Abstract
The joint, longitudinal trajectories of symptoms of disruptive behavior problems and of depression were examined in a community sample drawn from neighborhoods with elevated rates of delinquency. Growth mixture modeling was applied to a 6 year transition period from childhood to adolescence, age 10 to 16 years, to identify latent classes of trajectories for each symptom type. Several classes emerged for the two types of symptoms, namely a group of youth with high levels of disruptive behavior, a group with increasing levels, and a group with low levels, as well as a group with increasing levels of depression, a group with high levels, a group with decreasing levels, and a group with low levels. Within each symptom type, membership in either the high or in the increasing classes was related to a variety of problematic outcomes during emerging adulthood. The co-occurrence of the disruptive behavior and depression classes was then evaluated using parallel process analysis. Youth exhibiting high depressive symptoms were at increased risk for disruptive behavior problems, and youth with increasing disruptive behavior problems were at risk for depressive symptoms. However, only a very small number of youth had both a high depression trajectory and a high disruptive behavior trajectory. Implications of the findings for the design of prevention and treatment programs are discussed.
Keywords: Comorbidity, Disruptive behavior problems, Depression, Emerging adulthood, Longitudinal
Disruptive behavior problems (e.g., aggression, defiance, rule breaking, inattention) and depression problems (e.g., sadness, feelings of worthlessness, loss of interest in things that were once enjoyed, thoughts of suicide) in youth afflict a large number of children and adolescents (Wolff and Ollendick 2006). Youth living in impoverished neighborhoods are particularly vulnerable to the development of behavioral and emotional problems such as these (Leventhal and Brooks-Gunn 2000), but exposure to the various risks that are often associated with such neighborhoods does not always translate into psychopathology or other adjustment problems (Kellam and Rebok 1992; Rutter 1989). However, much of the knowledge about vulnerability was generated through cross sectional investigations, or from studies where data are available at only two points in time. To gain a better understanding of vulnerability, more information is needed about the stability, growth, and continuity of disruptive behavior and depressive symptoms across time. The use of latent growth curve analysis in particular can be an important tool in such understanding, allowing the estimation of the likely membership of youth in problematic classes of disruptive behavior or depressive symptoms, as well as the risk for poor outcomes during young adulthood given such membership.
While independently examining the growth of disruptive behavior and the growth of depression has value, the examination of their joint occurrence seems vital. The co-occurrence of symptoms of disruptive behavior problem and depressive symptoms has been well documented in the literature (Angold et al. 1999; Capaldi 1992; Capaldi and Stoolmiller 1999; Costello et al. 1999). Co-occurrence is a key driver of subsequent adjustment problems in a variety of theoretical models of lifespan development, such as Coercion Theory (Patterson et al. 1992). Knowing more about how symptoms are linked over time, as well as which youth are most at risk for co-occurring problems, may aid in the understanding of untoward developmental outcomes in young adulthood (e.g., drug use, arrest), and lead to more timely prevention and intervention strategies for subgroups of youth. The following sections describe the longitudinal course and co-occurrence of disruptive behavior problems and depression. In addition, the role of gender is discussed in relation to both problem behaviors.
Longitudinal Course of Disruptive Behavior Problems
A number of studies have used person centered analytic techniques to model disruptive behavior over time. Two types of problem behavior trajectories are often found: a “life-course persistent” trajectory, ascribed to youth who chronically display disruptive behavior beginning in early childhood (Moffitt 1993), and a “increasing problems” trajectory, attributed to youth who display a pattern of disruptive behavior that increases from school entry through adolescence (Moffitt and Caspi 2001). For instance, Schaeffer and colleagues (2006) identified distinct disruptive behavior trajectories among a community sample of at risk youth, including an early-starter pathway, an increasing disruptive behavior group, as well as a group with low levels of disruptive behavior across development. Youth with problem trajectories of disruptive behavior are at increased risk for conduct disorder, antisocial personality disorder, and police arrest (Schaeffer et al. 2006, 2003). This is particularly true for boys. Problematic outcomes such as substance abuse and internalizing problems also tend to be associated with disruptive behavior problems in youth (Zoccolillo 1992; Zoccolillo et al. 1997). Unfortunately, many of the studies evaluating disruptive behavior trajectories are limited to the early childhood or elementary school age groups (Cote et al. 2001; Schaeffer et al. 2006, 2003). Evaluations of trajectories for disruptive behavior from late childhood to early adolescence and associated emerging adulthood outcomes are needed.
Longitudinal Course of Depressive Symptoms
Studies examining longitudinal trends in symptoms of depression have often reported increases from late childhood to early adolescence (Angold et al. 2002; Ge et al. 2001; Twenge and Nolen-Hoeksema 2002). This is particularly true for girls. Several studies have utilized growth mixture modeling to determine individual trajectories during early adolescence (Dekker et al. 2007; Stoolmiller et al. 2005). For example, Brendgen and colleagues (2005) identified four distinct longitudinal trajectories of depressive symptoms in a sample of youth age 11 to 14 years. The trajectories included a group with low levels of depressive symptoms, a group with moderate levels, a group with high levels, and group with increasing levels. Similarly, Stoolmiller and colleagues (2005) identified four groups among a high risk sample of men age 15 to 24 years of age. However, they found a moderately depressed group and a high decreasing group, instead of a high group and an increasing group. Dekker and colleagues (2007) investigated the trajectories of depressive symptoms and gender differences in large community sample of children age 4 to 18 years using maternal report of depression and found six distinct trajectories for both boys and girls. Both boys and girls had trajectories of increasing symptoms. However, only boys were found to have decreasing trajectories. Additional research on developmental trajectories in late-childhood and early adolescence using self-reports of depressive symptoms is needed to clarify the number and the type of trajectories during this developmental period. Distal outcomes for youth with depressive symptoms include Major Depressive Disorder (Costello et al. 2006) and substance abuse (Sihvola et al. 2008). For instance, a prospective study of early adolescent twins revealed that depressive symptoms at age 14 significantly predicted substance abuse 3 years later (Sihvola, et al. 2008). Further, there is some evidence that depressive symptoms may actually reduce the risks of arrest in youth (Hirschfield et al. 2006). Thus, studies are needed that examine multiple possible outcomes such as substance abuse, arrest, and mental health problems, and how they relate to developmental trajectories.
Co-occurring Problems
Understanding how specific symptom clusters develop over time is important, but studies on the comorbidity of disruptive behavior problems and depression suggest that, in general, each is associated with increased risk for the other (Angold and Costello 1993). The overlap of disruptive behavior problems and depressive symptoms may occur because one set of etiological factors places an individual at risk for at least some of the symptoms or consequences of symptoms (but not necessarily all) in the other set. The National Comorbidity Survey Replication study found that conduct disorder preceded depression in 72 % of cases, and that youth with active or remitted conduct disorder were significantly more likely to develop depression later in life (Nock et al. 2006). Progression of disruptive behavior problems to depression has been hypothesized to be related to a series of developmental failures associated with early disruptive behavior problems (Capaldi and Stoolmiller 1999; Patterson et al. 1992). According to this “cascade” model, an aspect of the aforementioned Coercion Theory, early behavior problems contribute to parent, teacher, and peer rejection, as well as to school failure. This series of misfortunes affects youth social development (Kellam and Rebok 1992), contributes to deviant peer affiliations and negative attitudes, and ultimately leads to the development of depressed mood (Patterson and Stoolmiller 1991). On the other hand, Kovacs and colleagues (1988) found that in comorbid cases, depression was more often diagnosed before conduct disorder. In fact, as implied by the Hirschfield et al. (2006) findings, depression appeared to hold off disruptive behavior problems in these youth and protected them against the development of conduct disorder.
More recently, Chen and Simons-Morton (2009) evaluated the co-occurrence of disruptive behavior problems and depressive symptoms using a person-centered approach in a large community sample of adolescent boys and girls. Across a 3 year period, four developmental trajectories were identified for disruptive behavior problems and for depressive symptoms for both boys and girls. The probability of youth exhibiting both high levels of disruptive behavior problems and high levels of depressive symptoms ranged from 1 % to 2 % of the sample. This study indicated that few youth experienced co-occurrence of the problems during the study time period. Although this study had many design advantages over prior investigations, the study period was relatively brief. Studies of comorbidity, and outcomes related to such, are needed across longer periods of development.
Gender
Past research has found that boys were more likely to exhibit higher levels of disruptive behavior problems than girls (Loeber and Keenan 1994; Loeber et al. 1994), and that girls tend to have slightly higher levels of depressive symptoms (Wade et al. 2002). Gender differences have also emerged in studies investigating trajectories of disruptive behavior and of depressive symptoms. For instance, in one study, in addition to a high chronic subclass of disruptive behavior problems, boys were found to have an increasing disruptive behavior subclass, whereas, girls displayed a low-moderate disruptive behavior subgroup (Schaeffer et al. 2006). Whereas, Dekker and colleagues (2007) found differences in both the shape and the timing of depressive symptom trajectories among boys and girls. However, when examining the co-occurrence of trajectories, Chen and Simons-Morton (2009) found no gender differences with regard to disruptive behavior problems increasing risk for depression, but they did find that depressed boys had the highest risk of experiencing co-occurring conduct problems. Another study found that girls with serious disruptive behavior problems are at risk for later depression (Kendler et al. 2002). Gender appears to be an important factor to consider in the investigation of the trajectories of disruptive behavior, depression, and their co-occurrence. Additional studies are needed that examine the associations between gender, developmental trajectories and distal outcomes.
Purpose of This Study
In this longitudinal study, we examined the developmental trajectories of disruptive behavior problems and depressive symptoms among a community sample of youth from neighborhoods with elevated rates of juvenile delinquency. First, we used a person-centered approach to identify developmental trajectories of these two types of problems, and examined outcomes for youth with these trajectories during the period of “emerging adulthood”, which is hypothesized to span the period from late adolescence into the mid-20’ (Arnett 2000). According to life-course social field theories, a category that subsumes Coercion Theory, failure to adapt to important social demands can set the stage for additional problems during emerging adulthood, which in turn may lead to problems later in life (e.g., Kellam and Rebok 1992). Thus, understanding how problem classes of disruptive behavior and depressive symptoms in early adolescence impact behavioral and mental health outcomes during emerging adulthood has important implications for prevention and intervention efforts. Additionally, we identified the probability of co-occurring developmental trajectories within the sample.
We were interested in determining the growth trajectories for disruptive behavior problems and depressive symptoms during adolescence and related outcomes during emerging adulthood. Growth mixture modeling (GMM; Muthén 2004) was used to identify trajectory groups of disruptive behavior problems and depressive symptoms in an at risk community sample of early adolescents. GMM allows within-group heterogeneity such that individuals are not restricted to sharing the exact same pathway in a trajectory group. We hypothesized that, similar to prior research, an early starter and increasing disruptive behavior class would emerge. Based on past research we also expected at least four classes of depressive trajectories to emerge, including an increasing class, a class with high depressive symptoms, and a decreasing symptoms class. We expected that boys would be more likely to be in the high disruptive behavior class and the decreasing depressive symptom class, whereas, we hypothesized that girls would be more likely to be in the high and increasing depressive symptoms class. Youth with high levels of disruptive behavior or depressive symptoms during adolescence were expected to be more likely to have negative outcomes associated with emerging adulthood than youth with low levels.
In addition, we were interested in the developmental co-occurrence of disruptive behavior and depressive symptoms. We hypothesized that (a) a small portion of adolescents who exhibited high levels of disruptive behavior problems would also exhibit high levels of depressive symptoms, (b) a small portion with high levels in one domain would have low levels in the other, and (c) the majority of individuals would have low levels of both disruptive behavior problems and depressive symptoms over time. Finally, we were interested in whether youth in co-occurring classes would experience more negative outcomes in emerging adulthood.
Method
Participants
Participants (N=361) were the entire fifth grade cohort from a population-based randomized controlled trial on the prevention of childhood conduct problems (Linking the Interest of Families and Teachers [LIFT]; Eddy et al. 2000; Reid et al. 1999). The full LIFT sample of 671 children and their families was recruited from the population of first and fifth grade youth attending public elementary schools located in at risk neighborhoods in a moderate-size metropolitan area in the Pacific Northwest in the early 1990’s. Neighborhoods were designated “at risk” based on high rates of police contact regarding youth delinquency, relative to local area norms (i.e., the top 50 % of neighborhoods in terms of households with such contact). The 12 participating schools were randomly assigned to either a services as usual control condition or a school-based multimodal preventive intervention condition, and then to either have the first or the fifth grade classes in the school participate. All the students and their families in all such classes were then invited to be in the study, so no individual selection criteria (e.g., current levels of disruptive behavior or depression) were used to build the sample. The preventive intervention, which was delivered over a period of 10 consecutive weeks, included group based parent management training (Reid et al. 2002), child social and problem-solving skills training (Taylor et al. 1999), a version of the Good Behavior Game (Barrish et al. 1969; Stoolmiller et al. 2000) for the school playground, and parent–teacher communication aids. Full-time students and their families in the selected grade in each school were eligible for the study; 85 % of families participated fully, and 3 % participated in the child intervention only. Of youth participants, 51 % were female, 85 % were European American, 4 % Asian American, 4 % Latino American, 3 % Native American, 1 % African American, 2 % other, and 1 % did not report race or ethnicity. These percentages reflected the local population. Approximately 25 % of the families received some type of financial assistance. Further details about the randomized design, participant eligibility, and recruitment are described elsewhere (Eddy et al. 2003; Reid, et al. 1999).
Measures
Mother-reported disruptive behavior problems and youth-reported depressive symptoms were used to define trajectory groups. Assessments were conducted in the fall of fifth grade, the spring of fifth grade, and the spring of sixth, seventh, eighth, and tenth grades (ages 10 to 16 years). Some participants at the “fifth grade” assessment points were actually in the fourth grade, because some schools had fourth and fifth grade combined classes (see Eddy et al. 2003).
Disruptive Behavior Problems
Disruptive behavior problems were assessed using mother report on the Child Behavior Checklist (CBCL; Achenbach 1991). The CBCL is a 113-item informant-report measure for children ages 6 to 18 that has two broadband scales, Internalizing and Externalizing, and a number of more specific subscales (e.g., Attention Problems, Anxious/Depressed). Behavioral descriptors (e.g., “doesn't seem to feel guilty after misbehaving”) are rated by parents across three anchors (0=not true, 1=somewhat true, 2=very true), which are then summed to compute scores on each factor-analytically derived subscale. Scores are then indexed to national norms. For this study, we used the total score of maternal reports of the broadband Externalizing factor as a general measure of disruptive behavior problems. This factor comprises aggressive, oppositional, and delinquent behaviors, as well as inattentive, hyperactive, and impulsive behaviors. Psychometric properties of the CBCL are well established (see Achenbach 1991). Cronbach’s alpha internal reliability coefficients at the various time points were similar to those in the original normative sample (i.e., 0.80 to 0.90).
Depressive Symptoms
Symptoms of depression were assessed using the Child Depression Inventory (CDI; Kovacs 1992). The CDI is a 27-item self-rated assessment of depressive symptoms for children age 5–17. For each item the child has three possible answers: 0=absence of symptoms, 1=mild symptoms, and 2=definite symptoms. The CDI assesses important constructs for explanatory and predictive uses in terms of characterizing symptoms of depression in children and adolescents. The total score on the CDI was used to measure growth of depressive symptoms over time in this study. In past studies, internal reliability has been found to be good, with coefficients usually ranging from 0.71 to 0.89. Reliabilities at the various times points were similar in this sample.
Outcome Measures
To test the association between the identified disruptive behavior and depression trajectory classes and between the classes and outcomes during the emerging adulthood period (here, age 18 to 23 years), the following measures were used: youth report of depressive symptoms and conduct problems at age 18, police arrests (i.e., detained as a juvenile, arrested as an adult), alcohol problems, and drug problems, and diagnosis of antisocial personality disorder (ASPD) and major depressive disorder (MDD) made through standardized interviewing procedures. Youth report of depressive symptoms and conduct problems at age 18 were dichotomized to indicate if youth were in the subclinical or clinical range on distal outcomes. Although dichotomizing variables has become a controversial strategy in recent years, it has been found to be particularly useful for facilitating a comparison of risk across multiple factors because it allows the computation of meaningful measures of strength of relationship (e.g., odds ratios) that are easily understood by a wide audience (Farrington and Loeber 2000). Thus, we employ it here.
Emerging Adulthood Disruptive Behavior
Youth report of disruptive behavior problems during emerging adulthood was assessed using the Youth Self-Report (YSR; Achenbach 1991). The YSR is a 112-item measure that provides self-ratings for 20 competence and problem items paralleling those of the CBCL. Youths rate themselves for how true each item is now or was within the past 6 months, across three anchors (0=not true, 1=somewhat true, 2=very true), which are summed for each factor-analytically derived subscale. Psychometric properties of the YSR are well established (see Achenbach 1991). For the purposes of the outcome analyses, we used the broadband Externalizing scale. Internal reliability of this scale was acceptable (i.e., greater than 0.90) in this sample. We defined elevated externalizing symptoms as a t-score of 60 or higher because it is the cutoff used by the developer of the instrument (see Achenbach 1991). Therefore, for the purposes of this analysis we recoded the scale into a dichotomous variable, with youth in the subclinical and clinical range (t-score higher than 60) coded as 1 and all others coded as 0.
Emerging Adulthood Depression
Youth report of depressive symptoms during emerging adulthood was assessed using the Brief Symptom Inventory (BSI; Derogatis 1975). The BSI is a 53-item self-report symptom inventory designed to reflect current psychological symptom status for individuals age 13 years and older. Each item is rated on a 5-point Likert-type scale (i.e., 0 to 4) ranging from not at all to extremely. The items define a broad spectrum of perceived restrictions relative to physical and psychological symptoms occurring in the preceding 7-day period. Symptoms are assigned to nine subscales, which represent domains of psychopathology (e.g., Anxiety, Depression, Somatization). The Depression subscale was used for analysis. Internal consistency estimates for the Depression subscale is 0.85, similar to the reliability of the subscale in this sample. Correlations between subscale scores and those of the clinical scales of the Minnesota Multiphasic Personality Inventory (MMPI) and the Wiggins content scales of the MMPI range from r=0.46 to 0.72 for depression. We defined elevated depressive symptoms by a cutoff score of t≥60. This cutoff was used by the developer of the instrument and in previous reports to identify significant psychiatric symptoms. Therefore, for the purposes of this analysis the measure was recoded as a dichotomous variable, with youth in the subclinical and clinical range (t score higher than 60) coded as 1 and all others coded as 0.
Substance Use
Report of alcohol use was assessed using the Michigan Alcoholism Screening Test (MAST; Selzer 1971), a brief self-report questionnaire designed to detect problem drinking. It is widely used in clinical and research settings. The 24 items are used to assess symptoms and consequences of alcohol abuse, such as guilt about drinking; blackouts; loss of control; family, social, employment, and legal problems following drinking bouts; and help-seeking behaviors because of drinking. Individuals answer yes or no to each item. The items are weighted on a scale of 1 to 5, with items concerning prior alcohol-related treatment experiences and help-seeking behaviors receiving higher weights. The total score is derived by adding the weighted scores from all items that are endorsed. Studies indicate that the MAST possesses good internal reliability (generally from 0.80 to 0.90; Gibbs 1983). A similar value was found for this sample. For the purposes of this analysis we recoded the scale as a dichotomous variable, with individuals scored as having early to middle problems or established problems with drinking coded as 1 and nondrinkers or no problems with drinking coded as 0. Youth report of drug use was assessed using the Drug Abuse Screening Test (DAST; Skinner 1982). The DAST, a 28-item scale modeled on the MAST, classifies individuals on a continuum from low to high drug problem severity, has good internal consistency, and can differentiate drug abusers from alcohol abusers (Gavin et al. 1989). The reliability of the scale in this sample was acceptable. As with the MAST scores, the measure was recoded as a dichotomous variable to indicate individuals with problems with drugs coded as 1 and with no problems with drugs coded as 0.
Police Arrests
Court data about police arrests were obtained yearly from the county or appropriate jurisdiction in which a youth was currently residing. Juvenile arrests were dichotomized for analysis: 1 indicated the youth had one or more arrests before age 18, and 0 indicated no arrests before age 18. Adult arrests were also dichotomized, with 1 indicating one or more arrests between age 18 and 21 years and 0 indicating no arrests during this period.
Diagnostic Interview Schedule (DIS-IV)
The DIS-IV is a clinical interview designed to assess the presence or absence of major psychiatric disorders as outlined in the Diagnostic and Statistical Manual of Mental Disorders (American Psychological Association 1994). Psychometric properties of the DIS-IV have been studied extensively, including test–retest reliability studies, test–comparison studies, longitudinal studies, and factor analytic studies (e.g., Hwu and Compton 1994; Robins et al. 1981). For the purposes of this study we used the report of a diagnosis of MDD and ASPD. These diagnoses have been found to have fair to good reliability across studies (kappa 0.40 to 0.67; Dascalu et al. 2001). Reliabilities in this sample were similar to these values.
Analysis
Growth mixture modeling (GMM) using the Mplus version 6 statistical software package (Muthén and Muthén 2010) was used to identify patterns of growth in disruptive behavior problems and depressive symptoms over time. Time was treated as a fixed parameter in the models. The time points were fixed incrementally based on the spacing between assessment sessions (e.g., fall of Grade 5 fixed at 0, spring of Grade 5 at 0.5, spring of Grade 6 at 1.5, etc.). All analyses used automated multiple starting values in the optimization to reduce the risk that solutions represent local rather than global optima. Before mixture modeling, following standard practice, unconditional latent growth curve (LGC) models (without covariates) were estimated to determine the shape of the trajectories that would provide guidelines for subsequent analyses. The overall fit indices for the LGC models included the comparative fit index (CFI), the Tucker-Lewis index (TLI), and root mean square error of approximation (RMSEA) provided by Mplus. Models are regarded as acceptable if the CFI and TLI are greater than 0.9. A model with an RMSEA of less than 0.05 is regarded as a “good” fit, and an RMSEA of less than 0.08 is “acceptable” (McDonald and Ho 2002). The next step in the analysis was to fit the conditional LGC model by including intervention status and gender. Intervention status was included to statistically control for possible treatment effects. The GMM analyses were then conducted and based on the conditional LGC models, allowing variance across growth parameters for each model (Muthén 2004), To determine the relative fit of the models, we compared models with differing numbers of classes using the Akaike information criterion (AIC; Akaike 1987), the Bayesian information criterion (BIC; Schwartz 1978), and the sample-size adjusted Bayesian information criterion (aBIC; Sclove 1987). Additionally, we used a likelihood difference test, the Lo-Mendel-Rubin (LMR; Lo et al. 2001) which assesses the fit between two nested models that differ by one class. Typically, the smaller the information criteria, the better the model fit to the data. In addition, we evaluated the classification precision as indicated by estimated posterior class probabilities, summarized by the entropy measure (Ramaswamy et al. 1993). Entropy values close to 1.0 indicate higher classification precision with values higher than 0.80 indicating good classification (Muthén 2004). Lastly, a bootstrapped parametric likelihood ratio test (BLRT) procedure was used to confirm the best fitting model once other model fit indicators, class prevalence and interpretability were examined (see McLachlan 1987; Nylund et al. 2007). In our final analysis we evaluate the probability of individuals simultaneously being in a class for each of the two growth processes by integrating the trajectories of disruptive behavior and depression into one model using parallel process GMM.
Missing Data
The estimates of parameters in the models were adjusted for attrition. The Mplus computer program used full information maximum likelihood estimation under the assumption that the data were missing at random. Missing at random assumes that the reason for the missing data is either random or random after incorporating other variables measured in the study (Arbuckle 1996; Little 1995). Full information maximum likelihood is widely accepted as an appropriate way of handling missing data (Muthen and Shedden 1999; Schafer and Graham 2002). The percentage of youth in the sample who had missing data for disruptive behavior problems and depressive symptoms, respectively, at a given time point were as follows: missing 1 to 2 time points, 17.4 %, 16.9 %; missing 3 to 4 time points, 8.6 %, 8.6 %; and missing 5 or more time points, 9.9 %, 4.7 %. Youth with complete information on half or more of the time points did not differ significantly from youth who did not on either baseline disruptive behaviors or depressive symptoms. The Mplus software bases its estimates on all available time points for a given case. To assess the extent of missing data in the dataset, the Mplus software provides a bivariate covariance “coverage” matrix that gives the proportion of available observations for each indicator variable and pairs of variables, respectively. The minimum coverage necessary for models to converge is 0.10 (Muthén and Muthén 2010). In the present study, coverage ranged from 0.69 to 0.96, more than adequate for unbiased estimation.
Results
Descriptives
Table 1 provides means, standard deviations, and sample age and size for disruptive behavior problems and depressive symptoms across the six time points. The overall prevalence of the distal outcomes in the sample varied, but in some cases accounted for over one third of the sample. Approximately 14 % of youth reported having significant disruptive behavior problems and 8 % reported significant depressive symptoms at age 18. In addition, 25 % of the sample had one or more police arrests before age 18, 34 % had been arrested by police one or more times between age 18 and 21, 20 % reported having a significant alcohol problem, and 11 % reported having a significant drug problem at age 23. Regarding adult diagnoses of ASPD and MDD, 25 % had a diagnosis of adult-onset ASPD and 26 % had a diagnosis of MDD at the age of 23 years.
Table 1.
Means standard deviations, and sample size for disruptive behavior problems and depressive symptoms across the six waves
| Grade | Age M (SD) | Disruptive behavior M (SD) | Disruptive behavior N |
Depressive symptoms M (SD) |
Depressive symptoms N |
|---|---|---|---|---|---|
| 5 fall | 10.51 (0.53) | 8.84 (7.71) | 329 | 6.22 (5.92) | 348 |
| 5 spring | 11.00 (0.52) | 7.60 (7.25) | 321 | 6.41 (6.25) | 342 |
| 6 | 11.84 (0.52) | 7.87 (7.98) | 293 | 5.35 (5.65) | 310 |
| 7 | 12.81 (0.57) | 8.09 (8.36) | 282 | 5.75 (6.01) | 297 |
| 8 | 13.75 (0.58) | 7.61 (7.63) | 272 | 6.40 (5.86) | 288 |
| 10 | 15.68 (0.56) | 5.36 (5.85) | 265 | 6.75 (5.99) | 288 |
Disruptive Behavior Problems
Unconditional LGC models were first fit for disruptive behavior to determine the shape of the trajectories and variances in the growth factors. Including a slope parameter significantly improved the fit over that of the intercept model (Δχ2=43.55(3), p<0.001; CFI=0.98, TLI=0.98, RMSEA=0.05). Addition of a quadratic parameter did not improve model fit. All estimated variances in the intercept (σ2=43.52, p<0.001) and slope growth factor (σ2=0.67, p<0.001) were significantly different from zero, suggesting individual differences in pathways of disruptive behavior problems. Based on the fit of the unconditional model, conditional LGC models were estimated by incorporating gender and intervention status into the model with paths leading to the growth factors of disruptive behavior problems. Intervention status was not a significant predictor of the intercept or growth factor. Gender was a significant predictor of the intercept (β=0.27, p =0.019), indicating that males had higher average levels of disruptive behavior in the fall of fifth grade than females.
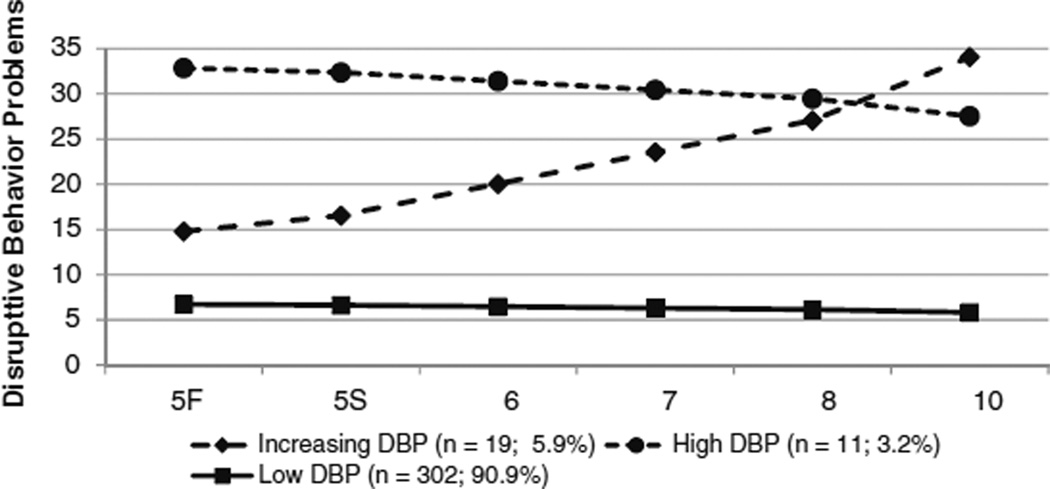
The GMM was an extension of the conditional LGC models formed by adding a latent categorical variable. As described in the analysis subsection, to determine the best-fitting GMM model, we considered the AIC, BIC, and aBIC indices, with the smaller value indicating a better fit model. In addition, entropy was considered in the determination (see Table 2). Class prevalence and interpretability (the extent to which an additional class provided unique information) were also considered when selecting the best-fitting models. Inspection of the three-class and four-class solutions indicated that although few adolescents were classified into the third class (n=11), inclusion of this class added significant information and was in line with theory and previous findings in the literature, whereas the addition of a fourth class in the model did not provide unique information, adding a group of youth with low levels of disruptive behavior that nearly overlapped with the current low level group. A bootstrap validation procedure with 5 successful replications confirmed that the three-class solution offered a better fit than did the two-class solution (log likelihood −5286.783, p<0.001; see McLachlan 1987). Therefore, the three-class solution was chosen. Neither sex nor intervention status predicted group membership for the classes. An inspection of the trends indicated that males were slightly more likely to be in the high disruptive behavior class than females (OR 1.63), however, this finding was not statistically significant. Youth in the intervention and in the control conditions were equally likely to be in each of the classes. The three trajectories included a group of adolescents exhibiting high levels of disruptive behavior (3.2 %), a group exhibiting disruptive behavior problems that increased over time (5.9 %), and a group exhibiting consistently low levels of disruptive behavior (90.9 %). After obtaining the predicted group membership from the GMM analyses, the estimated means were calculated and graphed (see Figure 1).
Table 2.
Fit Indices of growth mixture modeling for disruptive behavior problems and depressive symptoms
| Disruptive behavior problems | Depressive symptoms | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| LC | AIC | BIC | aBIC | LMR | Entropy | AIC | BIC | aBIC | LMR | Entropy |
| 2 | 10609.57 | 10678.06 | 10620.96 | 0.05 | 0.95 | 11173.97 | 11258.84 | 11189.05 | 0.03 | 0.96 |
| 3 | 10547.22 | 10627.13 | 10560.52 | 0.10 | 0.96 | 11069.73 | 11170.03 | 11087.55 | 0.70 | 0.94 |
| 4 | 10510.69 | 10602.01 | 10525.89 | 0.18 | 0.96 | 10998.25 | 11113.99 | 11018.82 | 0.02 | 0.93 |
| 5 | – | – | – | – | – | 10957.13 | 11088.30 | 10980.44 | 0.05 | 0.92 |
LC Latent class, AIC Akaike information criterion, BIC Baysian information criterion, aBIC adjusted Baysian information criterion, LMR Lo-Mendell-Rubin Adjusted Likelihood Ratio Test. Smaller values indicate better fit of the model. Entropy values close to 1.0 indicate higher classification precision. Bold indicates best fitting class model
Fig. 1.
Developmental trajectories of disruptive behavior problems from Grades 5 to 10
Following identification of the appropriate number of classes, the classes were used to predict distal outcomes using latent class regression analysis (Guo et al. 2006). We could then describe the association between the disruptive behavior problems subclasses and distal outcomes (see Table 3). The findings are reported in terms of odds ratios; that is, the odds that youth in the problem subclasses were more likely to exhibit negative outcomes than were those in the low disruptive behavior class. Mplus was unable to provide odds ratios or confidence intervals for two outcomes—youth-reported depression in adulthood and MDD diagnosis for the high disruptive behavior problems subclass—because of zero variance. For instance, 0 % of youth in the high class were diagnosed with MDD as an adult, a findings that strongly supports the distinctiveness of the class.
Table 3.
Odds ratios showing association between disruptive behavior problems and depressive symptoms subclasses and problems during emerging adulthood
| Outcome | Disruptive behavior problems | Depressive symptoms | |||
|---|---|---|---|---|---|
| Increasing vs. low | High vs. low | Increasing vs. low | Decreasing vs. low | High vs. low | |
| Self-reported depression age 18 | 6.59* (1.60–21.57) | – | 6.41* (1.01–40.83) | 1.99 (0.34–11.48) | 8.48* (1.62–44.39) |
| Self-reported disruptive behavior age 18 | 2.85* (1.03–6.70) | 3.28* (1.59–6.73) | 18.70* (4.38–79.80) | 4.27* (1.45–12.63) | 3.43 (0.54–21.60) |
| Arrested as juvenile | 7.85* (2.07–29.75) | 2.81 (0.65–12.24) | 1.72 (0.43–6.76) | 2.06 (0.78–5.41) | 2.07 (0.70–6.12) |
| Arrested as adult | 1.49 (0.54–4.12) | 10.32* (4.94–21.59) | 1.34 (0.38–4.52) | 1.78 (0.55–5.71) | – |
| Alcohol problems | 2.89* (1.05–4.36) | 2.19* (1.10–3.91) | 3.18 (0.89–11.35) | 0.70 (0.14–3.59) | 16.39* (1.47–166.67) |
| Drug problems | 1.72 (0.53–5.57) | 5.04* (2.25–11.33) | 3.04 (0.50–18.44) | 3.41 (0.95–12.22) | 4.06* (1.17–14.77) |
| ASPD | 0.38 (0.14–1.10) | 1.89 (0.99–3.61) | 3.53 (0.89–13.89) | 2.17 (0.75–6.25) | 0.78 (0.24–3.14) |
| MDD | 1.15 (0.39–3.37) | – | 4.74 (0.58–38.96) | 0.55 (0.13–2.27) | 2.12 (0.56–8.01) |
Range indicates 95 % confidence interval for odds ratios
–Unable to calculate odds ratio due to zero variance in outcome for problems class
p<0.05
Youth in the increasing and the high disruptive behavior problems classes were significantly more likely to exhibit significant disruptive behavior problems as young adults than were those in the low disruptive behavior class, by self-report (OR 2.85, 3.28, respectively). Interestingly, youth in the increasing disruptive behavior class were more likely to report significant depressive symptoms as young adults than youth in the low disruptive behavior class (OR 6.59) after controlling for baseline levels of depressive symptoms. Further, youth in the increasing disruptive behavior problems class were 8 times more likely to be arrested as juveniles, and 3 times more likely to report problems with alcohol as an adult than youth in the low disruptive behavior class. As young adults, youth in the high disruptive behavior problems class were significantly more likely to report problems with alcohol and drugs and 10 times more likely to be arrested as adults than were youth in the low disruptive behavior class.
Depressive Symptoms
The quadratic model fit significantly better than the linear model (Δχ2=42.53(4), p<0.001) for the unconditional LGC models for depressive symptoms (CFI=0.99, TLI=0.99, RMSEA=0.03). The quadratic growth factor model, however, was fixed to zero because of limited variance for the LGC and all subsequent analyses. All estimated variances in the intercept (σ2=23.74, p<0.001) and slope growth factor (σ2=6.02, p<0.001) were significantly different from zero, suggesting individual differences in pathways of depressive symptoms. Using the conditional LGC model, we found that intervention status was not a significant predictor of the intercept or growth factors. Sex was marginally significant with regard to slope (β=− 0.27, p =0.056), indicating that girls were more likely than boys to exhibit growth on depressive symptoms over time.
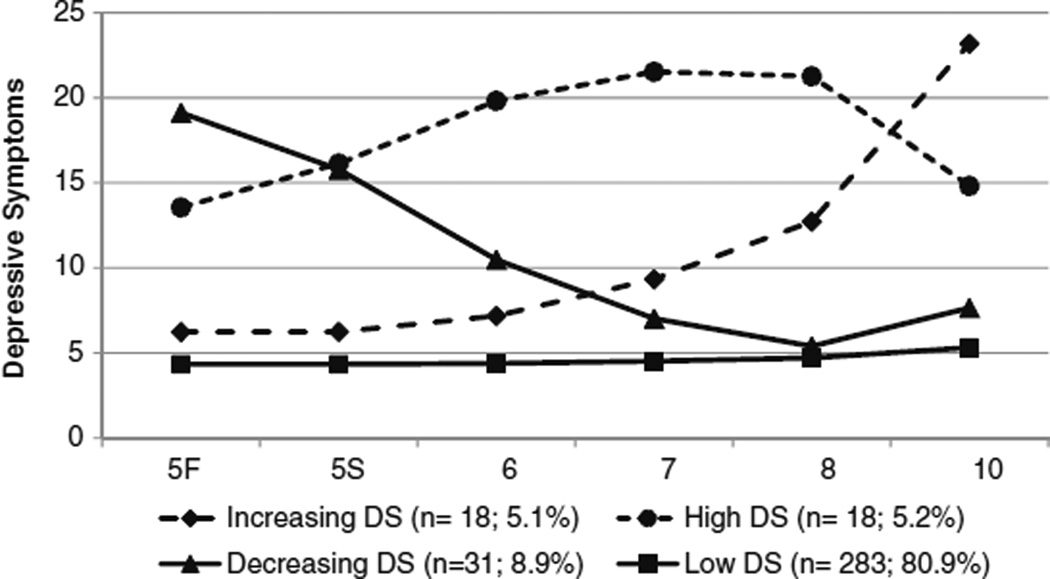
GMM analyses for depressive symptoms led to a four-class solution. The four-class solution added a class of youth with increasing depressive symptoms over time. The addition of a fifth class added no substantial information in that it produced a second low level depression subclass. A bootstrap validation procedure with 5 successful replications confirmed that the four-class solution offered a better fit than did the three-class solution (log likelihood −5508.86, p<0.001; see McLachlan 1987). Therefore, the four-class solution was chosen for further analyses. Neither sex nor intervention status was predictive of class membership. An inspection of the trends indicated that females were slightly more likely to be in the high (OR 2.38) or increasing depression (OR 2.70) classes than males, however, the findings were not statistically significant. Youth in the intervention and in the control conditions were equally likely to be in each of the classes. The four trajectories of depressive symptoms included a group with increasing symptoms (5.1 %), with high levels of depressive symptoms (5.2 %), with decreasing depressive symptoms (8.9 %), and with low levels of depressive symptoms (80.9 %). The estimated means for depressive symptoms were calculated and are represented in Figure 2.
Fig. 2.
Developmental trajectories of depressive symptoms from Grades 5 to 10
Latent class regression analyses were conducted to describe the association between the depressive symptom subclasses and distal outcomes (see Table 3). Outcomes for youth as young adults indicate that those in the increasing and high depressive symptoms class continued to report problems with depression compared to youth in the low depression class. Further, youth in the increasing depression class were 19 times more likely to report significant disruptive behavior problems than youth in the low class after controlling for baseline disruptive behavior. Youth in the decreasing depression class were also more likely to have significant disruptive behavior problems as young adults (OR 4.27) after controlling for baseline levels of disruptive behavior. Youth in the high depressive symptoms class were 16 times more likely to report alcohol problems and 4 times more likely to report drug problems as adults than youth in the low class.
Co-occurring Problems
The co-occurrence of disruptive behavior problems and depressive symptoms was evaluated using parallel process GMM analysis (Greenbaum and Dedrick 2007). Table 4 presents the estimated frequency and joint probability of membership in trajectory groups. For instance, 282 youth (81 %) were simultaneously in the low disruptive behavior and low depression trajectories, whereas only 1 individual was in the high disruptive behavior problems and high depressive symptoms co-occurring class.
Table 4.
Co-occurrence of disruptive behavior problems and depressive symptoms for adolescents
| Increasing DS | High DS | Decreasing DS | Low DS | |
|---|---|---|---|---|
| Estimated group membership | ||||
| Increasing DBP | 2 | 2 | 1 | 8 |
| High DBP | 0 | 1 | 3 | 15 |
| Low DBP | 13 | 6 | 17 | 282 |
| Joint probability of DBP and DS | ||||
| Increasing DBP | 0.006 | 0.006 | 0.003 | 0.023 |
| High DBP | 0.000 | 0.003 | 0.009 | 0.043 |
| Low DBP | 0.037 | 0.019 | 0.046 | 0.806 |
| Probability of DBP conditional on DS | ||||
| Increasing DBP | 0.133 | 0.222 | 0.048 | 0.026 |
| High DBP | 0.000 | 0.111 | 0.143 | 0.049 |
| Low DBP | 0.534 | 0.667 | 0.810 | 0.925 |
| Probability of DS conditional on DBP | ||||
| Increasing DBP | 0.154 | 0.154 | 0.078 | 0.612 |
| High DBP | 0.000 | 0.053 | 0.158 | 0.789 |
| Low DBP | 0.041 | 0.019 | 0.053 | 0.887 |
Although joint probabilities provide us with information about the probability of membership in more than one class, conditional probabilities may provide more meaningful information about co-occurrence. The lower portion of Table 4 provides two sets of conditional probabilities: the probability of membership in each disruptive behavior problems class conditional on each depressive class, and vice versa. For instance, when looking at joint probabilities, less than 1 % of adolescents who were in the high depressive symptoms class were also in the high disruptive behavior problems class. By contrast, a different distribution appears when we examine the probability of disruptive behavior problems conditional on depressive symptoms: among youth in the highest depressive symptoms class, 11 % of these youth were in the high disruptive behavior class, versus 5 % of youth in the low depressive symptoms being in the high disruptive behavior class. Similarly, 22 % of high depressive youth were in the increasing disruptive behavior class versus only 3 % of youth in the low depressive subclass being in the increasing disruptive behavior class. These findings indicate that exhibiting high depressive symptoms may increase the risk for co-occurring disruptive behavior problems. On the other hand, when one considers the probability of depression given disruptive behavior problems, youth in the high disruptive behavior problems class have a 5 % probability of being in the high depression class, whereas, 16 % of these youth are in the decreasing depression class, and 79 % in the low depression class. Fifteen percent of youth in the increasing disruptive behavior problems class were also in the increasing depression class or high depression class, versus 4 % of youth from the low disruptive class being in the increasing depression class and 2 % in the high depression class. These findings indicate that youth with increasing disruptive behavior problems are at an increased risk for co-occurring depression. No significant differences were found for gender with regard to co-occurring presentations (χ2=9.76(10), p=0.46). The low number of adolescents in co-occurring classes prevented formal examination of outcomes for youth with comorbid patterns during emerging adulthood. However, descriptive information is provided here for purposes of documentation. The percentages of youth within in each co-occurring trajectory who met criteria for the distal outcomes are provided in Table 5. For instance, 100 % of youth in the co-occurring high disruptive behavior and decreasing depressive symptom subclass had been arrested as juveniles, 50 % were arrested as an adult, 50 % reported alcohol problems, 100 % report problems with drugs, and 67 % were diagnosed with ASPD.
Table 5.
Percentage of youth within each co-occurring class meeting criteria for problems during emerging adulthood
| Increasing DS | High DS | Decreasing DS | Low DS | |
|---|---|---|---|---|
| Youth reported depressive symptoms | ||||
| Increasing DBP | 50 | 50 | 0 | 0 |
| High DBP | NA | 0 | 0 | 9 |
| Low DBP | 9 | 40 | 8 | 7 |
| Youth reported behavior problems | ||||
| Increasing DBP | 50 | 50 | 0 | 0 |
| High DBP | NA | 100 | 0 | 27 |
| Low DBP | 54 | 20 | 17 | 11 |
| Juvenile arrest | ||||
| Increasing DBP | 100 | 50 | 100 | 75 |
| High DBP | NA | 0 | 100 | 50 |
| Low DBP | 38 | 20 | 33 | 28 |
| Adult arrest | ||||
| Increasing DBP | 50 | 0 | 100 | 75 |
| High DBP | NA | 100 | 50 | 60 |
| Low DBP | 23 | 20 | 50 | 34 |
| Alcohol problems | ||||
| Increasing DBP | 0 | 50 | 100 | 25 |
| High DBP | NA | 0 | 50 | 40 |
| Low DBP | 54 | 40 | 25 | 16 |
| Drug problems | ||||
| Increasing DBP | 0 | 0 | 100 | 25 |
| High DBP | NA | 0 | 100 | 20 |
| Low DBP | 23 | 20 | 17 | 8 |
| ASPD | ||||
| Increasing DBP | 50 | 0 | 0 | 25 |
| High DBP | NA | 0 | 67 | 56 |
| Low DBP | 54 | 50 | 42 | 33 |
| MDD | ||||
| Increasing DBP | 50 | 50 | 100 | 0 |
| High DBP | NA | 0 | 0 | 10 |
| Low DBP | 54 | 60 | 8 | 26 |
Discussion
We proposed that investigating the longitudinal developmental trajectories between disruptive behavior problems and depressive symptoms and their co-occurrence could provide insights regarding the course of each, and perhaps shed light on the viability of interventions that address both. Our study used high quality assessment reports concerning a sample of youth across approximately 14 years of their lives. The results supported the hypothesis that multiple trajectories of disruptive behavior problems and depressive symptoms would be found, with the majority of youth exhibiting low levels of these problems. Three trajectory classes were found for disruptive behavior problems and four for depressive symptoms. The high disruptive behavior problems group likely represents “early starters,” and the increasing group represents “late starters”, as discussed elsewhere in the literature (e.g., Moffitt 1993). Youth in this early starter group had the most negative outcomes, including increased risk for arrest, and drug and alcohol problems as young adults. Interestingly, youth with increasing disruptive behavior problems shared similar risk for depression in early adulthood as youth in the increasing depression subclass. Youth in the increasing depression subclass were also significantly more likely to report disruptive behavior problems in early adulthood. This indicates heterotypic development of one problem to another (e.g., Angold et al. 1999), implying that for these youth, interventions targeting both symptoms may be warranted and could optimize the success of prevention and intervention efforts.
Nevertheless, similar to Chen and Simons-Morton (2009), this longitudinal analysis indicated that adolescent depression and disruptive behavior problems may have unique developmental trajectories; among this sample, only 1 % of youth showed high levels of both depression and disruptive behavior problems across time. However, and again similar to Chen and Simons-Morton (2009), being depressed increased risk for the co-occurrence of disruptive behavior problems (11 % in the high disruptive behavior problems class; 22 % in the increasing disruptive behavior problems class), and youth who increasingly engaging in disruptive behavior were at increased risk for depression (15 %). Prior research suggests that a history of disruptive behavior has a cascading effect on multiple outcomes and potential failure experiences that could account for increased risk of depression (Capaldi and Patterson 1991; Kiesner 2002; Patterson and Stoolmiller 1991). Moreover, the progression from failures to involvement with deviant peers (Dishion et al. 1991), and the ensuing chaos of those peer relationships could likely generate stress and depression (Brendgen et al., 2000). Not as easily explained, however, is the increased probability of disruptive behavior problems among youth who are predominantly depressed. A recent study which modeled co-occurring symptoms among adolescents (ages 12 to 19) found that early depressive symptoms predicted increases in delinquency over time, but—contrary to the failure model—early delinquency did not predict subsequent changes in depressive symptoms (Kofler et al., 2011). Kofler and colleagues (2011) suggested that this sequence supports an “acting out” model, whereby the irritability that is characteristic of depression may lead to aggression, rule breaking, and detrimental relationships with adults and peers, which in turn leads to worsening disruptive behavior problems. Not surprisingly, youth in co-occurring problem classes were more likely to meet criteria for problems during adulthood. For instance, 100 % of youth in the increasing disruptive behavior and increasing depression class were arrested as juveniles, whereas only 28 % of youth in the co-occurring low classes had been arrested as juveniles.
Despite consistent findings in gender differences in disruptive behavior problems and depression, we did not find gender to be a significant predictor of class membership. For instance, there has been evidence that boys tend to have higher rates of behavior problems (Loeber and Keenan 1994), whereas girls exhibit higher rates of depression (Wade et al. 2002). Boys in this sample did exhibit significantly higher levels of disruptive behavior problems in fifth grade than girls. There was a trend in the data showing that girls were slightly more likely to be in the high or increasing depressed classes and boys were slightly more likely to be in the high disruptive behavior problem class, however, these findings were not statistically significant. Unlike Chen and Simons-Morton (2009), we did not find gender to be associated with the conditional probabilities of risk for either problem. However, it is likely that the small sample size precluded finding significant differences in gender as well as intervention status in this study. Further studies are needed of a variety of (and larger) community samples to evaluate gender differences in the development of disruptive behavior problems and depression.
Interventionists who target disruptive behavior problems or depression may find it useful to consider the developmental etiology and course of the child and adolescent. In some cases, an adolescent presenting as depressed may be best served by an intervention targeting the reduction of disruptive behavior problems, such as a family intervention that focuses on parental monitoring and other family management practices (e.g., Dishion and Stormshak 2007). In other cases, a pure depression syndrome with little history of disruptive behavior problems may benefit from a more cognitive–behavioral approach directed to the child or adolescent, with supplementary support to the parents (Clarke et al. 2003). Adaptive tailored prevention and treatment designs allow intervention to be fit to the child’s developmental pattern and ecology that underlie the behavior problems and emotional distress (Collins et al. 2004).
There are several limitations that should be taken into consideration when interpreting the findings. First, though participants were drawn from a community sample, they were attending public schools located within neighborhoods selected because of locally high rates of juvenile delinquency. The current findings may not be generalizable to male and female adolescents growing up in other types of neighborhoods. Second, although we were able to evaluate the co-occurrence of growth trajectories, we were not able to statistically examine group differences on distal outcomes for the co-occurring subclasses due to very small cell sizes. Future research with a larger sample would allow such an examination.
Longitudinal follow-up of the young men and women in this sample clearly indicates that subclasses of disruptive behavior problems and depressive symptoms are prognostic of heightened risk. These early life difficulties set the stage for compromised patterns of adjustment that are evident during emerging adulthood, and that could be extant for the life course. Children and adolescents who experience depressive symptoms and/or disruptive behavior problems over time require attention. Continued work is needed on what type of attention is best for which youth. A science of intervention based on knowledge of developmental processes such as those examined here is germane to improving life outcomes.
Acknowledgments
This research was supported by grant R01 MH054248 from the Prevention Research Branch, NIMH, NIH, U.S. PHS, grant R01 HD054880 to the second and fourth author from the Social and Affective Development/Child Maltreatment and Violence Branch, NICHD, NIH, U.S. PHS, and grants DA07031 and DA16110 from the National Institutes of Health to the third author.
Contributor Information
Wendy M. Reinke, Email: reinkew@missouri.edu, Department of Educational, School, & Counseling Psychology, University of Missouri, Columbia, MO 65211, USA.
J. Mark Eddy, University of Washington, Seattle, WA, USA; Oregon Social Learning Center, Eugene, OR, USA.
Thomas J. Dishion, Arizona State University, Tempe, AZ, USA Child and Family Center, University of Oregon, Eugene, OR, USA.
John B. Reid, Oregon Social Learning Center, Eugene, OR, USA
References
- Achenbach TM. Manual for the child behavior checklist 4– 18 and 1991 profile. Burlington: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- American Psychological Association. Diagnostic and statistical manual of mental disorder. 4th ed. Washington: American Psychiatric Association; 1994. [Google Scholar]
- Angold A, Costello EJ. Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. The American Journal of Psychiatry. 1993;150:1779–1791. doi: 10.1176/ajp.150.12.1779. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8-17-year-olds: effects of age and gender. Journal of Child Psychology and Psychiatry. 2002;43:1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling: Issues and techniques. Mahwah: Erlbaum; 1996. [Google Scholar]
- Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. [PubMed] [Google Scholar]
- Barrish HH, Saunders M, Wolf MM. Good behavior game: Effects of individual contingencies for group consequences on disruptive behavior in a classroom. Journal of Applied Behavior Analysis. 1969;2:119–124. doi: 10.1901/jaba.1969.2-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brendgen M, Vitaro F, Bukowski W. Deviant friends and early adolescents’ emotional and behavioral adjustment. Journal of Research on Adolescence. 2000;10:173–189. [Google Scholar]
- Brendgen M, Wanner B, Morin AJ, Vitaro F. Relations with parents and with peers, temperament, and trajectories of depressed mood during early adolescence. Journal of Abnormal Child Psycholgy. 2005;33:579–594. doi: 10.1007/s10802-005-6739-2. [DOI] [PubMed] [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: II. A 2-year followup at Grade 8. Development and Psychopathology. 1992;4:125–144. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Patterson GR. Relation of parental transitions to boys' adjustment problems: I. A linear hypothesis: II. Mothers at risk for transitions and unskilled parenting. Developmental Psychology. 1991;27:489–504. [Google Scholar]
- Capaldi DM, Stoolmiller M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. Prediction to young-adult adjustment. Development and Psychopathology. 1999;11:59–84. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Chen R, Simons-Morton B. Concurrent changes in conduct problems and depressive symptoms in early adolescents: a developmental person-centered approach. Development and Psychopathology. 2009;21:285–307. doi: 10.1017/S0954579409000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke GN, DeBar LL, Lewinsohn PM. Cognitive behavioral group treatment for adolescent depression. In: Kazdin AEN, Weisz JR, editors. Evidenced-based psychotherapies for children and adolescents. New York, NY: Guilford Press; 2003. pp. 120–134. [Google Scholar]
- Collins LM, Murphy SA, Bierman KL. A conceptual framework for adaptive preventive interventions. Prevention Science. 2004;5:185–196. doi: 10.1023/b:prev.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello E, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescents: effects of timing and sex. Journal of Clinical Child Psychology. 1999;28:298–311. doi: 10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- Costello E, Foley DL, Angold A. 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: II. developmental epidemiology. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- Cote S, Zoccolillo M, Tremblay RE, Nagin D, Vitaro F. Predicting girls' conduct disorder in adolescence from childhood trajectories of disruptive behaviors. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:678–684. doi: 10.1097/00004583-200106000-00013. [DOI] [PubMed] [Google Scholar]
- Dascalu M, Compton WM, Horton JC, Cottler LB. Validity of DIS-IV in diagnosing depression and other psychiatric disorders among substance users. Drug and Alcohol Dependence. 2001;63:37. [Google Scholar]
- Dekker MC, Ferdinand RF, van Lang ND, Bongers IL, van der Ende J, Verhulst FC. Developmental trajectories of depressive symptoms from early childhood to late adolescence: gender differences and adult outcome. Journal of Child Psychology and Psychiatry. 2007;48:657–666. doi: 10.1111/j.1469-7610.2007.01742.x. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Brief symptom inventory. Baltimore: Clinical Psychometric Research; 1975. [Google Scholar]
- Dishion T, Stormshak E. Intervening in children's lives: An ecological, family-centered approach to mental health care. Washington: American Pyschological Association; 2007. [Google Scholar]
- Dishion T, Patterson G, Stoolmiller M, Skinner M. Family, school, and behavioral antecedents to early adolescent involvement with antisocial peers. Developmental Psychology. 1991;27:172–180. [Google Scholar]
- Eddy JM, Reid JB, Fetrow RA. An elementary school-based prevention program targeting modifiable antecedents of youth delinquency and violence: Linking the Interests of Families and Teachers (LIFT) Journal of Emotional & Behavioral Disorders. 2000;8:165–176. [Google Scholar]
- Eddy JM, Reid JB, Stoolmiller M, Fetrow RA. Outcomes during middle school for an elementary school-based preventive intervention for conduct problems: follow-up results from a randomized trial. Behavior Therapy. 2003;34:535–552. [Google Scholar]
- Farrington DP, Loeber R. Some benefits of dichotomization in psychiatric and criminological research. Criminal Behaviour & Mental Health. 2000;10:100. [Google Scholar]
- Gavin D, Ross H, Skinner H. Diagnostic validity of the Drug Abuse Screening Test in the assessment of DSM-III drug disorders. British Journal of Addiction. 1989;84:301–307. doi: 10.1111/j.1360-0443.1989.tb03463.x. [DOI] [PubMed] [Google Scholar]
- Ge X, Conger RD, Elder GH., Jr Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Developmental Psychology. 2001;37:404–417. doi: 10.1037//0012-1649.37.3.404. [DOI] [PubMed] [Google Scholar]
- Gibbs LE. Validity and reliability of the Michigan Alcoholism Screening Test: A review. Drug and Alcohol Dependency. 1983;12:279–285. doi: 10.1016/0376-8716(83)90071-6. [DOI] [PubMed] [Google Scholar]
- Greenbaum P, Dedrick R. Changes in use of alcohol, marijuana, and services by adolescents with serious emotional disturbance: a parralell-process growth mixture model. Journal of Emotional & Behavioal Disorders. 2007;15:21–32. [Google Scholar]
- Guo J, Wall M, Amemiya Y. Latent class regression on latent factors. Biostatistics. 2006;7:145–163. doi: 10.1093/biostatistics/kxi046. [DOI] [PubMed] [Google Scholar]
- Hirschfield P, Maschi T, White HR, Goldman-Traub L, Loeber R. The effects of mental health problems on juvenile arrests: Criminality, criminalization, or compassion? Criminology. 2006:593–630. [Google Scholar]
- Hwu H-G, Compton WM. Comparison of major epidemiological surveys using the Diagnostic Interview Schedule. International Review of Psychiatry. 1994;6:309–327. [Google Scholar]
- Kellam SG, Rebok GW. Building developmental and etiological theory through epidemiologically based preventive intervention trials. In: McCord J, Tremblay RE, editors. Preventing antisocial behavior: Interventions from birth through adolescence. New York: Guilford; 1992. pp. 162–195. [Google Scholar]
- Kendler KS, Sheth K, Gardner CO, Prescott CA. Childhood parental loss and risk for first-onset of major depression and alcohol dependence: the time-decay of risk and sex differences. Psychological Medicine. 2002;32:1187–1194. doi: 10.1017/s0033291702006219. [DOI] [PubMed] [Google Scholar]
- Kiesner J. Depressive symptoms in early adolescence: their relations with classroom problem behavior and peer status. Journal of Research on Adolescence. 2002;12:463–478. [Google Scholar]
- Kofler MJ, Ruggiero KJ, McCart MR, Zajac K, Saunders BE, Kipatrick DG. Depression and delinquency covariation in an accelerated longitudinal sample of adolescents. Journal of Consulting and Clinical Psychology. 2011;79:458–469. doi: 10.1037/a0024108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Children's depression inventory manual. Canada: Multi-Health Systems; 1992. [Google Scholar]
- Kovacs M, Paulauskas S, Gatsonis C, Richards C. Depressive disorders in childhood: III. A longitudinal study of comorbidity with and risk for conduct disorders. Journal of Affective Disorders. 1988;15:205–217. doi: 10.1016/0165-0327(88)90018-3. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull. 2000;126:309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- Little RJ. Modeling the dropout mechanism in repeatedmeasures studies. Journal of the American Statistical Association. 1995;90:1112–1121. [Google Scholar]
- Lo Y, Mendall NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Loeber R, Keenan K. Interaction between conduct disorder and its comorbid conditions: effects of age and gender. Clinical Psychology Review. 1994;14:497–523. [Google Scholar]
- Loeber R, Russo MF, Stouthamer-Loeber M, Lahey BB. Internalizing problems and their relation to the development of disruptive behaviors in adolescence. Journal of Research on Adolescence. 1994;4:615–637. [Google Scholar]
- McDonald RP, Ho M-HR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7:64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- McLachlan G. On bootstrapping the likelihood ratio test statistic for the number of components in a normal mixture. Applied Statistics. 1987;36:318–324. [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Developmental Psychopathology. 2001;13:355–375. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Muthén B. Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of quantitative methodology for the social sciences. Newbury Park: Sage; 2004. pp. 345–368. [Google Scholar]
- Muthén B, Muthén LK. Mplus users guide. Los Angeles: Muthén and Muthén; 2010. [Google Scholar]
- Muthen B, Shedden K. Finitemixturemodeling with mixture outcomes using the EM algorithm. Biometrics. 1999;6:463–469. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kazdin AE, Hiripi E, Kessler RC. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National Comorbidity Survey Replication. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2006;36:699–710. doi: 10.1017/S0033291706007082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- Patterson GR, Stoolmiller M. Replications of a dual failure model for boys' depressed mood. Journal of Consulting and Clinical Psychology. 1991;59:491–498. doi: 10.1037//0022-006x.59.4.491. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Reid JB, Dishion TJ. Antisocial Boys. In: Jenkins JM, Oatley K, Stein NL, editors. Human emotions: A reader. Malden: Blackwell; 1992. pp. 330–336. [Google Scholar]
- Ramaswamy V, DeSarbo W, Reibstein D, Robinson W. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Science. 1993;12:103–124. [Google Scholar]
- Reid JB, Eddy JM, Fetrow RA, Stoolmiller M. Description and immediate impacts of a preventive intervention for conduct problems. American Journal of Community Psychology. 1999;27:483–517. doi: 10.1023/A:1022181111368. [DOI] [PubMed] [Google Scholar]
- Reid JB, Patterson GR, Snyder J. Antisocial behavior in children and adolescents: A developmental analysis and model for intervention. Washington, DC: American Psychological Association; 2002. p. xi.p. 337. [Google Scholar]
- Robins LN, Helzer JE, Croughan JL, Ratcliff KS. National Institute of Mental Health diagnostic interview schedule: its history, characteristics, and validity. Archives of General Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Rutter M. Pathways from childhood to adult life. Journal of Child Psychology and Psychiatry. 1989;30:23–51. doi: 10.1111/j.1469-7610.1989.tb00768.x. [DOI] [PubMed] [Google Scholar]
- Schaeffer CM, Petras H, Ialongo N, Poduska J, Kellam S. Modeling Growth in Boys' Aggressive Behavior Across Elementary School: Links to Later Criminal Involvement, Conduct Disorder, and Antisocial Personality Disorder. Developmental Psychology. 2003;39:1020–1035. doi: 10.1037/0012-1649.39.6.1020. [DOI] [PubMed] [Google Scholar]
- Schaeffer CM, Petras H, Ialongo N, Masyn KE, Hubbard S, Poduska J, Kellam S. A comparison of girls' and boys' aggressive-disruptive behavior trajectories across elementary school: Prediction to young adult antisocial outcomes. Journal of Consulting and Clinical Psychology. 2006;74:500–510. doi: 10.1037/0022-006X.74.3.500. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schwartz G. Estimating the dimensions of a model. The Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Sclove LS. Application of a model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- Selzer ML. The Michigan Alcoholism Screening Test: the quest for a new diagnostic instrument. American Journal of Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Sihvola E, Rose R, Dick D, Pulkkinen L, Marttunen M, Kaprio J. Early-onset depressive disorders predict the use of addictive substances in adolescence: a prospective study of adolescent Finnish twins early-onset of depressive disorders and substance abuse. Addiction. 2008;103:2045–2053. doi: 10.1111/j.1360-0443.2008.02363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA. The drug abuse screening test. Addictive Behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Stoolmiller M, Eddy JM, Reid JB. Detecting and describing preventive intervention effects in a universal schoolbased randomized trial targeting delinquent and violent behavior. Journal of Consulting and Clinical Psychology. 2000;68:296–306. doi: 10.1037//0022-006x.68.2.296. [DOI] [PubMed] [Google Scholar]
- Stoolmiller M, Kim HK, Capaldi DM. The course of depressive symptoms in men from early adolescence to young adulthood: identifying latent trajectories and early predictors. Journal of Abnormal Psychology. 2005;114:331–345. doi: 10.1037/0021-843X.114.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor TK, Eddy JM, Biglan A. Interpersonal skills training to reduce aggressive and delinquent behavior: limited evidence and the need for an evidence-based system of care. Clinical Child and Family Psychology Review. 1999;2:169–182. doi: 10.1023/a:1021855022385. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Nolen-Hoeksema S. Age, gender, race, socioeconomic status, and birth cohort differences on the children's depression inventory: a meta-analysis. Journal of Abnormal Psychology. 2002;111:578–588. doi: 10.1037//0021-843x.111.4.578. [DOI] [PubMed] [Google Scholar]
- Wade TJ, Cairney J, Pevalin DJ. Emergence of gender differences in depression during adolescence: national panel results from three countries. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:190–198. doi: 10.1097/00004583-200202000-00013. [DOI] [PubMed] [Google Scholar]
- Wolff JC, Ollendick TH. The comorbidity of conduct problems and depression in childhood and adolescence. Clinical Child and Family Psychology Review. 2006;9:201–220. doi: 10.1007/s10567-006-0011-3. [DOI] [PubMed] [Google Scholar]
- Zoccolillo M. Co-occurrence of conduct disorder and its adult outcomes with depressive and anxiety disorders: a review. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:547–556. doi: 10.1097/00004583-199205000-00024. [DOI] [PubMed] [Google Scholar]
- Zoccolillo M, Meyers J, Assiter S. Conduct disorder, substance dependence, and adolescent motherhood. American Journal of Orthopsychiatry. 1997;67:152–157. doi: 10.1037/h0080220. [DOI] [PubMed] [Google Scholar]