Abstract
Cancer cells are long known to exhibit increased aerobic glycolysis, but glycolytic inhibition has not offered a viable chemotherapeutic strategy in part due to the systemic toxicity of antiglycolytic agents. However, recent studies suggest that a combined inhibition of glycolysis and mitochondrial function may help overcome this issue. In this study, we investigated the chemotherapeutic efficacies of mitochondria-targeted drugs (MTDs) in combination with 2-deoxy-D-glucose (2-DG), a compound that inhibits glycolysis. Using the MTDs termed Mito-CP and Mito-Q we evaluated relative cytotoxic effects and mitochondrial bioenergetic changes in vitro. Interestingly, both Mito-CP and Mito-Q synergized with 2-DG to decrease ATP levels in two cell lines. However, with time, the cellular bioenergetic function and clonogenic survival were largely restored in some cells. In a xenograft model of human breast cancer, combined treatment of Mito-CP and 2-DG led to significant tumor regression in the absence of significant morphological changes in kidney, liver, or heart. Collectively, our findings suggest that dual targeting of mitochondrial bioenergetic metabolism with MTDs and glycolytic inhibitors such as 2-DG may offer a promising chemotherapeutic strategy.
Keywords: Mitochondria, glycolysis, antioxidants, nitroxides, bioenergetics, breast cancer
INTRODUCTION
Emerging research in cancer chemotherapy is focused on exploiting the biochemical differences between cancer cell and normal cell metabolism (1,2). One of the fundamental changes that occurs in most malignant cancer cells is the shift in energy metabolism from oxidative phosphorylation to aerobic glycolysis to generate ATP (the Warburg effect) (3–5). Several agents that specifically inhibit glycolytic metabolism have been used as effective anticancer agents in cellular systems and in animal models (5,6). However, this approach has yielded fewer positive results in human patients (with the exception of imatinib), most likely due to dose-limiting side effects (e.g., neurotoxicity) (7). One of the most frequently used anti-glycolytic agents is 2-deoxy-D-glucose (R-DG) which is phosphorylated by hexokinase and subsequently inhibits ATP generated via the glycolytic pathway (7,8). However, high concentrations (~20 mM) of 2-DG were typically used to inhibit the glycolytic metabolism in cancer cells (9). 2-DG is undergoing clinical trials for treatment of glioma and its efficacy is limited by the systemic toxicity (10). A recent strategy to “hypersensitize” tumor cells involved the combined use of mitochondrial inhibitors (oligomycin and antimycin) or delocalized cationic compounds with 2-DG (11,12). Dual targeting of mitochondrial and glycolytic pathways was suggested as a promising chemotherapeutic strategy (13,14).
Recent work has revealed that cancer-promoting oncogenes and hypoxia-inducible factor (HIF-1α) also induce a glycolytic shift (15,16). Activation of oncogenic signaling pathways involving PI3K/ Akt/mTOR, c-Myc, Src, and Ras leads to enhanced glucose uptake and high glycolytic activity mimicking the Warburg effect in cancer cells (17,18). Thus, targeting of both mitochondrial bioenergetic function and the glycolysis pathway is an attractive experimental chemotherapeutic strategy. Previously, investigators have used agents (e.g., rhodamine-123, rotenone, antimycin, or oligomycin) that inhibit mitochondrial oxidative phosphorylation in combination with glycolytic inhibitors to eradicate tumor cells (19). In contrast, a similar treatment (rhodamine-123 and 2-DG) failed to elicit cytotoxic effects in normal epithelial cells (20). The rationale for this approach is that compromised oxidative phosphorylation in tumor cells leads to stimulation of glycolytic metabolism for ATP generation. Dichloroacetate (DCA), a pyruvate mimetic that inhibits pyruvate dehydrogenase kinase, shifts cellular metabolism from glycolysis to OXPHOS (21,22). However, DCA was selectively more toxic in cells with defective mitochondrial electron transport chain (22,23). As indicated earlier, mitochondrial targeting of drugs combined with 2-DG or other glycolytic inhibitors may be an extremely effective strategy to eliminate slow growing hypoxic tumor cells present in most solid tumors (12).
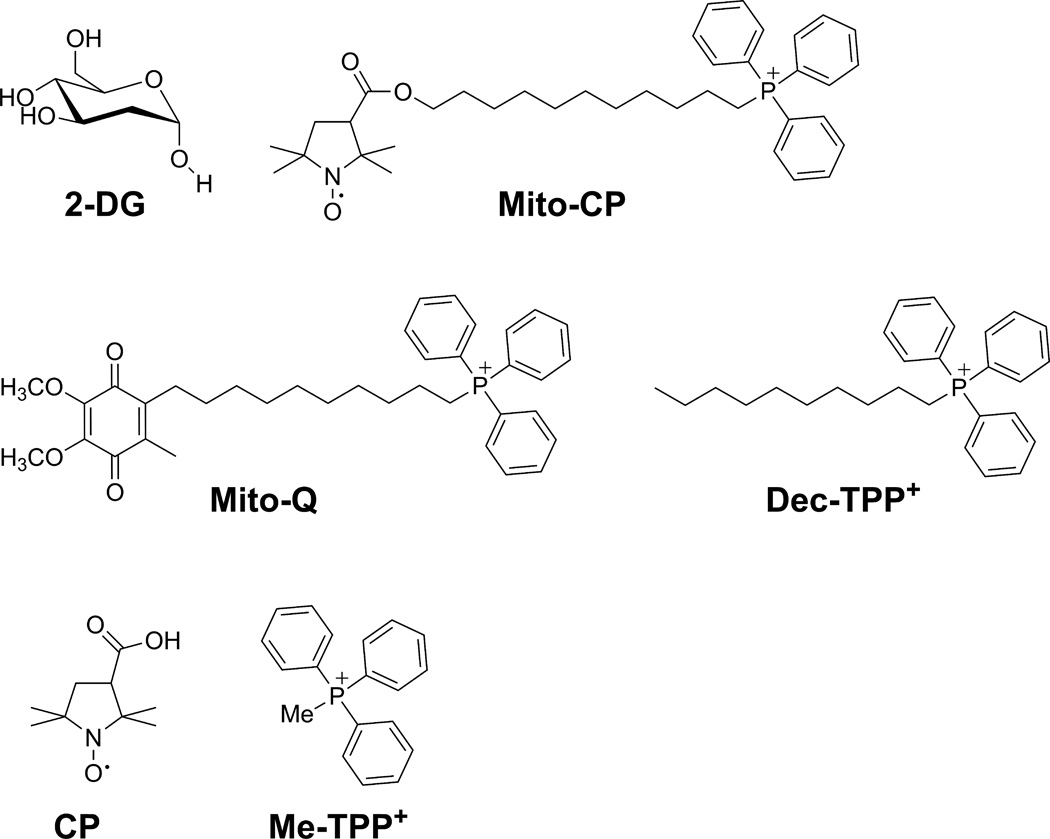
The accumulation of mitochondria-targeted delocalized lipophilic cations such as Mito-CP (Fig. 1) in tumor cells is controlled by several factors including the lipophilicity and the chain length of MTDs, the negative mitochondrial membrane potential, and the levels of p-glycoprotein mediated multidrug resistance (MDR) protein that actively pumps cationic drugs out of the tumor cells (24). Recent research showed that Mito-Q (coenzyme-Q conjugated to an alkyl triphenylphosphonium cation) and Mito-CP (a five-membered nitroxide, CP, conjugated to a TPP+) potently inhibited proliferation of breast cancer cells (MCF-7 and MDA-MB-231) or human colon cancer cells (HCT-116) (25,26). These mitochondria-targeted drugs (MTDs) did not significantly affect normal cell proliferation (25). In related studies, we have shown that the MTDs effectively mitigated the toxic side effects (cardiotoxicity or nephrotoxicity) induced by conventional chemotherapeutics such as doxorubicin or cis-platin (27). These results led us to postulate the following hypothesis: The combined use of MTDs (Mito-CP and Mito-Q) and 2-DG will synergistically enhance cytotoxicity selectively in cancer cells compared to either drug alone. In this study, we investigated the chemotherapeutic effects of 2-DG in combination with Mito-CP, Mito-Q, and other appropriate control compounds. Results from this study indicate that targeting mitochondria with small molecular weight antioxidants conjugated to an alkyl TPP+ and glycolytic inhibitors is a potentially promising and effective cancer treatment strategy.
Figure 1. Structures of 2-deoxy-D-glucose (2-DG), Mito-CP, Mito-Q, Dec-TPP+, Carboxy Proxyl (CP), Me-TPP+.
MATERIALS AND METHODS
Chemicals
Mito-CP and Mito-Q were synthesized as previously published (28,29) (see Fig. 1 for chemical structures). 2-DG, Carboxy-Proxyl (CP), methyl triphenylphosphonium (Me-TPP+), were purchased from Sigma-Aldrich (Milwaukee, WI). D-luciferin sodium salt was obtained from Caliper Life Sciences, Inc. (R-Decyl) triphenylphosphonium bromide (Dec-TPP+) was obtained from Alfa Aesar.
Cell culture
MCF-7, MCF-10A and MDA-MB-231 cells were acquired in the last two years from the American Type Culture Collection, where they are regularly authenticated. Cells were stored in liquid nitrogen and used within six months after thawing. Cell lines were grown at 37°C in 5% CO2. MCF-7 cells were maintained in MEM-α (Invitrogen) containing 10% fetal bovine serum, bovine insulin (10 µg/ml), penicillin (100 U/ml) and streptomycin (100 µg/ml). MCF-10A cells were cultured in DMEM/F12 media (1:1) (Invitrogen) supplemented with 5% horse serum, bovine insulin (10 µg/ml), epidermal growth factor (20 ng/ml), cholera toxin (100 ng/ml), and hydrocortisone (0.5 µg/ml), penicillin (100 U/ml) and streptomycin (100 µg/ml). MDA-MB-231 cells were cultured in DMEM, 10% fetal bovine serum, penicillin (100 U/ml) and streptomycin (100 µg/ml). The MDA-MB-231-luc cell line stably transfected with luciferase was cultured under the same conditions as the MDA-MB-231 cells described above. These cells were a kind gift from Dr. Michael B. Dwinell (Department of Microbiology and Molecular Genetics, Medical College of Wisconsin), and were recently described in detail (30). They are regularly assessed for standard growth characteristics, and tumorigenicity in nude mice.
Extracellular flux assay
The bioenergetic function of MCF-7 and MCF-10A cells in response to Mito-CP or 2-DG was determined using a Seahorse Bioscience XF24 Extracellular Flux Analyzer (Seahorse Bioscience). MCF-7 or MCF-10A cells were seeded in specialized V7 Seahorse tissue culture plates. One hour prior to the start of the experiment, cells were washed and changed to unbuffered assay medium adjusted to pH 7.4, final volume 675 µl (MEM-α for MCF-7, DMEM/F12 for MCF-10A). After establishing the baseline oxygen consumption rate (OCR) and extracellular acidification rate (ECAR), Mito-CP (1 µM) or 2-DG (5 mM) were administered through an automated pneumatic injection port of XF24. The changes in OCR and ECAR were monitored for 4 h. The resulting effects on OCR and ECAR are shown as a percentage of the baseline measurement for each treatment.
To determine the mitochondrial and glycolytic function of MCF-7 and MCF-10A cells in response to Mito-CP, Mito-Q, and 2-DG, we used the bioenergetic function assay previously described with several modifications (31,32). After seeding and treatment as indicated, MCF-7 cells and MCF-10A cells were washed with complete media and either assayed immediately, or returned to a 37°C incubator for 36 or 60 h. The cells were then washed with unbuffered media as described above. Five baseline OCR and ECAR measurements were then taken before injection of oligomycin (1 µg/ml) to inhibit ATP synthase, FCCP (1–3 µM) to uncouple the mitochondria and yield maximal OCR, and antimycin A (10 µM) to prevent mitochondrial oxygen consumption through inhibition of Complex III. From these measurements, indices of mitochondrial function were determined as previously described (31,32).
Intracellular ATP measurements
MCF-7, MCF-10A and MDA-MB-231 cells seeded at 2 × 104 per well in 96-well plates were treated continuously with 2-DG in the presence and absence of 1 µM of the indicated MTDs (Mito-CP or Mito-Q) or appropriate controls for 6 h. Intracellular ATP levels were determined in cell lysates using a luciferase-based assay per manufacturer’s instructions (Sigma Aldrich). Results were normalized to the total protein level in cell lysate measured in each well determined by the Bradford method (Bio-Rad).
Cell death and clonogenic assays
MCF-7 and MCF-10A cells seeded at 2 × 104 per well in 96-well plates were treated with 2-DG in the presence and absence of 1 µM MTDs for 6 h or 24 h, and dead cells were monitored by staining with Sytox Green per the manufacturer’s instructions (Invitrogen). Fluorescence intensities from cells grown in 96-well plate were acquired using a plate reader (Beckman Coulter DTX-880; Beckman-Coulter) equipped with 485 nm excitation and 535 nm emission filters. To measure the total cell number, half of the samples in each treatment group were permeabilized with digitonin (120 µM) when staining with Sytox Green and fluorescence intensities in digitonin-treated cells were taken as 100%. Data are represented as a percentage of dead cells after normalization to total cell number for each group.
For clonogenic assay, MCF-7, MDA-MB-231 and MCF-10A cells were seeded at 300 cells per dish in 6 cm cell culture dishes and treated with 2-DG in the presence and absence of 1 µM MTDs for 6 h. After 7–14 days, the number of colonies formed was counted. The cell survival fractions were calculated according to a published protocol (33).
Xenograft experiments
All protocols were approved by the Medical College of Wisconsin Institutional Animal Care and Use Committee. MDA-MB-231-luc cells (5 × 105 cells in 200 µl of a mixture of 1:1 PBS/Matrigel (BD Biosciences) were injected into the right mammary fat-pad of 8-week-old female SHO mice (Charles Rivers). Tumor establishment and growth were monitored by injecting D-luciferin per manufacturer’s instructions (Caliper Life Sciences) and detecting bioluminescence using the Lumina IVIS-100 In Vivo Imaging System (Xenogen Corp.) (30). The light intensities emitted from regions of interest were expressed as total flux (photons/second).
Two days after injection of cells, the mice were imaged to verify tumor establishment. Mice were then orally gavaged with either water (control), Mito-CP (40 mg/kg), 2-DG (1 g/kg) or a mixture of Mito-CP (40 mg/kg, final concentration) and 2-DG (1 g/kg, final concentration) five times/week (Monday through Friday). This treatment protocol was selected based on recent studies demonstrating that Mito-CP is cleared from plasma of mice within approximately 6 h of injection (34). After 4 weeks of treatment, the mice were sacrificed, and the tumor, kidney, heart and liver were removed and formalin fixed. These tissues were then paraffin embedded and stained with hematoxylin and eosin (H&E).
Statistics
All results are expressed as mean ± SEM. Comparisons among groups of data were made using a one-way ANOVA with Tukey's post hoc analysis. P value of <0.05 was considered to be statistically significant.
RESULTS
Effects of Mito-CP or Mito-Q alone and in combination with 2-DG on bioenergetic function in MCF-7 and MCF-10A cells
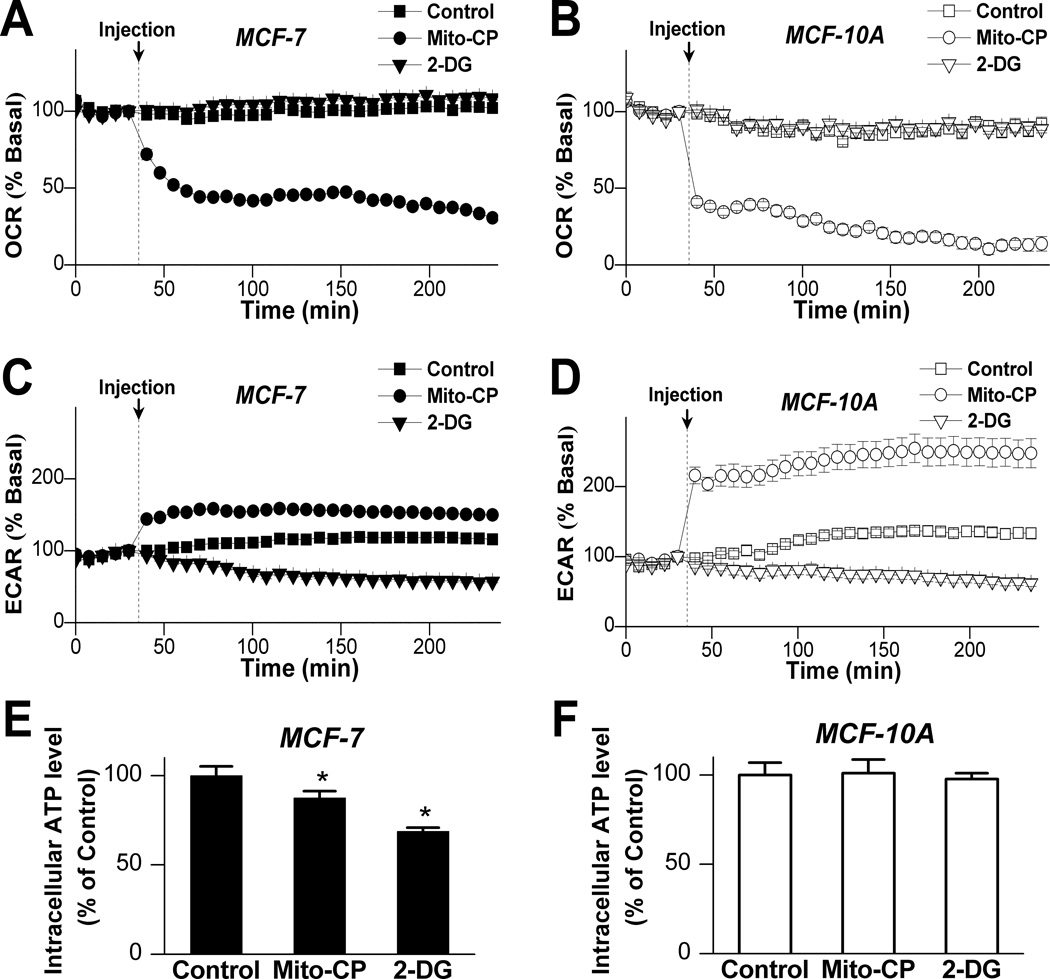
The OCR and ECAR (as a surrogate marker for glycolysis) were measured in a Seahorse Bioscience XF24 extracellular flux analyzer. The bioenergetic profiles obtained under various experimental conditions following Mito-CP and 2-DG treatments were determined according to the procedures outlined previously (31,32). As shown in Figure 2A and B, addition of Mito-CP (1 µM) greatly decreased the OCR in both MCF-7 and MCF-10A cells. Notably, Mito-CP stimulated ECAR levels in both MCF-7 and MCF-10A cells, signaling an increase in glycolysis likely to compensate for the loss of OCR. As expected, 2-DG (5 mM) that inhibits glycolysis decreased the ECAR by 40% (Fig. 2C and D). Under these conditions, individual treatment with either Mito-CP, or 2-DG slightly but significantly decreased the intracellular ATP levels in MCF-7 cells, but not in MCF-10A cells (Fig. 2E and F).
Figure 2. Bioenergetic profile of breast cancer cells (MCF-7) and non-tumorigenic mammary epithelial cells (MCF-10A) treated with Mito-CP or 2-deoxy-D-glucose.
(A–D) MCF-7 or MCF-10A cells were seeded to 30,000 cells/well in specialized V7 Seahorse tissue culture plates. Changes in OCR (A: MCF-7, B: MCF-10A) and ECAR (C: MCF-7, D: MCF-10A) were monitored at 37°C for 4 h. The resulting effects on OCR and ECAR are shown as a percentage of the baseline measurement for each treatment. Data shown are the means ± SEM (n=5 per treatment group). (E,F) MCF-7 and MCF-10A cells were treated with Mito-CP (1 µM) or 2-DG (5 mM) for 6 h. Intracellular ATP levels were monitored using a luciferase-based assay. Data shown are the means ± SEM, n=4 per treatment group. *, P < 0.05 vs. control.
The extent of relative increase in glycolytic activity after treatment with Mito-CP (1 µM) was notably higher in MCF-10A cells as compared to MCF-7 cells. To identify the source of the difference in ECAR stimulation between these cell lines, we next examined the potential for glycolysis stimulation in each cell line. ECAR was measured in MCF-7 cells cultured in media containing 5.5 or 17.5 mM glucose and in MCF-10A cells cultured in media containing 17.5 mM glucose (Supplementary Fig. 1A). After baseline ECAR was established, oligomycin was injected to the indicated final concentration. Because oligomycin inhibits mitochondrial ATP production and results in compensatory increases in glycolysis, the degree to which ECAR is stimulated by oligomycin should correlate with the cellular glycolytic potential. As shown in Supplementary Figure 1A, oligomycin caused a more robust stimulation of ECAR in MCF-10A cells than MCF-7 cells, regardless of the glucose concentration used to culture the MCF-7 cells. To confirm this, and rule out other effects of culture media differences, MCF-7 and MCF-10A cells were seeded as normal into Seahorse Bioscience culture plates. One hour prior to the start of the experiment, the media was changed in all wells to a specialized DMEM-based assay media lacking glucose and FBS. Baseline ECAR was measured, and then glucose was injected to a final concentration of either 5.5 or 17.5 mM to match routine culture conditions for each cell type (Supplementary Fig. 1B). This resulted in a stimulation of ECAR that was not significantly different between cell types or glucose concentrations (Supplementary Fig. 1B). Oligomycin was subsequently injected to a final concentration of 1 µg/ml in all wells, and stimulation of ECAR was monitored. MCF-10A cells had a significantly greater stimulation of ECAR than MCF-7 cells regardless of glucose concentration (Supplementary Fig. 1B and C). Reversal of ECAR stimulation due to both glucose and oligomycin administration was found to be dependent on glycolysis.Lastly, 2-DG was injected to a final concentration of 25 mM in all wells. 2-DG-dependent inhibition indicates that glucose- and oligomycin-stimulated ECAR was reflecting cellular glycolytic activity.
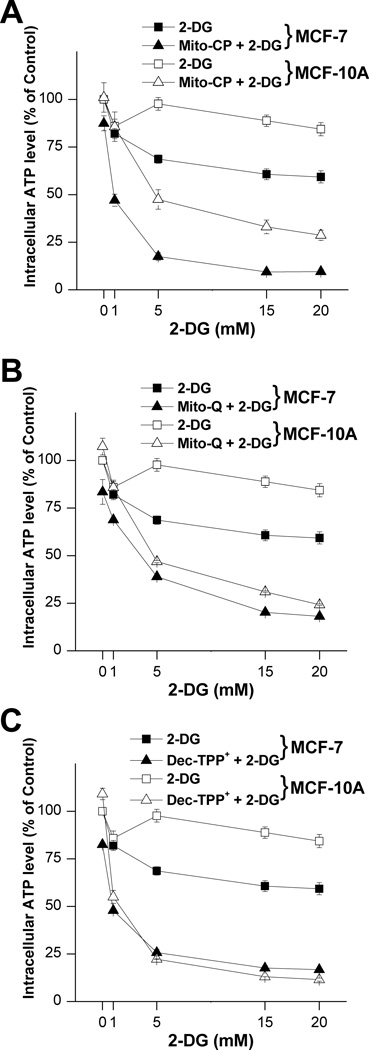
We next measured the intracellular ATP levels in MCF-7 and MCF-10A cells treated with different concentrations of 2-DG in the presence of Mito-CP (1 µM) and other control compounds (CP, TPP+, and Dec-TPP+). As shown in Figure 3A, Mito-CP and 2-DG together decreased the intracellular ATP levels in MCF-7 cells by 20–30% more than in MCF-10A cells. Treatment with Mito-Q or with TPP+ conjugated to a long-chain aliphatic hydrocarbon (Dec-TPP+) and 2-DG enhanced ATP depletion in both cell lines (Fig. 3B and Supplementary Fig. 2). In contrast to Mito-CP, treatment with CP or Me-TPP+ and varying levels of 2-DG did not cause enhanced intracellular ATP depletion (Supplementary Fig. 2A and B). Similar results were observed in another breast cancer cell line, MDA-MB-231 (Supplementary Fig. 3A and B). Notably, the enhancement of ATP depletion is not related to the delocalized cation only, as Me-TPP+ did not sensitize the cells to 2-DG (Supplementary Fig. 2). These results indicate that MTDs (Mito-CP and Mito-Q) with an antioxidant moiety (nitroxide group and Co-Q) conjugated to the TPP+ group via a long aliphatic carbon chain greatly potentiate ATP-depleting activity of 2-DG in MCF-7 cells.
Figure 3. MTDs synergize with 2-DG to decrease intracellular ATP levels in MCF-7 and MCF-10A cells.
(A–C) MCF-7 and MCF-10A cells seeded in 96-well plates were treated with 2-DG in the presence and absence of 1 µM of the indicated MTDs (Mito-CP or Mito-Q) or relevant controls for 6 h. Intracellular ATP levels were monitored using a luciferase-based assay. Data are represented as a percentage of control (non-treated) cells after normalization to total protein for each well. The calculated absolute values of ATP (nmol ATP/µg protein) for MCF-7 and MCF-10A control cells were 20.6±1.9 and 28.0±2.0, respectively. Data shown are the means ± SEM, n=4.
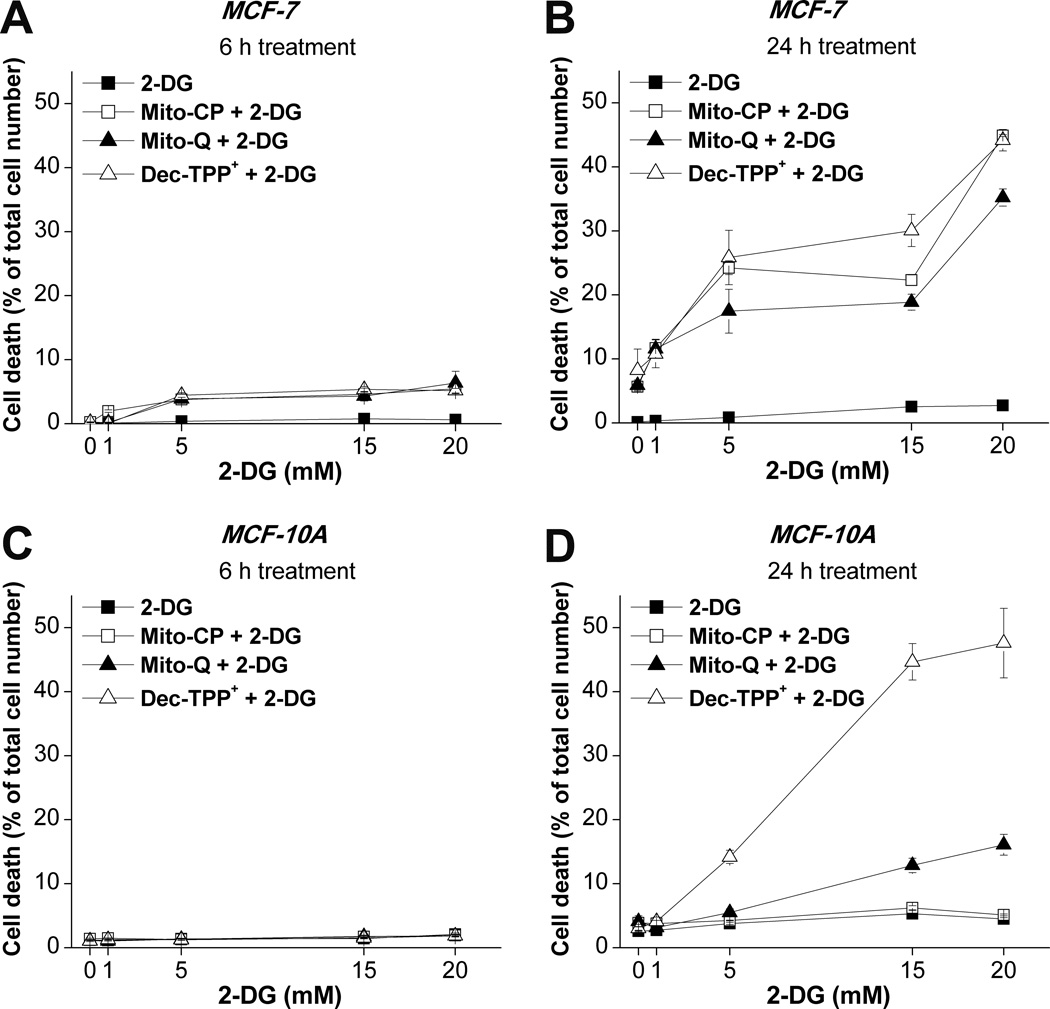
Cytotoxic effects of Mito-CP or Mito-Q in combination with2-DG in MCF-7 and MCF-10A cells
We measured the cytotoxicity after a 6 h and 24 h treatment of MCF-7 and MCF-10A with either Mito-CP (1 µM), Mito-Q (1 µM) or Dec-TPP+ (1 µM) and varying concentrations of 2-DG under the same experimental conditions as in Figure 3. The cytotoxicity data obtained by monitoring Sytox Green dye uptake normalized to the total number of cells and are shown in Figure 4. All three compounds caused a slight increase in 2-DG cytotoxicity in MCF-7 cells after a 6 h treatment (Fig. 4A) that was markedly increased after a 24 h treatment (Fig. 4B). Combined treatment with 2-DG and either Mito-CP or Mito-Q caused a more dramatic increase in cytotoxicity in MCF-7 cells compared to MCF-10A cells (Fig. 4B and D). In contrast, Dec-TPP+ (that was devoid of nitroxide or Co-Q moiety) was equally toxic in MCF-7 and MCF-10A cells in the presence of 2-DG (Fig. 4B and D). Similar trends were observed with regard to cell viability, as measured by the cell’s ability to reduce resazurin to resorufin. There was a modest decrease in cell viability (30–40%) after a 6 h treatment with Mito-CP (1 µM), Mito-Q (1 µM), or Dec-TPP+ (1 µM) with varying levels of 2-DG in MCF-7 or MCF-10A cells (Supplementary Fig. 4A–D). However, after a 24 h treatment, Mito-CP and Mito-Q decreased the viability of MCF-7 cells to a much greater extent as compared to MCF-10A cells (Supplementary Fig. 4B and D). These results are consistent with the cytotoxicity results (Fig. 4). The glucose concentration in the media used for MCF-7 and MCF-10A cells was different (5.56 mM vs. 17.5 mM). Therefore, we tested the effects of 2-DG at different concentrations. Notably, 2-DG (5 and 20 mM) did not significantly affect the colony formation, or cell death in MCF-10A cells (Fig. 4 and 5). Furthermore, we tested the cytotoxicity in MCF-7 cells cultured in media containing 17.5 mM glucose (same as in MCF-10A cells). Notably, combined treatment with 2-DG and Mito-CP for 24 h still caused a more dramatic increase in cytotoxicity in MCF-7 cells compared to MCF-10A cells (Fig. 4B, D and Supplementary Fig.5). In addition, the combined treatment with Mito-CP and 2-DG elicited greater cell death and decreased colony formation in MCF-7 cells, even when 2-DG was used at recommended glucose concentrations in the media for each cell type (5 mM in MCF-7 vs. 20 mM in MCF-10A). Incubation with the untargeted nitroxide CP or Me-TPP+ with different 2-DG levels did not significantly increase cytotoxicity of 2-DG in either cell line even after a 24 h treatment (Supplementary Fig. 6).
Figure 4. The effects of 2-DG in the presence and absence of MTDs on the extent of cell death in MCF-7 and MCF-10A cells.
MCF-7 and MCF-10A cells seeded in 96-well plates were treated with 2-DG in the presence and absence of 1 µM MTDs for 6 h (A,C) or 24 h (B,D), and cell death was monitored by staining with Sytox Green. Data are represented as a percentage of dead cells after normalization to total cell number for each group. Data shown are the means ± SEM, n=5.
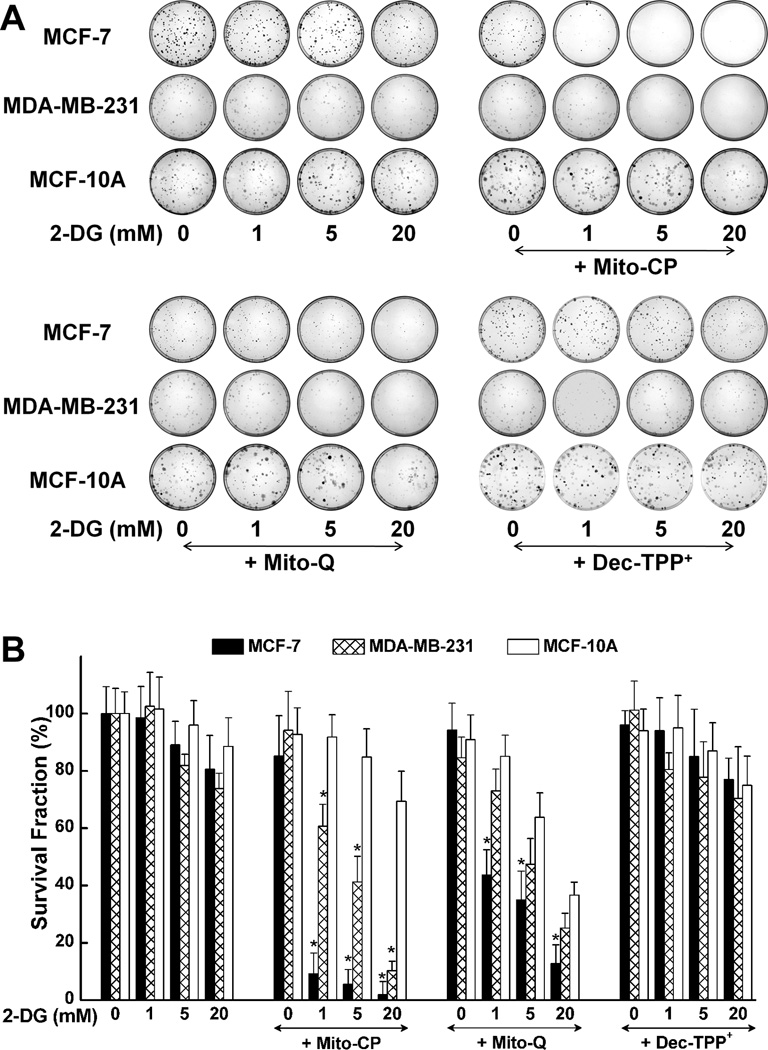
Figure 5. MTDs synergize with 2-DG to inhibit colony formation in MCF-7 and MDA-MB-231 cells but not in MCF-10A cells.
(A) MCF-7, MDA-MB-231 and MCF-10A cells were treated with 2-DG only (top, left), 2-DG in the presence of Mito-CP (1 µM) (top, right), 2-DG in the presence of Mito-Q (1 µM) for 6 h (bottom, left), 2-DG in the presence of Dec-TPP+ (bottom, right) and the number of colonies formed was counted. (B) The survival fraction was calculated under the same conditions as in (A). The calculated plating efficiency for MCF-7, MDA-MB-231 and MCF-10A cells was 55±6, 33±4 and 34±8, respectively. Data shown represent the mean ± SEM. *, P < 0.05 (n = 5) comparing MCF-7 and MDA-MB-231 with MCF-10A under the same treatment conditions.
Effects of Mito-CP, Mito-Q, or Dec-TPP+ and 2-DG on MCF-7, MDA-MB-231 and MCF-10A cell proliferation: Clonogenic analyses
One of the hallmarks of tumor cells is the ability to form colonies (33). As shown in Figure 5, addition of varying levels of 2-DG alone did not significantly decrease the colony formation in MCF-7, MDA-MB-231 or MCF-10A cells. In contrast, there was a decrease in colony formation in MCF-7 cells when treated with 2-DG in the presence of 1 µM Mito-CP or Mito-Q. Mito-CP was more potent than Mito-Q in inhibiting the colony formation (Fig. 5). Figure 5B also shows the survival fractions of MCF-7, MDA-MB-231 and MCF-10A cells calculated from the clonogenic survival assay. Both Mito-CP and Mito-Q more potently decreased the survival fraction in MCF-7 and MDA-MB-231 cells as compared to MCF-10A cells in the presence of 2-DG. Importantly, incubation with the Dec-TPP+ and different 2-DG levels for 6 h did not significantly decrease the survival fraction in either cell line (Fig. 5).
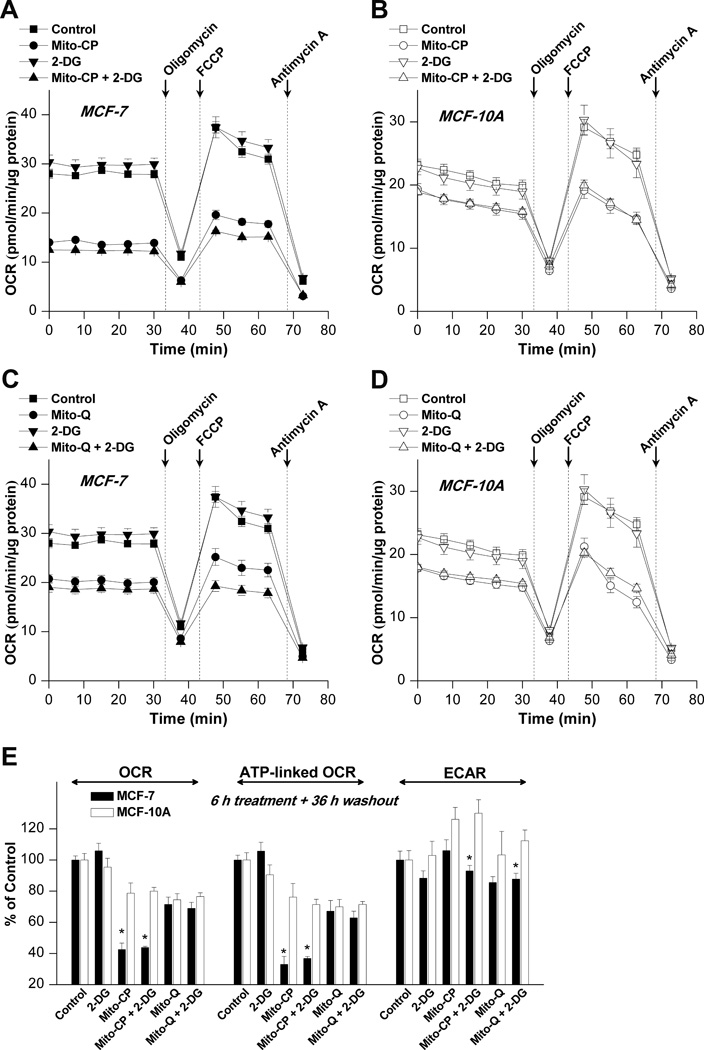
Effects of Mito-CP and Mito-Q alone and in combination with 2-DG on mitochondrial bioenergetic function in MCF-7 and MCF-10A cells
Although treatment with Mito-CP and Mito-Q in the presence of 2-DG dramatically decreased intracellular ATP levels in both MCF-7 and MCF-10A cells, the clonogenic survival analysis showed that this treatment selectively inhibited survival in MCF-7 to a much greater extent than in MCF-10A cells. This suggested that MCF-10A cells were able to recover from the combination treatment (mitochondrial and glycolytic inhibitors) whereas the MCF-7 cells failed to recover under the same conditions. To investigate this process in more detail, we monitored the mitochondrial bioenergetic function in MCF-7 and MCF-10A cells using the XF24 extracellular flux analyzer. The protocol for this experiment is shown in Supplementary Figure 7. As shown, both cell lines were treated with Mito-CP, Mito-Q, and 2-DG for 6 h followed by washout of the treatments, and returned to fresh culture media. After 36 h, OCR was measured and the effects of adding oligomycin, FCCP, and antimycin A were determined (Fig. 6A–D). The use of these metabolic modulators allows determination of multiple parameters of mitochondrial function. Interestingly, the most dramatic effect of Mito-CP was on basal OCR and the OCR linked to ATP production (Fig. 6E). These parameters were calculated from the traces in Fig. 6A–D (31,32). Notably, inhibition of OCR was persistent 36 h after removal of Mito-CP in MCF-7 cells, but not in MCF-10A cells. Mito-Q had a similar effect on mitochondrial function, although the degree of inhibition was markedly lower. The effects of Mito-CP and Mito-Q were also examined immediately after 6 h treatment with these compounds (Supplementary Fig. 8). Consistent with the data shown in Figure 2, after a 6 h exposure to either Mito-CP or Mito-Q, mitochondrial oxygen consumption was decreased. Curiously, the effect of these compounds was more dramatic in MCF-10A cells as compared to MCF-7 cells. Paired with the data in Figure 6, this suggests that MCF-10A cells are more adept at recovering from inhibition of mitochondrial function than MCF-7 cells. These data also show that the effect of 2-DG is not persistent after removal. As shown in Fig. 6E, this inhibition was reversed 36 h after removal of the 2-DG. Additionally, we found that inhibition of OCR persisted up to 60 h after washout of Mito-CP or Mito-Q. As shown in Supplementary Fig. 9, the mitochondrial function was similarly inhibited after 60 h following washout. Inhibition of mitochondrial function was persistent in MCF-7 cells but not in MCF-10A cells. Collectively, these data suggest that the mechanism for selective killing of MCF-7 cells when co-treated with 2-DG and MTDs is through irreversible mitochondrial inhibition.
Figure 6. The effects of 2-DG and MTDs on OCR and ECAR in MCF-7 and MCF-10A cells.
(A–D) MCF-7 and MCF-10A cells (20,000 cells/well) seeded in V7 culture plates were treated with the indicated compounds for 6 h. The cells were then washed with complete media (MEM-α for MCF-7 and DMEM/F12 for MCF-10A) and returned to a 37°C incubator for 36 h. The cells were then washed with unbuffered media as described. Five baseline OCR and ECAR measurements were then taken before injection of oligomycin (1 µg/ml), to inhibit ATP synthase, FCCP (1–3 µM) to uncouple the mitochondria and yield maximal OCR, and antimycin A (10 µM) to inhibit Complex III and mitochondrial oxygen consumption. The effects of MTDs and 2-DG on basal OCR, ATP-linked OCR and ECAR are shown in (E). *, P < 0.01 (n = 5) comparing MCF-7 with MCF-10A under the same treatment conditions.
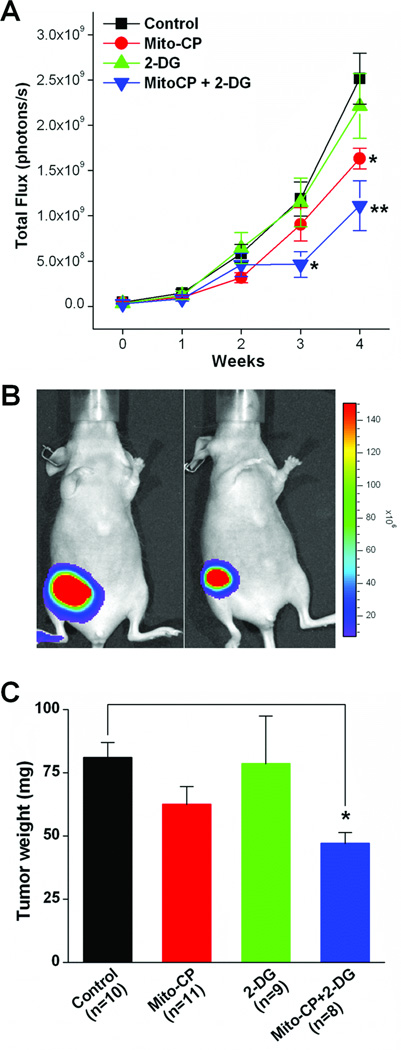
Effects of Mito-CP and 2-DG on tumor growth: Breast cancer xenograft model
We investigated the effects of the combined use of Mito-CP and 2-DG in an in vivo breast tumor model. Administration of 2-DG or Mito-CP alone had little or no effect on the rate of tumor growth in the xenograft mouse model (Fig. 7A). In contrast, the combined treatment of Mito-CP and 2-DG led to a significant decrease in the bioluminescence signal intensity (total flux) as compared to the control mice after 3 and 4 weeks of treatment (Fig. 7A and B). Furthermore, this combined treatment (Mito-CP plus 2-DG) for 4 weeks significantly diminished tumor weight (Fig. 7C) without causing any significant changes in kidney, liver and heart weight or other major morphological changes (as determined by H&E staining in Supplementary Fig. 10 and Table 1.
Figure 7. Combined treatment with Mito-CP and 2-DG inhibits MDA-MB-231-luc tumor xenograft growth.
Tumor growth was monitored weekly for 4 weeks following injection of MDA-MB-231-luc cells into the right mammary fat pad. Luminescence was monitored as described in the Methods and plotted as the light flux in photons/s (A). Representative images are shown in (B). At 4 weeks, tumors were excised. Wet tumor weight was measured, and is plotted in (C). Data shown represent the mean ± SEM (n≥8 per group). *, P < 0.05 and **, P < 0.01 vs. control group.
DISCUSSION
Previous research has shown that mitochondrial targeting of antioxidants could inhibit tumor cell proliferation (25,26). Delocalized phosphonium cations were shown to exert antitumor activity in several tumor cell lines (35,36). For example, it was recently reported that Mito-CP but not CP induced an increase in phosphorylated ERK1/2 in colon cancer cells (25). Furthermore, the selective toxicity of mitochondria-targeted vitamin-E succinate conjugated to TPP+ in tumor cells was attributed to enhanced mitochondrial localization and binding to complex 2 of the mitochondrial respiratory chain (37). In other studies, selective targeting of tumor-specific cellular energy metabolism synergistically exacerbated cytotoxicity in cancer cells treated with antiglycolytic agents or with inhibitors of fatty acid β-oxidation (38). A metabolic shift to glycolysis occurs during anti-angiogenic therapy with drugs (e.g., bevacizumab) that block vascular endothelial growth factor in glioblastoma (39). Upregulation of the PI3K/Akt pathway occurs during anti-angiogenic therapy. Adjuvant therapy with drugs (MTDs/2-DG combination) targeted to glycolytic and mitochondrial metabolism could be beneficial in anti-angiogenic therapy for treatment of brain tumors. 2-DG was shown to potentiate cisplatin-dependent antiproliferative effects in ovarian carcinoma cells expressing low levels of β-F1-ATPase (40). The combined treatment with 2-DG (inhibitor of aerobic glycolysis) also effectively enhanced the efficacy of doxorubicin-induced chemotherapy (41).
Thus, we surmised that mitochondria-targeted antioxidants and nitroxides (SOD mimetics) would preferentially inhibit tumor cell proliferation but not normal cell proliferation. Several recent studies demonstrated increased cancer cell death in the presence of antioxidant compounds, and the mechanism of action of Mito-CP and Mito-Q is presumed to require this antioxidant capability. However, in addition to their antioxidant properties, Mito-CP and Mito-Q might have other unique functions due to the presence of the alkyl chain tethered to the TPP+ group. Our results show that the methyl-triphenylphosphonium cation alone was not sufficient to affect cancer cell proliferation. In contrast, Decyl-TPP+ did increase cell death (Fig. 4), though the specificity for cancer cells was notably lost. The molecular target involved in enhancing the cytotoxic effects of TPP+-substituted compounds in tumor cells is presently unknown, nor do we fully understand the mechanism(s) by which Mito-CP and Mito-Q preferentially inhibit tumor cell proliferation.
The most salient difference between the response of MCF-7 and MCF-10A cells to MitoCP is in the stimulation of glycolysis in response to inhibition of mitochondrial oxygen consumption (Fig. 2). MCF-10A cells have a higher apparent ability to stimulate ECAR, indicating increased glycolytic function in response to Mito-CP. It is likely that this stimulation of glycolysis is better able to support ATP production in MCF-10A cells, as compared to MCF-7 cells (Fig. 2). Maintenance of ATP levels early in the treatment with Mito-CP suggests that the cells are better able to survive co-treatment with 2-DG. This may happen despite a loss of ATP in both cell lines when co-treated with Mito-CP and 2-DG (Fig. 3). It is also worth noting that mitochondrial oxygen consumption and glycolysis both recover more completely in MCF-10A cells as compared to MCF-7 cells (Fig. 6). This resilience likely underpins the preferential cytotoxicity of MitoCP and 2-DG cotreatment in MCF-7 cells both in vitro (Fig. 5) and in vivo (Fig. 7).
MDR-1 or p-glycoprotein, the product of the MDR1 gene, is a multi-drug transporter. Elevated levels of MDR-1 in cancer cells, therefore, antagonize the proapoptotic effects of anticancer drugs, rendering these cells resistant to apoptosis (42). Currently, the affinity of Mito-CP to p-glycoprotein mediated MDR recognition is not known. Previously, it was reported that simple nitroxides (e.g., Tempol) inhibit efflux of p-glycoprotein-mediated MDR-1 substrates suggesting that nitroxides act as competitive inhibitors of MDR-1 p-glycoproteins, thereby abrogating resistance to doxorubicin (43). The present results strongly suggest that 2-DG and Mito-CP (1 µM) synergistically induced cytotoxicity in MCF-7 and MDA-MB-231 cells. Previous EPR results indicate that mitochondrial Mito-CP levels in MCF-7 and MCF-10A cells were nearly identical (44). Several cancer cell lines in the NCI panel of 60 tumor cell lines, including MCF-7 and MDA-MB-231, exhibit only very low levels of p-glycoprotein expression (45). However, chemotherapy (i.e., doxorubicin) could induce multidrug resistance through phenotypic modification leading to elevated p-glycoprotein levels (46). Under these conditions, the intracellular levels Mito-CP could decrease via the pumping mechanism of p-glycoprotein; however, with decreased intracellular ATP caused by Mito-CP and 2-DG, the p-glycoprotein-mediated pump activity is hindered leading to enhanced accumulation of cationic drugs (47). A recent publication suggests that intracellular ATP levels are a key determinant of chemoresistance in colon cancer cells (48). This represents one hypothetical mechanism whereby inhibition of ATP levels by Mito-CP and 2-DG may further synergize with other classical antineoplastic drugs to enhance tumor cell death.
Bioluminescence imaging is one of the most widely used methods to monitor tumor growth and its therapeutic response (49). The substrate, luciferin, is oxidized by luciferase-expressing cancer cells while concomitantly emitting light (50). Thus, the signal intensity generally reflects the number of cancer cells and tumor size. The oxidation of luciferin by luciferase requires ATP as a co-substrate. ATP depletion should lead to diminished bioluminescence from luciferin, independent of the tumor cell number. In this study, the depletion of ATP caused by Mito-CP and 2-DG in cultured MDA-MB-231 cells (Supplementary Fig. 3) was correlated to the decrease of bioluminescence signal induced by the same treatment in MDA-MB-231-luc cells (Supplementary Fig. 11). The decrease in the signal intensity observed in the in vivo experiments may, therefore, be due to inhibition of cell growth or decrease in intracellular ATP levels in the tumor cells or both. The confirmation of the antiproliferative efficiency of MTDs in vivo stems from the tumor weight data, indicating a significantly lower tumor weight in xenograft mice treated with Mito-CP and 2-DG. The possibility of noninvasive monitoring of ATP levels during treatment with MTDs and/or anti-glycolytic agents in the in vivo xenograft breast cancer model is currently underway.
In summary, we report in this study that the combined use of a mitochondria-targeted antioxidant that is relatively nontoxic to normal cells and an anti-glycolytic agent (e.g., 2-DG) synergistically enhanced the cytotoxic potential in breast tumor cells. As has been demonstrated in earlier publications (26,28), an added value of this adjuvant therapy is the potential cytoprotective ability of MTDs (e.g., Mito-CP and Mito-Q) against conventional chemotherapy-induced mitochondrial oxidative damage in normal cells, thereby increasing the overall therapeutic index.
Supplementary Material
Acknowledgments
Financial support: This research was funded by the National Cancer Institute (grant R01 CA152810).
Footnotes
Conflict of Interest Statement: The authors declare that no real or perceived conflict of interest exists related to this study.
Supplementary information is available at the Cancer Research website.
REFERENCES
- 1.Hsu PP, Sabatini DM. Cancer cell metabolism: Warburg and beyond. Cell. 2008;134:703–707. doi: 10.1016/j.cell.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 2.Barger JF, Plas DR. Balancing biosynthesis and bioenergetics: metabolic programs in oncogenesis. Endocr Relat Cancer. 2010;17:R287–R304. doi: 10.1677/ERC-10-0106. [DOI] [PubMed] [Google Scholar]
- 3.Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324:1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gatenby RA, Gillies RJ. Why do cancers have high aerobic glycolysis? Nat Rev Cancer. 2004;4:891–899. doi: 10.1038/nrc1478. [DOI] [PubMed] [Google Scholar]
- 5.deGroof AJ, te Lindert MM, van Dommelen MM, Wu M, Willemse M, Smift AL, et al. Increased OXPHOS activity precedes rise in glycolytic rate in H-RasV12/EIA transformed fibroblasts that develop a Warburg phenotype. Mol Cancer. 2009;8:54. doi: 10.1186/1476-4598-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El Mjiyad N, Caro-Maldonado A, Ramirez-Peinado S, Munoz-Pinedo C. Sugar-free approaches to cancer cell killing. Oncogene. 2011;30:253–264. doi: 10.1038/onc.2010.466. [DOI] [PubMed] [Google Scholar]
- 7.Pelicano H, Martin DS, Xu RH, Huang P. Glycolysis inhibition for anticancer treatment. Oncogene. 2006;25:4633–4646. doi: 10.1038/sj.onc.1209597. [DOI] [PubMed] [Google Scholar]
- 8.Dwarakanath B, Jain V. Targeting glucose metabolism with 2-deoxy-D-glucose for improving cancer therapy. Future Oncol. 2009;5:581–585. doi: 10.2217/fon.09.44. [DOI] [PubMed] [Google Scholar]
- 9.Wu H, Zhu H, Liu DX, Niu TK, Ren X, Patel R, et al. Silencing of elongation factor-2 kinase potentiates the effect of 2-deoxy-D-glucose against human glioma cells through blunting of authophagy. Cancer Res. 2009;69:2453–2460. doi: 10.1158/0008-5472.CAN-08-2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dwarakanath BS, Singh D, Banerji AK, Sarin R, Venkataramana NK, Jalali R, et al. Clinical studies for improving radiotherapy with 2-deoxy-D-glucose: present status and future prospects. J Cancer Res Ther. 2000;5(Suppl 1):S21–S26. doi: 10.4103/0973-1482.55136. [DOI] [PubMed] [Google Scholar]
- 11.Liu H, Hu YP, Savaraj N, Priebe W, Lampidis TJ. Hypersensitization of tumor cells to glycolytic inhibitors. Biochemistry. 2001;40:5542–5547. doi: 10.1021/bi002426w. [DOI] [PubMed] [Google Scholar]
- 12.Kurtoglu M, Lampidis TJ. From delocalized lipophilic cations to hypoxia: Blocking tumor cell mitochondrial function leads to therapeutic gain with glycolytic inhibitors. Mol Nutr Food Res. 2009;53:68–75. doi: 10.1002/mnfr.200700457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lampidis TJ, Bernal SD, Summerhayes IC, Chen LB. Selective toxicity of rhodamine 123 in carcinoma cells in vitro. Cancer Res. 1983;43:716–720. [PubMed] [Google Scholar]
- 14.Pathania D, Millard M, Neamati N. Opportunities in discovery and delivery of anticancer drugs targeting mitochondria and cancer cell metabolism. Adv Drug Deliv Rev. 2009;61:1250–1275. doi: 10.1016/j.addr.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 15.Marin-Hernandez A, Gallardo-Perez JC, Rodriguez-Enriquez S, Encalada R, Moreno-Sanchez R, Saavedra E. Modeling cancer glycolysis. Biochim Biophys Acta. 2011;1807:755–767. doi: 10.1016/j.bbabio.2010.11.006. 2011. [DOI] [PubMed] [Google Scholar]
- 16.Semenza GL. HIF-1 and tumor progression: pathophysiology and therapeutics. Trends Mol Med. 2002;8(4 Suppl):S62–S67. doi: 10.1016/s1471-4914(02)02317-1. [DOI] [PubMed] [Google Scholar]
- 17.Elstrom RL, Bauer DE, Buzzai M, Karnauskas R, Harris MH, Plas DR, et al. Akt stimulates aerobic glycolysis in cancer cells. Cancer Res. 2004;64:3892–3899. doi: 10.1158/0008-5472.CAN-03-2904. [DOI] [PubMed] [Google Scholar]
- 18.Fan Y, Dickman KG, Zong WX. Akt and c-Myc differentially activate cellular metabolic programs and prime cells to bioenergetic inhibition. J Biol Chem. 2010;285:7324–7333. doi: 10.1074/jbc.M109.035584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Jong S, Holtrop M, de Vries H, de Vries EG, Mulder NH. Increased sensitivity of an adriamycin-resistant human small cell lung carcinoma cell line to mitochondrial inhibitors. Biochem Biophys Res Commun. 1992;182:877–885. doi: 10.1016/0006-291x(92)91814-7. [DOI] [PubMed] [Google Scholar]
- 20.Maher JC, Krisha A, Lampidis TJ. Greater cell cycle inhibition and cytotoxicity induced by a 2-deoxy-D-glucose in tumor cells treated under hypoxic vs. aerobic conditions. Cancer Chemother Pharmacol. 2004;53:116–122. doi: 10.1007/s00280-003-0724-7. [DOI] [PubMed] [Google Scholar]
- 21.Michelakis ED, Webster L, Mackey JR. Dichloroacetate (DCA) as a potential metabolic-targeting therapy for cancer. Brit J Cancer. 2008;99:989–994. doi: 10.1038/sj.bjc.6604554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michelakis ED, Sutendar G, Dromparis P, Webster L, Haromy A, Niven E, et al. Metabolic modulation of glioblastoma with dichloroacetate. Sci Transl Med. 2010;2(31):31ra34. doi: 10.1126/scitranslmed.3000677. [DOI] [PubMed] [Google Scholar]
- 23.Stockwin LH, Yu SX, Borgel S, Hancock C, Wolfe TL, Philips LR, et al. Sodium dichloroacetate selectively targets cells with defects in the mitochondrial ETC. Int J Cancer. 2010;127:2510–2519. doi: 10.1002/ijc.25499. [DOI] [PubMed] [Google Scholar]
- 24.Dellinger M, Pressman BC, Calderon-Higgenson S, Savaraj N, Tapiero H, Kolonias D, et al. Structural requirements of simple organic cations for recognition by multi-drug resistant cells. Cancer Res. 1992;52:6385–6389. [PubMed] [Google Scholar]
- 25.Weinberg F, Hamanaka R, Wheaton WW, Weinberg S, Joseph J, Lopez M, et al. Mitochondrial metabolism and ROS generation are essential for Kras-mediated tumorigenecity. Proc Natl Acad Sci USA. 2010;107:8788–8793. doi: 10.1073/pnas.1003428107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rao VA, Klein SR, Bonar SJ, Zielonka J, Mizuno N, Dickey JS, et al. The antioxidant transcription factor Nrf2 negatively regulates autophagy and growth arrest induced by the anticancer redox agent mitoquinone. J Biol Chem. 2010;285:34447–34459. doi: 10.1074/jbc.M110.133579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chandran K, Aggarwal D, Migrino RQ, Joseph J, McAllister D, Konorev EA, et al. Doxorubicin inactivates myocardial cytochrome c oxidase in rats: Cardioprotection by Mito-Q. Biophys J. 2009;96:1388–1398. doi: 10.1016/j.bpj.2008.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dhanasekaran A, Kotamraju S, Karunakaran C, Kalivendi SV, Thomas S, Joseph J, et al. Mitochondria superoxide dismutase mimetic inhibits peroxide-induced oxidative damage and apoptosis: Role of mitochondrial superoxide. Free Radic Biol Med. 2005;39:567–583. doi: 10.1016/j.freeradbiomed.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 29.Dhanasekaran A, Kotamraju S, Kalivendi SV, Matsunaga T, Shang T, Keszler A, et al. Supplementation of endothelial cells with mitochondria-targeted antioxidants inhibit peroxide-induced mitochondrial iron uptake, oxidative damage, and apoptosis. J Biol Chem. 2004;279:37575–37587. doi: 10.1074/jbc.M404003200. [DOI] [PubMed] [Google Scholar]
- 30.Wendt MK, Cooper AN, Dwinell MB. Epigenetic silencing of CXCL12 increases the metastatic potential of mammary carcinoma cells. Oncogene. 2008;27:1461–1471. doi: 10.1038/sj.onc.1210751. [DOI] [PubMed] [Google Scholar]
- 31.Dranka BP, Hill BG, Darley-Usmar VM. Mitochondrial reserve capacity in endothelial cells: The impact of nitric oxide and reactive oxygen species. Free Radic Biol Med. 2010;48:905–914. doi: 10.1016/j.freeradbiomed.2010.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nicholls DG, Darley-Usmar VM, Wu M, Jensen PB, Rogers GW, Ferrick DA. Bioenergetic profile experiment using C2C12 myoblast cells. J Vis Exp. 2010:2511. doi: 10.3791/2511. pii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Franken NA, Rodermond HM, Stap J, Haveman J, van Bree C. Clonogenic assay of cells in vitro. Nat Protoc. 2006;1:2315–2319. doi: 10.1038/nprot.2006.339. [DOI] [PubMed] [Google Scholar]
- 34.Mukhopadhyay P, Horvath B, Zsengeller Z, Zielonka J, Tanchian G, Holovac E, et al. Mitochondrial-targeted antioxidants represent a promising approach for prevention of cisplatin-induced nephropathy. Free Radic Biol Med. 2012;52:497–506. doi: 10.1016/j.freeradbiomed.2011.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manetta A, Gamboa G, Nasseri A, Podnos YD, Emma D, Dorion G, et al. Novel phosphonium salts display in vitro and in vivocytotoxic activity against human ovarian cancer cell lines. Gynecol Oncol. 1996;60:203–212. doi: 10.1006/gyno.1996.0026. [DOI] [PubMed] [Google Scholar]
- 36.Millard M, Pathania D, Shabaik Y, Taheri L, Deng J, Neamati N. Preclinical evaluation of novel triphenylphosphonium salts with broad-spectrum activity. PLos ONE. 2010;5:e13131. doi: 10.1371/journal.pone.0013131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dong LF, Jameson VJ, Tilly D, Cerny J, Mahdavian E, Marin-Hernandez A, et al. Mitochondrial targeting of vitamin E succinate enhances its pro-apoptotic and anti-cancer activity via mitochondrial complex II. J Biol Chem. 2011;286:3717–3728. doi: 10.1074/jbc.M110.186643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hernlund E, Ihrlund LS, Khan O, Ates YO, Linder S, Panaretakis T, et al. Potentiation of chemotherapeutic drugs by energy metabolism inhibitors 2-deoxyglucose and etomoxir. Int J Cancer. 2008;123:476–483. doi: 10.1002/ijc.23525. [DOI] [PubMed] [Google Scholar]
- 39.Keunen O, Johansson M, Oudin A, Sanzey M, Rahim SA, Fack F, et al. Anti-VEGF treatment reduces blood supply and increases cell invasion in glioblastoma. Proc Natl Acad Sci USA. 2011;108:3749–3754. doi: 10.1073/pnas.1014480108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hernlund E, Hjerpe E, Avall-Lundqvist E, Shoshan M. Ovarian carcinoma cells with low levels of beta-F1-ATPase are sensitive to combined platinum and 2-deoxy-D-glucose treatment. Mol Cancer Ther. 2009;8:1916–1923. doi: 10.1158/1535-7163.MCT-09-0179. [DOI] [PubMed] [Google Scholar]
- 41.Maschek G, Savaraj N, Priebe W, Braunschweiger P, Hamilton K, Tidmarsh GF, et al. 2-deoxy-D-glucose increases the efficacy of adriamycin and paclitaxel in human osteosarcoma and non-small cell lung cancersin vivo. Cancer Res. 2004;64:31–34. doi: 10.1158/0008-5472.can-03-3294. [DOI] [PubMed] [Google Scholar]
- 42.Sauna ZE, Smith MM, Muller M, Kerr KM, Ambudkar SV. The mechanism of action of multidrug-resistance-linked P-glycoprotein. J Bioenerg Biomembr. 2001;33:481–491. doi: 10.1023/a:1012875105006. [DOI] [PubMed] [Google Scholar]
- 43.Garibaldi MG, Terni F, Ravizza R, Meschini S, Marra M, Condello M, et al. The nitroxide Tempol modulates anthracycline resistance in breast cancer cells. Free Radic Biol Med. 2006;40:1409–1418. doi: 10.1016/j.freeradbiomed.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 44.Cheng G, Lopez M, Zielonka J, Hauser AD, Joseph J, McAllister D, et al. Mitochondria-targeted nitroxides exacerbate Fluvastatin-mediated cytostatic and cytotoxic effects in breast cancer cells. Cancer Biol Ther. 2011;12:707–717. doi: 10.4161/cbt.12.8.16441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Izquierdo MA, Shoemaker RH, Flens MJ, Scheffer GL, Wu L, Prather TR. Overlapping phenotypes of multidrug resistance among panels of human cancer-cell lines. Int J Cancer. 1996;65:230–237. doi: 10.1002/(SICI)1097-0215(19960117)65:2<230::AID-IJC17>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 46.Shukla S, Ohnuma S, Ambudkar SV. Improving cancer chemotherapy with modulators of ABC drug transporters. Curr Drug Targets. 2011;12:621–630. doi: 10.2174/138945011795378540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mirski SEL, Gerlach JH, Cole SPC. Multidrug resistance in a human small cell lung cancer cell line selected in adriamycin. Cancer Res. 1987;47:2594–2598. [PubMed] [Google Scholar]
- 48.Zhou Y, Tozzi F, Chen J, Fan F, Xia L, Wang J, et al. Intracellular ATP levels are a pivotal determinant of chemoresistance in colon cancer cells. Cancer Res. 2012;72:304–314. doi: 10.1158/0008-5472.CAN-11-1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Negrin RS, Contag CH. In vivo imaging using bioluminescence: a tool for probing graft-versus-host disease. Nat Rev Immunol. 2006;6:484–490. doi: 10.1038/nri1879. [DOI] [PubMed] [Google Scholar]
- 50.Sato A, Klaunberg B, Tolwani R. In vivobioluminescence imaging. Comp Med. 2004;54:631–634. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.