Abstract
Study Objective:
To determine if self-reported sleep duration was associated with weight-control behaviors among US high school students.
Design:
National Youth Risk Behavior Survey.
Setting:
United States, 2007.
Participants:
US high school students (N = 12,087).
Measurements:
Students were asked if they had engaged in several weight-control behaviors during the 30 days before the survey to lose or maintain weight. Self-reported sleep duration categories included very short (≤ 5 h), short (6 or 7 h), referent moderate (8 or 9 h), and long (≥ 10 h). Sex-specific logistic regression analyses with race/ethnicity, grade, and body mass index category as covariates were conducted using SUDAAN to account for complex study design.
Results:
Approximately half the students reported short sleep duration (51.8% of males and 54.3% of females), whereas very short sleep durations were reported by another 14.8% of males and 16.9% of females. Among males, very short sleepers were significantly (P < 0.05) more likely than moderate sleepers to report dieting (36.3% versus 26.1%), fasting (14.2% versus 4.3%), and purging (4.3% versus 1.1%) to lose or maintain weight during the 30 days before the survey. Among females, the respective very short, short, and moderate sleepers varied (P < 0.05) in dieting (59.9%, 55.0%, and 47.5% respectively), fasting (28.3%, 15.2%, and 10.3%, respectively), and taking diet pills (13.3%, 6.8%, and 4.3%, respectively). Prevalence of purging was significantly higher only for very short sleepers (12.3%, 6.0%, and 3.9%, respectively).
Conclusion:
Self-reported short sleep duration was associated with dieting and three unhealthy weight-control behaviors in this population. If our findings are confirmed, intervention studies should be conducted to examine the effect of educational interventions.
Citation:
Wheaton AG; Perry GS; Chapman DP; Croft JB. Self-reported sleep duration and weight-control strategies among US high school students. SLEEP 2013;36(8):1139-1145.
Keywords: Adolescence, sleep, weight management
INTRODUCTION
At a time when adolescents need more than 9 h of sleep per night for optimal health and well-being,1 social factors (such as 24-h access to cell phones and the Internet) and biological factors (such as delayed circadian rhythms) may combine to delay bedtimes,2–4 whereas school start times often advance wake-up times.5 As a result, adolescent students are often sleep deprived.6 Short sleep duration in adolescents has been associated with lowered academic performance, depressive mood, and behavioral problems.4,7–9 Shorter sleep duration has also been found to be associated with various risk behaviors, including smoking and alcohol use.8,10–12
Eating disorders often present during adolescence13 and are associated with a variety of unhealthy behaviors that include purging behaviors (e.g., self-induced vomiting or misuse of laxatives), fasting, or otherwise restricting food intake. The lifetime prevalence of eating disorders (anorexia nervosa, bulimia nervosa, or binge eating disorder) in the United States is estimated to be approximately 6% for women and 3% for men,14 but the prevalence of disordered weight-control behaviors and symptoms that do not meet the stringent criteria for an eating disorder diagnosis is likely much higher.15 Sleep complaints are common in young women with eating disorders and may predict the development of psychological disorders, such as depression or anxiety, that are frequently associated with eating disorders.16
To our knowledge, there is no literature on the possible association between sleep duration and weight-control strategies in the nonclinical adolescent population. Our objectives were to determine if self-reported short sleep duration was associated with perception of body weight or with the prevalence of several weight-control behaviors among US high school students.
METHODS
We used data from the 2007 National Youth Risk Behavior Survey (YRBS). The Youth Risk Behavior Surveillance System was developed by the Division of Adolescent and School Health, Centers for Disease Control and Prevention (CDC), to monitor the prevalence of youth health-risk behaviors, including unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual behaviors that result in sexually transmitted diseases, dietary behaviors, and physical activity behaviors. Students complete the anonymous, self-administered questionnaires during a single class period. Because the national YRBS is a public-use dataset, this research was exempt from review by an institutional review board. The National YRBS uses a three-stage cluster design to obtain a representative sample of high school students (9th through 12th grades, predominantly 14-18 y of age). Hispanic and black youth were oversampled in 2007. Sampling strategies have been reported elsewhere.17 Of 195 schools sampled, 157 (81%) participated; 84% of the students sampled at the participating schools submitted useable questionnaires. The overall response rate for the 2007 YRBS was 68%.
Usable data were available from 14,041 respondents to the 2007 National YRBS. Respondents who were not in grades 9 through 12 or for whom grade data were missing (n = 83), who did not identify their sex (n = 13), or who did not respond to the sleep duration question (n = 1,887) were excluded from the analysis. The final sample size for data analysis included 12,087 study respondents (85.8%).
Measures
Self-reported sleep duration was ascertained by the question, “On an average school night, how many h of sleep do you get?” Possible responses were “4 or less h,” “5 h,” “6 h,” “7 h,” “8 h,” “9 h,” or “10 or more h.” We formed four sleep duration categories: very short sleep (≤ 5 h), short sleep (6 or 7 h), moderate sleep (8 or 9 h), and long sleep (≥ 10 h). Although 9.25 h is often identified as the usual sleep need for adolescents,1 this sleep duration was obtained using polysomnographic data. At least one study, however, has found that adolescents using sleep diaries tend to underestimate the sleep they actually obtain as measured by actigraphy.18 Due to the uncertainty surrounding this issue, we chose 8 or 9 h as our referent group and labeled it as moderate rather than optimal.
Students were asked, “Which of the following are you trying to do about your weight?” Possible responses were “lose weight”, “gain weight”, “stay the same weight”, or “I am not trying to do anything about my weight.” Students were then asked if they had engaged in various behaviors to lose weight or keep from gaining weight during the 30 days before the survey. These behaviors included exercising; “eating less food, fewer calories, or foods low in fat” (dieting); and unhealthy weight-control behaviors such as “going without eating for 24 h or more (also called fasting)”; “taking diet pills, powders, or liquids without a doctor's advice”; and “vomiting or taking laxatives” (purging).
Because body image may affect weight-control behaviors, we compared students' objective weight status (based on body mass index, BMI) to their perceived weight status to assess how accurately they perceived their own weight status. BMI (kg/ m2) was calculated based on self-reported weight in pounds and height in inches. BMI percentile was generated for age and sex based on the 2000 CDC Growth Charts.19 We defined BMI categories, which were based on the following BMI percentiles: underweight (or at risk for underweight) (≤ 15th percentile), normal weight (> 15th percentile and < 85th percentile), overweight (≥ 85th percentile and < 95th percentile), and obese (≥ 95th percentile).20 BMI percentiles were set to missing if weight, height, sex, or age were not reported. BMI percentiles were also set to missing if weight, height, or BMI were outside the biologically plausible limits defined by the Division of Nutrition and Physical Activity, CDC.19
Participants were also asked, “How do you describe your weight?” Possible responses were “very underweight”; “slightly underweight”; “about the right weight”; “slightly overweight”; or “very overweight”. For our analysis, “very underweight” and “slightly underweight” were combined in one perceived weight category labeled “underweight”, whereas “slightly overweight” and “very overweight” were combined in another perceived weight category labeled “overweight.” Students who perceived themselves as thinner than their objective weight status (BMI category) were defined as underestimators. Underestimators included students who described themselves as underweight but were in the normal weight, overweight, or obese BMI catego-ries and students who described themselves as normal weight but were in the overweight or obese BMI categories. Students who perceived themselves as heavier than their objective weight status were defined as overestimators. Overestimators included students who described themselves as overweight but were in the normal weight or underweight BMI categories and students who described themselves as normal weight but were in the underweight BMI category. Students whose perceived weight status was comparable to their BMI category were defined as accurate estimators.
Statistical Analysis
All analyses were conducted using SAS-callable SUDAAN (version 10.0.0, RTI International, Research Triangle Park, NC) to account for the complex sampling design. Records were weighted based on student sex, race/ethnicity, and grade in school to adjust for student nonresponse and oversampling.17 Male and female students were analyzed separately due to expected sex-based differences in weight-control behaviors. Prevalence of weight overestimators or underestimators, attempting to lose or maintain weight, and the weight-control behaviors (exercising, dieting, fasting, taking diet pills, and purging) were assessed within sleep duration categories. Odds ratios (OR) and 95% confidence intervals (CI) adjusted for race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other/multi-racial [non-Hispanic]) and grade were calculated in multivariable logistic regression models for the likelihood of each outcome for each sleep duration category. Logistic regression models for the weight-control behaviors were also adjusted for BMI category. We used the moderate sleep duration category (8 or 9 h per night) as the referent. We also tested for linear trends across sleep duration categories using the Wald F-statistic. A P value < 0.05 was considered statistically significant for all tests.
RESULTS
Study Population
Students were predominantly white (63.2% of males, 62.3% of females), with approximately 15% black and 15% Hispanic students (Table 1). Only 31.4% of male students and 27.4% of female students reported sleeping 8 or 9 h (moderate sleep) on an average school night. Approximately half of students (51.8% of males and 54.3% of females) were short sleepers (6 or 7 h). Five h or less (very short sleep) was reported by 14.8% of males and 16.9% of females. Ten or more h (long sleep) was reported by a very small proportion of our sample (2.0% of male students and 1.3% of female students). Self-reported sleep duration varied by race/ethnicity and school grade. Among male students, non-Hispanic blacks (25.5%) were less likely to report moderate sleep duration than non-Hispanic whites (32.7%; pair wise t-value = 3.3, P = 0.002) or Hispanics (32.8%; pairwise tvalue = 2.7, P = 0.011). There was no significant difference in prevalence of moderate sleep duration by race/ethnicity among female students. Among male students, the proportion reporting moderate sleep duration was strongly associated with grade in school (9th: 42.5%, 10th: 33.3%, 11th: 25.9%, 12th: 20.3%). All between-grade differences were statistically significant (t-value > 2.6, P < 0.011). Among female students, the proportion was also strongly associated with grade in school (9th: 37.7%, 10th: 27.6%, 11th: 21.9%, 12th: 20.6%), although the difference between 11th and 12th grades was not statistically significant.
Table 1.
Characteristics of US high school students who responded to sleep duration question in the 2007 National Youth Risk Behavior Survey (YRBS)
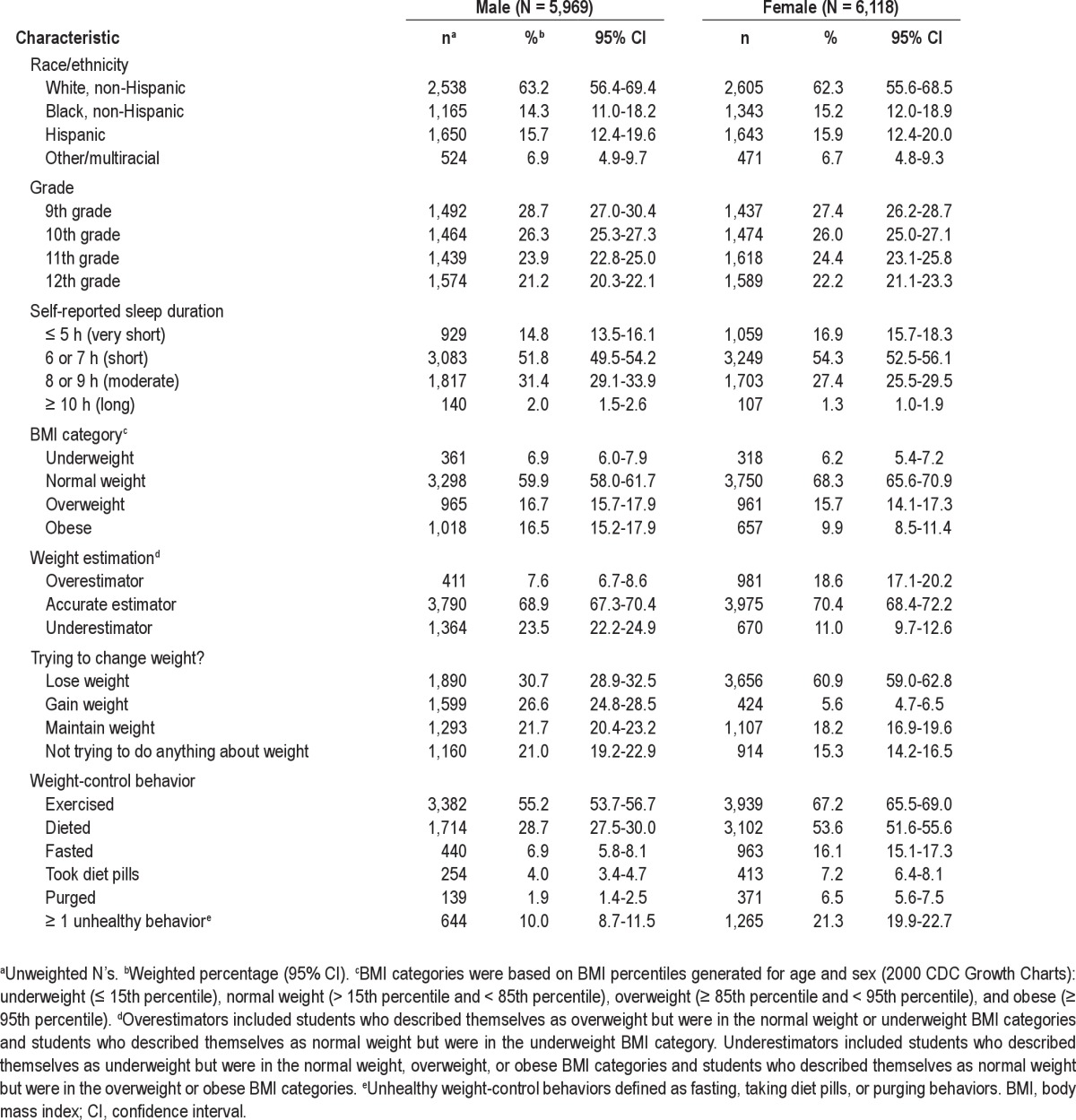
More than half of the students were in the normal weight category (59.9% of males and 68.3% of females), and approximately one in three were overweight or obese (33.2% of males and 25.5% of females) (Table 1). Most students were accurate estimators of their weight status (68.9% of males and 70.4% of females); however, females were more likely to be overes-timators of their weight status than males (18.6% versus 7.6%, respectively). Only 21.0% of males and 15.3% of females were not trying to do anything about their weight. There were 60.9% of female students and 30.7% of male students who were trying to lose weight; another 18.2% of females and 21.7% of males were trying to maintain their current weight. For each of the five weight-control behaviors evaluated, females were more likely to report engaging in the behavior than their male counterparts. The most common weight loss or maintenance behaviors were exercising (67.2% of females and 55.2% of males) and dieting (53.6% of females and 28.7% of males). At least one unhealthy weight-control behavior (fasting, taking diet pills, or purging) was reported by 10.0% of males and 21.3% of females.
Self-Reported Sleep Duration, Weight Status Estimation, and Weight-Control Behaviors
The sex-specific prevalence of overweight/obesity, weight status estimation, and various weight-control behaviors by sleep duration category are presented in Table 2. Among male students, overweight/obesity did not differ significantly by sleep duration. However, female students who were short sleepers (6 or 7 h) were less likely to be overweight/obese compared with the referent group (OR = 0.8; 95% CI = 0.7-1.0). Although unadjusted prevalences of overestimating weight status, underestimating weight status, and attempting to lose or maintain weight generally declined as sleep duration increased to the referent (8 or 9 h) in both males and females, these relationships failed to reach statistical significance among male students after adjustment for race/ethnicity and grade in multivariable logistic regression models. Long sleepers were more likely to be weight overestimators among male students (OR = 2.3; 95% CI = 1.1-5.1) and weight underestimators among female students (OR = 2.2; 95% CI = 1.1-4.6). Among female students, the odds of attempting to lose or maintain weight was higher among short sleepers compared to the referent, although there was no difference between the very short sleepers (≤ 5 h) and the referent group.
Table 2.
Prevalence and odds ratio of weight-estimation status and weight-control behaviors by sleep duration category
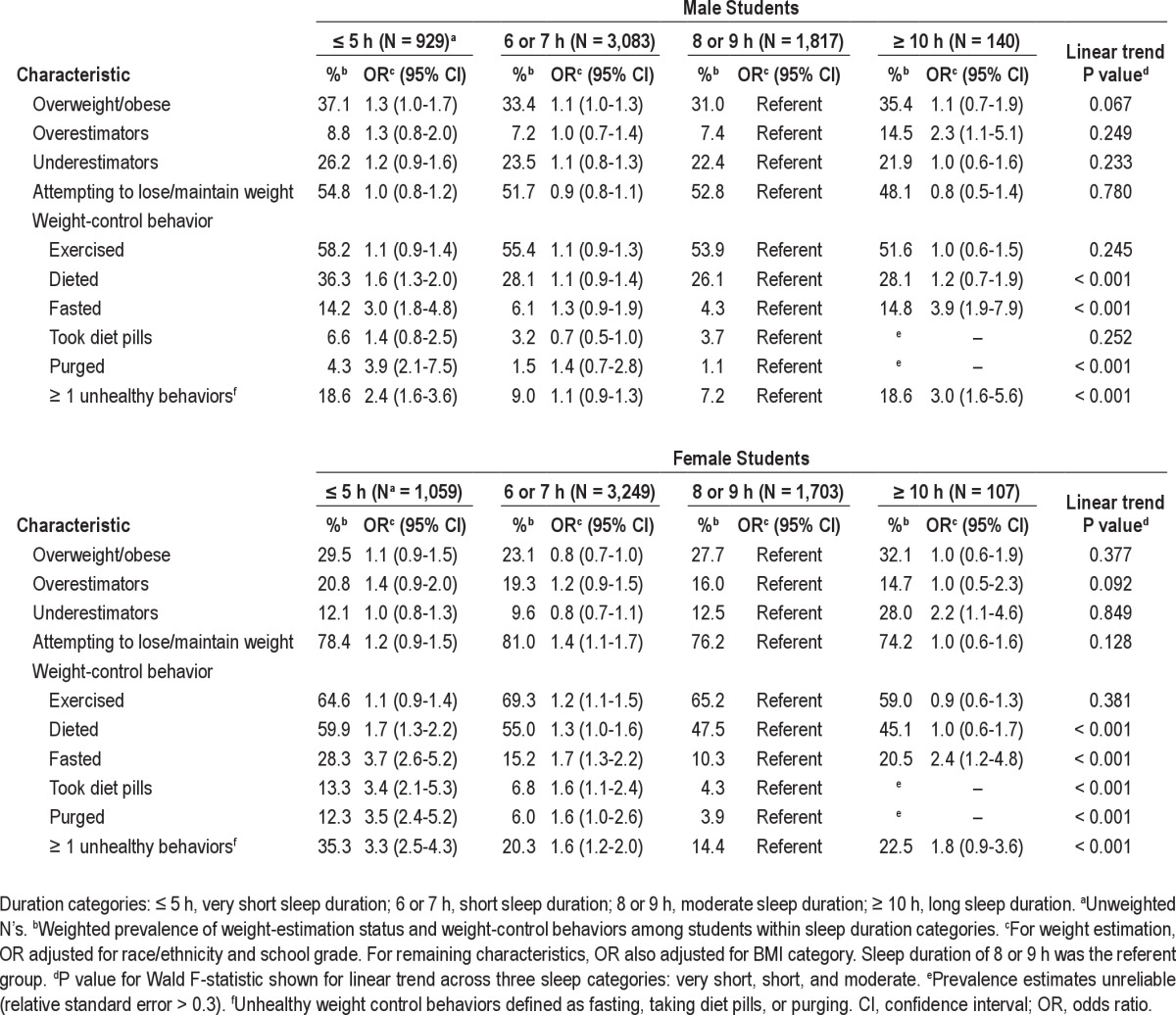
Among male students, self-reported sleep duration was inversely associated with dieting, fasting, and purging. Very short sleepers were significantly more likely than moderate sleepers to report dieting (OR = 1.6; 95% CI = 1.3-2.0), fasting (OR = 3.0; 95% CI = 1.8-4.8), and purging (OR = 3.9; 95% CI = 2.1-7.5) to lose or maintain weight during the 30 days before the survey. Short sleepers were less likely to report taking diet pills than moderate sleepers (OR = 0.7; 95% CI = 0.5-1.0). Among males, 18.6% of very short sleepers reported at least one of the unhealthy weight-control behaviors (fasting, taking diet pills, or purging) during the 30 days before the survey compared with 7.2% of moderate sleepers (OR = 2.4; 95% CI = 1.6-3.6). Long sleepers were also more likely to report fasting (OR = 3.9; 95% CI = 1.9-7.9) or at least one of the unhealthy weight-control behaviors (OR = 3.0; 95% CI = 1.6-5.6) compared with moderate sleepers.
Among female students, self-reported sleep duration was inversely associated (linear trend) with all weight-control behaviors except exercising (Table 2). Short sleepers were more likely to report exercising to lose or maintain weight than moderate sleepers (OR = 1.2; 95% CI = 1.1-1.5), but very short sleepers were no more likely to report this behavior than the moderate sleepers. Very short sleepers and short sleepers were significantly more likely than moderate sleepers to report dieting (OR = 1.7; 95% CI = 1.3-2.2 and OR = 1.3; 95% CI = 1.0-1.6, respectively), fasting (OR = 3.7; 95% CI = 2.6-5.2 and OR = 1.7; 95% CI = 1.3-2.2, respectively), and taking diet pills (OR = 3.4; 95% CI = 2.1-5.3 and OR = 1.6; 95% CI = 1.1-2.4, respectively). Prevalence of purging was significantly higher only for very short sleepers (OR = 3.5; 95% CI = 2.4-5.2). Long sleepers were more likely to report fasting (OR = 2.4; 95% CI = 1.2-4.8) compared to moderate sleepers. More than a third (35.3%; OR = 3.3; 95% CI = 2.5-4.3) of very short sleepers and 20.3% (OR = 1.6; 95% CI = 1.2-2.0) of short sleepers reported at least one of the three unhealthy weight-control behaviors during the 30 days before the survey, compared with 14.4% of moderate sleepers.
DISCUSSION
Obesity is a growing problem among adolescents. A substantial proportion of adolescents are attempting to lose or control their weight through healthy and unhealthy means. Fifty percent of the male students and four in five female students in our study were attempting to lose or maintain their weight, whereas 10.0% of male and 21.3% of female students reported that they had engaged in one of the unhealthy weight-control behaviors in the past mo. So that effective interventions to protect adolescent health can be implemented, possible targets for such interventions must first be identified. Lack of sleep may be one of those targets.
Two-thirds of high school students (66.6% of males and 71.2% of females) reported getting less than 8 h of sleep on school nights. This is comparable to the findings of the 2006 Sleep in America Poll conducted by the National Sleep Foundation.21 We found that very short sleep duration was associated with an increased prevalence of weight-control behaviors, especially unhealthy weight-control behaviors, in both male and female high school students. Among female students, a self-reported sleep duration of 6 to 7 h was also associated with an increased prevalence of most weight-control behaviors, even though this group was the least likely to be overweight or obese. We did not, however, find that sleep duration was associated with how students perceived their weight. Our results are in contrast with those of a study of Japanese adolescent girls that found that girls who overestimated their weight were more likely to sleep less than 7 h per night and to go to bed after 11:00 than girls whose perceived weight was more in line with their actual BMI.22
We are not aware of any previous investigations of the relationship of sleep with weight-control behaviors in the general population. Past studies have investigated the prevalence of sleep complaints, primarily insomnia, in patients with eating disorders. Sleep complaints are common in patients with anorexia nervosa.23 Although several polysomnographic studies have observed reduced overall sleep duration, reduced slow wave and rapid eye movement sleep, and low sleep efficiency in patients with anorexia compared with control patients, others have found no difference in sleep patterns.24–27 In a small Israeli study using actigraphy to measure sleep parameters, no difference in actigraphy measurements was found between patients with anorexia and control patients, although individuals with anorexia reported more difficulty falling asleep, more midsleep awakenings, and excessive daytime sleepiness.23 A similar study in women with bulimia nervosa (binge eating, followed by purging) found that the patients with bulimia were more likely to report difficulty falling asleep and waking up too early, as well as more excessive daytime sleepiness. In contrast with the nonsignificant actigraphy findings in individuals with anorexia, that study found that patients with bulimia fell asleep more than 1 h later and woke up about 1 h later than control patients, possibly due to the increased likelihood of bulimic behaviors during the evening hours.28 In a study of 400 women in whom an eating disorder had been diagnosed, half (50.3%) reported sleep disturbances, with a higher prevalence in patients exhibiting binge eating/purging behavior.16 A novel finding in our study was that long sleepers were more likely to report fasting among both male and female students. Long sleep duration has been linked to many health risks among adults, however, and may be a sign of depression.
Various mechanisms could contribute to the strong association we saw between self-reported short sleep duration and unhealthy weight-control behaviors. First, the weight-control behaviors could lead to shorter sleep. Chronic weight loss may cause biochemical changes that promote wakefulness. Hyperactivity is common in patients with anorexia, characterized by prolonged weight loss.29 Starvation results in sleep fragmentation and reduced slow wave sleep, possibly by alteration of levels of peptides involved in sleep regulation, such as leptin, orexin, and cholecystokinin. Weight restoration in patients with restricting anorexia results in deeper sleep.30 Further, a common adverse effect of many appetite suppressants is insomnia. Ephedrine and phentermine have been widely used as appetite suppressants and are both closely related to amphetamine, a stimulant with wake-promoting effects. Caffeine, a known stimulant, is also an ingredient in some preparations.
Sleep deprivation may contribute to impaired cognition and depressed mood, and thereby increase susceptibility to engaging in risky behaviors. Rather than merely being a consequence of depression, insomnia predicts depressive disorders. 31 Among adolescents, shorter weekday sleep duration has been found to be associated with increased depressive symptoms and overall poor mental health.8,32 As a result of reduced cognition and mood, sleep-deprived adolescents may not consider the possible consequences of their risky behavior. Diagnoses of depression and anxiety are common in patients with an eating disorder. Spindler and Milos found that frequency of binge eating, purging, and dieting was associated with anxiety disorders.33 Studies have shown that anxiety is associated with sleep complaints.34,35
The association between sleep and eating-disordered behaviors may not be a causal one; rather, a common factor may contribute to the development of both conditions. One such factor may be personality. A large cross-sectional study found that short sleep duration (≤ 6 h) was associated with high neuroticism and high self-criticism, after controlling for sociodemographic variables, psychiatric conditions, medical conditions, sedating medications, and broad personality dimensions.36 In a metaanalysis evaluating the association between personality and eating disorders, anorexia nervosa and bulimia nervosa were consistently characterized by perfectionism, obsessive-compulsiveness, and neuroticism, with differences in constraint/impulsivity (high constraint in anorexia, high impulsivity in bulimia) and novelty seeking (low in anorexia, high in bulimia).37 Individuals with insomnia tend to display similar personality traits, including high neuroticism, perfectionism, and internalization.38
It is not possible to determine causality due to the cross-sectional nature of the survey. Another drawback is that self-reported sleep duration was the only sleep-related question asked of the high school students. Future investigations should include questions related to sleep quality and sleep disorders, especially insomnia, as well as asking about sleep duration on weekend nights, circadian disorders, or circadian rhythm type (morningness-eveningness). A limitation of the study was the necessary reliance on self-reported sleep duration, height and weight for BMI calculation, and weight-control behaviors. Adults generally overestimate sleep duration,39,40 but one study comparing sleep duration from sleep diaries and actigraphy among adolescents found that the study participants underes-timated their sleep duration.18 However, the difference was on the order of 30 min. Adolescents tend to underestimate weight and overestimate height, with weight being underestimated more by overweight adolescents.41,42 Although the questions assessing weight-control behaviors have not been validated, the test-retest reliability is moderate.43 Kappa values ranged from approximately 40% for the unhealthy weight-control behaviors to almost 60% for the more general questions (e.g., trying to lose weight).43
CONCLUSION
We observed a relationship between self-reported short sleep duration and several weight-control behaviors. Although an association was found between sleep duration and dieting, which may be considered a relatively healthy weight-control behavior, the association with the unhealthy weight-control behaviors was even stronger. These results provide further evidence that inadequate sleep may contribute to increased risky behaviors among adolescents. Because this is the first study to document an association between short sleep duration and weight-control behaviors in the general adolescent population, more studies to confirm these results are warranted. If our findings are confirmed, intervention studies should be conducted to examine the effect of educational interventions that target sleep hygiene.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Dr. Wheaton was supported through a cooperative agreement between the Association for Prevention Teaching and Research (APTR) and the Centers for Disease Control and Prevention (CDC), award number 3U50CD300860. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Parts of this manuscript were presented at the American Public Health Association's 138th Annual Meeting and Exposition in Denver, CO on November 10, 2010.
REFERENCES
- 1.Carskadon MA, Harvey K, Duke P, Anders TF, Litt IF, Dement WC. Pubertal changes in daytime sleepiness. Sleep. 1979;2:453–60. doi: 10.1093/sleep/2.4.453. [DOI] [PubMed] [Google Scholar]
- 2.Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the 24/7 life-style: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123:e1005–10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 3.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16:258–62. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- 4.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 5.Millman RP. Excessive sleepiness in adolescents and young adults: causes, consequences, and treatment strategies. Pediatrics. 2005;115:1774–86. doi: 10.1542/peds.2005-0772. [DOI] [PubMed] [Google Scholar]
- 6.Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21:871–81. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- 7.Taras H, Potts-Datema W. Sleep and student performance at school. J Sch Health. 2005;75:248–54. doi: 10.1111/j.1746-1561.2005.00033.x. [DOI] [PubMed] [Google Scholar]
- 8.Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep, risk behaviors, and depressive symptoms: are they linked? Am J Health Behav. 2010;34:237–48. doi: 10.5993/ajhb.34.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smaldone A, Honig JC, Byrne MW. Sleepless in America: inadequate sleep and relationships to health and well-being of our nation's children. Pediatrics. 2007;119(Suppl 1):S29–37. doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- 10.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009;10:771–9. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 11.Bixler E. Sleep and society: an epidemiological perspective. Sleep Med. 2009;10(Suppl 1):S3–6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 12.McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, Perry GS. Relationships between hours of sleep and health-risk behaviors in US adolescent students. Prev Med. 2011;53:271–3. doi: 10.1016/j.ypmed.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 13.Kohn M, Golden NH. Eating disorders in children and adolescents: epidemiology, diagnosis and treatment. Paediatr Drugs. 2001;3:91–9. doi: 10.2165/00128072-200103020-00002. [DOI] [PubMed] [Google Scholar]
- 14.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–58. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Favaro A, Ferrara S, Santonastaso P. The spectrum of eating disorders in young women: a prevalence study in a general population sample. Psychosom Med. 2003;65:701–8. doi: 10.1097/01.psy.0000073871.67679.d8. [DOI] [PubMed] [Google Scholar]
- 16.Kim KR, Jung YC, Shin MY, Namkoong K, Kim JK, Lee JH. Sleep disturbance in women with eating disorder: Prevalence and clinical characteristics. Psychiatry Res. 2010;176:88–90. doi: 10.1016/j.psychres.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 17.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2007. MMWR Surveill Summ. 2008;57:1–131. [PubMed] [Google Scholar]
- 18.Beebe DW, Fallone G, Godiwala N, et al. Feasibility and behavioral effects of an at-home multi-night sleep restriction protocol for adolescents. J Child Psychol Psychiatry. 2008;49:915–23. doi: 10.1111/j.1469-7610.2008.01885.x. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. National YRBS Data User's Manual. 2007. [[accessed 2012 February 22]]. Available from: ftp://ftp.cdc.gov/pub/data/yrbs/2007/YRBS_2007_National_User_Guide.pdf.
- 20.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27. [PubMed] [Google Scholar]
- 21.Washington: National Sleep Foundation; 2006. [[accessed 2012 February 22]]. 2006 Sleep in America poll: summary of findings [Internet] Available from: http://www.sleepfoundation.org/sites/default/files/2006_summary_of_findings.pdf. [Google Scholar]
- 22.Mori K, Sekine M, Yamagami T, Kagamimori S. Relationship between body image and lifestyle factors in Japanese adolescent girls. Pediatr Int. 2009;51:507–13. doi: 10.1111/j.1442-200X.2008.02771.x. [DOI] [PubMed] [Google Scholar]
- 23.Latzer Y, Tzischinsky O, Epstein R. Sleep-wake monitoring in women suffering from anorexia nervosa. Eat Disord. 2001;9:159–66. doi: 10.1080/10640260127713. [DOI] [PubMed] [Google Scholar]
- 24.Lacey JH, Crisp AH, Kalucy RS, Hartmann MK, Chien CN. Weight gain and the sleeping electroencephalogram: study of 10 patients with anorexia nervosa. Br Med J. 1975;4:556–8. doi: 10.1136/bmj.4.5996.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levy AB, Dixon KN, Schmidt H. REM and delta sleep in anorexia nervosa and bulimia. Psychiatry Res. 1987;20:189–97. doi: 10.1016/0165-1781(87)90078-3. [DOI] [PubMed] [Google Scholar]
- 26.Walsh BT, Goetz R, Roose SP, Fingeroth S, Glassman AH. EEG-monitored sleep in anorexia nervosa and bulimia. Biol Psychiatry. 1985;20:947–56. doi: 10.1016/0006-3223(85)90191-x. [DOI] [PubMed] [Google Scholar]
- 27.Lauer CJ, Krieg JC, Riemann D, Zulley J, Berger M. A polysomnographic study in young psychiatric inpatients: major depression, anorexia nervosa, bulimia nervosa. J Affect Disord. 1990;18:235–45. doi: 10.1016/0165-0327(90)90074-i. [DOI] [PubMed] [Google Scholar]
- 28.Latzer Y, Tzischinsky O, Epstein R, Klein E, Peretz L. Naturalistic sleep monitoring in women suffering from bulimia nervosa. Int J Eat Disord. 1999;26:315–21. doi: 10.1002/(sici)1098-108x(199911)26:3<315::aid-eat9>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 29.Baranowska B, Baranowska-Bik A, Bik W, Martynska L. The role of leptin and orexins in the dysfunction of hypothalamo-pituitary-gonadal regulation and in the mechanism of hyperactivity in patients with anorexia nervosa. Neuro Endocrinol Lett. 2008;29:37–40. [PubMed] [Google Scholar]
- 30.Lauer CJ, Krieg JC. Sleep in eating disorders. Sleep Med Rev. 2004;8:109–18. doi: 10.1016/S1087-0792(02)00122-3. [DOI] [PubMed] [Google Scholar]
- 31.Riemann D, Voderholzer U. Primary insomnia: a risk factor to develop depression? J Affect Disord. 2003;76:255–9. doi: 10.1016/s0165-0327(02)00072-1. [DOI] [PubMed] [Google Scholar]
- 32.Kaneita Y, Ohida T, Osaki Y, et al. Association between mental health status and sleep status among adolescents in Japan: a nationwide cross-sectional survey. J Clin Psychiatry. 2007;68:1426–35. doi: 10.4088/jcp.v68n0916. [DOI] [PubMed] [Google Scholar]
- 33.Spindler A, Milos G. Links between eating disorder symptom severity and psychiatric comorbidity. Eat Behav. 2007;8:364–73. doi: 10.1016/j.eatbeh.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 34.Marcks BA, Weisberg RB, Edelen MO, Keller MB. The relationship between sleep disturbance and the course of anxiety disorders in primary care patients. Psychiatry Res. 2010;178:487–92. doi: 10.1016/j.psychres.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 35.Papadimitriou GN, Linkowski P. Sleep disturbance in anxiety disorders. Int Rev Psychiatry. 2005;17:229–36. doi: 10.1080/09540260500104524. [DOI] [PubMed] [Google Scholar]
- 36.Vincent N, Cox B, Clara I. Are personality dimensions associated with sleep length in a large nationally representative sample? Compr Psychiatry. 2009;50:158–63. doi: 10.1016/j.comppsych.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 37.Cassin SE, von Ranson KM. Personality and eating disorders: a decade in review. Clin Psychol Rev. 2005;25:895–916. doi: 10.1016/j.cpr.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 38.van de Laar M, Verbeek I, Pevernagie D, Aldenkamp A, Overeem S. The role of personality traits in insomnia. Sleep Med Rev. 2010;14:61–8. doi: 10.1016/j.smrv.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 39.O'Donoghue GM, Fox N, Heneghan C, Hurley DA. Objective and subjective assessment of sleep in chronic low back pain patients compared with healthy age and gender matched controls: a pilot study. BMC Musculoskelet Disord. 2009;10:122. doi: 10.1186/1471-2474-10-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brener ND, McManus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. J Adolesc Health. 2003;32:281–7. doi: 10.1016/s1054-139x(02)00708-5. [DOI] [PubMed] [Google Scholar]
- 42.Sherry B, Jefferds ME, Grummer-Strawn LM. Accuracy of adolescent self-report of height and weight in assessing overweight status: a literature review. Arch Pediatr Adolesc Med. 2007;161:1154–61. doi: 10.1001/archpedi.161.12.1154. [DOI] [PubMed] [Google Scholar]
- 43.Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health. 2002;31:336–42. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]


