Abstract
Background: Psychiatric disorders frequently co-occur with pathological gambling. The extent to which co-occurence extends to subsyndromal levels of gambling or differs between women and men is incompletely understood. Aim: To examine whether the association between psychiatric disorders and past-year gambling problems is stronger in women than men. Methods: Data from the National Epidemiological Survey of Alcoholism and Related Disorders (NESARC) (n = 43,093) were analyzed. Results: Increasing severity of past-year gambling problems was associated with increasing odds of most past-year Axis I and lifetime Axis II disorders, regardless of gender. Associations between gambling problems and major depression, dysthymia, panic disorder, and nicotine dependence were statistically stronger in women than in men. Conclusions: A severity-related association exists between past-year gambling problems and psychiatric disorders. The stronger associations in women suggest that gambling research, prevention and treatment efforts consider gender differences.
INTRODUCTION
Most people gamble without developing pathological gambling [27]. However, subsyndromal levels of gambling correlate, albeit less strongly than does pathological gambling, with adverse health measures including alcohol and substance abuse/dependence, depression, bankruptcy, and incarceration [6; 22; 28; 35]. These and other data [33] suggest that gambling problems lie along a continuum [28; 33].
Although women generally gamble less frequently and heavily than do men, gambling is associated with poorer measures of mental health, alcohol and substance abuse/dependence in women compared to men [7–9; 21; 22; 24]. Initial analyses of the recently fielded National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [13; 14] found that comorbidity between lifetime pathological gambling and other psychiatric disorders was substantial and significant [20]. These analyses also found that comorbidity between lifetime pathological gambling and several psychiatric disorders, most notably major depression, generalized anxiety disorder, and several substance use disorders, was stronger in women than in men [20]. However, previous analyses have concentrated exclusively on lifetime pathological gambling. With increasing interest in how gambling problems may lie along a continuum, there is a need to explore comorbidity with subsyndromal as well as pathological levels of gambling problems. Prior studies have also focused on lifetime measures of pathological gambling and other psychiatric disorders. It has been argued that past-year measures are not only less subject to recall bias, but also more germane from clinical and public health perspectives [11]. The current study examines the hypotheses that rates of psychiatric disorders increase across levels of past-year gambling problem severity in both women and men, and that these associations are stronger in women than in men.
METHODS
Sample
The NESARC study methodology has been described elsewhere in more detail [10; 14]. Conducted by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the U.S. Census Bureau, the NESARC sampled a nationally representative group of U.S. residents (citizens and non-citizens) age 18 and over living in non-institutionalized settings. Respondents were identified using multi-stage cluster sampling, where Census sampling units, households, and then members of households were sampled in sequence. The sample was enhanced with members of group living environments such as dormitories, group homes, shelters, and facilities for housing workers. Jails, prisons, and hospitals were not included. The study over-sampled Black and Hispanic households and respondents aged 18 to 24 in order to have sufficient statistical power to examine patterns of alcohol use in minority populations and young people, who may have otherwise been under-represented in a simple random sample. Weights have been calculated to adjust standard errors for these over-samples, the cluster sampling technique and non-response [13]. The final sample consisted of 43,093 respondents, representing an 81% response rate. All respondents gave written consent to participate, however the current investigation was exempt from IRB review because it utilized the publicly accessible NESARC data, which was stripped of all personal identifiers.
Measures
Diagnostic data derived from the Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM IV version (AUDADIS-IV) [10], a structured diagnostic assessment administered by trained lay interviewers. The instrument was tested for reliability and validity and found to be a good measure for detecting psychiatric disorders in a community sample [10].
The publicly accessible data from the NESARC contains diagnostic variables that have synthesized self-report data from the AUDADIS-IV into diagnostic categories based upon DSM-IV criteria. The data contain diagnostic variables for major depression, dysthymia, mania, and hypomania, panic disorder with and without agoraphobia, social phobia, simple phobia, generalized anxiety disorder, alcohol abuse, alcohol dependence, drug abuse, drug dependence, nicotine dependence, and pathological gambling [13]. The instrument provides the ability to distinguish past-year diagnoses, prior to past-year diagnoses, and lifetime diagnoses, and includes exclusions for illness and substance-induced symptoms where appropriate. We utilized the past-year diagnoses with illness and substance exclusions, thereby making the diagnoses ‘primary’ or independent diagnoses as defined by the DSM [1]. The use of past-year diagnoses also allows a more precise examination of psychiatric disorder co-occurrence, since symptoms of disorders we are considering to be co-occurring will have been present within one year of each other. This necessarily limits sample sizes, however, the gain of precision in addressing the issue of co-occurrence outweighs the need for larger sample sizes, particularly in a study sample this large.
The instrument also assesses seven Axis II personality disorders: antisocial, avoidant, dependent, histrionic, obsessive-compulsive, paranoid, and schizoid. Not every DSM-IV personality disorder was assessed due to subject burden and time constraints [12]. Since the Axis II disorders were assumed to be temporally stable constructs, no time periods were applied. Respondents were asked about how they felt or acted most of the time, throughout their lives, and regardless of situation. The assessments followed DSM-IV diagnostic criteria. To meet criteria, respondents had to endorse the required number of symptoms as well as report that at least one of the symptoms had caused significant social dysfunction [12].
The primary independent variable of interest in the present analyses was based on the ten diagnostic inclusionary criteria for pathological gambling. Five or more inclusionary symptoms are required for a DSM-IV diagnosis of pathological gambling [1]. Given data that suggest that gambling severity as defined by DSM criteria lies along a spectrum [29; 30; 33], we divided the sample into four groups: non-gamblers and low-frequency gamblers (those who reported that they had never gambled more than 5 times in a single year in their lifetime); low-risk gamblers (those who reported gambling more than 5 times in a year but with no symptoms of pathological gambling in the previous year); at-risk gamblers (those who reported 1 or 2 symptoms of pathological gambling in the previous year); and problem/pathological gamblers (PPG; those who reported 3 or more symptoms of pathological gambling in the previous year). The divisions of low-risk, at-risk, problem and pathological gamblers are identical to those recently used by other investigators in population-based samples of gamblers [9; 33] with the exception that the low frequency of pathological gambling (5 or more symptoms, less than 1% of the sample) necessitated the combination of the problem and pathological groups, a strategy that has been employed in prior gambling studies [5; 29; 30].
Other variables utilized in the analyses include self-reported gender, age in years, race/ethnicity (African-American, Hispanic, and Caucasian), education, current employment, marital status and household income in dollars. Race categories were non-mutually exclusive because respondents could endorse more than one racial category.
Data analyses
The primary research questions concerned gender differences in the association between past-year gambling problems and psychiatric disorders. To investigate, we first examined the association between gender, gambling problems and other socio-demographic variables in order to identify socio-demographic variables potentially influencing the relationship between gender, gambling problems, and psychiatric disorders. Next, we calculated unadjusted weighted rates of psychiatric disorders, stratified by both gender and gambling problems. Finally, we fit a series of logistic regression models where psychiatric and substance abuse variables were the dependent variables of interest and the four-level gambling problem variable, gender, and an interaction between gender and gambling problems were the independent variables of interest, adjusting for previously identified socio-demographic variables.
We also calculated tests for trend to determine whether there was a severity-related relationship between past-year gambling problems and psychiatric disorders. This was done by examining the change in fit between two nested logistic regression models: one where gambling problem severity was entered into the model categorized as outlined above, and another where an additional continuous measure of gambling problem severity was also entered into the model. The comparison of the fit of these two models using a change in log likelihood score and a Chi-square test for significance is a common method for determining if there is significant departure from linear trend.
Due to the design elements of the study sample, and the desire to estimate national rates of co-occurring disorders as accurately as possible, we analyzed data using SUDAAN software [26] and the NESARC-calculated weights.
RESULTS
The survey sample consisted of 18,518 men and 24,575 women. Compared to men, women were older, had lower household incomes, and were more likely to have some college education and less likely to have a college degree, less likely to be currently working, more likely to be previously married, and more likely to be African-American (Table 1). Associations between gambling problems and socio-demographic variables were largely similar across gender (Table 2), with the exception of race: among males, the problem/pathological gambling (PPG) groups were not different with respect to African-American race, while among females there was a strong association. For example, 31% of the female PPG group identified themselves as African-American (Chi-square = 21.37, df = 4, p = 0.0003) compared to 17% of the male PPG group (Chi-square = 6.01, df = 4, p = 0.122). Each tabulated socio-demographic variable was found to distinguish gender and/or gambling groups, and thus all were included in multivariable models.
Table 1.
Socio-demographic characteristics of the NESARC sample, by gender
| Characteristic | Males (n = 18,518) |
Females (n = 24,575) |
χ2 | p | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Education | ||||||
| Less than high school | 3369 | 15.95 | 4480 | 15.37 | 31.11 | < .0001 |
| High school graduate | 5264 | 28.74 | 7283 | 29.86 | ||
| Some college | 5250 | 28.92 | 7413 | 31.26 | ||
| College or higher | 4635 | 26.38 | 5399 | 23.51 | ||
| Employment | ||||||
| Full time | 11601 | 64.87 | 10666 | 43.01 | 155.00 | < .0001 |
| Part time | 1261 | 6.94 | 3002 | 13.75 | ||
| Not working | 5656 | 28.19 | 10907 | 43.24 | ||
| Marital Status | ||||||
| Married | 10398 | 64.41 | 11683 | 59.06 | 141.93 | < .0001 |
| Previously married | 3363 | 11.8 | 7754 | 22.66 | ||
| Never married | 4757 | 23.79 | 5138 | 18.27 | ||
| White race | 14569 | 84.19 | 18220 | 82.37 | 14.97 | 0.0003 |
| Black race | 3200 | 10.68 | 5400 | 12.4 | 19.63 | < .0001 |
| Hispanic ethnicity | 3722 | 12.27 | 4586 | 10.9 | 14.59 | 0.0003 |
| n | mean | n | mean | t | p | |
|
| ||||||
| Age in years | 18518 | 45.45 | 24575 | 47.12 | 91.1 | < .0001 |
| Household annual income ($) | 18518 | 52213 | 24575 | 42793 | 76.14 | < .0001 |
Ns represent actual number of respondents in each category; % indicate weighted percentages
Table 2.
Socio-demographic characteristics of the NESARC sample, by gender and gambling problem severity
| Characteristic | Males
|
χ2 | p | Females
|
χ2 | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non/LF-gamblers2,4 (n = 12,002, 65%) | Low-risk gamblers (n = 5,331, 29%) | At-risk gamblers (n = 536, 3%) | Problem/pathological gamblers (n = 133, 0.7%) | Non/LF-gamblers (n = 18,883, 77%) | Low-risk gamblers (n = 4,633, 19%) | At-risk gamblers (n = 409, 2%) | Problem/pathological gamblers (n = 100, 0.4%) | |||||
| Education | ||||||||||||
| Less than high school | 16.94 | 12.99 | 15.97 | 21.21 | 50.6 | < .0001 | 15.89 | 13.22 | 16.68 | 16.23 | 52.9 | < .0001 |
| High school graduate | 28.09 | 29.69 | 32.79 | 36.29 | 29.01 | 32.29 | 32.16 | 39.58 | ||||
| Some college | 27.62 | 31.86 | 29.70 | 24.51 | 30.65 | 33.44 | 38.54 | 33.78 | ||||
| College or higher | 27.35 | 25.46 | 21.54 | 18.00 | 24.45 | 21.05 | 12.62 | 10.41 | ||||
| Employment | ||||||||||||
| Full time | 65.17 | 64.47 | 65.55 | 62.04 | 3.68 | 0.7193 | 42.23 | 45.35 | 46.01 | 44.13 | 12.5 | 0.0668 |
| Part time | 7.01 | 6.70 | 6.73 | 11.89 | 13.78 | 13.58 | 14.87 | 13.68 | ||||
| Not working | 27.82 | 28.83 | 27.72 | 26.07 | 43.99 | 41.08 | 39.12 | 42.19 | ||||
| Marital Status | ||||||||||||
| Married | 63.80 | 67.92 | 56.35 | 46.23 | 63.09 | < .0001 | 58.95 | 61.75 | 54.81 | 48.77 | 55.1 | < .0001 |
| Previously married | 10.84 | 13.29 | 13.27 | 13.56 | 21.86 | 24.69 | 25.79 | 30.85 | ||||
| Never married | 25.36 | 18.79 | 30.38 | 40.21 | 19.19 | 13.56 | 19.41 | 20.37 | ||||
| White race1 | 83.64 | 85.91 | 84.17 | 70.23 | 17.02 | 0.0016 | 82.12 | 83.99 | 78.93 | 61.3 | 21.5 | 0.0003 |
| Black race | 10.7 | 10.17 | 11.97 | 17.12 | 6.01 | 0.122 | 12.4 | 11.5 | 16.65 | 30.83 | 21.4 | 0.0003 |
| Hispanic ethnicity | 13.97 | 8.78 | 9.34 | 7.36 | 31.47 | < .0001 | 12.1 | 7.05 | 5.55 | 5.5 | 27.4 | < .0001 |
| Age in years3 | 44.42 | 48.12 | 42.51 | 39.5 | 35.21 | < .0001 | 46.59 | 49.36 | 46.41 | 43.35 | 32.5 | < .0001 |
| Household income3 | 50967 | 54111 | 59048 | 47855 | 4.47 | 0.0187 | 42427 | 45301 | 38444 | 32339 | 5.44 | 0.0114 |
Race and ethnicity categories are not mutually exclusive
Numbers in table represent weighted percentages, stratified by gender
Numbers represent weighted mean values, stratified by gender
Non/LF = non or low-frequency gamblers
Baseline rates of psychiatric disorders differed by gender (Table 3). Consistent with data from the National Comorbidity Study, women had higher rates of most affective and anxiety disorders and lower rates of substance use disorders [17]. They were also more likely to meet criteria for avoidant (Chi-square = 18.91, df = 1, p < 0.0001), dependent (Chi-square = 6.9, df = 1, p = 0.01), and paranoid (Chi-square = 16.93, df = 1, p < 0.0001) personality disorder, and less likely to meet criteria for antisocial personality disorder (Chi-square = 122.84, df = 1, p < 0.0001) than were men.
Table 3.
Rates of psychiatric diagnoses in the NRSARC, by gender
| Diagnosis | Males (%) | Females (%) | χ2 | p |
|---|---|---|---|---|
| Major Depression | 4.87 | 9.08 | 108.32 | < .0001 |
| Dysthymia | 1.22 | 2.4 | 44.89 | < .0001 |
| Mania | 1.51 | 1.79 | 4.03 | 0.05 |
| Hypomania | 1.24 | 1.09 | 1.46 | 0.23 |
| Panic Disorder1 | 1.25 | 2.9 | 78.34 | < .0001 |
| Social phobia | 2.11 | 3.34 | 38.62 | < .0001 |
| Simple phobia | 4.56 | 9.5 | 142.08 | < .0001 |
| Generalized anxiety | 1.26 | 2.79 | 60.28 | < .0001 |
| Alcohol ab/dep2 | 12.35 | 4.87 | 154.81 | < .0001 |
| Nicotine dep | 14.15 | 11.48 | 34.53 | < .0001 |
| Drug ab/dep | 2.83 | 1.24 | 52.19 | < .0001 |
|
| ||||
| Personality Disorders: | ||||
| Avoidant | 1.91 | 2.76 | 18.91 | < 0.0001 |
| Dependent | 0.37 | 0.61 | 6.9 | 0.01 |
| Antisocial | 5.53 | 1.89 | 122.84 | < .0001 |
| Obsessive-compulsive | 7.87 | 7.89 | 0.01 | 0.95 |
| Paranoid | 3.83 | 4.95 | 16.93 | < .0001 |
| Schizoid | 3.18 | 3.07 | 0.31 | 0.58 |
| Histrionic | 1.89 | 1.8 | 0.29 | 0.59 |
With or without agoraphobia
ab/dep = abuse or dependence
The unadjusted associations between psychiatric disorders and number of gambling problems reveal several important observations (Table 4). First, higher rates of comorbidity were generally observed, in both men and women, with increasing numbers of gambling problems. Tests for trend were largely significant, indicating a “dose-response” association between increasing gambling problems and the odds of psychiatric comorbidity (statistical tests not shown in table). In addition, gender differences in these trends were identified. For example, the only non-significant trends were among men for depression, dysthymia, and dependent personality disorder, while the same trends were very significant among women (see Figure 1).
Table 4.
Rates of psychiatric diagnoses in the NESARC data, by severity of gambling problems
| Diagnosis | Non/LF-gamblers3 | Low-risk gamblers | At-risk gamblers | Problem/pathological gamblers | χ2 | p |
|---|---|---|---|---|---|---|
| Major Depression | 7.15 | 6.73 | 11.09 | 15.53 | 22.15 | 0.0002 |
| Dysthymia | 1.78 | 1.83 | 2.99 | 5.81 | 10.04 | 0.02 |
| Mania | 1.47 | 2.01 | 3.4 | 8.51 | 22.42 | 0.0002 |
| Hypomania | 1.04 | 1.3 | 3.9 | 2.51 | 15.72 | 0.003 |
| Panic Disorder1 | 2 | 2.17 | 5.98 | 7.12 | 17.9 | 0.001 |
| Social phobia | 2.62 | 3.09 | 4.53 | 9.6 | 14.1 | 0.005 |
| Simple phobia | 6.62 | 8.44 | 12.89 | 21.33 | 41.94 | < .0001 |
| Generalized anxiety | 1.94 | 2.39 | 2.88 | 7.66 | 10.54 | 0.02 |
| Alcohol ab/dep2 | 6.74 | 11.58 | 22.47 | 30.62 | 100.56 | < .0001 |
| Nicotine dep | 10.59 | 17.33 | 28.26 | 43.44 | 115.64 | < .0001 |
| Drug ab/dep | 1.64 | 2.6 | 6.28 | 5.91 | 34.59 | < .0001 |
|
| ||||||
| Personality Disorders: | ||||||
| Avoidant | 2.4 | 2.07 | 4.66 | 9.66 | 18.92 | 0.0008 |
| Dependent | 0.51 | 0.44 | 0.58 | 2.87 | 61.31 | < .0001 |
| Antisocial | 2.83 | 5.27 | 10.31 | 20.67 | 72.64 | < .0001 |
| Obsessive-compulsive | 7.16 | 9.59 | 16.02 | 24.59 | 61.31 | < .0001 |
| Paranoid | 4.06 | 4.82 | 10.05 | 25.88 | 52.47 | < .0001 |
| Schizoid | 2.86 | 3.65 | 5.89 | 15.76 | 30.92 | < .0001 |
| Histrionic | 1.66 | 1.96 | 5.44 | 13.34 | 30.69 | < .0001 |
With or without agoraphobia
ab/dep = abuse or dependence
Non/LF = non or low-frequency gamblers
Fig. 1.
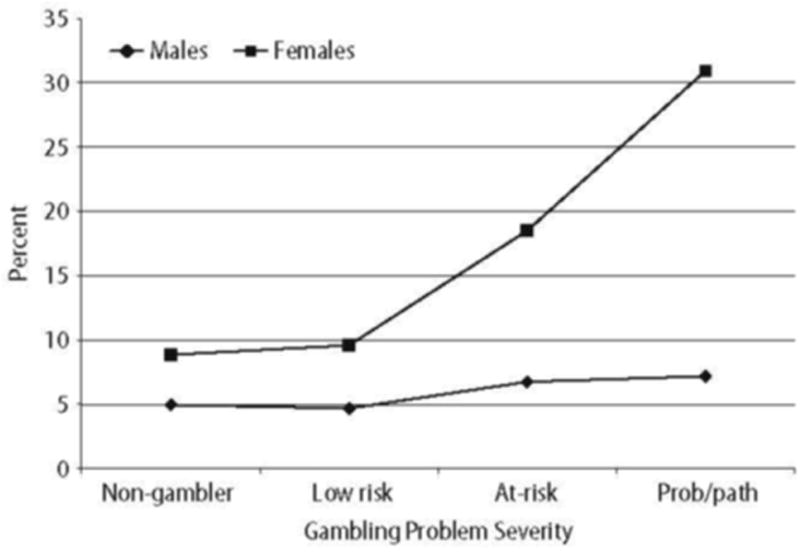
Rates of major depression by gambling problems and gender
The unadjusted rates of disorders stratified by gender and gambling problems highlight multiple important features (Table 5). First, the co-occurrence of gambling problems and several Axis I psychiatric disorders appeared stronger in women. For example, the co-occurrence of gambling problems and major depression, dysthymia, panic disorder, social phobia, and generalized anxiety disorder were statistically significant in women but not in men. Second, other Axis I disorders (mania, hypomania, simple phobia, alcohol abuse/dependence, nicotine dependence, and drug abuse/dependence) appeared to co-occur in a similar and significant pattern with gambling problems in both women and men. Third, Axis II disorders appeared to co-occur at similar rates across gambling problems in both women and men, with significant associations observed for avoidant, anti-social, obsessive-compulsive, paranoid, schizoid and histrionic personality disorders. The only Axis II disorder for which a significant association was not observed, dependent personality disorder, appeared limited by a low response rate, precluding meaningful comparisons. Fourth, the rates of psychiatric disorders follow consistent patterns with respect to gambling symptomatology, with increasing rates observed with increasing gambling severity.
Table 5.
Rates of psychiatric disorders in the NESARC data, by gender and gambling problem severity
| Diagnosis | Males
|
χ2 | p | Females
|
χ2 | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non/LF-gamblers3 | Low-risk gamblers | At-risk gamblers | Problem/pathological gamblers | Non/LF-gamblers3 | Low-risk gamblers | At-risk gamblers | Problem/pathological gamblers | |||||
| Major Depression | 4.96 | 4.68 | 6.75 | 7.18 | 4.59 | 0.21 | 8.85 | 9.59 | 18.5 | 30.92 | 22.7 | 0.002 |
| Dysthymia | 1.17 | 1.26 | 1.18 | 4.19 | 2.3 | 0.52 | 2.25 | 2.62 | 6.07 | 8.80 | 12.9 | 0.008 |
| Mania | 1.32 | 1.80 | 2.84 | 4.68 | 10.1 | 0.02 | 1.59 | 2.3 | 4.35 | 15.56 | 15.2 | 0.003 |
| Hypomania | 1.05 | 1.35 | 4.12 | 3.22 | 10.1 | 0.02 | 1.02 | 1.23 | 3.52 | 1.20 | 7.0 | 0.08 |
| Panic Disorder1 | 1.22 | 1.27 | 2.28 | 3.75 | 3.6 | 0.31 | 2.60 | 3.41 | 12.28 | 13.34 | 20.8 | 0.0004 |
| Social phobia | 1.96 | 2.31 | 3.16 | 10.14 | 7.8 | 0.06 | 3.13 | 4.16 | 6.85 | 8.60 | 11.9 | 0.01 |
| Simple phobia | 4.01 | 5.33 | 8.79 | 19.2 | 26.2 | 0.0001 | 8.64 | 12.76 | 19.88 | 25.27 | 45.4 | < .0001 |
| Generalized anxiety | 1.15 | 1.45 | 2.21 | 3.94 | 4.7 | 0.21 | 2.56 | 3.69 | 4.03 | 14.53 | 14.9 | 0.004 |
| Alcohol ab/dep2 | 9.95 | 15.31 | 27.25 | 36.60 | 72 | < .0001 | 4.25 | 6.41 | 14.31 | 19.60 | 38.1 | < .0001 |
| Nicotine dep | 11.52 | 18.27 | 26.07 | 43.96 | 85 | < .0001 | 9.87 | 16.02 | 31.99 | 42.50 | 81.6 | < .0001 |
| Drug ab/dep | 2.41 | 3.28 | 7.06 | 6.25 | 15.4 | 0.003 | 1.06 | 1.65 | 4.94 | 5.27 | 15.2 | 0.003 |
|
| ||||||||||||
| Personality Disorders: | ||||||||||||
| Avoidant | 1.98 | 1.53 | 4.39 | 7.90 | 11.4 | 0.01 | 2.73 | 2.81 | 5.13 | 12.90 | 9.2 | 0.04 |
| Dependent | 0.37 | 0.33 | 0.46 | 2.03 | 3.30 | 0.35 | 0.61 | 0.57 | 0.78 | 4.41 | 2.6 | 0.46 |
| Antisocial | 4.45 | 7.12 | 12.67 | 25.2 | 44.9 | < .0001 | 1.58 | 2.70 | 6.27 | 12.32 | 30.8 | < .0001 |
| Obsessive-compulsive | 7.04 | 9.35 | 13.85 | 23.42 | 30.5 | < .0001 | 7.25 | 9.91 | 19.72 | 26.74 | 39.9 | < .0001 |
| Paranoid | 3.35 | 4.19 | 7.68 | 28.03 | 30.7 | < .0001 | 4.61 | 5.69 | 14.08 | 21.91 | 25.3 | 0.0001 |
| Schizoid | 2.78 | 3.95 | 3.95 | 15.59 | 14.9 | 0.004 | 2.92 | 3.23 | 9.20 | 16.09 | 21.9 | 0.0003 |
| Histrionic | 1.59 | 1.97 | 5.58 | 15.78 | 23.8 | < .0001 | 1.71 | 1.95 | 5.21 | 8.83 | 9.9 | 0.03 |
With or without agoraphobia
ab/dep = abuse or dependence
Non/LF = non or low-frequency gamblers
Odds ratios from multivariate models investigating the strength of associations between psychiatric disorders and gambling problem groups are presented for each gender, using same-sex low-frequency/non-gamblers as the reference group (Table 6). Interaction term odds ratios tested whether the odds ratios for women are significantly different from those for men. Associations between gambling problems and psychiatric disorders in both women and men were slightly attenuated but continued to be robust after adjusting for potential confounders. The associations among women were generally stronger, and in several cases the differences reached statistical significance across gender groups. For example, in women the association between at-risk gambling and major depression carried an odds ratio of 2.33 (Slatterwaite adjusted F = 22.45, df = 1.63, p < 0.0001) and for PPG the odds ratio was 4.3 (F = 20.72, df = 1.61, p < 0.0001); these odds ratios were 1.8 (F = 5.13, df = 1.5, p = 0.0268) and 3.4 (F = 7.79, df = 1.16, p = 0.0069) times higher than the corresponding ones in men. Similar patterns were seen for dysthymia, panic disorder and nicotine dependence in the at-risk gamblers. In contrast, although the associations between Axis II disorders and gambling were quite strong for both women and men, they did not differ by gender with the exception of schizoid personality disorder, which was more strongly associated with at-risk gambling in women.
Table 6.
Adjusted odds ratios for psychiatric disorders in the NESARC data
| Diagnosis | Males
|
Females
|
Female vs male interactions
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR for Low-risk vs. Non/LF-gamblers1,2 | OR for At-Risk vs Non/LF-gamblers | prob/path vs Non/LF-gamblers | OR for Low-risk vs. Non/LF-gamblers | OR for At-Risk vs Non/LF-gamblers | prob/path vs Non/LF-gamblers | Low-risk gamblers | At-risk gamblers | Prob/path gamblers | ||
| Major Depression | 1.02 | 1.28 | 1.25 | 1.19* | 2.33† | 4.3† | 1.16 | 1.82* | 3.45** | |
| Dysthymia | 1.13 | 0.91* | 3.10 | 1.23 | 2.76† | 3.58* | 1.09 | 3.03* | 1.15 | |
| Mania | 1.60** | 2.11* | 3.02* | 1.71† | 2.70** | 9.59† | 1.06 | 1.28 | 3.13 | |
| Hypomania | 1.55* | 3.72† | 2.41 | 1.49* | 3.62† | 1.02 | 0.96 | 0.97 | 0.42 | |
| Panic Disorder | 1.09 | 1.82* | 2.90* | 1.40* | 5.22† | 5.42** | 1.28 | 2.86** | 1.85 | |
| Social phobia | 1.21 | 1.51 | 5.10† | 1.38** | 2.21** | 2.82* | 1.14 | 1.47 | 0.55 | |
| Simple phobia | 1.38† | 2.23† | 5.37† | 1.59† | 2.59† | 3.41† | 1.15 | 1.16 | 0.64 | |
| Generalized anxiety | 1.32 | 1.80 | 3.12 | 1.52† | 1.56 | 5.82† | 1.15 | 0.87 | 1.85 | |
| Alcohol ab/dep | 1.96† | 3.32† | 1.96† | 1.81† | 4.05† | 5.53† | 0.92 | 1.22 | 1.11 | |
| Nicotine dep | 1.84† | 2.55† | 5.40† | 1.82† | 4.07† | 6.08† | 0.99 | 1.59** | 1.12 | |
| Drug ab/dep | 1.84† | 2.88† | 2.00 | 2.11† | 5.23† | 4.44** | 1.15 | 1.82 | 2.22 | |
|
| ||||||||||
| Personality Disorders: | ||||||||||
| Avoidant | 0.85 | 2.14** | 3.50* | 1.13 | 1.84* | 4.65† | 1.32 | 0.86 | 1.33 | |
| Dependent | 1.06 | 1.14 | 4.30** | 1.10 | 1.21 | 6.12** | 1.03 | 1.06 | 1.43 | |
| Antisocial | 1.93† | 3.03† | 6.34† | 2.00† | 4.06† | 7.41† | 1.03 | 1.33 | 1.16 | |
| Obsessive-compulsive | 1.37† | 2.10† | 4.02† | 1.43† | 3.13† | 4.56† | 1.04 | 1.49 | 1.14 | |
| Paranoid | 1.46** | 2.26† | 9.90† | 1.41† | 3.27† | 4.50† | 0.97 | 1.45 | 0.45 | |
| Schizoid | 1.56† | 1.39 | 5.73† | 1.21 | 3.26† | 5.28† | 0.77 | 2.33* | 0.92 | |
| Histrionic | 1.45* | 3.40† | 9.52† | 1.32 | 3.07† | 4.50† | 0.92 | 0.9 | 0.47 | |
Odds ratios (OR) are adjusted for age, race/ethnicity, marital status, education, employment, and income
Non/LF = non or low-frequency gamblers
p < 0.05
p < 0.01
p < 0.001
DISCUSSION
The present study represents the first to our knowledge to investigate systematically for gender differences in the associations between Axis I and II psychiatric disorders and multiple-threshold levels of past-year gambling problems in a nationally representative sample. The findings largely support our a priori hypotheses that psychiatric disorders would be found in increasing frequency in association with increasing numbers of past-year gambling problems, and that many of these associations would be stronger in women than in men.
Rates of gambling and PPG
We found rates of problem/pathological gambling of 0.7% in men and 0.4% in women. These rates are lower than those previously reported [27] and may in part reflect differences in methodologies used to assess gambling pathology. For example, measures using DSM-IV diagnostic criteria tend to yield lower estimates of PPG than screening instruments (e.g., the South Oaks Gambling Screen) that have been used in multiple prevalence estimate studies of PPG [4]. Estimated rates of psychiatric disorders in general from the NESARC have been lower than those from other national surveys [18], and, although the precise reason for these differences is unknown, different methodologies, diagnostic criteria, or the time periods in which data were collected represent possible contributing factors. The high prevalence of any gambling behavior reported in community samples [9], along with the high proportions of low-risk gamblers (those acknowledging no symptoms of pathological gambling) in the NESARC sample, suggest that most men and women engage in low-frequency gambling without experiencing symptoms of pathological gambling.
Gender and psychopathology
Gender-specific NESARC rates of psychiatric disorders were generally consistent with data from the older National Comorbidity Study (NCS), although the NESARC-derived rates were often lower [18]. For example, rates of past-year major depression in the NCS were 7.7% and 12.9% for males and females, respectively, while they are 4.9% and 9.1% in the NESARC [18]. In general, however, the relative differences between men and women remained similar: women reported higher rates of major depression, dysthymia, and all assessed anxiety disorders, while men reported higher rates of substance abuse and dependence, and the magnitudes of gender differences were consistent across studies.
Gambling and psychopathology
The current findings corroborate those from prior clinical studies that have found high rates of co-occurrence between Axis I psychiatric disorders and PPG among patients in treatment [3]. The findings are also consistent with those from analyses of community data that found higher rates of major depression, schizophrenia, phobias, somatization, alcohol abuse/dependence, and nicotine dependence in problem gamblers compared to non-gamblers [5]. Elevated rates of major depression, simple and social phobias, alcohol abuse/dependence and nicotine dependence in the PPG group were also observed in the present study, while somatization and schizophrenia were not formally assessed. These similarities in findings were observed despite differences in diagnostic criteria (DSM-III vs. DSM-IV), diagnostic instruments (Diagnostic Instrument Schedule vs. AUDADIS-IV), year of study (1980 vs. 2001), the threshold used to define PPG (1 inclusionary criterion in the ECA vs. 3 inclusionary criteria in the NESARC), and geography of the sample (St. Louis vs. national). Given that other relevant differences are also likely to exist (e.g., changes in the US in availability and social acceptability of gambling in the past 20 years), the similarities in findings suggest a robust, temporally stable association between PPG and these disorders.
As in the ECA study [5], we found increasing prevalence of psychiatric disorders as the number of gambling problems increased. These results lend further strength to the suggestion that gambling problems be considered along a continuous spectrum [29; 33]. The most appropriate threshold for defining pathological gambling has been debated [33], with some researchers and clinicians advocating for additional diagnostic categories for gambling pathology for symptomatology not reaching the threshold for pathological gambling [31]. The finding that subsyndromal levels of gambling are associated with significant psychiatric symptoms highlights the importance of subsyndromal behaviors and the need for future research to define the characteristics of subsyndromal groups of gamblers.
Gambling and Axis II disorders
Prior community studies of psychiatric disorders have generally not included both gambling and personality disorder (PD) measures, with the exception of the inclusion of antisocial personality disorder measures in the ECA study [5]. Consistent with ECA findings, the NESARC data revealed a strong association between antisocial PD and PPG that was also significant, although weaker, in subsyndromal gamblers [5]. Studies of clinical samples have also frequently observed antisocial and other PDs in people receiving treatment for pathological gambling [2].
Elevated odds ratios were observed for all seven Axis II disorders when comparing PPG and non/low-frequency gambling groups. This finding is not unexpected given that PDs are frequently observed in people meeting criteria for a range of Axis I disorders [12]. Several potential explanations exist for the co-occurrence of PDs and PPG. First, certain personality traits such as impulsiveness or sensation seeking may predispose to risky or problematic gambling. Second, the presence of a PD may alter decisions to engage or persist in gambling, increasing the risk for more severe gambling problems [2]. Finally, common genetic or biological mechanisms may account for both PPG and PDs [12]. Clinically, the presence of PD may complicate the treatment of Axis I disorders, including PPG [2]. Conversely, high rates of comorbidity in clinical samples suggest that the presence of a PD may increase the likelihood of seeking mental health care [12]. Given both the high comorbidity rates and the relatively low rates of identification and treatment of PPG, it will be important for future research to explore the influence of PDs on both treatment seeking and clinical outcomes for PPG.
Gender, gambling and psychopathology
Our findings related to gender differences in gambling problems are consistent with other community samples that assessed gambling: men are more likely than women to gamble and to develop gambling-related problems [9; 27; 35]. Arguably the most important findings from the present study are the significant differences in the associations between gambling and Axis I psychiatric disorders across gender groups. In all cases in which a statistically significant interaction was observed, associations between gambling and psychopathology were stronger in women than in men. The most substantial differences were observed in the group of at-risk gamblers, those acknowledging one or two symptoms of pathological gambling. In this group, a stronger association was observed in women as compared with men for major depression, dysthymia, panic disorder and nicotine dependence. For each disorder, a positive odds ratio was also observed in the PPG comparison, suggesting a similar relationship across gender groups in the more severely affected group. However, only the variable of major depression reached statistical significance in the comparison testing the relationship across gender groups in the PPG group.
These findings have multiple implications. First, they further highlight the importance of considering subsyndromal groups of gamblers in investigating the potentially differential impact of gambling on men and women. Second, the findings suggest that different levels of gambling problems are associated with different risks in women and men. The finding that at-risk gambling in women is associated with more severe psychiatric symptoms than in men parallels those in the alcohol literature in which women experience more severe health-related problems at similar levels of alcohol consumption than do men [16]. Another gender-related phenomenological similarity between gambling and alcohol use disorders is the telescoping pattern of disease progression in women [32]. More research is needed to investigate further the nature of these gender-related differences, particularly as some of the factors postulated as contributing to these differences in alcohol risk (e.g., distribution and metabolism of alcohol in women as compared to men) do not seem applicable to gambling [16]. Regardless of the etiology, the findings suggest that gender differences be considered when developing guideline recommendations for gambling similar to those that currently exist for alcohol consumption [34].
Third, the stronger associations between at-risk gambling and multiple psychiatric disorders in women raises the possibility that gambling problems might impact the course of specific mood, anxiety and substance use disorders more greatly in women than in men. For example, it is possible that women may be more likely than men to gamble in order to relieve feelings of depression or anxiety, or that problem gambling may exacerbate depressive symptoms more in women than men [19]. The finding of a stronger association between nicotine dependence and gambling symptomatology in women suggests clinically relevant gender differences. Although the extent to which and nature in which gambling and smoking reinforce each other has not been empirically determined, tobacco smoking frequently occurs within gambling venues such as casinos [23]. Women as compared with men gamble more frequently on casino slot machines [22; 32], a form of gambling associated with tobacco use in problem gamblers [23]. The relationship between smoking and specific forms of gambling in multiple venues warrants investigation in a gender-informed fashion.
Fourth, the findings highlight a stronger relationship between depressed mood and gambling pathology in women as compared to men. Comorbidity between PPG and major depression was significantly higher in women, and comorbidity between at-risk gambling and both depression and dysthymia were also significantly higher in women. Disordered gambling and depression have long been linked [3], although the nature of the relationship remains incompletely understood. Some people, particularly women, gamble to escape dysphoria [19], and others become depressed following large gambling losses. A common genetic mechanism underlying the development of both gambling and mood disorders has been reported for men [25], although it is presently unclear if this finding extends to women. More research is needed to identify specific genetic and environmental mechanisms for the co-occurrence of gambling and mood disorders, define the natural histories of symptom progression in each domain, investigate for gender-specific factors, and generate more effective interventions.
Many studies published to date that investigate effective treatments for pathological gambling have excluded individuals with co-occurring mood pathology, limiting the generalizability of the findings. Given that some treatments (e.g., serotonin reuptake inhibitors) have demonstrated efficacy in the treatment of each disorder alone [15], trials of these and other drugs in patients with co-occurring disorders are warranted. Few pathological gambling treatment studies to date have examined gender differences in treatment response, and future studies, particularly of subjects with gambling and co-occurring psychiatric disorders, should incorporate gender considerations.
Several limitations of these data should be acknowledged. First, the cross-sectional nature of the data precludes our ability to identify specific factors that might mediate the identified associations, or to establish temporal patterns between disorders. Disorder-specific analyses of the inter-relationships between socio-demographic variables, gambling problems, and psychopathology may illuminate potential mediating variables. However, longitudinal data will best help to inform these issues. Second, low rates of pathological gambling were reported, necessitating the combination of problem and pathological gambling into a single category. There were also low rates of several other disorders, such as dependent personality disorder, which limit the ability to make meaningful comparisons. Similarly, non-gamblers and low-frequency gamblers were combined in analyses. The NESARC surveyors grouped together low frequency and non-gamblers and thus the available data do not allow for separating these groups. As the present investigation focused on past-year gambling problems as defined by individual DSM-IV inclusionary criteria for pathological gambling, we believe this grouping allows for feasible testing of our hypotheses. Nonetheless, future surveys should consider separating non-gamblers from low-frequency gamblers in order to allow for direct examination of differences related to gambling participation or lack thereof. Some clinically relevant psychiatric measures were lacking in the NESARC, including assessments of both Axis I (e.g., non-gambling impulse control disorders) and Axis II (e.g., borderline PD) disorders. Third, there are no established standards for categorizing gambling problems across a continuum. For example, past-year non- and low frequency gamblers were those who had not gambled more than 5 times in a year in their lifetime. In addition, we divided gambling groups into those with no symptoms, 1 or 2 symptoms, and 3 or more. Although these groupings have been utilized in previous studies, they are not based on empirically derived thresholds.
Conclusions
These data indicate significant associations between past-year gambling problems and psychopathology in both men and women. These data suggest that primary care and outpatient mental health settings actively screen all patients for symptoms of pathological gambling. The significantly stronger associations between mood and anxiety disorders and pathological gambling symptomatology in women as compared with men suggest that women with signs of depression or anxiety be particularly well-screened for pathological gambling. Given the differences between women and men in at-risk gambling and psychiatric disorders, it might be of relatively greater importance to target subsyndromal gambling in women as compared to men. Brief intervention strategies (e.g., motivational interviewing or enhancement techniques) that appear particularly helpful in targeting groups with subsyndromal symptoms might be particularly beneficial. Finally, unidentified gambling symptoms can complicate treatment of non-gambling psychiatric disorders and pathological gambling is common, and often goes unidentified, in patients with serious mental illness. These findings suggest that more intensive screening for pathological gambling symptoms is needed in psychiatric settings, and that intervention studies in multiple psychiatric domains should also assess gambling symptoms.
Acknowledgments
This work was supported by the Veteran’s Administration Hospital Mental Illness Research Education and Clinical Center (MIRECC VISN 1), and Women’s Health Research at Yale.
References
- 1.American Psychiatric Association Committee on Nomenclature and Statistics. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 2000. Text Revision. [Google Scholar]
- 2.Blaszczynski A, Steel Z. Personality disorders among pathological gamblers. J Gambling Stud. 1998;14:51–72. doi: 10.1023/a:1023098525869. [DOI] [PubMed] [Google Scholar]
- 3.Crockford DN, el-Guebaly N. Psychiatric comorbidity in pathological gambling: a critical review. Canadian Journal of Psychiatry – Revue Canadienne de Psychiatrie. 1998;43:43–50. doi: 10.1177/070674379804300104. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham-Williams RM, Cottler LB. The epidemiology of pathological gambling. Semin Clin Neuropsychiatry. 2001;6:155–166. doi: 10.1053/scnp.2001.22919. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham-Williams RM, Cottler LB, Compton WM, Spitznagel EL. Taking chances: Problem gamblers and mental health disorders – results from the St. Louis Epidemiologic Catchment Area Study. Am J Public Health. 1998;88:1093–1096. doi: 10.2105/ajph.88.7.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desai RA, Maciejewski PK, Dausey D, Caldarone BJ, Potenza MN. Health correlates of recreational gambling in older adults. American Journal of Psychiatry. 2004;161:1672–1679. doi: 10.1176/appi.ajp.161.9.1672. [DOI] [PubMed] [Google Scholar]
- 7.Desai RA, Maciejewski PK, Pantalon MV, Potenza MN. Gender differences among recreational gamblers: the association with alcohol use. Psychology of Addictive Behaviors. doi: 10.1037/0893-164X.20.2.145. in press. [DOI] [PubMed] [Google Scholar]
- 8.Desai RA, Maciejewski PK, Pantalon MV, Potenza MN. Gender differences in adolescent gambling: mental health correlates and gambling patterns. Annals of Clin Psychiatry. doi: 10.1080/10401230500295636. in press. [DOI] [PubMed] [Google Scholar]
- 9.Gerstein D, Hoffmann J, Larison C, Engelman L, Murphy S, Palmer A, Chuchro L, Toce M, Johnson R, Buie T, Hill MA. Gambling impact and behavior study. National Opinion Research Center, University of Chicago; 1999. [Google Scholar]
- 10.Grant BF, Dawson DA, Stinson FS, S Chou P, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug & Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 11.Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2005;61:1226–1233. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 12.Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Huang B. Co-occurrence of 12-month mood and anxiety disorders and personality disorders in the US: results from the national epidemiologic survey on alcohol and related conditions. Journal of Psychiatric Research. 2005;39:1–9. doi: 10.1016/j.jpsychires.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Grant BF, Kaplan K, Shepard J, Moore T. Source and Acuracy Statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2003. [Google Scholar]
- 14.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering R, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 15.Grant JE, Kim SW, Potenza MN. Advances in the pharmacological treatment of pathological gambling disorder. J Gambling Stud. 2003;19:85–109. doi: 10.1023/a:1021227214142. [DOI] [PubMed] [Google Scholar]
- 16.Greenfield SF. Women and alcohol use disorders. Harv Rev Psychiatry. 2002;10:76–85. doi: 10.1080/10673220216212. [DOI] [PubMed] [Google Scholar]
- 17.Kendler KS, Prescott CA, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in women and men. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchem H, Kendler JS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 19.Lesieur H, Blume SB. When lady luck loses: Women and compulsive gambling. In: Van Den Bergh N, editor. Feminist perspectives on addictions. Springer; New York: 1991. pp. 181–197. [Google Scholar]
- 20.Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gamblling and psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66:564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- 21.Potenza MN, Maciejewski PK, Desai RA, Caldarone B, Lynch W, Cavus I, Rounsaville BJ, Mazure CM. Characteristics of gamblers: Health measures and gender differences. Drug Alcohol Dependence. 2002;66:S141. [Google Scholar]
- 22.Potenza MN, Maciejewski PK, Mazure CM. A gender-based examination of past-year recreational gamblers. J Gambling Stud. 2006;22:41–64. doi: 10.1007/s10899-005-9002-4. [DOI] [PubMed] [Google Scholar]
- 23.Potenza MN, Steinberg MA, McLaughlin SD, Wu R, Rounsaville BJ, Krishnan-Sarin S, George TP, O‘Malley SS. Characteristics of Tobacco-Using Problem Gamblers Calling a Gambling Helpline. Am J Addictions. 2004;13:471–493. doi: 10.1080/10550490490483044. [DOI] [PubMed] [Google Scholar]
- 24.Potenza MN, Steinberg MA, McLaughlin SD, Wu R, Rounsaville BJ, O’Malley SS. Gender-related differences in the characteristics of problem gamblers using a gambling helpline. Am J Psychiatry. 2001;158:1500–1505. doi: 10.1176/appi.ajp.158.9.1500. [DOI] [PubMed] [Google Scholar]
- 25.Potenza MN, Xian H, Shah K, Scherrer JF, Eisen SA. Shared genetic contributions to pathological gambling and major depression in men. Arch Gen Psychiatry. 2005;62:1015–1021. doi: 10.1001/archpsyc.62.9.1015. [DOI] [PubMed] [Google Scholar]
- 26.Research Triangle Institute. SUDAAN Software. Research Triangle Institute; Research Triangle Park, NC: 2001. [Google Scholar]
- 27.Shaffer HJ, Hall MN. Updating and refining prevalence estimates of disordered gambling behavior in the United States and Canada. Can J Public Health. 2001;92:168–172. doi: 10.1007/BF03404298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shaffer HJ, Korn DA. Gambling and related mental disorders: A public health analysis. Annu Rev Public Health. 2002;23:171–212. doi: 10.1146/annurev.publhealth.23.100901.140532. [DOI] [PubMed] [Google Scholar]
- 29.Slutske WS, Eisen S, True WR, Lyons MJ, Goldberg J, Tsuang M. Common genetic vulnerability for pathological gambling and alcohol dependence in men. Arch Gen Psychiatry. 2000;57:666–674. doi: 10.1001/archpsyc.57.7.666. [DOI] [PubMed] [Google Scholar]
- 30.Slutske WS, Eisen S, Xian H, True WR, Lyons MJ, Goldberg J, Tsuang M. A twin study of the association between pathological gambling and antisocial personality disorder. J Abnorm Psychology. 2001;110:297–308. doi: 10.1037//0021-843x.110.2.297. [DOI] [PubMed] [Google Scholar]
- 31.Stinchfield R. Reliability, validity and classification accuracy of a measure of DSM-IV diagnostic criteria for pathological gambling. Am J Psychiatry. 2003;160:180–182. doi: 10.1176/appi.ajp.160.1.180. [DOI] [PubMed] [Google Scholar]
- 32.Taveres H, Zilberman ML, Beites FJ, Gentil V. Gender differences in gambling progression. J Gambling Stud. 2001;17:151–160. doi: 10.1023/a:1016620513381. [DOI] [PubMed] [Google Scholar]
- 33.Toce-Gerstein M, Gerstein DR, Volberg RA. A hierarchy of gambling disorders in the community. Addiction. 2003;98:1661–1672. doi: 10.1111/j.1360-0443.2003.00545.x. [DOI] [PubMed] [Google Scholar]
- 34.US Department of Agriculture. Discussion of Proposed Changes. 5 2000. for Dietary Guidelines for Americans. [Google Scholar]
- 35.Welte J, Barnes GM, Wieczorek WF, Tidwell M-C, Parker J. Gambling participation in the U.S. – Results from a national survey. J Gambling Stud. 2002;18:313–338. doi: 10.1023/a:1021019915591. [DOI] [PubMed] [Google Scholar]


