Abstract
Background
The implementation of comprehensive smoke-free laws has been associated with reductions in second hand smoke exposure at home in several high income countries. There is little information on whether these benefits extend to low and middle income countries with growing tobacco related disease burden such as India.
Methods
State and individual level analysis of cross-sectional data from the Global Adult Tobacco Survey India, 2009/10. Associations between working in a smoke-free indoor environment and living in a smoke-free home was examined using correlation at the state level and multivariate logistic regression at the individual level.
Results
The percentage of respondents employed indoors (outside the home) working in smoke-free environments who lived in a smoke-free home was 64.0% compared with 41.7% of those that worked where smoking occurred. Indian states with higher proportions of smoke-free workplaces had higher proportions of smoke-free homes (rs=0.54, p<0.005). In the individual level analysis, working in a smoke-free workplace was associated with a significantly higher likelihood of living in a smoke-free home (adjusted odds ratio = 2.07; 95% CI: 1.64, 2.52) after adjustment for potential confounders.
Conclusions
Implementation of smoke-free legislation in India was associated with a higher proportion of adults reporting a smoke-free home. These findings further strengthen the case for accelerated implementation of Article 8 of the Framework Convention on Tobacco Control (FCTC) in low and middle income countries.
Keywords: smoke-free legislation, second hand smoke exposure, home, India
INTRODUCTION
In addition to widespread use of smokeless tobacco, India has one of the largest populations of smokers in the world. Findings from the 2009/10 Global Adult Tobacco Survey (GATS) indicate that there were 110 million smokers in the country, with 16% of males smoking bidis and 10% smoking cigarettes(1). Over half (52.3%) of adults report exposure to SHS at home, with marked state-level variation (9.9% to 96.5%)(1). Exposure to SHS is higher in rural than urban areas (58.0% vs. 38.5%) and in lower socio-economic status households. Exposure to second hand smoke (SHS) is the main cause of smoking-induced harm to women (who have very low rates of smoking) and children(2).
To protect non-smokers from SHS, India implemented national legislation (Section 4 of the Cigarettes and other Tobacco Product Act 2003) prohibiting smoking in public places and workplaces in October 2008(3). The law is not comprehensive as it permits designated smoking areas in large restaurants and hotels and the penalty for violations is modest (200 rupee fine – US $3.80). Enforcement of the legislation, which is a state government responsibility, varies between states, between urban and rural areas, and between occupational groupings(4). In 2009–10, 29.9% of adults reported being exposed to SHS at work nationally, varying from 15.4% in Chandigarh to 67.9% in Jammu & Kashmir(1).
In the United States(5), Ireland(6), and Scotland(7), the implementation of comprehensive smoke-free laws has been associated with reductions in SHS exposure in the home. These findings indicate that smoke-free laws may change social norms around exposing others to second hand smoke in private as well as public places. However, there is little information about whether these benefits extend to populous, low and middle income countries with growing tobacco induced disease burdens such as India. We examined the association between the implementation of smoke-free legislation in public places and SHS exposure at home in India in 2009–10.
METHODS
Sample and data
This study uses cross-sectional data from the Global Adult Tobacco Survey (GATS), which was conducted in India during 2009–2010. A detailed description of the survey objectives and methods can be found elsewhere(4). In brief, GATS is the global standard for systematically monitoring adult tobacco use and assessing the impact of key tobacco control policies. GATS India was a household survey of non-institutionalized men and women aged 15 years and above in all 29 states (including Delhi) and two Union Territories (UTs) of Chandigarh and Puducherry. The survey uses a multi-stage cluster random sampling design to produce nationally representative estimates of tobacco use and tobacco control indicators. The overall response rate to GATS India was 91.8%. The total sample size of GATS India was 69,296 individual respondents. The data include individual weight to ensure it is nationally representative.
For the purpose of the study, we analysed data on respondents to GATS India who reported working indoors or both indoors and outdoors, but outside their home (13,522 respondents). After removing respondents with missing values, in either dependent or independent variables, our final sample consisted of 12,561 respondents (92.9% of those who reported working indoors).
Variables
The dependent variable for our study is whether the respondent reported living in a smoke-free home (yes/no), based on whether they report “anyone” having smoked inside their home in the past 30 days. The independent variable is whether the respondent reported working at smoke-free environment (yes/no), based on whether they had seen anyone smoke in indoor area in the place that they work in the past 30 days.
We included the following variables as covariates: age (15–29, 30–44, 45–59, 60 years and above), gender, residence (rural, urban), geographical regions (north, central, east, north east, west, south), smoking status (current smoker, current non-smoker), smokeless tobacco use (current user, current non-user), education (no formal education, primary school completed, secondary school completed, higher secondary school completed, college/university and above), employment type (employee or self-employed), and number of people in the household. See Appendix 1 for detailed description and the definition for the variables used in this study.
Statistical analysis
We assessed the state level associations between the proportion of respondents working in a smoke-free environment and the proportion having a smoke-free home using the Spearman rank correlation coefficient.
We assessed the individual-level association between working in a smoke-free environment and living in a smoke-free home using multivariate logistic regression. Adjusted odds ratio (AOR) was calculated for respondents who worked in a smoke-free indoor environment compared with those in a work environment where smoking occurs. Our model includes demographic and socioeconomic covariates (age, sex, residence, geographic location, education and employment type) to reduce the risk of confounding. To examine whether the association between working in a smoke-free environment and living in a smoke-free home differed by respondent's smoking status, we stratified our sample into smokers and non-smokers and ran separate analysis for these two samples. We tested whether the association differs in rural/urban settings by including an interaction term between smoke-free workplace and geographical location.
We tested for multicollinearity for covariates controlled for in our analysis. The multicollinearity diagnostics (VIF) were all less than 5, indicating that the assumption of reasonable independence among predictor variables was met. Sampling weights were used to account for the complex, multi-stage design of the GATS survey. We performed the statistical analyses using Stata 11.0.
RESULTS
Three quarters (75.4%) of the 12,561 respondents who worked indoors outside the home were aged 45 years or younger and most were men (83.9%). 17.7% of respondents were current smokers. 69.7% of respondents who worked indoors reported that their workplace was smoke-free (Table 1). 57.2% of respondents reported that they live in smoke-free home.
Table 1.
Descriptive statistics for respondent characteristics
| Respondents who work indoors (n=12,561) |
|||
|---|---|---|---|
| Weighted proportion | Smoke-free at home (percentage with 95% CI) | ||
| Smoke-free at work | 69.7 | 64.0% (64.0, 64.0) | |
| SHS at work | 30.3 | 41.7% (41.7, 41.7) | |
|
| |||
| Age | 15–29 | 34.3 | 53.1% (53.1, 53.1) |
| 30–44 | 41.1 | 58.8% (58.8, 58.8) | |
| 45–59 | 20.0 | 59.9% (59.8, 59.9) | |
| 60 and above | 4.6 | 62.4% (62.4, 62.5) | |
|
| |||
| Gender | Male | 83.9 | 56.4% (56.4., 56.4) |
| Female | 16.1 | 61.7% (61.6, 61.7) | |
|
| |||
| Residence | Rural | 49.7 | 49.0% (48.9, 49.0) |
| Urban | 50.3 | 65.4% (65.4, 65.4) | |
|
| |||
| Geographical Regions | North | 7.3 | 49.2% (49.1, 49.2) |
| Central | 22.2 | 42.4% (42.3, 42.4) | |
| East | 17.5 | 47.0% (46.9, 47.0) | |
| North-East | 4.1 | 40.1% (40.0, 40.1) | |
| West | 19.1 | 61.2% (61.2, 61.2) | |
| South | 29.8 | 76.1% (76.1, 76.1) | |
|
| |||
| Smoking status | Current Smoker | 17.7 | 28.8% (28.8, 28.8) |
| Current non-smoker | 82.3 | 63.4% (63.4, 63.4) | |
|
| |||
| Smokeless Tobacco use | Current user | 25.4 | 38.8% (38.8, 38.9) |
| Current non-user | 74.6 | 63.5% (63.5, 63.5) | |
|
| |||
| Education | No formal education | 11.4 | 39.1% (39.1, 39.1) |
| Primary school completed | 19.6 | 47.1% (47.1, 47.2) | |
| Secondary school completed | 35.0 | 57.6% (57.6, 57.6) | |
| Higher secondary school completed | 11.3 | 62.3% (62.3, 62.3) | |
| College/University and above | 22.8 | 71.8% (71.8, 71.9) | |
|
| |||
| Occupation | Employee | 58.9 | 58.7% (58.7, 58.7) |
| Self-employed | 41.1 | 55.1% (55.1, 55.1) | |
Respondents who reported that their workplace was smoke-free were significantly more likely to live in smoke-free homes compared to those who are exposed to SHS at workplace (64.0% vs. 41.7%) (Table 1). Women were significantly more likely to report that their homes were smoke-free than men (61.7% vs. 56.4%). Respondents living in urban areas were significantly more likely to live in smoke-free homes compared with those living in rural areas (65.4% vs. 49.0%). Respondents with higher levels of education were significantly more likely to live in smoke-free homes (71.8% for those with college/university degree and 39.1% without formal education). Current smokers were significantly less likely to live in smoke-free home (28.8%) than non-smokers (63.4%).
Figure 1 shows the relationship between the percentage of respondents working in a smoke-free environment and the percentage having a smoke-free home for India's 31 states and union territories. States with a higher percentage of smoke-free workplaces had a higher percentage of smoke-free homes (rs=0.54, p<0.005).
Figure 1. State level association between smoke-free at work and smoke-free at home.
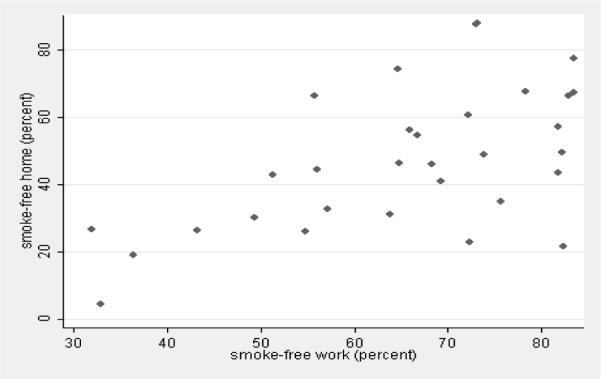
Note: Points represent averaged for each of 31 states and union territories (rs=0.54, p<0.005).
Working in a smoke-free environment was associated with a significantly higher likelihood of living in a smoke-free home (adjusted odds ratio = 2.07; 95% CI: 1.64, 2.62) in the individual level analysis (Table 2). This association persisted in the analysis stratified by smoking status for both smokers (AOR=2.21; 95% CI=1.84, 2.65) and non-smokers (AOR=1.60; 95% CI=1.13, 2.28). The association between working in a smoke-free workplace and living in a smoke-free home did not differ in rural and urban areas (p=0.298 for the interaction term).
Table 2.
Predictors of smoke-free home (multivariate logistic regression analysis)
| Adjusted Odds Ratio | 95% CI | P-value | VIF | |
|---|---|---|---|---|
| Smoke-free at workplace | 2.07 | (1.64, 2.62) | 0.0005 | 1.13 |
| Age | 1.02 | (1.01, 1.03) | 0.0005 | 1.05 |
| Gender (male as reference group) | ||||
| Female | 0.66 | (0.55, 0.79) | 0.0005 | 1.13 |
| Residence (rural as reference group) | ||||
| Urban | 1.54 | (1.29, 1.85) | 0.0005 | 1.18 |
| Geographical Regions (North as reference group) | ||||
| Central | 0.97 | (0.41, 2.27) | 0.942 | 1.28 |
| East | 1.44 | (0.61, 3.40) | 0.407 | 1.36 |
| Northeast | 1.13 | (0.48, 2.62) | 0.783 | 1.68 |
| West | 1.69 | (0.68, 4.20) | 0.261 | 1.43 |
| South | 4.27 | (1.45, 12.60) | 0.009 | 1.57 |
| Smoking status (current non-smoker as reference group) | ||||
| Current smoker | 0.22 | (0.16, 0.31) | 0.0005 | 1.28 |
| Smokeless tobacco use (Current non-user as reference group) | ||||
| Current user | 0.56 | (0.46, 0.68) | 0.0005 | 1.19 |
| Education (secondary school completed as reference group) | ||||
| No formal education | 0.52 | (0.37, 0.73) | 0.0005 | 1.25 |
| Primary school | 0.75 | (0.59, 0.96) | 0.024 | 1.30 |
| Higher secondary school | 1.23 | (0.96, 1.56) | 0.101 | 1.22 |
| College/University and above | 1.51 | (1.29, 1.75) | 0.0005 | 1.47 |
| Occupation (employee as reference group) | ||||
| Self-employed | 1.03 | (0.86, 1.22) | 0.776 | 1.12 |
| Number of people in household | 0.96 | (0.94, 0.99) | 0.001 | 1.05 |
Women were significantly less likely to live in a smoke-free home than men (AOR=0.66; 95% CI: 0.55, 0.79). Respondents living in urban areas were significantly more likely to live in smoke-free home than those in rural areas (AOR=1.54; 95% CI: 1.29, 1.85). Respondents with higher levels of education were significantly more likely to live in a smoke-free home. Current smokers were significantly less likely to live in a smoke-free home than non-smokers (AOR=0.22; 95% CI: 0.16, 0.31). The odds of living in a smoke-free home decreased with an increase in the number of household members (AOR=0.96; 95% CI: 0.94, 0.99 for each additional household member).
DISCUSSION
Implementation of smoke-free legislation in India was associated with a higher proportion of adults reporting smoke-free homes. These findings are consistent with previous studies conducted in high income countries including the United States(5), Scotland(7), Ireland(6), Wales, and New Zealand(8). For example, using a national representative sample in the United States, Cheng et al(5) found that people living in counties with comprehensive smoke-free legislation (covering workplaces, restaurants and bars) are seven times more likely to have smoke-free homes than those live in counties with no smoke-free laws. One study(9) from Hong Kong reported smoking displacement into the home following the introduction of smoke-free legislation, which the authors attributed to the typical urban high-rise living in Hong Kong. Our results show that India is more like the other, richer countries.
Our findings provide support for arguments of “norm spreading” whereby restrictions on smoking in public places reduces acceptability of exposing others to SHS more generally, including in the home(5, 7, 10). They provide evidence against “behavioural compensating” which argues that smoke-free legislation may displace smoking from public to private places(11).
Strength and Limitations
Our findings are based on a large, representative survey population which provides robust national level estimates of our key variables. The GATS survey is the global standard for monitoring the impact of key tobacco control policies. Limitations of the study include a reliance on self-reported measures for SHS exposure at work and home and smoking status, which is common in studies using cross-sectional survey data. There is evidence, however, that self-reported exposure to second hand smoking correlates well with objective measures, including cotinine measurement (12). The cross-sectional study design of the GATS limits causal interpretation of our findings. Poorer surveillance of tobacco use in low and middle income countries means that more robust pre-post or longitudinal study designs, such as those used in high income countries to examine this association, cannot yet be employed. In the absence of data on smoke-free homes prior to the implementation of the legislation, we cannot assert that smoke-free legislation at workplace causes increases in voluntary adoption of smoke-free practices at home. However, we were able to control for a large number of potentially confounding factors, including education, gender, smoking status and geographical location. The association between working in a smoke-free workplace and living in a smoke-free home was similar in rural and urban areas. However, due to differences in housing type in India, this may not translate into similar reductions in SHS exposure. Elimination of smoking inside modern urban dwellings, which are generally sealed with air conditioning, is likely to reduce SHS exposure to a greater extent than doing so in urban slum housing or housing in rural areas (where an outdoor “patio” is common) which are generally not sealed.
Conclusion
Our findings suggest that the implementation of smoke-free legislation in India may have resulted in substantial population health benefits. Associated reductions in SHS exposure in high income countries have led to well documented decreases in hospital admissions for asthma (in both children and adults)(13, 14), myocardial infarction, stroke and other cardiovascular events(15–21). Furthermore, these health benefits appear to accrue equally in affluent and poorer sections of society(22). This is important in India given growing evidence of the socio-economic patterning of tobacco use and tobacco related harm(23). Additional benefits will accumulate if the legislation has been successful in reducing smoking prevalence, something that should be examined in future research(24).
Achieving sustained and equitable reductions in SHS exposure is a high public health priority for India. Our findings highlight the importance of accelerating the implementation of existing national tobacco control legislation on smoke-free public places (Section 4 of the Cigarettes and Other Tobacco Products Act 2003) building on earlier successes in achieving smoke-free environments(25–28). This may require additional resources for states, which hold responsibility for enforcing the legislation, to strengthen compliance, particularly in rural areas and poorer communities. Consideration should also be given to increasing the fine for non-compliance (currently 200 Indian rupees) and removing existing provisions for designated smoking rooms in larger restaurants and hotels which are inconsistent with Article 8 of the Framework Convention for Tobacco Control (FCTC). Addressing variations in enforcement between rural and urban areas and between workplaces employing different occupational groups is important to ensure that associated health benefits of smoke-free laws are equitably distributed(4). Increasing awareness about the dangers of SHS through mass media campaigns and health professional advice remains important, particularly in rural areas and low SES groups who have high exposure(29).
What this study adds.
Implementation of smoke-free legislation in India was associated with a higher proportion of adults reporting smoke-free homes. Our findings provide support for arguments of “norm spreading” whereby restrictions on smoking in public places reduces acceptability of exposing others to SHS more generally, including in the home. Our findings highlight the importance of accelerating the implementation of existing national tobacco control legislation on smoke-free public places in India.
Acknowledgements
We are grateful for three anonymous referees for helpful comments.
Funding Funding for the GATS is provided by the Bloomberg initiative to reduce tobacco use, a program of Bloomberg Philanthropies.
There was no dedicated funding for this study. CM is funded by the Higher Education Funding Council for England and the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care scheme. SAG is American Legacy Foundation Distinguished Professor in Tobacco Control; his work on this project was also supported by National Cancer Institute Grant CA-61021. The Department of Primary Care & Public Health at Imperial College is grateful for support from the National Institute for Health Research Biomedical Research Centre Funding scheme, the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care scheme, and the Imperial Centre for Patient Safety and Service Quality. SA is supported by a Wellcome Trust Strategic Award Grant No Z/041825.
Appendix 1.
Dependent and independent variable definitions
| Variable | Definition |
|---|---|
| Smoke-free home | Respondent who is living under smoke-free home are defined as those who reported “never” to the following question: How often does “anyone” smoke inside your home? This does not include areas outside such as patios, balcony, garden, etc. that are not fully enclosed. |
|
Smoke-free workplace |
Respondent who is working in smoke-free workplace are defined as those who are not exposed to SHS at workplace. Individual who is exposed to SHS at workplace are those who answered yes to the following question: during the past 30 days, did anyone smoke in indoor areas where you work. This is among respondents who work outside the home and usually work indoors or both indoors and outdoors. |
|
Current tobacco smoker |
Person who currently smokes any tobacco product, either daily or occasionally. Smoking tobacco products include bidis, manufactured and hand-rolled cigarettes, pipes, cigars, hookah, water pipes, and other locally produced smoking tobacco products, e.g. chuttas, dhumti and chillum. |
|
Current smokeless tobacco user |
Person who currently uses any smokeless tobacco product, either daily or occasionally. Smokeless tobacco product include chewing tobacco products, such as, betel quid with tobacco, khaini, gutkha, paan masala, and other products like mishri, mawa, gul, bajjar, gudakhu, snuff, etc. |
|
Number of people in the household |
Indicates how many people live in the household of the respondent. This is the answer to the following question “in total, how many persons are living in this household?” |
| Age | Respondent's age |
| Gender | Respondent's gender |
| Education | Answer to the question “highest level of education”. Categorised into five levels (1) no formal education (2) primary school completed (includes answer “less than primary school completed”, “primary school completed”) (3) secondary school (includes answer less than secondary school completed, secondary school completed, (4) Higher secondary school completed (5) College/university and above (includes college/university completed, and post-graduate degree completed) |
| Occupation | Defined as respondents' occupation in last 12 months. Categorised into two categories (1) employee (include those answer government employee, and non- government employee) (2) self-employed. |
Footnotes
Ethical approval Not required
Contributors and sources CM conceived the article. JTL conducted and CM, SAG supervised the statistical analysis. JTL and CM wrote the paper and SA, SB and SAG revised it for important intellectual content.
REFERENCES
- 1.World Health Organization WHO report on the global tobacco epidemic. 2011 http://www.who.int/tobacco/global_report/2011/en/index.html.
- 2.Öberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. The Lancet. 377(9760):139–46. doi: 10.1016/S0140-6736(10)61388-8. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz R, Wipfli H, Samet J. World No Tobacco Day 2011: India's progress in implementing the framework convention on tobacco control. Indian J Med Res. 2011;133(5):455–7. [PMC free article] [PubMed] [Google Scholar]
- 4.International Institute for Population Sciences (IIPS) Global Adult Tobacco Survey India (GATS India) 2009–2010. Ministry of Health and Family Welfare, Government of India; New Delhi, India: 2010. [Google Scholar]
- 5.Cheng K-W, Glantz SA, Lightwood JM. Association Between Smokefree Laws and Voluntary Smokefree-Home Rules. American Journal of Preventive Medicine. 2011;41(6):566–72. doi: 10.1016/j.amepre.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fong GT, Hyland A, Borland R, Hammond D, Hastings G, McNeill A, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK Survey. Tobacco Control. 2006;15(suppl 3):iii51–iii8. doi: 10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akhtar PC, Currie DB, Currie CE, Haw SJ. Changes in child exposure to environmental tobacco smoke (CHETS) study after implementation of smoke-free legislation in Scotland: national cross sectional survey. BMJ. 2007;335(7619):545. doi: 10.1136/bmj.39311.550197.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edwards R, Thomson G, Wilson N, Waa A, Bullen C, O'Dea D, et al. After the smoke has cleared: evaluation of the impact of a new national smoke-free law in New Zealand. Tobacco Control. 2008;17(1):e2. doi: 10.1136/tc.2007.020347. [DOI] [PubMed] [Google Scholar]
- 9.Ho SY, Wang MP, Lo WS, Mak KK, Lai HK, Thomas GN, et al. Comprehensive smoke-free legislation and displacement of smoking into the homes of young children in Hong Kong. Tobacco Control. 2010;19(2):129–33. doi: 10.1136/tc.2009.032003. [DOI] [PubMed] [Google Scholar]
- 10.Mons U, Nagelhout GE, Allwright S, Guignard R, van den Putte B, Willemsen MC, et al. Impact of national smoke-free legislation on home smoking bans: findings from the International Tobacco Control Policy Evaluation Project Europe Surveys. Tobacco Control. 2012 doi: 10.1136/tobaccocontrol-2011-050131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adda J, Cornaglia F. The Effect of Bans and Taxes on Passive Smoking. American Economic Journal: Applied Economics. 2010;2(1):1–32. [Google Scholar]
- 12.Okoli CTC, Kelly T, Hahn EJ. Secondhand smoke and nicotine exposure: A brief review. Addictive Behaviors. 2007;32(10):1977–88. doi: 10.1016/j.addbeh.2006.12.024. [DOI] [PubMed] [Google Scholar]
- 13.Mackay D, Haw S, Ayres JG, Fischbacher C, Pell JP. Smoke-free Legislation and Hospitalizations for Childhood Asthma. New England Journal of Medicine. 2010;363(12):1139–45. doi: 10.1056/NEJMoa1002861. [DOI] [PubMed] [Google Scholar]
- 14.Millett C, Lee JT, Laverty AA, Glantz SA, Majeed A. Hospital Admissions for Childhood Asthma After Smoke-Free Legislation in England. Pediatrics. 2013 doi: 10.1542/peds.2012-2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sims M, Maxwell R, Bauld L, Gilmore A. Short term impact of smoke-free legislation in England: retrospective analysis of hospital admissions for myocardial infarction. BMJ. 2010;340 doi: 10.1136/bmj.c2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sebrié EM, Sandoya E, Hyland A, Bianco E, Glantz SA, Cummings KM. Hospital admissions for acute myocardial infarction before and after implementation of a comprehensive smoke-free policy in Uruguay. Tobacco Control. 2012 doi: 10.1136/tobaccocontrol-2011-050134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pell JP, Haw S, Cobbe S, Newby DE, Pell ACH, Fischbacher C, et al. Smoke-free Legislation and Hospitalizations for Acute Coronary Syndrome. New England Journal of Medicine. 2008;359(5):482–91. doi: 10.1056/NEJMsa0706740. [DOI] [PubMed] [Google Scholar]
- 18.Sargent RP, Shepard RM, Glantz SA. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study. BMJ. 2004;328(7446):977–80. doi: 10.1136/bmj.38055.715683.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naiman A, Glazier RH, Moineddin R. Association of anti-smoking legislation with rates of hospital admission for cardiovascular and respiratory conditions. Canadian Medical Association Journal. 2010;182(8):761–7. doi: 10.1503/cmaj.091130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herman PM, Walsh ME. Hospital Admissions for Acute Myocardial Infarction, Angina, Stroke, and Asthma After Implementation of Arizona's Comprehensive Statewide Smoking Ban. American Journal of Public Health. 2011;101(3):491–6. doi: 10.2105/AJPH.2009.179572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hahn EJ. Smokefree Legislation: A Review of Health and Economic Outcomes Research. American Journal of Preventive Medicine. 2010;39(6, Supplement 1):S66–S76. doi: 10.1016/j.amepre.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 22.Akhtar PC, Haw SJ, Levin KA, Currie DB, Zachary R, Currie CE. Socioeconomic differences in second-hand smoke exposure among children in Scotland after introduction of the smoke-free legislation. Journal of Epidemiology and Community Health. 2010;64(4):341–6. doi: 10.1136/jech.2008.084178. [DOI] [PubMed] [Google Scholar]
- 23.Sorensen G, Gupta PC, Pednekar MS. Social Disparities in Tobacco Use in Mumbai, India: The Roles of Occupation, Education, and Gender. American Journal of Public Health. 2005;95(6):1003–8. doi: 10.2105/AJPH.2004.045039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ. 2002;325(7357):188. doi: 10.1136/bmj.325.7357.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sinha D. Report on Global Youth Tobacco Survey (GYTS) 2002, Uttar Pradesh, India. Accessed from http://www.searo.who.int/LinkFiles/GYTS_Rep_UttarPradesh_2002.pdf in April 2012.
- 26.Sinha DN, Gupta PC, Warren CW, Asma S. Effect of School Policy on Tobacco Use by School Personnel in Bihar, India. Journal of School Health. 2004;74(1):3–5. doi: 10.1111/j.1746-1561.2004.tb06592.x. [DOI] [PubMed] [Google Scholar]
- 27.Bhandari U. A tobacco-free town. World Health Forum. 1998;19(301) [PubMed] [Google Scholar]
- 28.Tobacco News and Information Smoking ban on south's trains. Available from URL: http://www.tobacco.org/news/164057.html.
- 29.King BA, Mirza SA, Babb SD, Group ftGC. A cross-country comparison of secondhand smoke exposure among adults: findings from the Global Adult Tobacco Survey (GATS) Tobacco Control. 2012 doi: 10.1136/tobaccocontrol-2012-050582. [DOI] [PMC free article] [PubMed] [Google Scholar]


