Abstract
Objectives
The study objectives were to determine the feasibility and effects of providing therapeutic massage at home for patients with metastatic cancer.
Design
This was a randomized controlled trial.
Settings/location
Patients were enrolled at Oncology Clinics at a large urban academic medical center; massage therapy was provided in patients' homes.
Subjects
Subjects were patients with metastatic cancer.
Interventions
There were three interventions: massage therapy, no-touch intervention, and usual care.
Outcome measures
Primary outcomes were pain, anxiety, and alertness; secondary outcomes were quality of life and sleep.
Results
In this study, it was possible to provide interventions for all patients at home by professional massage therapists. The mean number of massage therapy sessions per patient was 2.8. A significant improvement was found in the quality of life of the patients who received massage therapy after 1-week follow-up, which was not observed in either the No Touch control or the Usual Care control groups, but the difference was not sustained at 1 month. There were trends toward improvement in pain and sleep of the patients after therapeutic massage but not in patients in the control groups. There were no serious adverse events related to the interventions.
Conclusions
The study results showed that it is feasible to provide therapeutic massage at home for patients with advanced cancer, and to randomize patients to a no-touch intervention. Providing therapeutic massage improves the quality of life at the end of life for patients and may be associated with further beneficial effects, such as improvement in pain and sleep quality. Larger randomized controlled trials are needed to substantiate these findings.
Introduction
Pain is one of the most common symptoms among patients with advanced cancer1,2 and these patients often suffer from poor symptom control.2,3 Available medications frequently have unwanted side effects that limit their use.2,3 Although massage has been advocated as a therapy that might improve symptom management in patients with cancer,4,5 the effects of massage among patients with advanced cancer have been relatively underinvestigated.2,3,6,7
It was hypothesized that providing therapeutic massage in the homes of patients with advanced cancer is feasible and that massage would lessen symptoms of these patients. The benefit of massage as an adjunctive therapy was investigated for management of pain, anxiety, and alertness for patients with metastatic cancer. It was also studied whether massage therapy improved the quality of life and sleep of these patients.
Methods
Study site
This study took place at Beth Israel Deaconess Medical Center (BIDMC) in Boston, MA. BIDMC provides cancer care to patients 18 years of age or older. Of patients seen in oncology clinics, approximately 1 in 4 patients participates in research protocols. In addition to physician visits, the clinics provide chemotherapy protocols, as well as nursing and social work visits. Enrollment and randomization of study patients occurred in the oncology clinic, but all massage treatments and control interventions occurred at the patient's home.
Study design
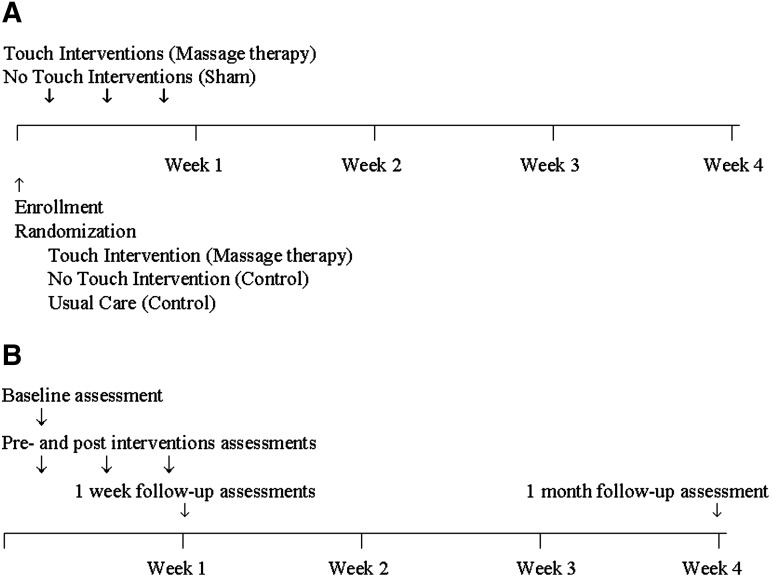
The study overview and the timing of the study procedures have been summarized in Figure 1. Patients were randomized to receive either massage or, as controls, a no-touch intervention by professional massage therapists or usual care. During the first week following enrollment, they received up to three treatments in their home. To gain more experience with the massage intervention, the authors randomized twice as many patients to the massage intervention as to the no-touch control intervention or the usual-care control groups.
FIG. 1.
A. Study overview; timing of interventions. B. Study overview; timing of assessments.
Selection of massage therapists
It was required that the massage therapists be members in good standing within their profession, experienced in multiple modalities of massage therapy, able to engage in sustained relationships with patients with advanced cancer, have valid licensure, possess membership in the American Massage Therapy Association or certification by the National Certification Board for Massage Therapy and Bodywork, carry their own malpractice and liability insurance, evidence of continuing education, and a minimum of 3 years full-time or 5 years part-time practice. To meet the particular needs of this study, it was required that massage therapists have training and experience in Swedish Massage as well as experience with patients at end of life. Since Massachusetts did not have statewide licensure at the time of the study, massage therapists were required to be licensed by local jurisdictions including Boston and the surrounding towns where the study took place.
Description of massage intervention
Patients received three visits by the professional massage therapists over the first week after the enrollment. Massage treatments were scheduled based on patient preferences, and the duration was between 15 and 45 minutes; both the duration and the amount of pressure was modified depending on patient comfort. A limited scope of practice was provided to the massage therapists that specified the allowed and disallowed massage modalities and techniques. Allowed techniques were both Swedish and non-Swedish massage including gliding/effleurage, gentle kneading/petrissage, compression, gentle stretching, rocking, light myofascial release, active and/or passive range of motion, warm or cool applications, and use of acupressure points as well as craniosacral holds thought to have calming and centering effects. No forms of friction, deep-tissue massage, or bodywork forms that required movement by the patients were allowed. Specific precautions were followed, which included modifications in pressure, site, and position, depending on clinical considerations. Therapists were asked to avoid massaging areas of known metastases, communicable disease, or recent incisions. Pressure was restricted to gentle pressure if a patient's platelet count was less than 50,000 on any given day. Nonallergenic and fragrance-free lotion and oils were available for use, depending on the preferences of the patient and therapist.
Description of control intervention
The authors wanted to separate out the effect of interacting with a massage therapist from massage itself, so the therapists performed no-touch control interventions, which had no healing intention. Although most of the therapists had experience with energy healing, the therapists were trained to avoid “healing intention” in the no-touch group by using distraction if necessary, created by counting backwards. For the no-touch control intervention, therapists were instructed to be with the patients between 15 and 45 minutes, depending on the patient's tolerance, and to hold their hands about 12 inches over the patient's body. In the usual-care control group, patients completed the same questionnaires but did not receive any visits from the massage therapists.
Study procedures
The oncology clinic electronic database was screened daily and patients were approached who were eligible based on their clinical diagnosis (solid cancer with evidence of metastases) and whether they lived within 25 miles of the hospital. Informed consent was obtained from all participants prior to randomization. Patients were told that the authors were conducting a study of nonpharmacologic treatments intended to improve symptom management. The protocols and procedures were reviewed and approved by the BIDMC Institutional Review Board, the Committee on Clinical Investigations.
Collected data
Data were collected from the patient's medical records including information on pain medications, diagnosis, goals of care, patient's Do Not Resuscitate status, and use of other alternative modalities of care. Data were also collected on patients' clinical status, use of medications, and other medical interventions. The patient's physicians were queried about the patient's expected prognosis for survival at 2 and 6 months using a questionnaire used in the SUPPORT project.1
Data collected by massage therapists before and after interventions
The therapists recorded the patient's anxiety, pain, and alertness using 0–10 scales (visual analogue scale9), and pulse and respiratory rate before and after the interventions. Therapists recorded the amount of time they spent with the patient as well as the time spent using on-body or off-body treatments, the amount of pressure used on the different body areas, the location of the massages, and reasons for terminating either the massage or the no-touch intervention. Patients were asked whether they believed they were in the active treatment arm of the study.
Data collected by study interviewers 1 week and 1 month after enrollment
Data on pain were collected using the pain severity and pain location subscales of the Brief Pain Inventory Short Form.10,11 This tool has been used as an outcome measure in patients with advanced cancer.12 The Pain Severity Subscale consists of four items that assess the worst, least, and average levels of pain within the past 24 hours as well as the current levels of pain. The pain location subscales ask patients to provide a graphic representation of the location of pain. These subscales have documented internal consistency (Cronbach α=0.87) and discriminative validity.11 Using standardized scales, information was also collected on quality of life,13 anxiety,11,14 alertness,11 sleep quality,15 and mood.16 Activities of daily living were measured using an adaptation of the Katz scale.1,17 Patients were asked about the current goals of care and their expectations of the study treatment. Additionally, standard demographic information was collected such as age, sex, race, marital status, education, diagnosis, religion, and importance of spiritual practice.
Monitoring for adverse events
To assess adverse effects, patients were interviewed on the telephone after both the first and third treatments. Patients were questioned about the evidence of any side effects or safety issues related to massage or no-touch intervention.
Statistical analysis
Descriptive statistics were used to quantify patient and caregiver demographics at baseline. Descriptive statistics were also used to quantify treatment characteristics of the massage- and no-touch control patients. To compare the between-group difference in the change from baseline to post-treatment, Kruskal-Wallis tests were used at 1-week follow-up and 1-month follow-up. Analyses followed the intention-to-treat paradigm. Descriptive statistics and analyses were performed using SAS version 9.1.3 (SAS Institute, Cary, NC). As a secondary post hoc analysis, the change in pain score was also examined, comparing the score just prior to the massage to the score after the massage therapy.
Results
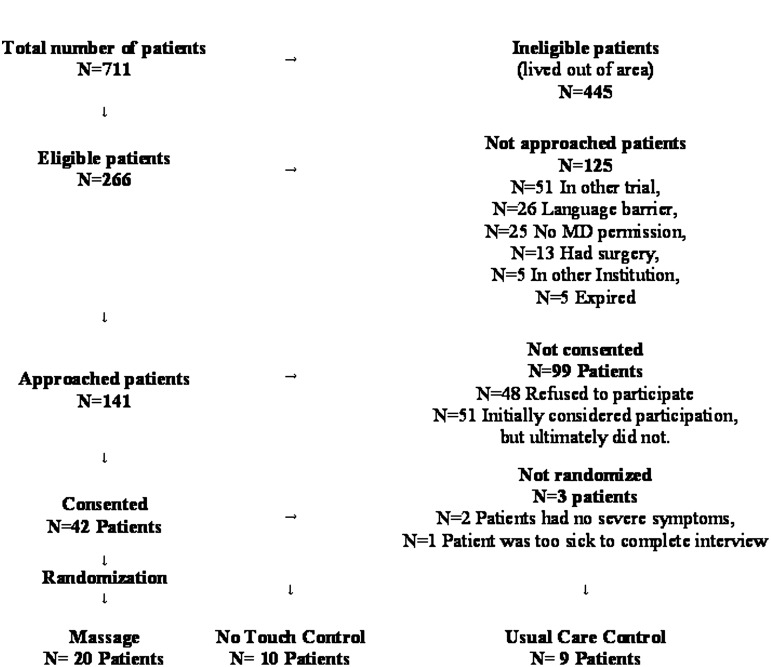
A Consolidated Standards of Reporting Trials (CONSORT) enrollment and randomization summary is shown in Figure 2. Demographic characteristics of the patients can be found in Table 1; they were similar in the massage group (Touch) and control groups (No Touch and Usual Care).
FIG. 2.
Consolidated Standards of Reporting Trials (CONSORT): Enrollment summary.
Table 1.
Demographic Characteristics
| Patient characteristics | Touch N=20 N (%) | No touch N=10 N (%) | Usual care N=9 N (%) | Total N=39 N (%) |
|---|---|---|---|---|
| Age, mean (SD) | 54.9 (12) | 54.9 (10) | 55.6 (9) | 55.1 (11) |
| Gender, female | 17 (85) | 9 (90) | 6 (67) | 32 (82) |
| Ethnicity | ||||
| Hispanic | 0 (0.0) | 1 (10.0) | 0 (0.0) | 1 (2.6) |
| White | 19 (95) | 10 (100) | 8 (89) | 37 (95) |
| Marital status | ||||
| • Married | 13 (65) | 6 (60) | 8 (89) | 27 (69) |
| • Other | 7 (35) | 4 (40) | 1 (11) | 12 (31) |
| Living alone | 3 (15) | 2 (20) | 0 (0) | 5 (13) |
| Not admitted to hospital in the last 12 months | 8 (40) | 6 (60) | 4 (44) | 18 (46) |
| Education | ||||
| • College grad or more | 10 (50) | 6 (60) | 5 (56) | 21 (54) |
| Employment | ||||
| • FT or PT | 5 (25) | 5 (50) | 4 (44) | 14 (36) |
| Household income | ||||
| • NA/refused/DK | 3 (15) | 3 (30) | 1 (11) | 7 (18) |
| • <$50K | 4 (20) | 2 (20) | 1 (11) | 7 (18) |
| • >$50K | 13 (65) | 5 (50) | 7 (78) | 25 (64) |
SD, standard deviation; FT, full time; PT, part time; NA, not applicable; DK, did not know.
Prior to randomization, nearly 80% of the patients preferred to be in the professional massage intervention group. The majority of patients had experience with massage. The most common diagnosis was breast cancer, affecting 22 of the 39 randomized patients (56%). Five (5) patients had colon cancer and 3 each had pancreatic or ovarian cancer. Comorbid illnesses were uncommon but included diabetes (N=2), chronic lung disease (N=1), mild liver disease (N=1), and connective tissue disease (N=1). Most patients had a good functional status, all patients were able to toilet independently, and 30 of 42 patients were able to bathe without assistance. Only 4 had difficulty ambulating and required assistance.
The characteristics of the interventions are summarized in Table 2; the duration and location of the Touch and No Touch interventions were statistically similar in the groups.
Table 2.
Intervention Characteristics
| Massage therapy characteristics (N=56) | Mean (SD) |
|---|---|
| Duration in minutes with patient | 68 (16) |
| Treatment duration in minutes | 46 (8) |
| Average pressure used (1=lightest, 5=deepest) | 2.1 (0.7) |
| Deepest pressure used (1=lightest, 5=deepest) | 2.8 (0.9) |
| Areas of body that received massage | % |
| Head | 62 |
| Face | 34 |
| Neck | 89 |
| Shoulder | 98 |
| Upper arm | 79 |
| Forearm | 77 |
| Hand | 79 |
| Chest | 28 |
| Abdomen | 15 |
| Upper back | 98 |
| Midback | 94 |
| Lower back | 89 |
| Hip | 53 |
| Thigh | 53 |
| Knee | 62 |
| Lower leg | 62 |
| Feet/foot | 79 |
| No-touch characteristics (N=23) | Mean (SD) |
| Duration in minutes with patient | 56 (14) |
| Treatment duration in minutes | 36 (8) |
| Areas of body over which hands were placed | % |
| Head | 96 |
| Chest/abdomen | 100 |
| Hips | 100 |
| Knees | 100 |
| Feet | 100 |
| Upper back | 74 |
| Lower back | 74 |
SD, standard deviation.
Table 3 shows the changes from baseline to 1-week and 1-month follow-up in the primary outcomes (pain, anxiety, and alertness) and in the secondary outcomes (quality of life and sleep) among patients randomized to the massage, No Touch, and control groups. There were no significant changes from baseline to 1-week or 1-month follow-ups in the primary outcomes (pain, anxiety, and alertness). Among the secondary outcomes, there was significant improvement in quality of life of the patients in the massage group compared to the control groups at 1 week (Physical well-being p=0.005 and McGill Total p=0.03). However, these differences were no longer significant at the 1-month follow-up.
Table 3.
Changes in Primary and Secondary Outcomes from Baseline to 1 Week and 1 Month in the Touch- (Massage), No-Touch Interventions, and Usual-Care Groups
| Touch (N=20) | No touch (N=10) | Usual care (N=9) | p-Value | ||
|---|---|---|---|---|---|
| Primary outcomesa | |||||
| Pain | 1 week | 0 (−2, 1) | 0 (−1, 2) | 0 (−3, 2) | 0.65 |
| 1 month | 0 (−1, 0) | 0 (−1.5, 0) | −2 (−2,−1) | 0.14 | |
| Anxiety | 1 week | 0 (−3, 0) | 0 (−3, 0) | 0 (−2, 0) | 0.92 |
| 1 month | 0 (−2, 0) | 0 (−1.5, 1) | 0 (−3, 0) | 0.85 | |
| Alertness | 1 week | 0 (0, 0) | 0 (−0.5, 0) | 1 (0, 2) | 0.10 |
| 1 month | 0 (−1, 0) | 0 (−1.5, 0) | 0 (0, 1) | 0.44 | |
| Secondary outcomesb | |||||
| Quality of life | |||||
| Physical well-being | 1 week | 1 (0, 2) | −0.5 (−2, 0.5) | 0 (−2, 0) | 0.005 |
| 1 month | 0 (−1, 1) | 0 (−3.5, 0) | 0 (0,0) | 0.27 | |
| Psychological well-being | 1 week | 1.125 (0, 2) | 0.25 (−0.5, 2) | 0 (0, 0.75) | 0.15 |
| 1 month | −0.125 (−0.5, 0.5) | 0.25 (−1.25, 1.5) | −0.75 (0,1.5) | 0.23 | |
| McGill total | 1 week | 0.45 (0, 1.23) | 0 (−0.66, 0.28) | 0 (−0.57, 0) | 0.03 |
| 1 month | 0 (−0.42, 0.3) | −0.18 (−1.29, 0.13) | 0 (0,0.58) | 0.33 | |
| Sleep | 1 week | −3.5 (−9, 0) | 0 (−7, 9) | −0.5 (−4, 1) | 0.25 |
| 1 month | −4 (−12, 0) | 0 (−12, 10) | 0 (−15,12) | 0.49 | |
Data reported as median (Q1, Q3).
Primary outcomes:
Pain 0=no pain to 10=most severe pain;
Anxiety 0=no anxiety to 10=most severe anxiety;
Alertness 0=not at all alert to 10=most alert.
Secondary outcomes:
Physical well-being over past 2 days (0=physically terrible – 10=physically well)
Psychological well-being over past 2 days (depressed, nervous/worried, sad, terrified of future) (0=always/extremely – 10=never/not at all) in other words (0=negative/worst – 10=positive/best)
Quality of Life (McGill Total); Mean of five submeasures (but not overall) (0=negative-10=positive)
Sleep (Richards-Campbell) 0=best sleep –50=worst sleep
Comparisons of the pre- and postintervention measures of the primary outcomes are shown in Table 4. In unadjusted analyses, pain decreased more after massage than after the No Touch intervention (p=0.04). However, when adjusted for the baseline value, the difference was no longer significant (p=0.18). There was no significant change in anxiety and alertness after either massage treatment or the No Touch intervention.
Table 4.
Pre–Post-treatment Measurements of the Primary Outcomes Within the Interventions by the Professional Therapists: Touch- (Massage) and No-Touch Interventions
| |
Touch |
No touch |
|
|
||
|---|---|---|---|---|---|---|
| |
N=55 |
N=23 |
p-Value |
|||
| Baseline mean±SD | Difference from baseline mean (95% CI) | Baseline mean±SD | Difference from baseline mean (95% CI) | Unadjusted | Adjusted by baseline | |
| Paina | 3.4±3.1 | −1.4 (−1.9, −0.9) | 1.9±2.2 | −0.5 (−1.2, 0.1) | 0.04 | 0.18 |
| Anxietyb | 3.1±2.7 | −2.0 (−2.6, −1.3) | 3.6±2.9 | −1.7 (−2.9, −0.5) | 0.72 | 0.80 |
| Alertnessc | 8.5±1.6 | −0.9 (−1.7, −0.2) | 9.3±1.5 | −0.5 (−1.2, 0.3) | 0.40 | 0.48 |
0=no pain to 10=most severe pain.
0=no anxiety to 10=most severe anxiety.
0=not at all alert to 10=most alert.
SD, standard deviation; CI, confidence interval.
Adverse events
There were no study-related adverse events. One (1) patient died during the study in the Usual Care control group. The patient was hospitalized on study day 5 and died 3 days later with comfort measures for metastatic ovarian cancer. There were two hospitalizations among patients receiving massage. One (1) patient was hospitalized with acute renal failure thought to be secondary to use of computed tomography contrast, while the second was hospitalized with increased pain and shortness of breath due to new pulmonary metastases. In the massage group, 1 patient had increased shortness of breath and 1 patient had increased pain following their second massage, but this was not thought to be due to the massage. There were no hospitalizations or worsening symptoms among patients receiving the No Touch intervention.
Discussion
This pilot randomized controlled trial suggests that providing therapeutic massage for patients with advanced cancer is feasible in the home setting and improves quality of life at 1-week follow-up, but the effect did not persist at 1 month. The post-treatment results showed that pain may decrease after therapeutic massage, which was not observed in the No Touch and Usual Care control groups. However, the difference in pain was no longer significant when adjusted for the baseline value.
Other investigators have reported decrease in pain after six shorter in-hospital or hospice massage therapy treatments3; however they also reported beneficial effects in their control intervention groups. The current study did not find significant changes in the other primary outcomes: anxiety and alertness. However, there were trends toward improvement in anxiety and alertness in the massage therapy group compared to the controls at the 1-week follow-up; the lack of significance may have been related to the relatively small sample size. A study with a larger sample size reported significant immediate positive mood changes and improved quality of life after massage3; however, in their study the control was simple touch, the duration of the intervention was 30 minutes, patients were in hospice, and there was no usual-care control group. Possibly, massage is of more benefit when provided in the context of palliative care, as was done in the study by Kutner et al.3 Similarly, the current study showed modest improvement in sleep quality in the massage group, and improvements were not observed in the control groups, but again these results were not significant, likely due to the small number of patients in the study.
Similar to the abovementioned randomized controlled trial,3 in the current study the quality of life of the patients improved significantly compared to control patients at 1-week follow-up. Together with these other data, the current study's results suggest that massages provided by therapists may have beneficial short-term effects on the quality of life of patients with advanced cancer.
This study had several limitations. Our small sample size limited our statistical power. The authors also were not able to blind our pre–post intervention data collection. Additionally, patient expectation for better outcome from massage might have biased the study against the control. Finally, heterogeneity in the type and stage of cancer of this study's patients may have resulted in variation of the effects of the interventions.
Conclusions
In conclusion, the results of this pilot randomized controlled trial among patients with advanced cancer support the hypothesis that providing massage and no-touch control interventions at home by professional therapists is feasible. Therapeutic massage resulted in significant improvement in short-term quality of life of these patients near the end of life. These results suggest that providing therapeutic massage may be associated with further beneficial effects, such as less pain and improved sleep quality, but larger randomized controlled trials are needed to substantiate these findings.
Acknowledgments
The authors thank the massage therapists (in alphabetical order) for providing therapeutic massage for the patients in this study: Laura C. Barricelli, LMT, Cynthia Ann Gillan, MA, LMT, Karen Ingwersen, LMT, MS, Diane R. Krause, LMT, Rita Rice, MS, MDiv, LMT, and Mary Sbuttoni, LMT, NCTMB. The authors also thank the study team, staffs, physicians, nurses, and all patients and families for their time and cooperation. Grant support was provided by the National Institutes of Health 5 R21 CA098487 (Dr. Russell S. Phillips) and 5 K24 AT00589 (Dr. Russell S. Phillips).
Disclosure Statement
No competing financial interests exist.
References
- 1.SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients: The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) JAMA. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 2.Toth M. Kahn J. Walton T, et al. Therapeutic massage intervention for hospitalized patients with cancer: Pilot study. J Altern Complement Med. 2003;9:117–124. [Google Scholar]
- 3.Kutner JS. Smith MC. Corbin L, et al. Massage therapy versus simple touch to improve pain and mood in patients with advanced cancer: A randomized trial. Ann Intern Med. 2008;149:369–379. doi: 10.7326/0003-4819-149-6-200809160-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilkinson S. Barnes K. Storey L. Massage for symptom relief in patients with cancer: Systematic review. J Adv Nurs. 2008;63:430–439. doi: 10.1111/j.1365-2648.2008.04712.x. [DOI] [PubMed] [Google Scholar]
- 5.Ernst E. Massage therapy for cancer palliation and supportive care: A systematic review of randomised clinical trials. Support Care Cancer. 2009;17:333–337. doi: 10.1007/s00520-008-0569-z. [DOI] [PubMed] [Google Scholar]
- 6.Soden K. Vincent K. Craske S, et al. A randomized controlled trial of aromatherapy massage in a hospice setting. Palliat Med. 2004;18:87–92. doi: 10.1191/0269216304pm874oa. [DOI] [PubMed] [Google Scholar]
- 7.Smith MC. Yamashita TE. Bryant LL, et al. Providing massage therapy for people with advanced cancer: What to expect. J Altern Complement Med. 2009;15:367–371. doi: 10.1089/acm.2008.0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collinge W. Kahn J. Yarnold P, et al. Couples and cancer: Feasibility of brief instruction in massage and touch therapy to build caregiver efficacy. J Soc Integr Oncol. 2007;5:147–154. doi: 10.2310/7200.2007.013. l. [DOI] [PubMed] [Google Scholar]
- 9.Ohnhaus EE. Adler R. Methodological problems in the measurement of pain: A comparison between the verbal rating scale and the visual analogue scale. Pain. 1975;1:379–384. doi: 10.1016/0304-3959(75)90075-5. [DOI] [PubMed] [Google Scholar]
- 10.Cleeland CS. Measurement of pain by subjective report. In: Chapman CR, editor; Loeser JD, editor. Advances in Pain Research and Therapy. New York: Raven Press; 1989. p. 16. [Google Scholar]
- 11.Cleeland CS. Ryan KM. Pain assessment: Global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129–138. [PubMed] [Google Scholar]
- 12.Twycross R. Harcourt J. Bergl S. A survey of pain in patients with advanced cancer. J Pain Symptom Manage. 1996;12:273–282. doi: 10.1016/s0885-3924(96)00149-2. [DOI] [PubMed] [Google Scholar]
- 13.Cohen S. Kamarck T. Mermelstein R. A global measure of perceived stress. J Health Soc Beh. 1983;24:385–396. [PubMed] [Google Scholar]
- 14.Spielberger C. Palo Alto, CA: Consulting Psychologists Press Inc.; 1983. Manual for the State-Trait Anxiety Inventory (Form Y) [Google Scholar]
- 15.Richards KC. O'Sullivan PS. Phillips RL. Measurement of sleep in critically ill patients. J Nurs Measure. 2000;8:131–144. [PubMed] [Google Scholar]
- 16.Shacham S. A shortened version of the Profile of Mood States. J Pers Assess. 1983;47:305–306. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- 17.Katz S. Ford AB. Moskowitz RW, et al. Studies of illness of the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]