with a recommendation. France has a principle medical body (De’le’ gation á l’IntégriteéScientifique) to focus on both the prevention of research fraud and the sanctions to be taken against individuals or institutions found guilty.[7,11] National Panel for Research Integrity has been proposed in United Kingdom as a joint venture between UK Universities and Department of Health to provide independent support to the Health and Biomedical Sciences Research Community to establish and demonstrate effective systems for research integrity and share/promote best practice.[12]
India also has no specific law pertaining to scientific fraud. The responsibility of investigating and taking action against fraudulent instances remains with the Universities or sponsors or Institutions and then they need to notify the same to Drug Controller General of India, a central body, which is responsible for approval of clinical trials in India.
CAN WE PREVENT FRAUD FROM EVER HAPPENING?
It probably might not be possible to completely prevent fraud but definitely measures can be taken to reduce its incidence to a great extent. In a 2008 “Nature” article entitled “Repairing Research Integrity,” Titus et al.[13] listed six strategies to champion research integrity:
Adopt zero tolerance-all suspected misconduct must be reported and all allegations must be thoroughly and fairly investigated.
Protect whistle-blowers-careful attention must be paid to the creation and dissemination of measures to protect whistleblowers.
Clarify how to report-establish clear policies, procedures and guidelines related to misconduct and responsible conduct.
Train the mentors-researchers must be educated to pay more attention to how they work with their junior team members.
Use alternative mechanisms-institutions need continuing mechanisms to review and evaluate the research and training environment of their institution, such as internal auditing of research records.
Model ethical behavior-institutions successfully stop cheating when they have leaders who communicate what is acceptable behavior, develop fair and appropriate procedures for handling misconduct cases, develop and promote ethical behavior and provide clear deterrents that are communicated.
CONCLUSION: CAN WE BUILD THE ‘CULTURE’ OF RESEARCH?
Research fraud is a reality which nobody can shy away from. Furthermore, clinical research is very vulnerable to fraud due to no effective mechanism in place for detecting, investigating and prosecuting fraud in most of the countries. Thus, it is very critical that “culture of research” be developed within the system, which should be based on basic fundamentals of integrity, openness and honest work. There must be official bodies in the country, which could investigate and prosecute clinical research fraud. Every organization involved in clinical research should have and implement clear policies and Standard Operating Procedures (SOPs), which encourage disclosures of fraud conduct. No matter the circumstances surrounding the case, research fraud should be considered very serious and should not be taken lightly. Open communication amongst the research groups on this important aspect of clinical research in addition to discussion on ongoing projects and practices may help reduce the incidence of fraud if not completely prevent it. Finally, the emphasis should be more on quality rather than quantity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sheehan JG. Fraud, conflict of interest, and other enforcement issues in clinical research. Cleve Clin J Med. 2007;74:S63–7. doi: 10.3949/ccjm.74.suppl_2.s63. [DOI] [PubMed] [Google Scholar]
- 2.Bhatt A. Quality of clinical trials: A moving target. Perspect Clin Res. 2011;2:124–8. doi: 10.4103/2229-3485.86880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jessen J, Robinson E, Bigaj S, Popiolek S, Goldfarb NM. Unreported clinical research fraud and misconduct. J Clin Res Best Pract. 2007;3:1–5. [Google Scholar]
- 4.NHS R and D Forum Advice for NHS Trusts: Research Misconduct and Fraud, 2004. [Last accessed 2013 Feb 4]. Available from: http://www.rdforum.nhs.uk/workgroups/rg/misconduct_0704.doc .
- 5.Weir C, Murray G. Fraud in clinical trials: Detecting it and preventing it. Significance. 2011:164–8. [Google Scholar]
- 6.Habermann B, Broome M, Pryor ER, Ziner KW. Research coordinators’ experiences with scientific misconduct and research integrity. Nurs Res. 2010;59:51–7. doi: 10.1097/NNR.0b013e3181c3b9f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barrett J. Fraud and misconduct in clinical research. In: Edwards DL, Fletcher J, Fox AW, Stonier PD, editors. Principles and Practice of Pharmaceutical Medicine. 2nd ed. England: John Wiley and Sons Ltd; 2007. pp. 631–41. [Google Scholar]
- 8.Huk JP, Huk J, Filip R. Fraud and misconduct in clinical research. J Pre-Clinical Clin Res. 2010;4:158–60. [Google Scholar]
- 9.Horne B, Dodsworth N. Fraud and misconduct in clinical trial. Quasar. 2011:17–21. [Google Scholar]
- 10.Al-Marzouki S, Roberts I, Marshall T, Evans S. The effect of scientific misconduct on the results of clinical trials: A Delphi survey. Contemp Clin Trials. 2005;26:331–7. doi: 10.1016/j.cct.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 11.Ankier SI. Dishonesty, misconduct and fraud in clinical research: An international problem. J Int Med Res. 2002;30:357–65. doi: 10.1177/147323000203000401. [DOI] [PubMed] [Google Scholar]
- 12.Stonier P, McInnes G, Murie J, Petrie J, Wells F. A national panel for research integrity: A proposed blueprint for the prevention and investigation of misconduct in biomedical research. Proc R Coll Physicians Edinb. 2001;31:253–5. [Google Scholar]
- 13.Titus SL, Wells JA, Rhoades LJ. Repairing research integrity. Nature. 2008;453:980–2. doi: 10.1038/453980a. [DOI] [PubMed] [Google Scholar]


