Abstract
Objective
To assess whether a specifically designed Yoga intervention can reduce hyperkyphosis.
Design
A 6-month, 2 group, randomized, controlled, single masked trial.
Setting
Community research unit.
Participants
118 women and men aged >60 years with kyphosis angle >40 degrees. Major exclusions were: serious medical comorbidity; use of assistive device; unable to hear or see adequately for participation; or unable to pass a physical safety screen.
Intervention
The active treatment group attended hour-long Yoga classes, 3 days per week, for 24 weeks. The control group attended a monthly luncheon/seminar and received mailings.
Measurements
Primary outcomes were change (baseline to 6 months) in Debrunner kyphometer-assessed kyphosis angle, standing height, timed chair stands, functional reach and walking speed. Secondary outcomes were change in: kyphosis index, flexicurve kyphosis angle, the Rancho Bernardo Blocks posture assessment and health-related quality of life (HRQOL).
Results
Compared to control participants, those randomized to Yoga experienced a 4.4% improvement in flexicurve kyphosis angle (p=0.006) and a 5% improvement in kyphosis index (p=0.004). The intervention did not result in statistically significant improvement in Debrunner kyphometer angle, measured physical performance or in self-assessed HRQOL (each p>0.1).
Conclusion
The decrease in flexicurve kyphosis angle in the Yoga treatment group shows that hyperkyphosis is remediable, a critical first step in the pathway to treating or preventing this condition. Larger, more definitive studies of Yoga or other interventions for hyperkyphosis should be considered. Targeting individuals with more malleable spines and using longitudinally precise measures of kyphosis could strengthen the treatment effect.
Keywords: kyphosis, hyperkyphosis, yoga, randomized controlled clinical trial
INTRODUCTION
Hyperkyphosis (“dowager’s hump”) is an excess forward curvature of the thoracic spine. A thoracic kyphosis angle of greater than 40 degrees, the 95th percentile value of thoracic kyphosis angles among young adults, is one operational definition of hyperkyphosis.1,2 Population prevalence rates of hyperkyphosis are unknown; however, they may be grossly approximated based on the prevalence of vertebral deformities, which occur in 10–45% in those aged between 50–90 years. 3–6 If only half of those with vertebral deformity had hyperkyphosis, its prevalence would range between 5 to 20% in parallel with advancing age. These estimates are conservative, because up to 70% of persons with hyperkyphosis do not have vertebral fractures.7–10
Adverse health outcomes associated with hyperkyphosis include physical functional limitations11–14, thoracic back pain9, respiratory compromise7, restricted spinal range of motion15 and osteoporotic fractures.16,17
Our biological model posits that there are bony, muscular, ligamentous, and postural contributors to hyperkyphosis and that some of these component causes of hyperkyphosis are remediable.18,19 Although it is commonly assumed that vertebral fractures are responsible for hyperkyphosis, only 42% of the variance in hyperkyphosis is accounted for by vertebral deformity20; the majority of persons with hyperkyphosis are vertebral fracture free.7,9,10 Other postulated, and potentially mutable, reasons for hyperkyphosis include: loss of anterior inter-vertebral disc height 10, 21–22; weakness of the erector spinae, abdominal muscles, and shoulder girdle11,23; postural abnormalities which lead to further weakness and shortening of under-used muscles, tendons and ligaments24; or low bone density which may lead to bowing of the spine without overt fracture.11 During normal stance, the center of gravity falls anterior to the thoracic spine, promoting greater vertebral body and inter-vertebral disc deformity anteriorly, compared to posteriorly; excess kyphosis places a relatively larger load on the anterior structures.25
The Yoga for Kyphosis Trial was a 6-month, single masked, randomized, controlled trial (RCT) of Yoga designed to improve thoracic kyphosis angle, posture, physical function and quality of life in older persons with hyperkyphosis. The RCT was based on the pre-post results of a single-armed pilot Yoga program.19 The central thesis of this RCT is that it may be possible to make hyperkyphotic persons “more upright" by strengthening the spinal erectors and core muscles, stretching the muscles of the shoulder and hip girdles and re-training posture, thereby improving the unfixed contributors to hyperkyphosis. In the longer term, more upright stance could lessen the anterior forces on the vertebral bodies and intervertebral disks, possibly preventing kyphosis progression.
METHODS
Study Design and Setting
The Yoga for Kyphosis Trial was a randomized, controlled, single masked clinical trial. All activities took place at the Yoga for Kyphosis offices, Westwood, California. The UCLA Institutional Review Board approved the protocol and participants gave written, informed consent.
The Yoga intervention group attended 3 Yoga classes per week for 6 months while the control intervention group received attention activities consisting of monthly luncheon-seminars and mailings. The randomized controlled trial (RCT) phase is the subject of this report. The study also included a 6-month post-RCT intervention, which will be reported subsequently.
The intended sample size was 120 evenly allocated to active and control treatments. To achieve a group size of approximately 30 in each arm and to allow staged recruitment, we implemented the intervention twice (Waves 1 and 2), enrolling roughly half the sample each time. Wave 1 received the RCT intervention between April and October 2005. Wave 2 received the RCT intervention between February and July 2006.
Participants
Participants were recruited from mailing lists; referrals from physicians, physical therapists and study participants; flyers; and senior education programs. Initial eligibility (e.g., age, willingness to accept randomization) was evaluated by phone. At an in-person screening, inclusion and exclusion criteria were assessed. Women and men aged 60 years or greater with adult-onset hyperkyphosis (noticed after age 50) were eligible if their measured Debrunner kyphometer angle was >40 degrees (see below). The following were exclusions: active angina; uncontrolled hypertension; high resting pulse or respiratory rate; unstable asthma or chronic obstructive pulmonary disease; cervical spine instability; unstable knee or shoulder joints; hemiparesis or paraparasis; use of assistive walking device; unable to hear or see adequately for participation; unable to comprehend and follow directions; unable to attend in-person classes; likely to move within one year; or has not had check-up by health care provider within 12 months (if not taking any prescription medications) or in the past 6 months (if any regular medicines taken) and not willing to do so prior to enrollment. Participants also had to stably execute the following safety tests: transition from standing to recumbent on the floor and get up from the floor to standing; lift both arms to shoulder level; stand with feet side-by-side for 30 seconds; and stand with feet hip-width apart for 60 seconds.
Randomization
Assignments were generated using randomly permuted blocks of sizes 4 and 6. Couples were randomized as a unit, to facilitate recruitment and retention and to avoid contamination; analyses were adjusted accordingly. Treatment assignments were placed in numbered, opaque envelopes and handed out in sequential order at the completion of the baseline visit. Researchers who conducted follow-up visits were unaware of assignments and participants were instructed not to reveal them.
Interventions
The active treatment group received Yoga, 3 days per week, one hour per session, for 24 weeks. The control group received monthly lunch/seminars, two hours per session, for the same duration.
Yoga intervention
The study used Hatha Yoga, which teaches asanas (poses) and pranas (breathing).26 By emphasizing mental and physical focus during the practice of asanas, Yoga attempts to build concentration and body awareness. It is a non-ballistic form of physical activity that uses slow, controlled movements (enhancing safety). Because Yoga postures are highly modifiable, they can be targeted at the mutable causes of hyperkyphosis while respecting the physical limitations of this population. We used a progressive series of poses that addressed flexibility, strength and proprioceptive awareness of all major appendicular and trunkal muscle groups. The first poses were done recumbent on the floor, a safe way to introduce controlled breathing and simple isometric and isotonic contractions of the arms, legs, and abdomen. Advancement was made to poses in a chair, on hands and knees, in the prone position and standing. Poses were modified versions of standard asanas, tailored to the physical capabilities of the population. An overview of the Yoga program is contained in Web Appendix 1.
Control intervention
The control intervention was designed to provide a social environment similar to Yoga. A doctoral level health educator facilitated 6 lunch-seminars, aimed at providing an emotionally positive and intellectually stimulating experience with socialization. Each session included lunch, an informational component (e.g., “What is stress and what can you do about it?”) and an interactive component (e.g., “Value Bingo”, an exercise in articulating personal priorities). Control participants also received a newsletter and a senior health magazine monthly.
Measurements
Baseline and follow-up visits included: 1) self-report survey of demographics, health conditions, health behaviors, and quality of life; 2) anthropometrics; and 3) physical performance testing. Measurements were made in the same order at all visits.
Reproducibility
Each anthropometric and physical performance outcome was measured 3 times (with repositioning) by the same staff member at each visit. The average of the 3 measures was used as the study outcome. The first and second of the 3 measures were used to assess intra-rater reliability. A second masked research associate, performed same-day measurements with repositioning in most instances (92 to 102 participants). Inter-rater reliability, assessed using intra-class correlation, ranged between 0.89 and 0.96 for the Debrunner and flexicurve kyphosis measures and between 0.73 and 0.93 for the other anthropometric and physical performance tests. Intra-rater reliability ranged between 0.93 and 0.98 for the Debrunner and flexicurve kyphosis measures and 0.86 and 0.94 for other anthropometric and physical performance tests.
Primary outcomes
The primary outcomes were change (baseline to 6 months) in Debrunner kyphometer-assessed kyphosis angle, standing height, timed chair stands, functional reach and walking speed. Primary outcomes were selected because they changed in response to the Yoga intervention in our single-armed pilot study.19
The Debrunner kyphometer consists of a protractor with a one-degree precision, mounted at the end of 2 double, parallel arms (Web Appendix 2). The upper arm of the kyphometer is placed on C-7 and the lower arm is placed on T-12. The circumscribed kyphosis angle is read from the protractor.9,27 Participants had 2 sets of Debrunner measures made to assess spinal flexibility: one standing in their usual, relaxed posture and one standing as tall as possible.28
Standing height was measured using a wall-mounted stadiometer.29 Hyperkyphosis precluded some from touching their heels to the wall; if so, we measured the distance between their heels and the wall and replicated this distance at follow-up. The timed chair stands test recorded the number of seconds required for a subject to stand up from a seated position 5 times without using their hands.30 The functional reach test evaluated an individual's ability to extend their arm forward without moving their base of support.31 The result is in centimeters; longer reach indicates better performance. The timed walk measured the time (seconds) that it takes to complete a 50-foot course at the fastest pace.32
Secondary outcomes
Secondary outcomes were change in: kyphosis index, flexicurve kyphosis angle, Rancho Bernardo Blocks and health-related quality of life (HRQOL). The kyphosis index was measured using a flexicurve, which conforms to the contour of the spine (Web Appendix 2).18,20 The cephalic end of the flexicurve is placed on C-7; it is molded to the spine in the caudal direction. The shape is traced onto paper and the apex kyphosis height is measured relative to the length of the entire thoracic spine; this ratio is the kyphosis index. Higher values indicate greater kyphosis. Using geometric formulae, the flexicurve inscribed kyphosis angle was also calculated from the flexicurve tracing. By definition, an inscribed angle is systematically less than a circumscribed angle. The Rancho Bernardo Blocks (RBS-Blocks) measure is an estimate of forward posture, but is not specific for thoracic kyphosis.33,13,17 With the participant lying supine on a flat surface, blocks are placed under the occiput to achieve a neutral head position (Web Appendix 2). The number of blocks required to achieve neutrality is the estimate of forward posture. Secondary HRQOL outcomes were assessed in multiple domains. The RAND 36-Item Health Survey 1.0 assessed: 1) physical functioning; 2) general bodily pain; 3) role limitations due to health; 4) role limitations due to personal or emotional problems; 5) mental health; 6) social functioning; 7) energy/fatigue; 8) health perceptions.34 Scores range from 0–100; higher scores indicate better function. T-scores were computed by normalizing the mean to 50. Pain was measured in greater detail with the RAND bodily pain questions34. This 12-item survey asks about the occurrence of bodily pain in the past 4 weeks; persons reporting any pain are asked 11 additional questions that gauge severity, frequency, duration, and number of days that pain interfered with usual activities as well as pain’s interference with mood, mobility, sleep, recreation, and life enjoyment. The pain interference items are scaled from 0 to 100, normalized to a mean of 50. The Activities-specific Balance Confidence (ABC) scale, is a 16- item survey that assesses a participant’s confidence that they will not fall during daily activities.35 Scores range from 16 to 160; higher scores correspond to greater falls efficacy (confidence that falls will not occur). We also calculated the ABC-6, which consists of the 6 most challenging items from the ABC scale.36 The ABC and ABC-6 were scaled to 100 to facilitate comparison to the HRQOL scales.
Covariates
Demographic descriptors, medical conditions, and health behaviors were recorded using standardized questionnaires. Usual physical activity was assessed using the average of the home and leisure domains from the PEPI physical activity scale. Values range from 1 to 4 corresponding to no, mild, moderate or intense usual activity.37–39 Vertebral deformities were read from baseline standing radiographs by a single, masked, expert musculoskeletal radiologist (LS). The criterion for prevalent fracture was at least 25% decrement in height in the anterior, middle, or posterior dimension of the vertebral body.
Adherence
Attendance at Yoga classes or at luncheon seminars was recorded. Those who attended 80% of the Yoga classes, or 4 of the 6 lunch seminars, were classified as adherent.
Side effects
To allow equal opportunity to observe possible side effects in the active and the control conditions, we used a monthly symptom checklist containing plausible side effects of the Yoga intervention (e.g., back pain, muscle cramps) as well as distractor symptoms expected to be unrelated to Yoga (e.g., constipation).
Sample size
Power calculations were based on plausible effect sizes for 2 primary outcomes for which we had pilot data, Debrunner Kyphometer angle and standing height; we assumed that the treatment difference would be 1.5 times the effect sizes observed in the 3-month pilot.19 We calculated the required sample size to detect the hypothesized between-group differences in mean within-subject change using a 2-sample t-test, under 80% power, 0.05 significance level and 2-sided hypothesis testing. Randomizing a sample of 120, assuming 20% attrition, the minimum detectable difference in Debrunner kyphosis angle was 7.82 degrees and the minimal detectable difference in height change was 0.12 cm.
Statistical Analysis
Baseline characteristics were summarized using frequencies for categorical variables and means and standard deviations for continuous variables. The 2 treatment arms were compared, and attriters and completers were compared, using Wilcoxon 2-sample rank sum tests and Fisher’s exact tests. Within subject changes from baseline to 6 months in anthropometric and physical performance outcomes were compared for the 2 treatment arms using Wilcoxon 2-sample rank sum tests.
Baseline values of most of the HRQOL scales were characterized by a “ceiling effect”: many participants were at the maximum value. To account for this right truncation, analyses of continuous HRQOL outcomes used longitudinal Tobit models.40 Ordinal categorical outcomes were analyzed using a method from Evans et al.41 Briefly, within-participant changes were ranked separately for each baseline outcome value, these ranks were transformed using normal scores, and the treatment arms were compared using Wilcoxon signed rank testing.
The occurrence of side effects (each month for each symptom) was compared using Fisher’s exact tests. The total number of symptomatic months (out of 6) that each symptom was reported was compared using Wilcoxon 2-sample rank sum tests. Longitudinal logistic regressions for each symptom indicated that trajectories (i.e., whether prevalence increased or decreased over time) did not vary significantly by treatment arm (results not presented). Symptom checklists were missing for at least 1 month for 57.5% of control group participants and for 31.6% of Yoga group participants (median numbers of checklists received were 4.95 and 5.31 respectively). Not having a symptom in the previous month was more strongly predictive of missing data in the subsequent month for control participants than for yoga participants. Thus, analyses employed multiple imputation42 of missing symptoms, imputed as a function of the participant’s own observed percentage of symptomatic months. Non-imputed analyses were not substantively different (data not shown).
RESULTS
Participant flow
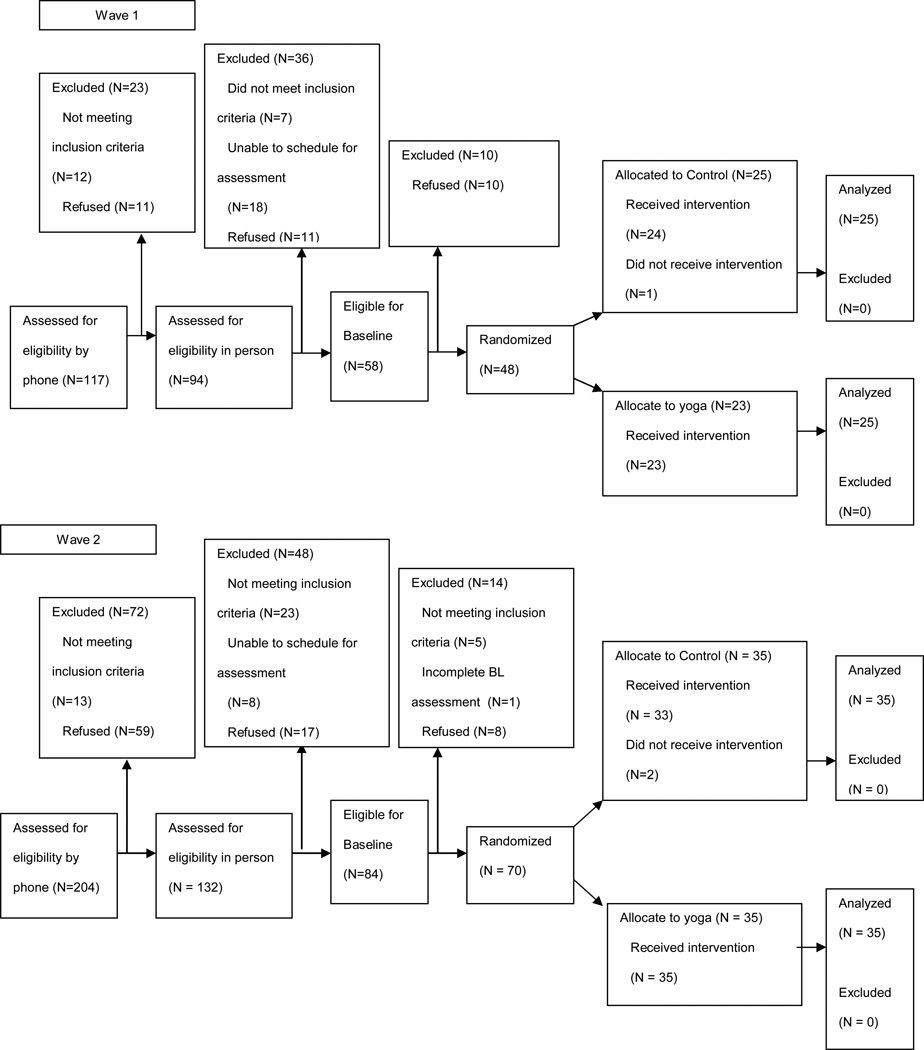
We completed 243 phone screenings and 172 in-person screenings to enroll 118 participants. Wave 1 randomized 48 participants, 23 to Yoga and 25 to the control intervention, delivered between April and October 2005. Wave 2 randomized 70 participants, 35 to Yoga and 35 to the control intervention, delivered between February and July 2006. Figure 1 depicts screening, enrollment and intervention delivery.
Figure 1.
Flow diagram of recruitment, enrollment, intervention delivery and number of participants who contributed data to the analysis in the Yoga for Hyperkyphosis Trial, by study wave.
Baseline characteristics
Mean age was 75.5 years (range 59.8 to 90); approximately 81% were women and 88% were Caucasian. In general, participants had high educational attainment, were not current smokers and had moderate alcohol consumption (Table 1). The average physical activity score was 2.3, which corresponds to activities such as light housework, gardening, carpentry, bowling, golfing, or walking at least 10 minutes daily. Characteristics were generally similar in the Yoga and control intervention groups, except that current employment and level of educational attainment were somewhat higher and usual physical activity was slightly lower in the Yoga group. Prevalent vertebral fractures were present in 25% of participants.
Table 1.
Baseline Demographic, Behavioral and Medical Characteristics of Study Sample, by Treatment Assignment and by Loss to Follow up
| Characteristic | Full sample (N=118) |
Yoga Intervention group (N=58) |
Control intervention group (N=60) |
p-value for treatment arm comparisons¶, |
Participants lost to follow- up (N=13) |
p-value comparing attriters and completers¶, |
|---|---|---|---|---|---|---|
| Age (yrs) | 75.5 ± 7.4 | 74.5 ± 7.6 | 76.5 ± 7.2 | 0.169 | 76.6 ± 7.4 | 0.526 |
| Body mass index (kg/m2) | 26.5 ± 4.6 | 26.3 ± 4.7 | 26.8 ± 4.5 | 0.521 | 25.9 ± 5.1 | 0.477 |
| Female gender: % (N) | 81.4 (96) | 82.8 (48) | 80.0 (48) | 0.814 | 92.3 (12) | 0.458 |
| Race/ethnicity: % (N) * | 0.408 | 0.006 | ||||
| Black | 5.1 (6) | 1.7 (1) | 8.5 (5) | 25.0 (3) | ||
| Hispanic | 4.3 (5) | 5.2 (3) | 3.4 (2) | 8.3 (1) | ||
| White | 88.0 (103) | 89.7 (52) | 86.4 (51) | 58.3 (7) | ||
| Other | 2.6 (3) | 3.5 (2) | 1.7 (1) | 8.3 (1) | ||
| Employed (paid or volunteer): % (N) * |
43.6 (51) | 60.8 (31) | 33.9 (20) | 0.041 | 33.3 (4) | 0.548 |
| Educational level: % (N)* | 0.034 | 0.118 | ||||
| < High school | 0.9 (1) | 0.0 (0) | 1.7 (1) | 8.3 (1) | ||
| High school | 6.8 (8) | 3.5 (2) | 10.2 (6) | 0.0 (0) | ||
| Some college | 28.2 (33) | 20.7 (12) | 35.6 (21) | 16.7 (2) | ||
| College or greater | 64.1 (75) | 75.9 (44) | 52.5 (31) | 75.0 (9) | ||
| Cigarette use: % (N) † | 0.574 | 0.426 | ||||
| Never | 56.0 (65) | 58.6 (34) | 53.5 (31) | 41.7 (5) | ||
| Former | 43.1 (50) | 39.7 (23) | 46.6 (27) | 58.3 (7) | ||
| Current | 0.9 (1) | 1.7 (1) | 0.0 (0) | 0.0 (0) | ||
| Current alcohol consumption: % (N) † |
54.3 (63) | 63.8 (37) | 44.8 (26) | 0.062 | 58.3 (7) | 1.000 |
| Drinks/wk (consumers) | 16.4 ± 18.9 | 15.1 ± 17.4 | 18.0 ± 21.0 | 0.680 | 14.9 ± 10.6 | 0.444 |
| Usual physical activity †,‡ | 2.3 ± 0.5 | 2.2 ± 0.5 | 2.4 ± 0.5 | 0.056 | 2.3 ± 0.5 | 0.923 |
| Chronic conditions (#) | 5.4 ± 3.0 | 5.6 ± 3.1 | 5.2 ± 2.8 | 0.672 | 5.4 ± 2.7 | 0.856 |
| Vertebral fractures *,§ | ||||||
| Any % (N) | 24.8 (29) | 27.8 (16) | 22.0 (13) | 0.526 | 50.0 (6) | 0.070 |
| Thoracic % (N) | 19.7 (23) | 22.4 (13) | 17.0 (10) | 0.493 | 41.7 (5) | 0.058 |
| Lumbar % (N) | 6.8 (8) | 8.6 (5) | 5.1 (3) | 0.490 | 8.3 (1) | 0.591 |
Missing for 1 control group participant
Missing for 2 control group participants
Physical activity assessed by PEPI activity scale. Scores range from 1 (low) to 4 (high) and represent average home and leisure activity (see Methods for additional detail).
Sum of “any” fracture less than thoracic plus lumbar because some participants had fractures of both spinal regions.
p-value from Wilcoxon rank-sum test or Fisher’s exact test
Baseline characteristics did not differ between participants who did or who did not complete the 6-month follow-up, with the exception of prevalent thoracic vertebral fracture (more common among attriters) and race/ethnicity. Non-white sample sizes were small, however. The characteristics listed in Table 1 did not differ between Wave 1 and Wave 2 (data not shown).
Baseline values of primary and secondary outcomes
Summarized in Table 2, on average, participants were moderately kyphotic, with a median Debrunner kyphosis angle of 58 degrees, a kyphosis index of 0.16 and a flexicurve kyphosis angle of 36 degrees. (The flexicurve kyphosis angle is inscribed, by definition systematically lower than the circumscribed Debrunner angle). Spinal flexibility, the difference between kyphosis angles measured during usual posture versus best posture, was −5.69 degrees (standard deviation, 4.10) using the Debrunner instrument. By flexicurve, spinal flexibility was −3.35 degrees (standard deviation, 2.51). Spinal flexibility did not differ by treatment assignment (data not shown).
Table 2.
Baseline Measures of Anthropometric, Physical Performance, and Health-Related Quality of Life (HRQOL) outcomes
| Median (25th percentile – 75th percentile) | ||||
|---|---|---|---|---|
| Anthropometric / Physical Performance: |
Full sample (N=118) | Yoga intervention group (N=58) |
Control intervention group (N=60) |
p-value (a) |
| Primary Outcomes: | ||||
| Debrunner angle (degrees) | 58.0 (51.0 – 65.0) | 56.2 (51.7 – 63.7) | 58.7 (49.0 – 65.5) | 0.502 |
| Height (cm) | 159.2 (153.4 – 166.7) | 158.1 (154.2 – 164.6) | 159.6 (151.9 – 167.4) | 0.557 |
| Chair stand (seconds) † | 14.7 (12.5 – 17.6) | 14.4 (12.5 – 17.2) | 14.9 (12.1 – 17.8) | 0.645 |
| Functional reach (cm) | 33.0 (29.0 – 38.4) | 32.2 (29.1 – 38.4) | 34.1 (28.9 – 38.2) | 0.807 |
| 50-foot walk (m/sec) ‡, | 1.34 (1.17 – 1.54) | 1.35 (1.19 – 1.58) | 1.32 (1.13 – 1.51) | 0.312 |
| Secondary Outcomes: | ||||
| Kyphosis index | 0.16 (0.14 – 0.19) | 0.16 (0.14 – 0.18) | 0.16 (0.14 – 0.19) | 0.687 |
| RBS blocks ठ| 2.67 (2.00 Р3.33) | 2.67 (2.00 Р3.33) | 2.67 (2.00 Р3.67) | 0.334 |
| Flexicurve angle (degrees) | 36.5 (31.6 – 41.5) | 36.1 (31.6 – 39.8) | 36.6 (31.3 – 41.7) | 0.518 |
| HRQOL Outcomes: | ||||
| RAND 36-item health survey 1.0:‡, | ||||
| Physical functioning | 85.0 (70.0 – 95.0) | 85.0 (70.0 – 95.0) | 85.0 (60.0 – 95.0) | 0.515 |
| Role limitations-physical | 100.0 (50.0 – 100.0) | 100.0 (50.0 – 100.0) | 100.0 (50.0 – 100.0) | 0.924 |
| Role limitations-emotional | 100.0 (100.0 – 100.0) | 100.0 (100.0 – 100.0) | 100.0 (100.0 – 100.0) | 0.452 |
| Energy / fatigue | 60.0 (50.0 – 75.0) | 65.0 (50.0 – 75.0) | 55.0 (50.0 – 75.0) | 0.320 |
| Emotional well-being | 80.0 (68.0 – 88.0) | 80.0 (68.0 – 88.0) | 80.0 (64.0 – 92.0) | 1.000 |
| Social functioning | 100.0 (77.5 – 100.0) | 100.0 (87.5 – 100.0) | 90.0 (67.5 – 100.0) | 0.067 |
| General health perceptions | 75.0 (60.0 – 85.0) | 75.0 (60.0 – 85.0) | 75.0 (60.0 – 85.0) | 0.563 |
| Bodily pain (single item) | 85.0 (70.0 – 100.0) | 90.0 (75.0 – 100.0) | 85.0 (65.0 – 100.0) | 0.163 |
| RAND Bodily Pain Survey: | ||||
| Any pain in past 4 weeks‡, | 75.2 (88) | 70.7 (41) | 79.7 (47) | 0.290 |
| Pain severity¶: | 0.442 | |||
| Mild | 37.5 (33) | 31.7 (13) | 42.55 (20) | |
| Moderate | 51.1 (45) | 58.5 (24) | 44.7 (21) | |
| Severe | 11.4 (10) | 9.8 (4) | 12.8 (6) | |
| Pain frequency: ¶ | 0.753 | |||
| Rare | 37.5 (33) | 39.0 (16) | 36.2 (17) | |
| Fairly / very often | 44.3 (39) | 46.3 (19) | 42.6 (20) | |
| Daily / almost daily | 18.2 (16) | 14.6 (6) | 21.3 (10) | |
| Pain interfered with daily activity (# days) §,¶f) |
0.0 (0.0 – 7.0) | 0.0 (0.0 – 6.5) | 0.0 (0.0 – 7.0) | 0.860 |
| Pain interference with QOL §¶ | 1.8 (1.4 – 2.4) | 1.8 (1.4 – 2.2) | 2.0 (1.2 – 2.8) | 0.356 |
| Visual analog pain severity ¶ | 4.0 (3.0 – 8.5) | 4.0 (3.0 – 9.0) | 5.0 (3.0 – 8.0) | 0.926 |
| Visual analog worst pain ¶ | 8.0 (4.0 – 12.0) | 8.0 (4.0 – 12.0) | 8.0 (4.0 – 12.0) | 0.619 |
|
Activities-specific Balance Confidence (ABC): |
||||
| Full ABC scale‡ | 88.0 (75.6 – 93.8) | 87.5 (78.8 – 93.8) | 88.1 (67.5 – 94.0) | 0.470 |
| ABC-6 ‡ | 75.0 (60.0 – 86.7) | 78.3 (63.3 – 86.7) | 75.0 (56.7 – 86.0) | 0.468 |
Comparison of treatment arms using Wilcoxon two-sample rank sum test for continuous outcomes and Fisher’s exact test for categorical outcomes
Missing data from 3 Yoga participants
Missing data from 1 control participant
Missing data from 1 Yoga participant
Subset who reported any pain in past 4 weeks
Missing data from 2 control participants
At baseline, Spearman correlations between each of the kyphosis measurements were statistically significantly different from zero and were: Debrunner angle with kyphosis index, 0.79; Debrunner angle with flexicurve kyphosis angle, 0.80; kyphosis index with flexicurve kyphosis angle, 0.99. Correlations between RBS blocks and Debrunner angle, kyphosis index and flexicurve kyphosis angle were 0.34, 0.34, and 0.35, respectively, substantially lower than correlations between other kyphosis measures.
Participants reported almost no limitations in role function related to physical or emotional health or in social function: median scores were 100. With the exception of the energy/fatigue domain, all other HRQOL scales were rated uniformly highly. Although health-related role limitations were generally absent, bodily pain was common. Three quarters endorsed some pain in the past 4 weeks; of these, approximately 60% stated their pain occurred fairly often to daily. Apparently, pain did not compromise function: the median number of days of interference with daily activity was zero. Falls efficacy was also high. All domains of HRQOL, pain reporting and falls efficacy were similar in the Yoga and the control intervention groups (Table 2) and in Wave 1 and Wave 2 (data not shown).
Intervention delivery
Overall, 50% of participants in the Yoga intervention group attended 80% or more of the Yoga classes (median % attended was 79.9%); Yoga adherence rates were 52.2% in Wave 1 and 48.6% in Wave 2. Among those randomized to the control condition, 71.7% attended at least 4 of 6 lunch-seminars (median number was 5); Wave 1 and Wave 2 lunch-seminar adherence rates were 76.0% and 68.6%, respectively.
Kyphosis, posture and height
Compared to the control intervention, Yoga resulted in statistically significant reductions in hyperkyphosis according to 2 of the 3 kyphosis measurement methods (Table 3). The median flexicurve kyphosis index decreased by 0.006 in those randomized to Yoga and increased by 0.003 among control participants (p=0.004), a 5% difference. The median flexicurve inscribed kyphosis angle lessened by 0.93 degrees in the Yoga intervention group while that of the control participants increased by 0.82 degrees (p=0.005), a 4.4% difference. Median Debrunner kyphosis angle diminished by 3 degrees in the Yoga group, but it also decreased by 1.33 degrees in the control group, a difference of 3% (p=0.437). The RBS blocks did not change in either group. A small (0.2% between-groups difference) treatment benefit was evident for standing height (p=0.054).
Table 3.
Unadjusted Treatment Arm Differences in Mean Within-Subject Change in Anthropometrics and Measured Physical Performance – Intent-to-Treat Analyses (N=105) *
| Median within-subject change (25th – 75th percentile) | |||
|---|---|---|---|
| Anthropometric and Physical Performance Outcomes |
Yoga intervention group (N=55) |
Control intervention group (N=50) |
p-value† |
| Primary Outcomes: | |||
| Debrunner kyphometer angle: | |||
| Absolute change (degrees) | −3.00 (−4.67, 0.67) | −1.33 (−6.67, 2.00) | 0.443 |
| % change | −5.17 (−8.38, 0.93) | −2.10 (−11.24, 2.67) | 0.437 |
| Height: | |||
| Absolute change (cm) | 0.30 (−0.17, 0.80) | 0.03 (−0.50, 0.43) | 0.057 |
| % change | 0.19 (−0.11, 0.48) | 0.02 (−0.30, 0.26) | 0.054 |
| Chair stand: ‡ | |||
| Absolute change (seconds) | −1.41 (−3.19, −0.27) | −0.80 (−2.80, 0.70) | 0.246 |
| % change | −10.11 (−20.63, −1.85) | −5.66 (−16.33, 6.19) | 0.138 |
| Functional reach: | |||
| Absolute change (cm) | −0.66 (−3.88, 2.71) | −1.48 (−4.81, 2.04) | 0.476 |
| % change | −2.23 (−12.44, 9.31) | −3.75 (−11.92, 5.24) | 0.472 |
| 50-foot walk: § | |||
| Absolute change (m/sec) | −0.02 (−0.09, 0.08) | −0.01 (−0.09, 0.07) | 0.760 |
| % change | −1.65 (−6.44, 5.91) | −0.83 (−5.37, 5.38) | 0.897 |
| Secondary outcomes: | |||
| Kyphosis index: | |||
| Absolute change | −0.006 (−0.015, 0.002) | 0.003 (−0.006, 0.008) | 0.004 |
| % change | −3.64 (−8.98, 1.34) | 1.71 (−3.41, 4.65) | 0.004 |
| Flexicurve angle: | |||
| Absolute change (degrees) | −0.93 (−3.30, 1.04) | 0.82 (−1.03, 2.06) | 0.005 |
| % Change | −2.25 (−8.09, 3.25) | 2.16 (−3.04, 6.08) | 0.006 |
| RBS blocks: §¶ | |||
| Absolute change (number) | 0.00 (−0.33, 0.33) | 0.00 (−0.83, 0.33) | 0.408 |
| % Change | 0.00 (−13.33, 12.50) | 0.00 (−25.00, 11.11) | 0.160 |
N=105 because 13 participants did not have follow-up visit
Comparison of treatment arms using Wilcoxon rank-sum test
Missing for 3 yoga group participants
Missing for 1 control group participant
Missing for 1 yoga group participant
Physical performance
The Yoga group cut 1.4 seconds from its chair stand time (a 10% improvement) and the control group’s chair stand time went down by about half as much, a between-groups difference of approximately 5%, which did not reach the level of statistical significance (Table 3). Functional reach and 50-foot walk time improved slightly in both groups.
HRQOL
Small changes in each of the HRQOL scales were apparent for both the Yoga and the control groups, ranging from approximately −2 to 8 points, but there were no statistically significant effects of treatment (data not shown; p>0.06 for all comparisons).
Side effects
Table 4 summarizes the percent of participants endorsing each of 8 plausible side-effect symptoms and each of 8 distractor symptoms at the first and final month of the RCT, as well as the mean number of months that each symptom was reported. Upper back pain was reported half as often in the Yoga group (average 0.9 months) compared to the control group (average 1.8 months) (p=0.01). In contrast to our expectation that the distractor symptoms would be reported with equal frequency in the 2 groups, the Yoga group reported fewer months during which they experienced early awakening (p=0.007) or insomnia (p=0.03).
Table 4.
Percent of Time Each Symptom was Reported in Months 1 and 6, and Numbers of Months (out of 6) that Each Symptom was Reported, by Treatment Assignment *
| SYMPTOMS | Yoga (N=56) | Control (N=59) | Yoga (N=56) | Control (N=59) |
|||
|---|---|---|---|---|---|---|---|
| Target Symptoms† |
% Symptoms Month 1 |
% Symptoms Month 6 |
% Symptoms Month 1 |
% Symptoms Month 6 |
Mean Number Symptomatic Months |
Mean Number Symptomatic Months |
p-value‡ |
| Low back pain |
48.6 | 38.9 | 42.4 | 38.6 | 2.4 | 2.3 | 0.88 |
| Leg cramps | 39.3 | 31.4 | 41.4 | 38.0 | 2.1 | 2.3 | 0.55 |
| Neck aches | 37.5 | 27.1 | 25.4 | 29.2 | 1.7 | 1.9 | 0.63 |
| Muscle stiffness |
31.8 | 26.4 | 33.2 | 39.0 | 1.9 | 2.0 | 0.70 |
| Upper back pain |
17.9 | 14.3 | 22.0 | 32.2 | 0.9 | 1.8 | 0.01 |
| Weight loss | 14.3 | 17.9 | 6.8 | 11.9 | 0.7 | 0.4 | 0.17 |
| Stress incontinence |
12.5 | 10.7 | 14.9 | 15.9 | 0.6 | 0.9 | 0.29 |
| Dizziness | 7.1 | 5.4 | 13.9 | 7.8 | 0.5 | 0.5 | 0.82 |
|
Distractor Symptoms§ |
|||||||
| Forgetfulness | 27.9 | 30.4 | 50.5 | 40.3 | 1.7 | 2.6 | 0.06 |
| Early awakening |
23.2 | 32.5 | 45.4 | 49.8 | 1.6 | 2.7 | 0.007 |
| Take naps | 20.4 | 23.2 | 36.3 | 29.8 | 1.3 | 2.0 | 0.07 |
| Difficult to concentrate |
19.6 | 22.5 | 28.8 | 24.4 | 1.3 | 1.6 | 0.37 |
| Insomnia | 12.5 | 13.2 | 33.9 | 25.8 | 0.8 | 1.6 | 0.03 |
| Constipation | 12.5 | 16.4 | 15.3 | 17.6 | 0.9 | 1.1 | 0.56 |
| Cold or virus | 11.4 | 14.6 | 21.0 | 10.2 | 0.7 | 0.7 | 0.84 |
| Tinnitus | 11.1 | 12.5 | 20.3 | 18.6 | 0.7 | 1.0 | 0.36 |
Based on results using multiple imputation; see Methods for details.
Target symptoms are those symptoms that were hypothesized to occur due to Yoga intervention
p-value for Wilcoxon 2-sample comparing # of months with symptoms in the Yoga and control interventions
Distractor symptoms were symptoms that were hypothesized to be unrelated to the Yoga intervention. There were an additional 17 distractors each of which was reported a lower frequency than the 8 distractors shown and which did not differ in frequency by treatment assignment.
Secondary analyses
We performed 5 pre-specified secondary analyses: 1) adjustment of all models for age, gender and presence of any vertebral fracture; 2) examination of results by adherence; 3) testing for an interaction between treatment and prevalent vertebral fracture; 4) testing for an interaction between treatment and baseline Debrunner kyphosis angle (above or below the sample median); and 5) testing for an interaction between treatment arm and dose (the number of Yoga classes or lunch-seminars attended) in the full sample and separately for each treatment arm. Results of pre-specified secondary analyses were not different from the intention-to-treat analyses (data not shown).
We conducted 2 non-pre-specified secondary analyses. The first was a test for interaction between treatment and high spinal flexibility (defined as the median value, −5.33 degrees), hypothesizing that persons with more pliable spines would benefit more. Participants randomized to the Yoga intervention with high spinal flexibility achieved a −3.5 (6%) degree median improvement in Debrunner kyphosis angle; among those with low spinal flexibility Yoga produced a −2.0 (3%) degree median improvement. Control group participants with high spinal flexibility realized a −3.0 degree (4.6%) median improvement in Debrunner kyphosis angle while control participants with low spinal flexibility had a 0.33 degree median change (0.55%) (p=0.3 for interaction).
Finally, 28 participants’ kyphosis measures were flagged during the study visits as difficult, either because the Debrunner kyphometer was not stable on the vertebral spines (i.e., “wobbled”) or because the thoracic and lumbar regions were both kyphotic (“C” shaped spine). Among those who were free from measurement difficulties, Yoga-assigned participants experienced a −5.40% decrease in Debrunner kyphosis angle and control group participants posted a −0.72% change (p=0.1 for interaction).
Discussion
This 6-month Yoga intervention resulted in statistically significant improvements in 2 hyperkyphosis outcomes: compared to control participants, those randomized to Yoga experienced a 4.4% greater improvement in flexicurve kyphosis angle and a 5% greater improvement in kyphosis index. The intervention did not result in any statistically significant gains in measured physical performance or in self-assessed HRQOL. No negative side effects of Yoga occurred; rather, compared to those randomized to luncheon-seminars, Yoga participants reported less upper back pain, early morning awakening and insomnia.
The intervention’s main goal was to reduce hyperkyphosis, which it accomplished based on the flexicurve assessments, but not based on the Debrunner kyphometer. The most likely explanation for these divergent results is that for long-term repeated measures, the flexicurve is more accurate and more precise than is the Debrunner instrument. The flexicurve traces the curvature of the entire spine, determining the thoracic kyphosis based on the inflection point between the thoracic kyphosis and lumbar lordosis. In contrast, the Debrunner kyphosis angle is defined by the position of the instrument on external landmarks that attempt to locate the C-7 and T-12 vertebrae9. Despite careful protocols the inferior landmark can be difficult to discern, especially when the lumbar lordosis has reversed and the entire thoraco-lumbar region is kyphotic ( “C” shaped).20,24 In addition, accuracy and precision can be diminished because the kyphometer sometimes wobbles on the T-7 or T-12 spinous processes. (Note that this instability may be lessened by using the protocol of Ohlen and colleagues, which places the kyphometer across two superior and two inferior spinous processes.43 Although the same-day reliabilities of the Debrunner kyphometer were similar to those of the flexicurve, the technical challenges of the Debrunner measure may have made its 6-month precision lower than that of the flexicurve. The secondary analysis of technically difficult measurements supported this hypothesis.
To our knowledge, there are no published randomized, controlled, physical activity-based interventions to correct hyperkyphosis that are directly comparable to this RCT. However a few non-randomized or non-controlled studies of physical activity interventions suggested that kyphosis improvements are possible. Itoi and colleagues randomized 60 postmenopausal women to a 2-year progressive back strengthening exercise vs. no intervention, but hyperkyphosis was not an entry criterion. The intention-to-treat analysis found no between-groups change in radiologically measured kyphosis angles, but a post-hoc, non-randomized analysis, which divided the study sample according to whether participants had achieved greater than or less than the median increase in back strength, reported a 2.8 degree improvement in radiological kyphosis angle among those in the high strength gain category,44 similar to the Yoga group’s decrease of 3 degrees by kyphometer. Katzman et.al., reported statistically significant pre-post improvements in kyphosis in a single arm, non-blinded, exercise intervention in 21 women aged 65+ years who had Debrunner-measured hyperkyphosis of at least 50 degrees and high spinal flexibility (at least −5 degrees).45 The investigators recorded a 6 degree reduction in usual-stance kyphosis, twice the size of our Yoga arm’s within-group reduction. This larger effect size may be due in part to selection based on spinal flexibility. Our secondary analysis demonstrated a kyphometer improvement of 4 degrees in the high spinal flexibility subgroup.
Other proposed interventions for hyperkyphosis include spinal orthoses, vertebroplasty and kyphoplasty. One RCT randomized women aged 60+ years with at least 1 vertebral fracture and hyperkyphosis of > 60 degrees to wear a spinal orthosis for 6 months or to a wait list (N=31, each arm).46 Although the authors did not report whether assessors were masked, the orthosis arm posted a 7.9 degree improvement in kyphosis angle compared to a 1.9-degree improvement in the control arm. A review of 69 clinical studies of vertebroplasty and kyphoplasty (none of which were RCTs) calculated a mean kyphotic angle restoration of 6.6 degrees for each of these techniques.47 Notably, the kyphotic angle is the wedge angle of the fractured vertebrae only, which is should not be confused with the kyphosis angle of the entire thoracic spine.
Changes in chair stand time, functional reach and walking speed did not differ by study arm, but there was a trend towards betterment of chair stand time: 10% in the Yoga arm and 5% in the control arm (p=0.134). We expected that chair stand time in the control condition would decline or remain stable during the 6-month study.48 Improved physical performance in the control participants could have resulted from augmented physical activity over time, but self-reported home and leisure physical activity did not rise (data not shown). More likely, the measurement was influenced by a practice effect, which has been reported for the chair stand and walk tests.49
Participants began with almost no role or emotional limitations due to health, thus these domains could not improve. Substantial general body pain was reported but pain was also unmoved by the intervention. Inquiring about bodily pain may have been too non-specific to capture the effect of Yoga, because on the monthly symptom checklist, the Yoga group reported statistically significantly less upper back pain (50% fewer months). The symptom checklist also chronicled less early awaking (40% fewer months) and insomnia (50% fewer months) in the Yoga group. Only half of the Yoga-assigned participants met the 80% adherence benchmark, possibly lowering the effectiveness of the intervention. However, we did not observe a stronger effect in adherent participants.
In summary, the principal limitations of our study are its small size and that it enrolled high functioning seniors, limiting generalizability to elders with functional limitations. However, this study must be considered developmental, not definitive. The improvement in flexicurve kyphosis angle supports the hypothesis that hyperkyphosis is remediable, which is an important, and novel, proof of concept. Larger, more definitive studies of Yoga for hyperkyphosis should be considered. Using self-reported function scales that were not limited by a ceiling effect, making two baseline measures of physical performance on separate days to account for the learning effect, targeting individuals with more malleable spines, using longitudinally precise measures of kyphosis and enhancing adherence could strengthen the observed effects of Yoga.
Supplementary Material
ACKNOWLEDGEMENTS
Source of Funding: Funding for conduct of the Yoga for Kyphosis Trial and investigator support for Drs. Greendale, Huang, Seeger and Crawford was provided by NIH/NICHHD (5 R01 HD045834). Dr. Karlamangla was supported by funding from the UCLA-Claude D. Pepper Older Americans Independence Center (1P30 AG028748).
Footnotes
Conflict of interest: The authors have no conflicts of interest.
Author contributions: Gail A. Greendale led the design and conduct of the study, collaborated in the conduct and interpretation of data analyses, obtained funding, and drafted the manuscript. Mei-Hua Huang, Arun S. Karlamangla and Leanne Seeger, MD each collaborated in the design and conduct of the study, contributed to the interpretation of the data analysis and had critical input to the manuscript. Sybil Crawford collaborated in the design and conduct of the study, conducted the data analysis and had critical input to the manuscript. All authors read and approved the final manuscript.
REFERENCES
- 1.Fon GT, Pitt MJ, Thies AC. Thoracic kyphosis: Range in normal subjects. Am J Roentgenol. 1980;134:979–983. doi: 10.2214/ajr.134.5.979. [DOI] [PubMed] [Google Scholar]
- 2.Voutsinas SA, MacEwan GD. Saggital profiles of the spine. Clin Orthop. 1986;210:235–242. [PubMed] [Google Scholar]
- 3.O'Neill TW, Felsenberg D, Varlow J, et al. The prevalence of vertebral deformity in european men and women: The European Vertebral Osteoporosis Study. J Bone Miner Res. 1996;11:1010–1018. doi: 10.1002/jbmr.5650110719. [DOI] [PubMed] [Google Scholar]
- 4.Davies KM, Stegman MR, Heaney RP, et al. Prevalence and severity of vertebral fracture: The Saunders County Bone Quality Study. Osteoporos Int. 1996;6:106–165. doi: 10.1007/BF01623941. [DOI] [PubMed] [Google Scholar]
- 5.Melton LJ, III, Lane AW, Cooper C, et al. Prevalence and incidence of vertebral deformities. Osteoporos Int. 1993;3:113–119. doi: 10.1007/BF01623271. [DOI] [PubMed] [Google Scholar]
- 6.Spector TD, McCloskey EV, Doyle DV, et al. Prevalence of vertebral fracture in women and the relationship with bone density and symptoms: The Chingford Study. J Bone Miner Res. 1993;8:817–822. doi: 10.1002/jbmr.5650080707. [DOI] [PubMed] [Google Scholar]
- 7.Leech JA, Dulberg C, Kellie S, et al. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis. 1990;141:68–71. doi: 10.1164/ajrccm/141.1.68. [DOI] [PubMed] [Google Scholar]
- 8.DeSmet AA, Robinson RG, Johnson BE, et al. Spinal compression fractures in osteoporotic women: Patterns and relationship to hyperkyphosis. Radiology. 1988;166:497–500. doi: 10.1148/radiology.166.2.3336728. [DOI] [PubMed] [Google Scholar]
- 9.Ensrud KE, Black DM, Harris F, et al. Correlates of kyphosis in older women. J Am Geriatr Soc. 1997;45:682–687. doi: 10.1111/j.1532-5415.1997.tb01470.x. [DOI] [PubMed] [Google Scholar]
- 10.Schneider DL, von Muhlen D, Barrett-Connor E, et al. Kyphosis does not equal vertebral fractures: The Rancho Bernardo study. J Rheumatol. 2004;31:747–752. [PubMed] [Google Scholar]
- 11.Chow RK, Harrison JE. Relationship of kyphosis to physical fitness and bone mass on post-menopausal women. Am J Phys Med. 1987;66:219–227. [PubMed] [Google Scholar]
- 12.Ryan SD, Fried LP. The impact of kyphosis on daily functioning. J Am Geriatr Soc. 1997;45:1479–1486. doi: 10.1111/j.1532-5415.1997.tb03199.x. [DOI] [PubMed] [Google Scholar]
- 13.Kado DM, Huang MH, Barrett-Connor E, Greendale GA. Hyperkyphotic posture and poor physical functional ability in older community-dwelling men and women: The Rancho Bernardo study. J Gerontol A Biol Sci Med Sci. 2005;60:633–637. doi: 10.1093/gerona/60.5.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takahashi T, Ishida K, Hirose D, et al. Trunk deformity is associated with a reduction in outdoor activities of daily living and life satisfaction in community-dwelling older people. Osteoporosis Int. 2005;16:273–279. doi: 10.1007/s00198-004-1669-3. [DOI] [PubMed] [Google Scholar]
- 15.Miyakoshi N, Itoi E, Kobayashi M, Kodama H. Impact of postural deformities and spinal mobility on quality of life in postmenopausal osteoporosis. Osteoporos Int. 2003;14(12):1007–1012. doi: 10.1007/s00198-003-1510-4. [DOI] [PubMed] [Google Scholar]
- 16.McGrother CW, Donaldson MM, Clayton D, et al. Evaluation of a hip fracture risk score for assessing elderly women: The Melton Osteoporotic Fracture (MOF) study. Osteoporos Int. 2002;13(1):89–96. doi: 10.1007/s198-002-8343-6. [DOI] [PubMed] [Google Scholar]
- 17.Huang MHH, Barrett-Connor E, Greendale GA, et al. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res. 2006;21(3):419–423. doi: 10.1359/JBMR.051201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Milne JS, Lauder IJ. Age effects in kyphosis and lordosis in adults. Ann Hum Biol. 1974;1:327–337. doi: 10.1080/03014467400000351. [DOI] [PubMed] [Google Scholar]
- 19.Greendale GA, McDivit A, Carpenter A, et al. Yoga for women with hyperkyphosis: Results of a pilot study. Am J Public Health. 2002;92:1611–1614. doi: 10.2105/ajph.92.10.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milne JS, Lauder IJ. The relationship of kyphosis to the shape of vertebral bodies. Ann Human Biol. 1976;3:173–179. doi: 10.1080/03014467600001281. [DOI] [PubMed] [Google Scholar]
- 21.Hendry NG. The hydration of the nucleus pulposus and its relation to intervertebral disc hydration. J Bone Joint Surg. 1958;40:132–144. doi: 10.1302/0301-620X.40B1.132. [DOI] [PubMed] [Google Scholar]
- 22.Resnick D. Degenerative diseases of the vertebral column. Radiology. 1985;156:3–14. doi: 10.1148/radiology.156.1.3923556. [DOI] [PubMed] [Google Scholar]
- 23.Sinaki M, Itoi E, Rogers JW, et al. Correlation of back extensor strength with thoracic kyphosis and lumbar lordosis in estrogen-deficient women. Am J Phys Med Rehabil. 1996;75:370–374. doi: 10.1097/00002060-199609000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Milne JS, Williamson J. A longitudinal study of kyphosis in older people. Age Ageing. 1983;12(3):225–233. doi: 10.1093/ageing/12.3.225. [DOI] [PubMed] [Google Scholar]
- 25.Roaf R. Vertebral growth and its mechanical control. J Bone Joint Surg [BR] 1960;42:40–59. doi: 10.1302/0301-620X.42B1.40. [DOI] [PubMed] [Google Scholar]
- 26.Iyengar BKS. Light on Yoga. New York: Schocken Books; 1979. [Google Scholar]
- 27.Lundon KMA, Li AMWY, Bibershtein S. Interrater and intrarater reliability in the measurement of kyphosis in postmenopausal women with osteoporosis. Spine. 1988;23:1978–1985. doi: 10.1097/00007632-199809150-00013. [DOI] [PubMed] [Google Scholar]
- 28.Hinman MR. Comparison of thoracic kyphosis and postural stiffness in younger and older women. Spine J. 2004;4:413–417. doi: 10.1016/j.spinee.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 29.Foreman TK, Linge K. The importance of heel compression in the measurement of diurnal stature viation. Appl Ergon. 1989;20:299–300. doi: 10.1016/0003-6870(89)90194-4. [DOI] [PubMed] [Google Scholar]
- 30.Csuka M, McCarty DJ. Simple method for measurement of lower extremity muscle strength. Am J Med. 1985;78:77–81. doi: 10.1016/0002-9343(85)90465-6. [DOI] [PubMed] [Google Scholar]
- 31.Duncan PW, Studenski S, Chandler J, et al. Functional reach: Predictive validity in a sample of elderly male veterans. J Gerontol. 1992;47:M93–M98. doi: 10.1093/geronj/47.3.m93. [DOI] [PubMed] [Google Scholar]
- 32.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 33.Kado DM, Huang MH, Greendale GA, et al. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: A prospective study. JAGS. 2004;52:1662–1667. doi: 10.1111/j.1532-5415.2004.52458.x. [DOI] [PubMed] [Google Scholar]
- 34.Hays RD, Sherbourne CD, Mazel TM. The RAND 36-item health survey 1.0. Health Econ. 1993;2:217–227. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- 35.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 36.Peretz C, Herman T, Hausdorff JM, et al. Assessing fear of falling: Can a short version of the Activities-specific Balance Confidence scale be useful? Mov Disord. 2006;21(12):2101–2105. doi: 10.1002/mds.21113. [DOI] [PubMed] [Google Scholar]
- 37.Marcus RD, Greendale GA, Blunt BA, Bush TL, Sherman S, Sherwin R, Whaner H, Wells BH. Correlates of bone mineral density in the Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. J Bone Miner Res. 1994;9:1467–1476. doi: 10.1002/jbmr.5650090920. [DOI] [PubMed] [Google Scholar]
- 38.Greendale GA, Barrett-Connor E, Edelstein S, et al. Dietary sodium and bone mineral density: results of a 16-year follow-up study. J Am Geriatr Soc. 1994;42:1050–1055. doi: 10.1111/j.1532-5415.1994.tb06208.x. [Cited in the Nutrition Research Newsletter, November/December 1994] [DOI] [PubMed] [Google Scholar]
- 39.Greendale GA, Bodin-Dunn L, Ingles S, et al. Leisure, home and occupational physical activity and cardiovascular risk factors in postmenopausal women: the postmenopausal estrogen/progestins intervention (PEPI) study. Arch Intern Med. 1996;156:418–424. [PubMed] [Google Scholar]
- 40.Berk KN, Lachenbruch PA. Repeated measures with zeros. Stat Methods Med Res. 2002;11:303–316. doi: 10.1191/0962280202sm293ra. [DOI] [PubMed] [Google Scholar]
- 41.Evans DA, Beckett LA, Albert MS, et al. Level of education and change in cognitive function in a community population of older persons. Ann Epidemiol. 1993;3:71–77. doi: 10.1016/1047-2797(93)90012-s. [DOI] [PubMed] [Google Scholar]
- 42.Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley and Sons; 1987. [Google Scholar]
- 43.Ohlén G, Spangfort E, Tingvall G. Measurement of spinal sagital configuration and mobility with Debrummer’s kyphometer. Spine. 1989;14(6):580–583. doi: 10.1097/00007632-198906000-00006. [DOI] [PubMed] [Google Scholar]
- 44.Itoi E, Sinaki M. Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age. Mayo Clin Proc. 1994;69(11):1054–1059. doi: 10.1016/s0025-6196(12)61372-x. [DOI] [PubMed] [Google Scholar]
- 45.Katzman WB, Sellmeyer DE, Stewart AL, et al. Changes in flexed posture, musculoskeletal impairments, and physical performance after group exercise in community-dwelling older women. Arch Phys Med Rehabil. 2007;88:192–199. doi: 10.1016/j.apmr.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 46.Pfiefer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004;83(3):177–186. doi: 10.1097/01.phm.0000113403.16617.93. [DOI] [PubMed] [Google Scholar]
- 47.Hulme PA, Krebs J, Ferguson SJ, et al. Vertebroplasty and kyphoplasty: A systematic review of 69 clinical studies. SPINE. 2006;31(17):1983–2001. doi: 10.1097/01.brs.0000229254.89952.6b. [DOI] [PubMed] [Google Scholar]
- 48.Reuben DB, Frank JC, Hirsch SH, et al. A randomized clinical trial of outpatient comprehensive geriatric assessment coupled with an intervention to increase adherence to recommendations. J Am Geriatr Soc. 1999;47:269–276. doi: 10.1111/j.1532-5415.1999.tb02988.x. [DOI] [PubMed] [Google Scholar]
- 49.Tager IB, Swanson A, Satariano WA. Reliability of physical performance and self-reported functional measures in an older population. J Gerontol A Biol Sci Med Sci. 1998;53(4):M295–M300. doi: 10.1093/gerona/53a.4.m295. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.